Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Schematic Pathophysiology of Stroke (CVA
Cargado por
mizzybaylonDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Schematic Pathophysiology of Stroke (CVA
Cargado por
mizzybaylonCopyright:
Formatos disponibles
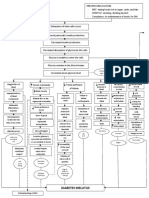
SCHEMATIC PATHOPHYSIOLOGY of CVA
Predisposing Factors: Contributing Factors:
Age (commonly 65 years old Hypertension
and above) Heart Disease
Heredity Diabetes Mellitus
Race (more common in High cholesterol level
African-Americans) Obesity
Gender (more common in Heavy alcohol
Males) consumption
Cigarette smoking
Sedentary lifestyle
Aneurysm
Head Injury
Precipitating Factor
ATHEROSCLEROSIS
Cerebral artery Cardiovascular artery atherosclerosis
atherosclerosis
Formation of plaque deposits
Formation of
plaque deposits Formation of thrombus
Detachment of the thrombus;
Thrombosis becomes an embolus
Travels and lodges in the cerebral arteries
Lysed or moved thrombus from vascular wall
Occlusion of
Leaking of blood from the fragile vascular wall /
cerebral blood
Rupture of the blood vessel
vessels
Cerebral hemorrhage
Hematoma that gradually enlarges
Compression on the nearby blood vessels
Sx: dizziness,
confusion,
Cerebral Hypoperfusion headache
Blood seeps into Impaired distribution of Oxygen and Glucose
the ventricles
Tissue hypoxia and cellular starvation
Cerebral ischemia
Obstruction of the
CSF passageway Initiation of the Ischemic Cascade
Failure in the production of ATP for energy
Failure of energy processes dependent
(ion pumping)
Depolarization of neurons Anaerobic metabolism
by the mitochondria
Intracellular calcium levels get too high
Release of excitatory amino acid Generates large
neurotransmitter glutamate amounts of lactic
Accumulation of acid
CSF in the ventricles Calcium influx
Metabolic
Generation of harmful chemicals like acidosis
free radicals, reactive oxygen species and
calcium-dependent enzymes
Ventricles dilate behind Breakdown of cell membrane
the point of obstruction
Breakdown of mitochondria
Apoptosis
Infarction with necrosis
Transient Ischemic Attack
If managed: If not managed:
Treatment Brain sustains an irreversible cerebral damage
Structural integrity loss of brain tissue and blood vessels
Recovery Breakdown of the protective blood-brain barrier
Cerebral edema
Compression of tissue
Sx: Headache, decreased LOC,
vomiting, impaired sensory and Increased ICP
motor function, changes in vital
signs
Impaired perfusion and function
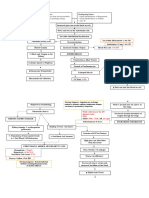
Middle Anterior Posterior Internal Vertebro- Antero- Postero-
Cerebral cerebral Cerebral Carotid basilar inferior inferior
Artery Artery Artery Artery System Cerebellar Cerebellar
Lateral Frontal Occipital Branches Cerebellum Cerebellum
hemisphere Lobe lobe; into and brain
, frontal, anterior ophthalmic, stem
parietal and PCA,
and medial
anterior
temporal portion of choroidal,
lobes, basal temporal ACA, MCA
ganglia lobe
Sx: Sx: Sx: Sx: Sx:
Sx:
foot and leg Mild contralateral Alternating Ataxia, paralysis
hemiparesis deficits contralateral hemiparesis motor of the larynx and
or hemiplegia, greater than hemiparesis, with facial
the arm, foot
weaknesses, soft palate, loss
altered sensory loss, asymmetry,
drop, gait ataxic gait, of sensation in
consciousness, pupillary homonymous
disturbances, contralateral face, sensation
homonymous dysfunction, hemianopsia,
deviation of hemisensory changes on
hemianopsia, loss of ipsilateral
eyes toward impairments, trunk and limbs,
inability to turn conjugate periods of
affected side, double vision, nystagmus,
gaze, blindness,
eyes toward expressive homonymous dysarthria,
aphasia, nystagmus, aphasia if
affected side, loss of depth dominant hemianopsia, Horner’s
confusion,
vision changes, perception, hemisphere nystagmus, syndrome,
amnesia, flat
dyslexia, affect, cortical is involved, paralysis, hiccups and
dysgraphia, apathy, blindness, Mild dysarthria, coughing,
aphasia, shortened homonymous Horner’s memory loss, vertigo, tinnitus,
agnosia, attention hemianopsia, syndrome disorientation, nausea and
span, loss of dyslexia, tinnitus, vomiting
memory mental memory hearing loss,
deficits, acuity, deficits, visual vertigo,
vomiting apraxia, hallucinations dysphagia,
incontinence
coma, altered
swallowing,
taste and smell
If managed: If not managed:
Poor cerebral perfusion Continued insufficiency of blood flow
Poor improvement Further compression of tissues
Cerebral death
Poor prognosis (coma)
Loss of neural feedback mechanisms
Supportive
care Cessation of physiologic functions
Cardiovascular Pulmonary GIT GUT Endocrin
System System e
System
Loss of Relaxatio Failure of Relaxation of Neurogenic Abnormal
cardiac n of the intestines and bladder thermoregulation,
muscle venous diaphragm sphincters Increased
function valves and secretions,
accessory Impaired ability to
muscles for Loss of synthesize WBC
Loss of sphincte
Sx: breathing for fighting
bowel r control
Bradycardia infection, Inability
control
Sx: Sx: of the pancreas to
Hypotensio Apnea produce digestive
n enzymes,
Impaired
Decreased regulation of
cardiac output blood calcium
levels
Systemic Failure
DEATH
También podría gustarte
- Transient Ischemic Attack Precipitating Factors Predisposing FactorsDocumento6 páginasTransient Ischemic Attack Precipitating Factors Predisposing FactorsYosef OxinioAún no hay calificaciones
- Pathophysiology - Tia VS CvaDocumento6 páginasPathophysiology - Tia VS CvaZeo Zafaralla100% (1)
- Pathophysiology ErDocumento3 páginasPathophysiology ErAlexa A. AldayAún no hay calificaciones
- Non-Modifiable, Partially Modifiable, and Modifiable Risk Factors for Atherothrombotic DiseaseDocumento15 páginasNon-Modifiable, Partially Modifiable, and Modifiable Risk Factors for Atherothrombotic DiseaseWiljohn de la CruzAún no hay calificaciones
- Soapie Charting: Date/ Time/ ShiftDocumento2 páginasSoapie Charting: Date/ Time/ Shiftspain michaelisAún no hay calificaciones
- Pathophysiology CVADocumento11 páginasPathophysiology CVAallyana kim figueroa lavarias100% (1)
- Narrowed Blood Vessels and Stroke Nursing CareDocumento4 páginasNarrowed Blood Vessels and Stroke Nursing CareChelsyann FerolinoAún no hay calificaciones
- Pathophysiology HeadinjuryDocumento1 páginaPathophysiology HeadinjuryK.b. Dequiña100% (1)
- Path o Client BasedDocumento3 páginasPath o Client BasedJane TuazonAún no hay calificaciones
- Nephrolithiasis Concept MapDocumento1 páginaNephrolithiasis Concept MapSebastianAún no hay calificaciones
- Pulmonary AngiographyDocumento3 páginasPulmonary AngiographyBiway RegalaAún no hay calificaciones
- Pathophysiology of BPHDocumento1 páginaPathophysiology of BPHJerome Matthew Hautea Amorado0% (1)
- NCP - Risk For Other-Directed ViolenceDocumento2 páginasNCP - Risk For Other-Directed ViolenceKasandra Dawn Moquia BerisoAún no hay calificaciones
- Drug Study CADocumento8 páginasDrug Study CAAna Marie Besa Battung-ZalunAún no hay calificaciones
- Bea Case StudyDocumento19 páginasBea Case StudyBea Flor Rapisura-PegadAún no hay calificaciones
- Comprehensive Table of Drugs: Cholinergic Agonists (Parasympathomimetics)Documento31 páginasComprehensive Table of Drugs: Cholinergic Agonists (Parasympathomimetics)filchibuffAún no hay calificaciones
- Factors and Symptoms of Bone CancerDocumento3 páginasFactors and Symptoms of Bone CancerJenievieve MerzaAún no hay calificaciones
- Addison's Disease (Primary Adrenal Insufficiency)Documento5 páginasAddison's Disease (Primary Adrenal Insufficiency)sunnnydayAún no hay calificaciones
- Pathophysiology of Head TraumaDocumento12 páginasPathophysiology of Head TraumaMohammad ZianuddinAún no hay calificaciones
- Peros: General AssessmentDocumento4 páginasPeros: General AssessmentKaycee TolingAún no hay calificaciones
- Pathophysiology MaiaDocumento2 páginasPathophysiology Maiajia88Aún no hay calificaciones
- DRUG-STUDY Piptaz ClindamycinDocumento2 páginasDRUG-STUDY Piptaz ClindamycinJAYMIE ROSE M. MANUELAún no hay calificaciones
- PATHOPHYSIOLOGYDocumento1 páginaPATHOPHYSIOLOGYJeroham CoAún no hay calificaciones
- نسخة 264889196 Tramadol Drug StudyDocumento1 páginaنسخة 264889196 Tramadol Drug StudyMeteab AlzhiryAún no hay calificaciones
- Uremic EnchepalopathyDocumento5 páginasUremic Enchepalopathyafdhalul mahfudAún no hay calificaciones
- Myonal, LevoprontDocumento1 páginaMyonal, LevoprontMarieCrisAún no hay calificaciones
- Acute Cholecystitis Ppt. DR Dilip S. RajpalDocumento42 páginasAcute Cholecystitis Ppt. DR Dilip S. Rajpaldiliprajpal73100% (1)
- OXYTOCINDocumento2 páginasOXYTOCINPang ProjectAún no hay calificaciones
- General Pathophysiology: Predisposing Factors: Precipitating FactorsDocumento2 páginasGeneral Pathophysiology: Predisposing Factors: Precipitating FactorsIrish Nicole DCAún no hay calificaciones
- NSTEMIDocumento33 páginasNSTEMIwaazalimahwahidAún no hay calificaciones
- Losartan Plus HydrochlorothiazideDocumento18 páginasLosartan Plus Hydrochlorothiazidegmsanto7Aún no hay calificaciones
- End Stage Renal Disease: A. Pathophysiology A. Schematic DiagramDocumento2 páginasEnd Stage Renal Disease: A. Pathophysiology A. Schematic DiagramSharmaine Camille de LeonAún no hay calificaciones
- Pathophysiology of Angina PectorisDocumento1 páginaPathophysiology of Angina PectorisCheryl100% (1)
- Pathophysiology Diagram of Congestive Heart FailureDocumento3 páginasPathophysiology Diagram of Congestive Heart FailureLeng Royo BrionesAún no hay calificaciones
- Flores Mary Jane Generic Drug ChartDocumento23 páginasFlores Mary Jane Generic Drug ChartKristine Dela CruzAún no hay calificaciones
- Nursing Care Plan for Hypertension ManagementDocumento5 páginasNursing Care Plan for Hypertension Managementbhavana100% (1)
- Diabetes Mellitus: Hyperglycemia (304 MG/DL, 13.2 MG/DL)Documento3 páginasDiabetes Mellitus: Hyperglycemia (304 MG/DL, 13.2 MG/DL)John Henry ValenciaAún no hay calificaciones
- Relationship Between CKD Stage and Pulmonary Edema on Chest X-RayDocumento6 páginasRelationship Between CKD Stage and Pulmonary Edema on Chest X-RayAnnisa RabbaniAún no hay calificaciones
- Annotated Group 2 Impetigo Concept Mapping 1Documento30 páginasAnnotated Group 2 Impetigo Concept Mapping 1DHANE ANN CAMPOSANOAún no hay calificaciones
- Jade R. Dinolan BSN-4: Diagnosi SDocumento5 páginasJade R. Dinolan BSN-4: Diagnosi SJhade Relleta100% (1)
- PATHOPHYDocumento3 páginasPATHOPHYArlly Faena AbadAún no hay calificaciones
- Pathophysiology Diagram of Kawasaki Disease: Precipitating Factors: Predisposing FactorsDocumento2 páginasPathophysiology Diagram of Kawasaki Disease: Precipitating Factors: Predisposing FactorsAb Staholic Boii100% (1)
- H MoleDocumento2 páginasH MoleJoanna Marie Datahan EstomoAún no hay calificaciones
- Chronic Kidney Disease GuideDocumento6 páginasChronic Kidney Disease GuideKyle Ü D. CunanersAún no hay calificaciones
- NCP of Difficulty of BreathingDocumento2 páginasNCP of Difficulty of BreathingMan GatuankoAún no hay calificaciones
- Omeprazole Nursing ResponsibilitiesDocumento2 páginasOmeprazole Nursing ResponsibilitiesRea LynAún no hay calificaciones
- DRUG STUDY (Lung Cancer)Documento10 páginasDRUG STUDY (Lung Cancer)Jobelle AcenaAún no hay calificaciones
- Family Nursing Care Plan for ConstipationDocumento4 páginasFamily Nursing Care Plan for ConstipationErika CadawanAún no hay calificaciones
- SabutamolDocumento1 páginaSabutamolKathzkaMaeAgcaoiliAún no hay calificaciones
- Pathophysiology of ObesityDocumento1 páginaPathophysiology of ObesityPoldo Josef AngeloAún no hay calificaciones
- Metformin classification, indications, actions, contraindications and nursing responsibilitiesDocumento7 páginasMetformin classification, indications, actions, contraindications and nursing responsibilitiesgateway1119Aún no hay calificaciones
- Patophy of PudDocumento4 páginasPatophy of PudClarence BravioAún no hay calificaciones
- Brand Name: Bambec Generic Name: Bambuterol HCL Indication: Bronchial AsthmaDocumento2 páginasBrand Name: Bambec Generic Name: Bambuterol HCL Indication: Bronchial AsthmaianecunarAún no hay calificaciones
- Pa Tho Physiology of Open FractureDocumento2 páginasPa Tho Physiology of Open FracturegiffersonbAún no hay calificaciones
- GRP 20 Final Abscess Case StudyDocumento14 páginasGRP 20 Final Abscess Case StudyBorja, Kimberly GraceAún no hay calificaciones
- Physical Examination and Review of Systems: Patient's Name / Room No. - 1Documento3 páginasPhysical Examination and Review of Systems: Patient's Name / Room No. - 1Raf DalidigAún no hay calificaciones
- Nursing Care Plan for Functional Urinary IncontinenceDocumento4 páginasNursing Care Plan for Functional Urinary IncontinenceJez RarangAún no hay calificaciones
- Diabetic Nephropathy Guide: Causes, Symptoms, TreatmentDocumento6 páginasDiabetic Nephropathy Guide: Causes, Symptoms, TreatmentIrma KurniawatiAún no hay calificaciones
- DRUG STUDY FINAL (Onco) PDFDocumento14 páginasDRUG STUDY FINAL (Onco) PDFFrancis Anthony LoslosoAún no hay calificaciones
- Cerebrovascular Accident (CVA) vs. Transient Ischemic Attack (TIA)Documento37 páginasCerebrovascular Accident (CVA) vs. Transient Ischemic Attack (TIA)Grace IgnacoAún no hay calificaciones
- Type A or Type B Personality Test (From Book)Documento2 páginasType A or Type B Personality Test (From Book)mizzybaylon100% (1)
- Activity IntoleranceDocumento4 páginasActivity IntolerancemizzybaylonAún no hay calificaciones
- Pathophysiology of Intestinal Adhesion and Stricture... by Mizzy BaylonDocumento2 páginasPathophysiology of Intestinal Adhesion and Stricture... by Mizzy BaylonmizzybaylonAún no hay calificaciones
- Pathophy of Appendicitis (Or) by Mizzy BaylonDocumento2 páginasPathophy of Appendicitis (Or) by Mizzy BaylonmizzybaylonAún no hay calificaciones
- WINSEM2017-18 CSE4003 ETH SJT501 VL2017185003777 Reference Material I Digital Signature TechniquesDocumento23 páginasWINSEM2017-18 CSE4003 ETH SJT501 VL2017185003777 Reference Material I Digital Signature Techniquesanon_687421514Aún no hay calificaciones
- Unit 1 Notes For Visual Basic Part 1 PDFDocumento38 páginasUnit 1 Notes For Visual Basic Part 1 PDFvipul kumarAún no hay calificaciones
- Sow English Year 3 2023-2024Documento12 páginasSow English Year 3 2023-2024Nizam QusyairiAún no hay calificaciones
- SolidCAM 2015 Turning and Mill Turn Training CourseDocumento282 páginasSolidCAM 2015 Turning and Mill Turn Training Coursehaclongdaica1987100% (2)
- EtherCAT Introduction 0905Documento86 páginasEtherCAT Introduction 0905Pâmella BernardesAún no hay calificaciones
- ENG 211 Academic Oral Presentation Skills Course OutlineDocumento2 páginasENG 211 Academic Oral Presentation Skills Course OutlineIvan GoncharovAún no hay calificaciones
- Advanced VocabBuilder ExercisesAndAnswerkey PDFDocumento24 páginasAdvanced VocabBuilder ExercisesAndAnswerkey PDFTere Fernandez MolinaAún no hay calificaciones
- Lesson 3: Grade 9 Mathematics DateDocumento4 páginasLesson 3: Grade 9 Mathematics DateAinu MuawidzahAún no hay calificaciones
- Root Words, Prefixes and Suffixes Used in Dental TermsDocumento2 páginasRoot Words, Prefixes and Suffixes Used in Dental TermssalahAún no hay calificaciones
- CS305 Microprocessors and Microcontrollers PDFDocumento2 páginasCS305 Microprocessors and Microcontrollers PDFlaraAún no hay calificaciones
- Life lessons from famous quotesDocumento102 páginasLife lessons from famous quotesThodoris DermatisAún no hay calificaciones
- Book Review - Toward A Structural Psychology of CinemaDocumento3 páginasBook Review - Toward A Structural Psychology of Cinema3xpositionalAún no hay calificaciones
- 12.sinif Ingilizce Yillik Plan 2023 2024 IndirDocumento6 páginas12.sinif Ingilizce Yillik Plan 2023 2024 IndirfckepenekAún no hay calificaciones
- Probability Homework HelpDocumento22 páginasProbability Homework HelpStatistics Homework SolverAún no hay calificaciones
- Matlab Tutorial and Linear Algebra ReviewDocumento34 páginasMatlab Tutorial and Linear Algebra ReviewRoihanNstAún no hay calificaciones
- Inglés Primaria Quinto 2 PDFDocumento25 páginasInglés Primaria Quinto 2 PDFmargantoniAún no hay calificaciones
- Sound Fields Radiated by Multiple Sound Sources ArraysDocumento45 páginasSound Fields Radiated by Multiple Sound Sources ArraysmewarulesAún no hay calificaciones
- Philosophy of ArtDocumento22 páginasPhilosophy of ArtHomer PunzalanAún no hay calificaciones
- Tania Joanna Dolphin Discursive Construction Hunza Pakistan Travel Writing 1889-1999Documento328 páginasTania Joanna Dolphin Discursive Construction Hunza Pakistan Travel Writing 1889-1999Pear DadaAún no hay calificaciones
- Resolve ISL Isolation on a TE PortDocumento3 páginasResolve ISL Isolation on a TE PortShashi KanthAún no hay calificaciones
- OneCommander User ManualDocumento403 páginasOneCommander User ManualRoner MouraAún no hay calificaciones
- Daily Lesson Plan on Farming Tools and MaterialsDocumento8 páginasDaily Lesson Plan on Farming Tools and MaterialsMike Lyster AlvarezAún no hay calificaciones
- Implementing and Configuring Modern SAN FC-NVMEDocumento45 páginasImplementing and Configuring Modern SAN FC-NVMEcresmakAún no hay calificaciones
- Analysis of Sorting Algorithms by Kolmogorov Complexity (A Survey)Documento19 páginasAnalysis of Sorting Algorithms by Kolmogorov Complexity (A Survey)Hesham HefnyAún no hay calificaciones
- AI CLIPS Language TutorialDocumento30 páginasAI CLIPS Language TutorialwalterancoAún no hay calificaciones
- AutoCAD 2006 Installing Network License Manager0Documento12 páginasAutoCAD 2006 Installing Network License Manager0gurugovindanAún no hay calificaciones
- HHM Biography Lesson PlanDocumento3 páginasHHM Biography Lesson Planapi-328353630Aún no hay calificaciones
- Aws - Sa NotesDocumento68 páginasAws - Sa NotesArcha MuraleedharanAún no hay calificaciones
- SUP 2023 Literary Studies CatalogDocumento20 páginasSUP 2023 Literary Studies CatalogStanford University Press100% (1)
- Hebrew Literature and the State of IsraelDocumento31 páginasHebrew Literature and the State of Israeljalebie talabangAún no hay calificaciones