Documentos de Académico
Documentos de Profesional
Documentos de Cultura
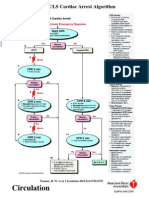
Advanced Cardiac Life Support Information From American Heart Association, Advanced Cardiac Life Support, 2006
Cargado por
karento10 calificaciones0% encontró este documento útil (0 votos)
97 vistas25 páginasTítulo original
Advanced_Cardiac_Life_SupportPP
Derechos de autor
© Attribution Non-Commercial (BY-NC)
Formatos disponibles
PPT, PDF, TXT o lea en línea desde Scribd
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Attribution Non-Commercial (BY-NC)
Formatos disponibles
Descargue como PPT, PDF, TXT o lea en línea desde Scribd
0 calificaciones0% encontró este documento útil (0 votos)
97 vistas25 páginasAdvanced Cardiac Life Support Information From American Heart Association, Advanced Cardiac Life Support, 2006
Cargado por
karento1Copyright:
Attribution Non-Commercial (BY-NC)
Formatos disponibles
Descargue como PPT, PDF, TXT o lea en línea desde Scribd
Está en la página 1de 25
Advanced Cardiac Life Support
Information from American Heart
Association, Advanced Cardiac
Life Support, 2006
By Cynthia Grice, R.N.,
M.S.N.
Establish unresponsiveness, not
breathing and pulselessness.
Begin CPR per BCLS standards
Respiratory Arrest
Both BCLS and ACLS interventions
Give O2
Open airway
Provide basic ventilation
Use airway if needed
Suctioning
Intubate if needed
Give 1 breath every 5-6 seconds
Hyperventilation can be harmful because it increases
intrathoracic pressure, decreases venous return to the
heart, and diminishes cardiac output. It may also
increase gastric inflation and predispose the patient to
vomiting and aspiration of gastric contents
Resp. arrest cont’d
During CPR the compression to
ventilation ratio is 30:2. But once an
advanced airway is in place, chest
compressions are no longer interrupted
for ventilations.
With ETT in place, give 1 breath every 6-
8 seconds approximately 10 breaths per
minute
Circulation
Check the patient’s carotid pulse for 5-10
seconds
If no pulse, start compressions 30:2 ratio
Perform chest compressions at a depth of
1 1/2 to 2 inches at a rate of 100/minute
Defibrillation
Defibrillation does not restart the heart.
Defibrillation stuns the heart and briefly
terminates all electrical activity, including VF
and VT. If the heart is still viable, its normal
pacemakers may eventually resume electrical
activity, return of spontaneous rhythm, that
ultimately results in a perfusing rhythm. In the
first few minutes after successful defibrillation,
however, any spontaneous rhythm is typically
slow and does not create pulses or perfusion.
CPR is needed for several minutes until
adequate heart function resumes. This is the
rationale for resuming immediate high quality
chest compressions after a shock.
Defibrillation
The earlier defibrillation occurs, the
higher the survival rate. When VF is
present, CPR can provide a small amount
of blood flow to the heart and brain but
cannot directly restore an organized
rhythm. Restoration of a perfusing
rhythm requires immediate CPR and
defibrillation within few minutes of the
initial arrest.
Be familiar with the AED
Defibrillation
Monophasic- defibrillate at 360 volts
Biphasic-defibrillate at 150 volts
Defib V tac or V fib
Give epinephrine, may also give
amiodarone
Defib and continue CPR in between
Stop for a few seconds, no more than 10,
if a rhythm is seen to feel for a pulse
May also give atropine or vasopressin
If acidotic give HCO3
Drugs-Vasopressors
Epinephrine 1mg IV/IO-repeat every 3-
5 minutes OR
Vasopressin 40 U IV/IO- may
substitute for the first or second dose
of epinephrine
Epinephrine may be given down the
ETT tube in there is no IV/IO access
1:1000, 2 to 2.5mg diluted in 5-10 ml
of NS injected into the ET tube
Epinephrine
Epinephrine Hydrochloride is used during
resuscitation primarily for its adrenergic
effects, ie, vasoconstriction.
Vasoconstriction increases cerebral and
coronary blood flow during CPR as mean
arterial pressure and aortic diastolic pressure
are increased.
Stimulates adrenergic receptors, producing
vasoconstriction, increasing blood pressure
and heart rate, and improving perfusion
pressure to the brain and heart.
Repeat epinephrine 1mg IV/IO every 3 to 5
minutes during cardiac arrest
Vasopressin
A nonadrenergic peripheral
vasoconstrictor. Overall, vasopressin
effects have not been shown to differ
from epinephrine.
Causes coronary and renal
vasoconstriction.
Dose 40 U IV/IO
Anticoagulents
Aspirin and Plavix are both antiplatlets or
prevent platlet aggregation
Heparin and coumadin are anticoagulents
Monitor heparin with APTT
Monitor coumadin with INR and PT
Antiarrhythmic Agents
Amiodarone
Magnesium sulfate
Lidocaine
Amiodarone
Consider amiodarone for treatment of VF or
pulseless VT unresponsive to shock delivery,
CPR, and a vasopressor. Amiodarone is a
complex drug that affects potassium, and
calcium channels. It also has adrenergic and B-
adrenergic blocking properties. Amiodarone is
available in vials and prefilled syringes. During
cardiac arrest amiodarone 300mg IV/IO push
for the first dose. If VF/pulseless VT persists,
consider giving a second dose of 150mg IV/IO
in 3-5 minutes.
Postresuscitation Maintenance
Therapy
Amiodarone for recurrent VF/VT:
Maximum cumulative dose: 2.2g over 24 hours
Start with IV bolus of 150 mg IV over 10 minutes
Follow by slow infusion of 360mg IV over the next 6
hours: 1mg/min.
Then a maintenance infusion of 540 mg IV over the
next 18 hours: 0.5 mg/min
The arrest dose is 300 mg IV/IO, repeated once if
necessary at 150mg IV/IO. If the drug has been given
during cardiac arrest, start infusion as indicated. May
give one 150mg IV bolus for recurrent VF/VT; then
seek expert consultation
Monitor for hypotension bradycardia and
gastrointestinal toxicity
Lidocaine
Lidocaine is an alternative antiarrhythmic of
long standing and widespread familarity. It has
no proven short term or long term efficacy in
cardiac arrest. Lidocaine is still included as an
alternative to amiodarone in settings where
amiodarone is not available.
Give lidocaine in a dose of 1 to 1.5 mg/kg
IV/IO. Repeat if indicated at 0.5 to 0.75 mg/kg
IV/IO over 5 to 10 minute intervals to a
maximum of 3 doses or 3mg/kg. If IV/IO
access is available, then the dose for ET
administration is 2 to 4 mg/kg.
Postresuscitation Maintenance
Therapy
If the patient has not received lidocaine during
the arrest:
Start with a loading dose of 1 to 1.5 mg/kg
every 5 to 10 minutes if needed to a total of 3
mg/kg
Follow with a continuous infusion of 1 to 4
mg/min.
If the drug has been used during cardiac
arrest, start infusion as indicated. May give
additional bolus for recurrent VF or VT up to 3
mg/kg; seek expert consultation.
Magnesium Sulfate
IV magnesium may terminate or prevent recurrent torsades de
pointes in patients who have a prolonged QT interval during
normal sinus rhythm. When VF/pulseless VT cardiac arrest is
associated with torsades de pointes, give magnesium sulfate at a
loading dose of 1 to 2 g IV/IO diluted in 10 ml D5W given over 5
to 20 minutes. If a prearrest 12 lead EKG is available for review.
Check the QT interval for prolongation. Remember that pulseless
VT is treated with an immediate high-energy shock, whereas
magnesium is an adjunctive agent to prevent recurrent or treat
persistent VT associated with torsades de pointes.
Magnesium sulfate is alos indicated for patients with known or
suspected low serum magnesium, such as patients with alcoholism
or other conditions associated with malnutrition or
hypomagnesemic states. For patients in refractory VF pulseless
VT, check the patient for history, if available, for one of these
conditions that suggest the presence of a reversible electrolyte
abnormality.
Pulseless Arrest
Initiate high quality CPR, check every 10
seconds for a pulse, advanced airway
placement
As soon as IV/IO access available give a
vasopressor: Epinephrine 1mg IV/IO repeat
every 3 to 5 minutes OR
Vasopressin 40 U IV/IO to replace first or
second dose of epinephrine
Give vasopressin only once.
If PEA is slow give Atropine 1 mg IV/IO, may
repeat every 3 to 5 minutes up to 3 doses
If still no pulse, continue CPR and epinephrine
Pulseless Electrical Activity (PEA)
Patients with PEA have poor outcomes. Rapid
assessments and aggressive management offer
the best chance of success. PEA may be
caused by a reversible problem. If you can
quickly identify a specific condition that has
caused or is contributing to PEA and correct it,
you may achieve resuscitation.
Consider frequent causes of PEA by recalling
the H’s and T’s
Analyze EKG for clues to the underlying cause
Recognize hypovolemia
Recognize drug overdose/poisonings
H’s
Hypovolemia
Hypoxia
Hydrogen ion ( acidosis)
Hyper/hypokalemia
Hypoglycemia
Hypothermia
T’s
Toxins
Tamponade (cardiac)
Tension pneumothorax
Thrombosis (coronary and pulmonary)
Trauma
Terminating Resuscitative Efforts
If a reversible cause is not rapidly identified and the
patient fails to responds to the BLS Primary Survey and
the ACLS Secondary Survey management, termination
of resuscitative efforts may be appropriate. The
decision to terminate resuscitative efforts rests with the
treating physician in the hospital and is based on
consideration of many factors including:
Time to CPR
Time to defibrillation
Comorbid disease
Prearrest state
Initial arrest rhythm
Response to resuscitative measures
Acute Coronary Syndromes
Unstable plaque
Plaque rupture
Unstable angina
Microemboli
Occlusive thrombus
Treat with O2, aspirin, nitroglycerin,
morphine, TPA Heparin/levenox, beta
blockers, plavix, ACE inhibitors, statin
therapy-lipitor, etc. Remember that
morphine is a venodilator
Critical time period for TPA for CVA
The critical time period for administration of
intravenous fibrinolytic therapy begins with the
onset of symptoms.
Immediate general assessment 10min.
Immediate neurologic assessment 25 min
CT of head 25 min
Interpretation of CT of head 45 min
Admin of TPA, timed from ED arrival 60 min
Admin. Of TPA, timed from onset of symptoms
3 hours
Admission to ICU 3 hours
También podría gustarte
- NCM 118B Emergency MedicationsDocumento110 páginasNCM 118B Emergency MedicationsJan Crizza Dale R. FrancoAún no hay calificaciones
- Management of Symptomatic Bradycardia and TachycardiaDocumento55 páginasManagement of Symptomatic Bradycardia and TachycardiaDewintha Airene NoviantiAún no hay calificaciones
- Cardiorespiratory ArrestDocumento51 páginasCardiorespiratory ArrestIrham KhairiAún no hay calificaciones
- Drugs in CPR - M.H.farjooDocumento37 páginasDrugs in CPR - M.H.farjooAnonymous 34umhBmBEAún no hay calificaciones
- Unit 5 Cardiac Emergencies: StructureDocumento27 páginasUnit 5 Cardiac Emergencies: StructurebtaleraAún no hay calificaciones
- Saudi CPR Guidlines in EnglishDocumento16 páginasSaudi CPR Guidlines in EnglishpiyushbamsAún no hay calificaciones
- 099 B SaroshDocumento14 páginas099 B SaroshUmair AnsariAún no hay calificaciones
- Emergency Drugs: Vasoppressors - Recommended by AHADocumento4 páginasEmergency Drugs: Vasoppressors - Recommended by AHAJaffy EspirituAún no hay calificaciones
- Epinephrine and other emergency drug doses and indicationsDocumento5 páginasEpinephrine and other emergency drug doses and indicationsColette Marie PerezAún no hay calificaciones
- Handbook of AnesthesiologyDocumento176 páginasHandbook of AnesthesiologyarmelzahfauziAún no hay calificaciones
- A (ACLS) - 2015: Dvanced Cardiac Life SupportDocumento52 páginasA (ACLS) - 2015: Dvanced Cardiac Life SupportNajmussaqibAún no hay calificaciones
- Emergency Medicine 1st Edition - DR - Waleed (101 Papers)Documento101 páginasEmergency Medicine 1st Edition - DR - Waleed (101 Papers)Mokhtar Moh100% (1)
- Emergency Oxygen Therapy for Cardiac IssuesDocumento11 páginasEmergency Oxygen Therapy for Cardiac IssuesMin Hong LuoAún no hay calificaciones
- Drugs Given During Cardiac Arres For CPRDocumento5 páginasDrugs Given During Cardiac Arres For CPREevyaj MimiAún no hay calificaciones
- Adult Advanced Life Support2Documento34 páginasAdult Advanced Life Support2drDilanAún no hay calificaciones
- Advanced Cardiac Life Support RC 275Documento40 páginasAdvanced Cardiac Life Support RC 275Rika Hardiyanti PagalaAún no hay calificaciones
- Dvanced Cardiac Life SupportDocumento72 páginasDvanced Cardiac Life Supportolivia100% (1)
- Advance Cardiac SuppDocumento32 páginasAdvance Cardiac SuppVijith.V.kumarAún no hay calificaciones
- FarmakologiDocumento69 páginasFarmakologikekeyirawanAún no hay calificaciones
- Acls STUDY GUIDE 2017Documento19 páginasAcls STUDY GUIDE 2017jamesomooreAún no hay calificaciones
- Current Clinical Strategies: Handbook of AnesthesiologyDocumento180 páginasCurrent Clinical Strategies: Handbook of AnesthesiologydramaganaAún no hay calificaciones
- ACLS Class Packet PDFDocumento9 páginasACLS Class Packet PDFImam GultomAún no hay calificaciones
- DEFIBrilatorDocumento43 páginasDEFIBrilatoranon_632568468Aún no hay calificaciones
- Basic Life SupportDocumento6 páginasBasic Life SupportbhongskirnAún no hay calificaciones
- Cardiac ArrestDocumento14 páginasCardiac ArrestCloudySkyAún no hay calificaciones
- Advanced Cardiac Life Support (ACLS) : By: Diana Blum MSN Metropolitan Community College Nursing 2150Documento16 páginasAdvanced Cardiac Life Support (ACLS) : By: Diana Blum MSN Metropolitan Community College Nursing 2150Vikneswara SoorianarayananAún no hay calificaciones
- Emergency Drug Therapy 1ceuDocumento7 páginasEmergency Drug Therapy 1ceuRN333Aún no hay calificaciones
- Pediatric Life SupportDocumento33 páginasPediatric Life SupportAndre montolaluAún no hay calificaciones
- Acls Pharmacology OverviewDocumento11 páginasAcls Pharmacology OverviewzoyaligAún no hay calificaciones
- 2014 February ALS Cardiac Arrest and ROSCDocumento37 páginas2014 February ALS Cardiac Arrest and ROSCAuliaFadhilahTasruddinAún no hay calificaciones
- Emergency Drug Review: UHHS BMH Paramedic Training ProgramDocumento116 páginasEmergency Drug Review: UHHS BMH Paramedic Training ProgramShailja HanumantaAún no hay calificaciones
- Lecture - 2 Advanced Cardiac Life SupportDocumento28 páginasLecture - 2 Advanced Cardiac Life SupportJixon GeorgeAún no hay calificaciones
- How To Stop Paroxysm of SVT and AF at Home and in HospitalDocumento35 páginasHow To Stop Paroxysm of SVT and AF at Home and in HospitalOlga Goryacheva100% (1)
- ACLS-Pediatric Wide Complex Tachycardia: Sample Medical GuidelinesDocumento2 páginasACLS-Pediatric Wide Complex Tachycardia: Sample Medical GuidelinesFebrialitaFatoniAún no hay calificaciones
- ACLS Drugs: Primary Medications Used in Cardiac Arrest AlgorithmsDocumento10 páginasACLS Drugs: Primary Medications Used in Cardiac Arrest AlgorithmsChintami Octavia100% (1)
- Cardiac ArrestDocumento30 páginasCardiac ArrestagnescheruseryAún no hay calificaciones
- Bradycardia and Tachycardia Treatment OptionsDocumento31 páginasBradycardia and Tachycardia Treatment OptionscmirceaAún no hay calificaciones
- 3 Pulseless Arrest - Non-Shockable RhythmsDocumento29 páginas3 Pulseless Arrest - Non-Shockable RhythmsTejas Vivek WaghAún no hay calificaciones
- PBLS - Pediatric Basic Life Support and Pediatric Advance Cardiac Life SupportDocumento135 páginasPBLS - Pediatric Basic Life Support and Pediatric Advance Cardiac Life SupportSteffiAún no hay calificaciones
- Assessment of The Acutely Ill PatientDocumento10 páginasAssessment of The Acutely Ill PatientZacmilo Dela TorreAún no hay calificaciones
- Cals ReviewbjvjvjDocumento14 páginasCals ReviewbjvjvjCarl Jay M Ocariza100% (1)
- Chapter3Shock CirculationDocumento13 páginasChapter3Shock CirculationSri AgustinaAún no hay calificaciones
- Acls Drug OverviewDocumento2 páginasAcls Drug OverviewBruce Abramowitz100% (1)
- Advanced Cardiac Life Support PDFDocumento9 páginasAdvanced Cardiac Life Support PDFYulias YoweiAún no hay calificaciones
- Atrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesDe EverandAtrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesCalificación: 4 de 5 estrellas4/5 (1)
- Mitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsDe EverandMitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsAún no hay calificaciones
- Advanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesDe EverandAdvanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesCalificación: 4 de 5 estrellas4/5 (6)
- Pacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe EverandPacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAún no hay calificaciones
- The Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?De EverandThe Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?Aún no hay calificaciones
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesDe EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesCalificación: 5 de 5 estrellas5/5 (1)
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesDe EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesCalificación: 5 de 5 estrellas5/5 (2)
- Mitral Valve Prolapse, A Simple Guide to The Condition, Treatment And Related ConditionsDe EverandMitral Valve Prolapse, A Simple Guide to The Condition, Treatment And Related ConditionsAún no hay calificaciones
- Cardioversion, A Simple Guide To The Condition, Types, Treatment of Arrhythmias And Related ConditionsDe EverandCardioversion, A Simple Guide To The Condition, Types, Treatment of Arrhythmias And Related ConditionsAún no hay calificaciones
- Alert Medical Series: Emergency Medicine Alert I, II, IIIDe EverandAlert Medical Series: Emergency Medicine Alert I, II, IIIAún no hay calificaciones
- Atrial Flutter (Flutter in the Heart) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe EverandAtrial Flutter (Flutter in the Heart) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAún no hay calificaciones
- TLE Pre-Assessment Most & Least Learned SkillsDocumento7 páginasTLE Pre-Assessment Most & Least Learned SkillsRd DavidAún no hay calificaciones
- B25 Pompe de Peinture PDFDocumento98 páginasB25 Pompe de Peinture PDFchahineAún no hay calificaciones
- HPC ReportDocumento316 páginasHPC ReportmamansgAún no hay calificaciones
- LESSON 1 PREPARE VEGETABLE DISHES OverviDocumento12 páginasLESSON 1 PREPARE VEGETABLE DISHES OverviKeym Garcia Galvez IIIAún no hay calificaciones
- Fault Location of Overhead Transmission Line With Noncontact Magnetic Field MeasurementDocumento10 páginasFault Location of Overhead Transmission Line With Noncontact Magnetic Field MeasurementJkAún no hay calificaciones
- EPG Health Report The Future of HCP Engagement Impact 2023Documento73 páginasEPG Health Report The Future of HCP Engagement Impact 2023paulilongereAún no hay calificaciones
- Full Test 14 (Key) PDFDocumento4 páginasFull Test 14 (Key) PDFhoang lichAún no hay calificaciones
- Pastillas DelightDocumento12 páginasPastillas DelightBryan DutchaAún no hay calificaciones
- (2022) Loneliness Is Associated With Maladaptive Schema Modes in Patients With Persistent Depressive DisorderDocumento5 páginas(2022) Loneliness Is Associated With Maladaptive Schema Modes in Patients With Persistent Depressive DisorderJúlio César SouzaAún no hay calificaciones
- Work Procedure For CCB Installation of Raised Floor 2Documento13 páginasWork Procedure For CCB Installation of Raised Floor 2ResearcherAún no hay calificaciones
- Types of Industrial DisputesDocumento12 páginasTypes of Industrial DisputesAntony MwangiAún no hay calificaciones
- Filipino Nurses' Deep Faith and Cultural Attitudes in HealthcareDocumento41 páginasFilipino Nurses' Deep Faith and Cultural Attitudes in HealthcareKeziah Marie Chua Santa-AnaAún no hay calificaciones
- Official Game GuideDocumento30 páginasOfficial Game GuideHhfugAún no hay calificaciones
- Chad Yakobson ThesisDocumento5 páginasChad Yakobson Thesiscrystaltorresworcester100% (2)
- اللائحة التنظيمية لسفن الكروز - النسخة العربية - TransDocumento10 páginasاللائحة التنظيمية لسفن الكروز - النسخة العربية - TranssalsabilAún no hay calificaciones
- Pdev 111 Week 1 20 1st SemesterDocumento123 páginasPdev 111 Week 1 20 1st SemesterReyn TabelismaAún no hay calificaciones
- Vishal Seminar Report StrokeDocumento40 páginasVishal Seminar Report StrokeVishal kaushikAún no hay calificaciones
- Effects of Climate Change and Global WarmingDocumento14 páginasEffects of Climate Change and Global WarmingSwetal SosaAún no hay calificaciones
- Thermax ION Exchange Resins SDS BrochureDocumento8 páginasThermax ION Exchange Resins SDS Brochureparthibanemails5779Aún no hay calificaciones
- 1 s2.0 S0149763418301957 MainDocumento24 páginas1 s2.0 S0149763418301957 MainjackAún no hay calificaciones
- A7V Variable Displacement PumpDocumento22 páginasA7V Variable Displacement PumpEduardo CramerAún no hay calificaciones
- Nigeria Trainers ManualDocumento131 páginasNigeria Trainers ManualVivi ALAún no hay calificaciones
- Chapter 4 MoldingDocumento46 páginasChapter 4 MoldingTamirat NemomsaAún no hay calificaciones
- Numerical Modelling of Drying Kinetics of Banana Flower Using Natural and Forced Convection DryersDocumento5 páginasNumerical Modelling of Drying Kinetics of Banana Flower Using Natural and Forced Convection DryersMuthu KumarAún no hay calificaciones
- Fire & Gas Design BasisDocumento2 páginasFire & Gas Design BasisAdil MominAún no hay calificaciones
- Antox Pickling Paste MSDSDocumento10 páginasAntox Pickling Paste MSDSKrishna Vacha0% (1)
- Philippine STEM Module Explains Photoelectric EffectDocumento12 páginasPhilippine STEM Module Explains Photoelectric EffectJp menorAún no hay calificaciones
- Exercise 2. Pair EssayDocumento2 páginasExercise 2. Pair Essayrjay manalo75% (4)
- Masagana High School: Module 4: Planning For Continuing Professional Development and Lac PlanningDocumento6 páginasMasagana High School: Module 4: Planning For Continuing Professional Development and Lac PlanningjhonaAún no hay calificaciones
- Climate and Cultural IdentityDocumento2 páginasClimate and Cultural IdentityCha AbolucionAún no hay calificaciones