Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Gastric Mucosal Damage in Water Immersion Stress Mechanism and Prevention With GHRP-6
Cargado por
Fitria DewinurDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Gastric Mucosal Damage in Water Immersion Stress Mechanism and Prevention With GHRP-6
Cargado por
Fitria DewinurCopyright:
Formatos disponibles
Online Submissions: http://www.wjgnet.
com/1007-9327office World J Gastroenterol 2012 June 28; 18(24): 3145-3155
wjg@wjgnet.com ISSN 1007-9327 (print) ISSN 2219-2840 (online)
doi:10.3748/wjg.v18.i24.3145 2012 Baishideng. All rights reserved.
BRIEF ARTICLE
Gastric mucosal damage in water immersion stress:
Mechanism and prevention with GHRP-6
Shu Guo, Qian Gao, Qing Jiao, Wei Hao, Xue Gao, Ji-Min Cao
Shu Guo, Qian Gao, Wei Hao, Xue Gao, Ji-Min Cao, De- dothelin-1 and thromboxane B2 and gastric heat shock
partment of Physiology and Pathophysiology, Institute of Ba- protein 70 were also assayed. GHRP-6 was injected
sic Medical Sciences, Chinese Academy of Medical Sciences, [intraperitoneal (IP) or intracerebroventricular (ICV)]
School of Basic Medicine, Peking Union Medical College, Bei- 2 h before the onset of stress to observe its potential
jing 100005, China
prevention of the mucosal lesion.
Qing Jiao, Department of Radiology, Taishan Medical College,
Taian 271016, Shandong Province, China
Author contributions: Guo S, Gao X and Cao JM designed the RESULTS: WRS for 6 h induced serious gastric muco-
2
research and wrote the manuscript; Guo S performed most of the sal lesion [lesion area, WRS 81.8 6.4 mm vs normal
2
experiments; Jiao Q performed the heart rate variability analysis; control 0.0 0.0 mm , P < 0.01], decreased the heart
Gao Q, Gao X and Hao W performed part of the animal study. rate, and increased the heart rate variability and gastric
Supported by National Natural Science Foundation of China, acid secretion, suggesting an increase in vagal nerve-
No. 81071072, No. 31171088 (to Cao JM) and No. 81000060 (to carrying stimuli. The mucosal injury was inversely cor-
Gao X) related with water temperature (lesion area, WRS at
Correspondence to: Ji-Min Cao, Professor, Department of 2 2
35 56.4 5.2 mm vs WRS at 23 81.8 6.4 mm ,
Physiology and Pathophysiology, Institute of Basic Medical Sci-
ences, Chinese Academy of Medical Sciences, School of Basic P < 0.01) and was consciousness-dependent. The in-
Medicine, Peking Union Medical College, 5 Dong Dan San jury could not be prevented by eye occlusion, but could
Tiao, Beijing 100005, China. caojimin@126.com be prevented by avoiding contact of the rat body with
Telephone: +86-10-65296959 Fax: +86-10-65296959 the water by dressing it in an impermeable plastic suit.
Received: December 21, 2011 Revised: March 31, 2012 When water was replaced by vegetable oil or liquid
Accepted: April 22, 2012 paraffin, there were gastric lesions in the same grade
Published online: June 28, 2012 of water immersion. When rat were placed in a cage
surrounded by sand, there were no gastric lesions. All
these data point to a remarkable importance of cutenu-
ous information transmitted to the high neural center
Abstract that by vagal nerves reaching the gastric mucosa. FS
AIM: To investigate the mechanism of gastric mucosal alone also induced serious gastric injury, but SR could
demage induced by water immersion restraint stress not induce gastric injury. Bilateral vagotomy or atropine
(WRS) and its prevention by growth hormone releasing prevented the WRS-induced mucosal lesion, indicating
peptide-6 (GHRP-6). that increased outflow from the vagal center is a deci-
sive factor in WRS-induced gastric injury. The mucosal
METHODS: Male Wistar rats were subjected to conscious lesions were prevented by prior injection of GHRP-6 via
or unconscious (anesthetized) WRS, simple restraint (SR), IP did, but not via ICV, suggesting that the protection is
free swimming (FS), non-water fluid immersion, immer- peripheral, although a sudden injection is not equivalent
sion without water contact, or rats were placed in a cage to a physiological release and uptake, which eventually
surrounded by sand. To explore the sensitivity structures may affect the vagal center.
that influence the stress reaction besides skin stimuli, a
group the rats had their eyes occluded. Cervical bilateral CONCLUSION: From the central nervous system, vagal
trunk vagotomy or atropine injection was performed in nerves carry the cutaneous stimuli brought about by the
some rats to assess the parasympathetic role in muco- immersion restraint, an experimental model for inducing
sal damage. Gastric mucosal lesions, acid output and acute gastric erosions. GHRP-6 prevents the occurrence
heart rate variability were measured. Plasma renin, en- of these lesions.
WJG|www.wjgnet.com 3145 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
2012 Baishideng. All rights reserved. species, the function of GHS on alternative physiological
systems has not been clearly elucidated. Studies over the
Key words: Growth substances; Gastric ulcer; Stress; Be- past two decades have demonstrated that GHS exerts its
havior and emotions; Autonomic nerve; Heart rate vari- physiological or pharmacological actions via GH-inde-
ability pendent pathways, except for its GH-dependent action[9].
In the cardiovascular system, GHRP and ghrelin exert
Peer reviewers: Stphane Supiot, MD, PhD, Department of
Radiation Oncology, Centre Ren Gauducheau, St-Herblain, protective effects, especially on myocardial infarction[10]
44800 Nantes, France; Jose Liberato Ferreira Caboclo, Professor, and heart failure[8,11,12]. Ghrelin and GHSR are expressed
Department of Surgery, FAMERP, Av Bady Bassit, 15025-900 in the rat and human stomach and may have significant
Rio de Janeiro, Brazil; Jackie Wood, PhD, Department of Physi- physiological/pharmacological effects on gastric func-
ology and Cell Biology, College of Medicine and Public Health, tion and diseases[13,14]. Ghrelin exerts a potent protective
The Ohio State University, 304 Hamilton Hall, 1645 Neil Av- action on the stomach of rats exposed to WRS[15]. How-
enue, Columbus, OH 43210-1218, United States
ever, whether or not GHRP also protects against stress-
Guo S, Gao Q, Jiao Q, Hao W, Gao X, Cao JM. Gastric mucosal induced gastric injury is unknown. GHRP are much
damage in water immersion stress: Mechanism and prevention smaller in molecular weight, effective when administered
with GHRP-6. World J Gastroenterol 2012; 18(24): 3145-3155 orally, more stable and economically cheaper than ghre-
Available from: URL: http://www.wjgnet.com/1007-9327/full/ lin, and with minimal toxicity, they are better prospects
v18/i24/3145.htm DOI: http://dx.doi.org/10.3748/wjg.v18. for developing drugs for gastric protection. The purpose
i24.3145 of the study was to further investigate the mechanism of
gastric stress ulceration using the WRS rat as a model and
observe the potential protective effect of GHRP-6 on
this gastric injury.
INTRODUCTION
Stress is an adaptive physiological response to disruption MATERIALS AND METHODS
of homeostasis. Serious stress can induce organ injury or
Stress procedures and animal grouping
contribute to diseases, such as gastric ulcers, hyperten-
A 78 4-mo old male Wistar rats of 310 10 g, were in-
sion, diabetes, and cancer. The stomach is one of the
volved in the study. Before the experiment, each animal
main targets of stress. Stress-induced gastric ulceration
was housed in a single cage that had wire-net bottoms to
is a typical example of stress-associated organ injuries[1].
avoid coprophagy and had free access to tap water and
Water immersion restraint stress (WRS) mimics the clini- regular chow for at least 7 d. All animals were starved for
cal acute gastric ulcerations caused by trauma, surgery, or 24 h before the onset of stress, but had free access to
sepsis[2] and has been widely accepted for studying stress tap water. Animals were conscious during the stress pro-
ulceration[3]. It is theoretically and clinically significant to cedures except those in the WRS + anesthesia group
demonstrate the mechanism of stress-induced gastric in- (described below), in which rats were anesthetized with
jury and develop respective therapeutic drugs. 50 mg/kg of sodium pentothal intraperitoneal (IP) dur-
Both psychological and physiological responses occur ing the whole 6-h stress procedures. The water tempera-
during stress and these are involved in the pathogenesis ture was set to 23 0.5, except in the WRS group, in
of gastric ulceration. The psychological responses include which three water temperatures were tested (see below).
anxiety, depression, feeling of helplessness, fear, threat The animals were randomly divided into 11 groups
of drowning, etc. The physiological responses include (n = 6 in each group/treatment): (1) WRS: rats were
neurohormonal and immunological activations, including lightly anesthetized by ether inhalation and four limbs
the involvement of corticotropin-releasing factor. These of each rat were restrained on a wooden plate (25 cm
two systems may interact during stressful challenges[4,5], 19 cm), with the upper limbs anchored at a horizontal
known as psychosomatic reactions. Nonetheless, the position and the lower limbs extended downward. After
mechanisms of gastric stress ulceration remain unclear. awakening (usually 10-15 min after ether anesthesia), rats
Developing protective drugs against gastric stress anchored on the wooden plates were immersed vertically
ulceration is an important clinical issue. Based on previ- (head up) in water to the level of xiphoid process in a
ous studies, agonizing the growth hormone secretagog water bath thermostatically controlled at 23 0.5, 19
receptor (GHSR) might be a strategy. Growth hormone 0.5 or 35 0.5, with or without constant pento-
releasing peptides (GHRP) are peptidyl growth hormone thal anesthesia, respectively (each n = 6). Anesthesia was
secretagogs (GHS) and are the synthetic ligands for the achieved with 50 mg/kg of sodium pentothal IP over the
GHSR. The family members of GHRP include GHRP-1, whole 6-h stress procedure; (2) simple restraint (SR): the
GHRP-2, GHRP-6 and hexarelin[6]. GHSR, and its natu- procedure was the same as in the WRS group except that
ral ligand ghrelin, are widespread in many tissues, includ- the water bath was empty; (3) free swimming (FS): rats
ing the gastrointestinal tract[7] and cardiovascular system[8]. were put into water (water depth 7 cm to avoid drown-
Although the GH-releasing actions of both the natural ing) and allowed free movement in the water for 6 h; (4)
and synthetic GHS have been demonstrated in different shallow water touch: rats were put into a water both (water
WJG|www.wjgnet.com 3146 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
depth 1 cm) and kept for free moving in the water for 6 h; Surface electrocardiograms recording and heart rate
(5) WRS + eye occlusion: animals were eye-occluded variability analysis
with adhesive plasters and then underwent the WRS pro- Surface electrocardiograms (ECG) were recorded with a
cedures, in an attempt to determine whether vision plays computer assisted BL-420S system (Chengdu Technol-
a role in the development of stress ulcers; (6) immersion ogy and Market Co. Ltd., Chengdu, China) with a sample
without water contact (NWCI): water immersion with the rate of 1000 HZ. To avoid the influence of circadian
rat body into a plastic bag to avoid water contact but the variation of gastric susceptibility, we restricted the ECG
rat could see the surrounding water; (7) non-water fluid recording time to 09:00-15:00 for all subjected animals. R
immersion: the procedure was the same as WRS except waves were detected off-line with wavelet transform algo-
that water was replaced by salad oil or liquid paraffin (each rithm and then by manual artifact removal. Linear param-
n = 6), in an attempt to elucidate if skin sensation can eters of heart rate variability (HRV), including mean R-R
differentiate different liquids and induce different gastric intervals, standard deviation of the normal-to-normal
responses; (8) burial in sand: the restrained rat was R-R intervals (SDNN) and root mean square of succes-
placed in a box, the space between the box wall and the sive difference (RMSSD) of R-R intervals, and non-linear
rat body was filled with fine sand, the level of filling sand parameter (Poincar plot) were analyzed as we previously
was also to the xiphoid process. To avoid compression of described[17].
the body, pieces of spongeous material were introduced
into the sand; (9) WRS + vagotomy and WRS + atropine: Vagotomy
rats underwent bilateral vagal nerve trunk cutting and Under light ether inhalation anesthesia, bilateral cervi-
then underwent WRS. Additional 6 WRS rats (without cal vagal nerve trunks were exposed and cut off. After
vagotomy) received atropine (1 mg/kg) IP injection 10 closure of the incision, rats were allowed 3 h to recover
min before the onset of WRS; (10) WRS + GHRP-6: the from the surgery and anesthesia before the WRS proce-
rat received GHRP-6 (100 g/kg) (ProSpec-Tany, Israel) dure.
IP or intracerebroventricular (ICV) injection 2 h before
the WRS procedure. For IP injection, GHRP-6 was dis- Measurement of gastric acid secretion
solved in saline, with a total volume of 0.25 mL per in- To avoid interrupting the development and observation
jection; for ICV injection, GHRP was diluted in artificial of gastric erosion, an additional 24 rats were used to mea-
cerebrospinal fluid, the volume and dosage of GHRP sure gastric acid secretion during the stress. These rats
per injection were 5 L and 20 g/kg; and (11) normal were randomly assigned to four groups: WRS, WRS +
control: rats were not submitted to any stress procedure. GHRP-6, RS and Normal + GHRP-6 groups, respectively
(each n = 6). Gastric acid outputs were measured accord-
Animals without GHRP-6 IP injection received same
ing to the reported protocols[18,19] with minor modifica-
volume (0.25 mL) of saline injection (placebo).
tions. After a 24-h fast, animals were anesthetized by light
The animal use protocol was approved by the Life
ether inhalation. For each animal, a transverse incision
Ethics Committee of Peking Union Medical College and
was made in the abdomen. Both cardia and pylorus were
was conducted in compliance with the United States Na-
intubated via incisions with open polyethylene cannulae
tional Institutes of Health Guidelines for the Care and and then ligated. The incisions were closed with thread
Use of Laboratory Animals (NIH Publication 85-23). adhesive to avoid water invasion, and ether was discon-
tinued. To remove any solid contents, the stomach was
Evaluation of gastric mucosal lesion gently rinsed with 2 mL of saline at 37 three times
After the stress procedures, animals were released from before the drainage of the gastric juice. Two milliliters
the plate and were decapitated under pentobarbital an- of saline warmed to 37 were then injected into the
esthesia. The stomachs were then harvested and opened stomach, left for 30 min and then aspirated and replaced
along the lesser curvature. The severity of mucosal le- by a fresh saline solution. The process was repeated twice
sions was grossly inspected and digitally photographed. to obtain acid secretion before stress and once every 30
Gastric tissues were then fixed in 10% formalin, dehy- min after the beginning of stress, for 3 h. The aspirated
drated and imbedded in paraffin wax. Paraffin sections of fluids were titrated to pH 7.0 with 0.01 mol/L (normality)
5 m were cut and stained with hematoxylin and eosin. NaOH using a pH meter, and acid output was calculated
Histological changes were checked under a microscope. as Eq/30 min.
The length and width of each lesion, including epithe-
lial cell damage, glandular disruption, vasocongestion, Intracerebroventricular cannulation
hemorrhage and deep necrosis, were measured by stere- At least one week before the ICV injection, a brain can-
oscopy and the total area of the lesions in one stomach nula made of polyethylene tubing (PE-10; Clay Adams,
was assessed by planimetry[16]. The measurement of ulcer Parsippany, NJ) was inserted into the left lateral cerebral
index was determined by protocol-blinded researcher. ventricle (A-P, 1.5 mm caudal to the bregma; L, 2.0 mm
The number of animals showing these histopathological lateral to the midline; V, 3.0 mm below the skull surface)
lesions in each group was compared with that of other under pentobarbital anesthesia (35 mg/kg, IP), as re-
groups. cently reported[20]. The cannula implanted into the brain
WJG|www.wjgnet.com 3147 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
was securely fixed by dental cement and synthetic resin. Table 1 The lesion areas of gastric mucosa in different groups
When injections were given to the rats, a microsyringe
for injection was directly connected to the cannula. ICV Group Lesion area (mm )
2
injections were performed only in conscious rats. WRS (23 ) 81.8 6.4b
WRS (19 ) 97.5 8.7b
Measurement of plasma renin activity, endothelin-1 and WRS (35 ) 56.4 5.2d
WRS + GHRP-6 12.0 2.8d
thromboxane B2 SR 0.0 0.0d
Blood was sampled from the ventroartery and prepared FS (23 ) 99.5 6.9b
for the measurements of stress-related vasoconstricti Shallow water touch 0.0 0.0d
ve factors. Kits for assaying the factors were purchased WRS + eye occlusion 91.2 8.4b
R + NWCI 0.0 0.0b
from the Peoples Liberation Army General Hospital, R + SO immersion 80.6 6.9b
Beijing, China. Plasma renin activity (PRA) was indicated R + LP immersion 82.3 7.1b
by the production of angiotensin I (Ang I) in a reaction R + sand immersion 0.0 0.0d
system including rat plasma (containing renin and an- WRS + anesthesia 0.0 0.0d
WRS + vagotomy 0.0 0.0d
giotensinogen), rabbit anti-human Ang I antiserum, Ang WRS + atropine 0.0 0.0d
I standards, and 125I-Ang I. Ang I was measured by the Normal control 0.0 0.0
respective radioimmunoassay (RIA) kit. The direct reac-
tion between sample plasma and Ang I antiserum served b
P < 0.01 vs simple restraint (SR) or normal control; dP < 0.01 vs water im-
as a control. The radiation intensity (counts/min) in each mersion restraint stress (WRS) group. FS: Free swimming; NWCI: Non-
water contact immersion; SO: Salad oil; LP: Liquid paraffin; R: Restraint.
tube was converted to nanograms per milliliter (ng/mL),
with reference to the Ang I standard curve. PRA was cal-
culated by the equation: PRA (ng/mL per hour) = (Ang I ogy, Inc., dilution 1:500) were added onto the membrane
concentration in test tube-Ang I concentration in control to react overnight at 4 and then incubated with rabbit
tube)/incubation time (h). All assays were performed in anti-goat horseradish peroxidase-conjugated secondary
duplicate. antibody (Santa Cruz, Inc., dilution 1:2500) for 1 h. The
Plasma endothelin-1 (ET-1) was measured with a RIA immunoreactive bands were visualized using Western
kit according to the manufacturers protocols. The prima- blotting luminal reagents and were scanned with Image
ry antibodies were rabbit anti-human ET-1 which showed Analysis software (Alpha Innotech, United States).
interactions with rat ET-1. We also used standards of
these hormones and blank controls to guarantee the qual- Statistical analysis
ity of the measurement. The measuring sensitivities were Data are presented as mean SD. Students t-test was
< 5 pg/mL for ET-1. The intra- and interassay variabili- used for two group comparison and analysis of variance
ties were < 10% and < 15% for ET-1. followed by Newman-Keuls multiple comparisons were
Plasma thromboxane B2 (TXB2) was measured with used in case for multiple comparisons. Differences with P
an RIA kit (Peoples Liberation Army General Hospi- value < 0.05 were considered significant.
tal, Beijing), according to the manufacturers protocols.
Thromboxane A2 (TXA2) is unstable (half-life 30 min)
and is rapidly metabolized to the relatively stable TXB2;
RESULTS
therefore, we used TXB2 as an indicator of TXA2 level. The water immersion restraint stress-induced gastric
One milliliter of blood was drawn from the abdominal mucosal lesion is skin-sensing dependent but is vision
aorta into a test tube containing 0.06 mL of indometh- or restraint independent
acin-EDTA solution and then mixed. The blood was Visual inspection showed that WRS for 6 h (water tem-
centrifuged at 3500 r/min for 15 min and the plasma was perature 23) induced serious gastric bleeding erosions,
separated and stored at -20. At the beginning of the as indicated by the mucosal hemorrhage and mucosal
measurement, the plasma was defrosted and centrifuged erosive lesion (Figure 1) and the calculated area of the
again at 3500 r/min for 10 min. The supernatant was lesions (Table 1). The hemorrhage was observed mainly
used to measure the TXA2 level using the RIA kit. in the gastric body and antrum, but not in the fundus
and duodenum (Figure 1). Under the microscope, the
Western blotting mucosa in the WRS rat was disrupted and covered with
The gastric mucosal tissues were harvested immediately coagulated blood and inflammatory cell infiltration (Fig-
after decapitation, and 100 mg of mucosal tissues for ure 1). Rats with SR did not show gastric mucosal lesions
each animal were used for the following procedures. Total (Figure 1, Table 1). Compared with the serious gastric
protein extracts were prepared by homogenizing mucosal mucosal damage in all the WRS rats (Figures 1 and 2), eye
tissues in lysis buffer. Protein (80 g per sample) electro- occlusion of WRS rats did not provide any protection
phoresis were subjected to sodium dodecylsulfate-poly- from the mucosal lesions (Figure 2, Table 1), suggesting
acrylamide gel and then transferred onto a nitrocellulose that vision does not play an important role in the patho-
membrane. Primary antibodies [goat anti-rat heat shock genesis of gastric damage. Rats with NWCI showed an
proteins 70 (HSP70), polyclonal] (Santa Cruz Biotechnol- intact mucosa (Figure 2, Table 1), again supporting that
WJG|www.wjgnet.com 3148 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
WRS
WRS + GHRP-6
Antrum
SR
Gastric body
Duodenum
Fundus
WRS WRS + GHRP-6 SR
Figure 1 Gross anatomy of rat gastric mucosa in different groups. Left three columns: The gross inspections of the gastric mucosa in water immersion restraint
stress (WRS), WRS + growth hormone releasing peptide-6 (GHRP-6) and simple restraint (SR) groups, respectively. Note that there were serious mucosal hemor-
rhages (black color) in the WRS group, while the hemorrhage was minimal in the WRS + GHRP-6 group. No mucosal hemorrhage was observed in the SR group; the
forth column: Hematoxylin-eosin staining of the mucosa, mucosal structure disruption and hemorrhage (brown color) were observed in the WRS group, but not in the
WRS + GHRP-6 and SR groups.
the view that vision is not important in inducing gastric In an attempt to determine if different liquids would lead
mucosal lesion. FS for 6 h also induced serious muco- to different response patterns in the gastric mucosa, we
sal bleeding erosions (Figure 2, Table 1), indicating that observed the effects of immersion with two other liquids
water immersion without restraint is also sufficient for (salad oil and liquid paraffin, which are not obviously
inducing gastric mucosal lesions. skin-hazardous) on gastric mucosa. Immersion to the
We also observed the influence of water temperature level of xiphoid process with either of the two liquids
on WRS-induced gastric mucosal lesions. WRS with cool induced similar gastric mucosal lesion (Figure 2, Table 1)
water (23) (Figure 1) or cold water (19) (Figure 2) as WRS did (Figure 2). Burying the body into sand (with
both induced serious mucosal lesions, but the extent of the head exposed) did not induce mucosal lesions (Figure
the lesions was smaller when warm water (35) was 2, Table 1). These results suggest that it is the liquid, but
used (Figure 2, Table 1). not the chemical nature of the liquid, that determines
whether the mucosal lesions would occur, and burying
The liquid immersion-induced gastric mucosal lesion the body in solid materials does not induce gastric muco-
depends on the deepening of immersion but not sal lesions.
depends on the nature of a liquid
Water immersion (WI) to the level of the xiphoid induced The WRS-induced gastric mucosal lesion depends
serious gastric mucosal lesions (Figure 1), but partial WI on the functional neural integrity and increased vagal
(shallow water tough) did not induce mucosal lesions outflow to the stomach
(Figure 2, Table 1), suggesting that the depth of the im- WRS without anesthesia (i.e., conscious rats) induced
mersion determines the occurrence of mucosal lesions. serious gastric mucosal lesions (Figure 1, Table 1), but
WJG|www.wjgnet.com 3149 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
WRS (23 ) WRS (23 ) + anes. WRS + eye occlusion Free swimming Shallow water touch
R +NWCI R +LP immersion R +SO immersion R +bury in sand WRS (19 )
WRS (19 ) + anes. WRS (35 ) WRS (35 ) + anes. WRS + vagotomy WRS + atropine
WRS + GHRP-6 (ICV)) WRS + GHRP-6 (IP) Normal control
Figure 2 Representative pictures of the gastric mucosa in different groups. WRS: Water immersion restraint stress; R: Restraint; NWCI: Immersion without wa-
ter contact; LP: Liquid paraffin; SO: Salad oil; Anes.: Anesthesia; ICV: Intracerebroventricular injection; IP: Intraperitoneal injection.
170 GHRP-6 + WRS b GHRP-6 + WRS GHRP-6 + WRS
3.8
WRS WRS b WRS b
2.2
RMDDF of R-R interval (ms)
SR b SR a SR
SDNN of R-R interval (ms)
Mean of R-R interval (ms)
b
b 3.4
150 2.0
a
3.0
1.8
130
1.6 2.6
110 1.4 2.2
0 1 2 3 4 5 0 1 2 3 4 5 0 1 2 3 4 5
t /h t /h t /h
Figure 3 Heart rate variability analyses showing the differences in mean R-R intervals, standard deviation of the normal-to-normal R-R intervals and root
mean square of successive difference of R-R intervals in different groups. Note that the mean R-R intervals gradually prolonged along with the progress of wa-
ter immersion restraint stress (WRS), whereas this prolongation was much less in the WRS + growth hormone releasing peptide-6 (GHRP-6) group. The mean R-R
intervals were shortened in the simple restraint (SR) group. The changes in standard deviation of the normal-to-normal (SDNN) and root mean square of successive
difference (RMSSD) was more significant in WRS group than the other two groups. aP < 0.05, bP < 0.01 vs WRS+GHRP-6 group.
WRS with anesthesia (unconscious rats) did not, no mat- tion of atropine also abolished the WRS-induced gastric
ter what a water temperature was used (Figure 2, Table mucosal lesion (Figure 2), further supporting the vagal
1). The HRV analyses (Figures 3 and 4) showed that the hypothesis of this injury.
R-R intervals of the ECG in WRS rats gradually became WRS stimulated gastric acid secretion (Figure 5), also
longer, in other words, the HR gradually decreased; the indicative of increased vagal efferent activity. Simple
SDNN and RMSSD of the R-R intervals increased, sug- restraint did not affect gastric acid output (Figure 5),
gesting an increase of HRV, underlying an increase of the indicating that restraint alone did not stimulate parasym-
vagal outflow. Simple restraint induced a gradual shorting pathetic activity. Bilateral vagotomy totally prevented the
in R-R intervals and decreases in SDNN and RMSSD development of WRS-induced mucosal lesions (Figure
(Figure 3), suggesting an increase in sympathetic outflow 2), also supporting the hypothesis that increased vagal
to the heart. The Poincar plot of R-R intervals (Figure outflow to the stomach plays a leading role in the devel-
4) also supported the above observations. Previous injec- opment of WRS-induced mucosal lesions.
WJG|www.wjgnet.com 3150 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
0h 1st h 2nd h 3rd h 4th h 5th h
A t /ms
100 100 100 100 100 100
WRS 160 160 160 160 160 160
200 200 200 200 200 200
100 160 200 100 160 200 100 160 200 100 160 200 100 160 200 100 160 200
B 100 100 100 100 100 100
WRS +
160 160 160 160 160 160
GHRP-6
200 200 200 200 200 200
100 160 200 100 160 200 100 160 200 100 160 200 100 160 200 100 160 200
C 100 100 100 100 100 100
SR 160 160 160 160 160 160
200 200 200 200 200 200
100 160 200 100 160 200 100 160 200 100 160 200 100 160 200 100 160 200
t /ms
Figure 4 Pointcar plots of the R-R intervals in different groups. A: The plots indicate that heart rate decreased gradually with time, and heart rate variability
(HRV) was increased as shown by the scattered pattern of the plots in the water immersion restraint stress (WRS) group, suggesting vagal overactivity in this group;
B: Changes of the heart rate and HRV in the WRS + growth hormone releasing peptide-6 (GHRP-6) group were much less than the WRS group; C: In the simple re-
straint (SR) group, the heart rate increased and the HRV was decreased as shown by the condensed geometry of the plots, suggesting increased sympathetic activity
in this group.
WRS SR SR WRS WRS + GHRP-6
WRS + GHRP-6 Normal + GHRP-6
140 HSP70
Gastric acid output (mEq/30 min)
120
100 b b
b b
b b-actin
80
a
60 Figure 6 Western blotting showing gastric mucosal protein levels of heat
shock proteins 70 in different groups. Note that there was substantial expres-
40 sion in the water immersion restraint stress (WRS) and simple restraint (SR)
groups, whereas the expression was minimal in the WRS + growth hormone
20 releasing peptide-6 (GHRP-6) group. HSP70: Heat shock proteins 70.
0 30 60 90 120 150 180
t /min
group; lesion area was zero in the SR group. GHRP-6 did
Figure 5 Gastric acid output in different groups. Note that water immersion not have a protective effect on the mucosa of WRS rats
restraint stress (WRS) induced significant increase in gastric acid output and
if administrated centrally via ICV (Figure 2), suggesting
growth hormone releasing peptide-6 (GHRP-6) (intraperitoneal) significantly
suppressed this increase. Simple restraint (SR) and GHRP-6 alone did not that the protective effect of GHRP-6 is mainly periph-
change the gastric acid output. aP < 0.05, bP < 0.01 vs WRS group. eral.
GHRP-6 alleviated the changes of HRV parameters
induced by WRS (Figures 3 and 4), and decreased the gas
GHRP-6 prevents WRS-induced gastric mucosal lesion tric acid output during WRS (Figure 5), suggesting that
mainly by suppressing the vagal effect on the stomach GHRP-6 protects the mucosa, at least in part, by suppres
GHRP-6 pre-injection via IP 2 h before the start of WRS sing the vagal efferent effect on the stomach.
dramatically prevented the WRS-induced mucosal bleed- GHRP-6 could alleviate the intensity of gastric stress
ing erosion; only very slight or no hemorrhaging was ob- response, which is reflected by the level of expression of
served in the WRS + GHRP-6 group (Figure 1). The HE HSP70 in the mucosa. Western blotting results showed
stains of the gastric tissues (Figure 1) also confirmed that that both the WRS and SR induced a high expression of
the mucosal injury/hemorrhage was minimal or not ob- HSP70 in the gastric mucosal tissues (Figure 6), indicat-
served in WRS rats pretreated with GHRP-6. Planimetry ing a nonspecific response of HSP70 expression to stress.
analyses (Table 1) showed that the lesion area was large in GHRP-6 pretreatment significantly decreased the protein
the WRS group; but was minimal in the WRS + GHRP-6 level of HSP70 in the WRS rats (Figure 6), suggesting a
WJG|www.wjgnet.com 3151 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
Table 2 The effect of growth hormone releasing peptide-6 this point, we examined gastric mucosal responses to im-
on the plasma levels of stress-related factors in rats mersion in different liquids or solid materials. Immersion
in either salad oil or liquid paraffin induced serious muco-
ET-1 Renin activity TXB2 sal hemorrhage similarly to WI, indicating that liquid im-
(pg/mL) (pg/mL) (ng/mL)
mersion-induced gastric mucosal injury does not depend
WRS 152.23 10.70d 1.71 0.59d 311.31 50.54d
on the chemical nature of a liquid, but depends on liquid
WRS + GHRP-6 115.11 4.08b 0.65 0.29a 125.84 8.36b
SR 97.11 4.71 0.11 0.03 69.93 22.13
itself. Burial in sand did not induce gastric lesions, even
when combined with restraint, suggesting that skin sen-
a
P < 0.05, bP < 0.01 vs WRS group; dP < 0.01 vs SR group. WRS: Water im- sors can differentiate whether a material is fluid or dry
mersion restraint stress; SR: Simple restraint; GHRP-6: Growth hormone matter, and immersion in a liquid or burial in dry ma-
releasing peptide-6; ET-1: Endothelin-1; TXB2: Thromboxane B2. terial would lead to different gastric mucosal responses.
Another possibility is that liquid immersion leads to lower
decrease in the stress intensity. body temperature compared with surrounding the body
WRS significantly increased the plasma levels of ET-1, with solid materials.
renin activity and TXB2 compared with that of the SR The present data also indicated that the functional
group, while GHRP-6 pretreatment significantly attenu- integrity of neural regulation is essential for the induction
ated the increases in these vasoconstrictive hormones (Ta of gastric mucosal injury by WRS. In conscious animals,
ble 2). WRS induced injury that was inversely related to water
temperature. However, in unconscious rats exposed to
even the most severe condition (19), no ulceration oc-
DISCUSSION curred, which agreed with the result of Murison et al[21].
The mechanism of WRS-induced gastric mucosal le- Pentobarbital does not block vagal output to the stom-
sion is complicated and not yet fully understood. The ach[22], but even enhances vagal output[21] ; therefore, the
pathogenesis of the injury may be recognized at different lack of gastric erosion by WRS in unconscious rats may
levels, for example, at psychological, physiological, psy- be caused by certain selective interruptions of CNS-sto
chosomatic[21], integrative, organic, cellular and molecular mach communications by the anesthesia, potentially in-
levels. This study focuses on the psychosomatic mecha- cluding sensation of body temperature and mobilization
nism of WRS-induced gastric mucosal lesions in vivo. of vasoconstrictive hormones, such as renin-angiotensin
We first differentiated the relative importance of the system[23], ET-1[24] and TXB2[25]. These vasoconstrictive
pathways by which the stress stimulus signals were sens factors may reduce gastric blood flow and lead to chang-
ed and transferred to the central nervous system (CNS). es in the ratio of gastric blood flow/acid output, which
When a conscious rat was immersed in water, it saw (intact favors the formation of gastric ulcers[26].
vision) that its body was almost drowning, which may Gastric acid secretion is controlled by sympathetic and
have induced fear. At the same time, the rats skin also parasympathetic nerves, and by certain hormones, such
sensed liquid immersion and generated a physiological re- as gastrin. Generally, sympathetic activity inhibits, and
sponse and subsequent psychological stress response. By parasympathetic activity stimulates, gastric acid secretion.
eye occlusion or NWCI manipulations, we determined Occasionally, sympathetic stimulation may also increase
that vision alone is not sufficient to induce gastric muco- gastric acid secretion, because adrenalin releases gastrin;
sal lesion, while WI alone is sufficient for the induction and vagal nerves may exert some sympathetic-like effect
of the lesion, because free swimming rats showed serious as they have adrenergic fibers. Our results indicate that
mucosal injury. These results also showed that immer- increased vagal efferent activity is the leading cause of
sion depth significantly affects the severity of mucosal WRS-induced gastric mucosal injury, because HRV analy-
lesions, as partial immersion in shallow water could not ses showed heart rate slowing and increasing of some
induce mucosal lesions. These results indicate that skin HRV parameters, and furthermore, bilateral vagotomy
sensation is the leading input pathway for WRS-induced or atropine totally prevented the injury induced by WRS.
gastric bleeding erosion. The cutaneous stimuli may reach This result is consistent with our previous study[17]. Our
the integrative structures of the upper central nervous HRV analyses also showed that restraint alone induced
system and, by the vagal pathway, produce gastric mucosa moderate sympathetic hyperactivity, while sympathetic
lesions. Rat is an animal of nocturnal habit; therefore hyperactivity in the stomach prevents WRS-induced gas-
vision is not a fundamental sense for its defense. In all tric injury formation mainly via the inhibition of gastric
environments, rat performs a cognitive map to run away acid secretion, as observed in stroke prone spontaneously
from an eventual predator. In an unstable environment, hypertensive rats[27].
such as fluid, they may aware of the difficulty of running Heart rate slowing is a universal response in all air-
away. breathing vertebrates when immersed in water (drown-
Skin receptors can sense temperature, touch and nox- ing or diving), this is called diving bradycardia[28]. Diving
ious stimulation. Whether or not skin sensors can also bradycardia is triggered by apnea and accentuated by im-
distinguish different liquids is unknown. To determine mersion of the face or whole body in cold water[28]. The
WJG|www.wjgnet.com 3152 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
diving response is mainly characterized by bradycardia, vagal complex); the other possibility is that GHRP-6 may
decreased cardiac output, peripheral vasoconstriction and also affect the vagal afferent nerves, which in turn affects
increased arterial blood pressure[29,30]. The physiological the neuronal reflex.
significance of this response is to conserve oxygen, a The protection of GHRP-6 on WRS-induced gas-
mechanism of defense against hypoxic damage[28,31]. Our tric injury could also be reflected by the level of expres-
previous[17] and present observations in the rat model in- sion of HSP70 in the gastric mucosal tissue. HSP are
dicate that bradycardia appears even when the immersion crucial for cell survival during and after various cellular
is partial and the face is not immersed (for example, im- stresses. WRS rapidly induces HSP70 expression and ac-
mersed to the xiphoid process in the present study), sug- cumulation; the HSP70 level is inversely correlated with
gesting that heart rate slowing during water immersion the severity of mucosal lesions[41]. GHRP-6 significantly
does not necessarily depend on face immersion. This decreased the HSP70 protein level in the gastric mucosa
reaction pattern may be formed in development, and is of WRS rats compared with WRS alone, indicating that
a heritable trait[32]. However, when humans are diving or the stress intensity is low in the GHRP-6 treated animals.
swimming for longer times (for example, 8-h swimming), This result also suggests that GHRP-6 can exert a cell
they usually do not develop gastric mucosal injury, while protective effect.
rats do. One potential mechanism for these differential Interestingly, we found that gastric mucosal injury never
gastric responses may be the psychological component: occurred in the gastric fundus, while ghrelin is secreted
a man who is diving or swimming knows that he is just predominantly by enteroendocrine cells in the gastric
at work or recreation and will not drown; therefore, he fundus, although ghrelin gene transcripts and ghrelin-
has no severe psychological reactions. By contrast, a rat producing cells are found throughout the gastrointestinal
would not think so, it would feel it was about to drown tract[13]. Whether the ghrelin-secreting fundus is ulcer-
and die, and therefore severe psychological responses resistant or only the acid-secreting areas (gastric body and
would be triggered, which may partially contribute to gas- antrum) are vulnerable to stress, deserves further investi-
tric injury. gation. It is possible that locally released ghrelin may have
Ghrelin, a peptide hormone originally isolated main a protective action on the fundic gastric mucosa.
ly from the stomach, is the endogenous ligand for the In conclusion, this study demonstrates that vision-trig
GHSR. In the gastrointestinal tract, ghrelin regulates gered psychosomatic responses do not play an important
the motility of the stomach and gut[33], gastric acid se- role in WRS-induced gastric mucosal lesions; however,
cretion[34] and gastric mucosal defense[35,36]. Intravenous skin sensation-induced increase of vagal outflow and
administration of rat ghrelin dose-dependently increases subsequent increase of gastric acid secretion do play a
both gastric acid secretion and gastric motility, actions leading role. Skin receptors cannot differentiate different
that are blocked by pretreatment with either atropine liquids, and immersion with different liquids induced the
or bilateral cervical vagotomy, but not by the histamine same gastric injury as WI does. GHRP-6 protects against
H2-receptor antagonist famotidine, suggesting ghrelin WRS-induced gastric lesions mainly by suppressing the
might have a physiological role in the vagal control of vagal effect on gastric mucosa, and this protection is
gastric function in rats[37]. Another study indicated that likely peripheral. The protective effect of GHRP-6 on
ghrelin inhibits gastric acid secretion[38]. This controversy gastric stress ulceration suggests a clinical application in
deserves further investigation. GHRP, the mimetic of treating stress-related gastric injury.
ghrelin, has been shown to have gastric motor effects[39].
However, the effect of GHRP on gastric acid secretion is COMMENTS
COMMENTS
unknown. We show here that WRS significantly increased
the gastric acid output, but restraint did not; GHRP-6 Background
Gastric ulcers are among the most frequently occurring stomach diseases
significantly suppressed WRS-stimulated gastric acid se across the world and stress is an important inducer of this disease. Therefore,
cretion, although GHRP-6 did not significantly affect the an understanding of the key mechanism of gastric stress ulceration and the de-
basal gastric acid output in normal rats. These results, velopment of preventive/therapeutic drugs are important in treating this disease.
combined with the HRV data, suggest that the protec- Research frontiers
tive effect of GHRP-6 on WRS-induced gastric mucosal How stress induces gastric ulcers is an old question that needs a new answer.
injury is affected, at least in part, by suppressing vagal ef- Most previous studies only looked at restricted areas, especially at the physi-
ological and molecular levels. Exploring the key mechanism and developing
ferent effect on the stomach, including gastric acid secre- therapeutic drugs for gastric stress ulcer are urgently required.
tion, as gastric acid play an important role in the develop-
Innovations and breakthroughs
ment of WRS-induced gastric ulcers[40]. Our results also In contrast to other mechanistic studies on gastric stress ulceration, this in-
indicate that the protective effect of GHRP-6 is likely vestigation focuses on the psychosomatic mechanisms of water immersion
peripheral, potentially by affecting the function of vagal and restraint stress (WRS)-induced gastric bleeding erosions, and found that
efferent terminals and/or cell protection. However, we increased outflow from the vagal center is the leading cause of WRS-induced
gastric injury. Skin sensation, but not vision, triggers the stress reaction via va-
cannot exclude the possibility that GHRP-6 might also
go-vagal reflex. The study also found that growth hormone releasing peptide-6
affect the vago-vagal or vago-sympathetic reflexes. One (GHRP-6), a synthetic agonist for growth hormone secretagogues receptor,
possibility is that GHRP-6 injected via ICV may not ef- prevents the occurrence of gastric mucosal lesions, mainly by suppressing the
fectively reach its target CNS site (for example, the dorsal vagal effect on the stomach.
WJG|www.wjgnet.com 3153 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
Applications 16 Konturek PC, Brzozowski T, Burnat G, Szlachcic A, Koziel
The study demonstrates the key signaling pathway by which water immersion J, Kwiecien S, Konturek SJ, Harsch IA. Gastric ulcer heal-
induces gastric mucosal damage in the rat, and provides the first evidence that ing and stress-lesion preventive properties of pioglitazone
GHRP-6 can prevent this damage. The study suggests a clinical application of are attenuated in diabetic rats. J Physiol Pharmacol 2010; 61:
GHRP in treating gastric stress ulceration. 429-436
Peer review 17 Xie YF, Jiao Q, Guo S, Wang FZ, Cao JM, Zhang ZG. Role
Discovering the mechanism of gastric stress ulceration is a prerequisite for the of parasympathetic overactivity in water immersion stress-
prevention and treatment of this disease. This study shows that skin sensation induced gastric mucosal lesion in rat. J Appl Physiol 2005; 99:
and the subsequent vago-vagal reflex play a key role in the development of 2416-2422
water immersion-induced gastric mucosal damage in the rat. GHRP-6 prevents 18 Said SA, El-Mowafy AM. Role of endogenous endothelin-1
this damage, probably by suppressing the vagal effect on the stomach. The in stress-induced gastric mucosal damage and acid secretion
study is innovative and with potential therapeutic interest. in rats. Regul Pept 1998; 73: 43-50
19 Kitagawa H, Fujiwara M, Osumi Y. Effects of water-immer-
sion stress on gastric secretion and mucosal blood flow in
REFERENCES rats. Gastroenterology 1979; 77: 298-302
20 Tanida M, Shen J, Kubomura D, Nagai K. Effects of anserine
1 Brodie DA, Hooke KF. The effect of vasoactive agents on on the renal sympathetic nerve activity and blood pressure
stress-induced gastric hemorrhage in the rat. Digestion 1971; in urethane-anesthetized rats. Physiol Res 2010; 59: 177-185
4: 193-204 21 Murison R, Overmier JB. Some psychosomatic causal fac-
2 Ernst H, Konturek PC, Brzozowski T, Lochs H, Hahn EG, tors of restraint-in-water stress ulcers. Physiol Behav 1993; 53:
Konturek SJ. Adaptation of gastric mucosa to stress. Effect 577-581
of ranitidine. J Physiol Pharmacol 1998; 49: 405-419 22 Lin WC, Yano S, Watanabe K. Stimulation of gastric acid
3 Uramoto H, Ohno T, Ishihara T. Gastric mucosal protection secretion by microinjection of pentobarbital into the ventro-
induced by restraint and water-immersion stress in rats. Jpn medial hypothalamus. Res Commun Chem Pathol Pharmacol
J Pharmacol 1990; 54: 287-298 1988; 60: 269-272
4 Robles TF, Carroll JE. Restorative biological processes and 23 Ender F, Labancz T, Rosivall L. Protective effects of the inhi-
health. Soc Personal Psychol Compass 2011; 5: 518-537 bition of the renin-angiotensin system against gastric muco-
5 Lin HP, Lin HY, Lin WL, Huang AC. Effects of stress, de- sal lesions induced by cold-restraint in the rat. Acta Physiol
pression, and their interaction on heart rate, skin conduc- Hung 1993; 81: 13-18
tance, finger temperature, and respiratory rate: sympathetic- 24 Duan YM, Li ZS, Zhan XB, Xu GM, Tu ZX, Gong YF. Chang-
parasympathetic hypothesis of stress and depression. J Clin es in endothelin-1 gene expression in the gastric mucosa of
Psychol 2011; 67: 1080-1091 rats under cold-restraint-stress. Chin J Dig Dis 2004; 5: 28-34
6 Xu XB, Cao JM, Pang JJ, Xu RK, Ni C, Zhu WL, Asotra K, 25 Kitagawa H, Kurahashi K, Fujiwara M. Gastric mucosal ero-
Chen MC, Chen C. The positive inotropic and calcium- sion due to a mucosal ischemia produced by thromboxane
mobilizing effects of growth hormone-releasing peptides on A2-like substance in rats under water-immersion stress. J
rat heart. Endocrinology 2003; 144: 5050-5057 Pharmacol Exp Ther 1986; 237: 300-304
7 Nikolopoulos D, Theocharis S, Kouraklis G. Ghrelins role 26 Arai I, Muramatsu M, Aihara H. Body temperature depen-
on gastrointestinal tract cancer. Surg Oncol 2010; 19: e2-e10 dency of gastric regional blood flow, acid secretion and
8 Cao JM, Ong H, Chen C. Effects of ghrelin and synthetic ulcer formation in restraint and water-immersion stressed
GH secretagogues on the cardiovascular system. Trends En- rats. Jpn J Pharmacol 1986; 40: 501-504
docrinol Metab 2006; 17: 13-18 27 Shichijo K, Ito M, Taniyama K, Sekine I. The role of sym-
9 Broglio F, Arvat E, Gottero C, Benso A, Prodam F, Deste- pathetic neurons for low susceptibility to stress in gastric
fanis S, Aimaretti G, Papotti M, Muccioli G, Deghenghi R, lesions. Life Sci 1993; 53: 261-267
Ghigo E. Natural and synthetic growth hormone secreta- 28 Alboni P, Alboni M, Gianfranchi L. Diving bradycardia: a
gogues: do they have therapeutic potential? Treat Endocrinol mechanism of defence against hypoxic damage. J Cardiovasc
2003; 2: 153-163 Med (Hagerstown) 2011; 12: 422-427
10 Rossoni G, De Gennaro Colonna V, Bernareggi M, Polvani 29 Ferretti G. Extreme human breath-hold diving. Eur J Appl
GL, Mller EE, Berti F. Protectant activity of hexarelin or Physiol 2001; 84: 254-271
growth hormone against postischemic ventricular dysfunc- 30 Gooden BA. Mechanism of the human diving response. In-
tion in hearts from aged rats. J Cardiovasc Pharmacol 1998; 32: tegr Physiol Behav Sci 1994; 29: 6-16
260-265 31 Andersson JP, Linr MH, Fredsted A, Schagatay EK. Car-
11 King MK, Gay DM, Pan LC, McElmurray JH, Hendrick diovascular and respiratory responses to apneas with and
JW, Pirie C, Morrison A, Ding C, Mukherjee R, Spinale FG. without face immersion in exercising humans. J Appl Physiol
Treatment with a growth hormone secretagogue in a model 2004; 96: 1005-1010
of developing heart failure: effects on ventricular and myo- 32 Fahlman A, Bostrom BL, Dillon KH, Jones DR. The genetic
cyte function. Circulation 2001; 103: 308-313 component of the forced diving bradycardia response in
12 Xu XB, Pang JJ, Cao JM, Ni C, Xu RK, Peng XZ, Yu XX, Guo S, mammals. Front Physiol 2011; 2: 63
Chen MC, Chen C. GH-releasing peptides improve cardiac 33 Blbl M, Babygirija R, Zheng J, Ludwig K, Xu H, Lazar J,
dysfunction and cachexia and suppress stress-related hor- Takahashi T. Food intake and interdigestive gastrointestinal
mones and cardiomyocyte apoptosis in rats with heart fail- motility in ghrelin receptor mutant rats. J Gastroenterol 2011;
ure. Am J Physiol Heart Circ Physiol 2005; 289: H1643-H1651 46: 469-478
13 Jeffery P, McDonald V, Tippett E, McGuckin M. Ghrelin in 34 Sakata I, Sakai T. Ghrelin cells in the gastrointestinal tract.
gastrointestinal disease. Mol Cell Endocrinol 2011; 340: 35-43 Int J Pept 2010; 2010: 945056
14 Suzuki H, Matsuzaki J, Hibi T. Ghrelin and oxidative stress 35 Baek YH, Lee KN, Jun DW, Yoon BC, Kim JM, Oh TY, Lee
in gastrointestinal tract. J Clin Biochem Nutr 2011; 48: 122-125 OY. Augmenting Effect of DA-9601 on Ghrelin in an Acute
15 Brzozowski T, Konturek PC, Drozdowicz D, Konturek SJ, Gastric Injury Model. Gut Liver 2011; 5: 52-56
Pawlik M, Sliwowski Z, Pawlik WW, Hahn EG. Role of 36 Adami M, Pozzoli C, Leurs R, Stark H, Coruzzi G. Hista-
central and peripheral ghrelin in the mechanism of gastric mine H(3) receptors are involved in the protective effect of
mucosal defence. Inflammopharmacology 2005; 13: 45-62 ghrelin against HCl-induced gastric damage in rats. Pharma-
WJG|www.wjgnet.com 3154 June 28, 2012|Volume 18|Issue 24|
Guo S et al . GRHP-6 prevents acute gastric ulcer in restrained rats
cology 2010; 86: 259-266 39 Qiu WC, Wang ZG, Wang WG, Yan J, Zheng Q. Gastric mo-
37 Torsello A, Locatelli V, Melis MR, Succu S, Spano MS, De- tor effects of ghrelin and growth hormone releasing peptide
ghenghi R, Mller EE, Argiolas A. Differential orexigenic 6 in diabetic mice with gastroparesis. World J Gastroenterol
effects of hexarelin and its analogs in the rat hypothalamus: 2008; 14: 1419-1424
indication for multiple growth hormone secretagogue re- 40 Li YM, Lu GM, Zou XP, Li ZS, Peng GY, Fang DC. Dynamic
ceptor subtypes. Neuroendocrinology 2000; 72: 327-332 functional and ultrastructural changes of gastric parietal
38 Sibilia V, Muccioli G, Deghenghi R, Pagani F, De Luca V, cells induced by water immersion-restraint stress in rats.
Rapetti D, Locatelli V, Netti C. Evidence for a role of the World J Gastroenterol 2006; 12: 3368-3372
GHS-R1a receptors in ghrelin inhibition of gastric acid se- 41 Rokutan K. Role of heat shock proteins in gastric mucosal
cretion in the rat. J Neuroendocrinol 2006; 18: 122-128 protection. J Gastroenterol Hepatol 2000; 15 Suppl: D12-D19
S- Editor Gou SX L- Editor Stewart GJ E- Editor Xiong L
WJG|www.wjgnet.com 3155 June 28, 2012|Volume 18|Issue 24|
También podría gustarte
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- Online Food Delivery Service Quality: Does Personal Innovativeness Matter?Documento5 páginasOnline Food Delivery Service Quality: Does Personal Innovativeness Matter?Fitria DewinurAún no hay calificaciones
- Klasifikasi NyeriDocumento6 páginasKlasifikasi NyeriFitria DewinurAún no hay calificaciones
- JCO 2008 Atchley 4282 8Documento7 páginasJCO 2008 Atchley 4282 8Fitria DewinurAún no hay calificaciones
- Sindrom Paraneoplastik 2Documento9 páginasSindrom Paraneoplastik 2Fitria DewinurAún no hay calificaciones
- Cancer Epidemiol Biomarkers Prev 2009 Antoniou 601 10Documento11 páginasCancer Epidemiol Biomarkers Prev 2009 Antoniou 601 10Fitria DewinurAún no hay calificaciones
- JCO 2008 Tan 5530 6Documento7 páginasJCO 2008 Tan 5530 6Fitria DewinurAún no hay calificaciones
- Sindrom Paraneoplastik 2Documento9 páginasSindrom Paraneoplastik 2Fitria DewinurAún no hay calificaciones
- Klasifikasi NyeriDocumento6 páginasKlasifikasi NyeriFitria DewinurAún no hay calificaciones
- Brca OutcomeDocumento9 páginasBrca OutcomeFitria DewinurAún no hay calificaciones
- 8005 WomenDocumento6 páginas8005 WomenFitria DewinurAún no hay calificaciones
- 8005 WomenDocumento6 páginas8005 WomenFitria DewinurAún no hay calificaciones
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2102)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Chapter 2Documento69 páginasChapter 2Lizi CasperAún no hay calificaciones
- Nuttall Gear CatalogDocumento275 páginasNuttall Gear Catalogjose huertasAún no hay calificaciones
- Ibragimova Lesson 4Documento3 páginasIbragimova Lesson 4Dilnaz IbragimovaAún no hay calificaciones
- Medical Equipment Quality Assurance For Healthcare FacilitiesDocumento5 páginasMedical Equipment Quality Assurance For Healthcare FacilitiesJorge LopezAún no hay calificaciones
- ADMT Guide: Migrating and Restructuring Active Directory DomainsDocumento263 páginasADMT Guide: Migrating and Restructuring Active Directory DomainshtoomaweAún no hay calificaciones
- Ericsson For Sale From Powerstorm 4SA03071242Documento8 páginasEricsson For Sale From Powerstorm 4SA03071242wd3esaAún no hay calificaciones
- DXFtoGerberConversionGuide Rev2!12!10 13Documento8 páginasDXFtoGerberConversionGuide Rev2!12!10 13Tomasz BarwińskiAún no hay calificaciones
- Crusader Castle Al-Karak Jordan Levant Pagan Fulk, King of Jerusalem MoabDocumento3 páginasCrusader Castle Al-Karak Jordan Levant Pagan Fulk, King of Jerusalem MoabErika CalistroAún no hay calificaciones
- Catalogo Escavadeira EC27CDocumento433 páginasCatalogo Escavadeira EC27CNilton Junior Kern50% (2)
- Papalia Welcome Asl 1 Guidelines 1 1Documento14 páginasPapalia Welcome Asl 1 Guidelines 1 1api-403316973Aún no hay calificaciones
- Vtoris 100% Clean Paypal Transfer Guide 2015Documento8 páginasVtoris 100% Clean Paypal Transfer Guide 2015Sean FrohmanAún no hay calificaciones
- IGCSE 0408 Unseen Poem QuestionsDocumento5 páginasIGCSE 0408 Unseen Poem QuestionsMenon HariAún no hay calificaciones
- ACTIX Basic (Sample CDMA)Documento73 páginasACTIX Basic (Sample CDMA)radhiwibowoAún no hay calificaciones
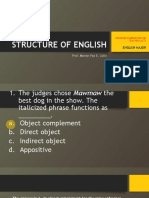
- LET-English-Structure of English-ExamDocumento57 páginasLET-English-Structure of English-ExamMarian Paz E Callo80% (5)
- OM Part B - Rev1Documento45 páginasOM Part B - Rev1Redouane BelaassiriAún no hay calificaciones
- Purification of Dilactide by Melt CrystallizationDocumento4 páginasPurification of Dilactide by Melt CrystallizationRaj SolankiAún no hay calificaciones
- LP MAPEH 10 1st Quarter Printing Final.Documento29 páginasLP MAPEH 10 1st Quarter Printing Final.tatineeesamonteAún no hay calificaciones
- Chapter S1 (Celestial Timekeeping and Navigation)Documento28 páginasChapter S1 (Celestial Timekeeping and Navigation)Марко Д. Станковић0% (1)
- دور أخلاقيات الأعمال في تحسين أداء المنظماتDocumento14 páginasدور أخلاقيات الأعمال في تحسين أداء المنظماتChaima LaifaAún no hay calificaciones
- PRINCIPLES OF TEACHING NotesDocumento24 páginasPRINCIPLES OF TEACHING NotesHOLLY MARIE PALANGAN100% (2)
- 5G NR Essentials Guide From IntelefyDocumento15 páginas5G NR Essentials Guide From IntelefyUzair KhanAún no hay calificaciones
- Science Grade 10 (Exam Prep)Documento6 páginasScience Grade 10 (Exam Prep)Venice Solver100% (3)
- International Business ManagementDocumento3 páginasInternational Business Managementkalaiselvi_velusamyAún no hay calificaciones
- Chemistry II EM Basic Learning MaterialDocumento40 páginasChemistry II EM Basic Learning MaterialMAHINDRA BALLAAún no hay calificaciones
- Alienation Thesis StatementDocumento8 páginasAlienation Thesis Statementafbteepof100% (2)
- Listening Tests 81112Documento13 páginasListening Tests 81112luprof tpAún no hay calificaciones
- Rate If Iodine and PropanoneDocumento3 páginasRate If Iodine and Propanoneshareef1Aún no hay calificaciones
- DILG Opinion-Sanggunian Employees Disbursements, Sign Checks & Travel OrderDocumento2 páginasDILG Opinion-Sanggunian Employees Disbursements, Sign Checks & Travel OrderCrizalde de DiosAún no hay calificaciones
- Ce Licensure Examination Problems Rectilinear Translation 6Documento2 páginasCe Licensure Examination Problems Rectilinear Translation 6Ginto AquinoAún no hay calificaciones
- Oral Com Reviewer 1ST QuarterDocumento10 páginasOral Com Reviewer 1ST QuarterRaian PaderesuAún no hay calificaciones