Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Konyol
Cargado por
JamaluddinLukmanTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Konyol
Cargado por
JamaluddinLukmanCopyright:
Formatos disponibles
Clinimetrics
Dizziness Handicap Inventory (DHI)
Description
The Dizziness Handicap Inventory (DHI) was developed to propose that a total score of 0–30 indicates mild, 31–60
measure the self-perceived level of handicap associated with moderate, and 61–100 severe handicap, and that scores
the symptom of dizziness (Jacobson and Newman 1990). relate well to levels of functional balance impairment.
The DHI has 25 items with 3 response levels, sub-grouped
into three domains: functional, emotional, and physical. A In contrast to the DHI, the DHIsf (Tesio et al 1999) is scored
shortened version, the Dizziness Handicap Inventory short in the opposite direction. Respondents choose between 2
form (DHIsf), reduced to 13 items with 2 response levels, statements, the first is scored 1 and the second is scored 0,
has been shown to compare favourably to the original with a possible maximum score of 13, where 13 indicates
version (Tesio et al 1999). no dizziness handicap and 0 maximum handicap.
Instructions to the client and scoring: The questionnaires Reliability, validity and sensitivity to change: Test-retest
take only 5–10 minutes to complete and score, and require reliability (r = 0.92 to 0.97) and internal consistency (α =
no special training to administer. For the DHI, respondents 0.72 to 0.89) has been demonstrated to be high with both the
choose one of three statements that most applies to them in DHI and DHIsf. There is evidence to support the construct
each section. The first statement is scored 0, the second is validity of the DHI and DHIsf and the instrument has been
scored 2, and the third is scored 4. The sum of the scores is able to detect statistically significant change over time in
the total score. Possible score ranges are 0–100; a higher group data. The DHI also has minimal floor and ceiling
score indicates worse handicap. Subscores for each of the effects (Enloe and Shields 1997).
three domains can also be calculated. Whitney et al (2004)
Commentary
The dizziness handicap inventory provides a useful, reliable The DHI may be suitable to predict postoperative dizziness
and valid measure of self-perceived handicap associated in patients with acoustic neuroma (Perex et al 2001).
with dizziness. It has been used predominantly in patients Recently it has also been suggested that a 5-point subscale
with peripheral and central vestibular pathology, but has identified from existing items of the DHI may be useful
also been used to evaluate subjective dizziness impairment in identifying patients with benign paroxysmal positional
in subjects with traumatic brain injury (Kaufman et al vertigo (Whitney et al 2005).
2005) persistent whiplash-associated disorders (Treleaven
et al 2005), and major anxiety disorders (Stabb et al 2004), In summary, the DHI is a reliable, comprehensively validated
and in the elderly (Whitney et al 1999). The DHI has been and clinically useful tool to measure self-perceived handicap
demonstrated to be sensitive to change with interventions associated with the symptom of dizziness from a variety of
(Enloe and Shields 1997, Badke et al 2005) and correlates causes. Clinicians may use the DHI or DHIsf to evaluate
well with selected functional measures of gait (Whitney et dizziness handicap as well as to demonstrate functional
al 2004). Significant correlations between specific objective outcomes in patients with dizziness following interventions.
measures of balance and DHI scores have also been A change of at least 10% in the score would be clinically
demonstrated (Kaufman et al 2005, Whitney et al 2004, relevant.
Treleaven et al 2005). Julia Treleaven
The University of Queensland
References
Badke M et al (2005): Ann Otol Rhinol Laryngol 114: 48–54. Stabb et al (2004): Laryngoscope 114: 1637–1641.
Enloe L and Shields R (1997): Phys Ther 77: 890–903. Tesio L et al (1999): Am J Phys Med Rehabil 78: 233–241.
Jacobson G and Newman C (1990): Arch Otolaryngol Head Treleaven J et al (2005): J Rehab Med 37: 224–229.
Neck Surg 116: 424–427.
Whitney S et al (2004): Otol Neurotol 25: 139–143.
Kaufman K et al (2005): Med Eng Phys Jul 22.
Whitney S et al (2005) Otol Neurotol 26: 1027–1033.
Perez N et al (2001): Acta Otolaryngol Suppl 545: 145–154.
Australian Journal of Physiotherapy 2006 Vol. 52 – © Australian Physiotherapy Association 2006 67
También podría gustarte
- Reporte Especial Resicitacion NeonatalDocumento17 páginasReporte Especial Resicitacion NeonatalAna León VigilAún no hay calificaciones
- Sunday NightDocumento26 páginasSunday NightJamaluddinLukmanAún no hay calificaciones
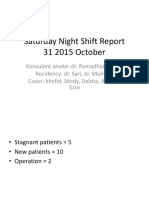
- Saturday Night ShiftDocumento16 páginasSaturday Night ShiftJamaluddinLukmanAún no hay calificaciones
- Jadwal Operasi Senin, 17 Juni 2019Documento1 páginaJadwal Operasi Senin, 17 Juni 2019JamaluddinLukmanAún no hay calificaciones
- DAFTAR TAMU SOK 2015 SYAHIDA InnDocumento4 páginasDAFTAR TAMU SOK 2015 SYAHIDA InnJamaluddinLukmanAún no hay calificaciones
- JumantikDocumento3 páginasJumantikJamaluddinLukmanAún no hay calificaciones
- Dizziness Handicap Inventory PDFDocumento2 páginasDizziness Handicap Inventory PDFJamaluddinLukmanAún no hay calificaciones
- Duty Report Sunday Morning 26-11-2017Documento14 páginasDuty Report Sunday Morning 26-11-2017JamaluddinLukmanAún no hay calificaciones
- Prospective Randomized Trial of TrimethoDocumento7 páginasProspective Randomized Trial of TrimethoJamaluddinLukmanAún no hay calificaciones
- Sunday Night - 24th FebDocumento6 páginasSunday Night - 24th FebJamaluddinLukmanAún no hay calificaciones
- Saturday Night ShiftDocumento25 páginasSaturday Night ShiftJamaluddinLukmanAún no hay calificaciones
- Study of Trunk Asymmetry in Normal Children and AdolescentsDocumento8 páginasStudy of Trunk Asymmetry in Normal Children and AdolescentsJamaluddinLukmanAún no hay calificaciones
- WEEKLY PLASTIC SURGERY ROUND REPORTDocumento38 páginasWEEKLY PLASTIC SURGERY ROUND REPORTJamaluddinLukmanAún no hay calificaciones
- Diagnosing and Managing Ibd PDFDocumento37 páginasDiagnosing and Managing Ibd PDFJamaluddinLukmanAún no hay calificaciones
- DHI Score PDFDocumento2 páginasDHI Score PDFAnonymous HNGH1oAún no hay calificaciones
- 1582 4356 1 PBDocumento9 páginas1582 4356 1 PBnurulanisa0703Aún no hay calificaciones
- Jurnal Terapi PDFDocumento5 páginasJurnal Terapi PDFJamaluddinLukmanAún no hay calificaciones
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- ComplexTrauma All PDFDocumento41 páginasComplexTrauma All PDFIuliaPopescu100% (2)
- Yale Psilo Dep Manual - Final W DOIDocumento79 páginasYale Psilo Dep Manual - Final W DOIChristian OrtizAún no hay calificaciones
- ABM Students' Stress Coping StrategiesDocumento21 páginasABM Students' Stress Coping StrategiesMercedita Balgos100% (1)
- Disturbance of Minimal Self Ipseity in SDocumento4 páginasDisturbance of Minimal Self Ipseity in Sferny zabatierraAún no hay calificaciones
- Guardian Emotional Release MethodDocumento13 páginasGuardian Emotional Release Methodpaulxe100% (2)
- Frustration and Externalization: The Psychoanalytic QuarterlyDocumento14 páginasFrustration and Externalization: The Psychoanalytic QuarterlyMarcosAún no hay calificaciones
- Mindfulness and Acceptance For Addictive Behaviors Applying Contextual CBT To Substance Abuse and Behavioral AddictionsDocumento354 páginasMindfulness and Acceptance For Addictive Behaviors Applying Contextual CBT To Substance Abuse and Behavioral AddictionsAlejandra Vergara83% (6)
- Attachment TheoryDocumento5 páginasAttachment TheoryUme HabibaAún no hay calificaciones
- Unlv Resource GuideDocumento56 páginasUnlv Resource Guideapi-212210463Aún no hay calificaciones
- 08.16.16 - Assessment of Substance Use-In ClassDocumento22 páginas08.16.16 - Assessment of Substance Use-In ClassKAún no hay calificaciones
- CBT WorkshopDocumento52 páginasCBT WorkshopKhoa Le Nguyen100% (13)
- Module 7 - Mental HealthDocumento28 páginasModule 7 - Mental HealthEdithaAún no hay calificaciones
- Zunkel Final Winter 21Documento30 páginasZunkel Final Winter 21Raghabendra ShahAún no hay calificaciones
- Krijn 2004 - Virtual Reality Exposure of Anxiety Disorders PDFDocumento23 páginasKrijn 2004 - Virtual Reality Exposure of Anxiety Disorders PDFJane DoeAún no hay calificaciones
- Positum International NewsDocumento10 páginasPositum International Newsica31blueAún no hay calificaciones
- Autism AssessmentDocumento37 páginasAutism AssessmentRafael Martins94% (16)
- Impact of Domestic Violence on ChildrenDocumento5 páginasImpact of Domestic Violence on ChildrenSmallz AkindeleAún no hay calificaciones
- Case Reports Catatonic and Psychotic Symptoms Owing To The Trauma of Captivity in A Cult EnvironmentDocumento6 páginasCase Reports Catatonic and Psychotic Symptoms Owing To The Trauma of Captivity in A Cult EnvironmentDeborah RiskinAún no hay calificaciones
- Effects of Alcoholism On Families: Children of Parents Who DrinkDocumento2 páginasEffects of Alcoholism On Families: Children of Parents Who DrinkmartinAún no hay calificaciones
- Original Post Tramatic Stress Index PTSI Test by Patrick Carnes PDFDocumento10 páginasOriginal Post Tramatic Stress Index PTSI Test by Patrick Carnes PDFNikiEnDanieTolkenAún no hay calificaciones
- Takeaway Tip SheetDocumento2 páginasTakeaway Tip Sheetapi-521314035Aún no hay calificaciones
- Behaviour Therapy NotesDocumento2 páginasBehaviour Therapy NotesPrathamanantaAún no hay calificaciones
- Ddis DSM 5Documento20 páginasDdis DSM 5AlexisMolinaCampuzanoAún no hay calificaciones
- Group Dynamics Adlerian Group Therapy SessionDocumento3 páginasGroup Dynamics Adlerian Group Therapy SessionAl John Ezekiel UdtuhanAún no hay calificaciones
- Providing Social Emotional Support to StudentsDocumento29 páginasProviding Social Emotional Support to Studentssri887Aún no hay calificaciones
- Test Bank Chapter 5: Psychosocial Alterations: Urden: Thelan's Critical Care Nursing, 5 EditionDocumento8 páginasTest Bank Chapter 5: Psychosocial Alterations: Urden: Thelan's Critical Care Nursing, 5 EditionAnonymous ZzjzIcmAún no hay calificaciones
- Schema Therapy For Borderline Personality Disorder A Comprehensive Review of Its Empirical Foundations, Effectiveness and ImplementationDocumento22 páginasSchema Therapy For Borderline Personality Disorder A Comprehensive Review of Its Empirical Foundations, Effectiveness and ImplementationMa Fernanda Claudio Sal100% (1)
- Putting The Pieces TogetherDocumento12 páginasPutting The Pieces Togethersandrashalom2100% (1)
- Attachment and Trauma: CongressDocumento17 páginasAttachment and Trauma: CongressOvidiu Berar100% (1)
- 01.pengantar PsikoterapiDocumento26 páginas01.pengantar PsikoterapiBabyCher StoresAún no hay calificaciones