Documentos de Académico
Documentos de Profesional
Documentos de Cultura
I1947 6094 12 2 110 PDF
Cargado por
hidayatul rahmoTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
I1947 6094 12 2 110 PDF
Cargado por
hidayatul rahmoCopyright:
Formatos disponibles
EXERCISE AND HEART FAILURE: ADVANCING KNOWLEDGE AND
IMPROVING CARE
Paulino Alvarez, M.D.; Bashar Hannawi, M.D.; Ashrith Guha, M.D., M.P.H.
Houston Methodist Hospital, Houston, Texas
Abstract
Exercise limitation is the hallmark of heart failure, and an increasing degree of intolerance is associated with poor prognosis.
Objective evaluation of functional class (e.g., cardiopulmonary exercise testing) is essential for adequate prognostication in
patients with advanced heart failure and for implementing an appropriate exercise training program. A graded exercise program
has been shown to be beneficial in patients with heart failure and has become an essential component of comprehensive cardiac
rehabilitation in these patients. An exercise program tailored to the patient’s preferences, possibilities, and physiologic reserve
has the greatest chance of being successful. Despite being safe, effective, and a guideline-recommended treatment to improve
quality of life, exercise training remains grossly underutilized. Patient, physician, insurance and practice barriers need to be
addressed to improve this quality gap.
Introduction fixed stroke volume.7 In this context, heart rate becomes the
Heart Failure (HF) is a progressive clinical syndrome that main driver to increase CO during exercise. Heart rate reserve
affects more than 5 million Americans at any given time.1 Caused is impaired in the vast majority of HF patients. Chronotropic
by impaired systolic or diastolic performance of the heart, HF incompetence, which is defined as the inability to increase heart
is characterized by exercise intolerance due to fatigue and/or rate proportionally to the degree of metabolic demands, affects
shortness of breath.1,2 between 25% to 70% of patients with HF and is probably related
In the first half of the 20th century, bed rest “from days to to beta-adrenergic receptor downregulation and desensitization
weeks to months” was recommended for heart failure patients.3 along with sinus node remodeling.8
Subsequently, research into understanding the mechanisms of In HF with preserved ejection fraction (HFpEF), chamber
exercise intolerance led to the development of evidence that stiffness prevents left ventricular (LV) diastolic volume from
supports the favorable effects of exercise training in heart failure increasing to accommodate increased venous return. In addition,
patients. Today, exercise training is one of the main components of an abnormal relaxation velocity versus heart rate relationship
comprehensive cardiac rehabilitation programs.4 causes a progressive decrease in lusitropic state as the heart rate
The objective of this review is to describe the determinants increases. Both mechanisms contribute to an increase in LV end
of exercise limitation in HF, how to assess exercise capacity of diastolic pressure (LVEDP) during exercise.9
HF patients, prognostic implications of exercise intolerance, and Comorbid coronary disease is present in more than 60% of pa-
essential components of exercise prescription. tients with HFpEF and HFrEF, and careful evaluation is key in
treating this potentially reversible cause of exercise limitation.
Mechanisms of Exercise Limitation in Heart Failure Myocardial ischemia due to decreased coronary flow reserve has
The human body’s response to exercise involves a complex been reported in patients with idiopathic dilated and hypertro-
interaction between lungs, heart, muscles, systemic and phic cardiomyopathy and contributes to impaired cardiac reserve
pulmonary vasculature. and mitochondrial respiration.5 From a during exercise.10, 11 Heart failure patients also experience skeletal
cardiovascular standpoint, increases in cardiac output (CO) and muscle hypoperfusion from decreased CO and increased peripher-
peripheral vasodilatation (i.e., a decrease in systemic vascular al vasoconstriction, which leads to metabolic and structural chang-
resistance) are crucial for delivering adequate oxygen to meet the es that reduce strength and increase fatigability. Recently, skeletal
body’s metabolic demands. Pathophysiological mechanisms of muscle receptors have been recognized as potential perpetuators
impaired exercise tolerance in HF include decreased contractility, of sympathetic hyperactivity.12 Myopathy of respiratory muscles
diastolic impairment, increased peripheral resistance, functional has been described as a significant contributor of dyspnea and ex-
mitral regurgitation, chronotropic incompetence, inadequate ercise intolerance in HF patients (Figure 1).13
distribution of blood flow (i.e., failure to direct CO to the
exercising muscles), abnormal skeletal muscle metabolism, Evaluation of Exercise Capacity
endothelial dysfunction, and abnormally high ergoreflex The New York Heart Association (NYHA) Functional
activation.6 Classification was introduced more than 80 years ago to provide
The modulation of sarcomeric function with changes in length a simple way of classifying the degree of exercise limitation in
described by the Frank-Starling relationship enables beat-to-beat patients with cardiac disease. Heart failure patients are classified
adaptation of CO to increase or decrease preload. Heart failure according to the severity of their symptoms, as follows:
patients with reduced ejection fraction (HFrEF) have the stroke
volume–preload function curve shifted to the right and flattened, • NYHA I: No symptoms and no limitations in ordinary
reflecting an almost-exhausted preload reserve with relatively physical activity.
110 houstonmethodist.org/debakey-journal MDCVJ | XII (2) 2016
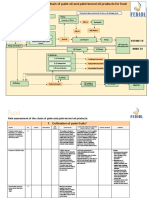
Figure 1. Mechanisms involved in exercise intolerance due to heart failure.
• NYHA II: Mild symptoms and slight limitation during Table 1 summarizes a variety of tests including stair
ordinary activity. climb, shuffle test, 6-minute walk test (SMWT), exercise
• NYHA III: Marked limitation in activity due to symptoms of electrocardiography, and cardiopulmonary exercise testing (CPET)
fatigue and dyspnea, even during less-than-ordinary activity; that allow quantitative evaluation of exercise capacity. The SMWT
comfortable at rest. and CPET are the most studied objective measures. The SMWT is a
• NYHA IV: Severe limitations and symptoms at rest. standardized, reproducible, low-tech test of exercise capacity that
measures the distance a patient can walk on a flat, hard surface in
Although useful for an initial ball park evaluation, the 6 minutes. It requires minimal equipment and no specific training
subjective nature of this system and the difficulty in recognizing of the technician performing the study. Given the self-paced nature
intermediate functional classes (II-III) limits its precision.14 of the study, results depend heavily on the motivation of the
Type Intensity Evaluation Standardized Reproducible Comments
Stair climb test Near Functional No No Climbing > 1 flight of stairs without stopping > 4
maximal capacity METS.
Incremental shuttle Near Functional Yes Yes Patients are required to walk at a speed dictated
test maximal capacity by audio signals from an audio tape recorder. The
walking speed is progressively increased. Good
correlation with peak VO2
Six minute walk test Near Functional Yes Yes Useful in patients with moderate to severe
maximal capacity impairment. Extensive experience in patients with
pulmonary and cardiac disease. Used to assess
response to interventions.
Exercise Maximal Ischemia Yes No* Analysis of heart rate response to exercise
electrocardiography and and heart rate recovery permit the evaluation
exercise of chronotropic incompetence and autonomic
duration dysfunction with additive prognostic information.
Cardiopulmonary Maximal Peak Yes Yes Gold standard. Incorporated in AHA/ACC and
stress testing VO2 and ISHLT guidelines for the evaluation of patients
exercise with advance heart failure. Not widely available.
duration. Trained staff required and specialized equipment.
*Probably related to the large intra-individual variability of electrocardiographic recordings at rest.
Table 1. Clinical exercise tests.
MDCVJ | XII (2) 2016 houstonmethodist.org/debakey-journal 111
Meta-analysis (ref) ExTraMATCH26 Davies27 Sagar28
Year 2004 2010 2014
Number of patients 801 3,647 4,740
Number of trials 9 19 33
Intervention Aerobic Aerobic. Five trials resistance Aerobic. Eleven trials resistance
training. training
Conclusions Safe and reduces mortality. Decreased heart failure-related Decreased overall and heart
hospitalization, improved quality failure-related admissions, no
of life. No significant difference in effect on mortality. Exercise also
short- or long-term mortality. improved quality of life.
ExTraMATCH: Exercise training meta-analysis of trials in patients with chronic heart failure
Table 2. Meta-analysis of exercise training in heart failure with reduced ejection fraction.
patient performing the test. Overall, the SMWT provides a global symptom and very difficult to quantify, has been associated with
evaluation of the systems involved in exercise tolerance.15 Recently an increased risk of hospitalization.22 Exercise limitation can be
self-administered SMWT using a smartphone application has been further quantified using CPET, which is a standard of care in HF
reported with promising results.16 clinics when evaluating a patient’s candidacy for transplant or
CPET requires specialized equipment and training of the mechanical device. Currently accepted thresholds of VO2 to be
technician performing the study and the physician interpreting the considered for either of these advanced HF therapies are 14 mL/
results. This highly standardized and reproducible test measures kg/min off beta blockers and < 12 mL/kg/min on beta blockers.24
gas exchange patterns, allowing the physician to determine which The prognostic value of CPET has been recently revisited and
organ system is limiting exercise capacity.17,18 Relevant parameters confirmed in a secondary analysis of the HF action trial.23 A recent
measured during CPET include: secondary analysis of HF-ACTION trial showed that peak VO2,
exercise duration, and percent predicted peak VO2% carried the
• Peak/maximal oxygen uptake (peak VO2): measures the strongest ability to predict and discriminate the likelihood of
maximal ability of the body to transport and utilize O2; death in patients with HFrEF. Another important finding of the
defines the limit of the cardiopulmonary system, is expressed same report was that prognosis associated with a given peak VO2
in milliliters of oxygen per kilogram of body weight per differed by sex. For example, a peak VO2 that corresponded to a
minute, and depends on effort, age, and gender; the prognosis 10% 1-year all-cause mortality was 10.9 mL/kg/min and 5.3 mL/
is worse in patients with HF if peak VO2 < 10 mL/kg/min. kg/min in men and women respectively.
• Ventilatory derived anaerobic threshold (VO2 at VT): the
point during exercise when there is a disproportionate Exercise as a Therapeutic Intervention
increase in energy production from anaerobic metabolism. Exercise training is defined as “exercise performed repetitively
• Respiratory exchange ratio (VCO2/VO2): overall indicator to increase the performance capacity of the cardiovascular system
of cardiorespiratory stress and a measure of subject effort; (aerobic exercise training) or muscular skeletal system (resistance
acceptable if ratio values > 1.1. exercise training).”24 The benefits of exercise training in HF
• Ventilatory efficiency (VE/VCO2 slope): represents the patients have been well documented. Results from systematic
perfusion that is matched to ventilation; independent of reviews and meta-analyses have shown that exercise training
subject effort, worse prognosis if slope is > 34. is not only safe but also is associated with a reduced risk of
• Other important parameters include blood pressure, heart rate hospitalization and a decrease in mortality (Table 2).25-27 HF-
response, exercise duration, continuous electrocardiographic ACTION was the largest multicenter randomized controlled trial
monitoring, and pulmonary function tests. of exercise training in HF. It included patients with HFrEF who
were classified as NYHA II-IV, and it demonstrated the safety of
The interpretation of CPET involves integrating all the exercise training. Hospitalizations after exercise occurred in 3.2%
parameters and considering additional comorbidities such as of the patients assigned to the supervised exercise program. The
anemia, obesity, lung diseases, and skeletal limitations. The most frequent obstacle to achieving the duration or intensity goal
insertion of a pulmonary artery catheter and arterial line before in at least one supervised exercise session was angina, followed
CPET may be considered when the cause of exercise limitation is by arrhythmia, pre-syncope or syncope, and hypoglycemia.28
not clear.23 The trial failed to show efficacy in all comers, but when adjusted
for other prognostic variables, exercise training was associated
Exercise as a Prognostic Tool with decreased all-cause mortality and hospitalization (HR =
The presence of symptoms in patients with LV systolic 0.89; 95% CI, 0.81-0.99; P = .03) and heart failure readmissions
dysfunction is a powerful negative prognostic indicator. For and HF-related mortality (HR = 0.85; 95% CI, 0.74-0.99; P = .03).
example, in the Studies of Left Ventricular Dysfunction (SOLVD) Increasing the duration of supervised exercise training may
prevention and treatment trials, the 3-year mortality rates in the be fundamental for the benefits of exercise training (Table 3).29
placebo group were 15% and 39%, respectively.19,20 The correlation Current guidelines state, “Exercise training (or regular physical
between NYHA functional class and mortality has also been activity) is recommended as safe and effective for patients
reported in patients with HFpEF.21 Fatigue, which is a vague with HF who are able to participate to improve functional
112 houstonmethodist.org/debakey-journal MDCVJ | XII (2) 2016
Trial (ref) Belardinelli30 HF-ACTION29
Number of patients 123 2,331
Population 59 years of age 59 years of age
27% women 28% women
NYHA II/III (100%) NYHA II/III (99%)
mean EF 37% median EF 25%
Follow-up 10 years 30.1 months
Intervention 60% of peak VO2, 2x/week for 6 months followed by Stage I: supervised. 60% of heart rate reserved, 3x/
70% of peak VO2, 3x/week for the rest of study (10 week for 2 weeks for 15-30 min followed by 70% of
yrs). heart rate reserved, 3x/week for 30-35 min for total of
Patients exercised at coronary club for the duration of 3 months.
the study, with supervised sessions every 6 months. Stage II: home-based. 60-70% of heart rate reserved
5x/week for 40 min.
Outcomes Increased peak VO2, improved quality of life, decreased No reduction in all-cause mortality or hospitalization.
hospital readmission, decreased cardiovascular
mortality
NYHA: New York Heart Association; EF: ejection fraction; VO2: oxygen consumption
Table 3. Landmark trials of exercise training in heart failure.
status Class IA.”30 Despite this recommendation, only 10.4% of Currently, CMS covers 36 sessions of cardiac rehabilitation,
eligible HF patients received cardiac rehabilitation referral after after which the patient must continue with unsupervised exercise
hospitalization for HF.31 training, adding several challenges for compliance.
On February 18, 2014, the Centers for Medicare and Medicaid
Services (CMS) expanded coverage for cardiac rehabilitation Exercise Training in Special Heart Failure Patient
services to “beneficiaries with stable, chronic heart failure, defined Populations
as patients with left ventricular ejection fraction of 35% or less Heart Failure with Preserved Ejection Fraction
and New York Heart Association (NYHA) class II to IV symptoms In a recent meta-analysis including 276 patients with HFpEF,
despite being on optimal heart failure therapy for at least six exercise training was associated with improved cardiorespiratory
weeks. Stable patients are defined as patients who have not had fitness as measured by peak oxygen uptake and quality of life.35
recent (≤ 6 weeks) or planned (≤ 6 months) major cardiovascular The mechanism by which this is achieved is through improvement
hospitalizations or procedures.”32 of peripheral factors such as skeletal muscle function, endothelial
function, and arterial stiffness.36
Main Components of an Exercise Prescription for Heart
Failure Patients Heart Transplant
Once contraindications to exercise therapy have been excluded After heart transplantation, patients remain with significant
and potential reversible causes of exercise intolerance (e.g., exercise intolerance when compared with an age- and sex-matched
decompensated heart failure, anemia, endocrine disorders) have healthy population. This is related mainly to the persistence of
been treated, an exercise prescription can be made (Figure 1). This peripheral factors including skeletal muscle dysfunction and
involves assessing the energy cost of the activity that is being impaired vasodilatory capacity. Lack of autonomic innervation
planned and whether or not the patient is able to safely exercise at also contributes to abnormal heart rate response. Exercise therapy
that specific level. The patient should perform a symptom-limited has consistently been associated with an improvement in peak
graded exercise test, preferably a CPET, which can provide key VO2, however, the optimal type of therapy remains to be defined.37
information about that patient’s specific goals.33 This quantitative
approach allows precise recommendations of the level of exercise. Left Ventricular Assist Devices
A moderate level, which is the most often prescribe, is defined as The effect of exercise on patients with left ventricular assist
40% to 60% of heart rate reserve (peak heart rate minus resting devices (LVAD) has been inconsistent throughout the literature,
heart rate), 40% to 60% of the VO2 reserve (peak VO2 minus resting partly due to the heterogeneity of the studies and the small sample
VO2), and a rating of perceived exertion 12 to 13. sizes. While some authors found that exercise did not lead to
Clinical variables such as age, gender, comorbidities, previous improvement in peak VO2, others found that it does improve
physical activity, and orthopedic/musculoskeletal factors must be peak VO2 as well as quality of life. Early progressive mobilization
considered when tailoring an appropriate exercise plan. There are can safely be started 1 week after LVAD implantation and
several patient and therapy related barriers to exercise therapy, exercise training can be started after 2 to 4 weeks, with maximal
therefore, the physician should carefully address any obstacles to improvement in exercise capacity after 12 weeks.38
compliance (as is done with drug therapies), empower the patient
with information about the efficacy and safety of exercise therapy, Conclusion
follow up with the patient’s exercise plan during every visit, and Exercise intolerance is common in patients with heart
encourage the patient on his or her accomplishments.34 failure and is multifactorial in causation. Exercise therapy is
MDCVJ | XII (2) 2016 houstonmethodist.org/debakey-journal 113
Figure 2. Approach to exercise training prescription.
HFrEF: heart failure with reduced ejection fraction; HFpEF: heart failure with preserved ejection fraction; HF: heart failure; BB: beta blocker; ACEI: angiotensin
converting enzyme inhibitor; ACS: acute coronary syndrome; AS: aortic stenosis; HOCM: hypertrophic obstructive cardiomyopathy; VO2: oxygen consumption;
ET: exercise training; f/u: follow-up
one of the most effective, safe, and underutilized treatments • Successful implementation of an exercise program depends
for exercise intolerance in HF. Recognition of patient and on recognizing and addressing patient, physician, insurance,
practice barriers for exercise therapy program implementation and practice barriers.
is important to help close this prevalent quality gap in the care
of HF patients. Conflict of Interest Disclosure: The authors have completed and submitted
the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement
Key Points: and none were reported.
• Exercise training is an essential component of comprehensive Keywords: heart failure, exercise, cardiopulmonary exercise testing
cardiac rehabilitation.
• Exercise training is a safe, effective, and guideline- References
recommended treatment to improve quality of life and 1. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and
morbidity in patients with heart failure. stroke statistics--2015 update: a report from the American Heart
• Objective evaluation of functional class should be performed Association. Circulation. 2015 Jan 27;131(4):e29-322.
early on in the assessment of patients with heart failure, 2. Katz AM. The “modern” view of heart failure: how did we get
regardless of their left ventricular ejection fraction. here? Circ Heart Fail. 2008 May;1(1):63-71.
• Tailoring an exercise program to the patient’s preferences, 3. Silverman ME. A view from the millennium: the practice of
abilities, and physiologic reserve increases satisfaction and cardiology circa 1950 and thereafter. J Am Coll Cardiol, 1999
adherence. Apr;33(5):1141-51.
114 houstonmethodist.org/debakey-journal MDCVJ | XII (2) 2016
4. Ades PA, Keteyian SJ, Balady GJ, et al. Cardiac rehabilitation 23. Keteyian SJ, Patel M, Krause WE, et al.; Variables Measured
exercise and self-care for chronic heart failure. JACC Heart Fail. During Cardiopulmonary Exercise Testing as Predictors of Mortality
2013 Dec;1(6):540-7. in Chronic Systolic Heart Failure. J Am Coll Cardiol. 2016 Feb
5. Wasserman K, et al. Anaerobic threshold and respiratory gas 23;67(7):780-9.
exchange during exercise. J Appl Physiol. 1973 Aug;35(2):236-43. 24. Thompson PD. Exercise prescription and proscription for
6. Piña IL, Apstein CS, Balady GJ, et al.; American Heart Association patients with coronary artery disease. Circulation. 2005 Oct
Committee on exercise, rehabilitation, and prevention. Exercise 11;112(15):2354-63.
and heart failure: A statement from the American Heart Association 25. Piepoli MF, Davos C, Francis DP, Coats AJ; ExTraMATCH
Committee on exercise, rehabilitation, and prevention. Circulation. Collaborative. Exercise training meta-analysis of trials in patients
2003 Mar 4;107(8):1210-25. with chronic heart failure (ExTraMATCH). BMJ. 2004 Jan
7. Hanft LM, Korte FS, McDonald KS. Cardiac function and 24;328(7433):189.
modulation of sarcomeric function by length. Cardiovasc Res. 2008 26. Davies EJ, Moxham T, Rees K, et al. Exercise training for systolic
Mar 1;77(4):627-36. heart failure: Cochrane systematic review and meta-analysis. Eur J
8. Brubaker PH, Kitzman DW. Chronotropic incompetence: causes, Heart Fail. 2010 Jul;12(7):706-15.
consequences, and management. Circulation. 2011 Mar 27. Sagar VA, Davies EJ, Briscoe S, et al. Exercise-based rehabilitation
8;123(9):1010-20. for heart failure: systematic review and meta-analysis. Open Heart.
9. Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and 2015 Jan 28;2(1):e000163.
diastolic heart failure: Part II: causal mechanisms and treatment. 28. O’Connor CM, Whellan DJ, Lee KL, et al.; HF-ACTION Investiga-
Circulation. 2002 Mar 26;105(12):1503-8. tors. Efficacy and safety of exercise training in patients with chronic
10. Hwang SJ, Melenovsky V, Borlaug BA. Implications of coronary heart failure: HF-ACTION randomized controlled trial. JAMA. 2009
artery disease in heart failure with preserved ejection fraction. J Am Apr 8;301(14):1439-50.
Coll Cardiol. 2014 Jul 1;63(25 Pt A):2817-27. 29. Belardinelli R, Georgiou D, Cianci G, Purcaro A. 10-year exercise
11. Gheorghiade M, Sopko G, De Luca L, et al. Navigating the training in chronic heart failure: a randomized controlled trial. J Am
crossroads of coronary artery disease and heart failure. Circulation. Coll Cardiol. 2012 Oct 16;60(16):1521-8.
2006 Sep 12;114(11):1202-13. 30. Yancy CW, Jessup M, Bozkurt B, et al.; American College of
12. Piepoli MF, Crisafulli A. Pathophysiology of human heart failure: Cardiology Foundation; American Heart Association Task Force
importance of skeletal muscle myopathy and reflexes. Exp Physiol. on Practice Guidelines. 2013 ACCF/AHA guideline for the
2014 Apr;99(4):609-15. management of heart failure: a report of the American College
13. Mancini DM, Henson D, LaManca J, Levine S. Respiratory muscle of Cardiology Foundation/American Heart Association Task
function and dyspnea in patients with chronic congestive heart Force on Practice Guidelines. J Am Coll Cardiol. 2013 Oct
failure. Circulation. 1992 Sep;86(3):909-18. 15;62(16):e147-239.
14. Fleg JL, Piña IL, Balady GJ, et al. Assessment of functional 31. Golwala H, Pandey A, Ju C, et al. Temporal Trends and Factors
capacity in clinical and research applications: An advisory from the Associated With Cardiac Rehabilitation Referral Among Patients
Committee on Exercise, Rehabilitation, and Prevention, Council on Hospitalized With Heart Failure: Findings From Get With The
Clinical Cardiology, American Heart Association. Circulation. 2000 Guidelines-Heart Failure Registry. J Am Coll Cardiol. 2015 Aug
Sep 26;102(13):1591-7. 25;66(8):917-26.
15. Pichurko BM. Exercising your patient: which test(s) and when? 32. Centers for Medicare & Medicaid Services [Internet]. Baltimore,
Respir Care. 2012 Jan;57(1):100-10; discussion 110-3. MD: Centers for Medicare & Medicaid Services; c2014. National
16. Brooks GC, Vittinghoff E, Iyer S, et al. Accuracy and Usability of a Coverage Determination (NCD) for Cardiac Rehabilitation Pro-
Self-Administered 6-Minute Walk Test Smartphone Application. Circ grams for Chronic Heart Failure (20.10.1); 2014 Feb 18 [cited
Heart Fail. 2015 Sep;8(5):905-13. 2016 Feb 25]. Available from: https://www.cms.gov
17. Balady GJ, Arena R, Sietsema K, et al. Clinician’s Guide to 33. Piepoli MF, Conraads V, Corra U, et al. Exercise training in heart
cardiopulmonary exercise testing in adults: a scientific statement failure: from theory to practice. A consensus document of the
from the American Heart Association. Circulation. 2010 Jul Heart Failure Association and the European Association for
13;122(2):191-225. Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail.
18. Albouaini K, Egred M, Alahmar A, Wright DJ. Cardiopulmonary 2011 Apr;13(4):347-57.
exercise testing and its application. Postgrad Med J. 2007 34. Conraads VM, Deaton C, Piotrowicz E, et al. Adherence of heart
Nov;83(985):675-82. failure patients to exercise: barriers and possible solutions: a position
19. Effect of enalapril on mortality and the development of heart failure statement of the Study Group on Exercise Training in Heart Failure of
in asymptomatic patients with reduced left ventricular ejection the Heart Failure Association of the European Society of Cardiology.
fractions. The SOLVD Investigattors. N Engl J Med. 1992 Sep Eur J Heart Fail. 2012 May;14(5):451-8.
3;327(10):685-91. 35. Pandey A, Parashar A, Kumbhani DJ, et al. Exercise training
20. Effect of enalapril on survival in patients with reduced left ventricular in patients with heart failure and preserved ejection fraction:
ejection fractions and congestive heart failure. The SOLVD meta-analysis of randomized control trials. Circ Heart Fail. 2015
Investigators. N Engl J Med. 1991 Aug 1;325(5):293-302. Jan;8(1):33-40.
21. Ahmed A, Aronow WS, Fleg JL. Higher New York Heart Association 36. Keteyian SJ. Exercise training in patients with heart failure and
classes and increased mortality and hospitalization in patients with preserved ejection fraction: findings awaiting discovery. J Am Coll
heart failure and preserved left ventricular function. Am Heart J. Cardiol. 2013 Aug 13;62(7):593-4.
2006 Feb;151(2):444-50. 37. Nytroen K, Gullestad L. Exercise after heart transplantation: An
22. Perez-Moreno AC, Jhund PS, MacDonald MR, et al.; Fatigue overview. World J Transplant. 2013 Dec 24;3(4):78-90.
as a predictor of outcome in patients with heart failure: analysis 38. Alsara O, Perez-Terzic C, Squires RW, et al. Is exercise training
of CORONA (Controlled Rosuvastatin Multinational Trial in Heart safe and beneficial in patients receiving left ventricular assist device
Failure). JACC Heart Fail. 2014 Apr;2(2):187-97. therapy? J Cardiopulm Rehabil Prev. 2014 Jul-Aug;34(4):233-40.
MDCVJ | XII (2) 2016 houstonmethodist.org/debakey-journal 115
También podría gustarte
- Jgxyfxjhcyxjgcgxhgcjhv. Jlbljvkhvuh Hvhgcgcug BjhvuhvuhDocumento1 páginaJgxyfxjhcyxjgcgxhgcjhv. Jlbljvkhvuh Hvhgcgcug Bjhvuhvuhhidayatul rahmoAún no hay calificaciones
- World Health Report 2004Documento96 páginasWorld Health Report 2004agniesia_rakAún no hay calificaciones
- Gestational Hypertension and Preeclampsia in Living Kidney DonorsDocumento10 páginasGestational Hypertension and Preeclampsia in Living Kidney Donorshidayatul rahmoAún no hay calificaciones
- Am J Clin Nutr 2007 Goldenberg 584S 90SDocumento7 páginasAm J Clin Nutr 2007 Goldenberg 584S 90Shidayatul rahmoAún no hay calificaciones
- AaDocumento7 páginasAahidayatul rahmoAún no hay calificaciones
- AlgoritmaDocumento8 páginasAlgoritmaTony RamirezAún no hay calificaciones
- Jurnal GenetikDocumento1 páginaJurnal GenetikMochammad Arsyi GAún no hay calificaciones
- The Prevalence of Constipation and Irritable Bowel Syndrome in Parkinson's Disease Patients According To Rome III Diagnostic CriteriaDocumento5 páginasThe Prevalence of Constipation and Irritable Bowel Syndrome in Parkinson's Disease Patients According To Rome III Diagnostic Criteriahidayatul rahmoAún no hay calificaciones
- RRDocumento4 páginasRRhidayatul rahmoAún no hay calificaciones
- Management of Hypertension and Diabetes Mellitus.31Documento6 páginasManagement of Hypertension and Diabetes Mellitus.31hidayatul rahmoAún no hay calificaciones
- RRDocumento4 páginasRRhidayatul rahmoAún no hay calificaciones
- The Prevalence of Constipation and Irritable Bowel Syndrome in Parkinson's Disease Patients According To Rome III Diagnostic CriteriaDocumento5 páginasThe Prevalence of Constipation and Irritable Bowel Syndrome in Parkinson's Disease Patients According To Rome III Diagnostic Criteriahidayatul rahmoAún no hay calificaciones
- Fullpapers Mgi63160222ccfull PDFDocumento5 páginasFullpapers Mgi63160222ccfull PDFFadhila NurrahmaAún no hay calificaciones
- Jurnal GenetikDocumento1 páginaJurnal GenetikMochammad Arsyi GAún no hay calificaciones
- Fgf13 Causes Synaptic Excitatory-Inhibitory: Disruption of Imbalance and Genetic Epilepsy and Febrile Seizures PlusDocumento16 páginasFgf13 Causes Synaptic Excitatory-Inhibitory: Disruption of Imbalance and Genetic Epilepsy and Febrile Seizures Plushidayatul rahmoAún no hay calificaciones
- Prospective Study of Fasting Blood Glucose and Intracerebral Hemorrhagic RiskDocumento7 páginasProspective Study of Fasting Blood Glucose and Intracerebral Hemorrhagic Riskhidayatul rahmoAún no hay calificaciones
- LAMPIRAN-LAMPIRANDocumento24 páginasLAMPIRAN-LAMPIRANhidayatul rahmo100% (1)
- PDocumento4 páginasPhidayatul rahmoAún no hay calificaciones
- The Effect of Insulin Resistance On House-Brackmann Grade of Facial Paralysis in Patients With Bell's PalsyDocumento4 páginasThe Effect of Insulin Resistance On House-Brackmann Grade of Facial Paralysis in Patients With Bell's Palsyhidayatul rahmoAún no hay calificaciones
- Diabetes Algorithm PDFDocumento32 páginasDiabetes Algorithm PDFStarlet Rhonadez Bito-onon OrielAún no hay calificaciones
- Bab I Pendahuluan: "Essay On The Shaking Palsy"Documento40 páginasBab I Pendahuluan: "Essay On The Shaking Palsy"hidayatul rahmoAún no hay calificaciones
- Arti Jurnal FixDocumento13 páginasArti Jurnal Fixhidayatul rahmoAún no hay calificaciones
- Khair PDFDocumento8 páginasKhair PDFtenriulengAún no hay calificaciones
- PPTDocumento50 páginasPPThidayatul rahmoAún no hay calificaciones
- Fgf13 Causes Synaptic Excitatory-Inhibitory: Disruption of Imbalance and Genetic Epilepsy and Febrile Seizures PlusDocumento16 páginasFgf13 Causes Synaptic Excitatory-Inhibitory: Disruption of Imbalance and Genetic Epilepsy and Febrile Seizures Plushidayatul rahmoAún no hay calificaciones
- Kariuki Et Al 2016Documento10 páginasKariuki Et Al 2016hidayatul rahmoAún no hay calificaciones
- Jurnal GenetikDocumento1 páginaJurnal GenetikMochammad Arsyi GAún no hay calificaciones
- Am J Clin Nutr 2007 Goldenberg 584S 90SDocumento7 páginasAm J Clin Nutr 2007 Goldenberg 584S 90Shidayatul rahmoAún no hay calificaciones
- j.1469-0691.2012.03798.x.pdf Scabies Journal PDFDocumento11 páginasj.1469-0691.2012.03798.x.pdf Scabies Journal PDFHafich ErnandaAún no hay calificaciones
- Kjped 57 384 PDFDocumento12 páginasKjped 57 384 PDFIrfanAún no hay calificaciones
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5783)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- 0 - Speech & Debate WritingDocumento12 páginas0 - Speech & Debate WritingRituja DasAún no hay calificaciones
- Schizo Ppt.Documento78 páginasSchizo Ppt.Nimisha ChackoAún no hay calificaciones
- ACE Sports Nutrition For Health Professionals PagesDocumento4 páginasACE Sports Nutrition For Health Professionals PagesHamada MansourAún no hay calificaciones
- Root Words, Prefixes and Suffixes Used in Dental TermsDocumento2 páginasRoot Words, Prefixes and Suffixes Used in Dental TermssalahAún no hay calificaciones
- M.SC Dietetics Personal StatementDocumento3 páginasM.SC Dietetics Personal StatementBEMIGHO OKEAún no hay calificaciones
- Customers - Food Allergies: Safe MethodDocumento2 páginasCustomers - Food Allergies: Safe MethodAlghubariAún no hay calificaciones
- OB FC Nov 2021 NLEDocumento9 páginasOB FC Nov 2021 NLEAlyssa SaibiAún no hay calificaciones
- Subliminal Mind Control Hemi Sync Basics What It Does and How Amp Why It WorksDocumento5 páginasSubliminal Mind Control Hemi Sync Basics What It Does and How Amp Why It Worksdruidess3Aún no hay calificaciones
- Rigging Plan 1671493342Documento131 páginasRigging Plan 1671493342AlfiAún no hay calificaciones
- L'anxiété de Performance À L'enfance Et L'adolescenceDocumento32 páginasL'anxiété de Performance À L'enfance Et L'adolescenceZakia ERRABIHAún no hay calificaciones
- The History and Culture of Japanese FoodDocumento284 páginasThe History and Culture of Japanese FoodDiana67% (6)
- Chogtu 2015Documento7 páginasChogtu 2015Maskur Fahmi ÄdibasAún no hay calificaciones
- The 14 IDEA Disability Categories DefinedDocumento7 páginasThe 14 IDEA Disability Categories DefinedRico Bautista SongSongCoupleAún no hay calificaciones
- 21 Day Flat Belly Fix Tea ReviewsDocumento7 páginas21 Day Flat Belly Fix Tea ReviewsSantiagoAún no hay calificaciones
- Ace Hot Work Permit Application Form PDFDocumento3 páginasAce Hot Work Permit Application Form PDFkevin100% (1)
- Tatalaksana Low Vision Pada Severe Visual Impairment Dengan Aphakia Dan Amblyopia DeprivatifDocumento12 páginasTatalaksana Low Vision Pada Severe Visual Impairment Dengan Aphakia Dan Amblyopia DeprivatifAURA PUTRIAún no hay calificaciones
- Checklist of Mandatory Documentation Required by ISO 13485:2016Documento15 páginasChecklist of Mandatory Documentation Required by ISO 13485:2016Ricky Mark100% (2)
- Carb Counting Type1Documento22 páginasCarb Counting Type1Dhanalakshmi ThiyagarajanAún no hay calificaciones
- Literature Review Intrauterine DeathDocumento5 páginasLiterature Review Intrauterine Deathaflsktofz100% (1)
- Essential Intrapartum and Newborn CareDocumento25 páginasEssential Intrapartum and Newborn CareMaria Lovelyn LumaynoAún no hay calificaciones
- Swim Training for HeroesDocumento8 páginasSwim Training for HeroesRaymondKarverAún no hay calificaciones
- Extraction of Caffeine From Tea Leaves Experiment Formal ReportDocumento6 páginasExtraction of Caffeine From Tea Leaves Experiment Formal ReportChristeline Fernandez50% (2)
- Academic Resilience and Adolescent StudentsDocumento4 páginasAcademic Resilience and Adolescent StudentsInternational Journal of Innovative Science and Research TechnologyAún no hay calificaciones
- Standard Days Method: SourcesDocumento2 páginasStandard Days Method: SourcesKim MedairosAún no hay calificaciones
- Zambia Daily Mail, Monday, January 3, 2022Documento16 páginasZambia Daily Mail, Monday, January 3, 2022Mulenga MwaleAún no hay calificaciones
- Dorothy Johnson PosterDocumento1 páginaDorothy Johnson Posterapi-519455077Aún no hay calificaciones
- CBSE Mock Test E03 English Term IIDocumento4 páginasCBSE Mock Test E03 English Term IIJohn DoeAún no hay calificaciones
- Risk Assessment Palm Food FEDIOL Final 160522Documento18 páginasRisk Assessment Palm Food FEDIOL Final 160522Jayashri chitteAún no hay calificaciones
- Assignment Ni Ayang Sa TechnologyDocumento2 páginasAssignment Ni Ayang Sa TechnologyJohn Mico MacatigbacAún no hay calificaciones
- Kettle Bell Workout MovesDocumento1 páginaKettle Bell Workout MovesRabiatul AdawiyahAún no hay calificaciones