Documentos de Académico
Documentos de Profesional
Documentos de Cultura
IndianJDermatol563262-3115414 083914
Cargado por
rizgah jawasTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
IndianJDermatol563262-3115414 083914
Cargado por
rizgah jawasCopyright:
Formatos disponibles
[Downloadedfromhttp://www.e-ijd.orgonTuesday,June05,2012,IP:182.3.112.
204]||ClickheretodownloadfreeAndroidapplicationforthisjournal
CME Article
PSORIASIS IN CHILDREN: AN INSIGHT
Sandipan Dhar, Raghubir Banerjee, Nilesh Agrawal1, Sharmila Chatterjee,
Rajib Malakar2
Abstract
Onset of psoriasis in childhood is quite common. Chronicity, inflammation and hyperproliferation are the cardinal features
by which the condition establishes its uniqueness. Clearance of disease may be farfetched in most patients and relapse is
frequent. Early recognition and management of psoriasis in children and adolescents is vital in therapy in children.
Key Words: Pediatric psoriasis, relapse, therapy
Introduction pathogenesis. Two types of psoriasis have been
distinguished considering the onset age. Type I (onset 15
Psoriasis is an inherited papulosquamous disorder with
40 years) accounts for the majority of cases (>75%) and
a variable clinical spectrum. As much as 40% of adult
shows a high degree of familial aggregation and strong
patients with psoriasis have reported manifestations of
association with HLA Cw6. Correspondingly, type II begins
this condition in childhood, with at least one-third of the
after the age of 40 years. Familial prevalence is observed to
patients demonstrating features of psoriasis before the age
be greater in childhood psoriasis than in adults, with 37%
of 16.1 years. The psychosocial impairment, in addition
of adult-onset patients and 49% of pediatric-onset patients
to the physical affliction that can result from psoriasis,
having first-degree family members affected with psoriasis.
is a reminder that early recognition and management of
Some studies have reported familial incidence to be as high
psoriasis in children and adolescents is crucial.[1]
as 89% in childhood cases of psoriasis.[4,5]
Epidemiology The epidermis of any individual with the psoriatic phenotype
A definitive paucity of studies exists in the epidemiological has the capacity to express clinical disease. Expression is
backdrop of childhood psoriasis. A study of 419 patients from linked to a complex interaction of cells of the epidermis,
North India revealed the pattern and prevalence of childhood cells of the dermis, cells of the immune system, and possibly,
psoriasis in patients less than 14 years of age. The peak age other noncellular humoral elements. The keratinocytes
of onset in boys was in the 610-year age group, whereas of psoriatic patients are unique in that the inherent
the majority of girls showed an onset of psoriasis between phenotype has a capacity for hyperproliferation and altered
the ages of 10 and 14 years. A positive family history was differentiation. Proliferation and differentiation are controlled
present in only 19 (4.5%) patients. These findings differ at the level of the gene. Thus, it is important to consider not
from those of previous studies in showing a delayed onset, only cytokines and growth factors released by the various
equal sex distribution and a less frequent history of familial cell types, but also the role of regulators of transcription,
occurrence.[2] In a recent study of 137 patients from China, translation, and the modification of the cytokines and growth
aged between 3 and 14 years, 64 were males (46.7%) factors. The large number of alterations of cytokine and
and 73 were females (53.3%). Eleven patients (8%) had a growth factor profiles within psoriasis causes us to postulate
family history of psoriasis. Infection was the most common that the genetic aberration in psoriasis is quite basic, that
precipitating factor (39, 28.5%). Seasonal influence was is, it is proximal to the common element in the cascade
found in 57 patients (41.6%). Exacerbations in winter and of inflammatory events that lead to a lesion of psoriasis.
spring were noted in 29 and 16 patients, respectively.[3] About 20 genetic loci associated with psoriasis have been
reported from linkage-based studies; only one of these
Multifactorial nature of the disease and epidemiological linkage-based loci, PSORS1, that includes the HLA-C gene
evidence point to genes playing a key role in the
Access this article online
From the Department of Pediatric Dermatology, Institute of Child Quick Response Code:
Health, Kolkata, India, 1Department of Paediatrics, Bedford Hospital Website: www.e-ijd.org
NHS Trust, Bedfordshire, UK, 2Department of Epidemiology, School
of Public Health and Health Services, The George Washington
University, Washington DC, USA. Address for correspondence:
DOI: 10.4103/0019-5154.82477
Dr. Sandipan Dhar, Flat 2A2, Block 2, 5, NSC Bose Road, Kolkata -
700 040, India. E-mail: drsandipan@gmail.com
Indian Journal of Dermatology 2011; 56(3) 262
[Downloadedfromhttp://www.e-ijd.orgonTuesday,June05,2012,IP:182.3.112.204]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Dhar, et al.: Psoriasis in children
on chromosome 6p21, has been universally confirmed and Natural History of the Disease and Triggers
is considered to confer susceptibility to early-onset psoriasis.
The goal of control versus cure is a more practical outcome
Accumulating evidence points to triggers like infections
of treatment. Many randomized controlled clinical trials
(Streptococcus), cold, stress, and drugs (Chloroquine and
involving children under the age of 12 years have reported
systemic Corticosteroids) either precipitating or worsening
on two topical treatments: calcipotriol and corticosteroids.
the disease in children.[6,7]
Avoidance of triggers like trauma (Koebner phenomenon),
Clinical Features including physical, surgical, or inflammatory trauma,
should be borne in mind in this age group. A strong
Pediatric psoriasis consists of three age groups of psoriatic association between pharyngitis by group A beta-hemolytic
patients like infantile psoriasis, a self-limited disease of streptococci and the clinical activity of psoriasis (guttate
infancy, psoriasis with early onset, and pediatric psoriasis psoriasis) is now well established and should be properly
with psoriatic arthritis. The varied clinical presentations investigated where relevant.[4,10]
in childhood include plaque-type, guttate, erythrodermic,
napkin, and nail-based disease. Like all forms of auto- Management Strategies
immunity, susceptibility is likely genetic, but environmental
Many studies have investigated the use of standard
triggers are required to initiate disease activity.
psoriasis therapies in children with psoriasis, including
How Different is the Presentation in Children? topical treatments, phototherapy, and systemic therapies.
Inflammatory nature of psoriasis has initiated study of
The disease in children is more pruritic, common in girls, the use of biologic agents in children, where targeted
and the lesions are relatively thinner, softer, and less treatments have a better safety profile.
scaly. Plaque type is the most common form of disease,
but certain clinical variants are rare in children like Topical Therapy
erythroderma, arthropathy, and localized and generalized
Moisturizers have a role in normalizing hyperproliferation,
pustular psoriasis. Psoriasis in children is more frequently
and they exert anti-inflammatory effects by way of the
precipitated by infections and manifests as acute guttate
physiologic lipids. An improved barrier function and
psoriasis. However, Indian studies show that children
hydration makes the epidermis less vulnerable to external
manifest the established plaque type of disease more
trauma, thereby reducing the induction of Koebnerization.
often, rather than the guttate variety. Facial involvement Pretreatment with emollients like mineral oil or vaseline
in children is a frequent observation in majority of the augments the therapeutic efficacy of narrow-band
reports, which varies from 18 to 46%, whereas mucosal ultraviolet-B therapy, possibly because it penetrates the
involvement has been rare in Indian children.[8] intercellular space, producing an optical matching effect
A study from North India reported that extensors of which enhances the UV transmission.[11]
the legs were the most common initial site affected Salicylic acid (6% ointment and 3% shampoo) is a
[105 (25%) cases], followed by the scalp [87 (20.7%)]. keratolytic agent that can be used for small plaques on the
Classical plaque psoriasis was the most frequent clinical scalp, palms, and soles in children older than 6 years.[12]
presentation [254 (60.6%) patients], followed by plantar
psoriasis [54 (12.8%)]. Nail involvement was observed Coal tar is antiproliferative and can be used as ointment,
in 130 (31%) cases. Pitting was the most common nail cream or solution in concentrations from 0.5 to 20%. Tar
change, followed by ridging and discoloration. Five is safe and effective for childhood psoriasis, mainly for
plaque type lesions. It can be used in combination with
children (1.1%) (three girls and two boys) had psoriatic
other medications like topical corticosteroids, salicylic acid
arthropathy. Koebnerization was observed in 27.9% of
and with UV irradiation. It is irritating on the face and
patients.[9]
flexures in children. Anthralin (dithranol) is a potent anti-
Another study showed that plaque psoriasis was the most inflammatory and antiproliferative agent used as "short-
common type (52.6%), followed by guttate psoriasis contact" or "minute" therapy, to reduce side effects like
(25.5%), psoriasis pustulosa (10.9%), and psoriasis irritation and temporary perilesional staining of the skin.
erythroderma (5.1%). Scalp was the most common initial In an open study of 58 children aged 510 years treated
site affected (50.3%), nail changes were found in 25.5%, with dithranol at concentrations up to 1%, remission was
but no mucosal involvement was observed.[3] achieved in 47 (81%) patients.[13]
Goeckerman therapy for psoriasis was first described
Associated Skin Conditions
at the Mayo Clinic in 1925, and in a study undertaken,
The co-morbidities of childhood psoriasis include allergic the responses were excellent (62% of patients had 90%
contact dermatitis, eczema, vitiligo and alopecia areata. clearance or greater, 23% had 8089% clearance of
Psoriasis is sometimes misdiagnosed as dermatitis lesions), hence proving it as an option for children with
seborrheica, neurodermatitis and balanitis. moderate to severe psoriasis.[14]
263 Indian Journal of Dermatology 2011; 56(3)
[Downloadedfromhttp://www.e-ijd.orgonTuesday,June05,2012,IP:182.3.112.204]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Dhar, et al.: Psoriasis in children
Corticosteroids still remain the mainstay topical treatment patient with guttate psoriasis was treated with amoxicillin/
of psoriasis, as they have anti-inflammatory and clavulanic acid (50 mg/kg/d), which cleared all lesions
antiproliferative properties and reduce erythema, scaling, after 20 days.[21,22]
and pruritus. Topical corticosteroids are used in chronic
Methotrexate (MTX) is an antimetabolite agent with
plaque type psoriasis as monotherapy or in combination
immunomodulatory and anti-inflammatory properties, and
with topical treatments like calcipotriol and tazarotene.
has advantages of efficacy, affordability and convenient
Lower potency preparations are indicated for facial, genital
weekly oral dose. In children, 0.20.4 mg/kg/wk orally is
and intertriginous skin areas, whereas thick hyperkeratotic
recommended. A review of 10 cases of childhood psoriasis
areas, such as the palms and soles, require high potency
treated with MTX showed a complete clearance in 20%
agents. Halobetasol cream 0.05% and clobetasol propionate
cases, almost complete clearance in 60% cases, and no
emulsion 0.05% seem to be efficacious treatments in
response in 10% of cases. MTX was given at an initial
childhood plaque psoriasis. Reported side effects were
dose of 0.030.24 mg/kg/wk and was increased according
relatively mild in the treatment period of 2 weeks. A case
to the patients response to 0.100.41 mg/kg/wk; duration
report described the use of hydrocortisone 1% ointment in
of treatment was from 6 to 178 weeks. A study revealed
a 2-year-old child with pustular psoriasis.[15,16]
the treatment results in childhood psoriasis with MTX in
Calcipotriene (calcipotriol) is a nonsteroidal alternative in seven children (four boys, three girls) over 7.5 years. Their
the treatment of mild to moderate plaque type psoriasis ages and duration of disease varied from 3.5 to 16 years
and has utility as monotherapy, as well as in combinations (mean 12.14 years) and from 4.8 months to 5 years (mean
with topical steroids. Oranje performed a randomized 2.2 years), respectively. Psoriatic erythroderma was seen
double-blind study in 77 juvenile patients with twice daily in three patients, generalized pustular psoriasis in two, and
applications for 8 weeks. The investigators reported a recalcitrant psoriasis and psoriatic arthropathy in one each.
decrease in psoriasis area-and-severity index (PASI) score Pre-MTX liver biopsy performed in four children showed
of 52% in the vitamin D group. The amount for use in grade I changes. MTX was given in a single weekly oral
children is a maximum dose of 75 g/week for children aged dose of 3.7525 mg (mean 16.6 mg). The duration of
over 12 years and 50 g/week for those aged 612 years.[17] treatment necessary to control the disease varied from 6
Topical tacrolimus (0.03%, 0.1%) ointment and pimecrolimus to 10 weeks (mean 7.9 weeks). Total duration of MTX
(1%) cream are nonsteroidal immunomodulating therapy was from 31.2 to 46.4 weeks (mean 38.8 weeks).
macrolactams which block the enzyme calcineurin, thereby Post-therapy disease-free interval ranged between 14.4 and
inhibiting the production of IL-2 and subsequent T-cell 16.8 weeks (mean 15.5 weeks). Follow-up after withdrawal
activation and proliferation. In two nonrandomized clinical of MTX was from 16 to 28 weeks (mean 22.3 weeks).
trials, treatment of facial and flexural psoriasis with Total cumulative MTX dose ranged from 390 to 960 mg
tacrolimus 0.1% was evaluated in which all patients showed (mean 683.6 mg). Side effects were nausea and vomiting
clearance after a treatment period varying from 2 to 30 days. reported in three patients.[23,24]
Tacrolimus 0.1% was also used in one case report in which Acitretin is an aromatic retinoid that acts in psoriasis by
facial psoriasis cleared totally.[18] its anti-inflammatory activity. Treatment should be initiated
Phototherapy is preferred in older children and adolescents and maintained at dosages at or below 0.51 mg/kg/d to
with moderate to severe disease in which topical treatments limit short- and long-term toxicities and therapy should
have failed. Guttate and thin plaque type lesions respond be continued for about 2 months after clinical remission.
best to phototherapy. NB-UVB shows good results in the Major limitation of oral retinoids (acitretin) in children is
treatment of plaque and guttate psoriasis in childhood and has the risk of growth retardation due to premature closure
comparatively milder side effects for the treatment duration of epiphyses on long-term use. In the open-label study,
studied. Two open-label studies were performed. Jain et al. three patients with psoriasis erythroderma were treated
examined NB-UVB treatment for 12 weeks. PASI 90 was with etretinate in a dosage ranging from 0.5 to 0.9 mg/
achieved in 60% of patients. It needs to be mentioned that kg/d. After 45 months of treatment, they all had complete
all the patients had skin type IV.[19] Tay et al. also studied clearance of erythema and scaling.[25] Etretinate was used as
NB-UVB treatment, where after a mean treatment of 11.9 a treatment for plaque psoriasis in two children where both
weeks, clearance was reached in all the patients.[20] the patients had an excellent response.[26]
Cyclosporine primarily acts by inhibiting T-cell function
Systemic Agents and interleukin (IL)-2 and is effective in severe forms
Role of oral antibiotics remains controversial. In one study, of psoriasis such as pustular or erythrodermic psoriasis
thiamphenicol was used and there was less than 50% or when other therapies are ineffective. Three patients
clearance of lesions. Four patients in a case series were with pustular psoriasis have been described in whom the
treated with erythromycin (50 mg/kg/d) for 2 weeks; in all administered dose was from 1 to 2 mg/kg/d. Complete
the patients, the psoriasis lesions disappeared completely. A disappearance of lesions was seen in two patients who were
Indian Journal of Dermatology 2011; 56(3) 264
[Downloadedfromhttp://www.e-ijd.orgonTuesday,June05,2012,IP:182.3.112.204]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Dhar, et al.: Psoriasis in children
treated for 12 and 6 months, and the third patient showed psoriasis to UVB therapy after pretreatment with a lubricating
a significant improvement after 5 months of treatment.[27] base. A single-blind controlled study. Pediatr Dermatol
2008;25:559-64
The inflammatory nature of psoriasis has also prompted 12. Fluhr JW, Cavallotti C, Berardesca E. Emollients, moisturizers,
further study of the use of biologic therapeutics in and keratolytic agents in psoriasis. Clin Dermatol 2008;26:380-6.
children, where targeted treatments may offer a safer 13. Zvulunov A, Anisfeld A, Metzker A. Efficacy of short-contact
option. Biologics are drugs including antibodies and fusion therapy with dithranol in childhood psoriasis. Int J Dermatol
proteins targeting cytokines like tumor necrosis factor that 1994;33:808-10.
plays an important role in psoriasis.[28] Etanercept has been 14. Kortuem KR, Davis MD, Witman PM, McEvoy MT. Results
found to be overall effective and well tolerated in children of Goeckerman treatment for psoriasis in children: A 20-year
and adolescents with moderate-to-severe plaque psoriasis. retrospective review. J Am Acad Dermatol 2007;56:AB9.
In a 48-week study, 211 patients with psoriasis (417 years 15. Kimball AB, Gold MH, Zib B, Davis MW. Clobetasol propionate
emulsion formulation foam 0.05%: Review of phase II open-
of age) were initially randomly assigned to a double-blind
label and phase III randomized controlled trials in steroid-
trial of 12 once-weekly subcutaneous injections of placebo responsive dermatoses in adults and adolescents. J Am Acad
or 0.8 mg of etanercept per kilogram of body weight (to Dermatol 2008;59:448-54.
a maximum of 50 mg), followed by 24 weeks of once- 16. Herz G, Blum G, Yawalkar S. Halobetasol propionate cream by
weekly open-label etanercept. At week 36, 138 patients day and halobetasol propionate ointment at night for the treatment
underwent a second randomization to placebo or etanercept of pediatric patients with chronic, localized plaque psoriasis and
to investigate the effects of withdrawal and retreatment. atopic dermatitis. J Am Acad Dermatol 1991;25:1166-9.
The primary end point was 75% or greater improvement 17. Oranje AP, Marcoux D, Svensson A, Prendiville J, Krafchik B,
from baseline in the PASI 75 at week 12.[29] Toole J, et al. Topical calcipotriol in childhood psoriasis. J Am
Acad Dermatol 1997;36:203-8.
Counseling 18. Clayton TH, Harrison PV, Nicholls R, Delap M. Topical
tacrolimus for facial psoriasis. Br J Dermatol 2003;149:419-20.
This chronic disease, punctuated by remissions and 19. Jain VK, Aggarwal K, Jain K, Bansal A. Narrow-band UV-B
exacerbations, has a profound impact on the quality of life phototherapy in childhood psoriasis. Int J Dermatol 2007;46:320-2.
of the child. The family must learn to deal with the illness, 20. Tay YK, Morelli JG, Weston WL. Experience with UVB
considering the psychological burden on the child. phototherapy in children. Pediatr Dermatol 1996;13:406-9.
21. Juanqin G, Zhiqiang C, Zijia H. Evaluation of the effectiveness
References of childhood generalized pustular psoriasis treatment in 30 cases.
1. Pootrakul L, Kalb RE. The management of psoriasis in children Pediatr Dermatol 1998;15:144-6.
and adolescents. G Ital Dermatol Venereol 2010;145:259-68. 22. Pacifico L. Acute guttate psoriasis after streptococcal scarlet
2. Kumar B, Jain R, Sandhu K, Kaur I, Handa S. Epidemiology of fever. Pediatr Dermatol 1993;10:388-9.
childhood psoriasis: A study of 419 patients from northern India. 23. Collin B, Ogboli M, Moss C. Methotrexate therapy in 10 children
Int J Dermatol 2004;43:654-8 with severe plaque psoriasis: P-29. Br J Dermatol 2006;155:33.
3. Wu Y, Lin Y, Liu HJ, Huang CZ, Feng AP, Li JW. Childhood 24. Kumar B, Dhar S, Handa S, Kaur I. Methotrexate in childhood
psoriasis: A study of 137 cases from central China. World J psoriasis. Pediatr Dermatol 1994;11:271-3.
Pediatr 2010;6:260-4. 25. Kim BS, Shin S, Youn JI, Lee YS. Treatment of erythrodermic
4. Dogra S, Kaur I. Childhood psoriasis. Indian J Dermatol psoriasis with etretinate. Ann Dermatol 1991;3:107-11.
Venereol Leprol 2010;76:357-65. 26. van der Rhee HJ, van Gelderen HH, Polano MK. Is the use of
5. Farber EM, Mullen RH, Jacobs AH, Nall L. Infantile psoriasis: A Ro 10-9359 (Tigason) in children justified? Acta Derm Venereol
follow up study. Pediatr Dermatol 1986;3:237-43. 1980;60:274-5.
6. Raychaudhuri SP, Gross J. A comparative study of pediatric 27. Kilic SS, Hacimustafaoglu M, Celebi S, Karadeniz A, Ildirim
onset psoriasis with adult onset psoriasis. Pediatr Dermatol I. Low dose cyclosporin A treatment in generalized pustular
2000;17:174-8. psoriasis. Pediatr Dermatol 2001;18:246-8.
7. Valdimarsson H. The genetic basis of psoriasis. Clin Dermatol 28. Pootrakul L, Kalb RE. The management of psoriasis in children
2007;25:563-7. and adolescents. G Ital Dermatol Venereol 2010;145:259-68.
8. Nanda A, Kaur S, Kaur I, Kumar B. Childhood psoriasis: 29. Paller AS, Siegfried EC, Langley RG, Gottlieb AB, Pariser D,
An epidemiological survey of 112 patients. Pediatr Dermatol Landells I, et al. Etanercept treatment for children and adolescents
1990;7:19-21. with plaque psoriasis. N Engl J Med 2008;358:241-51.
9. Kumar B, Jain R, Sandhu K, Kaur I, Handa S. Epidemiology of
childhood psoriasis: A study of 419 patients from northern India.
Int J Dermatol 2004;43:654-8.
How to cite this article: Dhar S, Banerjee R, Agrawal N, Chatterjee
10. Cassandra M, Conte E, Cortez B. Childhood pustular psoriasis S, Malakar R. Psoriasis in children: An insight. Indian J Dermatol
elicited by the streptococcal antigen: A case report and review of 2011;56:262-5.
the literature. Pediatr Dermatol 2003;20:506-10. Received: March 2011. Accepted: March 2011.
11. Jain VK, Bansal A, Aggarwal K, Jain K. Enhanced response of Source of support: Nil, Conflict of Interest: Nil.
265 Indian Journal of Dermatology 2011; 56(3)
También podría gustarte
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Proofs EuJMI 03 258Documento10 páginasProofs EuJMI 03 258rizgah jawasAún no hay calificaciones
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Tuberculosis LaryngitisDocumento15 páginasTuberculosis Laryngitisrizgah jawasAún no hay calificaciones
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- CASE Allergic RhinitisDocumento5 páginasCASE Allergic Rhinitisrizgah jawas100% (1)
- Anatomy of NoseDocumento8 páginasAnatomy of Noserizgah jawas100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- New Book "101 Costly HR Mistakes... and How To Fix Them" by Vanessa Nelson Released To Help Employers Avoid Costly HR Mistakes and Save MillionsDocumento2 páginasNew Book "101 Costly HR Mistakes... and How To Fix Them" by Vanessa Nelson Released To Help Employers Avoid Costly HR Mistakes and Save MillionsPR.comAún no hay calificaciones
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- Floret Fall Mini Course Dahlia Sources Updated 211012Documento3 páginasFloret Fall Mini Course Dahlia Sources Updated 211012Luthfian DaryonoAún no hay calificaciones
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- A Cook's Journey To Japan - Fish Tales and Rice Paddies 100 Homestyle Recipes From Japanese KitchensDocumento306 páginasA Cook's Journey To Japan - Fish Tales and Rice Paddies 100 Homestyle Recipes From Japanese KitchensEthan F.100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Schedule NDocumento3 páginasSchedule Nmittal kelaAún no hay calificaciones
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- An Energy Saving Guide For Plastic Injection Molding MachinesDocumento16 páginasAn Energy Saving Guide For Plastic Injection Molding MachinesStefania LadinoAún no hay calificaciones
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- White Vaseline: Safety Data SheetDocumento9 páginasWhite Vaseline: Safety Data SheetHilmi FauziAún no hay calificaciones
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- UgpeDocumento3 páginasUgpeOlety Subrahmanya SastryAún no hay calificaciones
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Free Higher Education Application Form 1st Semester, SY 2021-2022Documento1 páginaFree Higher Education Application Form 1st Semester, SY 2021-2022Wheng NaragAún no hay calificaciones
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- Metabolism of Carbohydrates and LipidsDocumento7 páginasMetabolism of Carbohydrates and LipidsKhazel CasimiroAún no hay calificaciones
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
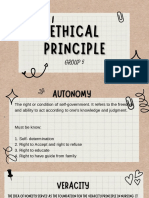
- Group 5 - Ethical PrinciplesDocumento11 páginasGroup 5 - Ethical Principlesvirgo paigeAún no hay calificaciones
- Debunking The Evergreening Patents MythDocumento3 páginasDebunking The Evergreening Patents Mythjns198Aún no hay calificaciones
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Safety AuditDocumento9 páginasSafety AuditRobena Nagum BagasAún no hay calificaciones
- Chap 6 - Karen HorneyDocumento95 páginasChap 6 - Karen HorneyDiana San JuanAún no hay calificaciones
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- Issue of HomosexualityDocumento4 páginasIssue of HomosexualityT-2000Aún no hay calificaciones
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- LIC Jeevan Labh Plan (836) DetailsDocumento12 páginasLIC Jeevan Labh Plan (836) DetailsMuthukrishnan SankaranAún no hay calificaciones
- PPC Production PlantDocumento106 páginasPPC Production PlantAljay Neeson Imperial100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- Blood DonationDocumento19 páginasBlood DonationsuruthiAún no hay calificaciones
- Chapter FourDocumento9 páginasChapter FourSayp dAún no hay calificaciones
- 13105389Documento22 páginas13105389Larry RicoAún no hay calificaciones
- Resume Massage Therapist NtewDocumento2 páginasResume Massage Therapist NtewPartheebanAún no hay calificaciones
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Frequency Inverter: User's ManualDocumento117 páginasFrequency Inverter: User's ManualCristiano SilvaAún no hay calificaciones
- Vital Statistics: Presented by Mrs - Arockia Mary Associate ProfDocumento17 páginasVital Statistics: Presented by Mrs - Arockia Mary Associate ProfraghumscnAún no hay calificaciones
- BCA2006 BCA GuideDocumento507 páginasBCA2006 BCA GuidePatrick LiaoAún no hay calificaciones
- Unit-7 (EVS)Documento32 páginasUnit-7 (EVS)g6614134Aún no hay calificaciones
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- Nodular Goiter Concept MapDocumento5 páginasNodular Goiter Concept MapAllene PaderangaAún no hay calificaciones
- Packed Bed Reactor Slides (B)Documento32 páginasPacked Bed Reactor Slides (B)Meireza Ajeng PratiwiAún no hay calificaciones
- Biodegradable Plastic Bag Manufacturing Industry-800655 PDFDocumento68 páginasBiodegradable Plastic Bag Manufacturing Industry-800655 PDFAryanAún no hay calificaciones
- BUERGER's Inavasc IV Bandung 8 Nov 2013Documento37 páginasBUERGER's Inavasc IV Bandung 8 Nov 2013Deviruchi GamingAún no hay calificaciones
- SA 8000 Audit Check List VeeraDocumento6 páginasSA 8000 Audit Check List Veeranallasivam v92% (12)
- Chapter 4 CrystallizationDocumento13 páginasChapter 4 Crystallizationprosedur0% (1)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)