Documentos de Académico
Documentos de Profesional
Documentos de Cultura
White Book
Cargado por
Sharad Indu SaikiaDescripción original:
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
White Book
Cargado por
Sharad Indu SaikiaCopyright:
Formatos disponibles
----------------------- Page 1----------------------WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICINE IN EUROPE Produced by the Section of Physical and Rehabilitation
Medicine, Union Europenne des Mdecins Spcialistes (UEMS), European Board of Physical and Rehabilitation Medicine and Acadmie Europenne de Mdecine de Radaptation in conjunction with European Society for Physical and Rehabilitation Medicine September 2006 ----------------------- Page 2----------------------Editors: Christoph Gutenbrunner Chairman, Professional Practice Committee, UEMS Section of Physical and Rehabili tation Medicine Anthony B. Ward President, UEMS Section of Physical and Rehabilitation Medicine M. Anne Chamberlain President, Acadmie Europenne de Mdecine de Radaptation Contributors: Prof. Andr Bardot (F) Prof. Michel Barat (F) Dr. Laurent Bensoussan (F) Prof. Mihai Berteanu (Ro) Dr. Pedro Cantista (P) Prof. Anne Chamberlain (UK) Dr. Nicolas Christodoulou (Cy) Dr. Alarcos Cieza (D) Prof. Alain Delarque (F) Prof. Jean-Pierre Didier (F) Prof. Veronika Fialka-Moser (A) Prof. Franco Franchignoni (I) Prof. Alessandro Giustini (I) Prof. Christoph Gutenbrunner (D) Prof. Gustaaf Lankhorst (NL) Prof. Lindsay McLellan (UK) Dr. Fernando Parada (P) Prof. Joo Pscoa Pinheiro (P) Prof. Michael Quittan (A) Prof. Bengt Sjlund (S) Prof. Henk Stam (NL) Prof. Gerold Stucki (D)
Prof. Guy Vanderstraeten (B) Dr. Jiri Votava (Cz) Prof. Jean-Michel Viton (F) Dr. Anthony Ward (UK)
Copyright 2006 by Section of Physical and Rehabilitation Medicine and European Bo ard of Physical and Rehabilitation Medicine, Union Europenne des Mdecins Spcialistes (UEMS) and Acadmie Europenne de Mdecine de Rad ptation. ----------------------- Page 3----------------------Foreword his book sets out the position of Physical and Rehabilitation Medicine (PRM ) in Europe. It defines the speTcialty, its work, the competencies of its practitioners and its relationships to other medical disciplines and professions allied to health. It also aims to ensure that PRM is seen as a Europ ean specialty, where high quality practitioners working to good standards of care can practise in accordance with the evidence-base and within the context of their differing national practices. In doing so, the book des cribes training and skills of PRM specialists in detail. It also gives the underlying principles of specialised re habilitation, which will allow policy makers, health planners, medical and paramedical colleagues to identify how PRM works and how it can assist the process of allowing people with disabilities to participate fully in Society. The Book has been produced by the UEMS Section of Physical and Rehabilitation Medicine under the authorship of its President and Chairman of the Professional Practice Committee and the President of the Acadmie Europenne de Mdecine de Radaptation. It has been adopted by the three bodies representing the specialty in Europe as a whole, the Section for Physical and Rehabilitation Medi cine of the Union Europenne des Mdecins Spcialistes, the Acadmie Europenne de Mdecine de Radaptation and the Europ ean Society of Physical and Rehabilitation Medicine, whose participation give it its authori ty. We, the editors have been assisted by the contributions from across Europe, b ut have developed the text in the interests of ensuring a uniform presentation and consistent approach. Consid erable thought has gone into producing a document, which fits into the systems across Europe in the light of some of the national differences. In particular, we would like to thank those who have contributed for their consi derable effort to produce a truly pan-European work: The names have been listed in alphabetical order above. The White Book is available via Sections website on www.euro-prm.org or throug h the General Secretariat of the UEMS Section. ANTHONY B WARD CHRISTOPH GUTENBRUNNER
M. ANNE CHAMBERLAIN President, UEMS Section President, Acadmie Vol. 42 - No. 4 4
Chairman, Professional Practice Committee 289 EUROPA MEDICOPHYSICA
----------------------- Page 4----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN CONTENTS Page Executive Summary 1. Introduction 2. Definitions 2. 2.1 Rehabilitation 292 295 295
295 2. 2.2 Physical and Rehabilitation Medicine 3. Relevance of rehabilitation for people with disabling conditions and to socie ty 296 2. 3.1 Epidemiological aspects 296 2. 3.2 The World Health Organisation Model of Functioning, Disability and Health in Rehabilitation 297 2. 3.3 Ethical aspects and human rights 299 2. 3.4 Rehabilitation and Health Systems 301 2. 3.5 Aims and outcomes of rehabilitation 302 4. Principles of Physical and Rehabilitation Medicine 302 2. 4.1 Learning processes as a basic principle of Physical and Rehabilitation Me dicine 302 2. 4.2 Aims of Physical and Rehabilitation Medicine 303 2. 4.3 The rehabilitation team 303 2. 4.4 Physical and Rehabilitation Medicine in different phases of the rehabilit ation process 304 2. 4.5 Effects of lack of rehabilitation 305 2. 4.6 Prevention 306 5. The Speciality of Physical and Rehabilitation Medicine 307 2. 5.1 Contribution of the Specialist in Physical and Rehabilitation Medicine to the rehabilitation 307 2. 5.1 process 2. 5.2 The Specialty of Physical and Rehabilitation Medicine in Europe 307
2. 5.3 Pathologies and conditions in Physical and Rehabilitation Medicine practi ce 308 2. 5.4 Diagnostics, assessment and evaluation 308 2. 5.5 Rehabilitation plan 309 2. 5.6 Interventions in Physical and Rehabilitation Medicine 309 2. 5.7 Physical and Rehabilitation Medicine practice - Clinical activities and s ettings 310 6. Standards in Physical and Rehabilitation Medicine 311 2. 6.1 Education and training 311 2. 6.2 Clinical Governance and competencies 313 2. 6.3 Continuing Professional Development and Medical Education 314 2. 6.4 The Section of Physical and Rehabilitation Medicine of the Union Europenne des Mdecins 314 2. 5.1 Spcialistes 2. 6.5 The Acadmie Europenne de Mdecine de Radaptation 316 2. 6.6 The European Society of Physical and Rehabilitation Medicine 317 7. Research in Physical and Rehabilitation Medicine 317 2. 7.1 Importance of research in establishing needs and the value of both curren t and new approa317 2. 5.1 ches 2. 7.2 Research facilities and resources 318 2. 7.3 Research training 318 2. 7.4 Publication of research findings 319 8. Future developments 319 2. 8.1 Philosophy 319 2. 8.2 Goals 319 9. References 320 290 December 2006 EUROPA MEDICOPHYSICA
----------------------- Page 5----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC
Page Appendix Ia. el Appendix Ib. tion Medicine Proposal for a new definition based on the ICF- Mod 322 Description of the Specialty of Physical Rehabilita 322
Appendix II. red by PRM SpeciaAppendix III. Appendix IV. habilitation Medicine Appendix V. the European Board Appendix VI. ing Professional
Examples of disabling conditions commonly encounte 323 lists PRM Specialists in Europe by UEMS Member States 324 Diagnostic tools and assessments in Physical and Re 325 Curriculum of studies and theoretical knowledge for 326 Diploma in PRM (Version 2005) Rules for Continuing Medical Education and Continu 330 Development of PRM Specialists
Delegates and members in the three organisations 331 Vol. 42 - No. 4 291 EUROPA MEDICOPHYSICA
----------------------- Page 6----------------------EDICINE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION M EXECUTIVE SUMMARY 1. Introduction ncurred by health services, had such services not been proPreventing the complications of immobility, brain injury 1. 1.1. This book has been written for: in (for which there is good evidence) leads to many 1. Policy makers in health care concerned with rehabilitation both qualitatively for the individual and quantitatively and disability. ms of the financial implications. 1. The general public and, in particular, people with disabilThe Bio-Psycho-Social Model of Disability. PRM is guidity and representatives of their organisations. a bio-psycho-social approach to rehabilitation. This was 1. Health care professionals in other medical specialties and d in cooperation with user organisations and adopts the professions allied to medicine. ternational Classification of Functioning Disability and (ICF), which was approved by the World Health Assembly 1. 1.2. It sets out the nature, area of work and parameters of ently as May 2001. The framework is aetiologically neutral Physical and Rehabilitation Medicine (PRM), the competencies of opts a terminology that is accepted worldwide to delinthe speciality and of its specialists, the clinical content of the unctioning both at individual and population levels. This work of the specialty and the nature of the education and trainork is useful for managing the individual nature of any ing of specialists in this field. The Greater European Space has been i vided. and pa benefits in ter 1. 3.2. ed by develope WHOs In Health as rec and ad eate f framew
litation programme and intervention. It identifies the been enlarged recently and this book seeks to promote the harying pathology, the problems at the level of organ funcmonisation of specialised PRM activity to help ensure that the pubg and the potential for restoring/optimising personal funclic and especially those experiencing disability are well served irrer preventing further limitation of activity. In addition, it conspective of their location. the ability to participate in society, which depends not only sonal functioning, but also on contextual factors affecting dividuals life and environment. 2. Definitions . Ethical aspects and human rights. Access to Rehabilitation asic human right, which is supported by the United Nations 1. 2.1. The World Health Organisations (WHO) definition of through its standards (1993) by the European Year for rehabilitation is: The use of all means aimed at reducing the ith Disabilities, 2003 and the 58th Resolution of the impact of disabling and handicapping conditions and at enabling Health Assembly (2005). In addition, many European people with disabilities to achieve optimal social integration ave anti-discrimination laws, which can be used to sup1. 2.2. The definition of PRM by the Union Europenne des ple with disabilities ad their families and assistants. Mdecins Spcialistes (UEMS) Section of PRM is an indepensts are routinely involved in discussions on ethical dent medical specialty concerned with the promotion of physgal dilemmas during the care of their patients. ical and cognitive functioning, activities (including behaviour), ity of access to rehabilitation and social participation withparticipation (including quality of life) and modifying persony kind of discrimination are fundamental to the provision al and environmental factors. It is thus responsible for the preactice of rehabilitation. PRM specialists are aware of the vention, diagnosis, treatments and rehabilitation management res put on individuals by differences in race, culture, reliof people with disabling medical conditions and co-morbidity nd sexual orientation. Rehabilitation has the aim of supacross all ages. peoples independent living and their autonomy and a holistic approach to facilitate this. is important to all sections of society across Europe. It 3. Relevance of rehabilitation for people ts the confirmation by both the International Year for with disabling conditions and to society ed People (1981) and the European Year for People with lities (2003) that access to rehabilitation after injury or 1. 3.1. The prevalence of disability is accepted in most European
rehabi underl tionin tion o siders on per the in 1. 3.3 is a b Charter People w World states h port peo PRM speciali and le Equ out an and pr pressu gion a porting takes PRM suppor Disabl Disabi illnes
s is a fundamental human right. countries as around 10%. Populations are ageing and this brings . People with disabilities should be active participants in increasing levels of disability. This is reflected in an increased eation and development of rehabilitation services. Good burden of care for individuals and, for society, with increased ce in rehabilitation makes sure that the person with discosts for health and social care. Survival from serious disease and ies is at the centre of a multi-professional approach and able trauma is improving but may leave an increasing number of e informed choices of treatment. If appropriate, the fampeople with often complex functional problems. Additionally, involved in the rehabilitation process too. the people of Europe have increasing expectations of main. Aims and outcomes of rehabilitation. The overall aim of rehataining good health tion is to enable people with disabilities to lead the life that Rehabilitation is effective in reducing the burden of disabilould wish, given any restriction imposed on their activities ity and in enhancing opportunities for people with disabilities. airments resulting from illness or injury as well as from Its cost is frequently no greater than would have otherwise personal context. In practice, this is often best achieved by a 292
1. 3.4 the cr practi abilit to mak ily is 1. 3.5 bilita they w by imp their
EUROPA MEDICOPHYSICA December 2006
----------------------- Page 7----------------------ICINE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MED
combination of measures to overcome or to work around their 5. The Specialty of Physical impairments and to remove or reduce the barriers to participation and Rehabilitation Medicine in the persons chosen environments. Such a process will optimise both activity and participation. The two fundamental outle of the specialist in PRM, the conditions treated, the comes of rehabilitation that have to be demonstrated are the perc tools, assessments and the interventions frequently sons well-being and their social and vocational participation. scussed in detail in Chapter 5 and Appendix IV. 4. Principles of Physical 6. Standards in Physical and Rehabilitation Medicine and Rehabilitation Medicine 1. 4.1. Learning is a modern and the most important part of RM is an independent medical specialty in all European the rehabilitation process. The PRM specialist is a teacher, espeexcept Denmark and Malta The duration of training cially when new concepts of plasticity and motor learning have y at least 4 years. There are variations in the training and to support rehabilitation programmes. PRM specialists have to f work across Europe but the European Board of PRM know the principles of adaptation and plasticity and to underoped a comprehensive system of post-graduate edustand the theoretical background of the principles of teaching
The ro diagnosti used are di
1. 6.1. P countries is usuall content o has devel cation, w
hich includes a curriculum, logbook and examinaaddition trainers are accredited and rehabilitation faciland learning.
tions. In
ities are accredited. There is continuing medical education with 1. 4.2. Physical and Rehabilitation Medicine aims at reducing the the purpo se of ten-yearly revalidation. Details can be found impairment caused by disease where possible in preventing comon the Bo ards website www.euro-prm.org. PRM specialists are plications, in improving functioning and activity and enabling active in providing undergraduate education, for the principles participation. All these activities have to take into account the indi- of rehab ilitation should be taught to all medical undergraduates viduals personal, cultural and environmental context. Practice is to ensure t he better care of all people with disabilities. in various facilities from acute care units to community settings. 1. 6.2. S pecialists in PRM have a holistic approach to people PRM specialists use specific diagnostic assessment tools and carwith acut e and chronic conditions. Their work is most frery out many types of treatments, including pharmacological, quently i n the management of the rehabilitation of conditions, physical, technical, educational and vocational interventions. such as m usculo-skeletal and neurological disorders, trauma, Rehabilitation is a continuous and coordinated process, which amputatio ns, pelvic organ dysfunction, cardio-respiratory insufstarts with the onset of an illness or injury and goes on right ficiency and the disability due to chronic pain and cancer. through to the individual achieving a role in society consistent with 1. 6.3. T he competencies of PRM specialists include, amongst his or her lifelong aspirations and wishes. others: 1. 4.3. Teams of health care professionals working closely Medica l assessment in determining the underlying diagtogether in multi-professional teams deliver rehabilitation in an nosis. organised goal-oriented, patient centred manner. PRM special Assess ment of functional capacity and the ability to change. ists are usually the leaders of these teams and are responsible Assess ment of activity and participation as well as confor their patients care in specialised PRM facilities. They also textual fac tors. work closely with other medical disciplines and, where reha Devisi ng a rehabilitation plan. bilitation becomes the main focus of clinical activity, will lead Knowle dge, experience and application of medical and this multi-disciplinary cooperation. physical treatments. Evalua tion and measurement of outcome. 1. 4.4. Physical and Rehabilitation Medicine in different phases of Preven tion and management of complications. the rehabilitation process. Rehabilitation can be provided in a Progno stication of disease/condition and rehabilitation number of settings, which range from specialised rehabilitation outcomes. centres and departments in acute hospitals to outpatient and dge of rehabilitations technology. community settings. Acute rehabilitation is important in order to ynamics and leadership skills. Knowle Team d
utilise plasticity as effectively and as early as possible and to ng skills. reduce the potential for complications. This requires not only a dge of social system and legislation on disablement. peripatetic team of rehabilitation professionals able to give advice ecialists promote undergraduate medical education in to all wards in a hospital, including intensive care, but also dediples of rehabilitation. This should be taught to all icated rehabilitation beds, with both under the responsibility of tudents to better care for all those with disabilities. a PRM specialist. Patients also require rehabilitation in dedicated re also available to help in the planning of services and rehabilitation facilities directed by PRM specialists and those with lgation of policies, which relate to their patients. All longstanding, often progressive disabilities and disorders, will ters relate to the needs of the population and to clinneed it in the community to ensure that their fitness, health and rnance of the services provided. There should be regabilities are maintained and their independence is promoted. t of these services and regular feed back from users. Vol. 42 - No. 4 ----------------------- Page 8----------------------CINE IN EUROPE
Teachi Knowle PRM sp the princ medical s They a the promu these mat ical gove ular audi
EUROPA MEDICOPHYSICA 293
WHITE BOOK ON PHYSICAL AND REHABILITATION MEDI realise tha ties are en establishin Europe, who to ensure e practice an nologies. Its and especia role of thi fits of reh people with 1. 8.2. One to work wit tries of Eu vices of th damental hu
7. Research in Physical t. This can only be achieved if comprehensive faciliand Rehabilitation Medicine sured and that PRM specialists play a central role in g these to gain equity of access for all people in PRM has fully endorsed the principles of evidence-based require them. The specialty of PRM is well equipped medicine and promotes an active research programme aiming xcellent clinical standards through evidence-based to understand the basic processes of rehabilitation and identid through the utilisation of newer research techfy the determinants both of recovery and of peoples capacity benefit has been demonstrated by scientific research to acquire new skills and learn. To continue to provide this lly the rapidly increasing knowledge of medicine. The evidence requires that such research be better funded. s book is to promote greater awareness of the beneabilitation and of PRMs contribution to the lives of disabilities of the most important aims of the specialty must be 8. Future Developments for Physical and Rehabilitation h others to the position where people in all counMedicine rope have access to a full range of rehabilitation sere highest calibre. This the specialty regards as a fun1. 8.1. The future goals for the specialty cover the development
man right. It is hoped that this of a culture of rehabilitation e information to engage with the with disabilities and one of the s end. 294
book will provide as a fundamental right for people specialty to roles of PRM specialists is to
readers with th achieve thi
December 2006
EUROPA MEDICOPHYSICA
----------------------- Page 9----------------------WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICINE IN EUROPE 1. Introduction ion and enhancement of specialist need for greater competency increas1.1. This book sets out the nature, area of work nt for PRM to redefine what it is, what and parameters of Physical and Rehabilitation it can best provide its services and Medicine (PRM) in Europe. Definitions of the speat standards of training should be cialty and the competencies expected of fully trained rants into the specialty. This book specialists in the field are given. It describes the clino these requirements. ical context of the work and the nature of education and specialist training. The book builds on the original White Book, which appeared in 1989.1 This was 2. Definitions important in the development of the specialty throughout Europe and was translated into many languages on for local use. Twenty years on, the enlargement of the European Union makes it an opportune time to has been defined by the WHO as update information about the specialty across Europe, ns aimed at reducing the impact of as the specialty assumes greater importance and dicapping conditions and at enabling advances in medicine and technology occur. ilities to achieve optimal social inte1.2. The book is primarily aimed at three groups: incorporates clinical rehabilitation but policy makers in healthcare, rehabilitation and endorses the concept of social pardisability issues; uiring a matching of the social envi the general public and, in particular, people with s of people with disabilities, so as disabilities and representatives of their organisations; l barriers to participation, be they health care professionals in other medical spel. cialties and professions allied to medicine. context, rehabilitation specifically opment, revalidat training. As the es, it is importa it can offer, how expertise, and wh demanded from ent aims to respond t
2.1. Rehabilitati Rehabilitation The use of all mea disabling and han people with disab gration.2 This definition also, importantly, ticipation as req ronment to the need to remove societa social or vocationa Within a health
as a process of active change by 1.3. The medical community in Europe has recento has become disabled acquires the ly been strengthened by the enlargement of the lls needed for optimal physical, European Union, offering further opportunities and social function.3 This definition challenges. This publication seeks to assist the process xplicit indication of the process that of harmonisation of specialist PRM activity to help people with disabilities in developensure that people with disabilities are well served by acities, which is the area most effecthe specialty irrespective of where they live in our y medical rehabilitation. enlarged community. Rehabilitation Medicine 1.4. Health care is undergoing great changes both at European and at national levels. There are increasehabilitation Medicine in Europe is a ing expectations of medical care from the general ecialty and has been defined by the public, which mirror the philosophical debate about RM as follows: human rights and responsibilities across society parendent medical specialty conticularly in relation to the full participation of people romotion of physical and cognitive with disabilities. Medical practice is continually evolvvities (including behaviour), particiing, with the raising of clinical standards and the need quality of life) and modifying perfor excellence through continuing professional develmental factors. It is thus responsible Vol. 42 - No. 4 295
has been defined which a person wh knowledge and ski psychological and provides a more e is undertaken by ing their own cap tively promoted b 2.2. Physical and Physical and R single medical sp UEMS Section of P PRM is an indep cerned with the p functioning, acti pation (including sonal and environ
EUROPA MEDICOPHYSICA
----------------------- Page 10----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN stroke, traumatic hood cancer, where rehabilitation hav outcomes;9-18 there is also a Europe. This place care, including PR Dealing with th
for the prevention, diagnosis, treatment and rehabilbrain injury, polytrauma and childitation management of people with disabling medbetter-organised acute care and ical conditions and co-morbidity across all ages. e led to greater survival and better Specialists in PRM have a holistic approach to people with acute and chronic conditions, examples n expectation of good health in of which are musculoskeletal and neurological diss further demands on all health orders, amputations, pelvic organ dysfunction, carM specialists. dio-respiratory insufficiency and the disability due to e consequence of disease and trau-
chronic pain and cancer. city following an insult to the brain PRM specialists work in various facilities from s that not only do patients lives acute care units to community settings. They use speis also a benefit to the health econcific diagnostic assessment tools and carry out treate expenditure of treating these ments including pharmacological, physical, technis will have a direct effect on care cal, educational and vocational interventions. Because lives and pensions.15-17 In particof their comprehensive training, they are best placed ch as immobility, pain, nutrition, to be responsible for the activities of multi-profesunication disorders, mood and sional teams in order to achieve optimal outcomes.4 bance become important in addition A comprehensive modular description of Physical and the complications of the preand Rehabilitation Medicine within the framework of g conditions. the ICF is in the discussion phase at an international is effective in reducing the burden of level and is described in Appendix Ia. enhancing opportunities for people An explanation of the two parts of the name of the There is evidence that it may be less specialty for Physical and Rehabilitation Medicine can viding no such service.14 Certainly, be found in Appendix Ib. ations of immobility (e.g. pressure ures), of brain injury (e.g. behavnd of pain (e.g. mood changes) 3. Relevance of rehabilitation for people enefits, for which there is good eviwith disabling conditions and to society 3.1. Epidemiological aspects Y OF FUNCTIONING AND DISABILITY 3.1.1. DEMOGRAPHIC CHANGE IN EUROPE studies have traditionally based About 10% of Western Europes population expeaetiological diagnoses. They rience a disability, as described in a British survey.5, 6 o address chronic disease as an Life expectancy is increasing among Europes 700 yet properly tackled the concepts million inhabitants, of whom 450 million live in rticipation and quality of life among European Union countries. For instance, life expectanlities as a population. cy in Germany rose by almost 3 years between 1990 ch is to deal with these problems and 2000, but by 2030, one person in four will be lthy Life Expectancy (HALE) and aged 65 or over.7, 8
ma, such as spasti or spinal cord, mean improve, but there omy by reducing th complications. Thi provision, working ular, problems, su incontinence, comm behavioural distur to systemic illness disposing disablin Rehabilitation disability and in with disabilities. expensive than pro preventing complic sores and contract ioural problems) a can lead to many b dence.19 3.1.2. EPIDEMIOLOG Epidemiological their methodology on have now started t entity, but have not of functioning, pa people with disabi A modern approa by focusing on Hea Disability-Adjuste
d Life-Years (DALYs). These are sumAs populations age, there is an increased level of opulation health that combine disability, which is reflected by an increased burden tality and non-fatal health outof care, increased costs for health and social care and population health in a single numthe impact of co-morbidities. Two important factors have to be considered: the incidence and prevalence of the survival from serious disease and trauma leaves ogies in the field (strokes, spinal an increasing number of people with complex probmatic brain injuries, amputations, lems and functional deficits. Many of these people , other neurological or musculoare young at the time of their event/injury and will surs, chronic pain, etc.), epidemiology vive for many decades. Examples are numerous, e.g. ider the: 296 December 2006
mary measures of p information on mor comes to represent ber. In addition to most frequent pathol cord lesions, trau rheumatic diseases skeletal condition in PRM should cons
EUROPA MEDICOPHYSICA
----------------------- Page 11----------------------CINE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDI
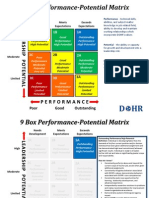
resultant loss of functioning in terms of the ICF parameters; Health condition
(disorder or disease) natural history of functions, activity and participation; need for and access to resources for use in rehabilitation (human resources, facilities, equipment, tions materials); ctures Activities Participation access to the available PRM resources. Such information aids the planning and prioritisation of regional, national and European services, in the funding of research and in the development of trainEnviromental Personal ing by giving information on the effectiveness and factors factors cost-effectiveness of PRM interventions. There are many reports giving the incidence and current framework of functioning and disability - the prevalence of the major disabling conditions seen in tional Classification of Functioning, Disability and Health PRM practice. Some examples are given in Appendix II. PRM is particularly concerned with their impact and a recent survey in Portugal reported that 0.7% of the entire
Body func and stru
Figure 1.The WHO Interna (ICF).20
evaluate th
e patient-relevant outcomes of an interpopulation is restricted to bed; 0.4% are restricted to sitting (require wheelchairs); 1.9% do not live in their PRM perspective, patients functioning own homes; 9% do not walk or have a significant limis seen as associated with and not merely itation in walking; 8.5% are limited in transferring to and from bed; 6.2% cannot use the toilet without help; ce of a health condition or disease. In 8.6% need help dressing or undressing; 3.6% of men and unctioning represents not only an outcome, starting point of the clinical assessment 5.3% of women have urinary incontinence; around 2.3% ervention. It is also important for quality have speech difficulties. The overall prevalence of all disabilities in the community is 10%.2 Moreover, functioning has to be seen as se interaction with the persons characIn summary, the epidemiological data support the d environment.22 Thus, the rehabilitative need for rehabilitation in Europe. Therefore the medets functioning, the environment, and ical specialty of PRM has a significant contribution to ersonal factors.11 Rehabilitation, theremake in the reduction of the burden of disease and to the empowerment of people with disabilities. with an in-depth understanding of the s of functioning and of its interactions l and environmental factors regardless of 3.2. The World Health Organization Model of Funcondition. The components of the biopsytioning, Disability and Health in Rehabilitation odel of functioning and disability 23, 24 as The WHO published its International Classification understanding of the interactions between of Functioning, Disability and Health in 2001.20 This seen in Figure 1. has been fundamental to the better analysis of the basis for this understanding is the bio-psyconsequences of disease and to the practice of Physical model of functioning, disability and health and Rehabilitation Medicine. d Health Organisation (WHO).20 Based on The assessment of the impact of a disease on an functioning with its components, Body individual differs when viewed from the medical or and Structures and Activities and from the rehabilitation perspective. From the medon, is seen in relation to the health condiical or disease perspective, patients functioning, dissideration, as well as personal and ability and health are seen primarily as the conse-
vention.21 From the and health a consequen addition, f but also the and the int management. having a clo teristics an process targ modifiable p fore, begins determinant with persona the health c chosocial m well as the them can be A useful cho-social of the Worl this model, Functions Participati tion under con environment
al factors (Figure 1).25, 26 Functioning is quences or the impact of a disease or health condition. e than disability in describing the interMedical interventions are targeted towards the diseen an individual with a health condition ease process and the ultimate goal of these interventextual factors (environment and persontions is to avoid the consequences on the individual. of that individual. Disability is often used as Both functioning and health must be measured to term for impairments, limitations in activVol. 42 - No. 4 297
more positiv action betw and the con al factors) an umbrella EUROPA MEDICOPHYSICA
----------------------- Page 12----------------------N MEDICINE IN EUROPE umatoid arthritis skeletal condition : Body functions: Participation: - vocational performance - family relations - recreation and leisure WHITE BOOK ON PHYSICAL AND REHABILITATIO Osteoarthritis, rhe or functional muscoloActivities
- pain king, use - range of motion - muscle weakness
- mobility: standing, wal of trasportation - grasping, handling of o
bjects
- coordination deficits - activities of daily liv ing, such as - social life - problems with energy and drive washing, dressing, shopp ing, - participation in political and religious functions and sleep disturbances preparation of meals activities Environmental factors: Personal factors: - work place - health behaviour - housing and transportation facilities
- coping strategies (sense of coherence) - family and friends - multi-morbidity - age and gender - health service and insurance - societal attitudes
Figure 2.Example for Applying the ICF-Model in Musculoskeletal Conditions.
ities and restrictions in participation. Recognising this or/and functions (e.g. reduced range of motion, muscan help when reading the literature. From the biocle weakness, pain and fatigue). psycho-social perspective presented here, functioning Activity is the execution of a task or action by an is implicitly addressed when disability is studied and individual and represents the individual perspective of vice versa. (An example for patients with muscufunctioning. loskeletal conditions is given in Figure 2). Participation refers to the involvement of an indi A health condition is an umbrella term for disdual in a life situation and represents the societal perease, disorder, injury or trauma and may also include spective of functioning. Difficulties at the activity levother circumstances, such as ageing, stress, congeniel are referred to as activity limitation (e.g. limitations tal anomaly, or genetic predisposition. It may also in mobility such as walking, climbing steps, grasping include information about pathogenesis and/ or aetior carrying). Problems an individual may experience ology. There are possible interactions with all comin his/her involvement in life situations are denoted ponents of functioning, body functions and strucas participation restriction (e.g. restrictions in comtures, activity and participation. munity life, recreation and leisure, but may be in Body functions are defined as the physiological lking too, if walking is an aspect of participation in functions of body systems, including mental, cognitive terms of life situation). and psychological functions. Body structures are the Environmental factors represent the complete anatomical parts of the body, such as organs, limbs background of an individuals life and living situaand their components. Abnormalities of function, as tion. Within the contextual factors, the environmental well as abnormalities of structure, are referred to as factors make up the physical, social and attitudinal impairments, which are defined as a significant devienvironment, in which people live and conduct their ation or loss (e.g. deformity) of structures (e.g. joints) lives. These factors are external to individuals and 298 SICA ----------------------- Page 13----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC Standards in developed int EUROPA MEDICOPHY December 2006
vi
wa
can have a positive or negative influence, i.e., they can December 1993 and is currently being represent a facilitator or a barrier for the individual. o a convention to provide persons with Personal factors are the particular background of ll participation and equality. This has been
disabilities fu
an individuals life and living situation and comprise ying down fundamental principles. features that are not part of a health condition, i.e. genof Europe has also published a series der, age, race, fitness, lifestyle, habits, and social backd documents on human rights for people ground. Risk factors could thus be described in both ies. In particular, it facilitated a declarapersonal factors (e.g. lifestyle, genetic make-up) and ropean Ministers responsible for the environmental factors (e.g. architectural barriers, livlicies for People with Disabilities, which ing and work conditions). Risk factors are not only in 2003.35 Its aims are to: associated with the onset, but interact with the disquality of life of people with disabling process at each stage. their families over the next decade; Physical and Rehabilitation Medicine is concerned res aimed at improving quality of life with the multi-professional promotion of a persons disabilities, which should be based functioning.27, 28 It depends upon a full assessment sessment of their situation, potential and understanding of a persons functioning. ICF Core Sets for different health conditions have been internationally agreed.29-31 They include as few action plan in order to achieve these ICF domains as possible to be practical, but as many as necessary to be sufficiently comprehensive to y of access to employment as a key describe the typical spectrum of problems in funcocial participation; tioning among patients with a particular condition. ative approaches, as persons with They are used in comprehensive, multidisciplinary hological and intellectual impairments assessments or in clinical studies. Thus, an ICF sheet can be used in combination with the ICF Core Sets to vities to enable a good state of physimprove internal reporting and documentation and al health in the later stages of life; to structure multidisciplinary care.32, 33 supportive structures around people ies in need of extensive support; 3.3. Ethical aspects and human rights provision of quality of services; 3.3.1. DISABILITY AND HUMAN RIGHTS grammes and resources to meet the ns with disabilities. Historically, it was thought sufficient to provide World Health Assembly adopted a care for people with disabilities. However, in the past n Disability, including Prevention, 20 years there has been a philosophical shift in Europe, nd Rehabilitation (World Health so that people with disabilities are regarded as citizens
important in la The Council of reports an with disabilit tion of Eu
Integration Po met in Malaga improve the abilities and adopt measu of people with on a sound as and needs; develop an goals; allow equit element for s adopt innov physical, psyc live longer; create acti ical and ment strengthen with disabilit promote the develop pro needs of perso In 2005 the Resolution Management o a
Assembly Resol
ution 58.23). It declared that, amongst with full autonomy and human rights. This is in the member states should: spirit of the UN Standard for Human Rights and has led in disability prevention activities; to legislation to prevent discrimination on the grounds strengthen community based rehaof disability. The UN declaration of Human Rights 34 states that a grammes linked to primary health care d in the health systems; person with disabilities should not be an object of care (a patient) throughout life. He or she is a citizen with ss to appropriate assistive techspecial needs related to a specific disability. These needs promote its development and other should be catered in the society but in a normal conge the inclusion of persons with text. Participation is fundamental and a central aspect of in society; this is access to society. This includes physical access e.g. and put into practice the most effecinto public and private areas and buildings, as well as o prevent disabilities; to public transport, information etc. Regulations on ision of adequate and effective medaccessibility have been established in several European people with special needs and to facilicountries for the construction of public buildings. The ess to such care including prostheses, UN General Assembly approved the development of UN riving aids and other devices; Vol. 42 - No. 4 299
other things, participate promote and bilitation pro and integrate facilitate acce nology and to means that encoura disabilities investigate tive actions t ensure prov ical care for tate their acc wheelchairs, d
EUROPA MEDICOPHYSICA
----------------------- Page 14----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN to encourage equity ticipate in rehabi 3.3.3. RIGHT TO RE Access to rehab European legislati disabilities shoul bilitation. Thus an
research and implement the most effective meaof access, e.g. to help mothers parsures to prevent disabilities in collaboration with comlitation programmes. munities and other sectors. Additionally it requested the Director-General to: HABILITATION intensify collaboration within the Organization ilitation is a basic human right. towards enhancing quality of life and promoting rights on makes it clear that people with and dignity of persons with disabilities; d have access to appropriate reha provide support to Member States in strength-
appropriate level of skills and trainening national rehabilitation programmes; ongst all rehabilitation profession support member states in collecting more reliable pecialist in PRM. PRM plays an data on all relevant aspects, including cost-effectivethis provision in advising on serness of interventions for disability prevention, rehand in participating with governbilitation and care; non-governmental organisations. further strengthen collaborative work within the nsibility to support organisaUnited Nations and with Member States, non-goveople with disabilities in order to ernmental organizations (NGOs), including organiy of access to rehabilitation and zations of people with disabilities; on. This is important because the promote studies of incidence and prevalence of human rights and the prevention disabilities as a basis for the formulation of strategies require further activity and develfor prevention, treatment and rehabilitation. dressed by the Union Europenne Disability Rights legislation has also been created in tes (UEMS) Section of PRM several European countries.36, 37 Some have had longstanding legislation with a general policy on the rehaEurope proposed disability rights legbilitation of people with disabilities (e.g. France has sentially covers the following:37 Disabled Persons Act since 1975), but the majority of ention and health education; countries have passed anti-discrimination legislation and diagnosis; only during last 15 years, e.g. Act of Equal Opporherapeutic aids; tunities for Disabled Persons (Germany), Framework Law (Italy), Constitution Act (Finland), Act on Provision of Rights of Persons with Disabilities (Hungary 1998), ance and training; Health for All 2004 (Slovenia), Disability Discrimination Act 1996 (UK), Toward Inclusion 2001 (UK) etc. All of ion and environment; these are enshrined in PRM practice and are supc and legal protection; ported by PRM specialists. ople involved in rehabilitation and ion of people with disabilities; 3.3.2. GENDER, RACE, CULTURE, RELIGION AND SEXUAL ORIENTATION ISSUES research. Equity of access to rehabilitation and social particN Standard 38 states that governipation without regard to discrimination of any kind op their own rehabilitation pro-
ing is required am als, including the s important role in vice development a mental bodies and PRM also has a respo tions of and for p achieve this equit societal integrati achievement of full of discrimination opment. This is ad des Mdecins Spcialis (see chapter 6.4). The Council of islation, which es disability prev identification treatment and t education; vocational guid employment; social integrat social, economi training for pe in social integrat information; statistics and Rule 3 of the U ments should devel
are fundamental to the provision and practice of rehaoups of persons with disabilities. bilitation. PRM specialists are aware of the pressures ould be based on the needs of put on individuals by differences in gender, race, cullities and on the principles of full ture, religion and sexual orientation. These pressures equality. All those needing rehabilmay impinge upon adaptive capacity by affecting e access to it. This holds also for body image, psychological state and well-being. xtensive or multiple disabilities. Rehabilitation has a holistic approach to support peoutilise the expertise of the orgaples independent living and, for many, religion and ople with disabilities when such spirituality are important in the rehabilitation process. grammes are developed or evaluatProgrammes already exist in rehabilitation facilities this standard is only partly adhered 300 December 2006
grammes for all gr Such programmes sh people with disabi participation and itation should hav those with e
Governments should nizations for the pe rehabilitation pro ed. Unfortunately,
EUROPA MEDICOPHYSICA
----------------------- Page 15----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC ing into accou treat patie provide acc facilitate dec obtain info informed refus determine t petent decisio protect pat prohibit ph be sensitiv and to differe remove arch tion, employme
to in most European countries, which represents a nt ethics and human rights, in order to: challenge both for PRM physicians and for society in nts with dignity and respect at all times; general. PRM practice is not based on a monolithic essible information to patients to medical model but takes into account social aspects ision making; and has a holistic view. It is founded on a bio-psychormed consent and how to allow social model within a continuum of care, taking into al; account both personal and environmental factors. It he ability of the patient to make comprovides personal empowerment for the users, conns; tributing to full participation in all aspects of life. ient privacy and confidentiality; Despite its confirmation of human rights by both the International Year for Disabled People (1981) and the ysical or psychological abuse; European Year for People with Disabilities (2003), e to cultural, religious and other beliefs access to rehabilitation after injury or illness remains nt treatment practices; a problem. This is in part due to a lack of resources, itectural, attitudinal, communicaof information to people with disabilities and to poor nt and other barriers to such per-
organisation of services resulting in a mismatch of provision to needs. The participation of many people with disabilities is hampered by traditional attitudes in ation and Health Systems Society, but improving the health and education of people with disabilities to enhance their participation nd funding of rehabilitation services needs further attention and PRM has a considerable e to state and depends on the health care role here. tems. Stakeholders in these systems cians, planners and organisations, which d social care, self-help groups and oth3.3.4. ETHICAL ISSUES OF HEALTH-RELATED REHABILITATION munity. People with disabilities should be active particiermined funding accounts for differences pants in the creation and development of rehabilitacute and to maintenance rehabilitation tion services. An example of their inclusion into rehaountries, insurance companies medical bilitation team working was seen in the EU HELIOS e about access to rehabilitation, espeprogram (1990-96) whose aim was to improve the field of maintenance rehabilitation. In possibilities for Handicapped People in Europe Living ute rehabilitation the general practiIndependently in an Open Society. One of its workmedical specialists send their patient ing parties gave the following recommendations for ion centres. In yet other countries, the good practice in rehabilitation: directly to inpatient rehabilitation hos the person with disabilities should be at the cencare practitioners may authorise spetre of a multi-professional approach and should be ient services in some states, but, in othable to make informed choices of treatment. He or she rral by the patient is acceptable. Europes should participate fully in the process and have the al systems prevent a detailed description right to receive services regardless of type of disabilch member state can provide the necity, age, gender, religion, ethnic origin, domicile and tion. re of rehabilitation services varies across financial resources; vision is patchy. Specialists in PRM family involvement should be included where r in many countries. Although the appropriate; ell regarded across Europe, there are continuous and coordinated measures should s in the number of specialists by counenable a return to usual environment and chosen role in the health system and in their con-
sons. 3.4. Rehabilit Access to a vary from stat and social sys include politi fund health an ers in the com Locally det in access to a and, in some c services decid cially in the others and in ac tioner and other to rehabilitat patient can go pitals. Primary cialist outpat ers, self-refe diverse nation of each and ea essary informa The structu Europe and pro are few in numbe specialty is w large difference try, in their
social and professional life; k. Appendix III shows the variation in rehabilitation strategies should be subject to useralists by country and, while an optibased evaluation. PRM specialists per unit of populaAll rehabilitation departments, programmes and o be set across Europe, there clearly practices should formulate clear operational plans takarity between states. Vol. 42 - No. 4 301
ditions of wor numbers of speci mal number of tion has yet t remains a disp
EUROPA MEDICOPHYSICA
----------------------- Page 16----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC sures implicitl of specific ob climb stairs, important by al Rehabilitati consequent on society. It is vidual function ing greater act complications benefits the in personal auto
3.5. Aims and outcomes of rehabilitation y make judgements about the relevance jective factors, such as the ability to A persons rehabilitation potential ( i.e. capacity to benefit from rehabilitation) cannot be formulated which may not be perceived as equally l people with disabilities. without knowing the natural history of his or her conon has the ability to reduce the burden dition. Some recover spontaneously, so that early disability both for individuals and for intervention may give the false impression that treatment has been efficacious.39-41 On the other hand, for shown to be effective in enhancing indimany, a lack of rehabilitation will reduce their evening and independent living by achievtual level of independence and quality of life.41 ivity, better health and by reducing Controlled studies, in which these factors have been and the effects of co-morbidities. This taken into account, have shown that early intervention dividual and society to include greater tends to be associated with an improved eventual nomy, improved opportunities for outcome whether or not full recovery occurs and other occupational activity. While even delayed or late intervention may confer useful actors are involved in return to indebenefit.42, 43 and work, PRM can prepare the indilies/carers to take maximal advantage The overall aim of rehabilitation is to enable peonities that are available. ple with disabilities to lead the life that they would
employment and many societal f pendent living vidual and fami of the opportu Rehabilitati
on has been shown to be effective not wish, given any inevitable restrictions imposed on ing individual functioning and indetheir activities by impairments resulting from illness or but in reducing the costs of depeninjury. In practice, this is often best achieved by a s been shown that the money spent on combination of measures to: is recovered with estimates of savings of overcome or to work around their impairments; old.45-47 remove or reduce the barriers to participation al level it is essential to measure outin the persons chosen environments; e the effectiveness of particular reha support their reintegration into society. entions and services. These outcome As a patient-centred process, it is appropriate to o relate directly to the specific objecoptimise both activity and participation. in the rehabilitation plan. The evaluA rehabilitation plan, therefore, has to account for ilitation has fundamental differences the wishes and resources of the individual, the progtion of disease-orientated medical nosis of their disabling medical condition, the nature d at limiting pathology or curing disof their physical and cognitive impairments and their tation can be successfully achieved in capacity to acquire the new knowledge and skills, re there is no biological recovery and which would enable them to enhance their levels of tions that are intermittently or steadiactivity and participation. In addition, it is necessary g. In the latter, rehabilitation may need to assess the extent, to which environmental barriers in a continuing programme that to participation (whether resulting from the physical tient to maintain levels of participation environment itself, or from the behaviour of other that would otherwise not have been people) could be lowered. Finally, a judgement has to hould be standard practice to audit serbe made about whether the resources are available to implement the plan. Demonstrating a persons wellbeing and social participation is an important feature of the fundamental outcome of patient-centred rehabilitation.43 4. Principles of Physical d Rehabilitation Medicine Well-being is probably a more secure indicator of success than quality of life since the objectives rocesses as a basic principle of Physical espoused in rehabilitation must reflect the unique ilitation Medicine
only in enhanc pendent living dency.44 It ha rehabilitation up to seventeen f At an individu comes to evaluat bilitation interv measures have t tives addressed ation of rehab from the evalua treatments aime ease. Rehabili conditions whe indeed in condi ly deterioratin to be delivered enables the pa and well-being achieved. It s vices.
an
4.1. Learning p and Rehab
wishes of the individual person although different people facing broadly similar situations may have difa modern part of the rehabilitation ferent objectives. Many current quality of life meaM specialist is a teacher, especially 302 December 2006
Learning is process. The PR
EUROPA MEDICOPHYSICA
----------------------- Page 17----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC process, which injury and goes achieving a ro lifelong aspira 4.3. The rehabi 4.3.1. REHABILI
when new concepts of adaptation (e.g. plasticity) and starts with the onset of an illness or motor learning have to support rehabilitation proon right through to the individual grammes. PRM specialists have to know the principles le in society consistent with his or her of adaptation and plasticity and to understand the tions and wishes. theoretical background of the principles of teaching and learning.47 litation team Knowledge of these principles may help to design strategies to enhance outcomes and avoid mal-adapTATION TEAMWORK tation. Effective modern concepts of motor learning 4 on is a multi-professional activity, which and recovery are developed with the aim of inducing ood communication between staff skill-acquisition relevant to the patient dailys life. al skills of the professionals involved. Such an approach is beneficial in preventing a learned the team must have clear rehabilitation non-use phenomenon and to restore function. the patient, in which the patient and However, too intensive a programme could be delecant others should be full participants. terious.48 Commonly learning involves instructions amwork in this setting is that the outconcerning how to do or how to perform a task. ter than the sum of the indiHowever, even without any explicit instruction a peronal inputs. Where teamwork scores is son has the capacity to understand how to do, simply of expertise and workload. There are using implicit learning. margins between the roles of the team Explicit and implicit learning are thought to tap cessful teams thrive on everyone into different neural pathways. The implicit learning espite professional boundaries. Most process is more robust to neurological injuries, espeteams for physical disability will comcially when memory has been severely impaired. Even ore of professionals as well as others
Rehabilitati depends upon g and the individu For it to work, objectives for his/her signifi The value of te put of the team is grea vidual professi in the sharing fairly blurred members and suc contributing d rehabilitation prise a basic c
though the first approach is currently more often used, articular needs. explicit and implicit learning procedures have potential in all aspects of Physical and Rehabilitation OFESSIONAL REHABILITATION TEAM Medicine.49 medical rehabilitation teams are led by n PRM. They are more than a collection 4.2. Aims of Physical and Rehabilitation Medicine ealth professionals and individuals work The principal aims of Physical and Rehabilitation k as part of a multi-professional team Medicine are to optimise social participation and qualhe roles and values of their colleagues. ity of life. This normally involves helping to empowwith the person with disabilities and er the individual to decide upon and to achieve the ppropriate, realistic and timely treatlevels and pattern of autonomy and independence in an overall coordinated rehabilitation that they wish to have, including participation in vocagoals are adjusted over time and tional, social and recreational activity, consistent with rogress. They are patient-centred and their human rights.49 a discipline-by-discipline basis. The Physical and Rehabilitation Medicine is effective in be asking. What are the goals for the five ways: herapist this week? but should be ask treating the underlying pathology; oals for the patient this week and . help to achieve them? In this way, reducing the impairment and/or disability; is able to enhance patient functioning preventing and treating complications; n by providing a coordinated source improving functioning and activity; advice and treatment for the person enabling participation. and the family, with the team acting All these activities take into account the individuals catalyst. personal, cultural and environmental context, folwithin the rehabilitation team is lowing the principles of the ICF (see chapter 3.2.). uctured team communication and regRehabilitation is a continuous and coordinated rences. The diagnosis, the functional Vol. 42 - No. 4 303
responding to p 4.3.2. MULTI-PR Specialised a specialist i of different h within them wor understanding t The team works family to set a ment goals with programme. The according to p are not set on team should not occupational t ing What are the g how can the O.T rehabilitation and participatio of information, with disabilities as provider and Cooperation ensured by str ular team confe
EUROPA MEDICOPHYSICA
----------------------- Page 18-----------------------
INE IN EUROPE
WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC gramme or to relatively li that the simp patient from the calmer, q ward often ha improvement in tion in agita selves as wel optimal respo acute general professional complex needs attempts to a restlessness blunting of s of the cognit Illustrati with by PRM s ventions can complications Case Histo traumatic bra impairments i inability to oping a lifeimpair the re tion, he quic
impact on functioning and activities as well as the undertake physical exertion may be ability of the patient to participate in the society are mited. Nevertheless, it has been observed discussed systematically, while communicating the le act of transferring a brain-injured possible risks and the prognosis of the disease. Short a busy surgical or neurosurgical ward to and long-term goals of the rehabilitation process are uieter atmosphere of a rehabilitation agreed and the appropriate interventions planned. s a therapeutic effect, consisting of The team members assessments are incorporated into attention and cognition and a reducthe written rehabilitation plan. The rehabilitation plan tion. These are important benefits in themwill be reviewed regularly. l as being essential pre-requisites for an nse to rehabilitation.51 The pressures of 4.3.3. MULTI-DISCIPLINARY REHABILITATION COOPERATION wards may render it difficult for multirehabilitation teams to treat patients with Close cooperation between medical specialties may and, in the absence of such treatment, be required in specialised rehabilitation where several lleviate symptoms such as anxiety and impairments and their consequent functional losses with medication may produce short term have to be addressed. The specialists need to agree a ymptoms whilst delaying the recovery common strategy, which incorporates all their interive functions needed for rehabilitation. ventions at the right times rather than address isolatve examples of the types of problem dealt ed treatments in an ad-hoc way. Regular face-to-face pecialists are given below: Early intercontact between the medical specialists is required prevent the development of secondary to achieve a common approach to the overall treatfollowing disease or trauma. ment strategy. PRM specialists should be involved as soon as posry 1.A 25 year-old man suffered a very severe sible in acute rehabilitation, even participating in the in injury following a road traffic accident. His intensive care unit.50 Similarly, continued input may be ncluded confusion, disorientation, agitation and an swallow. He was therefore at serious risk of develrequired from other medical specialists in acute rehathreatening aspiration pneumonia, which could bilitation wards, who will contribute to the rehabilicovery of his cerebral functioning further. In additation process by their own specialist interventions, kly developed lower limb contractures as a result
(e.g. tracheotomy closure in patients recovering from tion and muscular overactivity (spasticity). ventilatory assistance). In later rehabilitation and in the e, coordinated rehabilitation ensured that he was rehabilitation of people with longstanding disabilia quiet environment and helped to communicate d his situation. Treatment was aimed at lowering ties, cooperation with the primary care physician and hrough a behaviour management approach. He was other medical specialists is also required. percutaneous endoscopic gastrostomy (PEG) feedA decision is needed early on in the patients care as vent aspiration pneumonia and ensure adequate to who leads the process of care. This will change as e treatment of his contractures included the reducthe patient progresses from one phase to another, but, pasticity, physical therapy and serial splinting. After where the emphasis is on rehabilitation rather than f intensive rehabilitation, he was able to return roving behaviour. His swallowing recovered so resuscitation or acute medical/surgical treatment, the eat normally and his PEG was removed. He began PRM specialist should lead the decision-making process. e was later able to return to paid employment 4.4. Physical and Rehabilitation Medicine in different ry 2.A 52 year-old man with Type 2 diabetes a gangrenous foot had a trans-tibial amputation. He phases of the rehabilitation process perative counselling to allow him to cope with the 4.4.1. PHYSICAL AND REHABILITATION MEDICINE IN THE ACUTE s to his body and lifestyle. This included meaare him for dealing with sensory changes, body AND POST-ACUTE PHASE ance alterations and enable him to engage in Rehabilitation in the early stages of recovery after n. a severe illness or injury is greatly helped by an approapy started in the early postoperative phase with herapy and prevention of thrombosis and contracpriate environment, in which the patients fears and n was given to the production of an adequate anxieties can be addressed. In the early weeks, the ndaging and reduction of stump oedema. He ability to give sustained attention to a training prowith a temporary prosthesis and was measured 304 December 2006
of immobilisa Appropriat provided with and understan his anxiety t fitted with a ing tube to pre nutrition. Th tion of his s many months o home with imp that he could to walk and h Case Histo mellitus and was give preo coming change sures to prep image and bal rehabilitatio Physiother respiration t tures. Attentio stump with ba begun walking
EUROPA MEDICOPHYSICA
----------------------- Page 19----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC
for a permanent one. This was done with discussion with the of lack of rehabilitation patient on the level and nature of his physical requirements and goals. Consideration was given to the possible need for ehabilitation potential cannot be conhome, workplace or car adaptations. His journey to work parkolation from what would have been the ing, distance walked at work and other relevant factors such as ut rehabilitation. The question that leisure and family activities were explored. The patient was habilitation attempts to address is Will taught how to manage the stump and the prostheses. Three months after the amputation, he was independent in self-care, enefit from the rehabilitation programme including monitoring of his residual limb. He was able to return would not have occurred, had the recovto work and will be followed up for the rest of his life. to chance? The natural history of the d the consequent disabilities and disCase history 3.A 70 yr old woman with OA of the hip a major role in the eventual outcome underwent total hip replacement .At this time she was unable to walk, to bath or shower, or to put on her shoes. She was not abilitation. Some conditions recover able to drive. Post-operative management by the Dept of PRM and early intervention may give the consisted of intensive physiotherapy as well as later home exerion that therapy has been efficacious.39, 40 cises, so that she became able to walk both inside and outside hand, early intervention may be associthe house. She was allowed to return to driving within weeks; improved outcome even where full occupational therapy successfully addressed her activities of daily living. She was advised about her postoperative pronot occur.53 gramme so she could continue this at home. After her home of people with persisting disabilities and environment was checked and adaptations made, she was able s can be enhanced by rehabilitation, but, to live independently. tly, the consequence of them not havation may be to reduce independent func4.4.2. MAINTENANCE REHABILITATION IN STABLE , CHRONIC uality of life.54 In the acute hospital many DISABLING AND PROGRESSIVELY DETERIORATING CONroblems, such as nutrition, swallowing, DITIONS equipment issues may not be addressed is inevitably on treating the primary The other major strands of the work of PRM spehis is where PRM specialists can assist cialists are the maintenance and improvement of funccomplications and in ensuring an optition and the avoidance of predictable and preventable
4.5. Effects A persons r sidered in is outcome witho specialist re the patient b in a way that ery been left impairment an advantages play following reh spontaneously false impress On the other ated with an recovery does The lives their familie more importan ing rehabilit tioning and q correctable p mobility and as the focus impairment. T in preventing mal level of
functioning.55 In the absence of rehabilcomplications in stable, chronic disabling and prolications and loss of function may occur gressive deteriorating conditions. In some European countries (e.g. Austria, Germany, Italy, Poland), inpamay be delayed. Yet health services tient or day-clinic rehabilitation plays an important ory duty to provide rehabilitation serrole in the management of chronic conditions, e.g. health needs of all patients.56, 57 chronic musculoskeletal or neuromuscular disorders, ing may be found in the absence of rehachronic circulatory, respiratory and metabolic disr a variety of conditions: eases as well as skin diseases and urological or gynaeincluding weakness, cardio-respiracologic conditions. Intermittent bursts of intensive nt, muscle wasting, pressure sores, spasrehabilitation may also be used to combat decline in actures and osteoporosis; function even several years after an acute event.17 The main goals of maintenance rehabilitation meal problems; sures in chronic conditions are improvements in affectproblems; ed body functions and an increase in activities. Such d bowel problems (constipation and measures also encompass participation issues, such as ; return to work or avoidance of early retirement caused by health problems. Methods used include physical ion problems; therapies, training, diet, psychological interventions problems and an inability to benefit and health education. The clinical efficacy and posi; tive socio-economical effects are shown in open folehavioural problems; low-up-studies as well as in controlled trials.52, 53 and systemic illness from a variety of Systematic multi-professional health education prourinary tract and, cardio respiratory probgrammes have shown to be effective too. s mellitus; Vol. 42 - No. 4 305
itation, comp and discharge have a statut vices to meet The follow bilitation fo immobility tory impairme ticity, contr pain; nutritiona swallowing bladder an incontinence) communicat cognitive from learning mood and b ill-health causes, e.g. lems, diabete EUROPA MEDICOPHYSICA
----------------------- Page 20----------------------DICINE IN EUROPE TABLE I.Principles of prevention. g in which Prevention ve measures Settin Characteristics Examples preventi WHITE BOOK ON PHYSICAL AND REHABILITATION ME
dertaken Primary societal arenas Avoid disease or injury Speed reduction to prevent traffic accidents Reduction of risk factors for myocardial and cerebrovascular disease Secondary l and early rehadepartment Avoid effect and complicaPrevention of intracranial hypertentions of disease or injury sion in brain injury itself Prevention of stroke after myocardial infarction Prevention of immobility, tissue viability problems Prevention of contractures Tertiary prevention d maintenance n departments Avoid the effect of disease or Treatment of behavioural problems injury on the persons life, following brain injury i.e. limitation of activities Prevention of avoidable financial difand/or restriction of partificulties and unemployment after cipation disease or injury
are un Political and Primary care
Acute hospita bilitation
Post-acute an rehabilitatio
complications of underlying conditions. disease prevention does not just stop at prePhysical and Rehabilitation Medicine should continthe onset and impact of the condition, but ue to be involved with following patients up as they t the wider aspect of reducing the impact of the move into living in the community, in order to prevent: on all aspects of the persons life. Disease secondary health problems and social isolation; n is thus classified as primary, secondary or carers becoming exhausted by the burden of and the principles are as follows (Table I). care and thus break down of the domestic situation; specialists may be involved in disease or injury ion at all levels. The general principles of general practitioners or social workers being l training including cardiovascular, musculocalled on unnecessarily; l and coordinative performance should be con-
context, venting looks a disease preventio tertiary PRM prevent physica skeleta
emergency admissions back to hospital; This may contribute e.g. in the prevention unnecessary placements in residential or nursing ension, myocardial infarction, low back pain home care;8 ls. inappropriate and untimely prescription of disability equipment; PREVENTION OF SECONDARY COMPLICATIONS inability to update disability equipment in the light of advancing technology, e.g. neuroprostheses. e are generic secondary complications foldisease or trauma. These include pneumonia, The overall result of the lack of rehabilitation may sis, pressure sores, circulatory and muscular be that the person is left with a poorer functional tioning, osteoporosis and poor nutritional stacapacity and quality of life. In community settings, addition there are complications specific to there will be a wastage of resources. conditions, such as dysphagia following stroke, nary dysfunction in spinal cord injury. All these 4.6. Prevention addressed by the PRM-service with good effect. 4.6.1. HEALTH PROMOTION EFFECTS OF TERTIARY PREVENTION Health promotion is an underlying principle of all health care systems and thus prevention of disease and e is now considerable evidence that rehabiliits impact and complications is an essential element of produces real benefits 58-61 and improved functhe work of the medical profession. In a rehabilitation performance and participation outcomes and 306
sidered. of hypert and fal 4.6.2. Ther lowing thrombo decondi tus. In various and uri will be
4.6.3. Ther tation tional
EUROPA MEDICOPHYSICA December 2006
----------------------- Page 21----------------------NE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICI an overall anal er the assessme leagues; there has be in loss of acti sudden event, f
that, even later on, it still produces benefits.62 Those ysis of the situation and to bring togethwho have had rehabilitation are less likely to die and nts provided by non-medical colbe living in institutions after disease or injury. This effect is found in many disease groups and at all ages, en a significant impairment resulting although the young tend to do better. Most studies vity and/or participation following a confirm the value of two different aspects of rehabil-
or example a stroke, spinal cord injury itation. Firstly, most documented improvements are in functional outcome and, secondly, people with disng condition is likely to relapse or abilities going through rehabilitation units have less multiple sclerosis, rheumatoid arthritis; avoidable complications. There are less physical probures are available that can directlems (such as those associated with immobility, conirments or enhance well-being and tractures and pressure sores) and fewer psychological xample in medication for spasticity, problems, such as untreated depression. Although pain; there is clear evidence that an intensive period of rehabilitation after an acute event, such as head injury tment of the underlying condition or spinal cord injury produces clear, short-term funcations itself carries risks of disabling tional gains,43 there is also evidence that short-term quire monitoring; gains are lost unless longer-term support is availrisks of a disabling condition have able.50, 63 Even where the effectiveness of individual y changes in a patients lifestyle, for therapeutic modalities is lacking, the evidence supports transition from adolescence to adultthe effectiveness of multi-professional rehabilitation.64, ansition from education to employ65 Thus, longer-term contact with the person with disprocesses of ageing in later life. abilities is important in order to provide rehabilitain PRM work exclusively in this field so tion until natural recovery is complete and to prevent is not compromised by the demands the later development of avoidable complications. l care. The existence of a separate M is known to benefit patients.18 e competent specialists, who are spe5. The Specialty of Physical and wholly dedicated to the task. Patients and Rehabilitation Medicine bling physical conditions and particth complex needs require the atten5.1. Contribution of the Specialist in Physical and -professional team led by a specialist in Rehabilitation Medicine to the rehabilitation defines the nature of the work, which process cal rehabilitation approach and not y input. PRM provides the setting for organised rehabilitative care. This has been shown to be more effective and
or trauma; the underlyi recur, such as medical meas ly improve impa activity, for e incontinence or medical trea and its complic effects that re the medical been enhanced b example in the hood, in the tr ment and in the Specialists that their work of acute medica specialty of PR Patients deserv cially trained with major disa ularly those wi tion of a multi PRM. Chapter 4 requires a medi solely a therap
no more expensive than that provided on an ad hoc alty of Physical and Rehabilitation basis.19 PRM specialists also recognise the importance n Europe of longer-term follow-up. Improvements in physical sts are doctors trained in their discipline and cognitive functioning, say after brain injury, may e years 66 according to the national take many years to develop and not only do PRM tions of postgraduate medical training. specialists ensure that patients are optimally placed to ecialised in the management of a parbenefit from functional improvement, but they work r medical condition but focus on funcover prolonged periods, if indicated, to enhance perresulting from a variety of diseases sonal functioning and societal participation. cialising in the management of a speThe PRM specialist has a particularly important role medical condition. They provide medin rehabilitation when: eople with disabilities arising from there is a complex combination of impairments, nd trauma as well as other severe e.g. cognitive, behavioural and physical impairments, ns. The main goal of PRM intervenin which medical practitioners are trained to provide provement of physical and mental funcVol. 42 - No. 4 307
5.2. The Speci Medicine i PRM speciali for four or mor training regula They are not sp ticular organ o tional problems rather than spe cific organ or ical help for p chronic disease a health conditio tions is the im
EUROPA MEDICOPHYSICA
----------------------- Page 22----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN Additionally, P the rehabilitation gynaecological and 5.4. Diagnostics, PRM doctors rec diagnosis prior to rehabilitation. In aspects of functio tribute to the ful mining the treatme
tioning to enable patients to be active and improve MR specialists may be involved in their quality of life, so that they can engage in social of patients with psychosomatic, life. However, being doctors, they treat the underlydermatological conditions. ing disease, when required. If persistent symptoms and problems arise, functioning, activity and particiassessment and evaluation pation can still be promoted by specialised rehabilitation methods and techniques. They are thus able ognise the need for a definitive to empower those with medical conditions, which treatment and problem-orientated lead to functional deficits, e.g. neurological condiaddition, they are concerned with ning and participation that contions, other musculoskeletal diseases, amputations as l evaluation of the patient in deterwell as heart and lung diseases etc. nt goals.67 These are reached in
he person with disability, his or her 5.3. Pathologies and conditions in Physical and of the rehabilitation team. Rehabilitation Medicine practice assessment in PRM comprise all PRM-specialists deal with the management of functions and structures, activities patients with a multitude of different pathologies issues relevant for the rehabilitation (Appendix II). They are concerned with the impact of lly relevant contextual factors are these on personal functioning and participation. PRM y taking in PRM should include doctors aim to bring benefits no matter what the in all the ICF dimensions. underlying diagnosis. However, diagnosis serves to ain a diagnosis of structural deficits assist with prognostication of outcome and the potensease and the rehabilitation process tial for improvement. tions and techniques are used in al examination. These include laboThere are a number of general problems across the blood samples, imaging, etc. many health conditions, which PRM doctors face on tion and measurement of functional a daily basis. These may include: unctional potential with respect to prolonged bed rest and immobilisation, deconrocess constitute a major part of ditioning patients and causing loss of physical and . These include the clinical evalupsychological functioning; wer, range of motion circulatory and motor deficits producing weakness and loss of s. Technical measurements may personal functioning; ting (strength, electrical activity and spasticity leading to limb deformity and selfcirculatory functions (blood pressure, image problems; MG while resting and under strain), bladder and bowel dysfunctions commonly hers. PRM specialists may use found in disabled patients; rements of performance such as pressure ulcers as a risk of immobility in spinal netic muscle testing and other movecord injured, diabetic, deconditioned and elderly rehabilitation of patients with cerpatients; ecialised diagnostic measures will be phagia evaluation in patients with dysphagia people with swallowing disorders
conjunction with t family and members Diagnostics and dimensions of body and participation process. Additiona assessed. Histor
analysing problems In order to obt relevant to the di standard investiga addition to clinic ratory analysis of Clinical evalua restrictions and f the rehabilitation p diagnostics in PRM ation of muscle po respiratory function include muscle tes others), testing of heart frequency, E lung function and ot standardised measu gait analysis, isoki ment functions. In tain conditions sp required, e.g. dys
measurements in patients with losing the enjoyment of eating and are at risk of aspi, or executive function analysis in ration pneumonia and malnutrition; n injury.68, 69 pain syndromes; ies can be assessed in many ways. communication difficulties; rtant methods are: sexuality and sexual dysfunction covering idenvities of single functions pertity and self-image issues as well as organ functioning; ent (e.g. walking test, grip tests or mood, behaviour and personality changes; nts, performance in standard changes to family dynamics, personal relations, ttings). These tests can be evalucareer opportunities and financial security. (assessed by PRM-doctors or spe308 December 2006
stroke, urodynamic spinal cord injury patients with brai Patients activit Examples of two impo Standardised acti formed by the pati handling of instrume ised occupational se ated qualitatively
EUROPA MEDICOPHYSICA
----------------------- Page 23----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC reviewed and up forms the basis cation on patien PRM speciali ment of a rehab time frame in w should include diagnosis; presenting p (according to th the individu carer/family the professi actions to t
cialised therapists) or quantitatively (performance dated by the rehabilitation team and time, capacity to lift loads, and others). of team members regular communi Assessments of more complex activities, such ts progress during rehabilitation. as the activities of daily living (washing oneself, sts are responsible for the developdressing, toileting and others) and performance in ilitation plan and for identifying the day-to-day living (walking, sitting, etc.). These hich it should be delivered. The plan assessments may be performed by rehabilitation the following information: professionals or may be self rated using standardised questionnaires. roblems and preserved functions Participation is mainly analysed in interviews e ICF framework; see chapter 3.2.); with the patient through standardised questionnaires. als goals; Socio-economic parameters (e.g. days of sick leave) are goals; used in order to evaluate social or occupational paronals goals; ticipation problems. ake.
Many assessment instruments in PRM combine parameters of body functions, activities and participation. These may be used to decide on the indication for ions in Physical and Rehabilitation rehabilitation measures (assignment) or to assess the result of the intervention (evaluation). The approprierse interventions. PRM-specialists ate instruments have to be chosen in accordance with ervention plan based on the diagnosis the individual functional problem and the phase of the of the patient. Thereafter, the specialist rehabilitation process.70 s the intervention aiming at solving the The relevant contextual factors with respect to the or another team member may do so. social and physical environment are evaluated by intergs the PRM-specialist will prescribe the views or standardised ICF-based checklists. For the entions include: diagnosis of personal factors, e.g. coping strategies of the nterventions: patients standardised questionnaires are available. Many tools can be used to evaluate both global iming at restoration or improveand specific functional capacity as well as the rehaructures and/or function, e.g. pain bilitation process.71 Some cross the individual ICF mation therapy, regulation of muscle components. For instance, the Functional Indepennt of cognition, improvement of dence Measure (FIM) 72 and the Barthel Index 73 incormance, treatment of depression. porate aspects of body functions and activities as well ocedures, including injections and as relevant co-morbidities and the extent of external es of drug administration. support needed. The choice of measures will depend nd review of interventions. on the phase and aims of the rehabilitation process ion. and the functional capacity of the individual. treatments: A list of diagnostic methods can be found py techniques for reversible stiff Appendix IV. ted soft tissue dysfunctions. py and exercise therapy. 5.5. Rehabilitation plan py. PRM devise and employ a rehabilitation plan for cluding ultrasound, heat and cold applieach individual to direct his or her future problem-oritherapy (e.g. Laser therapy), hydrotherentated rehabilitation (Table II). Patients actively partherapy, diathermy, massage therapy ticipate in its development along with the other mem-
5.6. Intervent Medicine PRM uses div develop an int and disability either perform given problems In other settin therapy. Interv 1) Medical i Medication a ment of body st therapy, inflam tone, improveme physical perfor Practical pr other techniqu Assessment a Prognosticat 2) Physical in Manual thera joints and rela Kinesiothera Electrothera 3) Others in cations, photo apy and balneo and lymph ther
apy (manual lymphatic drainage). bers of the patient-centred rehabilitation team. The nal therapy to a) analyse activities, emphasis of the plan varies depending on the particf daily living and occupation, support ular problems encountered, but the essential elements tructures (e.g. splints), b) teach the have a similar basic format. The plan must be regularly to overcome barriers to activity of daily Vol. 42 - No. 4 309
4) Occupatio such as those o impaired body s patient skills
EUROPA MEDICOPHYSICA
----------------------- Page 24----------------------N MEDICINE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATIO
TABLE II.An example of a some of the problems addressed in a rehabilitation plan. Problem Goals
Possible interventions
Body functions and activities Physical activity Achieve safe transfers Posture and movement training using Increase indoor and outdoor mobil ity equipment as necessary (achieve/improve walking, climb ing stairs, using private and publi c transPosture and movement training portation) Explore and train in use of mobility aids nd Communication Improve communication, speaking a Training directed by speech and language comprehending therapy to improve language and articulation Exploration and training in the use of assistive technology, as required Behaviour and mood Improve behaviour Medication, psychotherapy, behavioural therapy and cognitive behavioural therNormalise mood Reduce depression and anxiety by counselling and medication Pain Reduce pain Analgesic drugs, physical therapies, stress apy
management, use of coping and other strategies nce Incontinence Promote bowel and bladder contine Bladder retraining, pelvic floor exercise, medication, use of catheters and stomas Inability to Care for Self Achieve ability to wash, groom, d ress and Analysis of component parts of activity, toilet self restoration of ability using alternative methods retraining Participation Inability to manage indeTeach to prepare and cook meals a nd Analysis of component parts of activity, pendently at home manage household activities restoration of ability using alternative methods or sources of help and/or and/or equipment and/or
equipment and/or retraining Loss of employment Return to work Analysis of component parts of activity and of getting to work, restoration of abilities, job adaptation, work retraining, workplace adaptations and equipment, improvement in access to and support at work living (e.g. adjusting private facilities), c) train in the 10) Disability equipment, assistive technology, prospresence of impaired function and cognition and d) thetics, orthotics, technical supports and aids. enhance motivation. 11) Patient education. 5) Speech and language therapy within the frame12) Rehabilitation nursing. work of complex specialized rehabilitation programmes. 5.7. Physical and Rehabilitation Medicine practice 6) Dysphagia management. Clinical activities and settings 7) Neuropsychological interventions. PRM specialists are involved in all stages of the 8) Psychological assessment and interventions, rehabilitation and recovery processes, as well as in the including counselling.
care of patients with chronic conditions. They practise 9) Nutritional therapy. in a variety of clinical settings ranging from acute care 310 YSICA ----------------------- Page 25----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC mation on the p functional stat discharge as we mendations for tation. In out patie there is a diff emphasis here i ation of treatm tional assessme gle series of t fessional rehab is adopted. Fol reassesses the ventions or dis as appropriate. PMR-speciali and family and patients general ists, particula needed in other ology, orthopae PMR speciali cialised commun for acquired br EUROPA MEDICOPH December 2006
facilities, stand alone rehabilitation centres, hospital resenting conditions, the patients based rehabilitation departments to community sete, activity capacity and participation at tings and independent specialist practice. Their activll as on the prognosis and recomities vary according to the clinical settings, but they further care, treatment and rehabiliadopt the same general principles of PRM in all. Specialised rehabilitation facilities are essential in nt departments and private practice, acute hospitals. There should be dedicated beds under erent emphasis on PRM practice. The the responsibility of a PRM specialist together with a s on diagnostic assessment and initiperipatetic rehabilitation team providing advice and ent. After an investigation and functreatments to patients in intensive care units and othnt, patients are prescribed either a siner acute wards. PRM provides the diagnostics and herapy (PT, OT, or others) or, if multi-proassessments as well as the interventions both for ilitation is required, a team approach patients in their dedicated facilities as well as for lowing treatment, the PRM-specialist patients in other wards. The consultative role of the patient and decides on further interPRM specialist helps to ensure that rehabilitation, charge back to the primary physician, functional restoration and prevention of secondary loss of function e.g. from immobilisation (such as consts cooperate closely with the patient tracture, pneumonia or thrombosis) start as soon as aim to communicate well with the possible. Early specialised rehabilitation prevents and practitioner and with other specialor reduces long-term restrictions of functioning.60-62 rly, when diagnostics or therapies are In the immediate period following injury, it is medical fields e.g. neurology, cardiknown that the simple act of transferring a braindic surgery etc. injured patient from a busy surgical or neurosurgical sts may in addition work with speward to the calmer, quieter atmosphere of a rehability rehabilitation teams (such as those itation ward has a therapeutic effect in itself and
ain injury, for chronic neurological disimprovement in attention, irritability and cognition is itional problems or for musculoskeletal observed.54 Acute general wards are not conducive to also provide advice to general comthe practice of multi-professional rehabilitation for patients with complex needs. In rehabilitation centres (including day-hospital care) and rehabilitation departments of acute hospi6. Standards in Physical tals all patients are seen by a PRM-specialist. He or she d Rehabilitation Medicine investigates the patient, performs functional assessments and explores the influence of contextual factors and training on functioning. The necessary interventions are selectST TRAINING ed, e.g. physical therapies, psychotherapy, occupational therapy, speech therapy, neuropsychological dependent medical speciality in all training, drugs or social interventions. Therapists also ies, except Denmark and Malta, but evaluate the patient prior to applying their intervencus varies somewhat according to diftion techniques. The results of the PRM-specialist traditions and laws. Training usually investigations and therapists functional assessments four and six years depending on form the basis for the rehab plan and further deci(Table III) (UEMS Charter on Training, sions made by the rehabilitation team. /16/EEC, 5 April 1993). Specialists in Decisions on discharging patients are the responm of mobility across UEMS member sibility of the PRM-specialist on the basis of team conuire certification from their national ference, in which the person with disability and the ities. Those with the latter are eligible family members actively participate. PRM-specialists d by the European Board of PRM, provide a comprehensive discharge report on the oped a comprehensive system of basis of the investigations and the information proucation for PRM-specialists (Appendix vided by the team members. This report covers inforts of: Vol. 42 - No. 4 311
ease, for trans disorders) and munity teams.
an 6.1. Education 6.1.1. SPECIALI PRM is an in European countr its name and fo ferent national lasts for between the country66 EC Directive 93 PRM have freedo states, but req training author to be recognise which has devel postgraduate ed V). This consis
EUROPA MEDICOPHYSICA
----------------------- Page 26----------------------MEDICINE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION
TABLE III.Name of the Specialty in UEMS Member States. Country Name of speciality
Austria zin und allgemeine Rehabilitation Belgium e en Revalidatie de Radaptation Croatia i rehabilitacija Cyprus Czech Republic lka stv Denmark Estonia atria Finland France de Radaptation Germany Rehabilitative Medizin Greece Hungary habilitci Iceland icine Ireland
Physikalische Medi Fysiche Geneeskund Mdecine Physique et Fizikalna medicine
Rehabilitan a fyzikln Fysiurgi Taastusravi ja fsia Fysiatria Mdecine Physique et Physikalische und
Fizioterapia es Re Endurhfingarlkningar Rehabilitation Med Medicina Fisica e -
Italy Riabilitativa tacija Latvia
Medicniska Rehabili Fizine medicina ir Mdecine Physique et Revalidatie Genees Fysikalsk medisin Medycyna fizykalna Medicina Fsica e de Medicina Fizica i d Fizikalna Medicina Fyziatria, balneolg Fizikalna in rehab Medicina Fisica y RehabiliteringsMed Mdecine Physique e
Lithuania reabilitacija Luxembourg de Radaptation Malta The Netherlands kunde Norway og rehabilitering Poland i rehabilitacja Portugal Reabilitao Romania e Recuperare Serbia and Montenegro I Rehabilitacija Slovakia ia and lieebn rehabilitcia Slovenia ilitacijska medicina Spain Rehabilitacin Sweden icin Switzerland
t de Radaptation zin und Rehabilitation Turkey habilitasyon United Kingdom icine a curriculum for postgraduate education conS covers the continuing medical education system taining basic knowledge and the application of PRM or the purpose of ten yearly revalidation. (See parain specific health conditions; raph 6.3 below). a standardised training course of at least four Further information on the regulations of this eduyears in a PRM department and registered in detail in ation and training system are available on the a uniform official logbook; ections website, www.euro-prm.org, where appli a single written annual examination throughout ion forms are also available. Europe; There are currently 10,280 PRM-specialists in a system of national managers for training and ope, of whom 2,000 are European Board certified accreditation to foster good contacts with trainees in nd 2,800 are trainees. Seventy training sites are recogtheir country; ised by the PRM-Board and a list of these is available n the website.75 standard rules for the accreditation of trainers and a process of certification; .1.2. UNDERGRADUATE TRAINING quality control of training sites performed by site visits of accredited specialists; The UEMS Section is gathering data on undergrad continuing professional development within the e training in PRM (i.e. for medical students) and will 312 SICA ----------------------- Page 27----------------------ICINE IN EUROPE
Physikalische Medi Fiziksel Tip ve Re Rehabilitation Med UEM f g
c S cat
Eur a n o
uat EUROPA MEDICOPHY December 2006
WHITE BOOK ON PHYSICAL AND REHABILITATION MED
report in the near future. The following principles are important in providing a systematic approach: SubSubSubAnyone may require rehabilitation in any health speciality speciality speciality skills skills skills setting (e.g. hospitals, general practice, nursing institutions). As a result, all physicians need to gain a (e.g. Rehabilita- (e.g. Rehabilita- (e.g. Phisical
tion of patients tion of patients Medicine or basic knowledge of rehabilitation, recognising that with spinal cord with muscolo- Sports Medicine) most will not practise as specialists in the field or carinjury) skeletal disorder and amputation) ry out specific rehabilitation measures. It is thus important that well-trained PRM specialists teach PRM in all undergraduate medical faculties and the followPhysical and Rehabilitation Medicine ing topics are required as a minimum: the principles of rehabilitation and the bio-psyCommon trunk: Internal Medicine, Surgery and others cho-social model of the international classification of functioning, disability and health; Basic medical skills the organisation and practice of rehabilitation Human and societal skills system (acute and post-acute rehabilitation, as well as rehabilitation programmes for patients with chronic ompetency principles. conditions); the principles and potential of physiotherapy, occupational therapy and other rehabilitation theranhanced by knowledge and experience of pies; lty work (Figure 3). Subspecialty compe comprehensive rehabilitation programmes and under development in some European their main indications; . the rehabilitative needs of patients with special petencies include: conditions (e.g. stroke, multiple trauma, low back assessment in determining the underpain, arthritis, cancer, etc.); gnosis; knowledge of the social system and legislation t of functional capacity and the abiliconcerning disability and rehabilitation at national nge; level, as well as ethical and human rights issues in ent of activity and participation as well rehabilitation. tual factors (personal characteristics and These concepts already form part of obligatory nt (see paragraph 3.2.); training in PRM in some European countries (Belgium, ge of core rehabilitation processes and France, Germany, Spain, UK) and some universities
Figure 3.C
further e subspecia tencies are countries Those com medical lying dia assessmen ty to cha assessm as contex environme knowled
(e.g. Vienna).75, 76 dence base; (see paragraphs 4.1 and 4.4) g a rehabilitation plan (see paragraph 6.2. Clinical Governance and competencies ge, experience and application of medNot only is it important that everyone has equiphysical treatments (including physical modaltable access to rehabilitation, but this should be comtural factors and others; see paragraph 5.6.); petently and sensitively delivered. Feedback from serion and measurement of outcome; vice users must be available to those responsible for ion and management of complications; these services. tication of disease/condition and rehaPRM specialists acquire a number of skills as part of n outcomes; their training. Their basic medical training gives them certain competencies, which are enhanced by knowlge of rehabilitations technology edge and experience acquired during their common s, prosthetics, technical aids and others); trunk training in internal medicine, surgery, psychianamics and leadership skills; try, etc. The core specialty competencies of PRM are g skills (patients, carer, team members provided during their specialist training and these are s); Vol. 42 - No. 4 ----------------------- Page 28----------------------E IN EUROPE 313
their evi devisin 5.5); knowled ical and ities, na evaluat prevent prognos bilitatio knowled (orthotic team dy teachin and other EUROPA MEDICOPHYSICA
WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN (www.euro-prm.org). their CME requirem and this is becoming well as European l lished in certain increasingly requi given in Appendix The first Europ the European Schoo
knowledge of social system and legislation on Doctors are required to fulfil disablement; ents before they can be validated basic knowledge of economic (and financial) an essential part of national as aspects of rehabilitation. ife. Obligatory CPD/CME is estabPRM specialists routinely use a number of other countries of Europe and is becoming aptitudes. They need good communication and interred in medical practice. The rules are personal skills and the ability to educate and manVI. age their patients and their families. They will adopt ean Board sponsored event has been strategies to allow patients to develop their own copl in Marseille on Posture and
ing skills. They will communicate with other agenwhich was established in 2000. cies (health and social-services and self-help groups) two-week course, which attracts to get the best for their patients. They also have a and other rehabilitation profesrole in the development of services for people with ver Europe. Other courses have also disabilities for which they will need relevant abilities. the Board and more will follow. 6.3. Continuing Professional Development n of Physical and Rehabilitation Medical Education he Union Europenne des Mdecins Continuing Professional Development (CPD) and Continuing Medical Education (CME) are an integral part of medical specialists professional practice and e des Mdecins Spcialistes PRM specialists need to demonstrate their continued in 1958 as the only statutory competence like all other doctors. CPD covers all e European Union to have a responaspects of updating medical practitioners, of which tal-based specialties. It is composed CME is one component. The specialty has set up varions for each specialty in Europe and ious teaching programmes across Europe, which serve ilitation Medicine was among the to educate PRM specialists and their colleagues in to be recognised as a distinct discirehabilitation teams. These cover basic science and tion was created 1971 and the clinical teaching topics, as well as investigational and PRM in 1991 as a part of the spetechnical programmes. t has, in particular, developed its trainA CME and CPD program is organised on European professional development base. As level for accreditation of international PRM congressf the European Commission, the es and events. The programme is based on the proe to the Standing Committee of visions of the mutual agreement signed between the national responsible medical organUEMS European Accreditation Council of CME (EACe. Specialties recognised in twoCME) and the UEMS-PRM-Section and Board (Chapter S member state are entitled to form 6.4). The European provisions are the same for all on. PRM is recognised as a core serspecialities. The PRM-Board has created the CPD/CME e 28 member states of the Greater Committee, which is responsible for the relevant conthe newer associate members tinuing programs within our speciality, for the accrede principles. PRM is one of the few itation of the several scientific events on European ight across Europe and is repreand
Movement Analysis, This is an annual doctors, engineers sionals from all o been set up under 6.4. The Sectio
Medicine of t Spcialistes 6.4.1. HISTORY The Union Europenn (UEMS) was created medical body in th sibility for hospi of specialist sect Physical and Rehab first specialties pline. The PRM sec European Board of cialist Section. I ing and continuing a statutory body o UEMS is accountabl Doctors, to which isations contribut thirds of each UEM a specialist secti vice in each of th European space and also adopt the sam to be recognised r
level and the scientific status of the Board Certified cil of the UEMS. PRM specialists. EACCME is responsible for coordinating this activND ROLE OF THE ORGANISATION ity for all medical specialties and the UEMS website gives details of the continuing medical education n Europe is therefore organised requirements for all specialists in Europe ction of the UEMS (Figure 4). This (www.uems.org). Each Board recognised PRM spey responsible to the European cialist is required to gain 250 educational credits over alth and is the only official meda five-year period for the purposes of revalidation ed by the European Union. The 314 December 2006
sented on the Coun
6.4.2. STRUCTURE A The specialty i through the PRM se is a statutory bod Commissioner of He ical body recognis
EUROPA MEDICOPHYSICA
----------------------- Page 29----------------------ICINE IN EUROPE ers n E.U. Advisory Committee on Medical Training s rs ical ) National Organisation of Medical Doctors (G.P.s and Specialist) National Organisation of Medical Specialist Specialist Professional and Scientific Associations Standing Comitate of European Docto Union of European Med Specialist (UEMS (UEMS) Specialist Secti Section Working Group European Board (see Fi European Parlament WHITE BOOK ON PHYSICAL AND REHABILITATION MED Council of Minist European Commissio
E.U. Directives
ons s and gure 5)
Figure 4.European Union Medical Organisations. Sections aim is to promote the specialty in a profesAffairs Committee; Clinical
sional capacity and to harmonise the specialty at a sional Practice Committee. European level through specialist training and continuing professional development through revalidation. MBERS It works to develop clinical standards in practice and to facilitate the specialty to undertake the required ing the accession of ten new member states research to develop it further. To this end, it is accountEuropean Union on 1st May 2004, there are able (as with other specialties) to the UEMS and has ropean Union full members along with started to work closely now with the European nd, Norway and Iceland. Romania, Bulgaria, Commission and the Council of Europe. It has active nd Turkey are observers. Within these counliaison with many bodies, such as the International ere are over 10,280 trained specialists with Society for Physical Medicine and Rehabilitation, the inees.75 The UEMS therefore has a major task American Academy of PMR and the Bone and Joint relevant link between all these countries at Decade. It has three main committees under an n level. The numbers of specialists in Executive Committee and Figure 5 demonstrates its and Rehabilitation Medicine across Europe tasks. The Section works closely with other European nsiderably and Appendix III shows the demoPRM bodies, such as the Acadmie Europenne de ls. Mdecine de Radaptation and the European Society l structure of PRM services across Europe of PRM. r despite the differences between health care The Committees of the Section are (Figure 5): Proposals for clinical standards are being Training and Education Committee (a statutory r during this process in the form of praccommittee - the European Board of PRM); d round health related groups. Vol. 42 - No. 4 ----------------------- Page 30----------------------MEDICINE IN EUROPE
Profes
6.4.3. ME Follow into the now 28 Eu Switzerla Croatia a tries, th 2,800 tra to make a a Europea Physical varies co graphic detai The genera is simila systems. put togethe tice base
EUROPA MEDICOPHYSICA 315
WHITE BOOK ON PHYSICAL AND REHABILITATION Executive Committee President, Secreta Treasurer, Assistant Se Chairman of Sub-Committ Committee Member
ry cretary ees
ittee Training Exam eciality
PRM Board
Professional Committee Content of PRM specialty
Clinical Affairs Comm Clinical standards
Site Visits
University/service/private practice Clinical issues in sp New service and academic posts
ivity
and Sub-specialty act
Education CME
Definition of academic Poss and clarification Between member states Career pathways
Research: links with European Society P Acadmie Europenne
RM
Congresses Exchanges
Demography Advertising and sponsorship Advise exec. committee on relation with: Other specialities and professions UEMS/ACMT, EU, WHO Figure 5.Structure of the UEMS Section of PRM. 6.4.4. TRAINING IN PHYSICAL AND REHABILITATION MEDICINE luding the specialtys curriculum can be obtained Specialist training is described in paragraph 6.4.1. ough the Sections website at www.euro-prm.org pendix V). The route to start training is slightly different in each country, but, despite different entry points to the specialist training programme, the curriculum has much . The Acadmie Europenne de Mdecine similarity across the continent and is consistent with Radaptation that of the American Board. The European Board of This body of up to 50 senior doctors in the specialty PRM has the task of harmonising specialist training oss Europe was created in 1969. Academicians are across Europe and has taken on the following roles.73 ited on the basis of their distinguished contribution European examination for recognition of spee specialty, particularly its humanitarian aspects. cialist training; aim of the Acadmie is to improve all areas of continuing professional development and medilitation for the benefit of those who need it. It inc thr (Ap
de
6.5
acr inv to th The rehab
ical education with ten-yearly revalidation; s promotes education and research across Europe, recognition of European trainers and g as a reference point in scientific, educational and units through site visits. earch matters, exchanging ideas and information, The eventual aim of this harmonisation is to produce ilitating the exchange of PRM doctors between difspecialists who can work across European health care ent countries and engaging in moral and ethical systems and allow national medical authorities/ ate. employers to recognise the knowledge and expertise Its motto is: Societas vir origo ac finis which can be of the specialists who have been trained in another nslated as Man is both the source and the goal of part of Europe. All aspects of the Section and Board, iety. 316 CA ----------------------- Page 31----------------------NE IN EUROPE
thu training actin res fac fer deb
tra Soc
EUROPA MEDICOPHYSI December 2006
WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICI State of the Ar Clinical Standar Effective Interventi Musculoskeletal Rehabilitation: 13th tion, Brighton, Advances in P Concepts, 14th Eu Vienna, Austria, Evidence Base Rehabilitation Med betes mellitus 1 tion, Madrid, Spain, Future Europe with standards s and course. Acco
The Acadmie is entirely independent. Its publicat in Rehabilitation Medicine tions support education and further research. It is ds, Measurement of Outcomes and responsible for a series of state of the art monoons in Neurological Rehabilitation, graphs, which include: Rehabilitation and Amputee La Plasticit de la Fonction Motrice. Ed. J-P.Didier European Congress of Rehabilita(Springer 2004). This to be produced in Italian in UK, 2002; 2007; MR Traditional and Modern Assessment in Physical Medicine and Rehabiliropean Congress of Rehabilitation, tation. Eds. M.Barat and F.Franchignoni (Maugeri 2004; Foundation Books 2004); d Rehabilitation, Physical and Vocational Rehabilitation. Ed. C.Gobelet and icine in lung transplant and in diaF.Franchignoni (Springer 2006); 5th European Congress of Rehabilita Les Fonctions Sphinctriennes. Ed A.Chantraine 2006. (Springer 2006). an Congresses for PRM will comply Further publications are due, such as in the field of et by the ESPRM for their organization oncological and pain rehabilitation.
rdingly, congresses will have a stanThe Academie debates ethical matters and in this me with half a day each for: acts as a guardian of the specialtys views. A recent debate was summarized and published as a brief comiology (basic sciences); munication, entitled Violence and Handicap.76 ology (rehabilitation technolSeveral courses are supported by the Acadmie, including the European School on Posture and nces (PRM in special health condiMovement Analysis in the University of Marseille which is supported by Erasmus funding. To encourning sciences (including epiage original research in the field of PRM by young l functioning and related topics). researchers, the Acadmie gives an annual prize, supported by the Swiss Paraplegic Association. Details of PRM does not depend on governmay be obtained from the Secretary. companies, politicians or other proon the activities of practitioners with6.6. The European Society of Physical and Rehabilitation Medicine The European Society of PRM was founded in 2003 7. Research in Physical and is concerned with research and teaching in PRM Rehabilitation Medicine in Europe. It succeeded the European Federation of Physical Medicine and Rehabilitation (established in of research in establishing needs 1963) and aims to coordinate European activities and lue of both current and new approachbe a vehicle for scientific exchange. The society offers individual membership to all eligible PRM specialists and federated membership members of the national endorsed the principles of evidencePRM societies in Europe. Individual membership is nd research in PRM has made great free of charge. The ESPRM is establishing an interacthe last two decades. Whereas the tive electronic platform (www.esprm.org), where chanisms of action of physical modalinformation can be found on research projects, on n have traditionally been central to scigrants and funding and offers updated information during the last 15 years, an increasing about courses, congresses, exchange funding, etc. ctive trials have been performed, in The ESPRM organizes biennial scientific conal efficacy of rehabilitation in many disgresses in the field. The main topics of the last three ow back pain, stroke, brain and spinal were:
dardised program functioning b functioning techn ogy); clinical scie tions); human functio demiology, socia The vitality ment, insurance fessionals, but in the field.
and 7.1. Importance and the va es PRM has fully based medicine a progress during physiological me ities of functio entific interest number of prospe which the clinic eases, such as l cord injury,77-7
9 rheumatoid arthritis, cardiovascular, Vol. 42 - No. 4 317 EUROPA MEDICOPHYSICA
----------------------- Page 32----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN entifically sounde bilitation. Government agen dence of the costusually require th ed because a wide to be available to the differing need patients. This really is tice produces resu play between
pulmonary and metabolic disorders, has been testr analysis of effectiveness in rehaed. For some conditions, meta-analyses of controlled trials are already available. cies and providers often seek evieffectiveness of rehabilitation and 7.1.1. RELEVANCE OF RESEARCH e service as a whole to be evaluatrange of different techniques has The specialty aims to foster an increased interest and the treating team in order to meet involvement in research in rehabilitation. Its vision is s of individuals in any group of that research is necessary to understand the basic processes of rehabilitation such as how individuals the nub of the problem, as PRM pracacquire new skills, and how the tissues of the body lts through a series of, or the inter(for example, the muscles, or neuronal pathways in the a number of interventions. central nervous system) can recover from or adapt to impact of a single rehabilitation the effects of trauma or disease. Research can also t real life and while essential for delineate the incidence and prevalence of disabiliive individual procedures to be ties, and identify the determinants both of recovery ramme, cannot in itself effectively and of the capacity to change, to acquire new skills, amme as a whole. There are curand to respond to rehabilitation. initiatives in addressing these techNew technologies emerge and should be adapted ic problems, so as to enable effecfor use by people with disabilities. Rehabilitation techutility to be regularly monitored in nology is one of the most important and promising ctice. research fields today and in the future. Tissue engineering and other modern technologies are conlities and resources tributing to this field. The costs of health care and of rehabilitation services will increase and politicians ant step that has to be made to will force health care providers to restrict their expensand amount of research in PRM is es and to show that they organize this care efficient-
Demonstrating the intervention is no identifying effect included in a prog evaluate the progr rently a number of nical and scientif tiveness and costrehabilitation pra
7.2. Research faci The most import improve the level to organize a plat
form for communication for all parly. PRM is a reliable partner in the discussion with rch activities in Europe. Information patients, politicians, ministries of health and insururrent projects, about funding and ance companies, as it has the capacity to base its arguocols, questionnaires, measuring ments on sound evidence in the public arena, which ge-programmes must become only research can provide. easily accessible for clinicians, nagers. To answer pressing ques7.1.2. CHALLENGES TO RESEARCH IN PHYSICAL tiveness of rehabilitation interventions REHABILITATION MEDICINE onsiderable funding for research. AND
ticipants in resea about future and c grants, about prot devices and exchan available and
researchers and ma tions on the effec will necessitate c To answer to th sitate considerabl the field of PRM. a national level, cooperation with o will help to reduc sonal and a commun
ese relevant questions will necesRehabilitation research does not sit comfortably e increase of funding for research in with standard approaches to basic science and medOn a European level as well as on ical practice research interventions. Progress in cliniresearch planning is necessary and metrics has been considerable. Therefore randomised ther research field is needed. This controlled studies are possible in many areas, but are e the impact of disabilities at a perless effective when the objectives sought and worked ity level. for in a group of subjects differ between individuals, especially when this occurs for personal or social ning rather than for biological reasons. The clinical trial designs that have been developed in the field of clinical requirements of rehabilitation ical psychology are often more fruitful and scientifie understood by all those practising cally appropriate than designs developed for the nce so much in rehabilitation requires assessment of drug effects. A combination of qualitaal and multi-disciplinary effort, multive and quantitative methods often provides a scisearch groupings and departments pro318 December 2006
7.3. Research trai The above techn research need to b rehabilitation. Si a multi-profession ti-professional re
EUROPA MEDICOPHYSICA
----------------------- Page 33----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC including quali scientific evid A scientific
vide the most fertile ground for training in the various ty assurance and treatments based on rehabilitation professions including medicine. It makes ence; little sense for clinicians to implement rehabilitation
basis to develop rehabilitation modholistically and in a multi-professional fashion, but to rds of care to guide clinical practice. undertake research exclusively in uni-professional research teams that are isolated from each other. Every effort is made to expose trainees in PRM to the benefits of such multi-professional and multidisciplinary research reach these goals in PRM, the following teams. Although the current resources in many countries quired: are still inadequate to meet the research training needs he general understanding and awareof all but the most gifted trainees in PRM, the situation ds of people with disabilities; is gradually improving. The cadre of trainees, who hold the benefits of rehabilitation. This will a PhD or equivalent level qualification in addition to their re in which access to adequate rehaprofessional qualification, will be the bedrock, upon een as a basic human right; which future research and academic activity depend. e understanding and cooperation ernmental organisations of people 7.4. Publication of research findings ecialty of PRM; The results of scientific research in PRM are pubcomprehensive rehabilitation facililished in general professional journals within each ope with specialized and well-trained country. At a European level specialists read a variteams and well resourced rehabilitation ety of scientific journals, which include the Journal ionally community based rehabilitaof Rehabilitation Medicine (which currently has the hould be in place for the managehighest impact factor worldwide), Disability and ling diseases; Rehabilitation, Clinical Rehabilitation, Archives of ensure that Physical and Physical Medicine and Rehabilitationand Europa cine has sufficiently well-trained Medicophysica and all of them publish multidisciPRM specialists available in all plinary research. ies; common high standards of care on rrent evidence. These should take into 8. Future developments y control and access to assistive tech8.1. Philosophy te new technical developments into Life expectancy is increasing in both developed his has a great deal to offer in assistand developing countries. More importantly, improvetation to produce better outcomes. ments in survival following injury and illness, as well
els and standa 8.2. Goals In order to measures are re to improve t ness of the nee to publicise lead to a cultu bilitation is s to deepen th between non-gov with and the sp to establish ties across Eur rehabilitation facilities. Addit tion structures s ment of chronic disab to set up systems to Rehabilitation Medi and competent
European countr to establish the basis of cu account qualit nology; to incorpora PRM practice. T ing rehabili
Increasing tech
nology should contribute significantly as an ageing population will result in an increased living and quality of live of people need for rehabilitation services in all European counes in Europe; tries, where the expectation of a high quality of life will cientific activities and research in the also increase.80 As a result, rehabilitation systems have habilitation with adequate funding to to be developed continuously considering the folcomes for those experiencing dislowing principles: Rehabilitation following injury or illness and in environment where people with chronic conditions is a basic human right;81 an fully participate in society. The PRM Equitable and easy access to all aspects of rehaork with people with disabilities in furbilitation including specialist rehabilitation medicine, m. assistive technology and social support for the entire asures will better enable people with population in Europe; contribute to society substantially to the Uniformly high standards of care in rehabilitation, ope. Vol. 42 - No. 4 319
to independent with disabiliti to promote s field of re
improve the out abilities; to support an disabilities c specialist will w thering this ai All these me disability to community in Eur
EUROPA MEDICOPHYSICA
----------------------- Page 34----------------------MEDICINE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION 2 MH
9. References 4. Stucki G, Kroeling P. Principles of rehabilitation. In: Hochberg MC, Silman AJ, Smolen JS, Weinblatt ME, Weisman
editors.Rheumatology. 3rd ed. Vol. 1. Edinburgh: Mosby; 2003. 1. European Academy of Rehabilitation Medicine, European p. 517-30. Federation of Physical and Rehabilitation Medicine, European 5. Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustun BT, Stucki G. Union of Medical Specialists (Physical and Rehabilitation Medicine Identification of candidate categories of the International Section): White Book on Physical and Rehabilitation Medicine. Classification of Functioning Disability and Health (ICF) for a Universidad Complutense de Madrid; 1989. Generic ICF Core Set based on regression modelling. BMC Medical 2. Martin J, Meltzer H, Eliot D. Report 1; The Prevalence of Disability Research Methodology 2006;6:36. among Adults. Office of Population, Census and Surveys, Social
6. Stucki G, Sigl T. Assessment of the impact of disease on the indiSurvey Division. OPCS Surveys of Disability in Great Britain, 1988vidual. Best Pract Res Clin Rheumatol. 2003;17:451-73. 89. London: HMSO; 1988. 3. Bax MCO, Smythe DPL, Thomas AP. Health care for physically 7. Stucki G, Sangha O. Principles of rehabilitation. In: Klippel JH, handicapped young adults. BMJ 1988;296:1153-5. Dieppe PA editors. Rheumatology. 2nd ed. London: Mosby; 1997. 4. UEMS-PRM-Section: Definition of Physical and Rehabilitation p. 11.1-11.14. Medicine. www.euro-prm.org. 2005. 8. Medical Rehabilitation for people with physical and complex dis5. Ward AB, Chamberlain MA. Disabled Young Adults. In: Evans abilities. Report of a working party. London: Royal College of CD, Goodwill J, Chamberlain MA editors. Rehabilitation of the Physicians; 2000. Physically Disabled Adult. 2nd ed. London: Chapman & Hall; 9. Steiner WA, Ryser L, Huber E, Uebelhart D, Aeschlimann A, Stucki 1996:191-8. G. Use of the ICF model as a clinical problem-solving tool in 6. Dennis M. Langhorne P. So stroke units save lives: where do we physical therapy and rehabilitation medicine. Phys Ther go from here? BMJ 1994;309:1273-7. 2002;82:1098-107. 7. Beyer HM, Beyer L, Ewert Th, Gadomski M, Gutenbrunner C, 0. Cieza A, Ewert T, Ustun TB, Chatterji S, Kostanjsek N, Stucki G. Krling P et al. Weibuch Physikalische Medizin und Rehabilitation. evelopment of ICF Core Sets for patients with chronic conditions. Physikalische Medizin: Rehabilitationsmedizin Kurortmedizin J Rehabil Med 2004;44 Suppl:9-11. 2002;12:M 1-M 30. 1. Stucki G, Grimby G. Applying the ICF in medicine. J Rehabil Med 8. Deutscher Bundestag (2004). Unterrichtung durch die Bundes2004;44 Suppl:5-6. regierung: Bericht der Bundesregierung ber die Lage behindertUstun B, Chatterji S, Kostanjsek N. Comments from WHO for the er Menschen und die Entwicklung ihrer Teilhabe. Drucksache Journal of Rehabilitation Medicine Special Supplement on ICF 15/4575: Bundesdruckerei, Berlin; 2005; p. 146. Core Sets. J Rehabil Med 2004;44 Suppl:7-8. 9. Rice-Oxley M, Turner-Stokes L. Effectiveness of brain injury reha3. Stucki G, Cieza A. Understanding functioning, disability and health bilitation. Clin Rehabil 1999;13 Suppl 1:7-24. in rheumatoid arthritis the basis for rehabilitation care. Curr 10. Redmond AD, Johnstone S, Maryosh J, Templeton J. A trauma Opin Rheumatol 2005;17:183-9. centre in the UK. Ann R Coll Surg Engl 1993;75:317-20. 4. UN Standard Rules to provide persons with disability full partici11. Templeton J. Organising the management of life-threatening pation and equality. New York: United Nations; 1994. injuries. J Bone Joint Surg Br 1994;76:3-5. 5. EU Council of Ministers Meeting, Malaga: European Union; 2003. 12. Kaste M, Skyhoj Olsen T, Orgogozo J, Bogousslavsky J, Hacke 6. Rehabilitation and integration of people with disabilities: policy and W. Organization of stroke care: education, stroke units and rehaintegration. Strasbourg: Council of Europe Publishing; 2003. 7th ed. bilitation. European Stroke Initiative (EUSI). Cerebrovasc Dis p. 369.
3 D
32.
3 3
2000;10 Suppl 3:1-11. 7. A coherent policy for people with disabilities. 1992. 13. Organised inpatient (stroke unit) care for stroke. Stroke Unit Recommendation R (92) 6. Strasbourg: Council of Europe; 1992. Trialists Collaboration. [update in Cochrane Database of Systematic The Standard Rules on the Equalization of Opportunities for Reviews]. Cochrane Database of Systematic Reviews; 2002. Persons with Disabilities (approved by UNO, 20 December 1993). 14. National Clinical Guidelines for Stroke. 2nd ed. Clinical EffectiNew York: United Nations; 1994. veness and Evaluation Unit, Royal College of Physicians. London: 9. Legh Smith JA, Denis R, Enderby PM. Selection of aphasic stroke Royal College of Physicians of London; 2004. patients for intensive speech therapy. J Neurol Neurosurg Psychiatry 15. Turner-Stokes L, Nyein K, Halliwell D. The Northwick Park care 1987;50:1488-92. needs assessment (NPCNA): a directly costable outcome meaure 0. Warner R. Stroke rehabilitation: benefits of educational initiatives. in rehabilitation. Clin Rehabil 1999;13:253-67. Br J Nurs 2000;9:2155-62. 16. Livingston MG, Brooks DN, Bond MR. Patient outcome in the 1. Grahn BE, Borgquist LA, Ekdahl CS. Rehabilitation benefits highyear following severe head injury and relatives psychiatric and ly motivated patients: a six-year prospective cost-effectiveness social functioning. J Neurol Neurosurg Psychiatry 1985;48:876-81. study. Int J Technol Assess Health Care 2004;20:214-21. 17. British Society of Rehabilitation Medicine Working Party Report on 2. Turner-Stokes L, Disler PB, Nair A, Wade DT. Multi-disciplinary Traumatic Brain Injury. London: British Society of Rehabilitation rehabilitation for acquired brain injury in adults of working age. Medicine; 1998. Cochrane Database Syst Rev 2005;(3):CD004170. 18. McLellan DL. Rehabilitation. BMJ 1991;303:355-7. 3. Wade DT. Community rehabilitation, or rehabilitation in the com19. Bent N, Tennant A, Swift T, Posnett J, Chamberlain MA. Team munity? Disabil Rehabil 2003;25:875-81. approach versus ad hoc health services for young people with 4. Turner-Stokes L. The evidence for the cost-effectiveness of rehaphysical disabilities: a retrospective cohort study. Lancet bilitation following acquired brain injury. Clin Med 2004;4:10-2 2002;360:1280-6. 5. Melin R, Fugl-Meyer AR. On prediction of vocational rehabilitation 20. World Health Organisation. International Classification of outcome at a Swedish employability institute. J Rehabil Med Functioning, Disability and Health: ICF: Geneva: WHO; 2001. 2003;35:284-9. 21. Stucki G, Ewert T, Cieza A. Value and application of the ICF in reha6. Didier JP. La plasticit de la fonction motrice. Collection de bilitation medicine. Disabil Rehabil 2002;24:932-8. lAcadmie Europenne de Mdecine de Radaptation. Paris: 22. Brandt E, Pope A. Enabling America: Assessing the Role of Springer Verlag; 2004. p.476. Rehabilitation Science and Engineering. Washington, DC: National 7. Krauth C, Hessel F, Klingelhfer HE, Schwelkert B, Hansmeier T, Academy Press; 1977. Wasem J. [Health Economic Evaluation of Rehabilitation 23. Stucki G. Rehabilitation medicine in rheumatic diseases. Curr Opin Programmes in the Rehabilitation Science Research Funding Rheumatol 2003;15:132-3. Programme in Germany]. Rehabilitation (Stuttg) 2005;44:297-306.
38.
320 ICA ----------------------- Page 35----------------------MEDICINE IN EUROPE
EUROPA MEDICOPHYS December 2006
WHITE BOOK ON PHYSICAL AND REHABILITATION 6
48. Boyd LA, Winstein CJ. Impact of explicit information on implicit 5. Guzmn J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, motor-sequence learning following cerebral artery stroke. Phys Bombardier C. Multidisciplinary bio-psycho-social rehabilitation for Ther 2003;83:976-89. chronic low back pain. (Cochrane Review). In: The Cochrane 49. Friberg F, Scherman MH. Can a teaching and learning perspective Library Issue 4. UK: John Wiley & Sons Ltd; 2004. deepen understanding of the concept of compliance? A theoreti6. Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhainen M, cal discussion. Scand J Caring Sci 2005;19:274-9. Hurri H et al. Multidisciplinary bio-psycho-social rehabilitation 50. Andr JMF. Fondements,stratgies et mthodes en mdecine ubacute low back pain among working age adults. (Cochrane physique et de radaptation. In: Held JP, Dizien O editors. Trait eview). In: The Cochrane Library Issue 4. UK: John Wiley & Sons de mdicine physique et de radaptation. Paris: Flammarion; 1999. td; 2004. p. 3-13. th 7. UEMS Charter on Specialty Training EC Directive 93/16/EEC. 51. SGB IX (9 Social law): Rehabilitation und Teilhabe behinderter Brussels. European Commission; 5 April 1993. Menschen. Beck-Texte. Dt. Mnchen: Taschenbuch-Verlag; 2001. Pradat-Diehl P, Azouvi P. Fonctions executives et rducation. 52. Garraway GM, Akhtar AJ, Prescott RJ, Hockey L. Management of Paris: Masson; 2006. acute stroke in the elderly: follow-up of a controlled trial. BMJ 9. Azouvi P, Perrier D, Van der Linden M. La rducation en neu1980;1:827-9. ropsychologie. Marseille: Solal; 1999. 53. Mazaux JM, De Seze M, Joseph PA, Barat M. Early rehabilitation 0. Mazaux JM. Aphasie. Paris: Masson; 2000. after severe brain injury: a French perspective. J Rehabil Medi 1. Tennant A. Principles and Practice of Measuring Outcome. In: 2001;33:99-109. Barat M, Franchignoni F editors. Advances in Physical Medicine and 54. Wade D. Investigating the effectiveness of rehabilitation profesRehabilitation: Assessment in Physical Medicine and Rehabilitation. sionsa misguided enterprise? Clin Rehabil 2005;19:1-3. Pavia: Maugeri Foundation Books; 2004. p. 35 55. Quintard B, Croze P, Mazaux JM, Rouxel L, Joseph PA, Richer E 2. Bethoux F, Calmels P. Guide de mesure et dvaluation en et al.Life satisfaction and psychosocial outcome in severe traumdecine physique et de radaptation. Paris: Roche; 2003. matic brain injuries in Aquitaine. Ann Readapt Med Phys 3. State University of New York at Buffalo. Guide to the use of the 2002;45:456-65. uniform dataset for medical rehabilitation (adult FIM). Version 4. 56. McLellan DL. Targets for rehabilitation. BMJ 1985;290:1514.
for s R L 6
68.
7 7
Buffalo, NY: State University of New York at Buffalo; 1993. 57. Nybo T, Sainio M, Muller K. Stability of vocational outcome in adulthood after moderate to severe pre-school brain injury. J Int 4. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Psychol Soc 2004;10:719-23. Md State M J 1965;14:61-5. 58. Association of British Neurologists, NeuroConcern Group of 5. Mau W, Glich M, Gutenbrunner C, Lampe B, Morfeld M, Medical Charities, British Society of Rehabilitation Medicine. Schwarzkopf SR et al. Lernziele im Querschnittsbereich Neurological Rehabilitation in the United Kingdom. Report of a Rehabilitation, Physikalische Medizin und Naturheilverfahren nach Working Party. London: British Society of Rehabilitation Medicine; der 9. Revision der Approbationsordnung fr rzte. Physikalische 1992. Medizin: Rehabilitationsmedizin, Kurortmedizin 2004;14:308-18. 59. NHS and Community Care Act 1990. London: HMSO; 1990. 6. Ward AB. Physical and Rehabilitation Medicine in Europe. J 60. Hall KM, Cope N. The benefits of rehabilitation in traumatic brain Rehabil Med 2006;38:81-6. injury: a literature review. J Head Trauma 1995;10:1-13. 7. Heilporn A, Andre JM, Didier JP, Chamberlain MA. Violence to and 61. Verplancke D, Snape S, Salisbury CF, Jones PW, Ward AB. A ranmaltreatment of people with disabilities: a short review. J Rehabil domised controlled trial of the management of early lower limb Med 2006;38:10-2. spasticity following acute acquired severe brain injury. Clin Rehabil 8. National Rehabilitation Guidelines Italian National Health Service2005;19:117-25. Ministry of Health Official Bulletin, Rome, 1998. 62. Stucki G, Stier-Jarmer M, Gadomski M, Berleth B, Smolenski U. 9. SPREAD National Stroke Guidelines- Italian National Health Service. [General early rehabilitation] Physikalische Medizin: 2001. www.sanita.it. Rehabilitationsmedizin, Kurortmedizin 2002;12:146-56. 0. Brain Injury Guideline Modena and Verona national Consensus 63. Glaesner, JJ, Harloff KJ, van de Weyer TH. [Rehabilitation in Acute Conference- 2001/2005 www.sanita.it Hospitals]. Fortschritt und Fortbildung in der Medizin 2005;29:13-9. 1. The Department of Health and Social Security: OPCS Surveys of 64. Franchignoni F, Salaffi F. Generic and specific measures for outdisability in Great Britain Report 1: The prevalence of disability come assessment in orthopaedic and rheumatological rehabilitaamong adults. 1988. tion. In: Barat M, Franchignoni F editors. Advances in Physical 2. Fifty-Eighth World Health Assembly: Resolution 58.23, Disability, Medicine and Rehabilitation: Assessment in Physical Medicine including prevention, management and rehabilitation. Geneva: and Rehabilitation. Pavia: Maugeri Foundation Books; 2004. p.58. World Health Organisation; 2005. Vol. 42 - No. 4 ICA ----------------------- Page 36----------------------E IN EUROPE
EUROPA MEDICOPHYS 321
WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN
el on ection]
APPENDIX Ia. Proposal for a New Definition Based on the ICF-Mod [Courtesy: G. Stucki and J. Melvin in cooperati with the professional Practice Committee of the UEMS-PRM-S
Based on the WHOs integrative model of human ing (e.g. depression , skin ulcers, thrombosis, joint functioning, PRM is the medical specialty with rehacontractures, oste oporosis and falls) and compensate bilitation as its core health strategy. It applies and for the absence or loss of body functions and strucintegrates the biomedical and engineering approach tures; to capitalise on a persons capacity through an 3) leading an d coordinating intervention proapproach, which builds on and strengthens the grammes to gain op timal performance in a multi-proresources of the person, provides for a facilitating fessional iterativ e problem-solving process; performenvironment and develops the persons performance ing, applying and in tegrating biomedical and engiin interacting with the environment. This includes the neering interventi ons; psychological and behavioral; diagnosis and treatment of health conditions. PRMs educational and coun seling; occupational and vocaeffectiveness is through: tional; social and architectural interventions; 1) assessing functioning in relation to health con4) providing gu idance to patients and their immeditions, personal and environmental factors includdiate environment, service providers and payers along ing prognosis; the potential to change the prognosis; the continuum of c are in all situations from the acute identification of long-term goals, intervention prohospital to the co mmunity; gramme goals, rehabilitation cycle goals and inter5) managing reh abilitation in health and multivention goals, as well as the evaluation of legal disagency services; ability; 6) advising the public to request and decision mak2) performing or applying biomedical and engiers to adopt and i mplement policies and programmes neering interventions to optimise capacity, including in health This (a) extends to sectors providing a physical modalities, pain relieving techniques; neufacilitating wider physical, social and economic enviropsychological interventions; nutritional and pharronment; (b) ensur es access to rehabilitation services macological interventions; engineering interventions as a human right; and (c) empowers PRM specialists including e.g. implants, prosthesis and orthoses, aids to provide timely and effective care to enable people and devices designed to stabilize, improve or restore experiencing/or at risk of disability to achieve and impaired body functions and structures. These will maintain optimal f unctioning in the interaction with minimise pain, fatigue and other symptoms, prevent the wider physical , social and economic environ-
impairments, medical complications and risks includ-
ment.
dicine
APPENDIX Ib. Description of the Specialty of Physical and Rehabilitation Me provided throug
Physical Medicine is the medical discipline that h multi-professional teamwork, covers, on a scientific basis, interventions aimed at herapists, occupational therapists improving physiological and mental functioning, iate health professionals, social using physiological mechanisms (such as reflexes, ional staff and engineers. (See functional adaptation and neuroplasticity), as well as physical and mental training. These are possible Medicine focuses not only on physafter an accurate functional diagnosis has been made but also on enabling people to parthrough functional testing, which is a specialised in society. This is over and above PRM competence. Physical Medicine is frequently efinition of Rehabilitation, which is 322 December 2006
including physiot and other appropr workers, educat
Chapter 5). Rehabilitation ical functioning, ticipate actively the established d
EUROPA MEDICOPHYSICA
----------------------- Page 37----------------------NE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICI
an active process by which those disabled by injury genital disabiliti es. To achieve this, activities such as or disease achieve full recovery, or, if full recovery is not self-care, walki ng, driving, shopping, learning and possible, realize their optimal physical, mental and many others will be trained in rehabilitation settings. social potential and are integrated into their most An overview of al l possible activities is listed in the appropriate environment2. Both are relevant to peoInternational Clas sification of Functioning, Disabilities ple with chronic illnesses, after trauma and with conand Health (ICF) 9 (see Chapter 3). APPENDIX II. Examples of disabling conditions commonly encountered by PRM s Musculoskeletal c Spinal disorde 1) Acute and c 2) Cervical spin 3) Thoracic spin Degenerative and
pecialists
The consequence of onditions rs Trauma hronic low back pain; Traumatic brain injury; e syndromes; Spinal cord injury; al disease; Multiple and complex trauma;
inflammatory joint disease; d poly-arthritis; Brachial plexus and peripheral nerve injuries; eumatism, (including fibromyalgia); Sports injuries; foot problems; Injuries associated with chronic disabling disease; loskeletal) pain syndromes; Occupational injuries. pain syndromes; igue syndromes and fibromyalgia. Neurological conditions isorders Stroke - including subarachnoid haemorrhage; Chronic disabling neurological conditions, e.g. isease; iciency; multiple sclerosis, Parkinsons disease; se; Central nervous system infections and abscess-
Other mono- an Soft tissue rh Complex hand and Osteoporosis; Chronic (muscu 1) Work-related 2) Chronic fat Cardiovascular d Coronary heart d Cardiac insuff Valvular disea Cardiomyopathi Peripheral vas tions; Arterial hyperte Respiratory conditio Asthma; Chronic obstructiv Pulmonary fibrosis Pneumoconiosis industrial injurie Obesity and meta Diabetes melli Metabolic syndro ruricaemia. Urinary tract co Chronic renal Urinary tract
es; es; cular disease, including amputa Central nervous system tumours; Spinal paralysis; nsion; Neuromuscular disorders and myopathies; Peripheral neuropathies, including Guillain-Barr ns Disease and nerve entrapment syndromes; Alzheimers Disease e pulmonary disease; Congenital conditions cerebral palsy, spina ; bifida, etc.; , including asbestosis and other Rare congenital problems. s. Acute and chronic pain conditions bolic conditions tus; Amputation (as consequence of posttraumatic, mes, hyperlipidaemia and hypevascular and in malignant diseases); Conditions after surgery (including organ transplantation), ICU treatment (including critical illness nditions polyneuropathy and immobilisation syndromes failure; (deconditioning) and multi organ failure).
tumours, including prostatic cancer; Vol. 42 - No. 4 323 EUROPA MEDICOPHYSICA
----------------------- Page 38----------------------MEDICINE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION Infec Bone Can sequ Age idiop Ol
Prostatism (prostatic hypertrophy); tious and immunological diseases Incontinence e.g. stress incontinence and postmarrow transplantation; surgical incontinence. Consequence of HIV infection. Gastrointestinal tract conditions cer and its consequences, including treatment Crohns Disease, Ulcerative colitis; elae and palliation Functional gastrointestinal disorders. related conditions Sexual dysfunction (other than neurological) Paediatric conditions, incl. congenital deformities, Sexuality issues; athic scoliosis, Perthes disease, spina bifida, etc.; Erectile dysfunction. d age problems.
States
APPENDIX III. PRM Specialists in Europe by UEMS Member
Practising PRM Country Specialists
Total No. No. of PRM
No. PRM
Total No.
No. of
specialists/ Population of Doctors of Specialists Specialties Trainees 100 000 pop.
Austria Belgium Croatia* Cyprus
134 450 299
85 80 40
29 100 38 700 15 600 2 000 35 000 15 000 8 968
1.85 4.40 6.80 0.90 4.67 2.18 11.70
13 150 16 365 8 200 1 850 27.000 6 000 4 312
7 300 000 10 240 000 4 600 000 1 000 000 10 300 000 5 500 000 1 351 000
44 24 43 41 80 23 40
9 Czech Republic 483 Denmark 120 Estonia 158
130 0
Finland France Germany Greece Hungary Iceland* Ireland Italy Latvia
152 1 760 1 571 164 140 10 5 2 200 120
30 125 65 33 27 3 2 350 7
19 000 183 700 394 432 60 700 40 829 900 6 050 307 600 8 588
2.92 2.97 1.96 1.49 1.38 3.72 0.13 3.85 5.42
10 500 95 000 261 437 15 200 29 280 4 650 160 000 7 437
5 200 000 61 300 000 80 000 000 11 000 000 10 117 000 270 000 4 000 000 59 000 000 2 300 000
35 38 43 37 92 33 51 45 46 No
Lithuania information available Luxembourg 8 Malta 1 The Netherlands 248 Norway* 183 Poland 900 Portugal 325 Romania* 690 Serbia and Montenegro 610 Slovakia information available Slovenia 68 Spain 2 150 Sweden 160 Switzerland* 269 Turkey* 1 300 United Kingdom 129 *) Not member of EU. 324 CA
0 0 78 58 120 100 164 120
810
2.00 0.25 1.65 3.00 2.30 3.25 3.14 5.80
520
400 000 400 000 15 000 000 4 300 000 39 000 000 10 000 000 22 000 000 10 500 00 27 30 58 46 58 41 No 39 51 60 44 36 58
39 800 18 404 109 000 29 950 44 630 25 000
16 500 13 982 65 000 14 530 37 670 20 000
19 292 20 50 200 57
4 547 157 900 27 000 25 251 91 000 150 000
3.40 4.89 1.88 3.59 1.86 0.27
3 362 70 000 17 600 23 170 33 000 21 000
2 000 000 44 000 000 8 500 000 7 502 000 70 000 000 58 000 000
EUROPA MEDICOPHYSI December 2006
----------------------- Page 39----------------------NE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICI
ion Medicine
APPENDIX IV. Diagnostic Tools and Assessments in Physical and Rehabilitat Activity and pa history/anam naires; relevant env 1) social situ 2) occupation er assets etc.; care needs; equipment ne environmenta tion). Special functio Gait analysi mentation for kinematic me ing temporal and trogoniometry, tems, digital vid etc.); kinetic (dynamometric p insole sensory etc.); surface EMG energetics. Quantification meas
Diagnosis and evaluation in PRM includes the folrticipation assessments lowing list. nesis, check-lists and questionDiagnosis of the disease ironmental factors; History; ation, family and friends, community; clinical examination; and employer, financial and oth clinical diagnostic tools, e.g. imaging, etc. Functional assessments eds (e.g. wheelchairs); l adaptations ( e.g. accommoda clinical functional examinations (e.g. muscle testing, range of motion, coordination, dexterity); standardised/clinical tests (timed up and go; functional reach, sit to stand and others) nal assessments technical tests (dynamometry: muscle endurance and strength; electrophysiologic testing, etc.); s laboratories, which contain instru rating scales and questionnaires, outcome measures; asures - patterns of motion includ somato-sensory testing (touch, temperature, presspatial parameters (goniometry/elecsure, pain, etc.); accelerometry, optoelectronic sys posture; mobility; reach, grasp and manipulaeocamera with dedicated software, tion; testing of sensation and special senses; ures - ground reaction forces latforms, pedobarography platforms, swallowing and nutrition; systems, portable walkway systems, sexuality; continence; activity in targeted muscles tissue viability (skin problems and pressure sores); bowel/bladder functioning; of other balance and mobility tasks
communication (speech, language and non-veric posturography, long term activibal); etc.). performance: activities of daily liv mood, behaviour, personality; gement, work and productive general health parameters, etc.; ding functional capacity evaluation neuropsychological testing (perception, memoysis), therapeutic driving evaluation, ry, executive functions, attention and others). ies. Vol. 42 - No. 4 325
(static and dynam ty monitoring, Occupational ing and home mana activities (inclu and job site anal leisure activit EUROPA MEDICOPHYSICA
----------------------- Page 40----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN APPENDIX V. Curriculum of studies and theoretical knowledge ) for the European Board Diploma in PRM (Version 2005 Application to levers; the differ to the locomotor s Knowledge of jo characteristics of Muscle contract tance, shortening ment. Factors
A) Specific Basic Knowledge of the Specialty the human body of systems of ent constituents of levers with relation Introduction: Philosophy, Objectives and Methodology ystem. of Physical and Rehabilitation Medicine. int structure, classification and 1) Historical aspects of the specialty. movements of joints. 2) Disability and the Rehabilitation Process. ions, internal and external resisof muscles and range of joint move2) a) Traditional medicine model. limiting the range of movement. 2) b) Physical and Rehabilitation Medicine model. muscles. Different mechanical types 2) c) Rehabilitation process. ion, mono and polyarticular mus3) Physical and Rehabilitation Medicine: an autoometric contractions, dynamic or isonomous specialty. ns. 2) a) Criteria for an autonomous specialty. ractions. Agonists, antagonists, syn2) b) Philosophy. ms. Kinetic chains. 2) c) Objectives. 2) d) Methodology.
Different types of of muscle contract cles. Static or is kinetic contractio Plyometric cont ergic muscle syste b) Specific. Physiology of j
oint and muscle function: spine 4) Role of a Specialist in Physical and Rehabilitation rt of the programme assumes a Medicine. led knowledge of the anatomy of 2) a) Medical tasks. em. 2) b) Medico social tasks. 2) c) Objectives and standards of the specialty. previous data to the analysis of nt in elementary activities of 2) d) Interdisciplinary work. ental positions and various posrehension, dexterity, walking, running Chapter 1. The fundamentals of Physical and Rehabilitation Medicine cal effects of exercise. Energy 1) Principles of general biomechanics, both kinetal regulation. Physiological costs, ic and kinematic. Forces, couples of forces, levers, pulmonary effects of exercise. moments, power, work, inertia, acceleration. demiology, methodology for clinical 2) Principles of behaviour and resistance of matecs. rials under force. A general understanding of strain and ed Medicine in the Specialty of the effects of strain. Characteristics of homogeneous ilitation Medicine. and composite materials. An elementary knowledge of the measurement of strain and deformity of various f cognitive function. materials. 3) Biomechanics: a general understanding of the ogy and basic physiopathology applications of the above paragraphs to living tissue. The biomechanics of the different tissues in the human ous system. body (particularly of the locomotor system). An eleervous system mentary knowledge of biomechanics of fluids and its rvous system application to fluids in the human body. 4) Study of human movement (kinesiology). r junction a) General. ogy of posture and movement. 326 December 2006
and limbs. This pa prerequisite detai the locomotor syst c) Applied. Application of posture and moveme human life: fundam tures, gestures, p and jumping. 5) The biochemi expenditure, therm cardiovascular and 6) Clinical epi research. Statisti 7) Evidence bas Physical and Rehab 8) ICF. 9) Assessment o Chapter 2. Physiol 1) Central nerv 2) Peripheral n 3) Autonomic ne 4) Muscle 5) Neuromuscula 6) Neurophysiol
EUROPA MEDICOPHYSICA
----------------------- Page 41----------------------INE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDIC c) Indic
7) Pain mechanisms; interaction of pain and move-
ations, prescriptions, controls on physment. eneral knowledge of technique, and techniques with regard to results of clinChapter 3. Clinical and functional assessment in ional assessment, type of pathology and Physical and Rehabilitation Medicine characteristics of each patient. Therapy modalities: utilisation of phys1) Clinical and functional assessment of joints and echniques, basic knowledge, the effects muscles; motor and sensory function. indications and contra indications. 2) Assessment of cognition, speech and language, herapy: galvanic currents; low, medium memory, behaviour, etc ... uency treatment. 3) Laboratory tests and imaging techniques. Rational al vibration. use of modern medical imaging in physical and rehaack. bilitation medicine. erapy: cold and heat treatment. 4) Quantitative evaluation by computerised recorderapy. ing of mechanical or kinetic phenomena (force plates) onal therapy. as well as movement or kinematic(s) (different modern tal ergonomics. forms of recording displacement of body segments). es and methods of occupational ther5) Electrodiagnosis: electromyography, nerve conduction studies and evoked potentials. s, equipment, technology and assess6) Pulmonary function tests. tional therapy. ications of occupational therapy: in 7) Cardiovascular function tests, oxygen saturation, raining, endurance training, in funcgraded exercise tests, physiological cost of energy. itation and in reintegration into the com8) Biochemical and pathological tests in current familial, domestic, professional and use in physical medicine and rehabilitation. aining). 9) Functional assessment: use and application of al assessment ,guidance and training. the ICF. Various scales, instruments, tests, and indices, nt and technical aids. utilised in conditions relevant to physical and rehaials used. bilitation medicine. ges. 10) Analysis of posture and movement (including ses (spine, limbs).
iotherapy: a g the choice of ical and funct the individual 2) Physical ical therapy t of treatment, a) Electrot and high freq b) Mechanic c) Biofeedb d) Thermoth e) Balneoth 3) Occupati Fundamen Principl apy. Material
ment in occupa The appl joint/muscle t tional rehabil munity (socioemployment tr Vocation 4*) Equipme a) Mater b) Banda c) Ortho
posturography and gait). heses: surgical indications for amputat for and rehabilitation of amputees. Chapter 4. Therapies in Physical and Rehabilitatherapy. tion Medicine ical aids and appliance : facilities, tools, means of transfers and of communi1) Physiotherapy onmental control, household equipment; a) Knowledge of the elementary techniques of re simple or sophisticated but likely to passive and active physiotherapy. Different techniques th disabilities in acquiring greater indeof manual and instrumental massage. Techniques of mproving their quality of life. functional rehabilitation of joint problems (manual chair advice and management. and instrumental). Muscle (re)training, stimulation of herapy. muscle activity, functional training. Techniques of siology of manual medicine. muscle strengthening, endurance training, retraining wledge. Clinical examination of the of abilities. b) Methods specific to physiotherapy in different Medicine and Rehabilitation specialists should have a pathologies. dge of materials used in orthoses and prostheses and nical properties. In addition, in those most commonly b) Techniques such as Cyriax, Mennell, etc ... owledge is expected of the process of their manub) Neuromuscular facilitation-inhibition technal extras, spare parts, and their application in clinical niques, e.g. Kabat, Bobath, Brunstrm, Vojta etc ... she should have a detailed knowledge of how to pred adapt them, to check on their application and to b) Management of lymphoedema rapeutic effects. Vol. 42 - No. 4 327
d) Prost tion. Equipmen e) Stoma f) Techn ADL equipment, cation, envir whether they a aid people wi pendence and i g) Wheel 5) Manual t Pathophy Anatomical kno *) Physical general knowle of their mecha used, further kn facture, additio practice; he or scribe them an assess their the EUROPA MEDICOPHYSICA
----------------------- Page 42----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN Chapter 5. The imm 1) Physiopathol ces on the a) Cardiovascul
spine and limbs. Dysfunction of intervertebral segobile patient ments. Principles of manual techniques. Indications ogy of immobilisation. Consequenand contra indications. Potential dangers of the manipulative acts. Clinical examination and assessment ar system.
6) Re-education in speech and language disorders, system. principles of and equipment and technology used in system. speech and language therapy. Language development stem (osteoporosis). in childhood. Assessment in speech therapy and its l and urological system. application to the rehabilitation of problems in articystem (skin-pressure sores). ulation, language (expression, comprehension, readtem. ing and writing). tal system. Assessment and management of swallowing disorogical system. ders. nd treatment of the above men7) Reintegration of people with disabilities into society. Principles and methods of clinical psychology and of social assistance (social work). Cognitive ocomotor system pathology in assessment (intellect, memory, concentration, behavical and Rehabilitation Medicine iour) and learning potential. Its application to cognitive and psychological and social abilities: memory and c conditions concentration, the patients understanding and accepory joint disease, polymyalgia tance of his problem, motivation for rehabilitation, tive tissue disorders. mood, difficulties in interpersonal relationships; vocarthropathies. gout, chondrocalcinosis. tional training and methods to ensure financial secucia, osteoporosis. rity. ease. Environmental implications. nd secondary malignant tumours of 8) Neuropsychological rehabilitation: assessment icular rheumatism. and management ular diseases. 9) Pharmacology: pharmacokinetics of drugs used ritis. in rehabilitation medicine; possible interactions with thology. the rehabilitation programme and with therapeutic sty. exercise. foot disorders. 10) Infiltration and injection techniques; acupunctary knowledge of joint surgery: ture otomy, arthrodesis.
b) Respiratory c) Nutritional d) Metabolic sy e) Nephrologica f ) Cutaneous s g) Muscular sys h) Musculoskele i) Neuropsychol 2) Prevention a tioned disorders. Chapter 6. Adult l Phys 1) Non traumati a) Inflammat
rheumatica, connec b) Crystal a c) Osteomala d) Pagets dis e) Primary a bone. f) Extra-art g) Neuromusc h) Osteoarth i) Spinal pa j) Arthropla l) Hand and m) An elemen arthroscopy, arthr
11) Extra-corporeal shock wave therapy in tenatigue syndrome and fibromyalgia. donitis. l pain syndrome. 12) Multidisciplinary pain management. nditions in adults. y and pathophysiology of tissue motor system. B) Applications to pathology. nd strains. ons. Traumatic and recurrent disloFor each of the following chapters, there has been no need to enter all the diverse descriptions of diseases : spinal (without neurological comincumbent on doctors in the specialty. It is sufficient : principles of specific treatment, to establish that specialists in Physical and ing surgery e.g. osteotomy. Rehabilitation Medicine should know, for each group disorders of the hand and foot. the clinical signs and symptoms, diagnostic tools, appropriate types of assessment and current therapy. ation. It is particularly important to know therapeutic effects procedures. of rehabilitation, the indications and contraindications. n and rehabilitation of complications. 328 December 2006
n) Chronic f o) Myofascia 2) Traumatic co a) Physiolog repair in the loco b) Sprains a c) Dislocati cations. d) Fractures plications), limbs repair time includ e) Specific 3) Burns: a) Classific b) Treatment c) Preventio
EUROPA MEDICOPHYSICA
----------------------- Page 43----------------------NE IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICI 3) Cardiomyop 4) Cardiac su Vascular diso Arterial syst 1) Arterial o gation, the plac tion at the vari 2) The rehabi stump, prostheti
Chapter 7. Physical and Rehabilitation Medicine athies and sport rgery rders: Physical and rehabilitation medicine related to sports em activities. cclusive disease of the legs: investiSports for people with disabilities. e of and technology of the rehabilitaous stages of the condition. Chapter 8. Physical and Rehabilitation Medicine. litation of amputees, care of the Nervous System Pathology cs.
Venous system 1) Central nervous system. ion and treatment of deep venous a) Vascular, neoplastic, traumatic, inflammatory, infective and degenerative conditions of brain and problems: ulcers, varicose ulcers. spinal cord. tem b) Spinal cord lesions: traumatic, neoplastic, others. Assessment and management of spinal cord lesions. ical and Rehabilitation Medicine c) Spinocerebellar degenerative conditions: in children Friedreichs disease, Strumpell Lorrain, etc. f child development: psychomod) Neuropsychological dysfunction. movement, sensory and cognitive 2) Peripheral nervous system. ting and evaluation of the stages of 3) Special sensory impairments ology in the developing locomotor Chapter 9. Physical and Rehabilitation Medicine ion between growth and anomalies and respiratory pathology eletal and joint structures. atrics cerebral palsy spina bifida 1) A fundamental appreciation of acute and chroncele. Infantile spinal amyotroic obstructive and restrictive syndromes. Aetiology -orthopaedic consequences of neuand therapeutic principles. ers, prevention, treatment and mon2) Principles of rehabilitation: functional assessment through pulmonary function tests. malformation of musculoskeletal sysa) Active and passive techniques of bronchial s, skeletal agenesis, congenital aplasias and postural drainage, manual clapping, instrumental hip dysplasia, club foot, other foot techniques. b) Patient education and training. turbances. c) Artificial ventilation, assisted respiration, domidiscrepancy. ciliary assisted respiration. Tracheostomy manage, congenital, secondary scolioses. ment. trauma: a general appreciation of traud) Equipment for assisted respiration. ation in children, notably bums and 3) a) Prevent thrombosis. 3) b) Venous Lymphatic sys
Chapter 11. Phys
1) Assessment o tor development, development. Tes development. 2) Pathophysi system. Interact in the musculosk 3) Neuropaedi and myelomeningo phies. The neuro rological disord itoring. 4) Congenital tem (spine, limb and dysplasias; malformations. 5) Growth dis 6) Lower limb 7) Idiopathic 8) Infantile ma and rehabilit
e) Surveillance and monitoring of treatment. hildren. 3) Their application ical and Rehabilitation Medicine Chapter 10. Physical and Rehabilitation Medicine in urological and sexual problems and cardiovascular pathology of physiology of continence of bladCardiac disorders: ntrol and anal sphincter functioning. 1) Cardiac rehabilitation in valvulopathy. hincter pathological conditions: neu2) Cardiac rehabilitation after myocardial infarcher. Urodynamics. Assessment and tion. Vol. 42 - No. 4 329
amputations in c
Chapter 12. Phys
1) Assessment der/sphincter co 2) Bladder/sp rological and ot treatment. EUROPA MEDICOPHYSICA
----------------------- Page 44----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN Chapter 14. Oncolo Chapter 15. Reinte dis 1) A general id agencies in the di Community: a) Health In b) Hospitali c) Hospitali d) Domicilia etc. e) Assistanc
3) Assessment and treatment. of ano-rectal sphincgical rehabilitation ter pathology and overactive bladder and bowel 4) Sexual consequences of neurological dysfunction gration and maintenance of including pregnancy in spinal paralysis. abled and elderly people at home. Chapter 13. Physical and Rehabilitation Medicine ea on the health and medico social in elderly people fferent countries of the European 1) The process of ageing in different systems: surance Systems Social Security. a) Central and peripheral nervous system: neusation, private and public. ronal ageing, influences on mood, cerebral functionsation at home. ing and feedback mechanisms. ry care, health workers, home helps, b) Musculoskeletal system c) Cardiovascular and respiratory system. e and surveillance by telephone and 2) An appreciation of the fundamentals of geriatric ation methods. pathology: epidemiology, pathology, evolution of the general organisation of rehaageing and therapy. ace and role of the specialist in phys3) Indications for geriatric patients for staying at ation medicine within these struc-
other telecommunic 2) Knowledge of bilitation, the pl ical and rehabilit
home or in an institutional placement.
tures.
alists
APPENDIX VI. Rules for Continuing Medical Education (CME) and Continuing Professional Development (CPD) of PRM Speci vidual during an a 3) Publications 1) i. Journals: 1) ii. Books: 4) Academic act 50 credits). 5) Self-educati 1) i. Personal 1) i. 5 credits 1) i. 3 credits journal. 1) ii. Internet mitted: 1) i. 1 credit son and a
Every Board certified specialist in PRM is expectccredited scientific event. ed to collect annually 50 credits. This is not mandain: tory, but specialists should have a total of 250 cred10 credits to each author. its over 5 years. Revalidation of Board certified PRM 10 credits for each chapter. specialists takes place ten years after certification and is based on CME credits. These may be: ivities (e.g. Ph.D. - copy submitted 1) Participation in scientific events: 1) 1 credit per academic hour attended (not more
on:
than 6 credits per day), or subscriber to journals of PRM: 1) 3 credits per half-day event, or / indexed journal, up to 2 journals. 1) 6 credits per full day event. , if subscriber to one non-indexed 2) Presenting scientific work (Giving lectures/presenting posters): PRM teaching lessons: if proof sub1) 5 credits, for each lecture, given by an individual during an accredited scientific event, /lesson or the credits provided for the les1) 3 credits, for each poster presented by an indire written at the electronic program. 330 December 2006
EUROPA MEDICOPHYSICA
----------------------- Page 45----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN UEMS-PRM-Section National Delegates Austria Prof. V Fialka-Moser Dr. A Vetra Prof M Quittan Dr. A. Vetra Prof. Th Lejeune Dr. A Juocevicius Prof. G Vanderstraeten Dr. G Grenod (President, European Board) Dr. N Christodoulou Prof. H Stam Dr K Sekelj-Kauzlari Latvia
Belgium
Lithuania Luxembourg Netherlands
Cyprus Croatia
Dr. M Terburg Czech Republic (Treasurer) Dr. J Vacek Dr. H Snekkevik Dr. J Votava Prof. J Kiwerski Dr. L Krohn Dr. P Cantista Dr. E Kyllnen Dr. F Parada- Pereira Dr. T Pohjolainen Prof. M Berteanu Prof. A Delarque (Secretary) Prof. G Devecerski Dr. G de Korvin Dr. A Skm (Deputy Secretary) Prof. C Gutenbrunner Dr. H Damjan (President, Professional Practice Committee) Prof. G Stucki Prof C Marincek Prof. X Michail Prof. LP Rodriguez Dr. K Stathi Prof. S Muoz Dr. M Tzara Prof J Borg Prof. T Bender Prof. B Sjlund (President, Clinical Affairs Committee) Prof. L Kullman Dr. R Frischknecht Dr. G Einarsson Dr. D Uebelhart Dr. M Delargy Prof. F Diner Dr. A McNamara Prof. Z Haselik Prof. F Franchignoni Prof. DL McLellan Prof. A Giustini Dr. AB Ward (President) 331 Switzerland Norway Poland Portugal
Denmark Finland
Romania Serbia and Monteneg Slovakia Slovenia
France ro
Germany
Greece
Spain
Sweden
Hungary
Iceland Ireland
Turkey
Italy
United Kingdom
Vol. 42 - No. 4
EUROPA MEDICOPHYSICA
----------------------- Page 46----------------------E IN EUROPE WHITE BOOK ON PHYSICAL AND REHABILITATION MEDICIN Academicians, Acadmie Europenne de Mdecine de Radaptation Prof M A Chamberlain (UK) (President) Prof
J Gatcheva (BUL) Prof. H Alaranta (FI) C Gobelet (CH) Prof JM Andr (F) eilporn (B) Prof M Barat (F) G Lankhorst (NL) Prof A Bardot (F) DL McLellan (UK) Prof M P Barnes (UK) McNamara (IRE) Prof C Bertolini (I) R Maigne (F) Prof A Chantraine (CH) C Marincek (SLO) Prof A Conradi (D) G Megna (I) Prof A Delarque (F) . X Michail (GR) Prof. H Delbrck (D) elze (D) Prof JP Didier (F) LP Rodriguez Rodriguez (E) Prof J Ekholm (S) B Sjlund (S) Mr W El Masry (UK) H Stam (NL) Prof M Eyssette (F) G Stucki (D) Prof. V Fialka Moser (A) A Tonazzi (I) Prof F Franchignoni (I) . G Vanderstraeten (B) Prof J Garcia-Alsina (E) B Ward (UK) Dr G Zck (CH) For the European Society of Physical and Rehabilitation Medicine Prof. H Stam (NL) (President) raeten (B) (Vice President) Prof. A Giustini (I) (Vice President) ) (Vice President) Prof. X Michail (Gr) (Vice President) T) (Secretary) 332 December 2006
Prof Dr A H Prof Prof Dr A Prof Prof Prof Prof Dr F O Prof Prof Prof Prof Prof Prof Dr A
Prof. G Vanderst Dr. A B Ward (UK Prof. Z Haselik ( EUROPA MEDICOPHYSICA
También podría gustarte
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Standard 7 CC Workbook1Documento25 páginasStandard 7 CC Workbook1Donna Mar25% (4)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- 9 BoxDocumento10 páginas9 BoxclaudiuoctAún no hay calificaciones
- Act 580 Counsellors Act 1998Documento37 páginasAct 580 Counsellors Act 1998Adam Haida & CoAún no hay calificaciones
- Non-Violent Crisis Intervention - Suicidal ThreatsDocumento9 páginasNon-Violent Crisis Intervention - Suicidal Threatspromoth007100% (2)
- MAMBA Vs LARADocumento2 páginasMAMBA Vs LARATherese MamaoagAún no hay calificaciones
- Minutes of The DefenseDocumento3 páginasMinutes of The DefenseGladys Sarah CostillasAún no hay calificaciones
- Red TaoDocumento214 páginasRed TaoMosi Ngozi (fka) james harris100% (2)
- Alternative Remedy IIDocumento6 páginasAlternative Remedy IINimisha DaharwalAún no hay calificaciones
- Digest - Cotiangco V Biliran Reorg 2Documento1 páginaDigest - Cotiangco V Biliran Reorg 2roncesAún no hay calificaciones
- The Social Psychology of False ConfessionsDocumento4 páginasThe Social Psychology of False ConfessionsIoana VoinaAún no hay calificaciones
- Beg Borrow and Steal Ethics Case StudyDocumento7 páginasBeg Borrow and Steal Ethics Case Studyapi-130253315Aún no hay calificaciones
- Asian Resurfacing of Road Agency Pvt. Ltd. and Ors. vs. Central Bureau of Investigation (28.03.2018)Documento30 páginasAsian Resurfacing of Road Agency Pvt. Ltd. and Ors. vs. Central Bureau of Investigation (28.03.2018)Rishabh Nigam100% (1)
- Bengals Lease Memorandum of UnderstandingDocumento5 páginasBengals Lease Memorandum of UnderstandingCincinnatiEnquirerAún no hay calificaciones
- 2 MPU2243 Culture and Human CommunicationDocumento11 páginas2 MPU2243 Culture and Human Communicationnurul shuhadaAún no hay calificaciones
- Frederic Chopin and George Sand RomanticizedDocumento11 páginasFrederic Chopin and George Sand RomanticizedAleksej ČibisovAún no hay calificaciones
- Rick Warren - Making Hard Changes in MeDocumento2 páginasRick Warren - Making Hard Changes in MeRicardo DelboniAún no hay calificaciones
- Role of Youth in SocietyDocumento9 páginasRole of Youth in SocietyDanna Krysta Gem Laureano100% (1)
- Quality Management Case Study Chapter 3 "The Case of The Missing Reservation"Documento3 páginasQuality Management Case Study Chapter 3 "The Case of The Missing Reservation"Quan TrinhAún no hay calificaciones
- Barangay Resolution SampleDocumento2 páginasBarangay Resolution SampleReese OguisAún no hay calificaciones
- PT 2 English ClassVIIIDocumento4 páginasPT 2 English ClassVIIIMyth White WolfAún no hay calificaciones
- Lat Naaaaaaaa!!!!!!Documento16 páginasLat Naaaaaaaa!!!!!!Niejay Arcullo LlagasAún no hay calificaciones
- Personal and Social Leadership CompetenciesDocumento2 páginasPersonal and Social Leadership CompetenciesTemur Sharopov100% (2)
- Evidence Piece 2Documento4 páginasEvidence Piece 2api-312051398Aún no hay calificaciones
- 07 - DHL Philippines Corp. v. Buklod NG Manggagawa NG DHL Philippines Corp., - BacinaDocumento2 páginas07 - DHL Philippines Corp. v. Buklod NG Manggagawa NG DHL Philippines Corp., - BacinaChaAún no hay calificaciones
- Kilayko V TengcoDocumento3 páginasKilayko V TengcoBeeya Echauz100% (2)
- Child Pornography-IJSRDocumento4 páginasChild Pornography-IJSRparnitaAún no hay calificaciones
- 4 - de La Torre v. CA, GR No. 160088 and GR No. 160565Documento1 página4 - de La Torre v. CA, GR No. 160088 and GR No. 160565Juvial Guevarra BostonAún no hay calificaciones
- Southwest Engineering Co. v. United StatesDocumento2 páginasSouthwest Engineering Co. v. United StatescrlstinaaaAún no hay calificaciones
- Proposal Submitted To HDFC ERGODocumento7 páginasProposal Submitted To HDFC ERGOTathagat JhaAún no hay calificaciones
- Lifespan Development: Why Is The Study of Lifespan Development Important?Documento23 páginasLifespan Development: Why Is The Study of Lifespan Development Important?mehnaazAún no hay calificaciones