Documentos de Académico
Documentos de Profesional
Documentos de Cultura
ECG Criteria For LVH
Cargado por
Leichombam DeepakDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
ECG Criteria For LVH
Cargado por
Leichombam DeepakCopyright:
Formatos disponibles
ECG criteria for LVH
There are several sets of criteria used to diagnose LVH via electrocardiography.[3] None of them is perfect, though by using multiple criteria sets, the sensitivity and specificity are increased. The Sokolow-Lyon index[4][5]: S in V1 + R in V5 or V6 (whichever is larger) 35 mm ( 7 large squares) R in aVL 11 mm The Cornell voltage criteria[6] for the ECG diagnosis of LVH involve measurement of the sum of the R wave in lead aVL and the S wave in lead V3. The Cornell criteria for LVH are:
S in V3 + R in aVL > 28 mm (men) S in V3 + R in aVL > 20 mm (women) The Romhilt-Estes point score system ("diagnostic" >5 points; "probable" 4 points):
ECG Criteria Voltage Criteria (any of): 1. R or S in limb leads 20 mm 2. S in V1 or V2 30 mm 3. R in V5 or V6 30 mm ST-T Abnormalities:
Points
ST-T vector opposite to QRS without digitalis
3 1 3 2 1
ST-T vector opposite to QRS with digitalis Negative terminal P mode in V1 1 mm in depth and 0.04 sec in duration (indicates left atrial enlargement) Left axis deviation (QRS of -30 or more) QRS duration 0.09 sec
Delayed intrinsicoid deflection in V5 or V6 (>0.05 sec)
Other voltage-based criteria for LVH include:
Lead I: R wave > 14 mm Lead aVR: S wave > 15 mm Lead aVL: R wave > 12 mm Lead aVF: R wave > 21 mm Lead V5: R wave > 26 mm Lead V6: R wave > 20 mm
[edit]
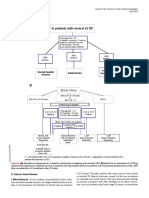
If there is left ventricular hypertrophy then this will result in :
a tall R wave (greater than 25mm in V5 or V6), or R plus S greater than 35 mm (1) a deep S in V1 or V2 if there is significant left ventricular 'strain' then there are also inverted T waves in V5 and V6 and possible ST depression left axis deviation may also be present QRS may be slightly prolonged
Notes:
a systematic review investigating the accuracy of ECGs in the diagnosis of LVH has been undertaken (2) o from the study data in primary care, a negative electrocardiogram result would reduce the typical pre-test probability from 33% to 31%. In secondary care the typical pre-test probability of 65% would be reduced to 63% o the authors concluded that electrocardiographic criteria should not be used to rule out left ventricular hypertrophy in patients with hypertension
Normal ecg
Diagnosis of myocardial infarction
ST elevation is measured at the junctional or J-point
The diagnosis of acute myocardial infarction is not only based on the ECG. A myocardial infarction is defined as:[2]
Elevated blood levels of cardiac enzymes (CKMB or Troponin T) AND One of the following criteria are met:
The patient has typical complaints, The ECG shows ST elevation or depression. pathological Q waves develop on the ECG A coronary intervention had been performed (such as stent placement)
So detection of elevated serum heartenzymes is more important than ECG changes. However, the cardiac enzymes can only be detected in the serum 5-7 hours after the onset of the myocardial infarction. So, especially in the first few hours after the myocardial infarction, the ECG can be crucial. ECG Manifestations of Acute Myocardial Ischaemia (in Absence of LVH and LBBB)are [3]:
ST elevation New ST elevation at the J-point in two contiguous leads with the cut-off points: 0.2 mV in men or 0.15 mV in women in leads V2V3 and/or 0.1 mV in other leads. ST depression and T-wave changes. New horizontal or down-sloping ST depression >0.05 mV in two contiguous leads; and/or T inversion 0.1 mVin two contiguous leads with prominent R-wave or R/S ratio 1
A study using MRI to diagnose myocardial infarction has shown that more emphasis on ST segment depression could greatly improve the yield of the ECG in the diagnosis of myocardial infarction (sensitivity increase from 50% to 84%).[4] Myocardial infarction diagnosis in left or right bundle branch block can be difficult, but it is explained in these seperate chapters:
Electrocardiogram
ECG of atrial fibrillation (top) and normal sinus rhythm (bottom). The purple arrow indicates a P wave, which is lost in atrial fibrillation.
Atrial fibrillation is diagnosed on an electrocardiogram (ECG), an investigation performed routinely whenever an irregular heart beat is suspected. Characteristic findings are the absence of P waves, with unorganized electrical activity in their place, and irregular R-R intervals due to irregular conduction of impulses to the ventricles.[5] However, irregular R-R intervals may be difficult to determine if the rate is extremely rapid.[10] QRS complexes should be narrow, signifying that they are initiated by normal conduction of atrial electrical activity through the intraventricular conduction system. Wide QRS complexes are worrisome for ventricular tachycardia, although in cases where there is disease of the conduction system, wide complexes may be present in AFib with rapid ventricular response. If paroxysmal AF is suspected but an ECG during an office visit only shows a regular rhythm, AF episodes may be detected and documented with the use of ambulatory Holter monitoring (e.g. for a day). If the episodes are too infrequent to be detected by Holter monitoring with reasonable probability, then the patient can be monitored for longer periods (e.g. a month) with an ambulatory event monitor.[5]
También podría gustarte
- Essential Cardiac Electrophysiology: The Self-Assessment ApproachDe EverandEssential Cardiac Electrophysiology: The Self-Assessment ApproachAún no hay calificaciones
- Basicelectrocardiogram ppt2013Documento134 páginasBasicelectrocardiogram ppt2013Catalin LeonteAún no hay calificaciones
- ECG Reporting: The AtriaDocumento5 páginasECG Reporting: The AtriaakochaAún no hay calificaciones
- ECG InterpretationDocumento83 páginasECG InterpretationJuana Maria Garcia Espinoza100% (2)
- ECG Hipertrofii Atriale Si Ventriculare, Blocuri de Ramura, IschemieDocumento60 páginasECG Hipertrofii Atriale Si Ventriculare, Blocuri de Ramura, IschemieAndreea ŞtefănescuAún no hay calificaciones
- ECG WorldDocumento139 páginasECG WorldsatyaAún no hay calificaciones
- ECG Module PrintableDocumento39 páginasECG Module PrintableAbu HibbaanAún no hay calificaciones
- ECG InterpretationDocumento168 páginasECG InterpretationPavi YaskarthiAún no hay calificaciones
- EKG Self Study GuideDocumento40 páginasEKG Self Study GuideArgee AlonsabeAún no hay calificaciones
- ECG - Module - Printable Analysis and Interpretation of ECGDocumento37 páginasECG - Module - Printable Analysis and Interpretation of ECGPankaj PatilAún no hay calificaciones
- Ecg Reporting: The Atria Normal AtriaDocumento5 páginasEcg Reporting: The Atria Normal AtriaChellamani UmakanthanAún no hay calificaciones
- Normal Atria: o o o o o o oDocumento5 páginasNormal Atria: o o o o o o oPoetraSyah اولياء 花火Aún no hay calificaciones
- ECG Kursus FKUSU DR A.majid 05 Juni 2007Documento37 páginasECG Kursus FKUSU DR A.majid 05 Juni 2007Shinta LissevaAún no hay calificaciones
- ElectrocardiogramDocumento52 páginasElectrocardiogramTuong HoangManhAún no hay calificaciones
- EKG Interpretation: UNS Cardiovascular Dept Medical Student Lecture SeriesDocumento85 páginasEKG Interpretation: UNS Cardiovascular Dept Medical Student Lecture Seriesandina rosmalianti100% (1)
- ECG Interpretation UnismaDocumento178 páginasECG Interpretation UnismadefinaAún no hay calificaciones
- ECG Changes in Left Ventricular HypertrophyDocumento25 páginasECG Changes in Left Ventricular HypertrophyMuhammad AsifAún no hay calificaciones
- Ecg Guidelines: Donna J. Castillo, MDDocumento76 páginasEcg Guidelines: Donna J. Castillo, MDBheck Magat100% (1)
- Basic of EcgDocumento82 páginasBasic of Ecgpopescuioana1Aún no hay calificaciones
- DrAbnet ECG - BasicsDocumento99 páginasDrAbnet ECG - BasicsAbnet WondimuAún no hay calificaciones
- ECG NormalDocumento9 páginasECG NormalDya AndryanAún no hay calificaciones
- Ecg Reading Made EasyDocumento59 páginasEcg Reading Made EasyAngealyn GaviolaAún no hay calificaciones
- ECG and ArrhythmiasDocumento25 páginasECG and ArrhythmiasRashed ShatnawiAún no hay calificaciones
- ElectrocardiogramDocumento11 páginasElectrocardiogramAbby BhevAún no hay calificaciones
- EcgDocumento18 páginasEcgmyla adapAún no hay calificaciones
- Right Ventricular StrainDocumento9 páginasRight Ventricular StrainhasaɴAún no hay calificaciones
- EcgDocumento57 páginasEcgenii_ta100% (9)
- 16-Handout - ECG Interpretation (Study This)Documento38 páginas16-Handout - ECG Interpretation (Study This)Sa GhAún no hay calificaciones
- Lead Avr PDFDocumento9 páginasLead Avr PDFsiddharthAún no hay calificaciones
- INTERPRETASI EKG MahasiswaDocumento43 páginasINTERPRETASI EKG MahasiswaMartin Susanto, MDAún no hay calificaciones
- Ecg Presentation 2013Documento40 páginasEcg Presentation 2013Samuel FpAún no hay calificaciones
- Electrocardiogram (Ecg) Introduction of Basic Principles: Dian Puspita SariDocumento47 páginasElectrocardiogram (Ecg) Introduction of Basic Principles: Dian Puspita SariArie Krisnayanti Ida AyuAún no hay calificaciones
- Basics of ECG: DR Subroto Mandal, MD, DM, DC Associate Professor, CardiologyDocumento206 páginasBasics of ECG: DR Subroto Mandal, MD, DM, DC Associate Professor, CardiologyRavi SharmaAún no hay calificaciones
- ECG A Methodical Approach - Leaflet Print - Patient UKDocumento7 páginasECG A Methodical Approach - Leaflet Print - Patient UKBen MpanzuAún no hay calificaciones
- Didactics ECGDocumento87 páginasDidactics ECGGenesis Poblacion100% (1)
- How To Take and Read An ECG ECG BasicsDocumento7 páginasHow To Take and Read An ECG ECG BasicsJessica Brittain-GeorgeAún no hay calificaciones
- ECG - Complete Heart BlockDocumento2 páginasECG - Complete Heart BlockCsilla DobrescuAún no hay calificaciones
- ECG Ischemie Si InfarctDocumento34 páginasECG Ischemie Si InfarctOana CristinaAún no hay calificaciones
- Electrocardiogram (ECG) : This Is The Lecture No. 4Documento51 páginasElectrocardiogram (ECG) : This Is The Lecture No. 4Aboodsha ShAún no hay calificaciones
- Ecg in DogsDocumento107 páginasEcg in DogsPLABITA GOSWAMI100% (2)
- ECG Brief NotesDocumento5 páginasECG Brief NotesKalpani Malsha UdawelagedaraAún no hay calificaciones
- LI NarvinDocumento14 páginasLI NarvinRosa Nurul FajriAún no hay calificaciones
- Ecg Basics: by DR Bashir Ahmed Dar Chinkipora Sopore Kashmir Associate Professor MedicineDocumento320 páginasEcg Basics: by DR Bashir Ahmed Dar Chinkipora Sopore Kashmir Associate Professor MedicinefarahtayabaAún no hay calificaciones
- ECG For InternsDocumento31 páginasECG For InternsAgus SyaifudinAún no hay calificaciones
- Onderwijs ECG Quiz 2019Documento15 páginasOnderwijs ECG Quiz 2019Kelsey van SonAún no hay calificaciones
- VT Versus SVT (With Aberrancy) : Adapted From, 2019Documento10 páginasVT Versus SVT (With Aberrancy) : Adapted From, 2019wddassdaAún no hay calificaciones
- Ecg Abnormal 1-HpwDocumento77 páginasEcg Abnormal 1-HpwAndre JuliantAún no hay calificaciones
- Ecg PDFDocumento70 páginasEcg PDFlauras3005Aún no hay calificaciones
- Dr. Adeel Ahmed Waheed: House Officer M-4Documento84 páginasDr. Adeel Ahmed Waheed: House Officer M-4Hussain AzharAún no hay calificaciones
- ECG Praktis Sesi 1 RestutiDocumento49 páginasECG Praktis Sesi 1 RestutiKaisun TeoAún no hay calificaciones
- ECG & ArrhythmiasDocumento8 páginasECG & ArrhythmiasDr. SobanAún no hay calificaciones
- Electrocardiograms (Ecgs)Documento86 páginasElectrocardiograms (Ecgs)nana wandhanaAún no hay calificaciones
- Interpreting ECGsDocumento4 páginasInterpreting ECGsdewitt.bernardAún no hay calificaciones
- Ecg Interpretation: Intervals and ComplexesDocumento7 páginasEcg Interpretation: Intervals and ComplexesBobet ReñaAún no hay calificaciones
- Understanding Intracardiac EGMs: A Patient Centered GuideDe EverandUnderstanding Intracardiac EGMs: A Patient Centered GuideAún no hay calificaciones
- ECG/EKG Interpretation: An Easy Approach to Read a 12-Lead ECG and How to Diagnose and Treat ArrhythmiasDe EverandECG/EKG Interpretation: An Easy Approach to Read a 12-Lead ECG and How to Diagnose and Treat ArrhythmiasCalificación: 5 de 5 estrellas5/5 (2)
- EKG Interpretation Basics Guide: Electrocardiogram Heart Rate Determination, Arrhythmia, Cardiac Dysrhythmia, Heart Block Causes, Symptoms, Identification and Medical Treatment Nursing HandbookDe EverandEKG Interpretation Basics Guide: Electrocardiogram Heart Rate Determination, Arrhythmia, Cardiac Dysrhythmia, Heart Block Causes, Symptoms, Identification and Medical Treatment Nursing HandbookAún no hay calificaciones
- 2021-Myocarditis, Pericarditis and Cardiomyopathy After COVID-19 VaccinationDocumento5 páginas2021-Myocarditis, Pericarditis and Cardiomyopathy After COVID-19 Vaccinationseguridadyambiente641Aún no hay calificaciones
- Ainul Haq Report 2Documento27 páginasAinul Haq Report 2Mohd AliAún no hay calificaciones
- GED Life Science 3. Human Body SystemsDocumento5 páginasGED Life Science 3. Human Body SystemsSapa PynGAún no hay calificaciones
- HemiplegiaDocumento22 páginasHemiplegiaunni4u2Aún no hay calificaciones
- JURNAL Diseksi AortaDocumento3 páginasJURNAL Diseksi AortaNurhidayantiAyaMSAún no hay calificaciones
- Regional Anesthesia and OutcomesDocumento5 páginasRegional Anesthesia and OutcomespitriaAún no hay calificaciones
- Metformin Ameliorates Diabetes With Metabolic Syndrome Induced Changes in Experimental RatsDocumento11 páginasMetformin Ameliorates Diabetes With Metabolic Syndrome Induced Changes in Experimental RatsGuadalupe Hernandez EquihuaAún no hay calificaciones
- MCQ Head & NeckDocumento5 páginasMCQ Head & NeckSyafiqah Ahmad100% (2)
- Syncope: By-Dr. Abdul RazakDocumento24 páginasSyncope: By-Dr. Abdul RazakAbdul RazakAún no hay calificaciones
- CH 9, 10 - Questions - TRANSPORT IN ANIMALS, DISEASES AND IMMUNITYDocumento22 páginasCH 9, 10 - Questions - TRANSPORT IN ANIMALS, DISEASES AND IMMUNITYPranitha RaviAún no hay calificaciones
- Why Dont You SmokeDocumento3 páginasWhy Dont You SmokeSholihin KamariAún no hay calificaciones
- Cardiac Ana & DxticsDocumento3 páginasCardiac Ana & Dxticsjames garciaAún no hay calificaciones
- Uses Uses Uses Uses: 3.5Cm 4Cm 4.5Cm 5Cm (F) 5.5Cm (M) Lvs Thick 1.1Cm Basal RV 4Cm Mid RV 3.5CmDocumento3 páginasUses Uses Uses Uses: 3.5Cm 4Cm 4.5Cm 5Cm (F) 5.5Cm (M) Lvs Thick 1.1Cm Basal RV 4Cm Mid RV 3.5CmAna Belen Viteri LuzuriagaAún no hay calificaciones
- Algoritm Disfunctie DiastolicaDocumento1 páginaAlgoritm Disfunctie DiastolicaNeacsu OvidiuAún no hay calificaciones
- Cirrhosis HandbookDocumento11 páginasCirrhosis HandbookJunjunAún no hay calificaciones
- Bedside Hemodynamic MonitoringDocumento26 páginasBedside Hemodynamic MonitoringBrad F LeeAún no hay calificaciones
- Ceu RevalidaDocumento421 páginasCeu RevalidaKENT DANIEL SEGUBIENSEAún no hay calificaciones
- Medical Terminology CH 9Documento104 páginasMedical Terminology CH 9ياسين المسطو100% (1)
- Week 2-Day 2 I. Objectives: S9LT-lab-26Documento5 páginasWeek 2-Day 2 I. Objectives: S9LT-lab-26GinalynMaacAún no hay calificaciones
- Rheumatic Fever and RHD-SA, HS - FIX PDFDocumento48 páginasRheumatic Fever and RHD-SA, HS - FIX PDFSyadza Rhizky Putri AkhmadAún no hay calificaciones
- Mofettes - English PresentationDocumento1 páginaMofettes - English Presentationhotel montanaAún no hay calificaciones
- Miller Anesthesia 7th Ed Chapter 34 Preop EvaluationDocumento66 páginasMiller Anesthesia 7th Ed Chapter 34 Preop Evaluationjbahalkeh100% (1)
- National Consensus On The Cardiological Treatment and Follow-Up of Kawasaki DiseaseDocumento22 páginasNational Consensus On The Cardiological Treatment and Follow-Up of Kawasaki DiseaseRamos Zavala Julio CesarAún no hay calificaciones
- Excess Deaths Involving CVD in England An Anlysis and ExplainerDocumento36 páginasExcess Deaths Involving CVD in England An Anlysis and ExplainerJamie White100% (2)
- Agnitundi Vati PDFDocumento5 páginasAgnitundi Vati PDFmahendra kumar sharmaAún no hay calificaciones
- Ascites of Cardiac Origin in A Dog - A Case StudyDocumento3 páginasAscites of Cardiac Origin in A Dog - A Case StudyFaisal MohommadAún no hay calificaciones
- LawsuitDocumento12 páginasLawsuitEthan SteinAún no hay calificaciones
- Dcia (Deep Circumflex Iliac Artery) FlapDocumento43 páginasDcia (Deep Circumflex Iliac Artery) FlapRohit SharmaAún no hay calificaciones
- Book 1 ExcelDocumento25 páginasBook 1 ExcelPVallAún no hay calificaciones
- Hotel Dpalma, Bandung 16 Maret 2018: Dr. Benny Prasetya PDocumento145 páginasHotel Dpalma, Bandung 16 Maret 2018: Dr. Benny Prasetya PkangheriAún no hay calificaciones