Documentos de Académico
Documentos de Profesional
Documentos de Cultura
A Un Año de La Pandemia de Influenza... ¿Estamos Preparados para Otra Crisis Global?
Cargado por
Alain SánchezTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
A Un Año de La Pandemia de Influenza... ¿Estamos Preparados para Otra Crisis Global?
Cargado por
Alain SánchezCopyright:
Formatos disponibles
Editorial
Pandemic influenza—(some) reasons to be cheerful?
There was no fanfare to accompany WHO’s declaration 18 449 people died and hundreds of thousands were
on Aug 10 that the world was entering a “post-pandemic severely affected around the world. It is a testament to
period” and that influenza A H1N1 had “largely run its global health-care systems that many were successfully
course”. But the aftershocks of the pandemic might last treated. However, the pandemic largely caught the
for a long time, so this announcement should herald the research community unawares. Although anecdotes and
start of a period of reflection. observational data have been gathered, few patients
From the first cases, in Mexico, in March, 2009, to were entered into randomised trials, and thus solid data
Getty Images
identification of the culprit virus took WHO’s global to inform treatment decisions for future pandemics
influenza surveillance network just 6 weeks. Then, with are lacking. Where they existed, countrywide plans for
only oseltamivir to protect the world’s population, the handling a pandemic were predicated on an outbreak of
cogs of the influenza vaccine production mechanism severe H5N1 influenza, but were too draconian for the
whirred into action. Normally competitive groups milder H1N1 strain, while many countries carried on with
collaborated, and countries around the world shared data business as usual.
on virus strains, despite fears that many would not do so Questions are rightly being asked about the influence
without a binding agreement guaranteeing vaccines in of the drug industry on WHO’s decision-making process,
return for data. Once a suitable seed strain was grown, but to focus on this alone would be foolish. Now is not
drug companies started to make a useable vaccine. From the time to apportion blame, but to ask: how can we do
virus identification to vaccine approval by the US Food better next time? First, we need to be better prepared.
and Drug Administration took 6 months. So far, so good. There needs to be global investment in responsive
But from here on, chinks in the pandemic preparedness vaccine production systems, which allow production to
armour started to appear. track demand. Plans are also required to ensure equitable
Vaccine production could have been quicker. Newer distribution of vaccines and antiviral drugs. Developed
methods that use cell culture, or baculovirus expression countries should not be able to stockpile unused vaccines,
systems, could be much more responsive than the egg- while people in the developing world go without. Planning
based method that is currently used. Until recently, for equitable worldwide vaccination will require the
financial considerations have meant that these newer development of a political framework to ensure adequate
techniques have not received the deserved attention funding, procurement agreements, and worldwide
from industry. Vaccine production was also limited to a distribution strategies well before the next outbreak.
handful of more developed countries, contributing to the Such plans will help to ensure that poorer countries have
familiar division between the haves and have-nots. WHO enough incentives to share information about emerging
and the UN Secretary General worked tirelessly to ensure virus strains, and do not feel that they are giving their
vaccine delivery to low-income and middle-income wealthier counterparts information, for no benefit.
countries, but from the outset were dogged by a lack of Preparedness plans also need to have the flexibility to be
vaccine-producing capacity, recalcitrant politicians, and able to cope with a range of pandemic severity.
inadequate plans. Even if vaccines reached developing Second, we need systems in place to maximise learning.
countries, a lack of infrastructure hampered deployment. Protocols and approvals should be ready for randomised
There was a stark contrast between countries rich enough trials of treatment strategies; these could then begin
to stockpile vaccines, and others (eg, Laos and Cambodia) recruiting as soon as an outbreak occurs. But finally,
who for many months had none. and perhaps most importantly, we need to rebuild a
Ironically, people in high-income countries used their relationship of trust with the public. The disparity between
vaccine stockpiles reluctantly. Around 80% of people in predicted and actual severity of this pandemic has severely
For more on Patient-oriented
the UK chose not to be vaccinated, many because they dented experts’ credibility, so now experts need to use all pandemic influenza research
doubted they were at serious risk. They were correct, methods at their disposal to engage the public. The best see Lancet 2009; 373: 2085–86.
For more on Confirmation of
but we know this only after the fact. Despite the fairly laid plans will come to nothing if people have lost faith in influenza infection see Lancet
mild course in most infected individuals, more than the information and interventions available. ■ The Lancet 2008; 372: 696–97.
www.thelancet.com Vol 376 August 21, 2010 565
También podría gustarte
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2103)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Roseola InfantumDocumento1 páginaRoseola Infantumshailesh284Aún no hay calificaciones
- Sexually Transmitted InfectionsDocumento104 páginasSexually Transmitted InfectionsNikki M. Arapol50% (2)
- Microbial Diseases of The Digestive SystemDocumento150 páginasMicrobial Diseases of The Digestive Systemone_nd_onlyuAún no hay calificaciones
- Crit Care Nurse 2014 Petlin 17 24Documento11 páginasCrit Care Nurse 2014 Petlin 17 24Barbara Sakura RiawanAún no hay calificaciones
- Bloodborne Pathogen Training PDFDocumento22 páginasBloodborne Pathogen Training PDFapi-282330630Aún no hay calificaciones
- Pretransfusion or Compatibility Testing: NotesDocumento7 páginasPretransfusion or Compatibility Testing: NotesABHINABA GUPTAAún no hay calificaciones
- RAPID AST FROM BLOOD CULUTURE-Methodology - EUCAST - RAST - v1 - 20181126 PDFDocumento3 páginasRAPID AST FROM BLOOD CULUTURE-Methodology - EUCAST - RAST - v1 - 20181126 PDFKhoa Vi Sinh BVCRAún no hay calificaciones
- 20-Dialysis 2016Documento10 páginas20-Dialysis 2016duchess juliane mirambelAún no hay calificaciones
- .PHEM Weekly Reporting Format - 1646640158000Documento17 páginas.PHEM Weekly Reporting Format - 1646640158000Getachew DemissieAún no hay calificaciones
- CertificateDocumento1 páginaCertificateSushma SinghAún no hay calificaciones
- Echinostoma IlocanumDocumento3 páginasEchinostoma IlocanumChristie Raye NapuliAún no hay calificaciones
- The All-Frequencies CAFL (AFCAFL)Documento27 páginasThe All-Frequencies CAFL (AFCAFL)Federico Ceriani100% (1)
- Paramyxovirus and RubellaDocumento65 páginasParamyxovirus and RubellaishlionAún no hay calificaciones
- Management of Condyloma Acuminata PDFDocumento6 páginasManagement of Condyloma Acuminata PDFGilankAún no hay calificaciones
- OIE - Terrestrial Animal Health Code - Version 8 - 2014 - Volume IIDocumento312 páginasOIE - Terrestrial Animal Health Code - Version 8 - 2014 - Volume IIWormInchAún no hay calificaciones
- Infectious Diseases Act, 2018Documento6 páginasInfectious Diseases Act, 2018Md. Fahim Shahriar MozumderAún no hay calificaciones
- Cefepime Vs Zosyn For Empiric Sepsis CoverageDocumento2 páginasCefepime Vs Zosyn For Empiric Sepsis Coveragetl drAún no hay calificaciones
- Angine Difteria: Dr. Cristiana OpreaDocumento39 páginasAngine Difteria: Dr. Cristiana OpreaAlexandra Andreea100% (1)
- SEM2 MALARIA Plasmodium Falciparum 2013Documento23 páginasSEM2 MALARIA Plasmodium Falciparum 2013odysseyfairy2739Aún no hay calificaciones
- Epps Motion For Compassionate ReleaseDocumento10 páginasEpps Motion For Compassionate Releasethe kingfishAún no hay calificaciones
- Pathophysiology of Koch's Disease (Tuberculosis) : Primary InfectionDocumento2 páginasPathophysiology of Koch's Disease (Tuberculosis) : Primary InfectionStephanie GapuzAún no hay calificaciones
- Herpetic Mucocutaneous Infections: HSV (HSV 1 & 2) & VZVDocumento32 páginasHerpetic Mucocutaneous Infections: HSV (HSV 1 & 2) & VZVJaneAún no hay calificaciones
- Central Ink Tattoo and Body Piercing Sign in FormDocumento1 páginaCentral Ink Tattoo and Body Piercing Sign in FormZag ManAún no hay calificaciones
- JC BiofireDocumento33 páginasJC Biofiresaurabh kaushikAún no hay calificaciones
- Aseptic MeningitisDocumento4 páginasAseptic MeningitisCheng XinvennAún no hay calificaciones
- National Guideline For Kala-Azar Case Management Bangladesh 2013Documento72 páginasNational Guideline For Kala-Azar Case Management Bangladesh 2013Kutu MiaAún no hay calificaciones
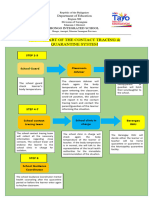
- Flow Chart of The Contact Tracing & Quarantine SystemDocumento1 páginaFlow Chart of The Contact Tracing & Quarantine Systemeugene louie ibarraAún no hay calificaciones
- Covid PresentationDocumento21 páginasCovid Presentationchici azriniAún no hay calificaciones
- Antimicrobial Susceptibility TestingDocumento14 páginasAntimicrobial Susceptibility TestingFatimah TambilawanAún no hay calificaciones
- Golden Point For PediatricsDocumento19 páginasGolden Point For PediatricsOmprakash SainiAún no hay calificaciones