Documentos de Académico
Documentos de Profesional
Documentos de Cultura
LANCET 2018 Long Term Outcomes For Neoadjuvant Versus Adjuvant Chemotherapy in Early Breast Cancer - Meta-Analysis of Individual Patient Data From Ten Randomised Trials
Cargado por
Yesenia HuertaTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
LANCET 2018 Long Term Outcomes For Neoadjuvant Versus Adjuvant Chemotherapy in Early Breast Cancer - Meta-Analysis of Individual Patient Data From Ten Randomised Trials
Cargado por
Yesenia HuertaCopyright:
Formatos disponibles
Articles
Long-term outcomes for neoadjuvant versus adjuvant
chemotherapy in early breast cancer: meta-analysis of
individual patient data from ten randomised trials
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG)*
Summary
Background Neoadjuvant chemotherapy (NACT) for early breast cancer can make breast-conserving surgery more Lancet Oncol 2018; 19: 27–39
feasible and might be more likely to eradicate micrometastatic disease than might the same chemotherapy given after Published Online
surgery. We investigated the long-term benefits and risks of NACT and the influence of tumour characteristics on December 11, 2017
http://dx.doi.org/10.1016/
outcome with a collaborative meta-analysis of individual patient data from relevant randomised trials. S1470-2045(17)30777-5
See Comment page 2
Methods We obtained information about prerandomisation tumour characteristics, clinical tumour response, surgery,
*Full list of members in the
recurrence, and mortality for 4756 women in ten randomised trials in early breast cancer that began before 2005 and appendix (pp 19–24) or at
compared NACT with the same chemotherapy given postoperatively. Primary outcomes were tumour response, https://www.ctsu.ox.ac.uk/
extent of local therapy, local and distant recurrence, breast cancer death, and overall mortality. Analyses by research/ebctcg
intention-to-treat used standard regression (for response and frequency of breast-conserving therapy) and log-rank Correspondence to:
methods (for recurrence and mortality). EBCTCG Secretariat, Medical
Research Council Population
Health Research Unit, Nuffield
Findings Patients entered the trials from 1983 to 2002 and median follow-up was 9 years (IQR 5–14), with the last Department of Population
follow-up in 2013. Most chemotherapy was anthracycline based (3838 [81%] of 4756 women). More than two thirds Health, Oxford OX3 7LF, UK
(1349 [69%] of 1947) of women allocated NACT had a complete or partial clinical response. Patients allocated NACT bc.overview@ndph.ox.ac.uk
had an increased frequency of breast-conserving therapy (1504 [65%] of 2320 treated with NACT vs 1135 [49%] of See Online for appendix
2318 treated with adjuvant chemotherapy). NACT was associated with more frequent local recurrence than was
adjuvant chemotherapy: the 15 year local recurrence was 21·4% for NACT versus 15·9% for adjuvant chemotherapy
(5·5% increase [95% CI 2·4–8·6]; rate ratio 1·37 [95% CI 1·17–1·61]; p=0·0001). No significant difference between
NACT and adjuvant chemotherapy was noted for distant recurrence (15 year risk 38·2% for NACT vs 38·0% for
adjuvant chemotherapy; rate ratio 1·02 [95% CI 0·92–1·14]; p=0·66), breast cancer mortality (34·4% vs 33·7%; 1·06
[0·95–1·18]; p=0·31), or death from any cause (40·9% vs 41·2%; 1·04 [0·94–1·15]; p=0·45).
Interpretation Tumours downsized by NACT might have higher local recurrence after breast-conserving therapy than
might tumours of the same dimensions in women who have not received NACT. Strategies to mitigate the increased
local recurrence after breast-conserving therapy in tumours downsized by NACT should be considered—eg, careful
tumour localisation, detailed pathological assessment, and appropriate radiotherapy.
Funding Cancer Research UK, British Heart Foundation, UK Medical Research Council, and UK Department of
Health.
Copyright © The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license.
Introduction the local (and, by implication, disseminated) tumour to
Neoadjuvant chemotherapy (NACT)—ie, chemotherapy different chemotherapy regimens, helping to guide
begun before breast cancer surgery—was introduced in subsequent drug selection.6,7 Conversely, by delaying
the 1970s,1 aiming to downstage locally advanced surgery, NACT might increase the risk of metastatic
(inoperable) disease and make it operable. NACT was spread, particularly for chemoresistant tumours.
subsequently extended to operable (early) breast cancer, Several randomised trials8–17 have compared NACT
mainly to allow breast-conserving surgery, and is now with the same chemotherapy given postoperatively.
widely used, particularly for large tumours.2–4 Further Interpretation of these trials is complicated, however, as
more, NACT might be somewhat more likely to eradicate the frequency of breast-conserving surgery often differed
micrometastatic disease than might chemotherapy between groups because of tumour shrinkage after
delayed until after surgery. NACT. In certain trials,14,15 some good responders to
NACT might mitigate the hypo thesised stimulatory NACT did not receive surgery, and high frequencies of
effect of surgery on occult disease5 and reduce tumour local recurrence with NACT in these trials have been
cell shedding during surgery. NACT might also provide attributed to omission of definitive local therapy. Any
useful in-vivo information about the chemosensitivity of such differences in the extent of surgery confound
www.thelancet.com/oncology Vol 19 January 2018 27
Articles
Research in context
Evidence before this study 4756 women in ten trials, found that the frequencies of clinical
The Early Breast Cancer Trialists’ Collaborative Group’s ongoing response and breast-conserving therapy were higher for smaller,
extensive searches of bibliographic databases, including higher-grade, and oestrogen receptor-negative and
MEDLINE, Embase, the Cochrane Library, and meeting abstracts progesterone receptor-negative tumours, and for one trial using
up to March 2017, identified 16 trials that compared anthracycline and taxane chemotherapy. Although responders
neoadjuvant chemotherapy (NACT) with the same to NACT had lower distant recurrence and breast cancer
chemotherapy postoperatively. Meta-analyses of published mortality than did non-responders, when responders and
reports indicate that NACT reduced the frequency of non-responders were combined, distant recurrence and breast
mastectomy but did not affect mortality. Interpretation is cancer mortality were similar for NACT and adjuvant
complicated, however, as the use of breast-conserving surgery chemotherapy. Local recurrence was, however, higher with
often differed between groups because of tumour shrinkage by NACT than with adjuvant chemotherapy, which persisted for
NACT. In certain trials, some patients with a good response did 10 years after treatment and was not confined to trials in which
not receive surgery. Hence, women allocated NACT retained surgery could be omitted after response to NACT.
more breast tissue than did those allocated adjuvant
Implications of all the available evidence
chemotherapy, and higher local recurrence frequencies in some
NACT is as effective as adjuvant chemotherapy in reducing the
neoadjuvant trials than in others have been attributed to
risk of distant recurrence and death from breast cancer.
omission of definitive local therapy.
However, NACT is associated with higher local recurrence than
Added value of this study adjuvant chemotherapy, which could be at least partly
We did a meta-analysis of individual patient data from trials explained by wider use of breast-conserving therapy after NACT
that compared NACT with the same chemotherapy given than with postoperative chemotherapy. Strategies to mitigate
postoperatively. We assessed effects of patient and tumour the increased local recurrence after breast-conserving therapy in
characteristics on tumour response, extent of local therapy, tumours downsized by NACT should be considered—eg, careful
local and distant recurrence, breast cancer death, and overall tumour localisation, detailed pathological assessment, and
mortality. This individual patient data meta-analysis, involving appropriate radiotherapy.
comparisons of the efficacy of NACT with that of about patient and tumour characteristics, treatments,
adjuvant chemotherapy.18,19 Another complication is that dates of any local recurrence (breast, chest wall, or
investigations of the influence of tumour characteristics regional nodes), distant recurrence, contralateral breast
on outcome need to use prerandomisation data, as or other second primary cancer, and date last known to
analyses by postsurgical characteristics would be be alive or date and underlying cause of death. To avoid
substantially biased by downstaging.20 To investigate bias, we sought data for tumour characteristics recorded
such issues in more detail than was possible in reviews18,19 before randomisation since these characteristics can be
of published data, we did a patient-level meta-analysis of altered by neoadjuvant treatment. We also requested
the trials that directly compared any NACT regimen tumour response after NACT (assessed mostly by
with the same regimen begun postoperatively. palpation and mammography). To investigate the
influence of NACT on extent of surgery, we sought
Methods details of surgery planned at randomisation and surgery
Study design and participants actually done. When planned surgery was unknown, it
We sought data from all randomised trials in early was inferred from clinical tumour size. Patient-level data
(ie, operable) breast cancer that began before 2005 and for radiotherapy were unavailable.
compared NACT with the same chemotherapy begun
after surgery (ie, standard adjuvant chemotherapy). Statistical analysis
NACT always started before surgery, although in some A detailed description of the statistical methods has been
trials, some of the chemotherapy in the NACT group previously published.22 Primary outcomes assessed were
was given postoperatively, whereas all chemotherapy in tumour response (complete response [no clinical
the control group had to be postoperative (so trials such evidence of disease after NACT], partial response
For more on trial identification as NSABP B-2721 were ineligible). Trial identification [≥50% reduction in initial size], or stable or progressive
and data checking see and data checking were as reported previously22,23 and disease [<50% reduction, no change, or increased tumour
https://www.ctsu.ox.ac.uk/
research/ebctcg/prisma-ipd-
conformed to the Preferred Reporting Items for size]), extent of local therapy (mastectomy, lumpectomy
statement-for-ebctcg.pdf Systematic Review and Meta-Analyses (Individual [either with or without radiotherapy], and radiotherapy
Patient Data).24 For every woman, we requested alone), local and distant recurrence, breast cancer death
information from the trial’s principal investigator or (via subtraction of the log-rank statistics of death without
another appropriate member of their research group recurrence from those of overall survival23), and overall
28 www.thelancet.com/oncology Vol 19 January 2018
Articles
mortality (death from any cause). Analyses were by Associations between baseline variables and outcome
intention to treat and are of first isolated local recurrence used prerandomisation values. Only two trials provided
(site not generally available), any distant recurrence pathological response data, so correlations of charac
(irrespective of previous local or contralateral recurrence), teristics with response to NACT use clinical response
breast cancer mortality, and all-cause mortality. data (available for eight of ten trials). Subgroup analyses
We treated deaths from new cancers of unknown primary compare outcomes in trials in which all women
sites as breast cancer deaths. When no recurrence was allocated NACT were, or were not, scheduled to receive
reported before breast cancer death, we assumed distant breast surgery and in women whose initially planned
recurrence to have just preceded it. We took deaths from local treatment was mastectomy or breast-conserving
an unknown cause without recorded recurrence to be therapy (lumpectomy with or without radiotherapy or
non-breast cancer deaths. Comparisons of NACT radiotherapy alone). Sensitivity analyses assess the
response and frequency of breast-conserving therapy potential effect27 on local recurrence of competing
used regression models,25 accounting for tumour size events (distant recurrence and death without
and trial. We stratified log-rank analyses by trial, recurrence) and of omission of trials with only first
follow-up year, age at entry (<35 years, 35–44 years, recurrences recorded. p values of 0·05 or less are
45–54 years, 55–69 years, and ≥70 years), and described as significant. Analyses used Stata 13.1 and
prerandomisation clinical nodal status (N0 or other). R 2.13.2.
In such analyses, if a log-rank statistic (o−e) has
variance v, then, defining z=(o−e)/√v and b=(o−e)/v, the Data sharing
event rate ratio (RR; NACT vs control) is estimated as Procedures for data access are available online. For data access procedures see
exp(b) with SE=(RR−1)/z. RRs and confidence limits https://www.ndph.ox.ac.uk/
about/data-access-policy
for RR are derived from those for b (by normal Role of the funding source
approximations). To test for a trend between n strata The funders of the study had no role in study design,
(eg, of age) in the effects of treatment, we supposed that data analysis, data interpretation, or writing of the
stratum number s (s=1,2,…,n) has log-rank statistics report. The secretariat had full access to all the data in
(o–e) and v (with grand total over all strata O–E and V). the study. The writing committee had final responsibility
We defined m, the mean stratum number, to be the sum, for the decision to submit for publication.
one term per stratum, of sv/V and define T to be the
sum, one term per stratum, of (s–m)(o–e).26 The variance Results
of T, var(T), is then the sum, one term per stratum, of Individual patient data were available from ten8–17 of
(s–m)²/v. The trend test statistic (ie, the change from one 16 eligible trials identified and from 4756 (91%) of the
stratum to the next in the log of the event RR) is then 5250 women in total (table 1, appendix pp 2, 6, 17). Trial
T/var(T), which has variance 1/var(T). Tests of whether entry year for participants was 1983–2002, median
two trends are the same involve subtraction of the follow-up was 9 years (IQR 5–14), with the last follow-up
corresponding trend test statistics from each other. in 2013, and median age was 49 years (43–57). 1604 deaths
A χ² statistic on one degree of freedom (χ²₁) for testing of occurred, including 248 (15%) without recurrence. Of the
whether some quantity Q differs significantly from zero 4756 women included in the analysis, 3838 (81%) were in
is given by Q/var(Q). A χ² test (on n–1 degrees of trials of regimens that included an anthracycline, one of
freedom) for heterogeneity can be obtained by subtracting which (902 women) also gave a taxane.13 Four trials
(O–E)²/V from the sum of the separate values, one per (918 women) used MMM (mitoxantrone, methotrexate,
stratum, of (o–e)²/v. For analyses by regression, we and mitomycin-C)11,12 or CMF (cyclophosphamide,
estimated RRs by maximum likelihood; tests for trend methotrexate, and fluorouracil)8,17 as NACT; in these
and heterogeneity were by likelihood ratio. trials, some chemotherapy in those allocated NACT was
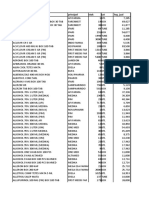
Trials Women (n) Deaths (n)† Median years per woman Woman-years by years since entry
(n)* (IQR) (thousands)
<10 10–19 ≥20 Total
No anthracycline or taxane8,11,12,17‡ 4 918 315 7·0 (4·2–9·3) 6·0 0·8 0·2 7·0
Anthracycline, no taxane9,10,14–16 5 2936 1163 10·2 (4·9–15·4) 22·1 7·7 <0·1 29·8
Anthracycline and taxane13 1 902 126 7·9 (5·0–10·7) 6·5 0·5 0 7·0
Total 10 4756 1604 8·6 (4·8–13·7) 34·6 9·0 0·2 43·7
*Data are missing for six small trials that randomised about 500 women, so they were not included in this analysis (appendix p 17). †Includes 1356 deaths with recurrence,
72 of unknown cause without recurrence, and 176 of known cause without recurrence. ‡In these trials, women allocated to the neoadjuvant group completed their
chemotherapy after surgery.
Table 1: Trials of neoadjuvant versus adjuvant chemotherapy that began by 2005
www.thelancet.com/oncology Vol 19 January 2018 29
Articles
given after surgery (table 1, appendix pp 3–4). No patients RR 1·28 [95% CI 1·06–1·55], p=0·01; figure 3A). However,
received trastuzumab. the RRs for local recurrence in these two sets of trials
Across all trials, NACT was associated with substantial were not significantly different (heterogeneity p=0·19).
tumour response (table 2), moderately increased use of Between-trial RRs for local recurrence ranged from
breast-conserving therapy in the NACT group compared 0·67 (95% CI 0·24–1·91) to 4·59 (1·19–17·8), but this
with the adjuvant chemotherapy group (figure 1), and an apparent heterogeneity was not significant (χ²10=11·8;
absolute increase in 15 year local recurrence of p=0·30; figure 4A). RRs for local recurrence also did
5·5% (95% CI 2·4–8·6; 21·4% for NACT vs 15·9% for not differ significantly between the three classes of
adjuvant chemotherapy), corresponding to a RR of chemotherapy used in these trials (figure 4, appendix
1·37 (95% CI 1·17–1·61; p=0·0001; figure 2A). The p 13), between trials in which chemotherapy in the NACT
incidence of local recurrence was significantly higher group was or was not completed after local therapy
with NACT than with adjuvant chemotherapy in years (appendix p 13), or between use or not of tamoxifen
0–4 (RR 1·35 [95% CI 1·11–1·64]; p=0·003) and (figure 5, appendix p 13).
5–9 (1·53 [1·08–2·17]; p=0·02), with few local recurrences We noted no significant differences between NACT and
after year 10. Sensitivity analyses indicated no substantial adjuvant treatment in 15 year distant recurrence (38·2% for
influence of competing risks from other breast events on NACT vs 38·0% for adjuvant chemotherapy; RR 1·02
the RRs for local recurrence (appendix p 18). [95% CI 0·92–1·14]; p=0·66), breast cancer death (34·4%
As anticipated,18,19 the absolute increase in 10-year local vs 33·7%; 1·06 [0·95–1·18]; p=0·31), or death from any
recurrence with NACT was largest in the two trials14,15 in cause (40·9% vs 41·2%; 1·04 [0·94–1·15]; p=0·45;
which, after NACT, many women did not have breast figure 2B, C, D). The RRs for these three outcomes did not
surgery (13·3% [95% CI 5·5–21·1]; 33·7% for NACT vs differ significantly between any subgroups of trials,
20·4% for adjuvant chemotherapy; RR 1·62 [95% CI including those for which use of surgery was or was not
1·20–2·19], p=0·002; figure 3B). In the other eight dependent on response to NACT, those using different
trials,8–13,16,17 surgery was scheduled irrespective of response types of chemotherapy, or those using or not using
to NACT, and the absolute increase in 10 year local tamoxifen (figure 3 C–F and figure 4B, appendix pp 7, 13).
recurrence was 3·2% (95% CI 0·6–5·8; 15·1% vs 11·9%; Three trials8,9,16 collected only first recurrence and death
rather than all events; however, sensitivity analyses
omitting these trials had no material effect on distant
Clinical response
recurrence estimates (appendix p 18). Mortality from
Complete* Partial† Stable or Unknown Total
causes other than breast cancer was no different between
progressive
disease‡ the NACT and adjuvant chemotherapy groups
(appendix p 7).
Planned breast-conserving therapy
Information about clinical tumour response was
Breast-conserving 215 (96%) 256 (90%) 119 (77%) 211 (81%) 801 (87%)
available for 1947 (82%) of 2387 patients allocated
Mastectomy 10 (4%) 30 (10%) 35 (23%) 48 (19%) 123 (13%)
NACT; 546 (28%) of 1947 had a complete response,
Unknown 0 0 0 2 (NA) 2 (NA)
803 (41%) of 1947 had a partial response, and
Total response§ 225/665 (34%) 286/665 (43%) 154/665 (23%) 261 (NA) 926 (100%)
598 (31%) of 1947 had stable or progressive disease
Planned mastectomy
(table 2, appendix p 8). The clinical tumour response to
Breast-conserving 75 (60%) 121 (41%) 30 (12%) 26 (36%) 252 (33%)
NACT affected surgical treatment decisions: more
Mastectomy 49 (40%) 175 (59%) 231 (88%) 47 (64%) 502 (67%)
women with a complete response had breast-conserving
Unknown 0 1 (NA) 2 (NA) 11 (NA) 14 (NA)
therapy (452 [83%] of 544) than did those with a partial
Total response§ 124/684 (18%) 297/684 (43%) 263/684 (38%) 84 (NA) 768 (100%)
response (541 [68%] of 799) or no response
Unknown planned therapy (246 [42%] of 588). Consequently, we noted an
Breast-conserving 162 (83%) 164 (76%) 97 (56%) 28 (49%) 451 (70%) imbalance by treatment group in the extent of surgery:
Mastectomy 33 (17%) 53 (24%) 76 (44%) 29 (51%) 191 (30%) although breast-conserving therapy was initially
Unknown 2 (NA) 3 (NA) 8 (NA) 38 (NA) 51 (NA) intended for equal numbers of patients in each group,
Total response§ 197/598 (33%) 220/598 (37%) 181/598 (30%) 95 (NA) 693 (100%) actual use of breast-preserving therapy (including no
All women surgery) was 1504 (65%) of 2320 in the NACT group
Breast-conserving 452 (83%) 541 (68%) 246 (42%) 265 (68%) 1504 (65%) versus 1135 (49%) of 2318 in the adjuvant chemotherapy
Mastectomy 92 (17%) 258 (32%) 342 (58%) 124 (32%) 816 (35%) group excluding patients with unknown surgeries
Unknown 2 (NA) 4 (NA) 10 (NA) 51 (NA) 67 (NA) (p<0·0001; figure 1, appendix pp 9, 10).
Total response§ 546/1947 (28%) 803/1947 (41%) 598/1947 (31%) 440 (NA) 2387 (100%) Figure 6 shows proportions of women with complete
clinical response according to patient and tumour
Data are n (%) or n/N (%). NA=not applicable. *No clinical evidence of disease. †≥50% reduction in tumour size.
‡<50% reduction or increase in tumour size. §Percentages are of those with a known response. characteristics. Complete response decreased with
increasing clinical tumour size (trend p<0·0001) and was
Table 2: Local therapy, planned versus done, in women allocated to neoadjuvant chemotherapy, by
higher with oestrogen receptor (ER)-negative biopsies
clinical response
than with ER-positive biopsies (p<0·0001) and with
30 www.thelancet.com/oncology Vol 19 January 2018
Articles
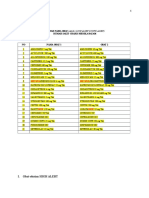
Number given BCT/women Ratio of BCT rates neoadjuvant:adjuvant Rate ratio of BCT
(95% CI)
Allocated Allocated
neoadjuvant adjuvant
Age at entry (years) (χ21=2·8; p=0·09)
<45 453/712 383/761 1·20 (1·11−1·30)
45−54 539/822 415/817 1·22 (1·13−1·31)
≥55 512/786 337/740 1·38 (1·27−1·51)
Clinical nodal status (χ21=6·3; p=0·01)
Negative 917/1338 730/1307 1·19 (1·12−1·25)
Positive 461/776 342/793 1·36 (1·24−1·49)
Unknown 126/206 63/218 2·11 (1·67−2·66)
Clinical tumour size (χ =43·1; p<0·0001)
2
1
1−19 mm 301/382 299/402 1·04 (0·97−1·12)
20−49 mm 1061/1547 746/1551 1·41 (1·33−1·50)
≥50 mm 124/337 71/323 1·68 (1·31−2·15)
Unknown 18/54 19/42 0·71 (0·43−1·15)
Biopsy ER and PR status (χ22=4·5; p=0·10)
ER+ and PR+ 226/343 150/345 1·51 (1·31−1·73)
ER+ and PR− 54/91 25/98 2·28 (1·57−3·31)
ER− and PR− 278/407 165/406 1·61 (1·42−1·84)
Unknown 946/1479 795/1469 1·13 (1·08−1·20)
Biopsy grade (χ21=2·5; p=0·12)
Well 32/66 17/60 1·67 (1·05−2·67)
Moderate 186/303 84/317 2·32 (1·90−2·84)
Poor 117/189 46/195 2·66 (2·02−3·50)
Unknown 1169/1762 988/1746 1·13 (1·08−1·18)
Biopsy grade and ER status (χ23=13·7; p=0·003)
Well or moderate, ER+ 141/237 77/234 1·78 (1·45−2·19)
Poor, ER+ 45/84 22/92 2·30 (1·53−3·47)
Well or moderate, ER− 76/128 21/138 3·86 (2·55−5·83)
Poor, ER− 71/104 24/103 2·85 (1·97−4·11)
Other or unknown 1171/1767 991/1751 1·15 (1·10−1·21)
Type of neoadjuvant chemotherapy (χ21=44·9; p<0·0001)
No anthracycline or taxane 329/446 292/439 1·07 (0·99−1·16)
Anthracycline, no taxane 891/1436 696/1438 1·24 (1·16−1·31)
Anthracycline and taxane 284/438 147/441 1·95 (1·68−2·25)
Planned local therapy (χ22=121·7; p<0·0001)
Radiotherapy only 167/200 144/190 1·10 (1·00−1·22)
Lumpectomy 634/724 623/735 1·03 (0·99−1·08)
Mastectomy 252/754 73/757 3·48 (2·74−4·43)
Unknown 451/642 295/636 1·53 (1·38−1·68)
Total 1504/2320 (64·8%) 1135/2318 (49·0%) 1·28 (1·22−1·34)
0·2 1·0 4·0
Lower frequency with NACT Higher frequency with NACT
Figure 1: BCT rate ratios
Numbers with BCT or mastectomy after chemotherapy. Excludes local therapy unknown (67 patients with NACT and 51 with adjuvant chemotherapies).
BCT=breast-conserving therapy. ER=oestrogen receptor. PR=progesterone receptor. NACT=neoadjuvant chemotherapy.
poorly differentiated tumours than with well or The strongest predictors of the effect of NACT on breast
moderately differentiated tumours (trend p=0·001, even conservation frequency were tumour size, planned local
after allowance for high-grade tumours tending to be ER therapy, and type of chemotherapy (all p<0·0001). The
negative), and was higher in the one trial13 that combined effect of NACT on surgery de-escalation was most
anthracycline and taxane therapy than in the other trials apparent among women with large (20–49 mm or
(p<0·0001). Age, nodal status, and planned local therapy ≥50 mm) tumours; we noted little effect of NACT on
did not affect response. breast conservation frequency in women with small
The proportion of women having breast-conserving (<20 mm) tumours. As expected, women with
therapy in various different subgroups in the NACT and mastectomy originally planned were more likely to have
adjuvant chemotherapy groups are shown in figure 1. lesser surgery than were those with breast-conserving
www.thelancet.com/oncology Vol 19 January 2018 31
Articles
A B
60 4756 women, 635 events 60 4756 women, 1562 events
15 year loss 5·5% (95% CI 2·4−8·6) 15 year loss 0·2% (95% CI −3·1 to 3·5)
RR 1·37 (95% CI 1·17−1·61) RR 1·02 (95% CI 0·92−1·14)
Log-rank p=0·0001 Log-rank p=0·66
50 50
NACT
Adjuvant Neoadjuvant
Distant recurrence at any time (%)
38·2%
40 40
33·8%
Local recurrence (%)
Adjuvant
38·0%
30 30 32·4%
Neoadjuvant 24·9%
21·4%
17·9%
20 20 23·5%
12·1%
Adjuvant
10 13·2% 15·9% 10
9·0%
0 0
0 5 10 15 0 5 10 15
Local recurrence crude rates (events per woman-years) Distant recurrence at any time crude rates (events per woman-years)
and log-rank analyses and log-rank analyses
Years 0−4 Years 5−9 Years 10−14 Years ≥15 Years 0−4 Years 5−9 Years 10−14 Years ≥15
Neoadjuvant 2·58 (245/9493) 1·43 (79/5528) 0·93 (26/2784) 2·16 (16/740) 5·69 (568/9983) 2·58 (162/6291) 1·49 (50/3351) 1·44 (14/974)
Adjuvant 1·95 (185/9477) 0·96 (54/5618) 0·69 (19/2769) 1·42 (11/772) 5·44 (535/9840) 2·54 (157/6187) 1·84 (60/3270) 1·74 (16/919)
Rate ratio 1·35 (1·11−1·64) 1·53 (1·08−2·17) 1·29 (0·70−2·38) 1·11 (0·48−2·57) 1·07 (0·94−1·21) 0·99 (0·79−1·24) 0·80 (0·55−1·18) 0·75 (0·35−1·61)
(95% CI) from 30·4/102·0 13·6/31·8 2·7/10·3 0·6/5·4 16·5/251·5 −0·6/75·5 −5·7/25·8 −1·9/6·7
(O−E)/V
C D
60 4756 women, 1329 deaths 60 4756 women, 1604 deaths
15 year loss 0·7% (95% CI −2·7 to 4·1) 15 year gain 0·3% (95% CI −3·2 to 3·8)
RR 1·06 (95% CI 0·95−1·18) RR 1·04 (95% CI 0·94−1·15)
Log-rank p=0·31 Log-rank p=0·45
50 50
Adjuvant
41·2%
Neoadjuvant
40 40
Breast cancer mortality (%)
34·4%
All-cause mortality (%)
31·9% Neoadjuvant
28·5% 40·9%
30 Adjuvant 30
33·7% 31·0%
26·6% 19·4%
18·1%
20 20
17·8%
16·2%
10 10
0 0
5 0 10 15 0 5 10 15
Time since trial entry (years) Time since trial entry (years)
Breast cancer mortality crude rates (events per woman-years) Any death crude rates (events per woman-years)
and log-rank analyses and log-rank analyses
Years 0−4 Years 5−9 Years 10−14 Years ≥15 Years 0−4 Years 5−9 Years 10−14 Years ≥15
Neoadjuvant 3·90 (412/10 567) 2·82 (191/6785) 1·93 (69/3570) 1·24 (13/1050) 4·22 (446/10 567) 3·51 (238/6785) 2·91 (104/3570) 3·52 (37/1050)
Adjuvant 3·49 (364/10 432) 2·81 (190/6771) 2·19 (78/3559) 1·18 (12/1014) 3·86 (403/10 432) 3·56 (241/6771) 3·20 (114/3559) 2·07 (21/1014)
Rate ratio 1·12 (0·97−1·30) 1·03 (0·84−1·27) 0·88 (0·63−1·21) 0·90 (0·41−1·97) 1·09 (0·95−1·25) 0·98 (0·81−1·17) 0·90 (0·68−1·18) 1·69 (0·95−2·99)
(95% CI) from 20·5/179·6 2·8/91·6 −4·8/36·6 −0·7/6·2 16·7/196·6 −2·7/112·2 −5·6/51·3 6·1/11·7
(O−E)/V
Figure 2: Effect of neoadjuvant versus adjuvant chemotherapy on recurrence and mortality
Local recurrence (A), distant recurrence (B), breast cancer mortality (C), and death from any cause (D). Three trials recorded causes of any deaths but only the first
breast cancer event. Hence, for these trials, distant recurrence includes the first distant recurrence as the first event and death from breast cancer. Error bars are
95% CIs. NACT=neoadjuvant chemotherapy. O–E=observed minus expected. RR=rate ratio. V=variance of O–E.
surgery originally planned. NACT with an anthracycline with other regimens. In women with node-positive
and taxane combination was also associated with disease, the rate ratio for BCT was higher than for those
substantially more surgery de-escalation than was NACT with node-negative disease (p=0·01). Despite the high
32 www.thelancet.com/oncology Vol 19 January 2018
Articles
A Surgery commonly used B Surgery less commonly used*
60 4094 women, 453 events 662 women, 182 events
10 year loss 3·2% (95% CI 0·6−5·8) 10 year loss 13·3% (95% CI 5·5−21·1)
RR 1·28 (95% CI 1·06−1·55) RR 1·62 (95% CI 1·20−2·19)
50
Log-rank p=0·010 Log-rank p=0·002
Neoadjuvant
NACT 33·7%
40
Local recurrence (%)
Adjuvant
24·5%
30
Neoadjuvant
20 15·1%
10·0% Adjuvant
10 Adjuvant 15·6% 20·4%
8·0% 11·9%
0
0 5 10 0 5 10
Local recurrence crude rates (events per woman-years) Local recurrence crude rates (events per woman-years)
and log-rank analyses and log-rank analyses
Years 0−4 Years 5−9 Years ≥10 Years 0−4 Years 5−9 Years ≥10
Neoadjuvant 2·12 (173/8164) 1·21 (57/4721) 0·85 (22/2577) 5·42 (72/1329) 2·73 (22/806) 2·11 (20/947)
Adjuvant 1·73 (142/8200) 0·94 (45/4778) 0·55 (14/2547) 3·37 (43/1277) 1·07 (9/840) 1·61 (16/994)
Rate ratio (95% CI) 1·26 (1·00−1·58) 1·35 (0·91−2·01) 1·32 (0·65−2·69) 1·63 (1·12−2·39) 2·30 (1·13−4·70) 1·15 (0·58−2·27)
from (O−E)/V 17·3/75·2 7·3/24·3 2·1/7·5 13·2/26·8 6·3/7·5 1·1/8·2
C Surgery commonly used D Surgery less commonly used*
60 4094 women, 1238 events 662 women, 324 events
10 year loss 1·8% (95% CI −1·4 to 5·0) 10 year gain 1·5% (95% CI −6·4 to 9·4)
RR 1·05 (95% CI 0·94−1·18) Adjuvant
RR 0·92 (95% CI 0·73−1·15)
50 43·5%
Distant recurrence at any time (%)
Log-rank p=0·38 Log-rank p=0·46
40 Neoadjuvant 32·1%
32·2%
Neoadjuvant
30 42·0%
24·1%
Adjuvant
30·4% 29·5%
20
22·0%
Figure 3: Time to recurrence
10 and breast cancer mortality
Local recurrence for surgery
0 commonly used (A) and less
0 5 10 0 5 10 commonly used (B), distant
Distant recurrence at any time crude rates (events per woman-years) Distant recurrence at any time crude rates (events per recurrence for surgery
and log-rank analyses woman-years) and log-rank analyses
commonly used (C) and less
Years 0−4 Years 5−9 Years ≥10 Years 0−4 Years 5−9 Years ≥10
Neoadjuvant 5·50 (470/8545) 2·29 (121/5284) 1·30 (40/3078) 6·81 (98/1438) 4·07 (41/1007) 1·92 (24/1248) commonly used (D), and
Adjuvant 5·07 (431/8496) 2·32 (122/5262) 1·77 (54/3050) 7·74 (104/1344) 3·78 (35/926) 1·93 (22/1139) breast cancer mortality for
Rate ratio (95% CI) 1·12 (0·97−1·28) 0·98 (0·75−1·26) 0·74 (0·49−1·13) 0·87 (0·65−1·17) 1·05 (0·66−1·68) 0·91 (0·50−1·66) surgery commonly used (E)
from (O−E)/V 22·8/205·9 −1·4/58·0 −6·6/21·8 –6·3/45·6 0·8/17·5 –1·0/10·7 and less commonly used (F).
Heterogeneity by surgery use:
E Surgery commonly used FF Surgery less commonly used*
local recurrence p=0·19,
60 4094 women, 1055 deaths 662 women, 274 deaths
distant recurrence p=0·29, and
10 year loss 2·7% (95% CI −0·3 to 5·7) 10 year gain 2·1% (95% CI −5·5 to 9·7)
RR 1·09 (95% CI 0·97−1·24) RR 0·93 (95% CI 0·73−1·19) breast cancer mortality
50 Log-rank p=0·15 Log-rank p=0·56 p=0·24. Error bars are 95% CIs.
Adjuvant
NACT=neoadjuvant
Breast cancer mortality (%)
35·4%
40 chemotherapy. O–E=observed
Neoadjuvant minus expected. RR=rate ratio.
27·5% V=variance of O–E. Three trials
30
19·7% recorded causes of any deaths
Neoadjuvant but only the first breast cancer
18·3% 33·3%
20 Adjuvant event. Hence, for these trials,
24·8% distant recurrence includes the
10 15·6% 16·6% first distant recurrence as the
first event and death from
breast cancer. *Includes
0
5 0 10 0 5 10 Institut Bergonié Bordeaux14
Time since trial entry (years) Time since trial entry (years) (in NACT group, 33% had
Breast cancer mortality crude rates (events per woman-years) Breast cancer mortality crude rates (events per woman-years) radiotherapy alone) and
and log-rank analyses and log-rank analyses Institut Curie S615 (in NACT
Years 0−4 Years 5−9 Years ≥10 Years 0−4 Years 5−9 Years ≥10 group, 51% had radiotherapy
Neoadjuvant 3·95 (356/9007) 2·48 (139/5610) 1·65 (53/3206) 3·59 (56/1560) 4·43 (52/1175) 2·05 (29/1414) alone; in adjuvant
Adjuvant 3·37 (301/8944) 2·49 (141/5662) 2·01 (65/3237) 4·23 (63/1488) 4·42 (49/1109) 1·87 (25/1336) chemotherapy group,
Rate ratio (95% CI) 1·19 (1·01−1·39) 1·03 (0·81−1·31) 0·82 (0·57−1·17) 0·81 (0·56−1·18) 1·03 (0·69−1·53) 1·03 (0·60−1·79)
from (O−E)/V
46% had radiotherapy alone)
26·4/152·1 2·1/67·4 −6·0/30·0 −5·8/27·6 0·7/24·2 0·4/12·9
trials.
www.thelancet.com/oncology Vol 19 January 2018 33
Articles
A Events/women Neoadjuvant events Ratio of annual event rates neoadjuvant:adjuvant
Preoperative vs postoperative Allocated Allocated Log-rank Variance
chemotherapy* neoadjuvant adjuvant O−E of O−E
Trials where preoperative chemotherapy included neither anthracyclines nor taxanes
BCCA Vancouver17 1C600M40F600 10/42 3/39 3·2 2·1
St George’s London¹² 4Mz7M35Mit7 11/53 8/50 1·5 4·3
RMH London 11 4Mz7M35Mit7 7/155 8/150 −1·4 3·5
Austrian BCSG VII⁸ 3C600×2M40×2F600×2 16/142 12/137 1·6 6·8
Austrian BCSG VII⁸ 3C600×2M40×2F600×2 11/74 4/76 3·8 3·5
Subtotal 55/466 (11·8%) 35/452 (7·7%) 8·8 20·2
1·55 (1·00−2·39); p=0·05
Trials using anthracyclines but not taxanes
IB Bordeaux14 3E50Vc1000M20; 3Mit10Tt20Vd4000 39/134 18/138 11·1 13·6
Institut Curie S615 4F500A25C500 75/200 50/190 9·5 28·9
NSABP B-189 4A60C600 124/760 105/763 9·0 55·1
NCI Bethesda16 5F400×3Fol500×3A15×3C600 2/26 1/27 0·1 0·5
EORTC 1090210 4F600E60C600 33/350 30/348 3·9 14·9
Subtotal 273/1470 (18·6%) 204/1466 (13·9%) 33·5 113·0
1·35 (1·12−1·62); p=0·002
Trials using anthracyclines and taxanes
ECTO Italy13 4E60P200; 4C600×2M40×2F600×2 38/451 30/451 4·9 16·4
Subtotal 38/451 (8·4%) 30/451 (6·7%) 4·9 16·4
1·35 (0·83−2·19); p=0·22
Total 366/2387 (15·3%) 269/2369 (11·4%) 47·2 149·5
99% CI 95% CI 1·37 (1·17−1·61); p=0·0001
Heterogeneity between three subtotals: χ22=0·3; p=0·85
Heterogeneity within subtotals: χ28=11·5; p=0·18
Heterogeneity between 11† trials: χ210=11·8; p=0·30
B
Trials where preoperative chemotherapy included neither anthracyclines nor taxanes
BCCA Vancouver¹⁷ 1C600M40F600 20/42 20/39 0·4 8·0
St George’s London¹² 4Mz7M35Mit7 19/53 17/50 0·6 8·0
RMH London 11 4Mz7M35Mit7 37/155 41/150 −5·0 17·8
Austrian BCSG VII⁸ 3C600×2M40×2F600×2 37/142 25/137 5·6 14·3
Austrian BCSG VII⁸ 3C600×2M40×2F600×2 23/74 23/76 1·2 10·3
Subtotal 136/466 (29·2%) 126/452 (27·9%) 2·8 58·4
1·05 (0·81−1·36); p=0·72
Trials using anthracyclines but not taxanes
IB Bordeaux14 3E50Vc1000M20; 3Mit10Tt20Vd4000 66/134 65/138 0·7 30·7
Institut Curie S615 4F500A25C500 97/200 96/190 −7·1 43·1
NSABP B-189 4A60C600 256/760 264/763 −5·4 122·7
NCI Bethesda16 5F400×3Fol500×3A15×3C600 3/26 7/27 −1·5 2·1
EORTC 1090210 4F600E60C600 139/350 122/348 11·1 59·3
Subtotal 561/1470 (38·2%) 554/1466 (37·8%) −2·2 258·0
0·99 (0·88−1·12); p=0·89
Trials using anthracyclines and taxanes
ECTO Italy13 4E60P200; 4C600×2M40×2F600×2 97/451 88/451 7·8 43·2
Subtotal 97/451 (21·5%) 88/451 (19·5%) 7·8 43·2
1·20 (0·89−1·62); p=0·23
Total 794/2387 (33·3%) 768/2369 (32·4%) 8·4 359·5
1·02 (0·92−1·14); p=0·66
99% CI 95% CI
Heterogeneity between three subtotals: χ =1·4; p=0·50
2
2 0·5 1·0 2·5
Heterogeneity within subtotals: χ28=8·2; p=0·42
Neoadjuvant better Adjuvant better
Heterogeneity between 11† trials: χ210=9·5; p=0·48
Figure 4: Rate ratios for the effect of neoadjuvant versus adjuvant chemotherapy on recurrence by trial
(A) Local recurrence. (B) Distant recurrence. Three trials recorded causes of any deaths but only the first breast cancer event. Hence, for these trials, distant recurrence includes the first distant recurrence
as the first event and death from breast cancer. The appendix (pp 3–4) contains a full description of each trial’s chemotherapy regimen. A=doxorubicin (adriamycin). BCCA=British Columbia Cancer
Agency. BCSG=Breast Cancer Study Group. C=cyclophosphamide. E=epirubicin. ECTO=European Cooperative Trial in Operable Breast Cancer. EORTC=European Organisation for Research and Treatment
of Cancer. F=fluorouracil. Fol=folinic acid. IB=Institut Bergonié. M=methotrexate. Mit=mitomycin-C. Mz=mitoxantrone. NCI=National Cancer Institute. NSABP=National Surgical Adjuvant Breast and
Bowel Project. O–E=observed minus expected. P=paclitaxel. Tt=thiotepa. Vc=vincristine. Vd=vindesine. *Chemotherapy regimens given preoperatively in those allocated neoadjuvant and
postoperatively in those allocated adjuvant chemotherapy. The number of cycles, agents, and drug doses (in mg/m) per cycle are given. †The Austrian BCSG VII trial8 has two entries to take into
account the two postoperative chemotherapies given to both randomised groups (appendix pp 3–4).
34 www.thelancet.com/oncology Vol 19 January 2018
Articles
frequency of clinical response in patients with breast-conserving frequencies. Age was not associated
ER-negative and poorly differentiated tumours, ER status with the freqeuncy of breast-conserving therapy.
and tumour grade were not associated with frequency of If the increased local recurrence in the NACT groups
breast-conserving therapy, although after accounting for (figure 3) is due to de-escalation of local therapy from
grade, ER-negative women did appear to have higher mastectomy to breast-conserving therapy, the RR for the
Events/women Ratio of annual event rates Rate ratio
neoadjuvant:adjuvant (95% CI)
Allocated Allocated
neoadjuvant adjuvant
Age at entry (years) (χ21=0·2; p=0·68)
<45 150/729 108/785 1·49 (1·16−1·92)
45−54 127/849 101/830 1·23 (0·94−1·60)
≥55 89/809 60/754 1·41 (1·02−1·95)
Clinical nodal status (χ21=0·2; p=0·66)
Negative 172/1349 135/1314 1·26 (1·00−1·58)
Positive 136/796 104/801 1·36 (1·05−1·76)
Unknown 58/242 30/254 1·95 (1·26−3·03)
Clinical tumour size (χ21=0·2; p=0·62)
1−19 mm 60/384 39/405 1·62 (1·06−2·48)
20−49 mm 233/1576 177/1559 1·28 (1·05−1·56)
≥50 mm 67/345 49/327 1·38 (0·92−2·07)
Unknown 6/82 4/78 1·25 (0·16−9·86)
Biopsy ER and PR status (χ22=0·1; p=0·96)
ER+ and PR+ 60/351 37/347 1·72 (1·14−2·59)
ER+ and PR− 20/100 16/98 1·72 (0·81−3·65)
ER− and PR− 76/425 41/413 1·85 (1·25−2·72)
Unknown 210/1511 175/1511 1·20 (0·98−1·48)
Biopsy grade (χ21=3·9; p=0·05)
Well 5/67 1/60 2·52 (0·45−14·04)
Moderate 54/312 26/321 2·16 (1·37−3·40)
Poor 15/198 20/196 0·90 (0·44−1·83)
Unknown 292/1810 222/1792 1·30 (1·09−1·55)
Biopsy grade and ER status (χ21=0·1; p=0·76)
Well or moderate, ER+ 27/244 14/235 1·98 (1·04−3·78)
Poor, ER+ 8/89 10/92 0·92 (0·34−2·53)
Well or moderate, ER− 31/131 13/141 2·58 (1·38−4·84)
Poor, ER− 7/108 10/104 0·97 (0·35−2·73)
Other or unknown 293/1815 222/1797 1·31 (1·09−1·56)
Type of neoadjuvant chemotherapy (χ22=0·3; p=0·84)
No anthracycline or taxane 55/466 35/452 1·55 (1·00−2·39)
Anthracycline, no taxane 273/1470 204/1466 1·35 (1·12−1·62)
Anthracycline and taxane 38/451 30/451 1·35 (0·83−2·19)
Planned local therapy (χ22=3·3; p=0·20)*
Radiotherapy only† 75/200 50/190 1·39 (0·96−2·00)
Lumpectomy 108/726 96/737 1·14 (0·86−1·52)
Mastectomy 125/768 79/762 1·66 (1·24−2·21)
Unknown 58/693 44/680 1·26 (0·84−1·90)
Period of follow-up (woman-years) (χ21=0·1; p=0·72)
Years 0–1 124/4421 97/4371 1·26 (0·96−1·65)
Years 2–4 121/5072 88/5106 1·45 (1·10−1·91)
Years 5–9 79/5528 54/5618 1·53 (1·08−2·17)
Years ≥10 42/3524 30/3542 1·22 (0·75−2·00)
Total 366/2387 (15·3%) 269/2369 (11·4%) 1·37 (1·17−1·61)
p=0·0001
0·5 1·0 2·5
Neoadjuvant better Adjuvant better
Figure 5: Local recurrence rate ratios
For lumpectomy versus mastectomy, χ²1=3·3; p=0·07. ER=oestrogen receptor. PR=progesterone receptor. *408 women with missing data had planned local therapy
imputed (appendix p 9). †Refers to Institut Curie S615 (appendix p 9).
www.thelancet.com/oncology Vol 19 January 2018 35
Articles
% (CR/total) CR rate ratio Rate ratio for clinical
CR (95% CI)
Age at entry (years) (χ21=0·7; p=0·40)
<45 29·8 (164/550) 1·04 (0·90−1·21)
45−54 29·0 (196/675) 1·03 (0·94−1·13)
≥55 25·8 (186/722) 0·90 (0·78−1·03)
Clinical nodal status (χ21=0·8; p=0·37)
Negative 28·6 (326/1138) 0·97 (0·88−1·07)
Positive 27·2 (168/617) 1·04 (0·93−1·16)
Unknown 27·1 (52/192) 1·14 (0·57−2·26)
Clinical tumour size (χ21=37·5; p<0·0001)
1−19 mm 34·6 (117/338) 1·27 (1·09−1·48)
20−49 mm 29·7 (390/1312) 0·99 (0·91−1·07)
≥50 mm 13·3 (35/264) 0·47 (0·35−0·64)
Unknown 12·1 (4/33) 0·66 (0·28−1·58)
Biopsy ER and PR status (χ22=21·8; p<0·0001)
ER+ and PR+ 31·9 (83/260) 0·77 (0·64−0·92)
ER+ and PR− 26·6 (21/79) 0·71 (0·50−1·02)
ER− and PR− 35·5 (117/330) 1·24 (1·09−1·41)
Unknown 25·4 (325/1278) 0·73 (0·49−1·08)
Biopsy grade (χ21=10·3; p=0·001)
Well 20·9 (14/67) 0·58 (0·36−0·91)
Moderate 36·0 (108/300) 0·93 (0·80−1·07)
Poor 44·6 (83/186) 1·15 (0·98−1·34)
Unknown 24·5 (341/1394) 1·08 (0·66−1·76)
Biopsy grade and ER status (χ23=16·9; p=0·0007)
Well or moderate, ER+ 31·4 (74/236) 0·76 (0·63−0·92)
Poor, ER+ 34·9 (29/83) 0·88 (0·66−1·17)
Well or moderate, ER− 37·2 (48/129) 1·04 (0·84−1·29)
Poor, ER− 52·9 (54/102) 1·32 (1·11−1·56)
Other or unknown 24·4 (341/1397) 0·88 (0·53−1·48)
Type of neoadjuvant chemotherapy (χ21=49·0; p<0·0001)
No anthracycline or taxane 18·5 (69/373) 0·36 (0·23−0·55)
Anthracycline, no taxane 26·0 (293/1125) 0·64 (0·47−0·87)
Anthracycline and taxane 41·0 (184/449) 1·13 (1·01−1·25)
Planned local therapy (χ21=0·3; p=0·57)
Radiotherapy only No response information
Lumpectomy 33·8 (225/665) 1·02 (0·91−1·14)
Mastectomy 18·1 (124/684) 0·97 (0·78−1·20)
Unknown 32·9 (197/598) 0·90 (0·64−1·25)
Total 28·0 (546/1947)
0·2 1·0 6·0
Clinical CR
Figure 6: Clinical complete response rate ratios
Three trials are excluded, as individual responses are not available; 440 women have missing clinical response data. CIs are group specific.25 Rate ratios are scaled such
that, within each category, their inverse variance-weighted sum is 1—ie, ratios are with respect to the mean CR. The appendix (p 6) contains data available for each
trial. CR=complete response. ER=oestrogen receptor. PR=progesterone receptor.
effect on local recurrence of allocation to NACT should be was for RRs in the subgroup by planned local therapy
greatest in women for whom mastectomy was originally (figure 5); although the p value for the trend in RR with
planned. 252 (33%) of 754 women converted from planned biopsy grade was 0·05, this p value could have been a
mastectomy to breast-conserving therapy. However, chance finding given that it was the most extreme from
although the RR for local recurrence among all women many subgroup analyses. Despite surgery de-escalation
planned to have a mastectomy was 1·66 (95% CI 1·24–2·21) being more common in larger tumours than in smaller
compared with 1·14 (0·86–1·52) for women with tumours, and in the trial combining anthracycline and
lumpectomy planned, the two-tailed test for heterogeneity taxane13 than in trials of other regimens, the proportional
was not significant (p=0·07; figure 5, appendix pp 11, 12). increases in local recurrence did not vary significantly by
Heterogeneity between the RRs for local recurrence tumour size or chemotherapy regimen (figure 5).
was lower across all other tumour characteristics than it RRs also did not differ by age, nodal status, ER or
36 www.thelancet.com/oncology Vol 19 January 2018
Articles
progesterone receptor status, or period of follow-up. surgery could be avoided completely in the event of a
Patient-level data for radiotherapy were not available, and complete clinical response to NACT. This apparent
trial-level data for radiotherapy intent and practice were heterogeneity of effect was, however, not significant, and
incomplete (appendix p 2), so the effect of radiotherapy NACT appeared to also have resulted in some increase in
on local recurrence cannot be studied. Radiotherapy was local recurrence in the aggregated results from the eight
scheduled for most women who had breast-conserving other trials. Hence, the increased local recurrence with
surgery and actual use of radiotherapy was more frequent NACT is not wholly explained by omission of surgery.
in the NACT than in the adjuvant therapy groups Other unexamined factors might also have contributed to
(appendix p 2). The RRs for distant recurrence and breast the increased local recurrence with NACT. For example,
cancer mortality did not vary by any tumour factor after NACT, tumour localisation can be difficult28 and
measured, type of chemotherapy, timing of chemotherapy response patterns can be heterogeneous,29 making
use in the NACT group, type of planned local therapy, or surgery technically more difficult than without use of
period of follow-up (appendix p 13). NACT. Differing use of radiotherapy or axillary surgery
As expected, distant recurrence and breast cancer in the NACT group might also have contributed to
mortality were substantially lower in complete the higher local recurrence, although patient-level
responders than in non-responders (appendix p 14). information about this factor was not available. Trial
However, women who had a complete clinical response reports indicate that radiotherapy was scheduled for
after NACT had a frequency of local recurrence similar to most women who had breast-conserving surgery and
that of partial responders or non-responders. Ordering of that actual use of radiotherapy was, if anything, more
trials by the percentage of patients with a complete frequent in the NACT than in the adjuvant therapy
clinical response to NACT did not reveal any significant groups. Thus, lesser use of radiotherapy after NACT than
trend of improved recurrence or breast cancer mortality that without NACT is unlikely to explain this increase in
RRs in trials with a higher frequency of response local recurrence. Indeed, even with radiotherapy, local
(appendix p 16). No patterns emerged between trials in failure is higher after breast-conserving surgery than
complete response when considering the year that the after mastectomy without radiotherapy.30
trial started or the frequency of breast-conserving therapy Our finding of an overall increase in local recurrence in
within a trial (appendix p 15). the trials using optimal local treatment is at odds with a
meta-analysis18 based on published data rather than
Discussion individual patient data, but this discrepancy could be
In early breast cancer, high frequencies of complete or because the meta-analysis included comparisons that were
partial clinical response can be achieved with NACT, confounded by differing background systemic therapy.
which can lead to a higher frequency of breast-conserving Tumour response is predictive of lower distant
therapy than with adjuvant chemotherapy. However, we recurrence and death than an absence of tumour response.
found NACT to be associated with a higher frequency of Compared with all women randomly allocated to adjuvant
local recurrence than was the same chemotherapy chemotherapy, outcomes were better for those with a
started after surgery. Reassuringly, the increase in local complete clinical response after NACT than for those with
recurrence was not associated with any significant a partial response and far better than for those with little
increase in distant recurrence or breast cancer mortality. or no response to NACT. However, even in trials with high
More than two thirds of patients receiving NACT frequencies of complete response, NACT was not
responded, with more than a quarter achieving complete significantly better than adjuvant chemotherapy with
clinical response, despite some trials using old respect to distant recurrence or breast cancer mortality.
chemotherapy regimens and four administering some of This finding could be because tumour characteristics that
the chemotherapy postoperatively. The one regimen that are associated with higher response—such as smaller
included both anthracycline and taxane had the highest tumour size—are also associated with lower distant
frequency of complete response. Within trials, response recurrence and are balanced between the NACT and
was more common in women with small, ER-negative adjuvant groups by random isation. In each trial, both
and progesterone receptor-negative, or high-grade groups eventually receive the same chemotherapy, so any
tumours, as measured before randomisation, but was differences between trials in the efficacy of chemotherapy
little affected by age, nodal status, or planned local regimens will apply to both groups. The CTNeoBC study6
therapy.8–17 As expected, use of NACT was associated with reported similar findings in that efficacy as assessed by
an increase in the use of breast-conserving therapy. high pathological complete response at the trial level did
An increase in the use of breast-conserving therapy in not correlate well with long-term efficacy.
women who responded well to NACT and who would A limitation of our meta-analysis is that we have not
otherwise have had mastectomy is a likely explanation been able to assess reliably whether presurgical systemic
for the increase in local recurrence in patients allocated therapy is more effective at eradicating micrometastatic
NACT. As anticipated,18,19 the absolute increase in local disease than the same chemotherapy administered after
recurrence was greatest in the two trials14,15 in which recovery from surgery because of the confounding
www.thelancet.com/oncology Vol 19 January 2018 37
Articles
effect of differences in the extent of surgery between P McGale, R Gray, and R Peto designed and carried out the analyses with
women allocated NACT and those allocated adjuvant computing assistance from Y Wang and Z Wang. P McGale, D Dodwell,
R Gray, G von Minckwitz, R Peto, and C Taylor drafted the report with
chemotherapy. A large trial with the same surgery and advice from S Anderson, J Bergh, L Gianni, C Lohrisch, and
radiotherapy in the NACT and adjuvant chemotherapy K I Pritchard. All writing committee members contributed to revising
groups could assess this question. At present, we cannot the report. Interim analyses were discussed by the steering committee
exclude the possibility that NACT does moderately and trialists who supplied data for the analysis.
reduce distant recurrence compared with the same Writing committee
chemotherapy given postoperatively, but that this P McGale, D Dodwell, R Gray, G Mannu, R Peto, C Taylor, Y Wang,
Z Wang, M Clarke, C Davies, R Bradley, J Braybrooke, H Pan (Medical
benefit was obscured by an increase in local recurrence Research Council Population Health Research Unit, Nuffield
due to less extensive surgery after NACT than in Department of Population Health, University of Oxford, Oxford, UK);
patients who did not receive NACT. Trials of radiotherapy C Lohrisch (Breast Cancer Outcomes Unit, British Columbia Cancer
after surgery indicate that substantially decreasing local Agency, Vancouver, BC, Canada); L Gianni (Istituto Nazionale Tumori,
Milan, Italy); S Anderson (Department of Biostatistics, University of
recurrence does also decrease breast cancer mortality, Pittsburgh Graduate School of Public Health, Pittsburgh, PA, USA);
with about one breast cancer death prevented for every K I Pritchard (Sunnybrook Odette Cancer Centre, Toronto, ON, Canada;
four local recurrences prevented.30 The small, J Bergh (Karolinska Institutet and University Hospital, Stockholm,
non-significant excess of breast cancer mortality in Sweden); G von Minckwitz (German Breast Group, Neu-Isenburg,
Germany).
patients allocated NACT is consistent with this risk
Groups (and key trialists) contributing data
ratio, so could therefore be due to the increase in local
Istituto Nazionale per lo Studio e la Cura dei Tumori, Milan, Italy
recurrence, but it could equally well be a chance finding. (P Valagussa, L Gianni, G Bonadonna); European Organisation for
The main aim of NACT in contemporary practice is to Research on the Treatment of Cancer (J Bogaerts, J van der Hage,
reduce the extent of breast surgery, thereby making C J H van de Velde); Austrian Breast and Colorectal Cancer Study
Group, Vienna, Austria (L Solkner, M Gnant, R Jakesz); Center for
breast conservation feasible in women who would
Cancer Research of the National Cancer Institute, Bethesda, MD,
otherwise need mastectomy. In the time since the trials USA. (S Steinberg, D Danforth, J Zujewski); Royal Marsden Hospital,
in this meta-analysis were done, pathology reporting, Sutton, London, UK (T Powles, S Ashley, H Ford, M Makris);
surgery, and radiotherapy have improved, and more St George’s Hospital, London, UK (J-C Gazet, C Coombes,
R Sutcliffe); National Surgical Adjuvant Breast & Bowel Project,
effective systemic neoadjuvant regimens have been
Pittsburgh, PA, USA (S Anderson, J Costantino, J Bryant, N Wolmark,
introduced than were available when these trials took E Mamounas, B Fisher); Fondation Bergonié—Comprehensive Cancer
place. These changes should increase the likelihood of Centre of South West France, Bordeaux, France (L Mauriac,
successful downstaging to allow conservative surgery in S Mathoulin); Cancer Control Agency of British Columbia, BC,
Canada (J Ragaz, I Olivotto); Institut Curie, Paris, France (B Asselain,
current and future practice. But, although improvements P Broet, S Scholl).
in treatment mean local recurrence risk should be lower
EBCTCG steering committee
than in these trials, our findings indicate that tumours J Bergh, K I Pritchard (co-chairs), K Albain, S Anderson, R Arriagada,
downsized by NACT might continue to be associated W Barlow, J Bartlett, E Bergsten-Nordström, J Bliss, F Boccardo,
with higher local recurrence risk after breast-conserving R Bradley*, E Brain, J Braybrooke*, D Cameron, M Clarke*, A Coates,
surgery than might tumours of the same dimensions R Coleman, C Correa, J Costantino, J Cuzick, N Davidson, C Davies*,
L Davies*, A Di Leo, D Dodwell*, M Dowsett, F Duane*, M Ewertz,
in women who have not received NACT. Strategies J Forbes, R Gelber, M Gnant, A Goldhirsch, P Goodwin, R Gray*,
to mitigate the increased local recurrence after D Hayes, C Hill, J Ingle, R Jagsi, W Janni, Z Liu*, S Loibl,
breast-conserving therapy in tumours downsized by E MacKinnon*, G Mannu*, M Martín, P McGale*, H Mukai, L Norton,
NACT should be considered—for example, careful Y Ohashi, S Paik, H Pan*, R Peto*, M Piccart, L Pierce, P Poortmans,
V Raina, P Ravdin, M Regan, J Robertson, E Rutgers, D Slamon,
tumour localisation, detailed pathological assessment, J Sparano, S Swain, C Taylor*, A Tutt, G Viale, G von Minckwitz,
and appropriate radiotherapy.31 Prospective randomised X Wang, T Whelan, N Wilcken, E Winer, N Wolmark, W Wood,
trials would also help to establish the optimal clinical M Zambetti. *EBCTCG Secretariat, Population Health Research Unit.
management in this context. Declaration of interests
NACT allows more breast-conserving therapy than The writing committee and EBCTCG secretariat declare no competing
does adjuvant chemotherapy and provides information interests.
about an individual patient’s response to a particular Acknowledgments
This study is supported by core funding to the Population Health
chemotherapy regimen. However, it appears to be no
Research Unit and Clinical Trial Service Unit, Nuffield Department of
better than postoperative adjuvant treatment at reducing Population Health, University of Oxford, from Cancer Research UK,
breast cancer mortality and, perhaps as a consequence of the British Heart Foundation, and the UK Medical Research Council, as
a reduction of the extent of surgery, NACT is associated well as by the UK Department of Health grant RRX108 and Cancer
Research UK grant C8225/A21133. The chief acknowledgement is to the
with moderately increased local recurrence risk, which
women in these trials and the trial personnel.
persists for at least 10 years.
References
Contributors 1 Rubens RD, Sexton S, Tong D, Winter PJ, Knight RK, Hayward JL.
The EBCTCG secretariat (C Boddington, R Bradley, J Burrett, M Clarke, Combined chemotherapy and radiotherapy for locally advanced
C Davies, L Davies, D Dodwell, F Duane, V Evans, L Gettins, J Godwin, breast cancer. Eur J Cancer 1980; 16: 351–56.
R Gray, S James, H Liu, Z Liu, E MacKinnon, G Mannu, P McGale, 2 Mougalian SS, Soulos PR, Killelea BK, et al. Use of neoadjuvant
T McHugh, P Morris, H Pan, R Peto, S Read, C Taylor, Y Wang, and chemotherapy for patients with stage I to III breast cancer in the
Z Wang) identified trials, obtained datasets, and had full access to them. United States. Cancer 2015; 121: 2544–52.
38 www.thelancet.com/oncology Vol 19 January 2018
Articles
3 Clough KB, Acosta-Marín V, Nos C, et al. Rates of neoadjuvant 18 Mieog JS, van der Hage JA, van De Velde CJ. Neoadjuvant
chemotherapy and oncoplastic surgery for breast cancer surgery: chemotherapy for operable breast cancer. Br J Surg 2007;
a French national survey. Ann Surg Oncol 2015; 11: 3504–11. 94: 1189–200.
4 Vugts G, Maaskant-Braat AJ, Nieuwenhuijzen GA, Roumen RM, 19 Mauri D, Pavlidis N, Ioannidis JP. Neoadjuvant versus adjuvant
Luiten EJ, Voogd AC. Patterns of care in the administration of systemic treatment in breast cancer: a meta-analysis.
neoadjuvant chemotherapy for breast cancer. A population-based J Natl Cancer Inst 2005; 97: 188–94.
study. Breast J 2016; 22: 316–21. 20 Feinstein AR, Fosin DM, Wells CK. The Will Rogers phenomenon
5 Fisher B, Gunduz N, Coyle J, Rudock C, Saffer E. Presence of a stage migration and new diagnostic techniques as a source of
growth-stimulating factor in serum following primary tumor misleading statistics for survival in cancer. N Engl J Med 1985;
removal in mice. Cancer Res 1989; 49: 1996–2001. 312: 1604–08.
6 Cortazar P, Zhang L, Untch M, et al. Pathological complete 21 Bear HD, Anderson S, Smith RE, et al. Sequential preoperative or
response and long-term clinical benefit in breast cancer: postoperative docetaxel added to preoperative doxorubicin plus
the CTNeoBC pooled analysis. Lancet 2014; 384: 164–72. cyclophosphamide for operable breast cancer: National Surgical
7 von Minckwitz G, Blohmer JU, Costa SD, et al. Response-guided Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol 2004;
neoadjuvant chemotherapy for breast cancer. J Clin Oncol 2013; 24: 2019–27.
31: 3623–30. 22 Early Breast Cancer Trialists’ Collaborative Group. Treatment of
8 Taucher S, Steger GG, Jakesz R, et al. The potential risk of early breast cancer. Volume 1, worldwide evidence 1985–1990.
neoadjuvant chemotherapy in breast cancer patients—results from Oxford: Oxford University Press, 1990.
a prospective randomized trial of the Austrian Breast and Colorectal 23 Early Breast Cancer Trialists’ Collaborative Group. Comparisons
Cancer Study Group (ABCSG-07). Breast Cancer Res Treat 2008; between different polychemotherapy regimens for early breast
112: 309–16. cancer: meta-analyses of long-term outcome among 100 000 women
9 Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative in 123 randomised trials. Lancet 2012; 379: 432–44.
chemotherapy in patients with operable breast cancer: nine-year 24 Stewart LA, Clarke M, Rovers M, et al. Preferred Reporting Items
results from National Surgical Adjuvant Breast and Bowel Project for a Systematic Review and Meta-analysis of individual participant
B-18. J Natl Cancer Inst Monogr 2001; 30: 96–102. data: the PRISMA-IPD Statement. JAMA 2015; 313: 1657–65.
10 van der Hage JA, van de Velde CJ, Julien JP, Tubiana-Hulin M, 25 Plummer M. Improved estimates of floating absolute risk. Stat Med
Vandervelden C, Duchateau L. Preoperative chemotherapy in 2004; 23: 93–104.
primary operable breast cancer: results from the European 26 Early Breast Cancer Trialists’ Collaborative Group. Effects of
Organization for Research and Treatment of Cancer trial 10902. chemotherapy and hormonal therapy for early breast cancer on
J Clin Oncol 2001; 19: 4224–37. recurrence and 15-year survival: an overview of the randomised
11 Powles TJ, Hickish TF, Makris A, et al. Randomized trial of trials. Lancet 2005; 365: 1687–717.
chemoendocrine therapy started before or after surgery for 27 Gelman R, Gelber R, Henderson IC, Coleman CN, Harris JR.
treatment of primary breast cancer. J Clin Oncol 1995; 13: 547–52. Improved methodology for analyzing local and distant recurrence.
12 Gazet JC, Ford HT, Gray R, et al. Estrogen-receptor-directed J Clin Oncol 1990; 8: 548–55.
neoadjuvant therapy for breast cancer: results of a randomised trial 28 Baron LF, Baron PL, Ackerman SJ, Durden DD, Pope TL Jr.
using formestane and methotrexate, mitozantrone and mitomycin Sonographically guided clip placement facilitates localization of
C (MMM) chemotherapy. Ann Oncol 2001; 12: 685–91. breast cancer after neoadjuvant chemotherapy. AJR Am J Roentgenol
13 Gianni L, Baselga J, Eiermann W, et al. A. Phase III trial evaluating 2000; 174: 539–40.
the addition of paclitaxel to doxorubicin followed by 29 von Minckwitz G, Untch M, Blohmer JU, et al. Definition and
cyclophosphamide, methotrexate, and fluorouracil, as adjuvant or impact of pathologic complete response on prognosis after
primary systemic therapy: European Cooperative Trial in Operable neoadjuvant chemotherapy in various intrinsic breast cancer
Breast Cancer. J Clin Oncol 2009; 27: 2474–81. subtypes. J Clin Oncol 2012; 30: 1796–804.
14 Mauriac L, MacGrogan G, Avril A, et al. Neoadjuvant chemotherapy 30 Early Breast Cancer Trialists’ Collaborative Group. Effects of
for operable breast carcinoma larger than 3 cm: a unicentre radiotherapy and of differences in the extent of surgery for early
randomized trial with a 124-month median follow-up. Ann Oncol breast cancer on local recurrence and 15-year survival: an overview
1999; 10: 47–52. of the randomised trials. Lancet 2005; 366: 2087–106.
15 Scholl SM, Asselain B, Palangie T, et al. Neoadjuvant chemotherapy 31 Gnant M, Harbeck N, Thomssen C. St. Gallen/Vienna 2017: a brief
in operable breast cancer. Eur J Cancer 1991; 27: 1668–71. summary of the consensus discussion about escalation and
16 Danforth DN Jr, Cowan K, Altemus R, et al. Preoperative de-escalation of primary breast cancer treatment. Breast Care 2017;
FLAC/granulocyte-colony-stimulating factor chemotherapy for 12: 102–07.
stage II breast cancer: a prospective randomized trial.
Ann Surg Oncol 2003; 10: 635–44.
17 Ragaz J, Baird R, Rebbeck P, et al. Preoperative (neoadjuvant)
versus postoperative adjuvant chemotherapy for stage I–II breast
cancer. Long-term analysis of British Columbia randomized trial.
Proc Am Soc Clin Oncol 1997; 16: 142a.
www.thelancet.com/oncology Vol 19 January 2018 39
También podría gustarte
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- ESMO Consensus Conference Recommendations On The Management of MetastaticDocumento46 páginasESMO Consensus Conference Recommendations On The Management of MetastaticYesenia HuertaAún no hay calificaciones
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Cirugi A Espan Ola: Anorectal Melanoma. An UpdateDocumento7 páginasCirugi A Espan Ola: Anorectal Melanoma. An UpdateYesenia HuertaAún no hay calificaciones
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Combi-D 2017Documento9 páginasCombi-D 2017Yesenia HuertaAún no hay calificaciones
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- Embarazo GemelarDocumento9 páginasEmbarazo GemelarYesenia HuertaAún no hay calificaciones
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Takayasu Arteritis Challenges in DiagnosisDocumento9 páginasTakayasu Arteritis Challenges in DiagnosisYesenia HuertaAún no hay calificaciones
- Chronic Granulomatous Disease A Review of Infectious and Inflamatory Complications PDFDocumento14 páginasChronic Granulomatous Disease A Review of Infectious and Inflamatory Complications PDFYesenia Huerta100% (1)
- Acute Otitis Media in Children Prevention of RecurrenceDocumento12 páginasAcute Otitis Media in Children Prevention of RecurrenceYesenia HuertaAún no hay calificaciones
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- Missing Data in StataDocumento12 páginasMissing Data in StataYesenia HuertaAún no hay calificaciones
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Lancet FQ PDFDocumento14 páginasLancet FQ PDFYesenia HuertaAún no hay calificaciones
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Anal Signs of Child Sexual Abuse: A Case - Control StudyDocumento7 páginasAnal Signs of Child Sexual Abuse: A Case - Control StudyYesenia HuertaAún no hay calificaciones
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Formulating A QuestionDocumento1 páginaFormulating A QuestionYesenia HuertaAún no hay calificaciones
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- Bladder Cancer LancetDocumento11 páginasBladder Cancer LancetYesenia HuertaAún no hay calificaciones
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Young Chinese DoctorsDocumento1 páginaYoung Chinese DoctorsYesenia HuertaAún no hay calificaciones
- Students' and Teachers' Use of FacebookDocumento15 páginasStudents' and Teachers' Use of FacebookYesenia HuertaAún no hay calificaciones
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- Stigma As Fundamental Cause of Population Health InequalitiesDocumento9 páginasStigma As Fundamental Cause of Population Health InequalitiesYesenia HuertaAún no hay calificaciones
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- Canamed 2019 - 2020Documento1908 páginasCanamed 2019 - 2020Cristian MihalacheAún no hay calificaciones
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- Acute Toxicity Study of Malli Chooranam A Siddha FormulationDocumento2 páginasAcute Toxicity Study of Malli Chooranam A Siddha FormulationInternational Journal of Innovative Science and Research TechnologyAún no hay calificaciones
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- Infant CPR Checklist PDFDocumento1 páginaInfant CPR Checklist PDFThea DavidAún no hay calificaciones
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Antiemetics - AMBOSSDocumento4 páginasAntiemetics - AMBOSSOpio IsaacAún no hay calificaciones
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The List of Questions For Exam in PharmacologyDocumento5 páginasThe List of Questions For Exam in PharmacologyAhmad Abu SamakAún no hay calificaciones
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Medical Devices PDFDocumento38 páginasMedical Devices PDFDr D Alwin , VetAún no hay calificaciones
- Jufe 3 10.30Documento38 páginasJufe 3 10.30LíaAún no hay calificaciones
- Metoclopramide DSDocumento1 páginaMetoclopramide DSAngelica Idio0% (1)
- Convention Modes of Mechanical Ventilation. DR - purwOKODocumento53 páginasConvention Modes of Mechanical Ventilation. DR - purwOKOIsnia WahibAún no hay calificaciones
- Handling Inhaler Devices Practical Guide Pharmacists 2011Documento88 páginasHandling Inhaler Devices Practical Guide Pharmacists 2011Hannah HalimAún no hay calificaciones
- Steroid Tapering and Supportive Treatment Guidance V1.0 PDFDocumento1 páginaSteroid Tapering and Supportive Treatment Guidance V1.0 PDFyunita hapsariAún no hay calificaciones
- Antiarrhythmic DrugsDocumento50 páginasAntiarrhythmic DrugsamirAún no hay calificaciones
- Types of Insulin PDFDocumento3 páginasTypes of Insulin PDFRetno WulanAún no hay calificaciones
- Med Org Kodigo CompleteDocumento39 páginasMed Org Kodigo CompletePaula PraxedesAún no hay calificaciones
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- Before So 2507Documento64 páginasBefore So 2507Lulu AzizahAún no hay calificaciones
- Suxamethonium Atracurium Cisatracurium Pancuronium Vecuronium RocuroniumDocumento1 páginaSuxamethonium Atracurium Cisatracurium Pancuronium Vecuronium Rocuroniumicen00bAún no hay calificaciones
- Glyburide (Glibenclamide) : Drug Information: Brand Names: USDocumento17 páginasGlyburide (Glibenclamide) : Drug Information: Brand Names: USAnonymous wmF9p2ejAún no hay calificaciones
- Ptsa 110123Documento114 páginasPtsa 110123Zefa FanyaAún no hay calificaciones
- Ethiopia FormularyDocumento543 páginasEthiopia Formularyabrham100% (1)
- Test Bank For Pharmacology and The Nursing Process 9th by LilleyDocumento6 páginasTest Bank For Pharmacology and The Nursing Process 9th by LilleyIrene Gillick100% (33)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Drug Senno Sides SennaDocumento1 páginaDrug Senno Sides SennaSrkocherAún no hay calificaciones
- Details of Conscious Caring: Product CatalogueDocumento6 páginasDetails of Conscious Caring: Product CatalogueBaharAún no hay calificaciones
- Plugin SwcsofrdDocumento3 páginasPlugin SwcsofrdUlziisuren NamkhaidavaaAún no hay calificaciones
- Onato Sami PharmaDocumento1 páginaOnato Sami PharmaNabeel Ahmed KhanAún no hay calificaciones
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Medications Commonly Used in Goats and Approximate Withdrawal TimesDocumento3 páginasMedications Commonly Used in Goats and Approximate Withdrawal TimesAmandaAún no hay calificaciones
- Harga 1 - PerdanaDocumento20 páginasHarga 1 - PerdanaSuzanSFauziahAún no hay calificaciones
- 2021 Concierge Refill Reminder ScriptDocumento15 páginas2021 Concierge Refill Reminder ScriptPablo PerezAún no hay calificaciones
- ObatDocumento9 páginasObatmarsenAún no hay calificaciones
- Unit 2 Notes-1Documento15 páginasUnit 2 Notes-1Manuel Christopher MontesclarosAún no hay calificaciones
- AminoglycosidesDocumento55 páginasAminoglycosidesIndira ButkoonAún no hay calificaciones
- Alex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessDe EverandAlex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessAún no hay calificaciones
- Merle's Door: Lessons from a Freethinking DogDe EverandMerle's Door: Lessons from a Freethinking DogCalificación: 4 de 5 estrellas4/5 (326)