Documentos de Académico
Documentos de Profesional
Documentos de Cultura
PCOS guideline methods for fertility outcomes
Cargado por
Alfa Febrianda0 calificaciones0% encontró este documento útil (0 votos)
18 vistas16 páginasJajja
Título original
Usg Kapan Diperlukan1
Derechos de autor
© © All Rights Reserved
Formatos disponibles
PPTX, PDF, TXT o lea en línea desde Scribd
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoJajja
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PPTX, PDF, TXT o lea en línea desde Scribd
0 calificaciones0% encontró este documento útil (0 votos)
18 vistas16 páginasPCOS guideline methods for fertility outcomes
Cargado por
Alfa FebriandaJajja
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PPTX, PDF, TXT o lea en línea desde Scribd
Está en la página 1de 16
International evidence-based guideline
for the assessment and management of
polycystic
ovary syndrome 2018
Bariatric surgery In women with PCOS
• What is the effectiveness of lifestyle interventions compared to bariatric surgery
for improving fertility and adverse outcomes?
• Justification Bariatric surgery improves weight loss and can improve
comorbidities associated with PCOS. However, evidence in relation to fertility and
pregnancy outcomes is limited, with some concerns about potential perinatal
adverse effects of bariatric surgery. Given the concerns about the potential
perinatal adverse effects of bariatric surgery and the remaining controversies, no
recommendation can be made at this time about the use of bariatric surgery to
improve fertility and pregnancy outcomes in women with PCOS.
In-vitro fertilisation In women with PCOS
• The GDG deemed IVF should be considered after failed ovulation
induction treatment with high pregnancy rates per cycle, especially in
younger women. Given the risks and the high costs that can be
prohibitive for many patients, IVF should be considered third line
medical therapy. It was noted that conception and delivery are highly
valued by health professionals and women with PCOS and even when
cost and risks are increased, many may elect to undertake IVF. Health
Professionals must weigh benefits and risk when advising PCOS
patients to enable an informed decision.
5.9b Gonadotropin releasing hormone protocol
• In women with PCOS undergoing IVF/ICSI treatment, is the
gonadotropin releasing hormone antagonist protocol or gonadotropin
releasing hormone agonist long protocol the most effective for
improving fertility outcomes?
• The duration of stimulation with a GnRH antagonist approach is
around a day shorter than the standard ‘long-down regulation’
approach with a GnRH agonist. The rate of OHSS appears less with a
GnRH antagonist approach in comparison to the standard ‘long-down
regulation’ approach with a GnRH agonis
5.9c Trigger type
• In women with PCOS undergoing GnRH antagonist IVF/ICSI treatment,
is the use of hCG trigger or GnRH agonist trigger the most effective
for improving fertility outcomes?
• The choice to trigger final oocyte maturation with GnRH-agonist
instead of hCG is important in prevention of OHSS as hCG alone
induces oocyte maturation but is associated with OHSS. GnRH-
agonist triggers are associated with lower pregnancy rates, primarily
in fresh embryo transfers, which can be overcome in frozen cycles
Choice of FSH
• In women with PCOS undergoing (controlled) ovarian (hyper) stimulation
for IVF/ICSI, does the choice of FSH effect fertility outcomes?
• Only one small study in PCOS has been identified investigating uFSH versus
rFSH in PCOS during ovarian stimulation for IVF/ICSI [578]. This study shows
similar results to a systematic review and meta-analysis in the general IVF
population, where extensive research has concluded no significant
difference in birth rate or OHSS was detected and no further research in
the general population was recommended. Hence clinical choice of
gonadotrophin should depend on availability, convenience and costs.
Exogenous luteinizing hormone (LH)
• In women with PCOS undergoing (controlled) ovarian (hyper)
stimulation for IVF/ICSI, is exogenous LH treatment during IVF ± ICSI
effective for improving fertility outcome?
• There is no anticipated effect or benefit to add exogenous LH
supplement in women with PCOS undergoing ovarian stimulation for
IVF ± ICSI. There is insufficient evidence to determine the benefits of
using or not using exogenous LH.
Adjunct metformin
• In women with PCOS undergoing (controlled) ovarian (hyper) stimulation
for IVF ± ICSI, is adjunct metformin effective for improving fertility
outcomes?
• Women and health professionals would generally value an increased
clinical pregnancy rate (with no evidence of a difference in miscarriage
rate) and reduced OHSS (with its associated morbidity and rarely
mortality). Gastrointestinal side effects were recognised, but noted as mild
and self-limiting and may be minimised with lower metformin starting dose
and extended release preparations. Metformin was noted to be low cost
and readily available, and while off label use was generally allowed,
explanation is required for use.
In-vitro maturation
• In women with PCOS, is in-vitro maturation (IVM) effective for improving
fertility outcomes?
• The GDG deemed that key elements to consider with IVM included; a clear
definition of the term IVM, use in clinical units with sufficient expertise and
advantages of reduced risk of OHSS. The group considered the lack of
evidence as important. It was considered that IVM could be offered to
achieve pregnancy and live birth rates that may approach those of standard
IVF ± ICSI treatment, where frozen embryos are used. Given the lack of
evidence the group voted for a conditional consensus recommendation
that neither favoured this option or other options (IVF), with strong
research recommendations
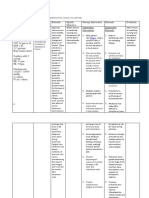
Guideline development methods
• The International evidence–based guideline for the assessment and
management of PCOS underpins an international initiative to engage
women affected by PCOS and their health professionals to improve
health outcomes
Guideline development methods
• In the development of this guideline, we have sought not only to
inform or consult with women affected by PCOS, but to partner with
and empower women with PCOS, who are the ultimate beneficiaries
of this work. We have engaged with international consumer bodies in
PCOS and infertility to this end. This included Polycystic Ovary
Syndrome Association Australia (POSAA) (Australia), Verity (United
Kingdom), PCOS Challenge (United States), RESOLVE: The National
Fertility Association (United States), and Victorian Assisted
Reproductive Treatment Authority (VARTA) (Australia), who were
actively engaged throughout the guideline process.
Guideline development methods
• Clinical question development and prioritization
• An International survey and Delphi exercise was conducted to
develop and prioritise clinical questions to be addressed. A further
prioritisation exercise was conducted within the topic specific GDGs
and consumer advisory groups to rank the importance of clinical
questions to guide the evidence team and to reach consensus on
which clinical questions were to be addressed by a systematic review
or by narrative review.
Guideline development methods
• GDG – 1 Screening, diagnostic assessment, risk assessment and life-
stage
• GDG 2 - Prevalence, screening, diagnostic assessment and
management of emotional wellbeing
• GDG 3 – Lifestyle management and models of care
• GDG 4 – Medical treatment
• GDG 5 – Screening, diagnostic assessment and management of
infertility
Guideline development methods
• Outcome prioritisation using the GRADE method
• The most relevant outcomes were prioritised by ranking their
importance by health professionals and consumers to help resolve or
clarify disagreements and assist with grading the
evidence. The importance of outcomes may vary across cultures and
from different perspectives e.g. patients, public, health professionals
or policy-makers
Guideline development methods
• Adaptation of existing evidence-based guidelines
• Here we have updated and expanded the scope and evidence contained in the
2011 Australian guideline and, where appropriate methods have been applied,
integrated the WHO guideline.
• Evidence reviews to answer the clinical questions
• The links between the body of evidence, the clinical need for the question and
the clinical impact of the resulting recommendation(s), including potential
changes in usual care and the way care is organised, acceptability, feasibility and
resource implications are clearly explained in the accompanying GRADE evidence
to decision framework supporting the recommendation.
Inclusion of studies
• To determine the literature to be assessed further, a reviewer scanned the titles,
abstracts and keywords of every record retrieved by the search strategy. Studies
were selected by one reviewer in consultation with colleagues, using the PICO
selection criteria established a priori.
• Appraisal of the methodological quality/risk of bias of the evidence
• Methodological quality of the included studies was assessed using criteria
developed a priori according to study design. Individual quality items were
investigated using a descriptive component approach. Any disagreement or
uncertainty was resolved by discussion among the GDG to reach a consensus.
También podría gustarte
- Ovulación en SOPDocumento10 páginasOvulación en SOPbeaprinaAún no hay calificaciones
- Literature Review On Obesity in PregnancyDocumento6 páginasLiterature Review On Obesity in Pregnancybsnyfpwgf100% (1)
- PCOS Guideline Summary 2023Documento35 páginasPCOS Guideline Summary 2023Saudamini Naik100% (1)
- Weight Loss InterventionDocumento21 páginasWeight Loss InterventionsamuelionardiAún no hay calificaciones
- © 2015 American College of PhysiciansDocumento70 páginas© 2015 American College of PhysiciansAriyoko PatodingAún no hay calificaciones
- Evidence Based Practice PartoDocumento12 páginasEvidence Based Practice PartobabyAún no hay calificaciones
- Recommendations From The Guideline For Pcos-NoprintDocumento16 páginasRecommendations From The Guideline For Pcos-NoprintpopasorinemilianAún no hay calificaciones
- Pregnant Mothers' KAP of Exercise During PregnancyDocumento24 páginasPregnant Mothers' KAP of Exercise During PregnancyBEREKETAún no hay calificaciones
- Guideline No. 389-Medical Management ofDocumento4 páginasGuideline No. 389-Medical Management ofNguyễn Văn TiếnAún no hay calificaciones
- Management PCOSDocumento16 páginasManagement PCOSariefandyAún no hay calificaciones
- Evidence-Based Clinical Practice Guideline - Reduction MammaplastyDocumento16 páginasEvidence-Based Clinical Practice Guideline - Reduction MammaplastyLuiggi FayadAún no hay calificaciones
- Guidelines For The Management of Pregnant Women With Obesity: A Systematic ReviewDocumento14 páginasGuidelines For The Management of Pregnant Women With Obesity: A Systematic ReviewMichael ThomasAún no hay calificaciones
- Two Up Cont CPG Intrapartum PDFDocumento98 páginasTwo Up Cont CPG Intrapartum PDFjojolilimomoAún no hay calificaciones
- FIGO HIP For Website 21 Feb 17Documento46 páginasFIGO HIP For Website 21 Feb 17Bob IrsanAún no hay calificaciones
- Fertility in Vitro Fertilisation Treatment For People With Fertility ProblemsDocumento12 páginasFertility in Vitro Fertilisation Treatment For People With Fertility ProblemsRobMarvinAún no hay calificaciones
- Articulo Oxitocina CelDocumento38 páginasArticulo Oxitocina CelMaripaz RossainzAún no hay calificaciones
- A Randomised Controlled Trial On The Effects of Structural Education Module Among Women With PCOS On Nutrition and Physical Activity ChangesDocumento11 páginasA Randomised Controlled Trial On The Effects of Structural Education Module Among Women With PCOS On Nutrition and Physical Activity ChangesRocío Vivancos NavarroAún no hay calificaciones
- Pregnancy Testing Prior To Anesthesia and SurgeryDocumento4 páginasPregnancy Testing Prior To Anesthesia and SurgeryelliasAún no hay calificaciones
- Recommendations From The 2023 International Evidence-Based Guideline For The Assessment and Management of Polycystic Ovary SyndromeDocumento23 páginasRecommendations From The 2023 International Evidence-Based Guideline For The Assessment and Management of Polycystic Ovary Syndromefbonilla100% (1)
- medley2018Documento9 páginasmedley2018David Rafael Cañez MartinezAún no hay calificaciones
- Management of Preterm LaborDocumento2 páginasManagement of Preterm LaborpolygoneAún no hay calificaciones
- Acog Practice Bulletin Summary: Obesity in PregnancyDocumento3 páginasAcog Practice Bulletin Summary: Obesity in PregnancyMariana Hernandez100% (1)
- Intl J Gynecology Obste - 2020 - Killeen - Examining The Use of The FIGO Nutrition Checklist in Routine AntenatalDocumento6 páginasIntl J Gynecology Obste - 2020 - Killeen - Examining The Use of The FIGO Nutrition Checklist in Routine AntenatalBenk Setsuna F. SeieiAún no hay calificaciones
- Benefits of Breastfeeding MoralesDocumento6 páginasBenefits of Breastfeeding MoralesMalaya MilesAún no hay calificaciones
- Critical Functions of The RhoGEFAnillin Element Within Septin Architectural Alpelisibg Through CytokinesisebvhlDocumento1 páginaCritical Functions of The RhoGEFAnillin Element Within Septin Architectural Alpelisibg Through Cytokinesisebvhlheightlute4Aún no hay calificaciones
- Jurnal Cbe 1Documento21 páginasJurnal Cbe 1Dewi SurayaAún no hay calificaciones
- AACE/ACE Disease State Clinical ReviewDocumento10 páginasAACE/ACE Disease State Clinical ReviewSanjay NavaleAún no hay calificaciones
- Jog 12115Documento7 páginasJog 12115niko4eyesAún no hay calificaciones
- Mohamed Dahir AbdiDocumento12 páginasMohamed Dahir AbdiDan guudAún no hay calificaciones
- Recommendations From The 2023 International Evidence-Based Guideline For The Assessment and Management of Polycystic Ovary SyndromeDocumento22 páginasRecommendations From The 2023 International Evidence-Based Guideline For The Assessment and Management of Polycystic Ovary SyndromeGunay AbbasovaAún no hay calificaciones
- Preconception Care: Maximizing The Gains For Maternal and Child HealthDocumento15 páginasPreconception Care: Maximizing The Gains For Maternal and Child HealthAnita Rezeki Carolina100% (1)
- Proposal CS DilveraryDocumento5 páginasProposal CS DilveraryhanadiAún no hay calificaciones
- Report For The Healthy Start Research To Practice Workgroup: Jennifer Carvalho SalemiDocumento45 páginasReport For The Healthy Start Research To Practice Workgroup: Jennifer Carvalho SalemiMelda SikumbangAún no hay calificaciones
- AbortionDocumento1 páginaAbortionVenus PlanetAún no hay calificaciones
- JURNAL BMI PREGNANCY + Crit AppDocumento55 páginasJURNAL BMI PREGNANCY + Crit Apppkm rejosariAún no hay calificaciones
- Usability, Acceptability, and Feasibility of The World Health Organization Labour Care Guide: A Mixed-Methods, Multicountry EvaluationDocumento10 páginasUsability, Acceptability, and Feasibility of The World Health Organization Labour Care Guide: A Mixed-Methods, Multicountry EvaluationDiksha chaudharyAún no hay calificaciones
- Jurnal Riza T1A-1Documento17 páginasJurnal Riza T1A-1Riza RsAún no hay calificaciones
- WHO Recommendations On Antenatal Care For A Positive Pregnancy Experience: Ultrasound ExaminationDocumento4 páginasWHO Recommendations On Antenatal Care For A Positive Pregnancy Experience: Ultrasound ExaminationramadeniramaAún no hay calificaciones
- Care of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManDocumento26 páginasCare of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManLaurence Docog100% (1)
- Pre-Pregnancy Care (Webinar 25.5.2022)Documento27 páginasPre-Pregnancy Care (Webinar 25.5.2022)SHELLY NOVITA SARI 1904053Aún no hay calificaciones
- Claudio Et Al HE Vol 3Documento17 páginasClaudio Et Al HE Vol 3Elizalde HusbandAún no hay calificaciones
- ASSESSMENT OF FACTORS AFFECTING EXCLUSSIVE BREAST GROUP 4 NewDocumento10 páginasASSESSMENT OF FACTORS AFFECTING EXCLUSSIVE BREAST GROUP 4 NewChris OchayaAún no hay calificaciones
- Junior Gynecology Rotation ObjectivesDocumento13 páginasJunior Gynecology Rotation ObjectivesaaaaaAún no hay calificaciones
- Contraceptionppt 1Documento22 páginasContraceptionppt 1Basma TaherAún no hay calificaciones
- PIIS0015028219324847Documento18 páginasPIIS0015028219324847Maged BedeawyAún no hay calificaciones
- Jurnal 10Documento2 páginasJurnal 10RickymaulanasaputraAún no hay calificaciones
- Mode Birth Review PointsDocumento82 páginasMode Birth Review PointsAna-Iulia PetcuAún no hay calificaciones
- Metode Istraživanja I Vrednovanja Zdravstvenih Intervencija - JDDocumento19 páginasMetode Istraživanja I Vrednovanja Zdravstvenih Intervencija - JDJelena DiAún no hay calificaciones
- PNACT388Documento2 páginasPNACT388Ieien MuthmainnahAún no hay calificaciones
- Peña2020 Article AdolescentPolycysticOvarySyndrDocumento16 páginasPeña2020 Article AdolescentPolycysticOvarySyndrpaolaAún no hay calificaciones
- HO 4 Essential Intrapartum Care 6may2013Documento12 páginasHO 4 Essential Intrapartum Care 6may2013Maedine Urbano-Briones100% (1)
- National Guidelines For Quality Obstetrics and Perinatal Care PDFDocumento410 páginasNational Guidelines For Quality Obstetrics and Perinatal Care PDFduncan100% (1)
- Guidelines On 8 Key Evidence Based Practices During Labour - 353Documento35 páginasGuidelines On 8 Key Evidence Based Practices During Labour - 353National Child Health Resource Centre (NCHRC)Aún no hay calificaciones
- Proforma Synopsis For Registration of SubjectDocumento15 páginasProforma Synopsis For Registration of SubjectTamilArasiAún no hay calificaciones
- Guideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementDocumento26 páginasGuideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementYo Me100% (1)
- Dr. Bahar - Audit Klinis - Medis - MB - Robson Edit 2Documento31 páginasDr. Bahar - Audit Klinis - Medis - MB - Robson Edit 2Prita MuliariniAún no hay calificaciones
- Journal Club: Moderator: Dr. Ruchi Srivastava Presenter: Dr. Shivangini SahayDocumento37 páginasJournal Club: Moderator: Dr. Ruchi Srivastava Presenter: Dr. Shivangini Sahayshivangini sahayAún no hay calificaciones
- What You Need to Know About IVF- A Comprehensive GuideDe EverandWhat You Need to Know About IVF- A Comprehensive GuideAún no hay calificaciones
- Differences in Sexual Function After Vaginal DeliveryDocumento3 páginasDifferences in Sexual Function After Vaginal DeliveryAlfa FebriandaAún no hay calificaciones
- GMR 6939Documento6 páginasGMR 6939Alfa FebriandaAún no hay calificaciones
- Higado Graso Agudo en El Embarazo AJG 2017Documento9 páginasHigado Graso Agudo en El Embarazo AJG 2017Fabrizzio BardalesAún no hay calificaciones
- CMJ 57 6 Peterlin 28051281Documento6 páginasCMJ 57 6 Peterlin 28051281Alfa FebriandaAún no hay calificaciones
- Prothrombin and Factor V Mutations in Women With ADocumento7 páginasProthrombin and Factor V Mutations in Women With AAlfa FebriandaAún no hay calificaciones
- AflpDocumento8 páginasAflprmiguel7Aún no hay calificaciones
- Poster Session IV: ObjectiveDocumento2 páginasPoster Session IV: ObjectiveAlfa FebriandaAún no hay calificaciones
- Aavs 7 1 17-23 PDFDocumento7 páginasAavs 7 1 17-23 PDFAlfa FebriandaAún no hay calificaciones
- Magnesium OyeDocumento11 páginasMagnesium Oyeade_fkuAún no hay calificaciones
- Corticotrophin Releasing Hormone As A Useful Marker To Identify The Pre-EclampsiaDocumento4 páginasCorticotrophin Releasing Hormone As A Useful Marker To Identify The Pre-EclampsiaAlfa FebriandaAún no hay calificaciones
- Leptin rs2167270 G A (G19A) Polymorphism May Decrease The Risk of Cancer: A Case Control Study and Meta Analysis Involving 19 989 SubjectsDocumento10 páginasLeptin rs2167270 G A (G19A) Polymorphism May Decrease The Risk of Cancer: A Case Control Study and Meta Analysis Involving 19 989 SubjectsAlfa FebriandaAún no hay calificaciones
- Haplotype AnalysisDocumento5 páginasHaplotype AnalysisAlfa FebriandaAún no hay calificaciones
- Single Nucleotide Polymorphisms of Follicle-Stimulating Hormone Receptor Promoter and Their Impacts To The Promoter ActivitiesDocumento10 páginasSingle Nucleotide Polymorphisms of Follicle-Stimulating Hormone Receptor Promoter and Their Impacts To The Promoter ActivitiesAlfa FebriandaAún no hay calificaciones
- Antenatal Care of Preeclampsia: From The Inverted Pyramid To The Arrow Model?Documento4 páginasAntenatal Care of Preeclampsia: From The Inverted Pyramid To The Arrow Model?Alfa FebriandaAún no hay calificaciones
- Pregnancy and Postpartum Risks for Venous ThrombosisDocumento6 páginasPregnancy and Postpartum Risks for Venous ThrombosisAlfa FebriandaAún no hay calificaciones
- A Rare Case of Meigs Syndrome in Pregnancy With Bilateral Ovarian MassesDocumento2 páginasA Rare Case of Meigs Syndrome in Pregnancy With Bilateral Ovarian MassesAlfa FebriandaAún no hay calificaciones
- Pregnancy and Postpartum Risks for Venous ThrombosisDocumento6 páginasPregnancy and Postpartum Risks for Venous ThrombosisAlfa FebriandaAún no hay calificaciones
- Antenatal Care of Preeclampsia: From The Inverted Pyramid To The Arrow Model?Documento4 páginasAntenatal Care of Preeclampsia: From The Inverted Pyramid To The Arrow Model?Alfa FebriandaAún no hay calificaciones
- 1 PDFDocumento7 páginas1 PDFAlfa FebriandaAún no hay calificaciones
- Haplotype AnalysisDocumento5 páginasHaplotype AnalysisAlfa FebriandaAún no hay calificaciones
- JokohjokDocumento2 páginasJokohjokAlfa FebriandaAún no hay calificaciones
- CMJ 57 6 Peterlin 28051281Documento6 páginasCMJ 57 6 Peterlin 28051281Alfa FebriandaAún no hay calificaciones
- TRF 12966Documento8 páginasTRF 12966Alfa FebriandaAún no hay calificaciones
- Success of External Cephalic Version With Terbutaline As Tocolytic AgentDocumento4 páginasSuccess of External Cephalic Version With Terbutaline As Tocolytic AgentAlfa FebriandaAún no hay calificaciones
- Aogs 13082Documento8 páginasAogs 13082Alfa FebriandaAún no hay calificaciones
- Iron Deficiency Anaemia In...Documento9 páginasIron Deficiency Anaemia In...Alfa FebriandaAún no hay calificaciones
- Endometriosis-Associated Infertility Causes and TreatmentsDocumento9 páginasEndometriosis-Associated Infertility Causes and TreatmentsAlfa FebriandaAún no hay calificaciones
- Anaemia Pregnancy: (Dieckmann 1944 I960)Documento13 páginasAnaemia Pregnancy: (Dieckmann 1944 I960)Alfa FebriandaAún no hay calificaciones
- Meigs' Syndrome and Pseudo-Meigs' Syndrome: Report of Four Cases and Literature ReviewsDocumento6 páginasMeigs' Syndrome and Pseudo-Meigs' Syndrome: Report of Four Cases and Literature ReviewsAlfa FebriandaAún no hay calificaciones
- Transfusion-Related Acute Lung Injury Risk Mitigation: An UpdateDocumento10 páginasTransfusion-Related Acute Lung Injury Risk Mitigation: An UpdateAlfa FebriandaAún no hay calificaciones
- Gene Therapy PDFDocumento3 páginasGene Therapy PDFJenny PastorAún no hay calificaciones
- Horseshoe Crab For Medical Science by Dr. Anil ChatterjiDocumento42 páginasHorseshoe Crab For Medical Science by Dr. Anil ChatterjiDr Bugs TanAún no hay calificaciones
- PEOPLE AS OMNIVORES: COSTS AND BENEFITS OF DIETDocumento10 páginasPEOPLE AS OMNIVORES: COSTS AND BENEFITS OF DIETsuleimanAún no hay calificaciones
- Fish TishDocumento151 páginasFish Tishabhinav_choudhary03Aún no hay calificaciones
- Dendrimers: Synthesis, Applications, and Properties: Nanoreview Open AccessDocumento10 páginasDendrimers: Synthesis, Applications, and Properties: Nanoreview Open AccessIonut StirbescuAún no hay calificaciones
- MH Introduction To HistologyDocumento46 páginasMH Introduction To HistologyFefê BrittoAún no hay calificaciones
- Bio Control LectureDocumento8 páginasBio Control Lecturedars23Aún no hay calificaciones
- Therapeutic Relationship NotesDocumento11 páginasTherapeutic Relationship NotesAlexandra StanAún no hay calificaciones
- Human Physiology IntroductionDocumento1 páginaHuman Physiology IntroductionChris_Barber09Aún no hay calificaciones
- 4.bilogical EffectsDocumento56 páginas4.bilogical Effectswajira sanjaya pereraAún no hay calificaciones
- General and Oral PathologyDocumento361 páginasGeneral and Oral Pathologyjoseph100% (3)
- Lecture Notes For Mental Health Nursing Psych NursingDocumento84 páginasLecture Notes For Mental Health Nursing Psych NursingAnn Michelle Tarrobago100% (2)
- PRM - Ma5 BookletDocumento25 páginasPRM - Ma5 BookletVan LabasanoAún no hay calificaciones
- Current Primary Open-Angle Glaucoma Treatments and Future DirectionsDocumento13 páginasCurrent Primary Open-Angle Glaucoma Treatments and Future DirectionsBenediktus BayuAún no hay calificaciones
- 22 Respiratory SystemDocumento99 páginas22 Respiratory SystemvanderphysAún no hay calificaciones
- Cerebellar LesionsDocumento3 páginasCerebellar LesionsMary100% (1)
- Gene TherapyDocumento36 páginasGene TherapySukesh Potla100% (2)
- Biliary Atresia Copy LNGDocumento10 páginasBiliary Atresia Copy LNGlloraoAún no hay calificaciones
- Final NPRD, 2021Documento28 páginasFinal NPRD, 2021Maruthi RoshanAún no hay calificaciones
- PURWOCENGDocumento6 páginasPURWOCENGAnonymous HPmfOqdwAún no hay calificaciones
- Respiratory SystemDocumento32 páginasRespiratory Systemapi-202513022Aún no hay calificaciones
- Nt-Probnp: The Gold Standard Biomarker in Heart FailureDocumento3 páginasNt-Probnp: The Gold Standard Biomarker in Heart FailureRiuin23Aún no hay calificaciones
- Stomatognathic SystemDocumento129 páginasStomatognathic Systemsurya kingsly100% (1)
- IB Biology Higher Level Human and Health Physiology NotesDocumento41 páginasIB Biology Higher Level Human and Health Physiology NoteshunarsandhuAún no hay calificaciones
- Bacterial Cell To Cell CommunicationDocumento338 páginasBacterial Cell To Cell CommunicationAllbiol100% (1)
- Clinical Success of Deproteinization in Hypocalcified Amelogenesis ImperfectaDocumento7 páginasClinical Success of Deproteinization in Hypocalcified Amelogenesis ImperfectaMelisa GuerraAún no hay calificaciones
- NCP - FatigueDocumento3 páginasNCP - Fatigueitsmeaya100% (1)
- ANAT 100 - Module 1 Summary NotesDocumento6 páginasANAT 100 - Module 1 Summary NotesRahul BhardwajAún no hay calificaciones
- Neuropsych Lec 5 Mental Status ExamDocumento2 páginasNeuropsych Lec 5 Mental Status ExamnkivcAún no hay calificaciones
- Introducing The Sorush Cancer Treatment Protocol (SCTP)Documento18 páginasIntroducing The Sorush Cancer Treatment Protocol (SCTP)SorushAún no hay calificaciones