Documentos de Académico
Documentos de Profesional
Documentos de Cultura
USDOJ ADA Oregon Investigation Matrix
Cargado por
Statesman Journal0 calificaciones0% encontró este documento útil (0 votos)
348 vistas12 páginasOregon Behavioral Health System Development and Program Outcome Measures BRAFT identifies statewide and regional barriers to development of comprehensive behavioral health crisis system. System development measures include: ___# of emergency room visits for adults with serious and persistent mental illness who are in crisis, inpatient hospital admits for adults with SPMI that are the result of a behavioral health crisis. Program outcomes measures include: 1) Ability to effectively manage behavioral health crises in a community setting; 2) Ability to provide appropriate access to behavioral health
Descripción original:
Derechos de autor
© Attribution Non-Commercial (BY-NC)
Formatos disponibles
PDF, TXT o lea en línea desde Scribd
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoOregon Behavioral Health System Development and Program Outcome Measures BRAFT identifies statewide and regional barriers to development of comprehensive behavioral health crisis system. System development measures include: ___# of emergency room visits for adults with serious and persistent mental illness who are in crisis, inpatient hospital admits for adults with SPMI that are the result of a behavioral health crisis. Program outcomes measures include: 1) Ability to effectively manage behavioral health crises in a community setting; 2) Ability to provide appropriate access to behavioral health
Copyright:
Attribution Non-Commercial (BY-NC)
Formatos disponibles
Descargue como PDF, TXT o lea en línea desde Scribd
0 calificaciones0% encontró este documento útil (0 votos)
348 vistas12 páginasUSDOJ ADA Oregon Investigation Matrix
Cargado por
Statesman JournalOregon Behavioral Health System Development and Program Outcome Measures BRAFT identifies statewide and regional barriers to development of comprehensive behavioral health crisis system. System development measures include: ___# of emergency room visits for adults with serious and persistent mental illness who are in crisis, inpatient hospital admits for adults with SPMI that are the result of a behavioral health crisis. Program outcomes measures include: 1) Ability to effectively manage behavioral health crises in a community setting; 2) Ability to provide appropriate access to behavioral health
Copyright:
Attribution Non-Commercial (BY-NC)
Formatos disponibles
Descargue como PDF, TXT o lea en línea desde Scribd
Está en la página 1de 12
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Population: Adults with serious and persistent mental illness (SPMI) with a special emphasis on those eligible to receive Title
XIX services.
Targeted Areas
System Development Measures
Program Outcome Measures
I. Behavioral
Health Crisis
System
A. Identification of statewide and regional barriers to development of
comprehensive behavioral health crisis system and strategies that will
be implemented to achieve identified program outcome performance
standards/goals.
1. Ability to effectively manage behavioral health crises in a
community setting as measured by:
___# of emergency room visits for adults with SPMI who
are in crisis
___# of inpatient hospital admits for adults with SPMI that
are the result of a behavioral health crisis
___# of adults with SPMI whose incarceration or jail time is
related to a behavioral health crisis
__# of individuals diverted from the criminal justice system
by law enforcement referral or linkage to the behavioral
health crisis system
___# of adults with SPMI whose homelessness or loss of
housing is related to a behavioral health crisis(es)
Note: Last three bullets are a system issue, for subsequent
discussion/
2. Ability to provide appropriate access to behavioral health
crisis services as measured by:
Behavioral health crisis hotline call standards, e.g., 24/7
coverage, response rates of 5 rings/30 seconds, abandonment
rate
CCOs meeting geographical access standards for each of the
following behavioral health crisis services: mobile crisis,
crisis walk-in clinic visit, crisis apartment/respite, and short-
term crisis stabilization, frontier alternatives
___% of mobile crisis teams that meet the timeliness of
response standard
___% of walk-in/drop-off crisis centers that meet the wait
time standard Note: Last three bullets for 2
nd
or 3
rd
year.
B.
1. ___# of Coordinated Care Organizations (CCOs) that operate a
single 24/7 behavioral health crisis hotline.
2. ___# of CCOs that teach law enforcement Crisis Intervention
Training and how to access the behavioral health crisis system
3. ___# of providers offering each of the following behavioral health
crisis services:
Mobile crisis teams
Walk-in/drop-off crisis centers
Crisis apartments/respite
Short-term crisis stabilization units
Agreed-upon alternatives to above crisis services in frontier area
C.
___% of service dollars for adults with SPMI that are used for each
of the following behavioral health crisis services:
Crisis hotline calls
Mobile crisis team
Walk-in/drop-off crisis centers
Crisis apartments/respite
)RUPDWWHG Superscript
)RUPDWWHG Superscript
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Areas
System Development Measures
Program Outcome Measures
Short-term crisis stabilization days/visits
Agreed-upon alternatives to above crisis services in frontier area
___# of service units per month per adult with SPMI who
receive each of the following behavioral health crisis
services: crisis hotline, mobile crisis, walk-in/drop-off crisis
center visit, crisis apartments/respite, short-term crisis
stabilization, and frontier alternatives.
___% of adults with SPMI (and or their family) that report
positively about the system response to a behavioral health
crisis event
3. ___% of adults with SPMI who have had a behavioral health
crisis and who experienced an improved level of functioning XX
months after the crisis event.
4. For those adults with SPMI who have a behavioral health
crisis event:
___% of adults who had a crisis intervention plan
___% of crisis intervention plans that were followed during
the crisis
___% of crisis intervention plans that were effective in
preventing an inpatient admission and/or emergency room
visit and/or jail admission.
D.
1. ___# of service units per adult with SPMI per month for each of
the following behavioral health crisis services:
Crisis hotline calls
Mobile crisis team
Walk-in/drop-off crisis center visits
Crisis apartment/respite visits
Short-term crisis stabilization days/visits
Agreed-upon alternatives to above crisis services in frontier area
2. ___# of adults with SPMI who received each of the following
types of behavioral health crisis services:
Crisis hotline calls
Mobile crisis team
Walk-in/drop-off crisis center visits
Crisis apartment/respite visits
Short-term crisis stabilization days/visits
Agreed-upon alternatives to above crisis services in frontier area
E.
___% of the care plans for adults with SPMI that include a current
crisis intervention plan.
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Areas
System Development Measures
Program Outcome Measures
II. Independent
Supported Housing
A. Identification of statewide and regional barriers to development of
independent supported housing for adults with SPMI and strategies
that will be implemented to achieve identified program outcome
performance standards/goals.
1. ___% of adults with SPMI who have been living (e.g., own
home, supported housing) in the community in a safe, stable
living environment for XX days. Note: Not first year.
2. ___# of adults with SPMI who reside in each of the following
settings:
Supported housing or own home
State Hospital
Adult foster care
Residential treatment home
Residential treatment facility
Secured residential treatment facility
3. The average length of stay for adults with SPMI in each of the
following settings:
An inpatient hospital setting
A State Hospital
Adult foster home
Residential treatment home
Residential treatment facility
Secure residential treatment facility
4. ___% of adults with SPMI who are living in a setting that is
at the appropriate level of care.
B.___# of available independent supported housing units for adults
with SPMI.
C. ___# of adults with SPMI who:
Reside in each of the following types of settings: independent
supported housing, own home, State hospital or a residential
care
1
setting
Moved from the State Hospital, inpatient hospital or residential
care setting into an independent supported housing setting
Moved from homeless shelters or jails into an independent
supported housing setting
Note: First bullet is for CCOs, second is for state to measure
D.1. ___% of service dollars for adults with SPMI living in supported
independent housing that are used for each of the following services:
Non-Title XIX supported housing services (e.g., rental subsidy,
move-in costs)
Community-based behavioral health services (e.g., ACT teams,
peer support, supported employment)
2. ___% of service dollars for adults with SPMI that are used for care
provided in:
1
Residential care refers to the four types of residential care in Oregon: adult foster homes, residential treatment homes, residential treatment facilities and secure
residential treatment facilities. The information for the measure would be provided for each type of residential care.
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Areas
System Development Measures
Program Outcome Measures
State Hospital
Each of the four types of residential care settings
___% of adults with SPMI who are homeless.
5.
___% of adults with SPMI reporting positively about:
Their living environment
Availability of independent supported housing and housing
support services (e.g., rental subsidy, move-in costs)
Note: OHA to measure, not CCOs.
E. ___# of services units per adult with SPMI per month for each of
the following:
Non-Title XIX supported housing services (e.g., rental subsidy,
move-in costs)
Community-based behavioral health services (e.g., ACT teams,
peer support, supported employment)
Services provided in each of the four types of residential care
settings
Services provided in the State Hospital
III.Community-
Based Behavioral
Health Services
A. Identification of statewide and regional barriers to development of
comprehensive community-based behavioral health services for
adults with SPMI and strategies that will be implemented to achieve
identified program outcome goals/benchmarks
1. ___% of adults with SPMI who:
Are employed
Have abstained from drug/alcohol use
Had a criminal justice event (jail, arrest, other interaction
with law enforcement, etc.)
Had a homeless event
Note: OHA to survey, not CCOs.
2. ___% of adults with SPMI who report that their se functional
level improved.
3. ___% of adults with SPMI reporting positively about each of
the following:
Outcomes (i.e., perception of care)
Improved level of functioning
B. ___# of providers offering each of the following community-
based behavioral health services:
Assertive community treatment
Crisis apartment/respite care
Intensive case management (out of office)
Peer support
Supported employment
Psycho-education and living skills training
Crisis hotline calls
Note: Above will be measured ifcovered by Medicaid.
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Areas
System Development Measures
Program Outcome Measures
Mobile crisis team
Walk-in/drop-off crisis center visits
Short-term crisis stabilization days/visits
Agreed-upon alternatives to above crisis services in frontier area
Service quality and appropriateness.
Social connectedness
___% of adults with SPMI who filed complaints related to:
Quality of care (substantiated and unsubstantiated)
Access and availability to services
Effectiveness/appropriateness of services
Note: OHA to gather complaint data for all receiving MH
services
5. Ability to provide appropriate access to community-based
behavioral health services as measured by:
CCOs meeting geographical access standards for each
community-based behavioral health service
___% of newly enrolled adults with SPMI who receive their
first routine services within XX days of their initial
assessment
___% of community-based behavioral health providers who
met the appointment availability standards for emergency,
urgent and routine care
___% of community-based behavioral health providers who
met the wait time standard
___% of adults with SPMI who reported positively about
their ability to access community-based behavioral health
services
___# of service units per month per adult with SPMI who
receive each of the community-based behavioral health
services.
For those with SPMI, the lengthy of time from enrollment
until first visit with provider of health services?
C. ___% of service dollars for adults with SPMI that are used for
each of the following community-based behavioral health services
2
:
Assertive community treatment
Crisis apartment/respite care
Intensive case management (out of office)
Peer support
Supported employment
Psycho-education and living skills training
Non-Title XIX supported housing services
Crisis hotline calls
Mobile crisis team
Walk-in/drop-off crisis center visits
Short-term crisis stabilization days/visits
Agreed-upon alternatives to above crisis services in frontier area
D. ___# of service units per adult with SPMI per month for each of
the following community-based behavioral health services:
Assertive community treatment
Crisis apartment/respite care
2
The list of community-behavioral health services may need to be modified once a specific description of the covered behavioral health services for
adults with SPMI is developed.
)RUPDWWHG Space After: 0 pt, Line spacing:
single, Bulleted + Level: 1 + Aligned at: 0" +
!ndent at: 0.2S"
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Areas
System Development Measures
Program Outcome Measures
Intensive case management (out of office)
Peer support
Supported employment
Psycho-education and living skills training
Non-Title XIX supported housing services
Crisis hotline calls
Mobile crisis team
Walk-in/drop-off crisis center visits
Short-term crisis stabilization days/visits
Agreed-upon alternatives to above crisis services in frontier area
2. ___# of adults with SPMI who received each of the following
community-based behavioral health services:
Assertive community treatment
Crisis apartment/respite care
Intensive case management (out of office)
Peer support
Supported employment
Psycho-education and living skills training
Non-Title XIX supported housing services
Crisis hotline calls
Mobile crisis team
Walk-in/drop-off crisis center visits
Short-term crisis stabilization days/visits
Agreed-upon alternatives to above crisis services in frontier area
Note: For those receiving Medicaid servicescies
___% of those with SPMI who receive routine health care
visists after enrollment?
6. ___# of adults with SPM residing in each of the following
settings:
Own home/supported housing
A State Hospital
Adult foster home
Residential treatment home
Residential treatment facility
Secure residential treatment facility
7. The average length of stay, admission and readmission rate
for adults with SPMI in each of the following settings:
An inpatient hospital setting
A State Hospital
Adult foster home
Residential treatment home
Residential treatment facility
Secure residential treatment facility
8. Coordination of care between physical health and behavioral
health providers is demonstrated by:
___% of behavioral health providers that communicate the
outcomes of a referral and/or service plan to the adult with
SPMIs primary care provider (PCP)
___% of behavioral health providers that have ongoing
communicate with the PCP for the adult with SPMI
___% of adults with SPMI who have had a PCP visit within
the past 12 months
E. ___% of adults with SPMI that have a current care plan (e.g., has
been reviewed and updated with the past XX months).
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Areas
System Development Measures
Program Outcome Measures
F. ___% of adults with SPMI that have had a PCP visit within the
past 12 months.
IV.Screening,
Assessment and
Early Intervention
Services
A. Identification of statewide and regional barriers to development of
screening, assessment and early intervention services and strategies
that will be implemented to achieve identified program outcome
performance standards/goals.
Ability to provide effective early intervention services as
reflected by:
___# of emergency room visits for adults with SPMI
___# of inpatient hospital admits for adults with SPMI
___# of 30 and 180 day readmission rates for inpatient
psychiatric care for adults with SPMI
___# of adults with SPMI that are referred/moved to the
State Hospital and/or one of the four residential care settings
___% of adults with SPMI with a criminal justice event (jail,
arrest, other interaction with law enforcement, etc.)
___% of adults with SPMI with a homeless event
Note: Last two are longer term issues.
Ability to provide appropriate access to early intervention
services as measured by:
CCOs meeting geographical access standards for each early
intervention health service
___% of newly enrolled adults with SPMI who receive their
first routine services within XX days of their initial
assessment
___% of providers who met the appointment availability
standards for early intervention services
___% of providers who met the wait time standard
___% of adults with SPMI who reported positively about
their ability to access assessment and early intervention
services
____# of service units per month per adult with SPMI who
B.
1. ___% of adults with SPMI that have current bio-psycho-social
assessments and a care plan that has been reviewed and updated
within the past XX months.
2.___% of adults with SPMI who have had a level of care assessment
during the past 12 months.
3. ___# of behavioral health screens (e.g., depression, substance
abuse) conducted by PCPs during initial health screens of newly
enrolled adults (all adults enrolled in a CCO not just adults with
SPMI).
Note: CCOs to baseline category B in second year.
C. ___# of providers offering each of the following early intervention
services:
Assessment (initial and review)
EASA program
Intensive in-home services/Assertive Community Treatment
Intensive case management
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Areas
System Development Measures
Program Outcome Measures
D. ___% of service dollars for adults with SPMI that are used for
each of the following early intervention services:
Assessment (initial and review)
EASA program
Intensive in-home services/Assertive Community Treatment
Intensive case management
receive each of the assessment and early intervention
services.
For those with SPMI, the length of time from enrollment
until first visit with provider of health services?
___% of those with SPMI who receive routine health care
visists after enrollment?
3. ___% of adults with SPMI whose report that their functional
level improved.
4. ___% of adults with SPMI reporting positively about each of
the following:
Satisfaction with the screening and assessment process
(including participation in the service planning process)
Note: Above bullet is longer term issue.
Outcomes (i.e., perception of care)
Improved level of functioning
Service quality and appropriateness
E.
1. ___# of service units per adult with SPMI per month for each of
the following early intervention services:
Assessment (initial and review)
EASA program
Intensive in-home services/Assertive Community Treatment
Intensive case management
2. ___# of adults with SPMI who received each of the following
assessment and early intervention services:
Assessment (initial and review)
EASA program
Intensive in-home services/Assertive Community Treatment
Intensive case management
3. ___% of adults with SPMI who had a follow-up after
hospitalization within 7 days and within 23 days.
)RUPDWWHG Font: 11 pt
)RUPDWWHG Normal, Space After: 0 pt, Line
spacing: single, No bullets or numbering
)RUPDWWHG Not Highlight
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Areas
System Development Measures
Program Outcome Measures
V. Quality
Assessment and
Process
Improvement
(QAPI) Program
A. Conduct assessment of current Quality Assessment and
Performance Improvement (QAPI) program and develop a plan for
establishment of a QAPI program that integrates behavioral health
and physical health at the State and individual CCO level. For the
CCOs this includes development of contractual requirements related
to QAPI.
1. New QAPI program is successfully implemented at the State
and each CCO establishes a QAPI program that meets
contractual requirements.
2. QAPI program structure at the State and CCO level is able to
demonstrate the operation of an effective system for continuous
quality improvement (identification of areas for improvement,
implementation of interventions, and improved outcomes).
3.The statewide comprehensive data system:
Includes accurate and timely encounter/claims/and client
demographic/clinical data for adults with SPMI.
Generates key management reports, including dashboards
with program outcome scores (statewide and at individual
CCO level).
Note: Timely and clinical data need to be defined.
4.The individual CCOs have methods data systems that are able
to
Identify adults with SPMI who are high-risk and would
benefit from intensive services. such as intensive case
management, ACT etc.
Generate key QAPI-related management reports, including
those that are submitted to the State
5. State meets agreed-upon outcome benchmarks and/or
implements interventions that result in improved outcome
values. Statewide PIPs successfully achieve outcome goal(s)
and demonstrate the ability to sustain the positive outcomes.
B. Establishment of integrated QAPI structure (committees, staff) at
State and individual CCO that includes expertise in the delivery of
care to adults with SPMI.
C. Development and implementation of comprehensive data system
(data warehouse) that allows for real time analysis of
encounter/claims and client demographic/clinical data and
monitoring of care delivered to adults with SPMI at level of
individual client, individual provider, individual CCO and overall
system of care.
D. Development of management reports and dashboards that allow
for monitoring of system performance for adults with SPMI.
E. Identification of statewide Performance Improvement Projects
(PIPs) that seeks improvement in an one of the identified areas of
poor performance in the behavioral health system for adults with
SPMI, one of which is behavioral health. .
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
Targeted Areas
System Development Measures
Program Outcome Measures
VI.Maximization of
Title XIX
Funds
A. Identification of statewide and regional barriers to
maximizing use of Title XIX funds and strategies that will be
implemented to achieve identified program outcome performance
standards/goals. This includes examining:
The Supplemental Security Income (SSI) and Title XIX
eligibility process for adults with SPMI
The types of funding (e.g., Title XIX, non-Title XIX) that are
used to pay for specific types of behavioral health services
The Title XIX status and qualifications of providers offering
behavioral health services to adults with SPMI
1. ___% of adults with SPMI in the Oregon behavioral health
system who:
Have been determined Title XIX eligible and are enrolled in
the States Medicaid program
Have been determined SSI eligible
Are eligible for Title XIX but are not enrolled in the States
Medicaid program
Have been denied Title XIX eligibility due to non-
completion of the application
2. ___% of Title XIX behavioral health services that are
provided to Title XIX adults with SPMI that that are paid for
with:
Title XIX funds
Non-Title XIX funds
3. ___% of behavioral health service dollars for Title XIX adults
with SPMI that are paid for with Title XIX funds.
4.___% of behavioral health providers/practitioners who are
qualified Title XIX providers and are able to receive Title XIX
dollars for the services they provide.
Notes:
1. Except if indicated the system development and program outcome measures will be calculated:
For the adult population with SPMI as a whole as well as for the Title XIX and non-Title XIX adult population with SPMI
)RUPDWWHG !ndent: Left: 0.11", First line:
0", Space After: 0 pt, Line spacing: single
Oregon Behavioral Health System Development and Program Outcome Measures
BRAFT Confiuential not foi uistiibution Page
On a statewide basis and for each individual CCO (or the state-contracted entity responsible for delivering the behavioral health
services to adults with SPMI).
Using a comprehensive behavioral health data set that includes data from the mental health and substance abuse systems.
2. For each of the system development measures, a baseline along with two years of annual interim benchmarks will need to be
established.
3. For each of the program outcome measures, a baseline along with a program outcome goal and an annual minimum performance
standard will need to be established.
También podría gustarte
- Complaint Summary Memo To Superintendent Re 8-9 BD Meeting - CB 9-14-22Documento4 páginasComplaint Summary Memo To Superintendent Re 8-9 BD Meeting - CB 9-14-22Statesman JournalAún no hay calificaciones
- Letter To Judge Hernandez From Rural Oregon LawmakersDocumento4 páginasLetter To Judge Hernandez From Rural Oregon LawmakersStatesman JournalAún no hay calificaciones
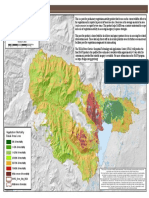
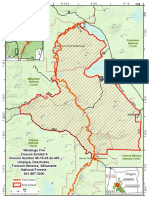
- Cedar Creek Fire Soil Burn SeverityDocumento1 páginaCedar Creek Fire Soil Burn SeverityStatesman JournalAún no hay calificaciones
- Cedar Creek Vegitation Burn SeverityDocumento1 páginaCedar Creek Vegitation Burn SeverityStatesman JournalAún no hay calificaciones
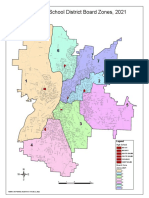
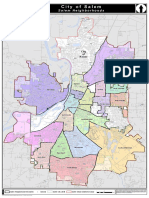
- School Board Zones Map 2021Documento1 páginaSchool Board Zones Map 2021Statesman JournalAún no hay calificaciones
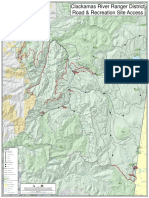
- Roads and Trails of Cascade HeadDocumento1 páginaRoads and Trails of Cascade HeadStatesman JournalAún no hay calificaciones
- Social-Emotional & Behavioral Health Supports: Timeline Additional StaffDocumento1 páginaSocial-Emotional & Behavioral Health Supports: Timeline Additional StaffStatesman JournalAún no hay calificaciones
- Mount Hood National Forest Map of Closed and Open RoadsDocumento1 páginaMount Hood National Forest Map of Closed and Open RoadsStatesman JournalAún no hay calificaciones
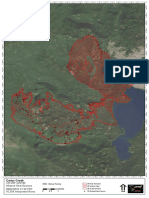
- Cedar Creek Fire Sept. 3Documento1 páginaCedar Creek Fire Sept. 3Statesman JournalAún no hay calificaciones
- Windigo Fire ClosureDocumento1 páginaWindigo Fire ClosureStatesman JournalAún no hay calificaciones
- Cedar Creek Fire Aug. 16Documento1 páginaCedar Creek Fire Aug. 16Statesman JournalAún no hay calificaciones
- All Neighborhoods 22X34Documento1 páginaAll Neighborhoods 22X34Statesman JournalAún no hay calificaciones
- Matthieu Lake Map and CampsitesDocumento1 páginaMatthieu Lake Map and CampsitesStatesman JournalAún no hay calificaciones
- Revised Closure of The Beachie/Lionshead FiresDocumento4 páginasRevised Closure of The Beachie/Lionshead FiresStatesman JournalAún no hay calificaciones
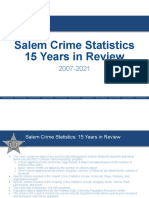
- Salem Police Intelligence Support Unit 15-Year Crime TrendsDocumento11 páginasSalem Police Intelligence Support Unit 15-Year Crime TrendsStatesman JournalAún no hay calificaciones
- Salem Police 15-Year Crime Trends 2007 - 2021Documento10 páginasSalem Police 15-Year Crime Trends 2007 - 2021Statesman JournalAún no hay calificaciones
- LGBTQ Proclaimation 2022Documento1 páginaLGBTQ Proclaimation 2022Statesman JournalAún no hay calificaciones
- Proclamation Parent & Guardian Engagement in Education 1-11-22 Final, SignedDocumento1 páginaProclamation Parent & Guardian Engagement in Education 1-11-22 Final, SignedStatesman JournalAún no hay calificaciones
- WSD Retention Campaign Resolution - 2022Documento1 páginaWSD Retention Campaign Resolution - 2022Statesman JournalAún no hay calificaciones
- BG 7-Governing StyleDocumento2 páginasBG 7-Governing StyleStatesman JournalAún no hay calificaciones
- Failed Tax Abatement ProposalDocumento8 páginasFailed Tax Abatement ProposalStatesman JournalAún no hay calificaciones
- Salem-Keizer Discipline Data Dec. 2021Documento13 páginasSalem-Keizer Discipline Data Dec. 2021Statesman JournalAún no hay calificaciones
- All Neighborhoods 22X34Documento1 páginaAll Neighborhoods 22X34Statesman JournalAún no hay calificaciones
- Salem Police 15-Year Crime Trends 2007 - 2015Documento10 páginasSalem Police 15-Year Crime Trends 2007 - 2015Statesman JournalAún no hay calificaciones
- Salem-Keizer Parent and Guardian Engagement in Education Month ProclamationDocumento1 páginaSalem-Keizer Parent and Guardian Engagement in Education Month ProclamationStatesman JournalAún no hay calificaciones
- Zone Alternates 2Documento2 páginasZone Alternates 2Statesman JournalAún no hay calificaciones
- Oregon Annual Report Card 2020-21Documento71 páginasOregon Annual Report Card 2020-21Statesman JournalAún no hay calificaciones
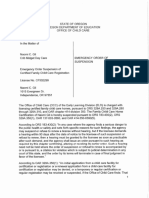
- Crib Midget Day Care Emergency Order of SuspensionDocumento6 páginasCrib Midget Day Care Emergency Order of SuspensionStatesman JournalAún no hay calificaciones
- SIA Report 2022 - 21Documento10 páginasSIA Report 2022 - 21Statesman JournalAún no hay calificaciones
- SB Presentation SIA 2020-21 Annual Report 11-9-21Documento11 páginasSB Presentation SIA 2020-21 Annual Report 11-9-21Statesman JournalAún no hay calificaciones
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (120)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2101)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Entry Form: Hospital Best Practices in Infection Prevention and Control Awards Year ViDocumento1 páginaEntry Form: Hospital Best Practices in Infection Prevention and Control Awards Year ViPeepsAún no hay calificaciones
- DAFTAR PUSTAKA Gadar 1Documento2 páginasDAFTAR PUSTAKA Gadar 1Rini WahyuniAún no hay calificaciones
- Preoperative Education: Preoperative Preparation Allows Patients ToDocumento6 páginasPreoperative Education: Preoperative Preparation Allows Patients ToLorenn AdarnaAún no hay calificaciones
- Capstone InterviewDocumento2 páginasCapstone Interviewapi-455342149Aún no hay calificaciones
- Minutes of The Meeting atDocumento3 páginasMinutes of The Meeting atNgomende DylanAún no hay calificaciones
- Holland & Knight Lobbying ContractDocumento44 páginasHolland & Knight Lobbying ContractmilesmoffeitAún no hay calificaciones
- Inc Tnai IcnDocumento7 páginasInc Tnai IcnDeena MelvinAún no hay calificaciones
- Kel 5 Roleplay Diabetes MellitusDocumento4 páginasKel 5 Roleplay Diabetes MellitusDesma LindaAún no hay calificaciones
- Pre-Analytical Errors - Make A Difference 2011Documento16 páginasPre-Analytical Errors - Make A Difference 2011YeeWei TanAún no hay calificaciones
- Open EMRDocumento38 páginasOpen EMRSuhail BhatiaAún no hay calificaciones
- Health Sector of Arunanchal PradeshDocumento14 páginasHealth Sector of Arunanchal PradeshJatin ChauhanAún no hay calificaciones
- Nursing Audit Tool PDFDocumento12 páginasNursing Audit Tool PDFjamieAún no hay calificaciones
- Directory of HospitalsDocumento8 páginasDirectory of HospitalsShannen AndradeAún no hay calificaciones
- Multitasking in NursingDocumento6 páginasMultitasking in NursingFlorenciaAbudOyanederAún no hay calificaciones
- Final ResearchDocumento65 páginasFinal ResearchHarbrinder GurmAún no hay calificaciones
- The Citadel Teacher S Notes PDFDocumento5 páginasThe Citadel Teacher S Notes PDFEve100% (2)
- TRAVELBEEDocumento25 páginasTRAVELBEEMrNars92% (12)
- Iffco Tokio List of Network HospitalsDocumento116 páginasIffco Tokio List of Network HospitalswithrjAún no hay calificaciones
- Usmc To&e E-43 NCBDocumento6 páginasUsmc To&e E-43 NCBleon_leeAún no hay calificaciones
- Capstone Clinical JudgmentDocumento8 páginasCapstone Clinical Judgmentapi-455232702Aún no hay calificaciones
- March 21, 2014Documento20 páginasMarch 21, 2014Anonymous KMKk9Msn5Aún no hay calificaciones
- Shock Resident LectureDocumento38 páginasShock Resident Lecturepapermate9293Aún no hay calificaciones
- Umbilical GranulomaDocumento3 páginasUmbilical GranulomaNina KharimaAún no hay calificaciones
- Operation TheatreDocumento22 páginasOperation TheatreAbirami100% (1)
- Mid South Dermatology - General Consent Patient FormDocumento1 páginaMid South Dermatology - General Consent Patient FormjtdermAún no hay calificaciones
- 13th Combined Manipal MangaloreDocumento4 páginas13th Combined Manipal MangalorePankaj VatsaAún no hay calificaciones
- Hospital Teams: Bahasa InggrisDocumento6 páginasHospital Teams: Bahasa InggrisIlhamAún no hay calificaciones
- Solving Math Word Problems: Steps Tips For Success ExampleDocumento3 páginasSolving Math Word Problems: Steps Tips For Success ExampleDhiman NathAún no hay calificaciones
- Sunset EyesDocumento1 páginaSunset EyesBilly Shan LastKagerooboroAún no hay calificaciones
- Emergency MedicineDocumento141 páginasEmergency Medicinenasibdin100% (9)