Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Ecsw 2016 Guidry-Grimes
Ecsw 2016 Guidry-Grimes
Cargado por
api-136237609Descripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Ecsw 2016 Guidry-Grimes
Ecsw 2016 Guidry-Grimes
Cargado por
api-136237609Copyright:
Formatos disponibles
2016 ETHICS & CLINICAL SOCIAL WORK
Laura Guidry-Grimes, PhD(c)
Center for Ethics @ MWHC
Clinical Ethicist
1
D ISCLAIMER AND C ONFLICT- OF-INTEREST
S TATEMENT
Disclaimer: Although this presentation is
representative of what we do here, my opinions
are my own and should not be taken as policy
for Medstar Washington Hospital Center or
Medstar Corporate.
Conflict-of-Interest (COI): I do not have any COI
relevant to this training program.
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
2
O UTLINE
Introduction to Ethics and Bioethics
Services
Historical Overview of Ethics and
Social Work
The “Difficult” Patient
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
3
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
4
WHAT IS ETHICS?
Ethics is the formal, systematic study of what
counts as the good, who we ought to be, what
types of responsibilities we have, and how we
should judge right from wrong action.
Ethicists provide reasons for choosing one
course of action over others
More than merely feeling something to be
desirable or preferable
Can be independent of religious, cultural, and
legal considerations
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
5
STEPS TO ETHICAL E VALUATION
What are the relevant facts?
Med state, psych state, social situation,
feasible options, etc.
Who or what could be affected by the way the
decision is resolved?
Who has a stake in the outcome?
What are the relevant ethical considerations?
Patient autonomy, professional integrity, fairness,
patient welfare, respect, pluralism/diversity,
religious freedom, etc.
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
6
STEPS TO ETHICAL E VALUATION
What is the primary ethics question? Others?
Separate from what should be done medically,
legally, culturally
Who is morally responsible for what?
Consider roles, institutional constraints
Which options are ethically permissible?
Which course of action is morally preferable?
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
7
B IOETHICS S ERVICES :
C ENTER FOR E THICS @ MWHC AS E XAMPLE
Ethics Consult Service
24 / 7, 365 days per year
Recommendations in chart and curbside coaching
Rounding
Ethics Committee
Organizational Ethics Subcommittee
Policy Subcommittee
Educational initiatives
Continuing training on EOL care, code status,
informed consent
Moral distress programming
Ad hoc talks
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
8
B IOETHICS SERVICES: W HERE WE A SSIST
Preventive ethics and crisis assistance
End of life and goals of care
Are there good moral reasons to withdraw LSTs?
Code status
Would resuscitation and intubation be more harmful than
beneficial? Should this decision be left to the family?
Surrogacy and capacity
Who is the ethically appropriate decision maker?
Professionalism
Is there a strict moral obligation to treat abusive patients?
Many, many others
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
9
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
10
EARLY THINKING U NDERLYING SW
Industrialization and urbanization at the end of
the 19th century economic and social
imbalances concerns about instability in
communities, consequences for government
“The Curse of Pauperism”
The poor treated as moral defectives, as sources
of unrest, as personally irresponsible if they did
not work
Poor communities treated paternalistically as
shiftless, in need of empirical study
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
11
PROGRESSION IN PROFESSIONAL SW
Shift in attitude after personal exposure to
poor individuals and their particular
circumstances
Addressing structural and environmental
causes (esp. public health barriers,
problems of industrialization)
Morally investigate social systems, rather
than poor individuals
Community advocacy against governmental
regulations that cause social imbalances and
economic oppression
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
12
EVOLVING ETHICS AT THE C ORE OF SW
Addressing barriers to personal fulfillment and
well-being
Institutionalized and embedded inequities
Identifying needs, improving access to resources
Problem-solving re: the systematic nature of
disadvantage and poverty
Inadequate housing, healthcare, alcoholism, and
violence demanded that a social worker take an
ethically investigative role with a focus on social
justice and social reform.
Seeing those in need of SW as distinct, complex
individuals
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
13
“VALUES AND ETHICS ARE THE L IFE-B LOOD
OF THE P ROFESSION ”
Beginning in the 1980s, increased attention
to applied ethics and ethical theory in SW
Development of a professional code of ethics
Progress of ethical attitudes to those in need
of SW helped to define the profession
Initial focus on socially-caused economic
imbalances has “evolved into an ambitious
attempt to grasp and resolve complex ethical
issues” (Reamer, 1998)
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
14
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
15
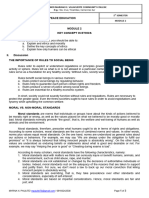
THE C OMMON PICTURE OF THE “D IFFICULT ”
PATIENT
15-60% of patients considered “difficult” by
treating physician
Some effects:
Stressed relationships, increased conflict
Negative feelings from all parties
Cracked professionalism
Unsuccessful treatments or poor compliance
Assumed causes:
Pt has a mental illness (perhaps undiagnosed)
Social or moral failures on the part of the pt
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
16
A NOTHER LOOK
“reframing the ‘difficult’ patient as someone
who perceives himself as wronged in the
medical encounter—perceives being
treated unfairly, disrespectfully, dismissively,
condescendingly, or offensively—generates
an ethical duty to address, validate,
repair, or assist in making amends”
(Fiester)
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
17
Q UESTIONS TO C ONSIDER
Whose perspective is being trusted and solicited?
Are there barriers to respectful communication?
What are the circumstances of this pt?
How might this pt’s health status be due to factors
outside of his/her control?
Is the label of “difficult” being applied mainly to pts
who are time-consuming, repeatedly/ increasingly ill, or
asking lots of questions of the physicians?
Is the medical team demonstrating empathy, moral
courage, and virtue?
Other questions to consider? Examples?
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
18
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
19
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
20
WHAT IS MORAL D ISTRESS ?
When you are in a morally charged situation,
believe you know what ought to be done, but
you are constrained from doing it
Perceived or actual powerlessness
Problem of moral residue, feeling compromised
Threat to moral integrity – “the sense of wholeness
and self-worth that comes from having clearly
defined values that are congruent with one’s actions
and perceptions” (Epstein & Delgado)
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
21
C ONSTRAINTS ON THE MORAL A GENT
Role obligations & competence
(e.g., nurse, not physician)
Laws, policies, codes
Power hierarchy
Realities of time
Limited resources, staff
LOS pressures
Others?
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
22
SOURCES & C ONTRIBUTING FACTORS
Individual, case-specific Institutional, systemic
disagreeable family hostile climate
abusive patient inadequate
mechanisms for safe
staff conflict reporting
demands for futile unclear or problematic
treatment policies or guidelines
poor communication insufficient training
misunderstanding of EOL distrust among staff
options
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
23
C RESCENDO E FFECT
After repeated MD, level of moral residue
builds
Insufficient preventive ethics and resolutions
Increasing sense of powerlessness, isolation
Negative effects on job satisfaction, well-
being, relationships, sense of agency
CE moral insensitivity, conscientious
objections, burnout
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
24
C OPING WITH AND PREVENTING MD
AACN Guide:
Ask: become aware MD is present
Affirm: make a commitment to address MD
Assess: identify sources of MD and make action plan
Act: implement strategies to preserve integrity
Moral distress programming
Discussions, workshops, educational sessions
Ethics involvement
Consultation, follow up, education
Organizational ethics and review of policies/practices
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
25
R EFERENCES & R ESOURCES
• American Association of Critical-Care Nurses. The 4A’s to Rise above Moral Distress. web:
<http://www.aacn.org/WD/Practice/Docs/4As_to_Rise_Above_Moral_Distress.pdf>
• Epstein, E. and S. Delgado. “Understanding and Addressing Moral Distress.” The Online
Journal of Issues in Nursing 15.3 (2010): web.
• Epstein, E. and A. Hamric. “Moral Distress, Moral Residue, and the Crescendo Effect.”
Journal of Clinical Ethics 20.4 (2009): 330-342.
• Fiester A. The ‘difficult’ patient reconceived: an expanded moral mandate for clinical ethics.
Am J Bioeth 2012;12(5):2-7.
• NASW Code of Ethics: http://www.socialworkers.org/pubs/code/default.asp
• NASW. “Social Work History.” http://www.naswdc.org/pressroom/features/general/history.asp
• Reamer, Frederic G. “The Evolution of Social Work Ethics.” Social Work 42.6 (1998): 488-
500.
• University of Kentucky Program for Bioethics. The Moral Distress Project. web:
<http://moraldistressproject.med.uky.edu>.
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
26
Laura Guidry-Grimes, PhD(c) | MWHC Center for Ethics
27
También podría gustarte
- Indiana DCS Lawsuit FilingDocumento66 páginasIndiana DCS Lawsuit FilingEmily FilipskiAún no hay calificaciones
- Strategic ManagementDocumento46 páginasStrategic ManagementWaseque Uddin Ahmed100% (2)
- 1610 EthicsDocumento44 páginas1610 EthicsIpraahim BashirAún no hay calificaciones
- Physical Therapist Professional EthicsDocumento4 páginasPhysical Therapist Professional EthicsJohn Gabriel BaduriaAún no hay calificaciones
- Solved by Verified Expert: Answer & ExplanationDocumento6 páginasSolved by Verified Expert: Answer & ExplanationDegoAún no hay calificaciones
- Ethics Solve QuestionsDocumento7 páginasEthics Solve QuestionsLifiAún no hay calificaciones
- ASSIGNMENT-Business EthicsDocumento10 páginasASSIGNMENT-Business EthicsMack RaoAún no hay calificaciones
- Research Papers Ethics and MoralityDocumento4 páginasResearch Papers Ethics and Moralityafnknohvbbcpbs100% (1)
- Presenters: Robert M. Gordon, PH.D., & Alan C. Tjeltveit, PH.DDocumento118 páginasPresenters: Robert M. Gordon, PH.D., & Alan C. Tjeltveit, PH.DSusi RutmalemAún no hay calificaciones
- Ethical Legal Issues Related To Gerontological Care HCDocumento41 páginasEthical Legal Issues Related To Gerontological Care HCtamika sealyAún no hay calificaciones
- Session 27 and 28Documento16 páginasSession 27 and 28GAAún no hay calificaciones
- Introspection InformationDocumento31 páginasIntrospection Informationsultana parvinAún no hay calificaciones
- Client Rights and ResponsibilitiesDocumento4 páginasClient Rights and ResponsibilitiesRuelRinconadaAún no hay calificaciones
- Making Ethical ChoicesDocumento52 páginasMaking Ethical ChoicesabdulqayyumaitAún no hay calificaciones
- Module 7 TemplateDocumento6 páginasModule 7 TemplateKelvin Cacstone NdunguAún no hay calificaciones
- Intelectual Disability Nas Stigma PDFDocumento240 páginasIntelectual Disability Nas Stigma PDFLidio Clemente100% (1)
- Paint It GrayDocumento18 páginasPaint It GrayJOHARIE SALIMAún no hay calificaciones
- Assignment 2Documento17 páginasAssignment 2sajan chhetriAún no hay calificaciones
- @clinical Ethics ToolboxDocumento4 páginas@clinical Ethics Toolboxjcouri33Aún no hay calificaciones
- Ethics Midterm CoverageDocumento38 páginasEthics Midterm CoverageLEAH HURTADAAún no hay calificaciones
- MGMT 371 Chapter Four: The Ethical and Social EnvironmentDocumento29 páginasMGMT 371 Chapter Four: The Ethical and Social EnvironmentreqabAún no hay calificaciones
- The Ethics of Being EthicalDocumento2 páginasThe Ethics of Being EthicalAnonymous gptX7l0ARXAún no hay calificaciones
- Theories of Ethical ReasoningDocumento43 páginasTheories of Ethical ReasoningJSeasharkAún no hay calificaciones
- Ethics in ResearchDocumento47 páginasEthics in ResearchSteven Paul DaclesAún no hay calificaciones
- Mid Term (Spring 2020) : Subject: Advanced Research Methods (Qualitative)Documento40 páginasMid Term (Spring 2020) : Subject: Advanced Research Methods (Qualitative)Ali IjazAún no hay calificaciones
- Mental Health Stigma - EditedDocumento8 páginasMental Health Stigma - EditedRoman -Aún no hay calificaciones
- Thesis Ethics PaperDocumento7 páginasThesis Ethics Paperlaurenbrownprovo100% (2)
- Dilemma and Moral DilemmaDocumento20 páginasDilemma and Moral DilemmaCaressa Velasco100% (1)
- Group 4 Ethics Bpa 1hDocumento28 páginasGroup 4 Ethics Bpa 1heriksonmartin49Aún no hay calificaciones
- Ethical Concerns in Government, Ethical Dilemmas in Private InstitutionsDocumento11 páginasEthical Concerns in Government, Ethical Dilemmas in Private InstitutionsGodha Kirana50% (2)
- Final Project in EthicsDocumento5 páginasFinal Project in EthicsEmieline AretaAún no hay calificaciones
- APA TemplateDocumento6 páginasAPA TemplateKamrul Hasan Sihab 212-11-1273Aún no hay calificaciones
- Brian Ven Climaco Bag-AoDocumento146 páginasBrian Ven Climaco Bag-Aosalman arompacAún no hay calificaciones
- Learning Packet 1 Introduction Key Concepts Updated For Nursing Students EditedDocumento15 páginasLearning Packet 1 Introduction Key Concepts Updated For Nursing Students EditedJhon Mhark GarinAún no hay calificaciones
- Medical Ethics Thesis TopicsDocumento7 páginasMedical Ethics Thesis Topicsygsyoeikd100% (2)
- A Question of Ethics Research and PractiDocumento13 páginasA Question of Ethics Research and PractiEDWIN CASTROAún no hay calificaciones
- A Framework For Ethical Decision MakingDocumento4 páginasA Framework For Ethical Decision MakingShiella Mae GrantosAún no hay calificaciones
- 1 - Introduction To EthicsDocumento70 páginas1 - Introduction To EthicsMohammed HussienAún no hay calificaciones
- A Framework For Ethical Decision MakingDocumento15 páginasA Framework For Ethical Decision MakingNarendra KumarAún no hay calificaciones
- Ethical Decision MakingDocumento23 páginasEthical Decision MakingMuhammad Na'im100% (9)
- Medical Ethics: DR - Nirmal K Meena Dept. of PSM RNT Medical College, UdaipurDocumento46 páginasMedical Ethics: DR - Nirmal K Meena Dept. of PSM RNT Medical College, UdaipurMysweet PenAún no hay calificaciones
- Ethics Oral RecitDocumento8 páginasEthics Oral RecitLei PangilinanAún no hay calificaciones
- Lecture 1 Role of Family and Society Lyst6297 240129 081145Documento15 páginasLecture 1 Role of Family and Society Lyst6297 240129 081145Pragnya ChowdharyAún no hay calificaciones
- Module 2 ReviewerDocumento8 páginasModule 2 ReviewerElmeerajh JudavarAún no hay calificaciones
- Guidance Note EthicsDocumento8 páginasGuidance Note EthicsSokhoeurn MourAún no hay calificaciones
- Cs 332 ReviewerDocumento3 páginasCs 332 ReviewerShenel SambranoAún no hay calificaciones
- Things Are Intrinsically and Instrumentally Good or Bad? and Give Examples of Things Intrinsically and Instrumentally Good or Bad in Your SocietyDocumento8 páginasThings Are Intrinsically and Instrumentally Good or Bad? and Give Examples of Things Intrinsically and Instrumentally Good or Bad in Your SocietyAbenezer SisayAún no hay calificaciones
- TesDocumento4 páginasTesRezki FahnisaAún no hay calificaciones
- Ethics - Module 2Documento3 páginasEthics - Module 2John michael AguharAún no hay calificaciones
- Medical Ethics LDocumento28 páginasMedical Ethics Lalmastar officeAún no hay calificaciones
- Introduction To Indonesian Code of EthicsDocumento21 páginasIntroduction To Indonesian Code of EthicsLady KweeAún no hay calificaciones
- Week 6 2013 - Ethics LectureDocumento27 páginasWeek 6 2013 - Ethics LectureGene Shav FalconerAún no hay calificaciones
- Ethical Decision Making Written ReportDocumento10 páginasEthical Decision Making Written ReportMateo MascardoAún no hay calificaciones
- 1notebook - Gs 4Documento4 páginas1notebook - Gs 4pragya singhAún no hay calificaciones
- A Framework For Ethical Decision Making - Markkula Center For Applied EthicsDocumento7 páginasA Framework For Ethical Decision Making - Markkula Center For Applied EthicsPeter BarnettAún no hay calificaciones
- The Golden Thread: Making Healthcare Decisions in NeighborhoodsDe EverandThe Golden Thread: Making Healthcare Decisions in NeighborhoodsAún no hay calificaciones
- Running Head: Social Ethics in The Community 1Documento10 páginasRunning Head: Social Ethics in The Community 1Erick OgolaAún no hay calificaciones
- LWS101 Week 2 Ethics PPTslidesDocumento44 páginasLWS101 Week 2 Ethics PPTslidesJanet YauAún no hay calificaciones
- Order 6996794.editedDocumento5 páginasOrder 6996794.editedproficientwriters476Aún no hay calificaciones
- Ethical TheoriesDocumento5 páginasEthical Theoriesapi-749269676Aún no hay calificaciones
- Medical Ethics and ProfessionalismDocumento71 páginasMedical Ethics and ProfessionalismHaymanot GirmaAún no hay calificaciones
- Ethics QuizDocumento3 páginasEthics QuizathierahAún no hay calificaciones
- Ethics and Art of Chart Noting Most Recent LGG STDocumento28 páginasEthics and Art of Chart Noting Most Recent LGG STapi-136237609Aún no hay calificaciones
- Ethical Insights For Addressing Conflict Between Families and The Medical Team RevDocumento27 páginasEthical Insights For Addressing Conflict Between Families and The Medical Team Revapi-136237609Aún no hay calificaciones
- Ethics and The Covid-19 Pandemic Everyday Challenges Uams LGG No NarrationDocumento42 páginasEthics and The Covid-19 Pandemic Everyday Challenges Uams LGG No Narrationapi-136237609Aún no hay calificaciones
- Understanding Autonomy in Psychiatric Care Psych Residency 10-11-18Documento17 páginasUnderstanding Autonomy in Psychiatric Care Psych Residency 10-11-18api-136237609Aún no hay calificaciones
- Threshold Elements - Voluntariness and CapacityDocumento18 páginasThreshold Elements - Voluntariness and Capacityapi-136237609Aún no hay calificaciones
- L G - G, P D: Assistant Professor of Medical Humanities & Bioethics Clinical EthicistDocumento35 páginasL G - G, P D: Assistant Professor of Medical Humanities & Bioethics Clinical Ethicistapi-136237609Aún no hay calificaciones
- This Again - Managing The Weight of Moral Distress LGG JWDocumento17 páginasThis Again - Managing The Weight of Moral Distress LGG JWapi-136237609Aún no hay calificaciones
- Moral Distress LGGDocumento17 páginasMoral Distress LGGapi-136237609Aún no hay calificaciones
- Ethical Dilemmas in The Pediatric Emergency Room LGGDocumento35 páginasEthical Dilemmas in The Pediatric Emergency Room LGGapi-136237609Aún no hay calificaciones
- Patient Rights LGGDocumento13 páginasPatient Rights LGGapi-136237609Aún no hay calificaciones
- Eric James F. Regoso, RN: ResponsibilitiesDocumento2 páginasEric James F. Regoso, RN: ResponsibilitiesPrincess Sardea-RegosoAún no hay calificaciones
- Ie2 Ce Tissue ManagementDocumento9 páginasIe2 Ce Tissue Managementh20pologtAún no hay calificaciones
- Case Study ON Hodgkin LymphomaDocumento8 páginasCase Study ON Hodgkin LymphomaMeena KoushalAún no hay calificaciones
- Project DescriptionDocumento2 páginasProject DescriptionArgha PaulAún no hay calificaciones
- AntidoteDocumento4 páginasAntidoteAnnalou Amadure Joaquin100% (1)
- The Impact of Therapeutic Community in Cagayan de Oro CityDocumento9 páginasThe Impact of Therapeutic Community in Cagayan de Oro CityJames BoundAún no hay calificaciones
- Crisis Intervention: Srinivasan ADocumento12 páginasCrisis Intervention: Srinivasan AsrinivasanaAún no hay calificaciones
- Journal of Pharmaceutical Sciences Volume 66 Issue 1 1977 (Doi 10.1002/jps.2600660104) Stephen M. Berge Lyle D. Bighley Donald C. Monkhouse - Pharmaceutical Salts PDFDocumento19 páginasJournal of Pharmaceutical Sciences Volume 66 Issue 1 1977 (Doi 10.1002/jps.2600660104) Stephen M. Berge Lyle D. Bighley Donald C. Monkhouse - Pharmaceutical Salts PDFDilipKumarTampulaAún no hay calificaciones
- Innovation Runs Deep: Accent The BenefitsDocumento2 páginasInnovation Runs Deep: Accent The BenefitsJavier De Aramburú PalermoAún no hay calificaciones
- Case Scenario AnalysisDocumento2 páginasCase Scenario AnalysisAmbot sa ImoAún no hay calificaciones
- Ovh and Castration NotesDocumento4 páginasOvh and Castration Notesapi-268411828Aún no hay calificaciones
- Hipopresivos, Eficaces o MarketingDocumento3 páginasHipopresivos, Eficaces o MarketingJaviMéndezAún no hay calificaciones
- KrokodilDocumento6 páginasKrokodilapi-252934043Aún no hay calificaciones
- Hospital Hygienic Laundry SystemDocumento34 páginasHospital Hygienic Laundry SystemEngr Awais Tahir MughalAún no hay calificaciones
- First Aid Procedure (Revised) 0-dDocumento19 páginasFirst Aid Procedure (Revised) 0-dFarizan BolkafliAún no hay calificaciones
- DDHDocumento30 páginasDDHsayedmAún no hay calificaciones
- Renal PhysiologyDocumento5 páginasRenal PhysiologyJayricDepalobosAún no hay calificaciones
- Peds Drug Mixing PDFDocumento18 páginasPeds Drug Mixing PDFeialcaheAún no hay calificaciones
- Guideline of Record-KeepingDocumento9 páginasGuideline of Record-KeepingGen LCAún no hay calificaciones
- Klinik Berhenti Merokok - Edited PDFDocumento47 páginasKlinik Berhenti Merokok - Edited PDFMuhammad Daniala SyuhadaAún no hay calificaciones
- Drug Study 3Documento2 páginasDrug Study 3Joshua Selwyn SalazarAún no hay calificaciones
- James M. Ellison, Helen H. Kyomen, Sumer Verma - Mood Disorders in Later Life, 2nd (2008) PDFDocumento394 páginasJames M. Ellison, Helen H. Kyomen, Sumer Verma - Mood Disorders in Later Life, 2nd (2008) PDFJaime Fernández-Aguirrebengoa100% (1)
- An Anatomic Technique For Establishing Leg Length During The Anterior Approach To Total Hip ArthroplastyDocumento5 páginasAn Anatomic Technique For Establishing Leg Length During The Anterior Approach To Total Hip Arthroplasty阿欧有怪兽Aún no hay calificaciones
- 10 Foods That Fight Visceral Belly Fat 0501Documento43 páginas10 Foods That Fight Visceral Belly Fat 0501Elvitz Valenzuela100% (2)
- Wound Care and Dressing ChecklistDocumento4 páginasWound Care and Dressing ChecklistGelo BallartaAún no hay calificaciones
- A New Simple Technique For Making Facial DimplesDocumento4 páginasA New Simple Technique For Making Facial DimplesdoctorbanAún no hay calificaciones
- MAXICAREDocumento8 páginasMAXICARERachelle BataoilAún no hay calificaciones