Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Immuno Chemo
Cargado por
nski2104Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Immuno Chemo
Cargado por
nski2104Copyright:
Formatos disponibles
PERSPECTIVES
of survival signals1. A generally accepted
OPINION current biochemical definition would
include the activation of a conserved series
of caspases2, a family of cysteine proteases
Immunotherapy and chemotherapy that facilitate the efficient dismantling of
the dying cell. When cells die by apoptosis,
a practical partnership phosphatidylserine, which in normal cells is
located on the inner leaflet of the plasma
membrane, translocates to the outer leaflet,
Richard A. Lake and Bruce W. S. Robinson where it acts as a molecular flag, interacting
with receptors expressed by a range of differ-
Abstract | This article discusses how recent there has been a paucity of methods to accu- ent cell types, including macrophages. In the
data have altered the way we understand rately analyse any changes. With increasingly absence of inflammatory signals, the
how dying tumour cells, particularly those sophisticated models and the development of macrophages phagocytose the apoptotic
killed by chemotherapy, engage with a range of tools to scrutinize the progress of remnants3. Apoptosis has long been consid-
antitumour immune responses. These data any anticancer immune responses to growing ered as non-immunogenic or even tolerizing,
have significant implications for the tumours, several recent studies have produced occurring in the absence of any inflamma-
development of new protocols combining unexpected results. When taken together, they tion4. Although the original definition of
chemotherapy with immunotherapy, indicate that there is a strong and develo- apoptosis excluded inflammation, it is now
indicating an exciting potential for ping case for combining chemotherapy and clear that innate immunity (BOX 1) can be
therapeutic synergy with general immunotherapy in cancer treatment. triggered by apoptosis and there has been
applicability to many cancer types. much speculation as to whether all forms of
Chemotherapy and cell death apoptosis are equivalent. Therefore, Restifo
Chemotherapy remains the treatment Different chemotherapies kill tumour cells in postulated that apoptosis occurring during
modality of choice for most advanced can- different ways and in the process they can development or tissue turnover is immuno-
cers. However, for solid tumours in particu- modulate the host immune system with con- logically bland, whereas apoptosis follow-
lar, it is rarely curative. Immunotherapy is a sequences that are only now beginning to be ing viral infections or ligation of the death
less conventional form of therapy and is fully elucidated. Here, we make the case for receptor FAS (also known as CD95) is
also rarely curative. Chemotherapy and adjuvant immunotherapy for patients under- intrinsically coupled to the production of
immunotherapy have usually been regarded going chemotherapy and we hypothesize how inflammatory signals that can trigger pow-
as unrelated or, more commonly, antagonis- different approaches to stimulating the erful immune responses5. Molecular flags
tic forms of therapy, so relatively few studies immune system could be used as the preferred which might be of either cellular or
have investigated the relationship between adjuvant therapy, depending on the particular microbial origin (BOX 1) differentiate
these treatments. Two a priori assumptions type of cancer and the choice of chemother- effete and harmless dying cells from those
have contributed to this state of affairs. First, apy. As tumour-cell death is the goal of most that are associated with danger so that
most chemotherapies kill target cells by chemotherapy, we will discuss how different harmless but potentially immunogenic
apoptosis and this mode of cell death has drugs kill tumour cells. We will then describe material is sequestered away from the
been regarded immunologically as either how each of the six key steps in the induction immune system, whereas antigens associ-
non-stimulatory or able to produce immune of an effective antitumour immune response ated with infection or danger are presented
tolerance a state where T cells can no (FIG. 1) might be altered by chemotherapy, in an immunogenic context3. The death of a
longer respond to the presented antigen by highlighting how these approaches could tumour cell, either naturally or induced by
mounting an immune response. Second, enable synergistic combinations of the two chemotherapy, where there is no inflamma-
lymphopaenia is a common side effect of forms of therapy to be used clinically. tion might be expected to appear like nor-
many anticancer drugs and this has also been mal tissue turnover, generating either no
assumed to be detrimental to any potential Death by apoptosis. Apoptosis is an intrinsic immune response (ignorance) or toler-
immune response. Although some studies mechanism by which cells die and it is ance. Some experiments support this
have probed the relationship between widely accepted that the willingness of cells hypothesis, showing that tumour-derived
chemotherapy and immune function in vivo, to die is usually countered by the provision antigens from a lymphoma and a solid
NATURE REVIEWS | C ANCER VOLUME 5 | MAY 2005 | 3 9 7
2005 Nature Publishing Group
PERSPECTIVES
positive outcome for this drug in combination
Lymph node
with a dendritic cell (DC)- (antigen-presenting
b CD8+ T cell
cell (APC))-based vaccination therapy20. Other
chemotherapy agents such as paclitaxel induce
an abnormal metaphase by damaging micro-
tubules and disrupting the mitotic spindle.
c Cyclin-dependent kinase 1 activation is abnor-
a Tumour cell
mally prolonged in paclitaxel-treated cells,
Tumour resulting in a bypassing of the G2 checkpoint
APC and cell death by mitotic catastrophe21,22. The
Antigen
CD8+ T cell
finding that paclitaxel is less effective than the
apoptosis-inducing drug doxorubicin when
coupled to a vaccination protocol for the treat-
Circulation
ment of aggressive breast cancer23 might indi-
cate that mitotic catastrophe errs on the side of
being immunologically bland.
e
Traffic Apoptosis and the immune response
It is evident that some mechanistic under-
f
d standing of the essential principles of
Tumour
blood vessel immune recognition is required before we
can discuss how dead and dying tumour
cells alter this process (BOX 1). It is generally
Memory T cell
accepted that the sort of immune response
that would be favourable to tumour elimina-
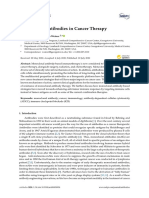
Figure 1 | The six steps necessary for an effective antitumour CD8+ T-cell response. Effective
destruction of tumours by antigen-specific CD8+ T cells is a multistep process. Each of these six steps is
tion will include the generation of large
required and can be modulated by a range of factors: tumour antigens must be present (a); these antigens numbers of interferon- (IFN)- and TNF-
must reach/load professional presenting cells antigen-presenting cells (APCs) in the draining lymph secreting CD8+ T cells with the capacity to
node (b); specific T cells must respond by proliferation (c); the circulating T cells must enter the tumour (d); directly lyse tumour-cell targets. Therefore,
once in the tumour the T cells must be able to overcome local immune-suppressive molecules to the key issues to be aware of in pairing
recognize and kill targets (e); memory cells should be generated (f). Cancer immunotherapy can fail at any chemotherapy with immunotherapy relate
of these steps, so the development of assays to analyse each of these steps in vivo (TABLE 1) has been
to the molecular flags associated with differ-
the key to beginning to understand how chemotherapy and immunotherapy interact. MHC; major
histocompability complex. ent forms of cell death and how they are
contextually interpreted.
There is increasing evidence that some
part of the apoptotic process is required for
tumour induce tolerance during tumour pro- been shown to increase the number of apop- generating an immune reaction. In a concep-
gression6,7. However, there is now increasing totic blasts in leukaemia11. Importantly, the tually simple series of experiments, Bonotte
evidence that, under the right circumstances, degree of apoptosis was found to correlate and colleagues showed that immunogenic
chemotherapy-induced tumour-cell death with clinical outcome for several different colon carcinoma cells were sensitive to apop-
can set the stage for an effective antitumour tumour types1214. tosis and died in vitro if they were starved of
immune response. growth factors. When these cells were made
Anticancer drugs can induce apoptosis Death by non-apoptotic mechanisms. resistant to apoptosis by overexpressing the
both by death-receptor-dependent and -inde- Apoptosis is not the only mechanism by which anti-apoptotic protein BCL2, they gave rise to
pendent pathways. Some anticancer drugs cells die. Non-apoptotic death pathways progressive tumours in vivo. Interestingly, the
increase the expression of death receptors, include necrosis, autophagy and mitotic cata- antigenicity of the BCL2-expressing apopto-
including FAS, tumour-necrosis factor strophe. These alternate forms of cell death are sis-resistant cells was not altered, because
(TNF) receptors and TNF-related apoptosis- differentiated by particular combinations of animals that had been pre-immunized with
inducing ligand receptors. Tumour cells morphological and biochemical changes15,16. parental immunogenic cells were able to
commonly show abnormalities to various Significantly, different chemotherapeutic drugs reject the BCL2-expressing cells24.
components of these pathways8, so tumours have been shown to induce different forms of Apoptosis might also be a necessary com-
are differentially sensitive to these drugs. cell death. Temozolomide, for example, is a rel- ponent of some vaccine strategies. The degree
Other drugs do not alter expression of death atively new alkylating agent that induces G2/M of apoptosis might help to explain the finding
receptors, but trigger apoptosis by inducing arrest and autophagy with no apoptosis17,18. that Alphavirus-based vaccines, which induce a
release of cytochrome c from mitochondria. There have been no systematic analyses of the high level of apoptosis, are generally highly
Although chemotherapeutic drugs induce effects of this drug on the immune system, but immunogenic despite the fact that they pro-
their primary damage in many different it is a powerful inhibitor of lymphocyte prolif- duce less antigen than conventional DNA-
ways, most of them induce apoptosis not eration, with only marginal effects on the activ- based vaccines. Leitner and colleagues switched
only in vitro but also in vivo 9,10. For example, ity of the natural-killer lymphocyte subset19. off apoptosis by overexpressing the anti-apop-
a diverse set of agents, including cytarabine, Indeed, a single case report focusing on a child totic gene BCL-XL in an Alphavirus-based
mitoxantrone, etoposide and topotecan, have with recurrent malignant glioma describes a immunization approach. As expected, they
398 | MAY 2005 | VOLUME 5 www.nature.com/reviews/cancer
2005 Nature Publishing Group
PERSPECTIVES
found that cells that were transfected with Box 1 | Alerting the immune system: difference, dose, danger and duration
BCL-XL lived longer and produced more anti-
gen, but in the absence of apoptosis the vaccine There are many ways that the host can eliminate unwanted cells. Probably the most effective
was significantly less protective25. Conversely, immunologically mediated host strategy is the deployment of cytotoxic T lymphocytes
DNA-based vaccination is enhanced by (CTLs) that can directly lyse targets and have the capacity to secrete effector cytokines such
delivering pro-apoptotic signals26,27. as interferon- and tumour-necrosis factor-. The conceptual problem for immunologists is
So what is the key feature of apoptosis that to understand how these cells can be targeted appropriately to discriminate between healthy
drives the acquired immune response? tissue, infected tissue and tumours.
Since Burnet defined the paradigm, immunologists have been comfortable with the view
Phosphatidylserine is probably the best-stud-
that the immune system works by having the capacity to discriminate between self and non-
ied molecular flag, but is almost certainly a
self 60. This concept of difference is of fundamental importance to the shape of the T-cell
downregulator of the immune response.
repertoire61. Tumours carry many mutations and it is now clear that most tumours express
Phosphatidylserine will become accessible to neo-antigens against which the host has a capacity to react. Of course, these antigens must
macrophages after non-apoptotic forms of cell achieve a threshold concentration, that is, dose, before they will trigger any response.
death when the plasma membrane loses its The paradigm of self was challenged by Matzinger and others, who suggested that the
integrity. But it is likely that there are separate primary drive to elicit an immune response was to protect against danger62,63. In the
signals associated with these dead cells, because absence of danger signals there is either no immune response or tolerance might be
the intracellular components that would oth- induced. Danger signals are thought to act principally at the level of antigen presentation
erwise be packaged into the apoptotic bodies to T cells to induce the professional
are released. Phosphatidylserine stimulates the antigen-presenting cells such as dendritic
production of a set of anti-inflammatory cells to mature and express stimulatory Cell and virus Cell and Cell and self
tumour antigen proteins only
mediators, including transforming growth ligands and cytokines. The simplest of the
factor-, prostanoids and interleukin-10 three main types of danger signal are the
(IL-10)28. It is now clear that recognition of conserved molecular motifs that are
phosphatidylserine, in the absence of any other ubiquitously carried by microorganisms64.
signal, has the capacity to suppress the release of Heat-shock proteins and uric acid are key
pro-inflammatory cytokines, including IL-12. among the mediators released by stressed
This occurs by direct transcriptional repression or damaged cells and can mark such cells
of the p35 IL-12 subunit, leading to a loss of for destruction by either T cells or natural-
IL-12 production29. It had been assumed that, killer cells. Missing self brings an
important supplementary concept an
because phagocytosis of cells dying by apopto-
immune response can be activated by the 'Dangerous' Weak Tolerizing
sis in vivo is efficient, tumour-cell apoptosis Cell damage No danger None of
loss of inhibitory signals that would (e.g. uric acid) signals these signals
would be likely to result in antigen sequestra-
normally block the initiation of immune Innate immunity No CD40
tion or tolerance induction. However, when responses against self . 65 activated signals
massive apoptosis occurs, the tolerogenic Toll-like Pro-
The fourth important D is duration receptors inflammatory
system might be overwhelmed, resulting in how long a particular antigen is around has triggered cytokines
secondary necrosis and release of pro-inflam- Inflammation
profound implications for the induction of Cytokines
matory mediators30. Some of the known immunological memory58. CD40 signals
activators of immune function include heat- These concepts are illustrated in the figure. Others
shock proteins (HSPs). The HSPs that are
induced by stressing apoptotic leukaemia cells
increases their capacity to activate DCs31.
Heat-stressed tumour cells induce changes in Non-apoptotic death and the immune The tumour immune response in vivo
DCs, including an upregulation of co-stimula- response. Few studies have investigated the The interaction between chemotherapy and
tory molecules (CD40, CD80 and CD86) immune response to non-apoptotic death immunotherapy has not been extensively
accompanied by an increase in IL-12 secre- caused by chemotherapy, largely because studied in vivo because the necessary tech-
tion. Under some circumstances, phagocytosis there are few such drugs; some of these nology has only recently been developed
of apoptotic cells leads to secretion of growth studies are cited above. Several studies (TABLE 1) . In vivo studies are necessary
and survival factors, including vascular based on in vitro work have found that because in vitro studies cannot accurately
endothelial growth factor32. Nevertheless, uric cell death by necrosis induces DCs to reflect the biology and dynamics of these
acid is probably the most powerful endoge- act as potent APCs, whereas apoptotic cell complex interactions. This technology
nous pro-inflammatory signal released from death does not have this effect34. Therefore, includes the development of appropriate
injured cells33. So it is clear that a series of in the steady state of normal tissue animal models and the ability to analyse
mediators interacting on a range of cell types turnover, apoptotic death seems to be tumour-antigen-specific immune responses
take part in a set of complex feedback interac- tolerogenic, whereas necrotic death is at each of the six key checkpoints of the
tions to determine the consequences of dead more likely to be associated with danger antitumour response (FIG. 1). These assays
cells for the immune system. And there is no and the induction of an immune response can help to determine where in the
single response to apoptotic cells, but, rather, (reviewed in REF. 35 and see BOX 1). The sequence of events a particular therapy
the response to such cells depends on the way immunological environment endured fails. For example, if the dose of antigen is
in which apoptosis has been induced, the following massive apoptotic cell death not limiting but the capacity of T cells to
amount of associated cellular stress and the after effective chemotherapy is likely to be expand is limited, then increasing the dose
pattern of regulatory cytokines. different, as discussed below. of antigen is unlikely to improve responses,
NATURE REVIEWS | C ANCER VOLUME 5 | MAY 2005 | 3 9 9
2005 Nature Publishing Group
PERSPECTIVES
Table 1 | Six key steps for specific CD8-mediated antitumour immunity mean that these antigens will induce a
response. The factors that determine whether
Step In vivo assay system for measuring response
an available antigen elicits an immune
Antigen threshold Quantification of levels of marker antigens by ELISA or western blot
response are explored in BOX 1.
Antigen presentation CFSE dye dilution assays66
T-cell response In vivo CTL assay using CFSE- and peptide-loaded target cells67; How might chemotherapy affect the dose of
tetramer analysis of tumour-specific T-cell numbers68; ELISPOT or antigens delivered for presentation? One of
intracellular cytokine staining for cytokine production can be
combined with other assays69 the key reference points for the generation of
a particular immune response is antigen dose
T-cell traffic Staining for T-cell infiltration; flow cytometry of extracted cells;
trafficking of dye-labelled cells (BOX 1). In a series of experiments using one
Target destruction Reduction in size of tumour; cytokine staining in tumour; function of of the above-described mouse models, we
cells extracted from the tumour were able to show that a tumour neo-antigen
Generation of memory Flow cytometry of extracted cells; adoptive transfer of extracted was constitutively and efficiently delivered to
cells; tumour growth after rechallenge the lymph nodes that drain the tumour, and
CSFE, 5,6-carboxyfluorescein diacetate succinimidyl ester; CTL, cytotoxic T lymphocyte; ELISA; enzyme- only those nodes, by a process known as
linked immunosorbance assay, ELISPOT: enzyme-linked spot recognition of specific T-cell function. cross-presentation39,40. Cross-presented anti-
gens cross from an exogenous source, which
typically delivers these antigens into the
whereas delivery of agents that support T-cell some will be efficiently delivered to the major histocompatibility complex class II
expansion is more likely to prove successful. immune system whereas others will not reach pathway, into the class I pathway, a pathway
These models and the tools to study them that threshold. When tumours regress with previously thought to be restricted to
have already produced new insights into anti- chemotherapy, increasing amounts of these endogenous antigens expressed exclusively by
tumour immune responses. We and others antigens are released from the dead and dying the cell itself. Despite this, little activation of
have transfected antigens into tumour cell lines cells and could be delivered into the antigen- antitumour CD8+ T-cell responses resulted
to act as markers to analyse tumour-specific presentation pathways, making them avail- except for low constitutive levels of cytotoxic
responses. These antigens do not alter the able to induce immune responses. It is likely T lymphocyte (CTL) activity restricted to the
immune response to the tumour, they simply that in this process some antigens that would draining lymph node. It is still not known
report back to the investigator what is hap- otherwise be below the threshold of availabil- whether live or dead or dying tumour cells
pening in vivo. The other crucial reagents in ity could now be presented to the hosts constitutively deliver these antigens into the
this system are tumour-antigen-specific T cells. immune system. This does not necessarily cross-presentation pathway.
Transgenic mice that express an identical T-cell
receptor on each functional T cell enable large
numbers of cells to be isolated and used to Table 2 | How chemotherapy could augment immunotherapy
analyse antigen presentation in vivo. These cells Essential steps in the Potential effects of chemotherapy on References
can be used as the cellular equivalent of induction of an antitumour the capacity of immunotherapy to
tumour-specific monoclonal antibodies. Using immune response destroy tumours
these tools, we can now begin to answer six key Antigen threshold Delivery of a broader range of different *
questions on how chemotherapy impacts on tumour antigens
the tumour immune response (TABLE 2). Antigen presentation Increased antigen cross-presentation 41
Partial activation of dendritic cells 41
How might chemotherapy affect the range of Priming of APCs for CD40 signal 50
antigens delivered for presentation? There
Killing subsets of APC 43
are large numbers, possibly tens or even
hundreds, of potential tumour antigens in T-cell response No tolerance induction by apoptotic tumour cells 41
any particular cancer3638. These are of two Lymphopaenia-related proliferation increases 57
tumour-specific T-cell response
types, neo and self, tumour antigens. Neo-
antigens are antigens that the host immune T-cell traffic Increased T-cell accumulation within tumour 50
system has never seen, so no tolerance has Target destruction Increased local tumour-antigen cross-presentation *
been induced. These are strong antigens and (permitting CD8 re-stimulation)
examples are mutated proteins and onco- Tumour debulking (less systemic suppression, 70
smaller target, less chance for escape variants etc.)
genic viruses. Self tumour antigens are
unmutated self proteins, but they are able to Partial sensitization of tumour cells for CTL lysis 55,56
induce immune responses because they have Generation of memory Promotion of long-term antigen-independent 58
limited expression in the host and therefore memory
limited opportunity for induction of toler- External regulation of Increased delivery of exogenous antigen 41
these steps
ance. Examples are proteins that have
expression limited to tumours and testes Increased CD4 help (for example, delivery of 50
CD40 signals)
(known as cancer-testis antigens) and dif-
ferentiation antigens that are not expressed Reduction in function of negative regulatory cells 44,46
in early life. These tumour antigens will be Induction of homeostatic proliferation 59
present at different concentrations so that *Not yet demonstrated in tumour models. APC, antigen-presenting cell; CTL, cytotoxic T lymphocyte.
400 | MAY 2005 | VOLUME 5 www.nature.com/reviews/cancer
2005 Nature Publishing Group
PERSPECTIVES
We hypothesized that if live cells were the a No tumour b Tumour only c Tumour and gemcitabine
main source of cross-presented antigens, one Undivided cells Dividing cells Dividing cells
would expect to see a relative loss of antigen
presentation in the draining lymph node fol-
lowing effective chemotherapy. In fact, not
Forward scatter
only was there no reduction in tumour-anti-
gen cross-presentation (FIG. 2), but when the
data were analysed by correcting for tumour
size, the amount of cross-presentation, as
determined by proliferation of the cells used
as markers of cross-presentation, approxi-
CFSE
mately doubled41. Because these assays are
functional, it is impossible to accurately quan- Figure 2 | Apoptosis delivers increased antigen loads into the antigen-presentation pathway.
BALB/c mice bearing tumours were treated with gemcitabine and antigen presentation was analysed by
tify how this change in proliferation equates
adoptively transferring tumour-antigen-specific lymphocytes that were labelled with the marker dye 5,6-
to the precise increase in the number of carboxyfluorescein diacetate succinimidyl ester (CFSE). Three days later, fluorescence-activated cell
molecules of antigen that appear in the cross- sorting was used to determine the proliferation status of the labelled lymphocytes. When no tumour
presentation pathway, but, based on other antigen is present there is no division and the peak of CFSE-loaded lymphocytes (marked with an arrow)
studies, this might correspond to a tenfold retains a high dye concentration (a). During normal tumour growth there is clear evidence of antigen
increase in the dose of antigen42. Certainly, it delivery, as additional peaks demonstrating a halving of CFSE concentration become visible (arrows in b).
After drug-induced apoptosis there is increased antigen presentation manifest as increased numbers of
is clear that chemotherapy-induced apoptosis
dividing cells (arrows in c).
in vivo does not sequester tumour antigens.
Rather, apoptotic tumour cells are a good
source of cross-presented tumour antigens.
Our published work on the effects of humoral (B-cell-mediated antibody) response are extracted and transferred to animals
chemotherapy-induced tumour-cell death for maximal efficacy might be compromised with immunogenic tumours, these tumours
in vivo has largely concentrated on the in patients treated with gemcitabine. start to grow progressively. A single admin-
anti-metabolite gemcitabine. This drug can istration of CTX to animals bearing tolero-
induce massive tumour-cell apoptosis both How might chemotherapy affect the antitu- genic, progressively growing tumours
in vitro and in vivo, is widely used in mour T-cell response in the draining lymph depletes regulatory T cells and delays the
human cancers, and in tumour-bearing node? Despite increasing tumour-antigen growth of the tumour. When CTX is com-
animals can reduce the volume of estab- presentation in the draining lymph node, bined with an immunotherapy that is not
lished tumours by over 80%. The observa- chemotherapy does not usually induce an curative by itself, the combination has the
tion that a gemcitabine-resistant tumour effective antitumour response by itself. In capacity to eradicate established tolerogenic
did not show any increase in tumour-anti- the clinic, it is rare for cancers that have par- tumours in animal models46.
gen cross-presentation indicated that the tially regressed in response to chemotherapy Given that an organism has a T-cell
capacity of chemotherapy-induced tumour- to then continue to regress through repertoire with the capacity to recognize a
cell death to load the draining lymph nodes immune mechanisms when the treatment given antigen (the issue of difference), two
with antigen was entirely attributable to the stops. Animal experiments support the view fundamental questions operationally define
induction of tumour-cell death and not that chemotherapy, as a single protocol that whether the immune system will respond
related to any non-specific effects of the is not curative, does not usually induce an to it. The first is whether the antigen is pre-
drug either on the cross-presenting func- immune response (see the section on mem- sent above a threshold dose level and the
tions of APCs or on the endogenous ory below). The notable exception to this second is whether the antigen is dangerous.
immune response41. Therefore, we hypothe- observation is cyclophosphamide (CTX). These questions are of course put and
size that any drug that kills tumour cells by The immunomodulatory effects of CTX answered in biochemical terms (BOX 1).
apoptosis will result in an increase in the have been known for a long time. In 1974, Duration of exposure to antigen also has
amount of cross-presented antigen. when the vogue for describing immune profound consequences for the develop-
Other ways that chemotherapy could responses in terms of suppressor circuits ment of immunological memory and is dis-
affect antigen presentation include a differen- was at its height, it was found that some cussed below. Understanding the specific
tial toxicity for particular subsets of cells. forms of tolerance could be reversed by molecular events that transmit dose and
Gemcitabine differentially depletes B cells and CTX. Appropriate doses of CTX have no danger signals is important for understand-
induces a profound suppression of antitu- major direct effect on the number of lym- ing how antitumour chemotherapy and
mour antibody responses43. B cells are phocytes but act by removing T-suppressor- immunotherapy could interact.
bona fide APCs and might drive immune cell activity 44. Suppressor cells are now more Cross-presented antigens will be ignored
responses towards the generation of antibod- usually characterized as regulatory T cells45. if there are no T cells with receptors of
ies and away from the generation of CTLs. Above, we discussed how immunogenic appropriate specificity. When there are
Removing them with gemcitabine does not colon carcinoma cells could be manipu- T cells that can respond, cross-presented
seem to be detrimental to specific antitumour lated and made tolerogenic by inhibiting antigen can lead to their activation and pro-
cellular immunity and might be useful in their tendency to apoptose. Tolerogenic liferation or can induce tolerance28,47. Cross-
combination chemoimmunotherapy proto- colon carcinoma cells grow progressively tolerance has been described for the antigen
cols, the aim of which is to generate CTLs. By in vivo with a corresponding expansion of used in our studies influenza virus
contrast, vaccination protocols requiring a regulatory T cells. If these regulatory T cells haemagglutinin (HA) when it is expressed
NATURE REVIEWS | C ANCER VOLUME 5 | MAY 2005 | 4 0 1
2005 Nature Publishing Group
PERSPECTIVES
as a self-antigen rather than as a tumour Viral signals can also drive this process, tumour-infiltrating T cells50. We speculate
neo-antigen. Transgenic Ins-HA mice as post-chemotherapy administration of that this occurs because of changes in the
express HA in the islet cells of the pancreas tumour-antigen-containing virus slows balance of inflammatory mediators in the
as a normal self-protein. These animals do tumour growth, whereas in the absence of local milieu. Overall, the increase in the
not develop immune-mediated insulitis or chemotherapy there is no effect41. number of tumour-infiltrating T cells could
diabetes when exposed to HA-specific CTLs, The reason why chemotherapy-induced be a direct effect of the drug on the tumour
because cross-presentation of HA is followed cell death primes rather than tolerizes host stroma or indirect, as a consequence of
by rapid activation and deletion of respon- immune responses is not yet known. It is increased phagocytosis. It is also possible
der T cells48. This process is known as possible that tumours create a partial that chemotherapy primes a tumour-
peripheral tolerance and is a well-estab- inflammatory environment, characterized specific CD4+ T-helper-cell response, as we
lished mechanism for avoiding destructive by the accumulation of macrophages and
autoimmune reactions49. the release of some pro-inflammatory
Tumour tissue might have been cytokines like TNF and IL-6 with the asso- a Anti-CD40 therapy without apoptosis
expected to behave like self-tissue and so ciated symptoms of weight loss, anorexia, 100
cross-tolerize antitumour T cells in the fevers and thrombocytosis. This balance
same way. It does not. Furthermore, between pro- and anti-inflammatory medi-
80
chemotherapy does not reduce the fre- ators might block CTL induction, but
quency of tumour-antigen-specific T cells. additional chemotherapy could increase the
Percent survival
Although it increases the rate of cross-pre- pro-inflammatory mediators such as HSPs 60
sentation and therefore the amount of anti- to sufficient levels to induce CD8+ T-cell
gen available to potentially cross-tolerize, it responses51. The increased number of dead
40
does not substantially reduce the activity of and dying tumour cells is also likely to
CTLs in vivo. Overall, the data do not sup- invoke an increase in phagocytosis, and if
port the view that the induction of tumour- these cells are activated, particularly by the 20
cell apoptosis tolerizes the tumour-specific release of intracellular contents, they might
CD8+ T-cell response. release more pro-inflammatory cytokines
0
However, chemotherapy-induced anti- and so increase the responsiveness of APCs 0 20 40 60 80 100 120 140
gen cross-presentation is not a null event. to cross-presented tumour antigens52. Days after tumour injection
Rather, it provides a fertile environment for Another possible direct effect of
Control
priming the host immune system for other chemotherapy on cross-priming has been Anti-CD40
immunostimulatory signals. Constitutive attributed to alkylating agents. In fact, any
tumour-antigen cross-presentation results drugs that modify DNA might have partic- b Anti-CD40 therapy with apoptosis
in cross-arming of effector CTLs, but these ular effects on the host immune response.
100
cells remain in the lymph node that drains For example, co-culture of immature DCs
the tumour. This pathway is the default with tumour cells treated with melphalan
process. What then determines whether an and chlorambucil caused the DCs to upreg- 80
APC that is loaded with antigen activates or ulate co-stimulatory molecules, secrete IL-12
Percent survival
tolerizes any T cells that it encounters? and efficiently activate T cells 53. These 60
One molecule on the APC that, when effects could be recapitulated using DNA
triggered, can cause a switch from tolerance purified from the killed tumour cells, sup-
40
to activation is CD40. CD40 signals deliv- porting the hypothesis that DNA damage is
ered to antigen-loaded APCs drive the itself recognized as inflammatory 53. The
process of T-cell priming and expansion precise mechanisms whereby chemother- 20
and also induce peripheral dissemination of apy partially primes APCs and antitumour
these CTLs so that they leave the lymph T-cell responses is now under investigation,
0
node and circulate. In the process, they as are the ways in which this can be aug- 0 20 40 60 80 100 120 140
retain strong antitumour killing capacity. mented by agents other than CD40 and
Days after tumour injection
Importantly, these T cells are now enabled tumour-antigen-containing viruses.
to destroy established tumours40. Whether Anti-CD40 before gemcitabine
these CD40 signals occur only in the drain- How might chemotherapy affect T-cell traf- Control (gemcitabine alone)
ing lymph node or at the tumour target site fic? One of the stumbling blocks in tumour Anti-CD40 after gemcitabine
is not yet clear. However, when CD40 signals immunology is the observation that it is Figure 3 | Established tumours can be
are delivered to hosts bearing large tumours possible to generate an antitumour cured when immunotherapy is delivered
it is no longer effective. It is clear though response that is measurable in the circula- following apoptosis induction. Mice with
that induction of apoptosis in large tumours tion but these T cells never enter the established tumours were treated with
not only loads the APCs with tumour anti- tumour. Why would they? Entry of T cells immunotherapy (anti-CD40 antibody) without
gens but also sensitizes them to CD40 sig- into any tissue is a highly orchestrated event chemotherapy (a) before a full course of the
apoptosis-inducing agent gemcitabine (b) or
nals, curing most mice studied in this way. and, as discussed above, untreated tumours following the same chemotherapy (c).
This immunotherapy is much more effec- are probably bland and anti-inflammatory. Phosphate-buffered saline injections were
tive if delivered after apoptosis-induced We have found that single-protocol used as controls. KaplanMeier survival curves
antigen loading rather than before50 (FIG. 3). chemotherapy caused an increased influx of are shown.
402 | MAY 2005 | VOLUME 5 www.nature.com/reviews/cancer
2005 Nature Publishing Group
PERSPECTIVES
have previously reported that these T cells single-protocol chemotherapy does not Clinical implications
can increase the infiltration or retention of induce an immune response if the tumour Measuring antitumour immune responses
CD8+ T cells into tumour sites39. continues to grow progressively. We became in humans has been difficult because of the
aware of the potential of chemotherapy to lack of defined tumour antigens and the
How might chemotherapy affect target-cell facilitate memory by rechallenging the occa- lack of available tools to study the six key
destruction? Even if tumour antigens are effi- sional long-term survivors of chemotherapy steps in vivo.
ciently presented, and even if T-cell responses (<2% of single-protocol-treated animals) However, the observations from animal
are induced and these cells traffic into with tumorigenic numbers of cells. They models have several implications for plan-
tumour sites, this still might not be enough all survived. ning future studies combining immunother-
to cause tumour destruction. There is some It has now been demonstrated that CD8+ apy with chemotherapy in human clinical
evidence to indicate that in order to work T-cell memory evolves differently if antigen cancer trials. First, as the level of cross-pre-
efficiently, CTLs require re-stimulation by persists. When antigen is removed, such as sented tumour antigen from established
professional APCs located in the tumour40. after an acute infection or successful tumours is increased by chemotherapy, it is
This process might invoke further rounds of chemotherapy, CD8+ T cells undergo anti- likely that the tumour itself will be a good
proliferation, so increasing the CTL fre- gen-driven proliferation and then differen- source of tumour antigens. This indicates
quency, and it might affect the threshold sen- tiate into effector CD8+ T cells and a small that there is no a priori requirement to
sitivity at which these cells are triggered as number of these cells develop into memory define, clone and purify individual tumour
well as qualitatively affect the secretion of CD8 + T cells. These cells persist for long antigens. Immunotherapy could then be
IFN and TNF. How and if chemotherapy periods in the absence of antigen. They aimed at boosting responses to endogenous
alters this process is not known, but the undergo homeostatic proliferation in cross-presented tumour antigens rather than
capacity of chemotherapy to deliver response to IL-7 and IL-15, and they delivering more antigen by, for example, vac-
increased antigen loads to APCs is not likely respond vigorously to antigen 57. By con- cination. Second, it cannot be assumed that
to be restricted to the draining lymph nodes trast, if antigen persists such as during a all drugs, even those that are known to
the APCs within tumours are also likely to chronic infection or during tumour growth, induce apoptosis, will have the same effects
receive increasing amounts of antigen, pro- even after a partial response to chemother- on the immune system as gemcitabine. At
viding at least some of the signals required apy, the antigen-independent phase of present, such data are not available for most
for CD8+ T-cell re-stimulation within memory CD8+ T-cell differentiation does drugs and future drug evaluation will
tumours. Effective chemotherapy results in not occur and memory CD8+ T cells are not require careful analysis. Third, individual
tumour debulking, which will change the properly induced 58. Obviously, antigens tumours will vary in their resistance to dif-
effector T cell to tumour-target ratio. This from a growing tumour would continue to ferent chemotherapy agents and to apopto-
could result in a non-linear amplification of be presented to the immune system, at least sis, and we do not know whether there is a
the ability of CTLs to kill targets. partially recapitulating the environment of direct relationship between death and prim-
Another way that chemotherapy could a chronic infection. Chemotherapy offers ing in this regard. It will be important to
augment the capacity of tumour-infiltrating the opportunity to modulate this process in determine which tumour characteristics
lymphocytes to deliver their effector response two ways that might prove beneficial to the make them suitable and this might require
is by upregulating death receptors54. Because induction of an effective immune response. individualization for each patient, by
T cells can use this pathway to kill targets, this First, chemotherapy might reduce the microarray analysis of apoptosis pathways.
can make the tumour cells more susceptible threshold of antigen delivery to the draining Fourth, as post-chemotherapy delivery of
to T-cell-mediated destruction55. These same node to a sufficiently low level to achieve immunotherapy was always more effective
drugs also have the capacity to sensitize can- the antigen-independent rest period that is than pretreatment, the timing of such
cer cells to lysis by weak, or low-avidity, CTLs required for the development of memory. immunotherapy is likely to be crucial. Also,
that would not otherwise kill them56. Drugs Second, if the chemotherapy induces some we noted that if the immunotherapy was
such as doxorubicin and methotrexate pro- level of lymphocyte loss (lymphopaenia), delayed following chemotherapy all the ben-
mote apoptosis in some tumour cells by the curious homeostatic response that is efits disappeared, presumably because either
inducing an upregulation in transcription of triggered to try to restore lymphocyte num- the antigen-loaded APCs were cleared or the
the gene encoding FAS ligand54. Other bers and fill the space might increase the partial priming of those APCs for CD40 sig-
chemotherapy agents alter apoptosis path- frequency of tumour-reactive T cells in the nals disappeared. In cancer immunotherapy
ways in different ways, thereby altering the process. These processes might have a role trials it is usual to leave about 1 month
threshold of apoptosis sensitivity. Where dif- in the effects of chemotherapy that have between cessation of chemotherapy and
ferent pathways to cell death synergize, we been observed in some experimental proto- commencement of immunotherapy. The
can hypothesize that these effects are likely to cols. For example, increased responses were data discussed above indicate that a protocol
increase the sensitivity of cancer cells to observed in melanoma patients who in which immunotherapy immediately fol-
immunologically mediated killing. received non-myeloablative chemotherapy lows chemotherapy, probably in repeating
before the adoptive transfer of activated cycles, might be more effective. Finally the
How might chemotherapy affect the genera- tumour-reactive T cells 59. Chemotherapy most appropriate adjuvant immunotherapy
tion of immunological memory? In addition might have increased the cross-presentation to be used in such studies can only be
to the antitumour effector responses of tumour cells in this trial; however, the determined empirically.
described above, the development of long- increased engraftment might have been As described above, immunotherapy in
term immunological memory could pro- independent of antigen stimulation and the form of an APC-directed CD40 signal
vide protection from both recurrence and might have occurred primarily as a result following chemotherapy-induced apop-
metastases. Previously, we have noted that of homeostasis. tosis cures most tumour-bearing mice.
NATURE REVIEWS | C ANCER VOLUME 5 | MAY 2005 | 4 0 3
2005 Nature Publishing Group
PERSPECTIVES
Humanized versions of CD40 antibodies are 7. Cuenca, A. et al. Extra-lymphatic solid tumor growth is 31. Feng, H., Zeng, Y., Graner, M. W. & Katsanis, E.
not immunologically ignored and results in early induction Stressed apoptotic tumor cells stimulate dendritic cells
now becoming available for clinical trials, of antigen-specific T-cell anergy: dominant role of cross- and induce specific cytotoxic T cells. Blood 100,
and studies combining chemotherapy with tolerance to tumor antigens. Cancer Res. 63, 90079015 41084115 (2002).
(2003). 32. Golpon, H. A. et al. Life after corpse engulfment:
this antibody can be undertaken. Another 8. Ozoren, N. & El-Deiry, W. S. Cell surface Death Receptor phagocytosis of apoptotic cells leads to VEGF
way to deliver a CD40 signal is through signaling in normal and cancer cells. Semin. Cancer Biol. secretion and cell growth. FASEB J. 18, 17161718
13, 135147 (2003). (2004).
CD4+ T cells, so protocols that induce strong 9. Mesner, P. W. Jr, Budihardjo, II & Kaufmann, S. H. 33. Shi, Y., Evans, J. E. & Rock, K. L. Molecular identification
antitumour CD4 responses could also be Chemotherapy-induced apoptosis. Adv. Pharmacol. 41, of a danger signal that alerts the immune system to dying
461499 (1997). cells. Nature 425, 516521 (2003).
combined with chemotherapy in the same 10. Kaufmann, S. H. & Earnshaw, W. C. Induction of 34. Sauter, B. et al. Consequences of cell death: exposure to
way. Viruses might also be used as adjuvants, apoptosis by cancer chemotherapy. Exp. Cell Res. 256, necrotic tumor cells, but not primary tissue cells or
4249 (2000). apoptotic cells, induces the maturation of
but in our studies the effects were not as 11. Li, X. et al. Apoptotic cell death during treatment of immunostimulatory dendritic cells. J. Exp. Med. 191,
powerful as those seen with CD40. leukemias. Leuk. Lymphoma 13 (Suppl. 1), 6570 423434 (2000).
(1994). 35. Skoberne, M., Beignon, A. S. & Bhardwaj, N. Danger
At least some of the past failures of 12. Kim, R., Nishimoto, N., Inoue, H., Yoshida, K. & Toge, T. signals: a time and space continuum. Trends Mol. Med.
immunotherapy can now be explained An analysis of the therapeutic efficacy of protracted 10, 251257 (2004).
infusion of low-dose 5-fluorouracil and cisplatin in 36. Robbins, P. in Tumor immunology: molecularly defined
based on our current ability to analyse anti- advanced gastric cancer. J. Infect. Chemother. 6, antigens and clinical applications (eds Parmiani, G. &
tumour immune responses in vivo. For 222228 (2000). Lotze, M.) 11 (Harwood Academic Publishers, London,
13. Cassinelli, G. et al. A role for loss of p53 function in 2002).
example, we might have used IL-2 in situa- sensitivity of ovarian carcinoma cells to taxanes. Int. J. 37. Novellino, L., Castelli, C. & Parmiani, G. A listing of
tions where not enough antigen was avail- Cancer 92, 738747 (2001). human tumor antigens recognized by T cells: March
14. Salomons, G. S. et al. Bcl-2 family members in childhood 2004 update. Cancer Immunol. Immunother. 54,
able in the lymph nodes, we might have acute lymphoblastic leukemia: relationships with features 187207 (2005).
waited too long before commencing at presentation, in vitro and in vivo drug response and 38. Kawakami, Y. & Rosenberg, S. A. Human tumor antigens
long-term clinical outcome. Leukemia 13, 15741580 recognized by T-cells. Immunol. Res. 16, 313339
immunotherapy after chemotherapy and (1999). (1997).
we might have picked the wrong adjuvants 15. Okada, H. & Mak, T. W. Pathways of apoptotic and non- 39. Marzo, A. L., Lake, R. A., Robinson, B. W. S. & Scott, B.
to combine with chemotherapy. Certainly, apoptotic death in tumour cells. Nature Rev. Cancer 4, T cell receptor transgenic analysis of tumor-specific CD8
592603 (2004). and CD4 responses in the eradication of solid tumors.
the capacity we now have to analyse the 16. Edinger, A. L. & Thompson, C. B. Death by design: Cancer Res. 59, 10711079 (1999).
precise way in which each component of apoptosis, necrosis and autophagy. Curr. Opin. Cell Biol. 40. Stumbles, P. A. et al. Cutting Edge: Tumor-specific CTL
16, 663669 (2004). are constitutively cross-armed in draining lymph nodes
the host antitumour immune system 17. Levine, B. & Klionsky, D. J. Development by self- and transiently disseminate to mediate tumor regression
engages with specific tumour antigens that digestion: molecular mechanisms and biological following systemic CD40 activation. J. Immunol. 173,
functions of autophagy. Dev. Cell 6, 463477 59235928 (2004).
are destroyed by chemotherapy drugs will (2004). 41. Nowak, A. K. et al. Induction of tumor cell apoptosis
enable any new clinical trials to be designed 18. Kanzawa, T. et al. Role of autophagy in temozolomide- in vivo increases tumor antigen cross-presentation,
induced cytotoxicity for malignant glioma cells. Cell Death cross-priming rather than cross-tolerizing host tumor-
on rational scientific foundations. A Differ. 11, 448457 (2004). specific CD8 T cells. J. Immunol. 170, 49054913
first encouraging example of the clinical 19. Pagani, E. et al. DNA repair enzymes and cytotoxic (2003).
effects of temozolomide: comparative studies between 42. Nelson, D., Bundell, C. & Robinson, B. In vivo cross-
reality of combining chemotherapy and tumor cells and normal cells of the immune system. presentation of a soluble protein antigen: kinetics,
immunotherapy in melanoma patients has J. Chemother. 15, 173183 (2003). distribution, and generation of effector CTL recognizing
20. De Vleeschouwer, S. et al. Transient local response and dominant and subdominant epitopes. J. Immunol. 165,
now been published, as discussed above59. persistent tumor control in a child with recurrent 61236132 (2000).
Although the specific protocol was techni- malignant glioma: treatment with combination therapy 43. Nowak, A. K., Robinson, B. W. & Lake, R. A.
including dendritic cell therapy. Case report. Gemcitabine exerts a selective effect on the humoral
cally challenging, the clinical outcome was J. Neurosurg. Spine 100, 492497 (2004). immune response: implications for combination
extremely promising. 21. Jordan, M. A. et al. Mitotic block induced in HeLa cells by chemo-immunotherapy. Cancer Res. 62, 23532358
low concentrations of paclitaxel (Taxol) results in (2002).
Richard A. Lake is at the Tumour abnormal mitotic exit and apoptotic cell death. Cancer 44. Polak, L. & Turk, J. L. Reversal of immunological
Immunology Group, School of Medicine and Res. 56, 816825 (1996). tolerance by cyclophosphamide through inhibition of
22. Russell, P. & Nurse, P. cdc25+ functions as an inducer in suppressor cell activity. Nature 249, 654656
Pharmacology, Western Australian Institute for
the mitotic control of fission yeast. Cell 45, 145153 (1974).
Medical Research, Perth, 6009, Australia. (1986). 45. Fehervari, Z. & Sakaguchi, S. Development and function
23. Eralp, Y. et al. Doxorubicin and paclitaxel enhance the of CD25+CD4+ regulatory T cells. Curr. Opin. Immunol.
Bruce W. S. Robinson is at the School antitumor efficacy of vaccines directed against HER 16, 203208 (2004).
of Medicine and Pharmacology, 2/neu in a murine mammary carcinoma 46. Ghiringhelli, F. et al. CD4+CD25+ regulatory T cells
4th Floor, G-block, model. Breast Cancer Res. 6, R275R283 (2004). suppress tumor immunity but are sensitive to
Sir Charles Gairdner Hospital, Nedlands, Perth, 24. Bonnotte, B. et al. Bcl-2-mediated inhibition of apoptosis cyclophosphamide which allows immunotherapy of
6009, Australia. prevents immunogenicity and restores tumorigenicity of established tumors to be curative. Eur. J. Immunol. 34,
spontaneously regressive tumors. J. Immunol. 161, 336344 (2004).
Correspondence to R.A.L. 14331438 (1998). 47. Heath, W. R. & Carbone, F. R. Cross-presentation in viral
e-mail: rlake@cyllene.uwa.edu.au 25. Leitner, W. W. et al. Apoptosis is essential for the immunity and self-tolerance. Nature Rev. Immunol. 1,
increased efficacy of alphaviral replicase-based DNA 126134 (2001).
doi: 10.1038/nrc1613 vaccines. Vaccine 22, 15371544 (2004). 48. Morgan, D. J., Kreuwel, H. T. & Sherman, L. A.
Published online 20 April 2005 26. Sasaki, S., Amara, R. R., Oran, A. E., Smith, J. M. & Antigen concentration and precursor frequency
Robinson, H. L. Apoptosis-mediated enhancement of determine the rate of CD8+ T cell tolerance to
1. Raff, M. C. Social controls on cell survival and cell death. DNA-raised immune responses by mutant caspases. peripherally expressed antigens. J. Immunol. 163,
Nature 356, 397400 (1992). Nature Biotechnol. 19, 543547 (2001). 723727 (1999).
2. Degterev, A., Boyce, M. & Yuan, J. A decade of 27. Chattergoon, M. A. et al. Targeted antigen delivery to 49. Miller, J. F. & Morahan, G. Peripheral T cell tolerance.
caspases. Oncogene 22, 85438567 (2003). antigen-presenting cells including dendritic cells by Annu. Rev. Immunol. 10, 5169 (1992).
3. Savill, J. & Fadok, V. Corpse clearance defines the engineered Fas-mediated apoptosis. Nature Biotechnol. 50. Nowak, A. K., Robinson, B. W. & Lake, R. A. Synergy
meaning of cell death. Nature 407, 784788 (2000). 18, 974979 (2000). between chemotherapy and immunotherapy in the
4. Kerr, J. F., Wyllie, A. H. & Currie, A. R. Apoptosis: a 28. Steinman, R. M., Turley, S., Mellman, I. & Inaba, K. The treatment of established murine solid tumors. Cancer
basic biological phenomenon with wide-ranging induction of tolerance by dendritic cells that have Res. 63, 44904496 (2003).
implications in tissue kinetics. Br. J. Cancer 26, captured apoptotic cells. J. Exp. Med. 191, 411416 51. Srivastava, P. Interaction of heat shock proteins with
239257 (1972). (2000). peptides and antigen presenting cells: chaperoning of the
5. Restifo, N. P. Building better vaccines: how apoptotic cell 29. Kim, S., Elkon, K. B. & Ma, X. Transcriptional innate and adaptive immune responses. Annu. Rev.
death can induce inflammation and activate innate and suppression of interleukin-12 gene expression following Immunol. 20, 395425 (2002).
adaptive immunity. Curr. Opin. Immunol. 12, 597603 (2000). phagocytosis of apoptotic cells. Immunity 21, 643653 52. Fadok, V. A., Bratton, D. L., Guthrie, L. & Henson, P. M.
6. Sotomayor, E. M. et al. Cross-presentation of tumor (2004). Differential effects of apoptotic versus lysed cells on
antigens by bone marrow-derived antigen-presenting 30. Rovere, P. et al. Delayed clearance of apoptotic macrophage production of cytokines: role of proteases.
cells is the dominant mechanism in the induction of T-cell lymphoma cells allows cross-presentation of intracellular J. Immunol. 166, 68476854 (2001).
tolerance during B-cell lymphoma progression. Blood 98, antigens by mature dendritic cells. J. Leukoc. Biol. 66, 53. Rad, A. N. et al. The differential influence of allogeneic
10701077 (2001). 345349 (1999). tumor cell death via DNA damage on dendritic cell
404 | MAY 2005 | VOLUME 5 www.nature.com/reviews/cancer
2005 Nature Publishing Group
PERSPECTIVES
maturation and antigen presentation. Cancer Res. 63,
51435150 (2003).
54. Friesen, C., Herr, I., Krammer, P. H. & Debatin, K. M. OPINION
Involvement of the CD95 (APO-1/FAS) receptor/ligand
system in drug-induced apoptosis in leukemia cells.
Nature Med. 2, 574577 (1996).
55. Bergmann-Leitner, E. S. & Abrams, S. I. Treatment
of human colon carcinoma cell lines with anti-
Post-prenylation-processing enzymes
neoplastic agents enhances their lytic sensitivity to
antigen-specific CD8 + cytotoxic T lymphocytes.
Cancer Immunol. Immunother. 50, 445455
(2001).
as new targets in oncogenesis
56. Yang, S. & Haluska, F. G. Treatment of melanoma with
5-fluorouracil or dacarbazine in vitro sensitizes cells to
antigen-specific CTL lysis through perforin/granzyme- Ann M. Winter-Vann and Patrick J. Casey
and Fas-mediated pathways. J. Immunol. 172,
45994608 (2004).
57. Kaech, S. M. et al. Selective expression of the interleukin 7
Abstract | RAS and many other oncogenic with various human cancers7, and is a princi-
receptor identifies effector CD8 T cells that give rise to proteins undergo a complex series of ple step in a mechanism that can efficiently
long-lived memory cells. Nature Immunol. 4, 11911198
(2003).
post-translational modifications that are transform tissue-explant human cells8. In
58. Wherry, E. J., Barber, D. L., Kaech, S. M., Blattman, initiated by the addition of an isoprenoid addition, many cancers contain alterations in
J. N. & Ahmed, R. Antigen-independent memory
CD8 T cells do not develop during chronic viral
lipid through a process known as elements that lie upstream of RAS in signalling
infection. Proc. Natl Acad. Sci. USA 101, prenylation. Following prenylation, these cascades such as the amplified expression
1600416009 (2004).
59. Dudley, M. E. et al. Cancer regression and
proteins usually undergo endoproteolytic or mutational activation of tyrosine kinases
autoimmunity in patients after clonal repopulation with processing by the RCE1 protease and and the resultant hyperactivation of RAS is
antitumor lymphocytes. Science 298, 850854
then carboxyl methylation by a unique thought to contribute to tumorigenesis7,9,10.
(2002).
60. Burnet, F. M. Immunological recognition of self. Science methyltransferase known as The targeting of RAS signalling pathways is
133, 307311 (1961). isoprenylcysteine carboxyl therefore important for research into the
61. Mason, D. A very high level of crossreactivity is an
essential feature of the T-cell receptor. Immunol. Today methyltransferase (ICMT). Although development of therapeutics.
19, 395404 (1998). inhibitors that have been designed to In addition to the RAS proteins them-
62. Matzinger, P. Tolerance, danger, and the extended family.
Annu. Rev. Immunol. 12, 9911045 (1994). target the prenylation step are now in selves, several other CAAX proteins are
63. Janeway, C. A. Jr. The immune system evolved to advanced-stage clinical trials, their utility involved in the initiation and progression of
discriminate infectious nonself from noninfectious self.
Immunol. Today 13, 1116 (1992). and efficacy seem to be limited. Recent cancer (TABLE 1). The RHO family of GTPases,
64. Medzhitov, R. & Janeway, C., Jr. Innate immune findings, however, indicate that the which includes RAC and CDC42, is implicated
recognition: mechanisms and pathways. Immunol. Rev.
173, 8997 (2000). inhibition of these post-prenylation- in both oncogenesis and metastasis11,12.
65. Medzhitov, R. & Janeway, C. A. Jr. Decoding the patterns processing steps particularly that of Increased signalling by yet another GTPase,
of self and nonself by the innate immune system. Science
296, 298300 (2002). ICMT-catalysed methylation might RAP1A, has been associated with myeloprolif-
66. Lyons, A. B. & Parish, C. R. Determination of lymphocyte provide a better approach to the control eration13. Constitutive activation of G-protein-
division by flow cytometry. J. Immunol. Methods 171,
131137 (1994). of cancer-cell proliferation. coupled receptor (GPCR) pathways can also
67. Oehen, S. & Brduscha-Riem, K. Differentiation of naive contribute to transformation1418, and the
CTL to effector and memory CTL: correlation of effector
function with phenotype and cell division. J. Immunol.
A broad class of eukaryotic proteins contain -subunits of heterotrimeric G proteins are all
161, 53385346 (1998). a carboxy-terminal CAAX motif, in which CAAX proteins16. The list of CAAX proteins
68. Davis, M. M. et al. Ligand recognition by T cell
receptors. Annu. Rev. Immunol. 16, 523544
the C denotes cysteine, the A residues are also includes many phosphatases and kinases
(1998). usually aliphatic, and X represents any mutations in several of these are associated
69. Miyahira, Y. et al. Quantification of antigen specific CD8+
T cells using an ELISPOT assay. J. Immunol. Methods
amino acid1,2. The CAAX motif directs pro- with cancer19,20. Finally, in both normal and
181, 4554 (1995). teins through a series of post-translational transformed cells, CAAX proteins including
70. North, R. J. & Kirstein, D. P. T-cellmediated concomitant
immunity to syngeneic tumors. I. Activated macrophages
modifications that are initiated by the the nuclear lamins A and B, and the cen-
as the expressors of nonspecific immunity to unrelated attachment of a 15-carbon farnesyl or a tromeric proteins CENP-E and CENP-F are
tumors and bacterial parasites. J. Exp. Med. 145,
275292 (1977).
20-carbon geranylgeranyl lipid to the cys- involved in processes that are important for cell
teine residue by protein farnesyltransferase division and nuclear-envelope assembly/disas-
Acknowledgements (FTase) or protein geranylgeranyltrans- sembly21,22. Therefore, it is clear that CAAX
We thank the current and former members of the Tumour
Immunology Group, but we are particularly grateful to R. van der ferase-I (GGTase-I), respectively3. Following proteins have a diverse range of functions
Most for proof reading the evolving manuscript and consistently the attachment of the isoprenoid, the AAX inside cells, but one common theme is that
thought-provoking debate. We apologize for our failure to fully
acknowledge many important contributions to this area. This tripeptide is removed in a reaction that is many of these proteins are involved in intracel-
research was supported by grants from the National Health and catalysed by a prenyl-protein-specific pro- lular regulatory processes that are important
Medical Research Council of Australia and the Cancer Council of
Western Australia. R.L. is supported by the Insurance tease known as RCE1, whereas in the third for tumorigenesis.
Commission of Western Australia. processing step a methyl group is trans- The most widely documented function of
Competing interests statement ferred to the now C-terminal prenylcysteine prenylation is to direct CAAX proteins to
The authors declare no competing interests. by the enzyme isoprenylcysteine carboxyl cellular membranes, although, in many
methyltransferase4,5 (ICMT; FIG. 1). cases, the modified C terminus is important
Online links Although many proteins are probably in proteinprotein interactions as well1,23.
DATABASES subject to the CAAX-processing pathway Regardless of how the protein uses its modi-
The following terms in this article are linked online to: (BOX 1), members of the RAS family of fied cysteine residue, one aspect is very clear
Entrez Gene:
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=gene GTPases, which almost all contain the CAAX the modifications are crucial for the bio-
BCL2 | BCL-XL | CD40 | FAS | IFN | IL-10 | IL-12 | IL-6 | TNF motif, are particularly interesting because of logical activities of the proteins2427. For this
National Cancer Institute: http://cancer.gov/
melanoma
their well-established role in oncogenesis6,7. reason, the CAAX protein prenyltransferases,
Access to this interactive links box is free online. Mutational activation of RAS is associated most notably FTase, have been the focus of
NATURE REVIEWS | C ANCER VOLUME 5 | MAY 2005 | 4 0 5
2005 Nature Publishing Group
También podría gustarte
- Immunogenic Cell Death in Cancer Review 2019Documento12 páginasImmunogenic Cell Death in Cancer Review 2019Kudelko MatAún no hay calificaciones
- Terapia Inmunomoduladora 1Documento9 páginasTerapia Inmunomoduladora 1Nathy Pasapera AlbanAún no hay calificaciones
- Melero 2007Documento12 páginasMelero 2007Django BoyeeAún no hay calificaciones
- The Future of Immune Checkpoint Therapy: Padmanee Sharma and James P. AllisonDocumento6 páginasThe Future of Immune Checkpoint Therapy: Padmanee Sharma and James P. Allisonlos mejores icfesAún no hay calificaciones
- Harnessing Bene Fit From Targeting Tumor Associated Carbohydrate AntigensDocumento9 páginasHarnessing Bene Fit From Targeting Tumor Associated Carbohydrate Antigensspin_echoAún no hay calificaciones
- Inmunoterapia en Cancer de PulmonDocumento7 páginasInmunoterapia en Cancer de PulmonJorge ZegarraAún no hay calificaciones
- Targeted Therapies CCR2008Documento7 páginasTargeted Therapies CCR2008Marie ChaisanaAún no hay calificaciones
- Biologic Therapies: What and When?: ReviewDocumento10 páginasBiologic Therapies: What and When?: ReviewRameshKrishnanAún no hay calificaciones
- Aranda 2015Documento11 páginasAranda 2015TrabelsiAún no hay calificaciones
- Eisenberg 2012Documento13 páginasEisenberg 2012Juan G. Ovalles B.Aún no hay calificaciones
- Natural Killer Cell Immunomodulation: Targeting Activating, Inhibitory, and Co-Stimulatory Receptor Signaling For Cancer ImmunotherapyDocumento9 páginasNatural Killer Cell Immunomodulation: Targeting Activating, Inhibitory, and Co-Stimulatory Receptor Signaling For Cancer Immunotherapyhoangphuong08101992Aún no hay calificaciones
- Immunopotentiation: Immunopotentiation Can Be Defined As The ProcessDocumento67 páginasImmunopotentiation: Immunopotentiation Can Be Defined As The ProcesssamyAún no hay calificaciones
- Advancing Immunology ResearchDocumento60 páginasAdvancing Immunology ResearchgeorgescumirelaligiaAún no hay calificaciones
- Polymer Drug Conjugates As Potent Against Cellular ApoptosisDocumento8 páginasPolymer Drug Conjugates As Potent Against Cellular ApoptosisGourav DasAún no hay calificaciones
- Host Defence Mechanisms Against TumorsDocumento7 páginasHost Defence Mechanisms Against TumorsHamam AmastrdamAún no hay calificaciones
- Immunotherapeutic Strategies for the Treatment of GliomaDe EverandImmunotherapeutic Strategies for the Treatment of GliomaAún no hay calificaciones
- Cancer Immunotherapy Beyond Checkpoint BlockadeDocumento16 páginasCancer Immunotherapy Beyond Checkpoint Blockaderaxi bacumabAún no hay calificaciones
- Ru Ella 2013Documento25 páginasRu Ella 2013Ruben NatarîșAún no hay calificaciones
- Immune Checkpointtargeted Therapy Cancer and Autoimmune Diseases Represent Two Sides of The Same CoinDocumento4 páginasImmune Checkpointtargeted Therapy Cancer and Autoimmune Diseases Represent Two Sides of The Same Coinpratiwi eka rahmawatiAún no hay calificaciones
- (24508608 - Journal of Veterinary Research) Mechanisms of Tumour Escape From Immune SurveillanceDocumento8 páginas(24508608 - Journal of Veterinary Research) Mechanisms of Tumour Escape From Immune Surveillancekalppena naiduAún no hay calificaciones
- Kroemer 2015Documento11 páginasKroemer 2015ADanAlfaAún no hay calificaciones
- Cancer Immunology: Bench to Bedside Immunotherapy of CancersDe EverandCancer Immunology: Bench to Bedside Immunotherapy of CancersAún no hay calificaciones
- Pancreatic CancerDocumento9 páginasPancreatic Cancernski2104Aún no hay calificaciones
- ImmunityDocumento3 páginasImmunityHypermedic MXAún no hay calificaciones
- Tumor Immune Microenvironment in Cancer Progression and Cancer TherapyDe EverandTumor Immune Microenvironment in Cancer Progression and Cancer TherapyPawel KalinskiAún no hay calificaciones
- Celulas InmunoterapiaDocumento6 páginasCelulas InmunoterapiaDome Leon TapiaAún no hay calificaciones
- Fimmu 10 01205Documento16 páginasFimmu 10 01205Vostie1811Aún no hay calificaciones
- Research Guide: Improve Immunity in Clinical PracticeDocumento8 páginasResearch Guide: Improve Immunity in Clinical PracticeNacer BechouAún no hay calificaciones
- Microbiome Derived Metabolome As A PotenDocumento3 páginasMicrobiome Derived Metabolome As A PotenJULIETAAún no hay calificaciones
- Weiner 1Documento8 páginasWeiner 1Raúl ChoqueAún no hay calificaciones
- Principles of Cancer Treatment by ChemotherapyDocumento6 páginasPrinciples of Cancer Treatment by ChemotherapySisy AnandaAún no hay calificaciones
- Immunological Aspects of Cancer ChemotherapyDocumento15 páginasImmunological Aspects of Cancer Chemotherapyprashantb07.2409Aún no hay calificaciones
- Fonc 08 00086Documento14 páginasFonc 08 00086Siska HarapanAún no hay calificaciones
- Immune Crosstalk in Cancer Progression and Metatic Spread (2020)Documento15 páginasImmune Crosstalk in Cancer Progression and Metatic Spread (2020)EshaAún no hay calificaciones
- The Paradox of Tumor-Associated Neutrophils Fueling Tumor Growth With Cytotoxic SubstancesDocumento7 páginasThe Paradox of Tumor-Associated Neutrophils Fueling Tumor Growth With Cytotoxic SubstancesPilar AufrastoAún no hay calificaciones
- Drug Acting On Immune SystemDocumento7 páginasDrug Acting On Immune SystemAnne Giselle PatocAún no hay calificaciones
- 2021-Review-Tumour Neoantigen Mimicry by Microbial Species in Cancer ImmunotherapyDocumento11 páginas2021-Review-Tumour Neoantigen Mimicry by Microbial Species in Cancer ImmunotherapyCristian Felipe Sandoval QuiñonezAún no hay calificaciones
- Fimmu 11 00139Documento3 páginasFimmu 11 00139carlosAún no hay calificaciones
- Targeted Therapy in Oncology: Update ArticleDocumento5 páginasTargeted Therapy in Oncology: Update ArticleRajeev GuptaAún no hay calificaciones
- Antibodies 09 00034Documento20 páginasAntibodies 09 00034nazli meerahAún no hay calificaciones
- Tumor MicroenvironmentDe EverandTumor MicroenvironmentPeter P. LeeAún no hay calificaciones
- Dysregulation of Apoptotic Signaling in Cancer: Molecular Mechanisms and Therapeutic OpportunitiesDocumento26 páginasDysregulation of Apoptotic Signaling in Cancer: Molecular Mechanisms and Therapeutic OpportunitiesFrontiersAún no hay calificaciones
- Acetaminophen-Induced Liver Injury: From Animal Models To HumansDocumento8 páginasAcetaminophen-Induced Liver Injury: From Animal Models To HumansMiguel Adrian GaonaAún no hay calificaciones
- 10 1056@NEJMra1911109 PDFDocumento11 páginas10 1056@NEJMra1911109 PDFMартин ДончевAún no hay calificaciones
- Immunointervention in Autoimmune Diseases: Papers Based on an International Meeting in Paris, France, in June 1988De EverandImmunointervention in Autoimmune Diseases: Papers Based on an International Meeting in Paris, France, in June 1988J. F. BachAún no hay calificaciones
- Art 1Documento9 páginasArt 1Duayt StiflerAún no hay calificaciones
- Brentuximab Vedotin - Driven Microtubule Disruption Results in Endoplasmic Reticulum Stress Leading To Immunogenic Cell Death and Antitumor ImmunityDocumento16 páginasBrentuximab Vedotin - Driven Microtubule Disruption Results in Endoplasmic Reticulum Stress Leading To Immunogenic Cell Death and Antitumor ImmunitySamet KaradoğanAún no hay calificaciones
- Cancer ImmunologyDocumento21 páginasCancer ImmunologyYuda PrabawaAún no hay calificaciones
- Green-Tsui2013 Article ImpactOfAnesthesiaForCancerSurDocumento22 páginasGreen-Tsui2013 Article ImpactOfAnesthesiaForCancerSurNataAún no hay calificaciones
- Molecules: A Review On Cancer Immunotherapy and Applications of Nanotechnology To Chemoimmunotherapy of Different CancersDocumento24 páginasMolecules: A Review On Cancer Immunotherapy and Applications of Nanotechnology To Chemoimmunotherapy of Different CancersJuan Vera SanchezAún no hay calificaciones
- A Mathematical Approach To Distinguish Spontaneous From Induced Evolution of Drug Resistance During Cancer TreatmentDocumento20 páginasA Mathematical Approach To Distinguish Spontaneous From Induced Evolution of Drug Resistance During Cancer Treatmentsysbio10Aún no hay calificaciones
- CA A Cancer J Clinicians - May June 2005 - Ghobrial - Targeting Apoptosis Pathways in Cancer TherapyDocumento17 páginasCA A Cancer J Clinicians - May June 2005 - Ghobrial - Targeting Apoptosis Pathways in Cancer Therapyonur ateşAún no hay calificaciones
- Review On Macrophages in Tumors Feb 2019 NatureDocumento14 páginasReview On Macrophages in Tumors Feb 2019 NatureKudelko MatAún no hay calificaciones
- WRR 12952Documento14 páginasWRR 12952randomaeiou7273Aún no hay calificaciones
- 1 s2.0 S104453232100066X MainDocumento17 páginas1 s2.0 S104453232100066X MainAnita DewiAún no hay calificaciones
- Cancer Immunology and ImmunotherapyDocumento15 páginasCancer Immunology and ImmunotherapyRamona PalalogosAún no hay calificaciones
- KCBT 18 07 1323596 PDFDocumento19 páginasKCBT 18 07 1323596 PDFFitria Rizky AmaliaAún no hay calificaciones
- Reviews: Systemic Immunity in CancerDocumento15 páginasReviews: Systemic Immunity in Cancerliliana-contrerasAún no hay calificaciones
- Rycan 2021200134Documento6 páginasRycan 2021200134Sakkuru Yeyen LiviaAún no hay calificaciones
- Immunosupresive AgentDocumento12 páginasImmunosupresive AgentTamam JauharAún no hay calificaciones
- Spooky Scary SkeletonDocumento6 páginasSpooky Scary SkeletonPiano Covers0% (1)
- 6 1 1 P SR StudentresponsesheetDocumento4 páginas6 1 1 P SR Studentresponsesheetapi-245157052Aún no hay calificaciones
- ScienceGeography3ResourceSample PDFDocumento9 páginasScienceGeography3ResourceSample PDFmargantoniAún no hay calificaciones
- Lab 18Documento2 páginasLab 18Shamarie Love MaribaoAún no hay calificaciones
- Large Intestine CA 2Documento21 páginasLarge Intestine CA 2Worku KifleAún no hay calificaciones
- Cell CytoplasmDocumento55 páginasCell Cytoplasmnicolaer111100% (1)
- Reviewer of Anatomy and Physiology (Basics)Documento3 páginasReviewer of Anatomy and Physiology (Basics)Sophia AndayaAún no hay calificaciones
- June 2016 (v3) QP - Paper 2 CIE Biology IGCSEDocumento20 páginasJune 2016 (v3) QP - Paper 2 CIE Biology IGCSEKamikazi GloriaAún no hay calificaciones
- Blood ProductDocumento35 páginasBlood Productrajan kumar100% (3)
- Muscular System MindmapDocumento1 páginaMuscular System MindmapMayeliz UrvinaAún no hay calificaciones
- 9B Respiration - Gaseous Exchange in Man PDFDocumento18 páginas9B Respiration - Gaseous Exchange in Man PDFabdulrehman mughalAún no hay calificaciones
- Immunology of The Lymphatic System PDFDocumento180 páginasImmunology of The Lymphatic System PDFCNPOULISAún no hay calificaciones
- MVW 020Documento9 páginasMVW 020SofyanAún no hay calificaciones
- Mitosis PresentationDocumento24 páginasMitosis Presentationapi-267309851Aún no hay calificaciones
- Bio Mechanics of Spinal ColumnDocumento59 páginasBio Mechanics of Spinal ColumnOnwaree Ing100% (4)
- The Skeletal SystemDocumento3 páginasThe Skeletal SystemMiguel GumatayAún no hay calificaciones
- Cervical and Shoulder 2020Documento14 páginasCervical and Shoulder 2020Eduardo OlivaAún no hay calificaciones
- KP 2. Pengaruh Agen Biologi Dan Mekanisme Perubahan Sel Serta Penyakit Yang DitimbulkannyaDocumento28 páginasKP 2. Pengaruh Agen Biologi Dan Mekanisme Perubahan Sel Serta Penyakit Yang DitimbulkannyaShintia Surya PutriAún no hay calificaciones
- Connective TissueDocumento62 páginasConnective Tissuehnm mnhAún no hay calificaciones
- Module 5 HomeworkDocumento4 páginasModule 5 HomeworkCj LinceAún no hay calificaciones
- Floyd17 TB Ch12Documento5 páginasFloyd17 TB Ch12sdjuknicAún no hay calificaciones
- Nephrotic SyndromeDocumento38 páginasNephrotic SyndromeSwati SharmaAún no hay calificaciones
- Bast 1928Documento5 páginasBast 1928silviaAún no hay calificaciones
- Study Guide: Cytokines Associated With Innate ImmunityDocumento12 páginasStudy Guide: Cytokines Associated With Innate ImmunityxxxxxxxAún no hay calificaciones
- Physiology of Hemostasis - Dr. Rahmat Dani Satria PH.D., SP - PK (K)Documento27 páginasPhysiology of Hemostasis - Dr. Rahmat Dani Satria PH.D., SP - PK (K)Viand NugrohoAún no hay calificaciones
- Cell StrucutreDocumento40 páginasCell StrucutreJeevitha VanithaAún no hay calificaciones
- Unit 1 Anatomy, Physiology and The Human Body: Learning OutcomesDocumento91 páginasUnit 1 Anatomy, Physiology and The Human Body: Learning OutcomesDeolita BadiangAún no hay calificaciones
- Gastric Neuroendocrine TumorsDocumento17 páginasGastric Neuroendocrine TumorsNelsonLopezAún no hay calificaciones
- Pigeon DissectionDocumento10 páginasPigeon DissectionAnonymous 3NmUUDtAún no hay calificaciones
- Body Systems Chart System Illustration Structures Function: DigestiveDocumento3 páginasBody Systems Chart System Illustration Structures Function: DigestiveMicaela DAún no hay calificaciones