Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Hypertension in Pregnancy-Latest
Cargado por
shahiraaz0 calificaciones0% encontró este documento útil (0 votos)
75 vistas32 páginasmim
Título original
Hypertension in Pregnancy-latest
Derechos de autor
© © All Rights Reserved
Formatos disponibles
PPT, PDF, TXT o lea en línea desde Scribd
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentomim
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PPT, PDF, TXT o lea en línea desde Scribd
0 calificaciones0% encontró este documento útil (0 votos)
75 vistas32 páginasHypertension in Pregnancy-Latest
Cargado por
shahiraazmim
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PPT, PDF, TXT o lea en línea desde Scribd
Está en la página 1de 32
Jumarni Binti Abdurachman
Aizuddin Azim Bin Zainuddin
Definition
Chronic HPT
Gestational HPT (PIH)
Pre-eclampsia
Eclampsia
Raised BP; EITHER
Systolic BP > 140mmHg previously
normotensive
Diastolic BP > 90mmHg
An increase of 15 mmHg and 30 mmHg diastolic and
systolic BP levels above baseline BP is no longer
recognized as hypertension if absolute values are below
140/90 mmHg. Nevertheless, this warrants close
observation, especially if proteinuria and hyperuricaemia
are also present (CPG 2008)
Chronic hypertension - hypertension that is present at the booking visit or
before 20 weeks or if the woman is already taking antihypertensive
medication when referred to maternity services. It can be primary or
secondary in etiology.
Eclampsia - convulsive condition associated with pre-eclampsia.
Gestational hypertension (PIH) - is new hypertension presenting after 20
weeks without significant proteinuria.
Pre-eclampsia - new hypertension presenting after 20 weeks with significant
proteinuria.
Severe pre-eclampsia - pre-eclampsia with severe hypertension and/or with
symptoms, and/or biochemical and/or haematological impairment.
Significant proteinuria- if the urinary protein:creatinine ratio is greater than 30
mg/mmol or a validated 24-hour urine collection result shows greater than 300
mg protein.
New onset of hypertension after
20 weeks gestation
Molar
pregnancy
Primigravida
Multiple
pregnancy
DM
Polyhydramnios
Hydrop
fetalis
Previous
h/o PIH
Maternal Fetus
Eclampsia
Renal failure
Thrombocytopenia
Abruptio placenta
Sub-capsular hemorrhage
and liver dysfunction
-- HELLP
Heart failure
Pulmonary oedema
Retinal hemorrhage
IUGR
Fetal hypoxia &
IUD
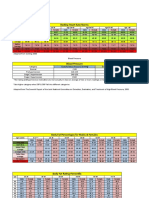
Degree of hypertension
Mild hypertension
(140/90 to 149/99
mmHg)
Moderate hypertension
(150/100 to
159/109 mmHg)
Severe hypertension
(160/110 mmHg or
higher)
Admit to hospital
No Yes Yes (until blood pressure is
159/109 mmHg or lower)
Treat
No oral labetalol as first-line
treatment to keep:
diastolic blood pressure
between 80100 mmHg
systolic blood pressure less
than 150 mmHg
oral labetalol as first-line
treatment to keep:
diastolic blood pressure
between 80100 mmHg
systolic blood pressure
less than 150 mmHg
Measure blood pressure
Not more than once a
week
At least twice a week
At least four times a day
Test for proteinuria
At each visit
At each visit Daily
Blood tests
Only those for routine
antenatal care
Test kidney function,
electrolytes, full blood count,
transaminases, bilirubin
# Do not carry out further
blood tests if no proteinuria at
subsequent visits
Test at presentation and
then monitor weekly:
kidney function,
electrolytes, full blood
count, transaminases,
bilirubin
Fetal kick chart
Daily CTG
U/S (detect growth restriction- fetal growth &
AFI)
Umbilical blood flow monitoring by doppler
SHOULD NOT USE:
ACE inhibitors
blocker agent (propanolol) : a/w fetal growth
restriction in long term use
Diuretics : reduce plasma volume thus may cause
IUGR
DO NOT REDUCE blood pressure TOO QUICKLY. It
may compromise utero-placental blood flow
Only CURE is
DELIVERY
Indications for delivery
Inability to control maternal
blood pressure
Progressive deterioration in
renal/hepatic function
Signs/symptoms of impending
eclampsia
Progressive thrombocytopenia
Severe IUGR/signs of fetal
distress
Hypertension that is present at the booking
visit or before 20 weeks or if the woman is
already taking antihypertensive medication
when referred to maternity services. It can
be primary or secondary in etiology.
Renal disease - Glomerulonephritis
- Renal artery stenosis
- Diabetic nephropathy
- Polycystic kidneys
Endocrine causes - Phaechromocytoma
- Conns Syndrome
- Cushings
Others -Coarctation of aorta
Women with chronic hypertension may require a
change in the type of antihypertensive agent
used pre-pregnancy
The drugs of choice in pregnancy:
Methyldopa
labetalol
Atenolol has been shown to lead to fetal growth
restriction.
The use of ARBs & ACEIs is contraindicated in
pregnancy.
High blood pressure with proteinuria
Also known as
Gestational proteinuric hypertension
Preeclamptic toxemia (PET)
Affects many organs i.e. placenta, kidney,
liver, heart, brain
Reduced blood flow
Clinically diagnosed in the presence of de novo hypertension after gestational
week 20, and one or more of the following:
i. Significant proteinuria.
ii. Renal insufficiency: serum creatinine >90 mol/l or oliguria.
iii. Liver disease: raised transaminases and/or severe right upper quadrant or
epigastric pain.
iv. Neurological problems: convulsions (eclampsia), hyperreflexia with clonus or
severe headaches, persistent visual disturbances (scotoma).
v. Haematological disturbances: thrombocytopenia, coagulopathy, haemolysis.
vi. Fetal growth restriction.
This is followed by normalisation of the BP by three months postpartum.
Oedema is no longer part of the definition of preeclampsia. Either excessive
weight gain or failure to gain weight in pregnancy may herald the onset of
preeclampsia.
Moderate risk
Primigravida
Extremes of age (<20, >40)
Pregnancy interval >10 years
Family history of pre-eclampsia
Multiple pregnancy
High risk
Hypertensive disease in previous pregnancies
Chronic kidney disease
Autoimmune (e.g. SLE, antiphospholipid
syndrome)
Diabetes mellitus
Chronic HPT
Maternal
Eclampsia
Renal failure
Thrombocytopenia
Abruptio placenta
HELLP (hemolysis, elevated liver enzymes, lo platelet
count)
Heart failure
Pulmonary edema
Retinal hemorrhage *fundoscopy during physical
examination
Fetal (reduced placental blood flow)
IUGR
Fetal hypoxia
Intrauterine death (IUD)
Headache
Nausea, vomitting
Blurring of vision, papilloedema
Hyperreflexia
Epigastric pain liver involvement
Sudden increase of edema (e.g. facial
puffiness)
Lethargy hemolytic anemia
Routine test
Full blood count
Hb anemia
Platelet count <150
Liver function
Elevated liver enzymes (e.g. AST)
Renal values
Serum creatinine >150 umol/L
Serum uric acid >5.6 mg/dL
Sensitive indicator of renal damage in pre-
eclampsia
Oliguria <500mL/24hr
Proteinuria
Proteinuria
1. 24-hour urine protein
>300mg/ 24hr significant
>5g/ 24hr impending eclampsia
2. Urine dipstick
+, ++ or +++
To rule out renal disease, UTI,
contamination, etc
Transabdominal ultrasound to look for
growth restriction (abdominal circumference)
Doppler ultrasound to assess umbilical
artery blood flow
Cardiotocography
Fetal kick chart
Cure: To deliver
Same as gestational hypertension in
pregnancy
High BP, proteinuria + convulsion
Life-threatening, an obstetric emergency
Secure airway
Keep patient at left lateral decubitus position
Reduce risk of aspiration
Improves uterine blood flow (relieves obstruction
of vena cava by gravid uterus)
Protect patient from injuring herself
IV MgSO4 4g for 5 min
Then, 1g/hr for 24 hours
Further dose of 2-4g for 5 min
if recurrent seizures
If BP high, IV bolus Labetolol 20mg
Consider delivery of baby
Do vaginal examination for possibility of
vaginal delivery
If not possible, do caesarean section
También podría gustarte
- Cardiopulmonary NPTE Questions FlashcardsDocumento61 páginasCardiopulmonary NPTE Questions Flashcardsdina sharaf100% (4)
- Exercise Physiology Lab ReportDocumento9 páginasExercise Physiology Lab Reporthumzak199286% (7)
- Forceps Delivery For Gravidocardiac PatientsDocumento80 páginasForceps Delivery For Gravidocardiac PatientsTots A. Macahilo-LayawonAún no hay calificaciones
- 10.cephalopelvic DisproportionDocumento2 páginas10.cephalopelvic DisproportionSiti Shafariah100% (1)
- 11-Vital Signs Unit 12 To 17Documento74 páginas11-Vital Signs Unit 12 To 17Rashid HussainAún no hay calificaciones
- C+F-Intracranial Pressure in Dogs and CatsDocumento13 páginasC+F-Intracranial Pressure in Dogs and Catstaner_soysuren100% (2)
- 1 - Presentation - Management of Preclamplsia, Mild and ModerateDocumento22 páginas1 - Presentation - Management of Preclamplsia, Mild and ModeratesharonAún no hay calificaciones
- Hypertension Lecture For Cci 2013Documento74 páginasHypertension Lecture For Cci 2013Hannie CruelAún no hay calificaciones
- Hypertensive Disorder in PregnancyDocumento56 páginasHypertensive Disorder in PregnancyESCA GabrielAún no hay calificaciones
- Hypertension in Pregnancy CompiledDocumento67 páginasHypertension in Pregnancy CompiledRaiza Love Caparas-PablicoAún no hay calificaciones
- Ectopic Pregnancy: DR .Urmila KarkiDocumento27 páginasEctopic Pregnancy: DR .Urmila KarkiBasudev chAún no hay calificaciones
- How To Read A CTGDocumento11 páginasHow To Read A CTGiwennieAún no hay calificaciones
- Hydatidiform MoleDocumento10 páginasHydatidiform MoleLisa TurnerAún no hay calificaciones
- Gastric CancerDocumento7 páginasGastric CancerMicah PingawanAún no hay calificaciones
- Posterior Urethral ValveDocumento6 páginasPosterior Urethral ValveMustafa AadanAún no hay calificaciones
- What Is A Retained Placenta?Documento4 páginasWhat Is A Retained Placenta?Baharudin Yusuf Ramadhani0% (1)
- Myoma UteriDocumento21 páginasMyoma UteriLangitBiruAún no hay calificaciones
- Antenatal Obstetric ComplicationsDocumento40 páginasAntenatal Obstetric ComplicationsArhum SiddiqiAún no hay calificaciones
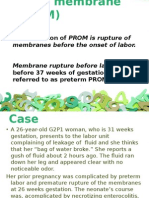
- Preterm Prelabour Rupture of MembranesDocumento12 páginasPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanAún no hay calificaciones
- PPROMDocumento63 páginasPPROMSaraMohammedAún no hay calificaciones
- IUGRDocumento22 páginasIUGRSairindri SahooAún no hay calificaciones
- Ectopic PregnancyDocumento11 páginasEctopic PregnancyPrincess BalloAún no hay calificaciones
- PPH Introduction 1Documento95 páginasPPH Introduction 1regine maeAún no hay calificaciones
- PIHDocumento18 páginasPIHArtyom GranovskiyAún no hay calificaciones
- Antepartum Haemorrhage MXDocumento22 páginasAntepartum Haemorrhage MXAmir Hilmi Abd AzizAún no hay calificaciones
- Hyper Emesis GravidarumDocumento22 páginasHyper Emesis Gravidarumchandu ranaAún no hay calificaciones
- Anticougulation in PregnancyDocumento21 páginasAnticougulation in PregnancyLubna AliAún no hay calificaciones
- Poly and OligohydramniosDocumento39 páginasPoly and OligohydramniosMohamed Atef MohamedAún no hay calificaciones
- A Nursing Case Study On EctopicPregnancy PDFDocumento60 páginasA Nursing Case Study On EctopicPregnancy PDFSteffiAún no hay calificaciones
- Complications of The Third Stage of LabourDocumento6 páginasComplications of The Third Stage of LabourSong QianAún no hay calificaciones
- Shoulder DystociaDocumento27 páginasShoulder DystociaSameena ParikhAún no hay calificaciones
- Per Vaginal Bleeding in PregnancyDocumento33 páginasPer Vaginal Bleeding in PregnancyKai Wei LimAún no hay calificaciones
- Abruptio Placenta B-1Documento29 páginasAbruptio Placenta B-1drsachinhAún no hay calificaciones
- Intrauterine Fetal DemiseDocumento7 páginasIntrauterine Fetal DemiseElaisa Mae Delos SantosAún no hay calificaciones
- 26a. Post Partum HemorrhageDocumento35 páginas26a. Post Partum HemorrhageAubrey100% (1)
- Pelvic Organ ProlapseDocumento68 páginasPelvic Organ ProlapseAlyanna CrisologoAún no hay calificaciones
- 2016 Chronic Hypertension in PregnancyDocumento13 páginas2016 Chronic Hypertension in PregnancydkasisAún no hay calificaciones
- CPD, Dystocia, Fetal Distress OutputDocumento8 páginasCPD, Dystocia, Fetal Distress OutputJohn Dave AbranAún no hay calificaciones
- Anaemia in Pregnancy md3 MhsDocumento26 páginasAnaemia in Pregnancy md3 MhsjerrydanfordfxAún no hay calificaciones
- Hypertension in Pregnancy: Topic List: May 14, 2012Documento55 páginasHypertension in Pregnancy: Topic List: May 14, 2012Karl-Heinz Leonhardt RowikaAún no hay calificaciones
- Amniotic Fluid Embolism (AFE)Documento26 páginasAmniotic Fluid Embolism (AFE)sanjivdas100% (1)
- PIHDocumento30 páginasPIHPatcharavit PloynumponAún no hay calificaciones
- Acute Cholecystitis Ppt. DR Dilip S. RajpalDocumento42 páginasAcute Cholecystitis Ppt. DR Dilip S. Rajpaldiliprajpal73100% (1)
- Anaemia in PregnancyDocumento28 páginasAnaemia in PregnancyUsman G. HingoroAún no hay calificaciones
- And Vaginal Bleeding (In Ruptured Ectopic Pregnancy)Documento9 páginasAnd Vaginal Bleeding (In Ruptured Ectopic Pregnancy)Clareen JuanicoAún no hay calificaciones
- Session13 - Endometrial CaDocumento27 páginasSession13 - Endometrial CaCHALIE MEQUAún no hay calificaciones
- PROM SANJIDA FInal 2Documento32 páginasPROM SANJIDA FInal 2Saiful islam RonyAún no hay calificaciones
- Endometrial Polyps: Irregular Menstrual BleedingDocumento4 páginasEndometrial Polyps: Irregular Menstrual BleedingLuke ObusanAún no hay calificaciones
- Hep B in PregnancyDocumento42 páginasHep B in PregnancyAbraham ChiuAún no hay calificaciones
- Ectopic PregnancyDocumento26 páginasEctopic PregnancyDavid SitinjakAún no hay calificaciones
- Preeclampsia: Clinical Features and Diagnosis - UpToDateDocumento70 páginasPreeclampsia: Clinical Features and Diagnosis - UpToDateMaria Belen LoorAún no hay calificaciones
- OB Lec ArellanoDocumento834 páginasOB Lec Arellanoervin_agena394Aún no hay calificaciones
- Definition of Placenta PreviaDocumento3 páginasDefinition of Placenta Previashan6ersAún no hay calificaciones
- 68 Abnormal PeuperiumDocumento44 páginas68 Abnormal PeuperiumGodsonYeboah-AwudziAún no hay calificaciones
- Pelvic Inflammatory DiseaseDocumento3 páginasPelvic Inflammatory DiseaseokaciaAún no hay calificaciones
- 16 Amniotic Fluid EmbolismDocumento46 páginas16 Amniotic Fluid EmbolismAhmed TarigAún no hay calificaciones
- Multiple Pregnancy: Dr. A. Farid Abdullah, SP - OG, M.KesDocumento33 páginasMultiple Pregnancy: Dr. A. Farid Abdullah, SP - OG, M.KesAndi Farid AAún no hay calificaciones
- DVT in PregDocumento2 páginasDVT in Pregkhadzx100% (2)
- Hellp Syndrome: Prepared By: Jamie Niña Faye CDocumento10 páginasHellp Syndrome: Prepared By: Jamie Niña Faye CJamie DyAún no hay calificaciones
- Anaemia in PregnancyDocumento41 páginasAnaemia in PregnancyWan Ahmad FaizFaizalAún no hay calificaciones
- THROMBOPHLEBITISDocumento50 páginasTHROMBOPHLEBITISmers puno100% (3)
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAún no hay calificaciones
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAún no hay calificaciones
- Handling Prolongation ClaimsDocumento17 páginasHandling Prolongation ClaimsshahiraazAún no hay calificaciones
- Assessment of Damages in Tort and ContractDocumento14 páginasAssessment of Damages in Tort and ContractshahiraazAún no hay calificaciones
- CLJ 2001 8 71 Zulrafiq101Documento9 páginasCLJ 2001 8 71 Zulrafiq101shahiraazAún no hay calificaciones
- Chia See Yin & OrsDocumento12 páginasChia See Yin & OrsshahiraazAún no hay calificaciones
- Occupational Safety, Health and Environmental Management and The Law of Negligence in MalaysiaDocumento14 páginasOccupational Safety, Health and Environmental Management and The Law of Negligence in MalaysiashahiraazAún no hay calificaciones
- Wisma Sime Darby SDN BHD V Wilson Parking (M) SDN BHD: Prepared By: Nurul Atilia Shahira ZulkifliDocumento3 páginasWisma Sime Darby SDN BHD V Wilson Parking (M) SDN BHD: Prepared By: Nurul Atilia Shahira Zulkiflishahiraaz100% (1)
- Psychiatric EmergenciesDocumento27 páginasPsychiatric EmergenciesshahiraazAún no hay calificaciones
- Expected Autopsy Findings: - BrainDocumento3 páginasExpected Autopsy Findings: - BrainshahiraazAún no hay calificaciones
- Vital SignDocumento6 páginasVital SignElsye FitriasariAún no hay calificaciones
- Hemodynamic MonitoringDocumento10 páginasHemodynamic MonitoringDivya Joy100% (1)
- 3 Series Upper Arm Blood Pressure Monitor: Instruction ManualDocumento30 páginas3 Series Upper Arm Blood Pressure Monitor: Instruction ManualAlAún no hay calificaciones
- Effects of Electromagnetic Forces of Earth On HumansDocumento6 páginasEffects of Electromagnetic Forces of Earth On HumansArtist MetuAún no hay calificaciones
- Congestive Heart Failure (CHF) : Causes DiagnosisDocumento6 páginasCongestive Heart Failure (CHF) : Causes DiagnosisSOPHIA LOISE TEJANO FULACHEAún no hay calificaciones
- Kevin M O'saugnesi: Tavi 24 Arteriuli Hipertenzia, Stenokardia, Miokardiumis Infarqti Da Gulis UkmarisobaDocumento47 páginasKevin M O'saugnesi: Tavi 24 Arteriuli Hipertenzia, Stenokardia, Miokardiumis Infarqti Da Gulis UkmarisobaTamari AbesadzeAún no hay calificaciones
- SHAKTI THAKUR MedicalDocumento3 páginasSHAKTI THAKUR MedicalNokia5gMHPartner's ReportsAún no hay calificaciones
- Resting Heart Rate NormsDocumento3 páginasResting Heart Rate Normstre100% (1)
- GE Dinamap Pro 110-410 - Service ManualDocumento42 páginasGE Dinamap Pro 110-410 - Service ManualNGUYEN TAN KHUONGAún no hay calificaciones
- Arterial Blood Pressure RegulationDocumento21 páginasArterial Blood Pressure Regulationnaresh sharmaAún no hay calificaciones
- Weight-Bearing Exercise For Better Balance (WEBB)Documento44 páginasWeight-Bearing Exercise For Better Balance (WEBB)Neha BhasinAún no hay calificaciones
- Rheumatic Fever and Rheumatic Heart Disease: PediatricsDocumento8 páginasRheumatic Fever and Rheumatic Heart Disease: PediatricsRea Dominique CabanillaAún no hay calificaciones
- Pregnancy & Its Anaesthetic ImplicationsDocumento29 páginasPregnancy & Its Anaesthetic ImplicationsDadik WijayaAún no hay calificaciones
- Autonomic Nervous System Activity in Emotion: A Review: Sylvia D. KreibigDocumento52 páginasAutonomic Nervous System Activity in Emotion: A Review: Sylvia D. KreibigeddyputriAún no hay calificaciones
- Gilbert - Cardiac Output MeasurementDocumento7 páginasGilbert - Cardiac Output MeasurementCaos_123100% (1)
- Preeclampsia Case StudyDocumento13 páginasPreeclampsia Case StudyBiway RegalaAún no hay calificaciones
- RESEARCH Chapter 1Documento18 páginasRESEARCH Chapter 1Shadab28Aún no hay calificaciones
- Overview of Hypertension in AdultsDocumento27 páginasOverview of Hypertension in AdultsMedByteAún no hay calificaciones
- EMT Basic Hemorrhage and ShockDocumento71 páginasEMT Basic Hemorrhage and ShockPaul VogtAún no hay calificaciones
- Chapter 15: Cardiovascular System: Shier, Butler, and Lewis: Hole's Human Anatomy and Physiology, 13Documento26 páginasChapter 15: Cardiovascular System: Shier, Butler, and Lewis: Hole's Human Anatomy and Physiology, 13Elvin MoletaAún no hay calificaciones
- Hypertension in ChildrenDocumento32 páginasHypertension in ChildrenmikhaelyosiaAún no hay calificaciones
- Tintinalli Shock PDFDocumento13 páginasTintinalli Shock PDFfueny8gmailAún no hay calificaciones
- Hypertensive Disorders in Pregnancy: 2019 National GuidelineDocumento14 páginasHypertensive Disorders in Pregnancy: 2019 National GuidelinerizkaAún no hay calificaciones
- Gunshot WoundsDocumento36 páginasGunshot Woundschrisr3100% (1)
- Arterial LinesDocumento38 páginasArterial LinesRabeed MohammedAún no hay calificaciones