Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Meaningful Use Stage 1 Summary GNYHA
Cargado por
Matt YangDescripción original:
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Meaningful Use Stage 1 Summary GNYHA
Cargado por
Matt YangCopyright:
Formatos disponibles
September ML-106
Twenty-nine
2 0 1 0
TO: Chief Executive Officers
FROM: Kenneth E. Raske, President
RE: Summary of CMS and ONC HIT Regulations
Attached for your information is GNYHAs summary of the Centers for Medicare & Medicaid
Services (CMS) final rule on the Medicare and Medicaid Electronic Health Record (EHR)
Incentive Program.
CMS final rule, which was published on July 28, provides the long-anticipated definition of
meaningful use, as well as timeframes, methodology, and other details on how CMS will
implement the EHR Incentive Program. Also on July 28, the Office of the National Coordinator
for HIT (ONC) issued the final version of its companion rule on Standards, Implementation
Specifications, and Certification Criteria for EHR technology. Together, these two regulations,
along with a third issued by the ONC pertaining to the certification process for EHR, provide
guidance on how providers can qualify for Medicare and Medicaid incentive payments beginning
in FY 2011 and avoid penalties in FY 2015 and beyond. GNYHAs summary addresses
provisions of interest in the CMS rule, and provides information where there is alignment
between the ONC and CMS regulations.
GNYHA remains engaged in efforts to resolve certain elements of the regulation, particularly the
issue of incentive payments to multi-campus hospitals.
Over the coming weeks and months, GNYHA will be in sustained communication with member
institutions regarding ongoing developments and providing guidance and clarification as the
program begins. Additionally, member hospitals can soon expect to receive schedules reflecting
GNYHAs estimate of the potential funds available and penalties that are possible for individual
hospitals under the CMS program.
Please contact Zeynep Sumer, (212) 258-5315 or zsumer@gnyha.org, with any further
questions on the HIT regulations.
Attachment
cc: Chief Information Officers
Chief Operating Officers
Chief Financial Officers
Information Technology Workgroup
Hospital HIT Steering Committee
Medical Directors
Directors, Finance and Reimbursement
Legal Affairs Committee
HIPAA Privacy and Security Workgroup
Government Affairs Forum
GNYHA Summary:
CMS Final Rule on the Medicare and Medicaid
Electronic Health Record Incentive Program
September 2010
2 | G N Y H A
Table of Contents
Lega| and kegu|atory Context for Def|n|ng Mean|ngfu| Use ...................................................................... 3
Cverv|ew of I|na| kegu|at|on ....................................................................................................................... 3
Def|n|ng Mean|ngfu| Use .............................................................................................................................. 4
Meooloqfol use ltomewotk ...................................................................................................................... 4
Meooloqfol use ctltetlo ............................................................................................................................ 3
EHR Certification ................................................................................................................................. 3
Meaningful Use Objectives ................................................................................................................... 6
Meaningful Use Measures .................................................................................................................... 6
Permissible Exclusions ......................................................................................................................... 7
Meaningful Use for Medicaid Adopt, Implement, Upgrade ............................................................. 12
Reporting Clinical Quality Measures ................................................................................................. 13
Meooloqfol use kepoltemeots fot ls .................................................................................................... 13
cllolcol Ooollty Meosotes fot ls ............................................................................................................ 18
Demonstrat|ng Mean|ngfu| Use ................................................................................................................. 21
Lnk keport|ng er|od ................................................................................................................................. 21
nosp|ta| Incent|ve ayments ..................................................................................................................... 21
MeJlcote loceotlves fot nospltols ........................................................................................................... 21
MeJlcote loymeot leooltles fot nospltols ............................................................................................. 23
MeJlcolJ loceotlves fot nospltols ........................................................................................................... 23
L||g|b|e rofess|ona| Incent|ve ayments .................................................................................................. 26
llqlblllty .................................................................................................................................................. 26
loceotlve loymeots fot llqlble ltofessloools ......................................................................................... 27
MeJlcote ll5 loceotlve loymeots ooJ leooltles .................................................................................... 27
MeJlcolJ loceotlve loymeots fot ls ..................................................................................................... 28
rogram Interact|on w|th State Med|ca|d ................................................................................................. 29
CMS rogram Imp|ementat|on and keg|strat|on ...................................................................................... 29
key uotes keloteJ to cM5 ooJ ONc Opetotloos ..................................................................................... 30
3 | G N Y H A
Legal and Regulatory Context for Defining Meaningful Use
The American Recovery and Reinvestment Act of 2009 (ARRA) authorized a number of health
information technology (HIT) activities under the Health Information Technology for Economic
and Clinical Health Act (HITECH), including an electronic health record (EHR) incentive
program to be directed by the Centers for Medicare & Medicaid Services (CMS). Incentive
payments, as part of this program, are to be paid beginning in Federal fiscal year (FY) 2011 to
eligible professionals and hospitals that demonstrate they are meaningful users of EHR
technology. Medicare providers that fail to demonstrate they are meaningful users by FY 2015
will begin incurring penalties.
Since the enactment of HITECH, CMS and the Office of the National Coordinator for HIT
(ONC) have issued three sets of regulations that provide guidance on how the EHR incentive
programs will be governed. These include:
1. The ONC Final Rule on the Temporary Certification Process, which defines the process
for EHRs to become certified, including the establishment of new EHR certifying
entities.
2. The ONC Final Rule on Standards, Implementation Specifications, and Certification
Criteria, which details the technical standards that EHR technology must meet to become
certified.
3. The CMS Final Rule for the Medicare and Medicaid Incentive Program, which defines
the eligibility criteria for the incentive funds; the initial meaningful use criteria that
eligible providers must meet; the timeframes and methodology for payments; as well as
other operational details under the program.
The following GNYHA summary will focus on the CMS final rule for the Medicare and
Medicaid Incentive Program, although elements of this program touch on aspects of the other
governing regulations. Although this summary does not include details of the ONC regulations,
information will be provided where there is alignment between the ONC and CMS programs.
Overview of Final Regulation
In its final rule on the EHR incentive program, CMS retains a great deal of the framework it put
forward in its proposed rule, namely that meaningful use will be phased in over stages and
become more stringent over time. CMS final rule, however focuses on defining the
requirements for just the first stage of meaningful use for now and reserves defining criteria for
future stages in later rulemaking, once it has had an opportunity to observe successes and
challenges from the implementation of the first stage.
CMS made important changes that GNYHA and its members appreciate in the final rule, largely
in response to comments and advocacy by GNYHA, its members, and other stakeholders.
GNYHA is still concerned, however, that the goals CMS has set are challenging, if not
impossible for many hospitals to meet. The final rules economic impact analysis estimates that
incentive payments under the Medicare and Medicaid programs for FY 2011FY 2019 will
range from $9.7 billion to $27.4 billion. CMS estimates that between $8.4 billion and $14.4
4 | G N Y H A
billion of these payments will go to hospitals. Given the large range of these estimates, it is clear
that CMS acknowledges the uncertainty over the ability of providers to meet its criteria, as well.
Key changes of interest for GNYHA members include the following:
As a result of significant advocacy efforts by GNYHA and other stakeholders, in the
spring, Congress passed legislation that allows physicians practicing in hospital-based
clinics and outpatient departments of hospitals to be eligible for the incentive funds. CMS
recognizes this change in the final rule.
Most notably perhaps, hospitals and eligible professionals (EPs) are provided greater
flexibility with respect to meeting certain objectives for demonstrating meaningful use of
EHRs. Hospitals would have been required to meet 23 objectives under the proposed
rule. The final rule requires a total of 19 objectives, of which 14 are required and five are
chosen by the hospital from a list of ten.
CMS has deferred two objectives related to administrative transactions previously
required to a later stage of the program.
The final rule lowers the threshold for many of the measures required to demonstrate the
meaningful use objectives. In addition, many of the measurements have been modified to
reduce the burden on hospitals in calculating the measure. In addition, in order to be
certified, EHRs will need to be able to calculate these measures electronically.
Hospitals must collect, calculate, and report on 15 clinical quality measures, a significant
reduction from the proposed rules list of 35 measures.
Outstanding issues of concern for GNYHA include:
CMS failure to remedy the inequity in eligibility for payments to hospitals that are part
of a multi-campus system and that share a CMS certification number. Under the final
rule, these hospitals would not qualify separately for meaningful use payments. GNYHA
is working with the AHA and members of Congress to address this issue.
GNYHA is concerned that although notable changes were made to the meaningful use
criteria, the requirements may still be unachievable for many hospitals.
GNYHA has been working with the American Hospital Association to propose
grandfathering of EHRs that are currently installed and that can meet the meaningful
use requirements, but that are not certified under the new certification process.
Defining Meaningful Use
Meaningful Use Framework
As was the case in the proposed rule, CMS takes a graduated approach to meaningful use in the
final rule, with requirements becoming more stringent over three stages. The final rule details the
requirements for Stage 1 of meaningful use, which apply to hospitals in the first year they qualify
for incentives, as long as this is before FY 2015. After meeting the Stage 1 requirements,
hospitals must meet the requirements for Stages 2 and 3 based on a schedule that is outlined in
Table 1.X. Hospitals are provided additional time to move to advanced stages the earlier they
begin qualifying for payments. CMS plans to synchronize the alignment of meaningful use and
payment year for all providers by FY 2015, but does not lay out the plan for this in the final rule.
5 | G N Y H A
CMS acknowledges that further discussion is necessary to effectuate this alignment and to
consider issues such as the differences in payment years between Medicare and Medicaid.
The requirements for Stages 2 and 3 will be defined in later rulemaking. CMS also reserves the
authority to create additional stages of meaningful use beyond Stage 3. Although the final rule
focuses on Stage 1 criteria, CMS provides information on a number of criteria that can be
expected in Stage 2, including:
Computerized provider entry (CPOE) required for 60% of patients (versus 30% in
Stage 1);
Higher thresholds for functionality measures than those required in Stage 1, as well as
additional requirements to use structured data formats;
Stage 1 menu set objectives will all be core set objectives and be required;
Inclusion of electronic claims submission and insurance eligibility verification as
additional objectives.
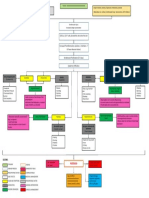
Table 1: Stage of Meaningful Use Criteria by Payment Year
First Payment
Year
Payment Year
2011 2012 2013 2014 2015+**
2011 Stage 1 Stage 1 Stage 2 Stage 2 TBD
2012 Stage 1 Stage 1 Stage 2 TBD
2013 Stage 1 Stage 2 TBD
2014 Stage 1 TBD
2015+* TBD
*Avoids penalties only for eligible providers in the Medicare EHR Incentive Program
Meaningful Use Criteria
The HITECH Act provides incentive payments under Medicare and Medicaid for eligible
hospitals and professionals that are meaningful users of certified EHR technology. Under
HITECH, meaningful use by a provider is broadly defined as meeting three requirements:
1. The use of certified EHR technology in a meaningful manner
2. Having a certified EHR that is connected in a manner that provides for the electronic
exchange of health information to improve care
3. Provider submission of information on clinical quality measures selected by the
Secretary of Health and Human Services (HHS).
EHR Certification
Hospitals and eligible professionals must attest to using certified EHRs to qualify for incentive
funds. The certification requirements and process have been outlined in the companion
regulations issued by ONC. As part of the temporary certification process that is outlined in the
regulations, ONC is accepting and reviewing applications from organizations that wish to
become certifying bodies and has named three entities thus far to assess and deem EHRs as
certified. However, there are currently no certified EHRs on the market today. ONC expects the
first wave of certified EHRs before the end of the year.
6 | G N Y H A
Related to this, the ONC rule on certification criteria, standards, and implementation
specifications defines the requirements that EHR vendors must meet in order to have their
systems certified under the new process. The certification criteria parallel the CMS meaningful
use criteria and essentially ensure that certified EHR products are meaningful use-ready.
Additionally, ONC has included certification criteria that would enable EHRs to automatically
calculate the functionality measures with a percentage calculation. The criteria also include
calculation and submission of all clinical quality measures that are required by CMS.
Hospitals should be aware, however, that the ONC rule on certification criteria specifies that
certification can be for either a complete EHR that meets all of the certification criteria or a
combination of EHR modules that can meet at least one of the certification criteria. Hospitals are
responsible for ensuring that their EHR system is certified. In the case of hospitals using multiple
EHR components to achieve meaningful use, each component being used for achieving
meaningful use status and to qualify for incentive payments, must work together and have been
certified. ONC will keep a running list on its Web site (http://healthit.hhs.gov) of all complete
EHR systems and EHR system components that are certified. GNYHA encourages hospitals to
speak with their vendors regarding vendor plans for product certification, and should also be
mindful that the specific version of an EHR system or component that they are using has been or
will be certified.
Meaningful Use Objectives
Under HITECH, hospitals and eligible professionals must also use certified EHRs in a
meaningful manner and for electronic exchange to qualify for incentive funds. The CMS
proposed rule required hospitals to meet 23 objectives with no flexibility in prioritizing certain
objectives over others in the early adoption years. In the final rule, CMS offers some flexibility
by dividing the list of objectives for hospitals to meet in Stage 1 into a core set of 14 required
objectives and a menu set of ten objectives from which hospitals must choose five, for a total
of 19 objectives. Hospitals are further required to choose at least one public health objective
from the menu list.
CMS has made several notable changes to the list of objectives required to be met for meaningful
use in the final rule. These include the following:
Two objectives related to administrative transactions previously required were deferred to
a later stage of the program.
CMS has added two new objectives in the menu set, including one related to providing
condition-specific patient education resources and another related to recording advance
directives in the EHR.
The final rule lowers the measurement thresholds for some of the provider objectives.
Hospitals must collect, calculate, and report on 15 clinical quality measures, a significant
reduction from the proposed rules list of 35 quality measures.
Meaningful Use Measures
Each objective has a corresponding measure so that providers may demonstrate to CMS that they
have met the objective. CMS specifies that measures are calculated in one of three ways.
7 | G N Y H A
1. Percentage of all patients, including those with records in the EHR, for which the
denominator is determined by the hospital, the numerator is determined by the EHR,
and the measure is calculated through the EHR.
2. Percentage of patients with records in the EHR for which the numerator and the
denominator values are determined by the EHR and the measure is calculated through
the EHR.
3. Yes/No attestation, for which hospitals would need to enable functionality in the EHR
or that a hospital has performed a test of an EHR capability. For measures that require
a testing of capability to exchange information, CMS indicates that hospitals may use
a dummy case for this test and that the criteria will be considered met even if the test
fails. However, if the test exchange is successful, CMS expectation is that the
capability is then enabled and regular exchange instituted.
In response to the comments it received from the hospital community and others, CMS modified
the functionality measures in several ways:
CMS lowered the threshold on a number of the measures, including the requirement for
the use of CPOE, from 80% of physicians to just 30 % of unique patients.
CMS has added emergency department admissions to the denominator of most of the
measures. Hospitals will need to include patient records with Place of Service codes 21 or
23 (emergency department and inpatient settings) in their denominator to calculate these
measures. Since a majority of hospital admissions are likely to be through the ED,
hospitals will need to have certified EHR systems in their EDs as well as in their inpatient
units.
In order to reduce the burden of calculating and reporting each of the measures, CMS has
modified measures that in the proposed rule required manual calculation and the ONC
certification criteria now include calculating functionality measures as well.
Lastly, CMS has changed many of the definitions for the denominator of the measures to
counting unique patients versus patient encounters or physicians. This, in many cases,
will make it easier for hospitals to meet the criteria.
Permissible Exclusions
New in the final rule is a provision that allows hospitals to indicate to CMS that a functionality
objective does not apply to them. Hospitals may exclude certain objectives if they did not have
any patients to whom the objective applied or if they did not have enough cases to calculate the
measure. These exclusions would be in addition to the five measures from the menu set of
measures that a hospital can defer, so that by excluding a measure, hospitals reduce the number
of measures they need to meet. CMS specifies a total of seven measures for possible exclusion
based on the criteria.
A complete list of the hospital objectives, measures, measure calculation types, and measure
exclusions are in Table 2.
8 | G N Y H A
Table 2: Stage 1 Hospital Objectives for Meaningful Use
OBJECTIVE MEASURE
CALCULATION
METHOD*
ELIGIBLE
FOR
EXCLUSION
Core Set: Hospitals must achieve all of the following objectives and meet the required thresholds.
1. Use CPOE for medication
orders directly entered by
any licensed health care
professional who can enter
orders into the medical
record per state, local, and
professional guidelines
More than 30% of unique patients
with at least one medication in
their medication list admitted to
the eligible hospitals inpatient or
emergency department (POS 21 or
23) have at least one medication
order entered using CPOE
Patients with records in
the EHR
No
2. Implement drug-drug and
drug-allergy interaction
checks
The eligible hospital has enabled
this functionality for the entire
EHR reporting period
Yes/No No
3. Record demographics
Preferred language
Gender
Race
Ethnicity
Date of birth
Date and preliminary
cause of death in the event
of mortality in the eligible
hospital
More than 50% of all unique
patients admitted to the eligible
hospitals inpatient or emergency
department (POS 21 or 23) have
demographics recorded as
structured data
All patients No
4. Maintain an up-to-date
problem list of current and
active diagnoses
More than 80% of all unique
patients admitted to the eligible
hospitals inpatient or emergency
department (POS 21 or 23) have
at least one entry or an indication
that no problems are known for
the patient recorded as structured
data
All patients No
5. Maintain active medication
list
More than 80% of all unique
patients admitted to the eligible
hospitals inpatient or emergency
department (POS 21 or 23) have
at least one entry (or an indication
that the patient is not currently
prescribed any medication)
recorded as structured data
All patients No
6. Maintain active medication
allergy list
More than 80% of all unique
patients admitted to the eligible
hospitals inpatient or emergency
department (POS 21 or 23) have
at least one entry (or an indication
All patients No
9 | G N Y H A
OBJECTIVE MEASURE
CALCULATION
METHOD*
ELIGIBLE
FOR
EXCLUSION
that the patient has no known
medication allergies) recorded as
structured data
7. Record and chart changes
in vital signs:
Height
Weight
Blood pressure
Calculate and display
BMI
Plot and display growth
charts for children 2-20
years, including BMI
For more than 50% of all unique
patients age 2 and over admitted
to eligible hospitals inpatient or
emergency department (POS 21 or
23), height, weight and blood
pressure are recorded as structured
data
Patients with records in
the EHR
No
8. Record smoking status for
patients 13 years old or
older
More than 50% of all unique
patients 13 years old or older
admitted to the eligible hospitals
inpatient or emergency
department (POS 21 or 23) have
smoking status recorded as
structured data
Patients with records in
the EHR
Yes
9. Implement one clinical
decision support rule
related to a high-priority
hospital condition, along
with the ability to track
compliance with that rule
Implement one clinical decision
support rule
Yes/No No
10. Report hospital clinical
quality measures to CMS
or the States
For FY 2011, provide aggregate
numerator, denominator, and
exclusions through attestation
N/A No
For FY 2012, electronically
submit the clinical quality
measures
11. Provide patients with an
electronic copy of their
health information
(including diagnostic test
results, problem list,
medication lists,
medication allergies,
discharge summary,
procedures), upon request
More than 50% of all patients of
the inpatient or emergency
departments of the eligible
hospital (POS 21 or 23) who
request an electronic copy of their
health information are provided it
within 3 business days
Patients with records in
the EHR
Yes
10 | G N Y H A
OBJECTIVE MEASURE
CALCULATION
METHOD*
ELIGIBLE
FOR
EXCLUSION
12. Provide patients with an
electronic copy of their
discharge instructions at
time of discharge, upon
request
More than 50% of all patients who
are discharged from an eligible
hospital inpatient department or
emergency department (POS 21 or
23) and who request an electronic
copy of their discharge
instructions are provided it
Patients with records in
the EHR
Yes
13. Capability to exchange key
clinical information (for
example, discharge
summary, procedures,
problem list, medication
list, medication allergies,
diagnostic test results),
among providers of care
and patient-authorized
entities electronically
Performed at least one test of
certified EHR technology's
capacity to electronically
exchange key clinical information
Yes/No No
14. Protect electronic health
information created or
maintained by the certified
EHR technology through
the implementation of
appropriate technical
capabilities
Conduct or review a security risk
analysis per 45 CFR 164.308
(a)(1) and implement security
updates as necessary and correct
identified security deficiencies as
part of its risk management
process
Yes/No No
Menu Set: Hospitals must achieve five of the following objectives and meet the required thresholds. In
choosing the five objectives, hospitals must include at least one of three public health objectives (8, 9, or 10).
1. Implement drug-formulary
checks
The eligible hospital has enabled
this functionality and has access to
at least one internal or external
drug formulary for the entire EHR
reporting period
Yes/No No
2. Record advance directives
for patients 65 years old or
older
More than 50% of all unique
patients 65 years old or older
admitted to the eligible hospitals
inpatient department (POS 21)
have an indication of an advance
directive status recorded
Patients with records in
the EHR
Yes
3. Incorporate clinical lab-
test results into certified
EHR technology as
structured data
More than 40% of all clinical lab
test results ordered by an
authorized provider of the eligible
hospital for patients admitted to its
inpatient or emergency
department (POS 21 or 23) during
the EHR reporting period whose
Patients with records in
the EHR
No
11 | G N Y H A
OBJECTIVE MEASURE
CALCULATION
METHOD*
ELIGIBLE
FOR
EXCLUSION
results are either in a
positive/negative or numerical
format are incorporated in
certified EHR technology as
structured data
4. Generate lists of patients
by specific conditions to
use for quality
improvement, reduction of
disparities, research or
outreach
Generate at least one report listing
patients of the eligible hospital
with a specific condition
Yes/No No
5. Use certified EHR
technology to identify
patient-specific education
resources and provide
those resources to the
patient if appropriate
More than 10% of all unique
patients admitted to the eligible
hospitals inpatient or emergency
department (POS 21 or 23) are
provided patient-specific
education resources
All patients No
6. The eligible hospital that
receives a patient from
another setting of care or
provider of care or
believes an encounter is
relevant should perform
medication reconciliation
The eligible hospital performs
medication reconciliation for more
than 50% of transitions of care in
which the patient is admitted to
the eligible hospitals inpatient or
emergency department (POS 21 or
23)
Patients with records in
the EHR
No
7. The eligible hospital that
transitions its patient to
another setting of care or
provider of care or refers
its patient to another
provider of care should
provide summary of care
record for each transition
of care or referral
The eligible hospital that
transitions or refers its patient to
another setting of care or provider
of care provides a summary of
care record for more than 50% of
transitions of care and referrals
Patients with records in
the EHR
No
8. Capability to submit
electronic data to
immunization registries or
Immunization Information
Systems and actual
submission in accordance
with applicable law and
practice
Performed at least one test of
certified EHR technology's
capacity to submit electronic data
to immunization registries and
follow up submission if the test is
successful (unless none of the
immunization registries to which
the eligible hospital submits such
information has the capacity to
receive the information
electronically)
Yes/No Yes
12 | G N Y H A
OBJECTIVE MEASURE
CALCULATION
METHOD*
ELIGIBLE
FOR
EXCLUSION
9. Capability to submit
electronic data on
reportable (as required by
state or local law) lab
results to public health
agencies and actual
submission in accordance
with applicable law and
practice
Performed at least one test of
certified EHR technologys
capacity to provide electronic
submission of reportable lab
results to public health agencies
and follow-up submission if the
test is successful (unless none of
the public health agencies to
which the eligible hospital
submits such information has the
capacity to receive the
information electronically)
Yes/No Yes
10. Capability to submit
electronic syndromic
surveillance data to public
health agencies and actual
submission in accordance
with applicable law and
practice
Performed at least one test of
certified EHR technology's
capacity to provide electronic
syndromic surveillance data to
public health agencies and
follow-up submission if the test is
successful (unless none of the
public health agencies to which an
eligible hospital submits such
information has the capacity to
receive the information
electronically)
Yes/No Yes
*Measures are required to be calculated by one of three methods. See the section titled
Meaningful Use Measures for details.
Meaningful Use for Medicaid Adopt, Implement, Upgrade
The final rule clarifies and finalizes CMS proposal for a common framework for meaningful
use for both Medicare and Medicaid. State Medicaid programs are allowed to propose to CMS
state-specific modifications to meaningful use as long as they are limited to public health
objectives and registries and do not require EHR functionality beyond what is included in the
ONC certification criteria. However, hospitals that qualify as meaningful users under Medicare
will be deemed qualified under Medicaid and will not need to meet any additional criteria
imposed by states.
Providers that are eligible for the Medicaid incentive funds may qualify, in their first adoption
year, by adopting, implementing, or upgrading to certified EHR technology. This means that in
the first year that hospitals or eligible professionals receive funding under the Medicaid program,
they can do so for activities related to working towards becoming a meaningful user of EHRs.
However, in order to qualify, the provider must be in the process of adopting, implementing or
upgrading an EHR that has been deemed certified under the new certification process.
13 | G N Y H A
Reporting Clinical Quality Measures
The third element for meaningful use as defined by Congress under HITECH is to submit
clinical quality measure data with the use of certified EHR technology to HHS. CMS intends,
through the electronic reporting of these data, to move from the reporting of quality measures
using claims data to direct reporting from the clinical record.
In the proposed rule, CMS put forward a total of 35 clinical quality measures on which hospitals
must report. The list included measures from a number of clinical areas with a majority of the
measures having not been electronically specified. At that time, CMS acknowledged that a great
deal of work would need to be done by measure developers and vendors before the measures
could be reported.
In the final rule, CMS has eliminated all of the measures that are not currently electronically
specified, leaving a list of 15 measures focused in the areas of stroke care, prevention, treatment
of venous thromboembolisms, and ED throughput. Each of these remaining measures has
technical specifications that have been developed and that are available at
www.cms.gov/qualitymeasures/03_Electronicspecifications.asp#topofpage. Each is also
endorsed by the National Quality Forum and has been adopted by the Hospital Quality Alliance.
However, none of the 15 measures is included in the current Reporting Hospital Quality Data for
the Annual Payment Update (RHQDAPU) program, and is not included among the list put
forward in the final Inpatient Prospective Payment System (IPPS) rule identifying measures to
be reported to CMS for payment for the upcoming year.
Since there is currently no capacity for electronic submission of clinical quality data to CMS, in
2011 hospitals are expected to attest to using a certified EHR to capture and calculate each of the
clinical quality measures. In addition, hospitals would need to submit a summary report as it is
generated from their certified EHR. This summary report would include information on the
numerator, denominator, and all patient exclusions for a measure, as well as the beginning and
ending dates for the reporting period.
Hospitals must also report to CMS on all measures for which they have applicable cases, without
regard to payer. In addition, hospitals must report on all measures for which they did not see
patients. In this case, a hospital would report that it had zero cases in the denominator for that
measure. Therefore, all hospitals must report on all clinical quality measures, regardless of
whether it applies to their patient population.
In the proposed rule, CMS included a separate list of measures on which Medicaid providers
must report. In the final rule, CMS eliminates this requirement and states that the required
clinical quality measures under the Medicare program also apply to the Medicaid program.
In 2012, CMS anticipates having developed a portal through which hospitals can submit
summary information on the clinical quality measures directly to CMS through their EHR
systems. CMS will develop and post information on the technical requirements to submit data
through this portal by April 1, 2011. CMS also plans to provide alternate methods for providers
to submit information, including through a health information exchange, a health information
organization, or through a registry.
14 | G N Y H A
CMS list of clinical quality measures on which eligible hospitals must report are in Table 3
below.
Table 3: Stage 1 Hospital Clinical Quality Measures for Meaningful Use
MEASURE GROUP MEASURE NAME
Emergency Department
Throughput
Median time from ED arrival to ED departure for admitted
patients
Admission decision time to ED departure time for admitted
patients
Stroke Discharge on anti-thrombotics
Anticoagulation for atrial fibrillation/flutter
Thrombolytic therapy for patients arriving within 2 hours of
symptom onset
Anti-thrombotic therapy by day 2
Discharge on statins
Stroke education
Rehabilitation assessment
Venous Thromboembolism
(VTE)
VTE prophylaxis within 24 hours of arrival
Anticoagulation overlap therapy
Platelet monitoring on unfractionated heparin
VTE discharge instructions
Intensive care unit VTE prophylaxis
Incidence of potentially preventable VTE
15 | G N Y H A
Meaningful Use Requirements for EPs
Eligible professionals have similar requirements to meet to qualify as meaningful users of EHRs
and earn incentive funds, with a few exceptions. EPs must meet 15 core set measures and an
additional five measures from a menu set of 10 measures, for a total of 20 measures to qualify.
Like hospitals, EPs would also have to choose one public health measure from the menu set.
A list of the functionality objectives, measures, measure calculation methods, and measure
exclusions for EPs are listed in Table 4.
Table 4: Stage 1 Meaningful Use Objectives and Measures for Eligible Professionals
OBJECTIVE MEASURE
CALCULATION
METHOD*
ELIGIBLE
FOR
EXCLUSION
Core Set: EPs must achieve all of the following objectives and meet the required thresholds.
1. Use CPOE for medication orders
directly entered by any licensed
health care professional who can
enter orders into the medical
record per state, local and
professional guidelines
More than 30% of unique patients
with at least one medication in their
medication list seen by the EP have at
least one medication order entered
using CPOE
Patients with records
in the EHR
Yes
2. Implement drug-drug and drug-
allergy interaction checks
The EP has enabled this functionality
for the entire EHR reporting period
Yes/No No
3. Generate and transmit permissible
prescriptions electronically (eRx)
More than 40% of all permissible
prescriptions written by the EP are
transmitted electronically using
certified EHR technology
Patients with records
in the EHR
Yes
4. Record demographics
Preferred language
Gender
Race
Ethnicity
Date of birth
More than 50% of all unique patients
seen by the EP have demographics
recorded as structured data
All patients No
5. Maintain an up-to-date problem
list of current and active
diagnoses
More than 80% of all unique patients
seen by the EP have at least one
entry or an indication that no
problems are known for the patient
recorded as structured data
All patients No
6. Maintain active medication list
More than 80% of all unique patients
seen by the EP have at least one
entry (or an indication that the patient
is not currently prescribed any
medication) recorded as structured
data
All patients No
7. Maintain active medication
allergy list
More than 80% of all unique patients
seen by the EP have at least one
entry (or an indication that the patient
has no known medication allergies)
All patients No
16 | G N Y H A
OBJECTIVE MEASURE
CALCULATION
METHOD*
ELIGIBLE
FOR
EXCLUSION
recorded as structured data
8. Record and chart changes in vital
signs:
Height
Weight
Blood pressure
Calculate and display BMI
Plot and display growth
charts for children 2-20 years,
including BMI
For more than 50% of all unique
patients age two and over seen by the
EP, height, weight, and blood
pressure are recorded as structured
data
Patients with records
in the EHR
Yes
9. Record smoking status for
patients 13 years old or older
More than 50% of all unique patients
13 years old or older seen by the EP
have smoking status recorded as
structured data
Patients with records
in the EHR
Yes
10. Implement one clinical decision
support rule relevant to specialty
or high clinical priority along
with the ability to track
compliance of that rule
Implement one clinical decision
support rule
Yes/No No
11. Report ambulatory clinical
quality measures to CMS or the
States
For 2011, provide aggregate
numerator, denominator, and
exclusions through attestation
N/A No
For 2012, electronically submit the
clinical quality measures
12. Provide patients with an
electronic copy of their health
information (including diagnostic
test results, problem list,
medication lists, medication
allergies), upon request
More than 50% of all patients of the
EP who request an electronic copy of
their health information are provided
it within 3 business days.
Patients with records
in the EHR
Yes
13. Provide clinical summaries for
patients for each office visit
Clinical summaries provided to
patients for more than 50% of all
office visits within 3 business days
Patients with records
in the EHR
Yes
14. Capability to exchange key
clinical information (for example,
problem list, medication list,
medication allergies, diagnostic
test results), among providers of
care and patient authorized
entities electronically
Performed at least one test of certified
EHR technology's capacity to
electronically exchange key clinical
information
Yes/No No
17 | G N Y H A
OBJECTIVE MEASURE
CALCULATION
METHOD*
ELIGIBLE
FOR
EXCLUSION
15. Protect electronic health
information created or maintained
by the certified EHR technology
through the implementation of
appropriate technical capabilities
Conduct or review a security risk
analysis per 45 CFR 164.308 (a)(1)
and implement security updates as
necessary and correct identified
security deficiencies as part of its risk
management process
Yes/No No
Menu Set: EPs must achieve five of the following objectives and meet the required thresholds. In choosing the five
objectives to meet, EPs must include at least one of two public health objectives (9 or 10).
1. Implement drug-formulary
checks
The eligible EP has enabled this
functionality and has access to at least
one internal or external drug
formulary for the entire EHR
reporting period
Yes/No No
2. Incorporate clinical lab-test
results into certified EHR
technology as structured data
More than 40% of all clinical lab tests
results ordered by the EP during the
EHR reporting period whose results
are either in a positive/negative or
numerical format are incorporated in
certified EHR technology as
structured data
Patients with records
in the EHR
Yes
3. Generate lists of patients by
specific conditions to use for
quality improvement, reduction
of disparities, research or
outreach
Generate at least one report listing
patients of the EP with a specific
condition
Yes/No No
4. Send reminders to patients per
patient preference for
preventive/follow up care
More than 20% of all unique patients
65 years or older or 5 years old or
younger were sent an appropriate
reminder during the EHR reporting
period
Patients with records
in the EHR
Yes
5. Provide patients with timely
electronic access to their health
information (including lab results,
problem list, medication lists,
medication allergies) within four
business days of the information
being available to the EP
More than 10% of all unique patients
seen by the EP are provided timely
(available to the patient within four
business days of being updated in the
certified EHR technology) electronic
access to their health information
subject to the EPs discretion to
withhold certain information
All patients Yes
6. Use certified EHR technology to
identify patient-specific education
resources and provide those
resources to the patient if
appropriate
More than 10% of all unique patients
seen by the EP are provided patient-
specific education resources
All patients No
18 | G N Y H A
OBJECTIVE MEASURE
CALCULATION
METHOD*
ELIGIBLE
FOR
EXCLUSION
7. The EP who receives a patient
from another setting of care or
provider of care or believes an
encounter is relevant should
perform medication reconciliation
The EP performs medication
reconciliation for more than 50% of
transitions of care in which the patient
is transitioned into the care of the
EP
Patients with records
in the EHR
Yes
8. The EP who transitions their
patient to another setting of care
or provider of care or refers their
patient to another provider of care
should provide summary of care
record for each transition of care
or referral
The EP who transitions or refers
his/her patient to another setting of
care or provider of care provides a
summary of care record for more than
50% of transitions of care and
referrals
Patients with records
in the EHR
Yes
9. Capability to submit electronic
data to immunization registries or
Immunization Information
Systems and actual submission in
accordance with applicable law
and practice
Performed at least one test of certified
EHR technology's capacity to submit
electronic data to immunization
registries and follow up submission if
the test is successful (unless none of
the immunization registries to which
the EP submits such information has
the capacity to receive the information
electronically)
Yes/No Yes
10. Capability to submit electronic
syndromic surveillance data to
public health agencies and actual
submission in accordance with
applicable law and practice
Performed at least one test of certified
EHR technology's capacity to provide
electronic syndromic surveillance data
to public health agencies and
follow-up submission if the test is
successful (unless none of the public
health agencies to which an EP
submits such information has the
capacity to receive the information
electronically)
Yes/No Yes
Clinical Quality Measures for EPs
Like hospitals, eligible professionals also have to report on a set of clinical quality measures in
order to qualify for incentive funds. EPs are required to report on three core measures that are
mandatory for all EPs, as well as three additional measures chosen from a list of 38 measures.
Unlike for hospitals, if an EP reports a denominator of zero for a core measure, the EP must
choose an additional alternate core measure on which to report. EPs can be required to report on
up to three additional alternate core measures in this case.
Each of the EP clinical quality measures has been specified for collection through the EHR. The
technical specification for these measures can be found at
www.cms.gov/qualitymeasures/03_Electronicspecifications.asp#topofpage.
19 | G N Y H A
As is the case for hospitals, EP measures are the same for Medicare as they are for Medicaid.
However, since EPs do not qualify for payments under both programs and must choose either
Medicare or Medicaid, they must report clinical quality measure information to their state if they
wish to qualify for the Medicaid incentives. Again, as is the case for hospitals, in 2011, EPs
would need to attest to using a certified EHR to capture and calculate quality measure data and
use an electronic submission for reporting in 2012. Clinical quality measures for EPs can be
found in Table 5.
Table 5: Clinical Quality Measures for Eligible Professionals
CONDITION MEASURE
Core Measures (Must be Reported)
Hypertension Blood pressure management
Prevention Tobacco use assessment and tobacco cessation
intervention
Adult weight screening and follow-up
Alternate Core Measures (Required for Submission if any of the Core Measures = Zero)
Prevention
Weight assessment and counseling for children and
adolescents
Preventive care and screening: influenza
immunization for patients 50 years old
Childhood immunization status
Must Choose three of the Following 38 Measures to Report on:
Diabetes
Hemoglobin A1c poor control
Hemoglobin A1c control (8.0%)
Low Density Lipoprotein (LDL) management and
control
Blood pressure management
Diabetic retinopathy: documentation of presence or
absence of macular edema and level of severity of
retinopathy
Diabetic retinopathy: communication with the
physician managing ongoing diabetes care
Eye exam
Urine screening
Foot exam
Ischemic Vascular Disease Blood pressure management
Use of aspirin or another antithrombotic
Complete lipid panel and LDL control
Pneumonia vaccination for older adults
Breast cancer screening
Colorectal screening
20 | G N Y H A
Preventive Care
Smoking and tobacco use cessation, medical
assistance:
(a) advising smokers and tobacco users to quit
(b) discussing smoking and tobacco cessation
medications
(c) discussing smoking and tobacco use
cessation strategies
Initiation and engagement of alcohol or other drug
dependence treatment
Prenatal care: screening for Human
Immunodeficiency Virus (HIV)
Prenatal care: anti-D immune globulin
Controlling high blood pressure
Cervical cancer screening
Chlamydia screening for women
Cancer
Oncology breast cancer: hormonal therapy for
stage IC-IIIC estrogen receptor/progesterone
receptor positive breast Cancer
Oncology colon cancer: chemotherapy for stage III
colon cancer patients
Prostate cancer: avoidance of overuse of bone scan
for staging low-risk prostate cancer patients
Coronary Artery Disease (CAD)
Beta-blocker therapy for CAD patients with prior
myocardial Infarction
Drug therapy for lowering LDL-cholesterol
Oral antiplatelet therapy prescribed for patients
with CAD
Heart Failure
Angiotensin-Converting Enzyme (ACE) or
Angiotensin Receptor Blocker (ARB) therapy for
left ventricular systolic Function
Beta-blocker therapy for left ventricular systolic
dysfunction
Warfarin therapy patients with atrial fibrillation
Depression
Anti-depressant medication management: (a)
effective acute phase (b) effective continuation
phase treatment
Glaucoma Primary open angle glaucoma: optic nerve
evaluation
Asthma Asthma pharmacologic therapy
Asthma assessment
Use of appropriate medications for asthma
Pharyngitis Appropriate testing for children with pharyngitis.
Imaging Low back pain: use of imaging studies
21 | G N Y H A
Demonstrating Meaningful Use
Once hospitals and EPs are certain they meet the meaningful use criteria with a certified EHR,
they can submit an attestation that identifies their certified EHR and the results of their
performance on all of the meaningful use functionality measures. There will be a common
method for demonstrating meaningful use for Medicare and Medicaid. States will develop their
own, CMS-approved plans for deeming providers qualified.
Reporting will take place through a secure mechanism that CMS has yet to establish. Providers
may attest as early as April 2011 for any EHR reporting period between October 1, 2010 and
March 30, 2011. For subsequent reporting periods, providers may attest as soon as they have
finished a reporting period and will have 60 days after the end of the reporting period to make an
attestation.
CMS will post online for each payment year the names of all providers that were deemed
meaningful users and that received incentive payments.
EHR Reporting Period
In order to receive payments, hospitals and EPs must demonstrate meaningful use during the
EHR reporting period of the relevant payment year. For a providers first payment year, which is
the first year that it qualifies for incentive payments, CMS allows for a shortened reporting
period of any 90-day period within the payment year. Therefore, hospitals may demonstrate that
they are meaningful users during a 90-day period beginning as early as October 2010. For
hospitals that want to qualify for incentive payments in FY 2011, the EHR reporting period can
begin as late as July 2011.
After the first payment year, providers must demonstrate that they are meaningful users for an
entire payment year.
For hospitals receiving payments for adopting, implementing, or upgrading to certified EHR
technology under the Medicaid program, the payment year immediately following the first
Medicaid payment year will also have a 90-day reporting period.
Hospital Incentive Payments
The ARRA provides Medicare and Medicaid HIT incentive payments to eligible hospitals who
are meaningful users of HIT.
Medicare Incentives for Hospitals
Eligibility
The ARRA statute provides Medicare HIT incentive payments to subsection (d) hospitals, or
hospitals that are reimbursed under the Medicare inpatient acute care prospective payment
system (PPS). Hospitals and units excluded from the acute care PPS such as psychiatric,
rehabilitation, long term care, childrens, and cancer hospitals are not eligible to receive
Medicare HIT incentive payments. Critical access hospitals (CAH) are eligible to receive
incentive payments, but based on a separate formula.
22 | G N Y H A
Despite wide opposition from the provider community, CMS finalized its proposal to use the
Medicare provider number, also known as the CMS Certification Number (CCN), to define a
hospital for incentive payment purposes. Payments to eligible hospitals will therefore be made to
each provider as distinguished by the provider number in the hospital cost report. This policy
does not provide multi-campus hospitals with separate payments for each individual campus.
Legislation was recently introduced by the House Ways & Means Committee and the House
Energy & Commerce Committee that would provide multi-campus hospitals with incentive
payments for its main provider hospital, as well as for each hospital campus or remote
location. Hospitals would be given the choice of the following two incentive payment methods:
1) a $2 million base payment for each campus and one discharge-related amount for the total
discharges across the entire system; or 2) one $2 million base payment amount and a discharge-
related amount for each campus location based on the average number of discharges per campus.
GNYHA strongly supports this legislation.
Medicare Incentive Payments
As proposed, the Medicare incentive payment would be equal to:
($2 million base amount + $200 per discharge for all-payer acute discharges 1,150 -
23,000) * the hospitals Medicare share, adjusted for charity care * the applicable
transition factor.
The incentive payment consists of a $2 million base amount plus a discharge-related amount,
which equals $200 per all-payer acute care discharges for total discharges between 1,150 and
23,000. The first 1,149 discharges and all discharges above 23,000 are disregarded. This sum is
multiplied by the Medicare share. The Medicare share is the sum of Medicare FFS days and
Medicare HMO days, divided by total hospital days. The denominator, total hospital days, is
adjusted by a charity care adjustment. The charity care adjustment is calculated as total charges
minus charity care charges, divided by total charges. The effect of this adjustment is to provide a
higher incentive payment to hospitals that provide a greater percentage of charity care. The
resulting amount is then multiplied by a transition factor, which phases down over the period in
which the hospital is eligible to receive incentive funds as is shown in Table 6.
23 | G N Y H A
Table 6: Hospital Payments by Fiscal Year
FY 2011 2012 2013 2014 2015
2011 100% ---- ---- ---- ----
2012 75% 100% ---- ---- ----
2013 50% 75% 100% ---- ----
2014 25% 50% 75% 75% ----
2015 ---- 25% 50% 50% 50%
2016 ---- ---- 25% 25% 25%
Hospitals may begin receiving incentive payments in FY 2011; CMS expects to begin making
payments to qualifying hospitals in May 2011. The last year in which a hospital may become a
meaningful user eligible to receive incentive payments is FY 2015 and no incentive payments
will be made after FY 2016. Only hospitals qualifying as a meaningful user by FY 2013 will
receive their full incentive allocation; hospitals qualifying in later years will receive reduced
amounts.
In the final rule CMS clarified that hospitals must qualify as a meaningful user in each
consecutive year in order to receive their full incentive allocation. If the hospital does not qualify
for incentive payments in one year, the following year will be paid at a reduced transition
amount. For example, if the hospitals first qualifying year is 2011 but they do not qualify in the
following year (i.e., 2012) and then qualify again in 2013, the transition amount for 2013 would
be 50%. The hospital would have missed the opportunity to receive the 75% transition amount
they should have received in 2012.
Payment Example
Hospitals characteristics:
o Per discharge amount
Total acute discharges = 19,500
Qualifying HIT discharges = 19,500 1,149 = 18,351
o Medicare share
Medicare FFS + Medicare HMO days = 46,000
Total days = 105,000
Medicare share = 43.8%
o Charity care adjustment
Charity care charges = $5,000,000
Total charges = $450,000,000
= ($450,000,000 - $5,000,000) / 450,000,000 = 98.9%
24 | G N Y H A
Therefore, the Medicare incentive payment would be calculated as follows:
o = [$2,000,0000 + ($200 * 18,351)] * .438 / .989
o = $2,511,999
And for each year, with the transition adjustment applied, assuming that the hospital
becomes a meaningful user before FY 2013 and that the hospital qualifies in consecutive
years, the annual payments for each year would be as follows:
o Year 1: $2,511,999 * 100% = $2,511,999
o Year 2: $2,511,999 * 75% = $1,883,999
o Year 3: $2,511,999 * 50% = $1,255,999
o Year 4: $2,511,999 * 25% = $627,999
o Total maximum 4-year Medicare incentive payments = $6,279,996
Data Sources and Process for Payment
In order to calculate the incentive payment amount, CMS will use hospital Medicare cost reports
as the data source to determine discharges, Medicare days, total days, and the charity care
adjustment. The metrics needed to compute the hospitals incentive payments will be taken from
the following Medicare cost report worksheets displayed in Table 7:
Table 7: Medicare Cost Report Worksheets for Computing Hospital Incentive Payments
Metric Revised Cost Report
Worksheet Column Line
Discharges
E-1, Part II
S-3, Part I
-
15
1
14, 15, 17
Medicare FFS IP Days
E-1, Part II
S-3, Part I
-
6
2
1, 8-12, 16, 17
Medicare HMO IP Days
E-1, Part II
S-3, Part I
-
6
3
2, 3, 4
Total Inpatient Days
E-1, Part II
S-3, Part I
-
8
4
1, 8 - 12
Charity Care Charges
E-1, Part II
S-10
-
-
6
20
Total Charges
E-1,Part II
C, Part I
-
8
5
200
A preliminary incentive amount will be paid based on the hospitals most recently submitted 12-
month cost report with a final incentive payment to be based on the hospitals settled cost report
that begins after the beginning of the payment year. Hospital incentive payments will be
calculated by the FIs/MACs, but the distribution of payments will be made through a single
payment contractor, who will issue a single initial payment per year after the provider has
demonstrated that it meets the meaningful use criteria for a given FY. CMS expects that
25 | G N Y H A
payments will be made to providers within 1546 days after meeting the meaningful use
requirements.
Medicare Payment Penalties for Hospitals
In addition to the payment incentives, the ARRA also included Medicare hospital market basket
update penalties for those hospitals that are not meaningful users in FY 2015 and each
subsequent FY. The penalties are applied to the applicable FY in which the hospital does not
qualify as a meaningful user and are not cumulative so that hospitals have a constant incentive to
meet the meaningful use criteria (i.e. if a hospital does not meet the meaningful use definition in
FY 2015, but does in FY 2016, the payment penalty would only apply for FY 2015). The
payment penalties apply as follows:
FY 2015: 25% of the market basket update;
FY 2016: 50% of the market basket update; and
FY 2017 and each FY thereafter: 75% of the market basket update.
The penalties apply in addition to any other market basket reductions from Federal health reform
and/or penalties in effect for the provider, such as a market basket reduction for a hospital failing
to report data under the Medicare Quality Incentive Reporting Program. CMS has not yet
proposed how the payment penalties would be calculated/applied, but is expected to do so in
future rulemaking.
Medicaid Incentives for Hospitals
Eligibility
The ARRA statute provides Medicaid HIT incentive payments to acute care hospitals (including
cancer hospitals and CAHs), and childrens hospitals.
Acute care hospital: CMS defines an acute care hospital as a health care facility where the
average length of stay (LOS) is less than 25 days and where the facilitys last four digits of its
CCN (Medicare provider number) are in the range of 00010879 or 13001399. Included in this
category are general short-term hospitals, cancer hospitals, and CAHs. CAHs were previously
not eligible for Medicaid incentives under the proposed rule. CMS states that its intent is to
capture hospitals that are classified as general acute care hospitals and cancer hospitals under the
Medicare program; it is not CMSs intent to capture hospitals that are classified as LTCHs for
Medicare purposes (hospitals with a Medicare LOS of 25 days or more).
Childrens hospital: The final rule defines childrens hospitals as separately certified childrens
hospitals, either freestanding or a hospital-within-hospital, where the last four digits of its CCN
in the range of 33003399, and predominantly treats individuals under 21 years of age.
Similar to the Medicare incentive program, CMS will use the CCN to identify hospitals for
purposes of calculating Medicaid incentive funds. There are however, some important
differences in the hospital eligibility criteria for Medicaid incentive payments compared to
Medicare incentive payments. In order to qualify for Medicaid incentive payments, acute care
26 | G N Y H A
hospitals (including CAHs) must meet the meaningful use criteria discussed above, and must
also have a Medicaid volume percentage of at least 10%. Childrens hospitals are not subject to
the 10% requirement.
Hospitals may begin qualifying for and receiving incentive payments in FY 2011; the last year in
which a hospital may begin receiving Medicaid incentive payments is in FY 2016. Unlike the
Medicare program, the statute did not include Medicaid payment penalties for those hospitals
that do not meet the meaningful use criteria beginning in FY 2015. Hospitals may only qualify to
receive Medicaid incentive payments in one state.
Medicaid Incentive Payments
The hospital Medicaid incentive formula is structured similar to the Medicare incentive formula,
except that the hospitals Medicaid share, adjusted for charity care, will be applied in lieu of the
Medicare share. Similar in concept to the Medicare share, the Medicaid share would be
calculated as the (Medicaid FFS + Medicaid HMO days) / [Total days * charity care adjustment].
CMS intends to count inpatient bed days in the same way they are counted for Medicare
purposes. In New York State, inpatient detoxification, drug rehabilitation, and alcohol
rehabilitation services are considered exempt, non-acute services for Medicaid purposes, but are
considered acute care services by Medicare. Under this final rule, these days would be classified
as acute care for purposes of calculating the hospitals Medicaid share. The number of discharges
used in the discharge related amount for the three years following the first payment year
(considering the four year payment scenario) will be calculated by applying the hospitals most
recent three years average annual rate of growth, whether positive or negative.
The aggregate amount of incentive payments that a hospital may receive will be determined
using the Medicare transition adjustments described above (100% for year one, 75% for year
two, 50% for year three, and 25% for year four). States have flexibility however, to distribute
incentive payments over a minimum of three years and a maximum of six years, instead of over
the prescribed four-year transition period for Medicare. The funding amount that a hospital may
receive in any one year is capped at 50% of its estimated total allowable Medicaid incentive
payment and 90% over two years. GNYHA has strongly recommended to New York State that it
provide the maximum amount of funding allowed.
States will be responsible for calculating the hospital-specific amounts and may use data sources
such as Medicare cost reports, Medicaid cost reports, Medicaid claims information, and hospital
financial statements. Similar to the Medicare incentives, states may use data from the cost report
year prior to the payment year to determine payments.
Eligible Professional Incentive Payments
Eligibility
Eligible professionals (EPs) are also eligible for HIT incentive payments. For Medicare
incentives, EPs are generally defined as physicians such as a doctor of medicine or osteopathy,
dental surgery or medicine, podiatric medicine, optometry, and chiropractics. For Medicaid
incentives, the definition is more expansive and includes dentists, certified nurse-midwives,
27 | G N Y H A
nurse practitioners, and physician assistants practicing in a Federally Qualified Health Center
(FQHC) or Rural Health Clinic.
Hospital-based eligible professionals physicians are excluded from qualifying for EP incentive
funds. These are defined as physicians who furnish substantially all their services in an inpatient
or emergency room setting. In the proposed rule, services provided in outpatient settings were
also included in the definition of hospital setting. As part of the Continuing Extensions Act of
2010, in a provision strongly supported by GNYHA, Congress changed this definition, so in the
final rule hospital-based setting is restricted to services provided in inpatient and emergency
room settings. This allows some hospital-based EPs who practice substantially all of their
covered services in outpatient settings to qualify for incentive payments. This determination will
be made based on site of service and without regard to any employment or billing arrangement
between the EP and any other provider (such as a hospital). In addition, the hospital-based
exclusion does not apply to EPs practicing predominantly in FQHCs or RHCs, even if they are
hospital-owned.
Substantially all is defined as a physician who furnishes 90% or more of his or her Medicare-
covered professional services during a relevant EHR reporting period in a hospital setting. CMS
will determine an EPs qualification based on Medicare physician claims data and classify
physicians who bill at least 90% of their Medicare claims using certain place of service (POS)
codes, identifying the location in which the service was provided, as hospital-based. The POS
codes that will be classified as hospital-based setting include POS 21Inpatient Hospital, and
POS 23Emergency Room, Hospital.
Incentive Payments for Eligible Professionals
Unlike hospitals, EPs are eligible to receive HIT incentive payments from either the Medicare or
Medicaid program, but not both. The EP must notify CMS of which program they choose to
participate in. Once elected, an EP will be permitted to switch between programs, but only one
time, and only prior to 2015.
EPs are allowed to reassign their incentive payments to either an employer with whom the
physician has a contractual arrangementwhere the employer or entity can bill for and receive
payment for covered services provided by the EP, or to an entity that promotes the adoption of
EHR technology. However, EPs may reassign their incentive payments to only one entity, or
only one employer if the EP practices at more than one place of employment.
Medicare FFS Incentive Payments and Penalties
EPs are eligible to receive incentive payments in an amount based on 75% of the estimated
Medicare-allowed charges for all covered professional services provided in a payment year,
subject to an annual cap, which varies based on the eligibility payment year. If the first year an
EP qualifies as a meaningful user is either 2011 or 2012, the EP may receive a maximum of
$18,000; if the first qualifying year is 2013, the maximum eligible payment is $15,000, and
$12,000 in 2014. The maximum aggregate amount of incentive payments an EP can receive
under Medicare is $44,000. The annual limits and total maximum incentive payments for EPs are
provided in the table below. Payments may be received for up to five years, but not after 2016,
and EPs that do not qualify as meaningful users prior to 2015 will not receive any incentive
28 | G N Y H A
payments. In addition to these amounts, EPs practicing predominantly in a federally designated
health professional shortage areas (HPSAs), defined as providing at least 50% of their services in
a HPSA, will receive an additional 10%. EPs will receive incentive payments in a single,
consolidated annual payment following CMS verification of eligibility for the payment year.
Table 8: Medicare Incentive Payments for EPs by Payment Year
CY 2011 2012 2013 2014 2015+
2011 $18,000 ---- ---- ---- ----
2012 $12,000 $18,000 ---- ---- ----
2013 $8,000 $12,000 $15,000 ---- ----
2014 $4,000 $8,000 $12,000 $12,000 ----
2015 $2,000 $4,000 $8,000 $8,000 $0
2016 ----- $2,000 $4,000 $4,000 $0
Total $44,000 $44,000 $39,000 $24,000 $0
Similar to hospitals, beginning in 2015, EPs that are not meaningful users of EHR are subject to
Medicare payment penalties. The penalties would be applied to the Medicare physician fee
schedule rates as follows: for 2015, the penalty is 1%; for 2016, the penalty is 2 %; for 2017, the
penalty is 3%, and, for 2018 and thereafter, the penalty can be adjusted by the HHS Secretary to
be between 3% and 5%, but never more than 5%. The Secretary may grant hardship waivers
from the payment penalties for EPs for whom complying with the meaningful use criteria would
cause extreme hardship. In no case may an EP receive a hardship waiver for more than five
years.
Medicaid Incentive Payments for EPs
In order to qualify for Medicaid incentive funds, an EP must have a Medicaid patient volume of
at least 30%. There are two exceptions to this rule: 1) the qualifying threshold for pediatricians is
20%; and 2) for EPs practicing predominantly in an FQHC or RHC, the qualifying threshold is
30% but it is based on patient volume attributable to needy individuals, which CMS interprets
to mean as Medicaid, CHIP, or uninsured individuals. States have the option to select the
specified methodology for determining patient volume from CMS provided options, or from a
state designed methodology subject to CMS approval.
The Medicaid incentive payments for qualifying EPs are based on 85% of the net average
allowable costs of purchasing and using an EHR. Per the ARRA statute, the net allowable
costs are capped at $25,000 in the first year and $10,000 for each of five subsequent years
thereafter, or $75,000 throughout the HIT incentive program. Therefore, the maximum Medicaid
incentive payment that an EP could receive is 85% of $75,000, or $63,750, more than the
maximum allowed under Medicare. EPs are eligible to receive incentive payments over six
years. There is no transition factor applied to Medicaid incentive payments, and regardless
which year is the first year of qualifying as a meaningful user, EPs are eligible to receive the
maximum allowable amount over the entire six years. The annual limits and total maximum
incentive payments for EPs are provided in the table below. Pediatricians that meet the minimum
29 | G N Y H A
20% threshold but not the non-pediatrician EP threshold of 30% receive reduced incentive
payments, capped at $42,500 over the six-year period.
Table 9: Medicaid Incentive Payments for EPs by Payment Year
CY 2011 2012 2013 2014 2015 2016
2011 $21,250 ---- ---- ---- ---- ----
2012 $8,500 $21,250 ---- ---- ---- ----
2013 $8,500 $8,500 $21,250 ---- ---- ----
2014 $8,500 $8,500 $8,500 $21,250 ---- ----
2015 $8,500 $8,500 $8,500 $8,500 $21,250 ----
2016 $8,500 $8,500 $8,500 $8,500 $8,500 $21,250
2017 ---- $8,500 $8,500 $8,500 $8,500 $8,500
2018 ---- ---- $8,500 $8,500 $8,500 $8,500
2019 ---- ---- ---- $8,500 $8,500 $8,500
2020 ---- ---- ---- ---- $8,500 $8,500
2021 ---- ---- ---- ---- ---- $8,500
Total $63,750 $63,750 $63,750 $63,750 $63,750 $63,750
Program Interaction with State Medicaid
State Medicaid programs may receive 100% match under Federal financial participation (FFP)
on incentive payments they make to Medicaid providers for the adoption, implementation,
upgrade, and the meaningful use of EHRs. Additionally, states will receive 90% of their
administrative costs related to managing the Medicaid EHR incentive programs for their state,
including oversight activities and promotion of health information exchange.
State Medicaid programs will establish their own processes for determining eligibility, deeming
providers as qualified for incentive payments, and distributing payments. State participation in
the EHR incentive program is voluntary and states that wish to participate must submit their
formal HIT plans to CMS on how they will administer the program. Medicaid programs will
begin on a rolling basis, as CMS approves state HIT plans.
CMS Program Implementation and Registration
Although ARRA authorizes payments under the EHR incentive program as early as October
2010, CMS will start the program in January 2011. However, as previously stated, the first
30 | G N Y H A
hospital EHR reporting period will still begin in October 2010 for those hospitals that wish to
demonstrate that they are meaningful users.
Beginning in January 2011, CMS will make available a registration portal at
http://www.cms.gov/EHRIncentivePrograms/50_Registration.asp#TopOfPage for hospitals
and EPs to register for the EHR program. Providers are urged to begin registering for the
program at this time, rather than waiting until they are ready to attest to qualifying for payments.
Registering for the program will not obligate providers in any way.
In order to register, providers must have the following:
1. A national provider identification (NPI) number;
2. Registration for the Provider Enrollment, Chain and Ownership System (PECOS)
database;
3. An active user account in the National Plan and Provider Enumeration System
(NPPES).
Key Dates Related to CMS and ONC Operations
Fall-Winter 2010 Based on the ONC temporary certification process rule, ONC anticipates
that certified EHR technology will be available for purchase or upgrade by hospitals.
January 2011 Launch of CMS single-registration portal for both Medicare and Medicaid
incentive programs.
April 1, 2011 Hospitals and EPs may begin attesting to meeting the meaningful use criteria
with a certified EHR.
Mid-May 2011 CMS will begin making Medicare EHR incentive payments to providers that
qualify and that have made an attestation.
También podría gustarte
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- QPMC Liph 2019Documento69 páginasQPMC Liph 2019JovelleAnneMondragonAún no hay calificaciones
- Thai Healthcare Initiation ReportDocumento88 páginasThai Healthcare Initiation ReportwenjiechanAún no hay calificaciones
- Psychiatric Practice TestDocumento4 páginasPsychiatric Practice TestARIS100% (1)
- Chronic multifactorial autoimmune dermatitisDocumento1 páginaChronic multifactorial autoimmune dermatitisEran Mark RojasAún no hay calificaciones
- Good Manufacturing PracticeDocumento2 páginasGood Manufacturing PracticeBogdan BerariuAún no hay calificaciones
- Martha Rogers Written AssignmentDocumento9 páginasMartha Rogers Written Assignmentapi-101279115Aún no hay calificaciones
- Save the natural tooth or place an implant ? A Periodontal decisional criteria to perform a correct therapy. Ricci, Ricci & Ricci. The International Journal of Periodontics & Restorative Dentistry, 2011; 31, 29-37. .pdfDocumento10 páginasSave the natural tooth or place an implant ? A Periodontal decisional criteria to perform a correct therapy. Ricci, Ricci & Ricci. The International Journal of Periodontics & Restorative Dentistry, 2011; 31, 29-37. .pdfanonimoAún no hay calificaciones
- Foundations - 2 (Part 2)Documento54 páginasFoundations - 2 (Part 2)Minatulahamida Al-fitra KadayunanAún no hay calificaciones
- 6439-Article Text-59821-1-10-20231030Documento12 páginas6439-Article Text-59821-1-10-20231030Rakhmat RamadhaniAún no hay calificaciones
- Lecture 1Documento41 páginasLecture 1Aan KurniawanAún no hay calificaciones
- Clínica Oftalmológica Del Caribe (COFCA) ColombiaDocumento11 páginasClínica Oftalmológica Del Caribe (COFCA) ColombiaJulio Martinez-ClarkAún no hay calificaciones
- C1 Level specialized language exam details for physiciansDocumento2 páginasC1 Level specialized language exam details for physiciansgriscaxxxAún no hay calificaciones
- Narrative Therapy EbookDocumento12 páginasNarrative Therapy EbookSonia Esteves100% (7)
- Relational Coordination: An Exploration of Nursing Units, An Emergency Department and In-Patient TransfersDocumento108 páginasRelational Coordination: An Exploration of Nursing Units, An Emergency Department and In-Patient TransferssaqibshahzadAún no hay calificaciones
- Imunisasi Input Jan-JuliDocumento79 páginasImunisasi Input Jan-Juliiis muniartiAún no hay calificaciones
- Tamil Nadu vital statistics 2020Documento6 páginasTamil Nadu vital statistics 2020Dr Aamir Yousuf AhangarAún no hay calificaciones
- 1001 Arab Inventions WorksheetDocumento4 páginas1001 Arab Inventions WorksheetVictorAún no hay calificaciones
- Manual Physical Therapy For Chronic Pain The Complex Whole Is Greater Than The Sum of Its PartsDocumento4 páginasManual Physical Therapy For Chronic Pain The Complex Whole Is Greater Than The Sum of Its PartsVizaAún no hay calificaciones
- Updated Medicare AEP Ebook 2022-2023Documento14 páginasUpdated Medicare AEP Ebook 2022-2023Sandra Amaya EscobarAún no hay calificaciones
- HEC CaseDocumento7 páginasHEC Caseeatonal1801100% (2)
- Self-Assessment of Nursing Standards of PracticeDocumento17 páginasSelf-Assessment of Nursing Standards of Practiceapi-260548731100% (1)
- ENDODONTICS (Ingle) PDFDocumento1022 páginasENDODONTICS (Ingle) PDFAnonymous Bt6favSF4Y78% (9)
- Assam State Neet-Ug Merit List For Mbbs/Bds Courses, Session-2020Documento431 páginasAssam State Neet-Ug Merit List For Mbbs/Bds Courses, Session-2020Asif IqbalAún no hay calificaciones
- KeynoteAdvanced Unit9 Readingp103Documento3 páginasKeynoteAdvanced Unit9 Readingp103Anh-5A-18 Vũ Ngọc ThảoAún no hay calificaciones
- PQRI - Biosimilar OverviewDocumento20 páginasPQRI - Biosimilar OverviewNgoc Sang HuynhAún no hay calificaciones
- PHCmanual 2010Documento359 páginasPHCmanual 2010primaryhcAún no hay calificaciones
- Himachal Pradesh Aayush ListDocumento9 páginasHimachal Pradesh Aayush ListplanetsandtarotAún no hay calificaciones
- Diamond Select Ingenuity 128Documento2 páginasDiamond Select Ingenuity 128Sepak OdokAún no hay calificaciones
- Benefits of CounsellingDocumento2 páginasBenefits of CounsellingJc OnyekwereAún no hay calificaciones
- 10 1001@jama 2020 0930Documento12 páginas10 1001@jama 2020 0930Dobson Flores AparicioAún no hay calificaciones