Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Anesthesia - Dr. Firmalino
Cargado por
miguel cuevasTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Anesthesia - Dr. Firmalino
Cargado por
miguel cuevasCopyright:
Formatos disponibles
ANESTHESIA ORGANS EFFECTS
Cardiovascular System
Dr. Firmalino Arterial Pressure
Halothane
Anesthesia Desflurane
Suppression of pain of a surgical procedure Enflurane
Analgesia Sevoflurane
Loss of pain sensation from other causes Isoflurane
General Anesthesia Bradycardia
With loss of consciousness Halothane
Local Anesthesia Tachycardia
Patient is awake Isoflurane
Desflurane
No Effect on Rate
GENERAL ANESTHESIA Methoxyflurane
Sevoflurane
1. Inhalation Myocardial Depression
2. Parenteral All inhaled anesthesia
o IM GREATEST depression
o IV Enflurane
Halothane
LEAST depression
Stages of General Anesthesia
Nitrous oxide
1. Analgesia
Arrhythmia
2. Delirium/ excitement
Halothane
3. Surgical
4. Medullary paralysis
Respiratory
MOST depressant
PharmacoKINETICS of General Anesthesia
Isoflurane
1. Flow
Enflurane
o Anesthesia machine lungs blood brain
Depress mucocilliary function pooling of mucus (atelectasis,
metabolism elimination
pneumonia)
2. Factor
Bronchodilation
o Tension difference or partial pressure between alveoli
Halothane
and blood
Enflurane
o From higher to lower concentration
Irritation & coughing difficult induction
3. Uptake & distribution
Desflurane
4. Solubility
5. Concentration in inspired air
6. Pulmonary ventilation
Brain
7. Pulmonary blood flow Cerebral Blood Flow undesirable ICP
8. Arteriovenous concentration Enflurane (potential seizure)
9. Elimination Nitrous Oxide (least in cerebral blood flow)
HEPATOTOXIC
PharmacoDYNAMICS Halothane (Fatal hepatitis)
Mechanism of Action of GENERAL anesthesia
1. Depresses the activity of the neurons
NEPHROTOXIC
2. Interacts with lipid matrix of nerve membrane which leads to
Methoxyflurane
changes in ion flux
o RESULTS to membrane HYPERPOLARIZATION (inhibitory
Malignant Hyperthermia
action) via activation of ligand gated K+ channel linked
Halothane
to neurotransmitters (Ach, Dopamine, NE, Serotonin)
o TARGET: to activate GABA receptor Chloride channel Syndrome
(mediator of inhibitory synaptic transmission) o Hyperthermia
o RESULT: activity of neurons, sensory transmission o Tachycardia
o Rigidity
Ideal Characteristics of Inhalational Anesthetics: o Hypertension
o Hyperkalemia
Rapid & pleasant induction & recovery
o Acidosis
Rapid changes in depth of anesthesia
Due to free calcium in muscle
Adequate relaxation of smooth muscle
Treatment: DANTROLENE (prevents release of Calcium)
Absence of toxic effect
Wide margin of safety
Page | 1 jhojho terrobias.2016
CHRONIC TOXICITY SEVOFLURANE
Mutagenicity no evidence o Non-irritant to airway
Fluroxene & ether (no longer used)
Carcinogenecity no evidence NON-HALOGENATED
Reproductive ETHER
st
Miscarriage o 1 anesthetic
Teratogenic o No longer used
Hematotoxic o Explosive & flammable
Nitrous Oxide (Megaloblastic Anemia) CHLOROFORM
o No longer used
CLINICAL USE o Non explosive & non flammable
Rarely used alone
Combined with IV anesthetics GASEOUS
Commonly used NITROUS OXIDE
o Nitrous oxide o Only inorganic gas w/ anesthetic property
o Desflurane o Non-explosive
o Sevoflurane o Potent analgesic
o Isoflurane o Weak anesthetic
o Halothane o No muscle relation
o No CVS effect
NOT USED ANYMORE o Anesthetic of choice, combined w/ Halothane
Methoxyflurane (nephrotoxic) CYCLOPROPANE
Chloroform (hepatotoxic) o No longer used
Cyclopropane & ether (explosive, flammable) o Explosive
o Flammable
CLASSIFICATION
Gas (Nitrous Oxide, Cyclopropane) INTRAVENOUS ANESTHETIC
VOLATILE LIQUID Usually used as ADJUNCT to inhaled anesthetics
HALOGENATED o Sometime used alone
o Halothane o Do not require anesthesia machine
o Isoflurane DRUGS used as IV ANESTHETICS
o Sevoflurane Barbiturates
o Methoxyflurane Benzodiazepine
o Enflurane Ketamine
o Desflurane Profopol
NON HALOGENATED Etomidate
o Ether Opiate
o Chloroform
SHORT-ACTING IV ANESTHETICS
HALOGENATED Rapid onset
HALOTHANE Out-patient
o Choice in ASTHMA (bronchodilation effect) Barbiturate Thiopental
o TOXICITY Ketamine
Arrhythmia, Hepatitis Profopol
Malignant hyperthermia Opiate
ENFLURANE
o CNS irritability seizure LONG-ACTING IV ANESTHETICS
o Nephrotoxic (fluoride byproduct) Slow onset
o Cardiac depression
Cant be used for induction
o salivation & tracheobronchial secretion
Maintenance if used w/ inhalation
o Non hepatotoxic
Pre-op meds relax patients & reduce anxiety
ISOFLURANE
Benzodiazepines (diazepam, midazolam, lorazepam)
o Non hepatotoxic
w/ retrograde amnesia patients do not remember the
o Non nephrotoxic
unpleasant surgery
o Non cardiotoxic
o Choice in CARDIAC SURGERY
ULTRA SHORT ACTING BARBITURATES
METHOXYFLURANE
THIOPENTAL
o Most toxic
o Onset: 10-20 seconds
DESFLURANE
o Last for: 20-30mins
o BP & CO
o For short procedures
o No hepatorenal toxicity
o Airway irritant
Page | 2 jhojho terrobias.2016
CARDIAC MUSCLE Effects
LOCAL ANESTHESIA LOW concentration Anti-arrhythmic
HIGH dosage arrhythmia
Blocks nerve conduction locally, thus blocks pain sensation
thru SODIUM channel BLOCKADE CLINICAL PHARMACOLOGY
SHORT acting
CHEMISTRY o Procaine
o Chlorprocaine
ESTER
INTERMEDIATE acting
o Cocoine
o Lidocaine
o Procaine
o Mepivacaine
o Tetracaine
o Prilocaine
o Benzocaine
AMIDE LONG acting
o Lidocaine o Tetracaine
o Mepivacaine o Bupivacaine
o Bupivacaine o Etidocaine
o Etidocaine o Ropivacaine
o Prilocaine
o Ropivacaine ONSET
FASTER if MIXED with SODIUM BICARBONATE CO2
increases penetration of anesthesia into membrane
PharmacoKINETICS SLOW in INFECTION acidic inflammation
ABSORPTION
Local anesthesia has to stay where injected to sustain its ROUTES
effect Topical
Once absorbed losses its effect as a local anesthesia Local infiltration
& systemic effect or toxicity may potentially happen
Nerve block
More vascular tissue absorbs drug faster duration
Spinal intrathecal
is shorter
Epidural
Vasoconstrictor EPINEPHRINE delays absorption &
Caudal
prolongs local effect
TOXICITY
PharmacoDYNAMICS Only when the anesthesia is ABSORBED in circulation
Mechanism of Action CNS TOXICITY
Binding with SODIUM channel receptor of nerve LOW DOSE
membrane o Sleepiness
Blockade of the excitable membrane of axon = blocking o Lightheadedness
nerve impulse o Visual/ auditory disturbance
o Restlessness
Action of Local Anesthesia on Nerve o Circumoral/ tongue numbness
Both sensory & motor blockade HIGH DOSE
Motor Paralysis o Nystagmus
o Maybe undesirable in normal delivery w/c o Muscle twitching
require abdominal muscle contraction o Convulsion
o Desirable in abdominal operations like CS o CNS depression
(requires abdominal muscle relaxation) o Death
o PREVENTION/TREATMENT: Diazepam,
Actions on Nerve barbiturates, O2
Autonomic parasympathetic blockade NERVE TOXICITY
o vasoDILATION, HYPOtension Prolonged motor/ sensory with CHLORPROCAINE or
SEQUENCE of Blockade LIDOCAINE if used as spinal Anesthesia
o Autonomic
o Temperature CVS TOXICITY
o Pain Blocks SODIUM channel in heart pacemaker, excitability,
o Touch conduction
o Deep pressure Blocks CALCIUM channel depress contraction
o Motor (hypotension: BUPIVACAINE)
Except COCAINE (vasoconstriction & HYPERtension) blockade
Actions on Nerve of NE reuptake
In EXTREMITY Cause ischemia & ulceration if used in nasopharyngeal
o Proximal sensory fibers are located in the mucosa
st
OUTER layer blocked 1 before distal fibers
Page | 3 jhojho terrobias.2016
BLOOD TOXICITY
Methhemoglobinemia PRILOCAINE ANESTHESIA
ALLERGY th
Katzung 11 edition
Common with ESTERS (metabolized to P-aminobenzoic
acid which cause the allergy)
Physiologic state induced by GENERAL anesthesia
Analgesia
Amnesia
Loss of consciousness
Inhibition of sensory and autonomic reflexes
Skeletal muscle relaxation
Ideal anesthetic drug would induce:
Smooth & rapid loss of consciousness
Allowing prompt recovery after its administration is
discontinued
Wide margin of safety
Devoid of adverse effects
Balanced anesthesia techniques
Use of combinations of IV and inhaled drugs
Monitored anesthesia care techniques
Oral or parenteral sedatives in combination with local
anesthetics
TYPES of GENERAL ANESTHESIA
1. INTRAVENOUS anesthetics
Alone or in combination with other anesthetic & analgesic
drugs
Barbiturates (thiopental, methohexital)
Benzodiazepines (midazolam, diazepam)
Propofol
Ketamine
Opioid analgesics (morphine, fentanyl, sufentanil, alfentanil,
remifentanil)
Miscellaneous sedative-hypnotics (etomidate,
dexmedetomidine)
2. INHALED anesthetics
Most commonly used inhaled anesthetics:
o Isoflurane
o Desflurane
o Sevoflurane
Volatile liquids that are aerosolized in specialized vaporizer
delivery systems
Nitrous Oxide gas at ambient temperature & pressure,
adjuvant to volatile agents
Balanced Anesthesia
Combination of IV & inhaled
Sevoflurane (volatile anesthetics) induction of anesthesia
Propofol (intravenous anesthetics) infused for
maintenance of anesthesia
Muscle relaxants facilitate tracheal intubation & optimize
surgical conditions
Potent opioid & cardiovascular drugs ( blockers, 2 agonists,
Ca channel blockers) control transient autonomic
responses to noxious surgical stimuli
Page | 4 jhojho terrobias.2016
STAGES of ANESTHESIA (Guedels signs) o Blood:gas partition coefficient
Stage of ANALGESIA Useful index of solubility
Analgesia without amnesia Defines the relative affinity of an
anesthetic for the blood
Later in stage I: both analgesia & amnesia produced
DESFLURANE & NITROUS OXIDE
Stage of EXCITEMENT
Insoluble in blood
Delirious & may vocalized but is definitely amnesic
LOW blood:gas partition
Respiration: irregular both in volume & rate
coefficient
Retching & vomiting may occur
o LOW blood SOLUBILITY diffuses from the lung
To limit duration & severity: rapidly increasing the
into the arterial blood
concentration of agent
Few molecules are required to raise its
Ends: reestablishment of regular breathing
partial pressure
Stage of SURGICAL ANESTHESIA
Arterial tension rises RAPIDLY
Begins: recurrence of regular respiration o MODERATE HIGH solubility (halothane &
Extends to complete cessation of spontaneous respiration isoflurane)
(apnea)
More molecules dissolve before partial
Four planes: (changes in) pressure changes significantly
o Ocular movements Arterial tension of the gas increases LESS
o Eye reflexes rapidly
o Pupil size o NITROUS OXIDE
*signs of increasing depth of anesthesia Low solubility
Stage of MEDULLARY DEPRESSION Reaches high arterial tension RAPIDLY
Deep stage RAPID equilibration with the brain
Severe depression of CNS FAST onset of action
o Vasomotor center in the medulla
o Respiratory center in the brain stem B. Anesthetic CONCENTRATION in the INSPIRED AIR
o Direct effects on BOTH maximum tension (alveoli)
Anticholinergic drugs (atropine, glycopyrrolate) & rate of increase in its tension in arterial blood
Used to decrease oral & airway secretions o INCREASE CONCENTRATION
Treat BRADYcardia Increase the rate of induction by
Can also DILATE pupils increasing the rate of transfer into the
Opioid Analgesics blood according to Ficks law
Depressant effects on both the respiratory function & HR o MODERATE CONCENTRATION
Enflurane, Isoflurane, halothane
Most reliable indication that stage III is achieved: Advantageous
Loss of purposeful motor & autonomic responses to noxious Often administered in combination with
stimuli a LESS soluble agent (Nitrous Oxide)
Reestablishment of a regular respirator pattern Reduce time required for loss
of consciousness
Adequacy of the DEPTH of anesthesia is assessed by: Achievement of a surgical
Monitoring changes in respiratory & cardiovascular depth of anesthesia
responses to specific surgical stimuli
Changes in electroencephalographic based cerebral indices C. PULMONARY VENTILATION
Vital signs: most common method of assessing depth of o Rate of rise of anesthetic gas tension in arterial
anesthesia blood is DIRECTLY dependent on BOTH rate &
Automated cerebral monitoring techniques depth of ventilation
o EEG signals o INCREASE ventilation only a slight increase in
o Bispectral index arterial tension with LOW blood solubility
o Auditory evoked potential o HYPERVENTILATION INCREASES speed of
o Physical state index induction of anesthesia with inhaled anesthetics
o Cerebral state index that would normally have a SLOW onset
o State & response entropy (irregularity) of EEG o DEPRESSION of respiration(opioids) SLOWS the
waveforms onset of anesthesia
PharmacoKINETICS D. PULMONARY BLOOD FLOW
Uptake & Distribution of INHALED anesthetics o INCREASE (CO) SLOWS the rate of rise in
arterial tension (moderate-high blood solubility)
Concentration of inhaled anesthetic is proportional to its
partial pressure (tension) Exposes a larger volume of blood to the
anesthetic agent in the alveoli
A. SOLUBILITY
o One of the most important factors influencing the increasing rate of rise in the arterial
tension of inhaled anesthetic
transfer of an anesthetic from the lungs to the
arterial blood o Patients with circulatory SHOCK combined
effects of DECREASED CO (pulmonary blood flow)
Page | 5 jhojho terrobias.2016
& INCREASE ventilation ACCELERATE induction Reverse transfer process cannot be
of anesthesia (halothane & isoflurane) enhanced because concentration in the
lungs cannot be reduced below zero
E. ARTERIOVENOUS CONCENTRATION GRADIENT o Beginning of recovery phase anesthetic gas
o Dependent mainly on uptake of the anesthetic by tension in different tissues may be quite variable
the tissues (nonneuronal tissues) INSOLUBLE in blood (LOW blood:gas partion coefficients) &
o Venous blood RETURNING to the lungs may brain eliminated at FASTER rates
contain significantly LESS anesthetic than arterial RAPID WASH OUT RATE rapid recovery from anesthetic
blood effects
o GREATER difference in anesthetic gas tension o Nitrous oxide
MORE time it will take to achieve equilibrium with o Desflurane
brain tissue o Sevoflurane
o Anesthetic entry into tissues is influenced by HALOTHANE 2x soluble in brain & 5x more soluble in
factors that determine transfer of anesthetic from blood
lung to intravascular space o Elimination SLOW
Tissue:blood partition coefficients Duration of exposure:
Rates of blood flow to the tissues o MORE SOLUBLE (halothane, isoflurane)
Concentration gradients Recovery is SLOW after PROLONGED
o INDUCTION PHASE (& initial phase of maintenance administration)
period) o Accumulation of anesthetics in muscle, skin & fat
Tissues that exert greatest influence on INCREASES with PROLONGED exposure
the arteriovenous anesthetic Blood tension may DECLINE SLOWLY
concentration gradient are those that are during recovery (anesthetic eliminated
HIGHLY PERFUSED (brain, heart, liver, slowly)
kidneys, splanchnic bed) CLEARANCE via the LUNGS
Receive 75% of the resting CO o Major route of elimination
Volatile anesthetics w/ HIGH SOLUBILITY o Hepatic metabolism may also contribute to
in HIGHLY perfused tissues venous elimination
blood concentration will initially be very HALOTHANE
LOW & equilibrium with the arterial o Oxidative metabolism formation of
blood is achieved SLOWLY trifluoroacetic acid and release of bromide &
o MAINTENANCE of anesthesia with inhaled chloride ions
anesthetics o LOW OXYGEN TENSION halothane is
Drug continues to be transferred at rates metabolized to chlorotrifluoroethyl free radical
dependent on solubility of the agent, (capable of reacting with the hepatic membrane
concentration gradient between blood components HALOTHANE-INDUCED HEPATITIS)
and tissue and tissue blood flow Isoflurane & Desflurane
Muscle & skin 50% of total body mass o least metabolized of the fluorinated anesthetics
Anesthetics accumulate more with only trace concentrations of trifluoroacetic
SLOWLY acid appearing in the URINE even after prolonged
Receive only 1/5 of the resting administration
CO Enflurane & Sevoflurane
Most anesthetic agents are HIGHLY o metabolism results in the formation of fluoride ion
soluble in ADIPOSE tissues LOW blood Methoxyflurane
perfusion to theses tissues DELAYS o renal fluoride levels do not reach toxic levels under
accumulation normal circumstances
Equilibrium is Unlikely to occur o 70% is metabolized by liver
with most anesthetics during a o Released fluoride ions can produce nephrotoxicity
typical 1-3 hour operation Sevoflurane
o Degraded by contact with the carbon dioxide
ELIMINATION absorbent in anesthesia machines
Blood:gas partition coefficient o Yielding a vinyl ether (compound A) renal
o One of the most important factors governing rate damage if HIGH concentrations are absorbed
of recovery Extent of Hepatic Metabolism (ranking)
Other factors: 1. Methoxyflurane
o Pulmonary blood flow 2. Halothane
o Magnitude of ventilation 3. Enflurane
o Tissue solubility of the anesthetic 4. Sevoflurane
2 Features of the recovery phase 5. Isoflurane
o Transfer of an anesthetic from lungs to blood can 6. Desflurane
be ENHANCED by INCREASING its concentration in 7. Nitrous oxide not metabolized by human tissues |
inspired air bacteria in the GIT may be able to break down the
nitrous oxide molecule
Page | 6 jhojho terrobias.2016
PharmacoDYNAMICS o HIGH concentrations activity is depressed
MECHANISM of ACTION (cardiorespiratory collapse stage IV)
Both inhaled & IV depress spontaneous & evoke activity of
neurons in many regions of the brain DOSE-RESPONSE CHARACTERISTICS: The Concept of Minimum
Alveolar Anesthetic Concentration & the Continuum of CNS
Meyer-Overton principle interactions of these agents
Depression
with the lipid matrix of the nerve membrane that were
thought to lead to secondary changes in ion flux Quantal dose-response principles
o Useful estimate of anesthetic potency for both
1. Primary molecular target of GENERAL anesthetics: inhaled & IV
o GABAA receptor-CHLORIDE channel (major INHALATION anesthesia
mediator of inhibitory synaptic transmission) o Partial pressure of inhaled anesthetic in the brain
o Pentameric assembly of 5 proteins derived from equals that in the lung when steady-state
several polypeptide subclasses conditions are achieved
Volatile anesthetic concentration percentage of the
Inhaled anesthetics, barbiturates, benzodiazepine, alveolar gas mixture or partial pressure of anesthetic as a
etomidate, propfol) percentage of 760mmHg
Facilitate GABA-mediated inhibition at Minimum Alveolar Concentration (MAC)
GABAA receptor o Median concentration that results in immobility in
Both inhaled & IV with sedative-hypnotic properties 50% of patients when exposed to a noxious
DIRECTLY activate GABAA receptors stimulus
o LOW concentrations: facilitate the action of GABA o Surrogate measure of the anesthetic requirement
to INCREASE CHLORIDE ion flux o MAC value >100% for Nitrous Oxide:
Benzodiazepines (lack general anesthetic properties Least potent
diazepam, lorazepam) Must be supplemented with other agents
o Facilitate GABA action but have NO direct actions to achieve full surgical anesthesia
on GABAA receptors even at HIGH concentrations o A dose of 1 MAC of any anesthetic prevents
in the absence of GABA movement in response to surgical incision in 50%
of patients
Ser270 & Ala291 critical for the enhancement of GABAA
o Individual patients may require 0.5-1.5 MAC
receptor function by volatile anesthetics
o MAC values DECREASE in elderly patients & with
KETAMINE
HYPOthermia
o Unique dissociate anesthetic with analgesic
Not affected greatly by sex, height,
properties
weight
o Does not produce its effects vial facilitation of
o Chronic use of centrally active drugs, alcohol abuse
GABAA receptor functions
& pregnancy INCREASE the anesthetic requirement
o Its CNS activity appears to be related to
o IV drugs (opioid, sympatholytics, sedative-
antagonism of the action of the GLUTAMIC ACID
hypnotics) administered as adjuvant to the volatile
(excitatory NT) on the N-methyl-D-aspartate
anesthetics, MAC is DECREASED in a dose-related
channel receptor
fashion
Inspired concentration should be
2. MEMBRANE HYPERPOLARIZATION (inhibitory) via
DECREASED
activation of POTASSIUM channels
IV anesthetics produce similar dose-dependent continuum of
o Linked to NT (Ach, dopa, NE, Serotonin)
CNS depression
o Inhaled anesthetics DECREASE the duration of
o LOW concentration produce anxiolytic & light
opening NICOTINIC receptor-activated cation
levels of sedation
channels (action that DECREASES the excitatory
o INCREASED produce a progressively
effects of Ach at cholinergic synapses)
INCREASING DEPTH Of sedation
o Most inhaled anesthetics INHIBIT nicotinic Ach
receptor isoforms (4 subunit)
ORGAN SYSTEM EFFECTS of INHALED ANESTHETICS
3. Strychnine-sensitive GLYCINE receptor A. CARDIOVASCULAR
o Another ligand-gated ion channel that may Decrease MAP
function as a target for inhaled anesthetics o Halothane
o Can elicit channel opening directly & independently o Desflurane
of their facilitatory effects on NT binding o Enflurane
o Sevoflurane
Neurons in the SUBSTANTIA GELATINOSA of the DORSAL o Isoflurane
horn of the spinal cord very sensitive to even LOW Halothane & Isoflurane
concentrations of anesthetic drugs o Reduced arterial pressure caused by reduction in
Interrupts sensory transmission in the spinothalamic tract CO
(including nociceptive stimuli) Isoflurane, Desflurane, Sevoflurane
Neurons in the respiratory & vasomotor centers of the o Depressant effect on arterial pressure decrease in
medulla INSENSITIVE to the depressant effects of general systemic vascular resistance with minimal effect on
anesthetics CO
Page | 7 jhojho terrobias.2016
Change in HR C. BRAIN
o Directly altering rate of sinus node depolarization Decrease metabolic rate of the brain
o Indirectly shifting the balance of ANS activity More soluble volatile agents increase cerebral blood
BRADYCARDIA Halothane flow (decrease cerebral vascular resistance)
o Direct vagal stimulation Increase cerebral blood flow
Increase HR o Undesirable to patient with increase ICP (brain
o Isoflurane tumor or head injury)
o Desflurane Volatile anesthetic-induced increases in cerebral blood
Transient sympathetic activation with flow increase cerebral blood volume = increase ICP
elevation of catecholamine levels increase Nitrous oxide
HR & BP o Least likely to increase cerebral blood flow
All inhaled anesthetics tend to increase Right atrial LOW concentrations all halogenated agents have
pressure (dose-related) depression of myocardial similar effects on cerebral blood flow
function HIGH concentrations increase cerebral blood flow is
GREATER myocardial depressant effects LESS with less soluble ages (desflurane & sevoflurane)
o Enflurane
o Halothane D. KIDNEY
Depress the myocardium (concentration-dependent) Decrease GFR & renal blood flow
o Nitrous oxide Increase filtration fraction
o Combination with potent inhaled (volatile)
anesthetics minimize cardiac depressant effects E. LIVER
(anesthetic-sparing effect) Concentration-dependent decrease in hepatic blood
Factors that influence cardiovascular effects of inhaled flow (15%-45% below the preinduction value)
anesthetics
o Surgical stimulation F. UTERINE SMOOTH MUSCLE
o Intravascular volume status Nitrous oxide
o Ventilator status o Little effect on uterine musculature
o Duration of anesthesia Halogenated anesthetics
Hypercapnia releases catecholamines o Potent uterine muscle relaxants
o Attenuate the decrease after 5 hours of anesthesia o Concentration-dependent fashion
Concomitant use of blockers reduces adaptive o Useful: intrauterine fetal manipulation or manual
effect extraction of a retained placenta
Halothane & Isoflurane But can lead to intrauterine bleeding
o Sensitize the myocardium to circulating
catecholamines TOXICITY
Ventricular arrhythmias A. HEPATOTOXICITY (Halothane)
o Patients with cardiac disease given with
Postoperative hepatic dysfunction associated with
sympathomimetic drugs or high circulating levels of
o Blood transfusions
endogenous catecholamines (anxious patients, use
o Hypovolemic shock
of epi-containing local anesthetics, inadequate
o Other surgical stresses
intraoperative anesthesia/analgesia, with
Obese patients
pheochromocytoma)
o Most susceptible especially when exposed more
than once in a short period of time
B. RESPIRATORY
In animals: formation of reactive metabolites that either
All inhaled anesthetics (except nitrous oxide)
cause direct hepatocellular damage or initiate immune-
o Dose-dependent decrease in tidal volume &
mediated response
increase in respiratory rate (decrease in minute
TFA (trifluoroacetylated proteins) during
volume)
biotransformation
All volatile anesthetics respiratory depressant
Isoflurane & enflurane most depressant
B. NEPHROTOXICITY
Volatile anesthetics
Metabolism of Methoxyflurane, Enflurane, Sevoflurane
o Increase apneic threshold
= formation of fluoride ions
o Decrease ventilator response to hypoxia
Methoxyflurane and Enflurane
Ventilator depressant effects of inhaled anesthetics
o Metabolized in part by renal enzymes generating
counteracted by surgical stimulation
fluoride ions intrarenally
Depress mucociliary function in airway
Sevoflurane degradation by carbon dioxide
Prolonged anesthesia pooling of mucus = atelectasis absorbents in anesthesia machines = formation of
& postoperative respiratory infection haloalkene, compound A (metabolized by renal -lyase
Halothane & sevoflurane bronchodilation to form thoacylhalide = proximal tubular necrosis)
o Induction agents of choice (airway problems Renal dysfunction (methoxyflurane) caused by
asthma, COPD, bronchitis) inorganic fluoride released during the extensive
metabolism of this anesthetic by hepatic & renal
enzymes
Page | 8 jhojho terrobias.2016
C. MALIGNANT HYPERTHERMIA BARBITURATES
Autosomal dominant genetic disorder of skeletal muscle
Thiopental most commonly used
that occurs in susceptible individual undergoing general
Thiamylal identical to thiopental
anesthesia with volatile agents & muscle relaxants
THIOPENTAL
(succinylcholine)
o IV bolus injection rapidly crosses BBB
Rapid onset of tachycardia & hypertension
o Rapidly diffuses out of the brain
Severe muscle rigidity
o Redistributed to muscle & fat
Hyperthermia
o Single dose brief period of unconsciousness
Hyperkalemia o Metabolized at the rate of only 12-16% per hour
Acid-base imbalance with acidosis that follows exposure o Less than 1% excreted unchanged by the kidney
to 1 or more of the trigerring agents o LARGE doses: dose-dependent DECREASES in
Increase in free calcium concentration in skeletal muscle arterial BP, SV, CO
cells o Potent respiratory depressant = transient apnea &
TREATMENT: lowering sensitivity of medullary respiratory center
o Dantrolene (to reduce calcium release for the to CO2
sarcoplasmic reticulum) METHOHEXITAL
o Appropriate measures to reduce body o Shorter-acting
temperature o Rapid elimination
o Restore electrolyte and acid-base balance o Can cause central excitatory activity (myoclonus)
o Useful for neurosurgical procedures involving
D. CHRONIC TOXICITY ablation of seizure foci
a. Mutagenicity o Drug of choice: undergoing ECT
NEITHER mutagens nor carcinogens o For short ambulatory procedures
Plasma:brain equilibrium occurs rapidly (<1min) high lipid
solubility
b. Effects on reproductive organs cerebral blood flow but less than O2 consumption
Risk of abortion higher in pregnant ICP & blood volume are NOT increased: THIOPENTAL
patients who underwent anesthesia & desirable drug for patient w/ cerebral swelling (head trauma,
surgery not related to pregnancy brain tumors)
c. Hematotoxicity hepatic blood flow & GFR
Nitrous oxide Prolonged exposure Produce no AE on hepatic or renal function
DECREASES methionine synthase activity
Can exacerbate acute intermittent porphyria (inducing
= MEGALOBLASTIC anemia
production of hepatic -aminolevulinic acid (ALA) synthase)
CLINICAL USE of INHALED ANESTHETICS BENZODIAZEPINES
Volatile anesthetics rarely used alone for induction &
maintenance except in children Diazepam, lorazepam, midazolam
o Preanesthetic medication and adjuvants during
Combined with IV agents (balanced anesthesia technique)
surgical procedures under local anesthesia
Desflurane & Sevoflurane low blood:gas coefficient (more
Drug of choice: PREMEDICATION
rapid recovery and fewer postoperative adverse effect)
Diazepam & lorazepam not water soluble
o IV use needs non-aqueous vehicles (causes pain
and local irritation)
INTRAVENOUS ANESTHETICS Midazolam water-soluble, benzodiazepine of choice for
parenteral administration
(thiopental, methohexital, etomidate, ketamine, propfol) o More rapid onset
o Shorter elimination HL (2-4hours)
Most IV anesthetics lack antinociceptive (analgesic) Slower onset of CNS depressant effects
properties Reach plateau @ a depth of sedation that is inadequate for
Potency is adequate for short superficial surgical procedures surgical anesthesia
when combined with Nitrous oxide or local anesthetics or LARGE doses prolongs the post-anesthetic recovery
both period and can produce a high incidence of anterograde
Adjunctive use of potent opioids: amnesia
o Improved cardiovascular stability FLUMAZENIL (antagonist) to accelerate recovery
o Enhanced sedation o Multiple dosing to prevent recurrence of the CNS
o Perioperative analgesia depressant effects
o Enhance ventilator depressant effects
o Increase postop emesis
Benzodiazepines
o Provide anxiolysis, sedation, amnesia as part of
inhalational, IV or balanced
o Slower onset
o Slower recovery
Page | 9 jhojho terrobias.2016
OPIOID ANALGESICS
FOSPROPOFOL water-soluble prodrug of propofol
HIGH doses have been used in combination with LARGE
o May ameliorate some of the problems associated
doses of BENZO to achieve a general anesthetic state
with propofol
(cardiac surgery or other major surgery)
REMIFENTANIL potent & extremely short-acting to
minimize residual ventilator depression ETOMIDATE
HIGH doses chest wall (& laryngeal) rigidity; acute Carboxylated imidazole
tolerance, postoperative morbidity & mortality after Limited cardiovascular reserve
cardiac surgery Major advantage: minimal cardiovascular & respiratory
LOWER doses of FENTANYL & SULFENTANIL depression
o used as adjunct to both IV & inhaled anesthetics to Produces a rapid loss of consciousness with minimal
provide perioperative analgesia hypotension even in elderly patients with poor
ALFENTANIL & REMIFENTANIL cardiovascular reserve
o Shorter-acting HR unchanged
o Co-induction agents with IV sedative-hypnotics Apnea low
anesthetics No analgesic effects
o Rapid onset of action Coadministration of opioid analgesics is required to
REMIFENTANIL decrease cardiac responses during tracheal intubation &
o Rapidly metabolized by esterases in the blood & lessen spontaneous muscle movements
muscle tissues Initial dose recovery is less rapid compared with propofol
o Does not interfere with the clearance of other Distribution is rapid
compounds metabolized by plasma cholinesterase Extensively metabolized in the liver & plasma to inactive
(esmolol, mivacurium, succinylcholine) metabolites
Can be administered @ LOW doses: 2% excreted unchanged in the urine
o Epidural & subarachnoid (spinal) routes to produce Pain on injection
postop analgesia Myoclonic activity
FENTANYL & DROPERIDOL (butyophenone related to Postoperative nausea & vomiting
haloperidol) = analgesia & amnesia and combined with Adrenocortical suppression via inhibitory effects on
Nitrous Oxide provide a state referred to as steriodogenesis with decreased plasma levels of cortisol after
NEUROLEPTANESTHESIA single dose
Prolonged infusion in critically ill patients hypotension,
PROPOFOL electrolyte imbalance, oliguria (adrenal suppressive effects)
(2,6 diisopropylphenol)
Onset same as barbiturates KETAMINE
Recovery is more rapid 2 isomers (S(+) and R(-) ketamine)
Reduced postop nausea & vomiting & a sense of well-being Dissociative anesthetic state
Used for both induction & maintenance of anesthesia o Catatonia
Agent of choice: AMBULATORY surgery o Amnesia
Monitored anesthesia care technique & in diagnostic suites o Analgesia
for procedural sedation o With or without loss of consciousness (hypnosis)
Effective in producing prolonged sedation in critical care Arylcyclohexylamine related to phencyclidine (PCP)
settings MOA: blockade of the membrane effects of the excitatory NT
Can lead to delayed arousal prolonged use GLUTAMIC acid @ the NMDA receptor subtype
Prolonged use of HIGH-dose propofol infusions for sedation Highly lipophilic
of critically ill young children = severe acidosis in presence of Rapidly distributed into well-perfused organs (brain, liver,
respiratory infections & neurologic sequelae upon kidney)
withdrawal Urinary & biliary excretion
Distribution HL: 2-8 minutes Only IV anesthetic that possess both anesthetic & analgesic
Redistribution HL: 30-60minutes properties
Rapidly metabolized in the liver (10x faster than thiopental) Ability to produce dose-related cardiovascular stimulation
Excreted in the urine as glucuronide & sulfide conjugates w/ HR, Arterial BP, CO
less than 1% of parent drug excreted unchanged Peak: 2-4 minutes after IV bolus injection
Produces a dose-related depression of central ventilator Slowly decline to normal values over the next 10-20mins
drive & transient apnea Cardiovascular effect: stimulating the central sympathetic
Marked decrease in BP during induction of anesthesia nervous system
through decreased peripheral arterial resistance and o Inhibiting reuptake of NE @ sympathetic nerve
venodilation terminals
Direct negative inotropic effect in plasma epi & NE after IV bolus as early as 2 minutes
Pain @ the site of injection most common AE of bolus cerebral blood flow, oxygen consumption, ICP
administration Potentially dangerous: ICP
Admixture or pretreatment with LIDOCAINE (20-50mg) RR
most effective approach to minimize the pain on injection
Page | 10 jhojho terrobias.2016
Upper airway muscle tone is well maintained and airway Intercostal (highest)
reflexes are usually preserved Caudal
Postop disorientation, sensory & perceptual illusions, vivid Epidural
dreams (EMERGENCE PHENOMENA) Brachial plexus
Diazepam, Propofol given before admin of ketamine Sciatic nerve
o Reduces incidence of these AE EPINEPHRINE (vasoconstrictor)
Useful: poor-risk geriatric patient o Reduce systemic absorption of local anesthetics
o High-risk patients in cariogenic or septic shock (decreasing blood flow)
(cardiostimulatory properties) o Important with intermediate or short durations of
LOW doses: for outpatient anesthesia in combination with action
propofol (monitored anesthetic technique) & children o Procaine, lidocaine, mepivacaine
undergoing painful procedures o Spinal anesthesia act directly on the cord to
S (+) isomer possesses psychotomimetic side effects both enhance and prolong local anesthetic
induced spinal anesthesia
2 adrenoceptor inhibits release of
substance P
LOCAL ANESTHESIA reduce sensory neuron firing
Clonidine & dexmedetomidine prolong local anesthetic
Nociception pain awareness effect in subarachnoid space and on peripheral nerves
o Mediated by nerve ending receptors in peripheral Epinephrine combination of reduced systemic absorption,
tissues enhanced local neuronal anesthetic uptake, 2 receptor
o Transmitted to the CNS by primary afferent fibers activation
o Relayed by secondary afferent fibers to the brain o Prolonging local anesthetic effect up to 50%
Reversibly block impulse conduction Vasoconstrictors
SODIUM channels primary means of action potential o Less effective in prolonging anesthetic action of
generation bupivacaine and ropicavaine
Block pain sensation from specific areas of the body More lipid-soluble, long-acting
(sympathetic vasoconstrictor impulse) Highly tissue bound
st
Cocaine 1 local anesthetic Cocaine
o High surface (topical) activity
CHEMISTRY o Intrinsic sympathomimetic properties
Lipophilic group (aromatic ring)
Ester links more prone to hydrolysis (shorter duration of DISTRIBUTION
action) Widely distributed after IV bolus administration
Weak bases Sequestration in lipophilic storage sites (fats)
Usually made available as salts to increase solubility and Initial rapid distribution brain, liver kidney, heart
stability Slower distribution phase muscle & GIT
In the body: uncharged base or cation
Cationic form most active form at the receptor site METABOLISM & EXCRETION
because it cannot readily exit from closed channels Converted in the liver (amide type) or plasma (ester type)
Uncharged form rapid penetration of biologic membranes water-soluble metabolites
Less effective when injected into infected (ACIDIC) tissues Excreted in the urine
smaller percentage of local anesthetic is nonionized & Acidification of urine
available for diffusion across the membrane in an o Promotes ionization of the tertiary amine base to
environment with low extracellular pH more soluble water charged form = rapid
elimination
ESTER TYPE
PharmacoKINETICS o Hydrolyzed very rapidly in the blood by
Usually administered by injection into dermis and soft tissues butyrycholinesterase (pseudocholinesterase) to
around nerves inactive metabolites
ABSORPTION o PROCAINE & CHLOROPROCAINE
Factors in Systemic absorption: Very short plasma HL (<1min)
o Dosage AMIDE TYPE
o Site o Hydrolyzed by liver cytochrome P450
o Drug-tissue binding o Prilocaine (fastest) > lidocaine > mepivacaine >
o Local tissue blood flow ropicavaine = bupivacaine & levobupivacaine
o Use of vasoconstrictors (epi) (slowest)
o Physiochemical properties o Toxicity to patients with hepatic disorder
More rapid absorption Decreased hepatic elimination in reduced hepatic blood flow
o Application to a highly vascular area (tracheal
mucosa or tissue surrounding intercostal nerves)
Block of large nerves
o Maximum blood levels decrease according to the
site of administration
Page | 11 jhojho terrobias.2016
PharmacoDYNAMICS
MECHANISM of ACTION STRUCTURE-ACTIVITY CHARACTERISTICS of LOCAL ANESTHETICS
Blockade of voltage-gated SODIUM channels Smaller & more highly lipophilic = FASTER rate of interaction
o Depolarization: Na close (inactivate); K open with SODIUM channel receptor
o Outward flow of K: repolarizes membrane Lidocaine, Procaine, Mepivacaine
Disruption of SODIUM channel function: o More water soluble
o Biologic toxins: Batrachotoxin, aconitine, Tetracaine, Bupivacaine, Ropivacaine
veratridine, scorpion venoms o Less water soluble
Bind to receptors and prevent activation o More potent
Prolonged influx of Na depolarizing o Longer durations
membrane o Bind more extensively to proteins and can be
o Marine toxins: tetrodotoxin & saxitoxin displaced from these binding sites by other
Block Na channels by binding to the protein-bound drugs
channel receptors near the extracellular
surface OTHER ACTION on NERVES
Resemble local anesthetics Not limited to the desired loss of sensation from sites of
o TTX-resistant neurons noxious stimuli
Responsible for pain transmission Spinal anesthesia
Primary targets for local anesthetics in o Motor paralysis may impair respiratory activity
producing spinal (subarachnoid) o Residual autonomic nerve blockade can lead to
anesthesia hypotension, urinary retention
Local anesthetics bind to receptors near the INTRAcellular Direct application to the nerve root
end of the SODIUM channel and block the channel in a time o Smaller B & C fibers are blocked first
and voltage-dependent fashion o Motor function blocked last
INCREASE concentration
o Increase threshold for excitation 1. Effect on fiber DIAMETER
o Impulse conduction slows Block small fibers distance can passively
o Rate of rise of the action potential declines propagate an electrical impulse is shorter
st
o Action potential amplitude decreases Small-diameter fibers 1 to fail to conduct
o Ability to generate an action potential completely electrical impulses
abolished Myelinated nerves atleast 2 & 3 successive
Myelinated fibers critical length (2-3 nodes) nodes must be blocked
Blockade is VOLTAGE and TIME dependent Preganglionic B fibers are blocked before the
o Low affinity for local anesthetics smaller unmyelinated C fibers
Channels in rested state 2. Effect of Firing FREQUENCY
Predominate at more negative Blockade is more marked at HIGHER frequencies of
membrane potential depolarization
o Higher affinity Sensory (pain) fibers have a high firing rate and
Activated (open state) long AP duration
Inactivated channels Motor fibers fire @ a slower rate and have shorter
Predominate at more positive membrane AP duration
potential Type A delta & C fibers smaller-diameter fibers
o Effect of given drug concentration is more marked that participate in high-frequency pain
in rapidly firing axons transmission
Refractory period LENGTHENED o Fibers are blocked earlier and with lower
Nerve conducts fewer electrical impulses concentrations
ELEVATED extracellular CALCIUM 3. Effect of Fiber POSITION in the Nerve Bundle
o Partially antagonizes action of local anesthetics Large nerve trunks
st
o Calcium-induced increase in the surface potential o Fibers located circumferentially 1 to
on the membrane be exposed
INCREASE in extracellular POTASSIUM Extremities
o Depolarize the membrane potential o Proximal sensory fibers outer portion
o Favor inactivated state of the nerve trunk
o Enhancing effect of local anesthetics o Distal sensory innervation central core
SPINAL ANESTHESIA of the nerve
st
o Local anesthetics can inhibit transmission via: Sensory analgesia 1 develop PROXIMALLY
SUBSTANCE P (neurokinin 1) 4. Effects on OTHER EXCITABLE Membranes
NMDA receptors Weak direct NM blocking effects
AMPA receptors Widely used as antiarrhythmic agents at
o Contribute to the analgesia (subarachnoid concentrations LOWER Than those required to
administration) produce nerve block
Block other ion channels
o Nicotinic acetylcholine channels (spinal cord)
Page | 12 jhojho terrobias.2016
CLINICAL PHARMACOLOGY of LOCAL ANESTHETICS Systemic local anesthetic drugs
Usual Routes of Administration o Adjuvants to the combination of TCA
o Topical (amitriptyline) & anticonvulsants (carbamazepine)
o Injection in the peripheral nerve ending (perineural who fail to respond to the combination of
infiltration) antidepressant & anticonvulsant
o Major nerve trunks (blocks)
o Injection into the epidural or subarachnoid spaces TOXICITY
surrounding spinal cord CNS
o IV regional anesthesia (BIER BLOCK) short surgical A. CNS toxicity
procedures involving upper &/ lower extremities Local anesthetics have the ability to produce in HIGH
o Local anesthetic infiltration of autonomic sympathetic plasma concentrations
fibers evaluate role of sympathetic tone (peripheral o Sleepiness
vasospastic disorders) o Light-headedness
o Injection in trigger points diagnostic & therapeutic o Visual & auditory distrubances
purposes (recurrent pain tactile stimulation) o Restlessness
SHORT-acting EARLY symptom of toxicity
o Procaine o Circumoral & tongue numbness
o Chloroprocaine o Metallic taste
INTERMEDIATE HIGHER concentrations
o Lidocaine o Nystagmus
o Mepivacaine o Muscular twitching
o Prilocaine When large doses are required:
LONG-Acting o Premedication of parenteral BENZODIAZEPINE
o Tetracaine (diazepam/midazolam)
o Bupivacaine SEIZURE
o Levobupivacaine o Hyperoxemia beneficial after onset of seizure
o Ropivacaine o Hypercapnia & acidosis may lower the seizure
Short & intermediate acting can be PROLONGED by threshold (hyperventilation)
increasing dose or adding a vasoconstrictor agent Increases blood pH
(EPINEPHRINE or Phenylephrine) Lowers extracellular potassium
o Slows the removal of local anesthesia Hyperpolarizes transmembrane potential
o Decreases the blood level & probability of Favors resting state of Na channels
cardiovascular & CNS toxicity Decreased local anesthetic toxicity
Onset can be ACCELERATED by adding SODIUM o Seizure-induced:
BICARBONATE (1-2ml) TX: IV anesthetic drugs
o Maximizes amount of drug in more lipid-soluble (thiopental, propofol,
(unionized) form) midazolam)
Repeated injections of local anesthetics = loss of Muscular manifestation TX:
effectiveness (ex. Tachyphylaxis) due to extracellular acidosis succinylcholine
o Deplete buffering capacity B. COCAINE
o Ensuing acidosis increases the extracellular cationic Can produce severe cardiovascular toxicity
form HPN, arrhythmias, acute myocardial failure
o Diffuses poorly = tachyphylaxis
o Common in CSF NEUROTOXICITY
Pregnancy HIGH concentrations
o Increase susceptibility to toxicity o Direct neural toxicity
o Epidural Bupivacaine cardiac arrest Chloroprocaine, Lidocaine
Topical local anesthesia o More neurotoxic when used for spinal anesthesia
o Requires rapid penetration across the skin or TRANSIENT RADICULAR IRRITATION
mucosa (neuropathic symptoms)
o Limited tendency to diffuse away from the site of o Pooling of high concentrations of local anesthetic in
application the cauda equina region
Cocaine
o Excellent penetration CARDIOVASCULAR
o Local vasoconstrictor Direct effects on cardiac and smooth muscle membranes
o Used for ENT procedures Indirect effects on autonomic nervous system
Local anesthetics have membrane-stabilizing effects (both Blockade of Na channels
parenteral & oral) o Depress cardiac pacemaker activity, excitability,
o Treat patients with neuropathic pain syndromes conduction
Involved uncontrolled, rapid, sensory, Except Cocaine
fiber firing o Can depress myocardial contractility,
o Produce direct arteriolar dilation = hypotension
Page | 13 jhojho terrobias.2016
COCAINE
o Blockade of NE reuptake= vasoconstriction & HPN
o Cardiac arrhythmias
Bupivacaine
o More cardiotoxic
o Bupivacaine-induced blockade of Na channels is
potentiated by long AP duration of cardiac cells
compared with nerve fibers
ECG: slow idioventricular rhythm with
broad QRS complexes
o Propofol can be useful in resuscitation
HEMATOLOGIC
Prilocaine (large doses)
o Accumulation of metabolite o-toluidine (oxidizing
agent capable of converting hemoglobin to
methemoglobin)
o Sufficient methemoglobin:
Cyanotic
Blood chocolate-colored
o Elevated methemoglobinemia
Decompensation in patients with
preexisting cardiac or pulmonary disease
TX: IV methylene blue or ascorbic acid
ALLERGIC REACTION
Ester type metabolized to p-aminobenzoic acid
o Responsible for allergic reactions
Page | 14 jhojho terrobias.2016
También podría gustarte
- Minerals SummaryDocumento2 páginasMinerals Summarymiguel cuevasAún no hay calificaciones
- Surgical Pathology Trans No 7. The LIVER DR ROXAS by MCD Recoverd 1Documento14 páginasSurgical Pathology Trans No 7. The LIVER DR ROXAS by MCD Recoverd 1miguel cuevasAún no hay calificaciones
- Vitamins Notes PDFDocumento3 páginasVitamins Notes PDFmiguel cuevas100% (1)
- Pathology Final Practical ExaminationDocumento40 páginasPathology Final Practical Examinationmiguel cuevasAún no hay calificaciones
- Male PhysiologyDocumento2 páginasMale Physiologymiguel cuevasAún no hay calificaciones
- Cytogenetics Disorders PDFDocumento7 páginasCytogenetics Disorders PDFmiguel cuevasAún no hay calificaciones
- Sex Determination and DifferentiationDocumento3 páginasSex Determination and Differentiationmiguel cuevasAún no hay calificaciones
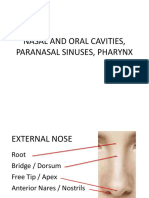
- Nasal and Oral Cavities, Paranasal Sinuses, PharynxDocumento112 páginasNasal and Oral Cavities, Paranasal Sinuses, Pharynxmiguel cuevasAún no hay calificaciones
- Hypolipedemic AgentsDocumento9 páginasHypolipedemic Agentsmiguel cuevasAún no hay calificaciones
- (New) Drugs Used For Gastrointestinal DiseasesDocumento59 páginas(New) Drugs Used For Gastrointestinal Diseasesmiguel cuevasAún no hay calificaciones
- Histo Pracs - Respi and Brain PDFDocumento17 páginasHisto Pracs - Respi and Brain PDFmiguel cuevasAún no hay calificaciones
- 1 Patho5 - Kidney I 2015bDocumento10 páginas1 Patho5 - Kidney I 2015bmiguel cuevasAún no hay calificaciones
- Diseases of The Peripheral Nervous SystemDocumento8 páginasDiseases of The Peripheral Nervous Systemmiguel cuevasAún no hay calificaciones
- First Aid: FM 4-25.11 NTRP 4-02.1 AFMAN 44-163 (I)Documento224 páginasFirst Aid: FM 4-25.11 NTRP 4-02.1 AFMAN 44-163 (I)Giuseppe TrovatoAún no hay calificaciones
- Anti-Viral and Anti-Fungal AgentsDocumento212 páginasAnti-Viral and Anti-Fungal Agentsmiguel cuevas100% (1)
- RBC - Patho BDocumento129 páginasRBC - Patho Bmiguel cuevasAún no hay calificaciones
- Infectious Diseases - BacteriaDocumento9 páginasInfectious Diseases - Bacteriamiguel cuevas100% (1)
- Female Genital Tract Infections and PathologyDocumento16 páginasFemale Genital Tract Infections and Pathologymiguel cuevasAún no hay calificaciones
- SynapseDocumento45 páginasSynapsemiguel cuevasAún no hay calificaciones
- 1.18 MycobacteriumDocumento6 páginas1.18 Mycobacteriummiguel cuevasAún no hay calificaciones
- CHF and Diuretics Trans Limpin MissionDocumento12 páginasCHF and Diuretics Trans Limpin Missionmiguel cuevasAún no hay calificaciones
- Microbiology Lecture 8 & 9 - Systemic & Opportunistic Mycoses (Raroromiki Trans)Documento3 páginasMicrobiology Lecture 8 & 9 - Systemic & Opportunistic Mycoses (Raroromiki Trans)miguel cuevasAún no hay calificaciones
- Glycogenolysis and GlycogenesisDocumento11 páginasGlycogenolysis and Glycogenesismiguel cuevas100% (2)
- Anti-Psychotic NewestDocumento118 páginasAnti-Psychotic Newestmiguel cuevasAún no hay calificaciones
- Breast PathologyDocumento27 páginasBreast Pathologymiguel cuevasAún no hay calificaciones
- He Ma To PoiesisDocumento98 páginasHe Ma To Poiesismiguel cuevasAún no hay calificaciones
- Second Messengers-OLFU-MD 2017Documento66 páginasSecond Messengers-OLFU-MD 2017Melissa SalayogAún no hay calificaciones
- Subcutaneous Mycoses Identification and TreatmentDocumento75 páginasSubcutaneous Mycoses Identification and Treatmentmiguel cuevasAún no hay calificaciones
- Cell Cycle, Apoptosis and CancerDocumento13 páginasCell Cycle, Apoptosis and Cancermiguel cuevas100% (1)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Introduction to Philippine LiteratureDocumento61 páginasIntroduction to Philippine LiteraturealvindadacayAún no hay calificaciones
- Cable Drag ChainDocumento44 páginasCable Drag ChainsunhuynhAún no hay calificaciones
- The Biologic Width: - A Concept in Periodontics and Restorative DentistryDocumento8 páginasThe Biologic Width: - A Concept in Periodontics and Restorative DentistryDrKrishna DasAún no hay calificaciones
- The Message Development Tool - A Case For Effective Operationalization of Messaging in Social Marketing PracticeDocumento17 páginasThe Message Development Tool - A Case For Effective Operationalization of Messaging in Social Marketing PracticesanjayamalakasenevirathneAún no hay calificaciones
- The Syntactic Alignments Across Three-Ar PDFDocumento441 páginasThe Syntactic Alignments Across Three-Ar PDFabiskarAún no hay calificaciones
- Business Research Chapter 1Documento27 páginasBusiness Research Chapter 1Toto H. Ali100% (2)
- PHY3 BJune 2004Documento1 páginaPHY3 BJune 2004api-3726022Aún no hay calificaciones
- SDH PDFDocumento370 páginasSDH PDFClaudia GafencuAún no hay calificaciones
- (Homebrew) ShamanDocumento15 páginas(Homebrew) ShamanVictor Wanderley CorrêaAún no hay calificaciones
- Idioma IV Cycle Q1 Exam (2021-1) - STUDENTS ANSWERDocumento9 páginasIdioma IV Cycle Q1 Exam (2021-1) - STUDENTS ANSWEREdward SlaterAún no hay calificaciones
- 2.3 Temperature Conversions: Chapter 2 Energy and MatterDocumento18 páginas2.3 Temperature Conversions: Chapter 2 Energy and MatterBeverly PamanAún no hay calificaciones
- Three Laws of RoboticsDocumento2 páginasThree Laws of RoboticsBav VAansoqnuaetzAún no hay calificaciones
- Plumbing Layout and SpecificationsDocumento1 páginaPlumbing Layout and SpecificationsLiza P. PaculanangAún no hay calificaciones
- Understanding the Difference Between Positive and Normative EconomicsDocumento21 páginasUnderstanding the Difference Between Positive and Normative EconomicsKevin Fernandez MendioroAún no hay calificaciones
- Expository TextsDocumento2 páginasExpository TextsJodi PeitaAún no hay calificaciones
- Brief History of Gifted and Talented EducationDocumento4 páginasBrief History of Gifted and Talented Educationapi-336040000Aún no hay calificaciones
- Filipino Catholic Wedding Ceremony LiturgyDocumento8 páginasFilipino Catholic Wedding Ceremony LiturgyHoney Joy ChuaAún no hay calificaciones
- Dada and Buddhist Thought - Sung-Won Ko PDFDocumento24 páginasDada and Buddhist Thought - Sung-Won Ko PDFJuan Manuel Gomez GarcíaAún no hay calificaciones
- Advanced Java Thread Lab ExercisesDocumento9 páginasAdvanced Java Thread Lab ExercisesafalonsoAún no hay calificaciones
- Hsse S 005 - Hsse in ProjectsDocumento11 páginasHsse S 005 - Hsse in ProjectsAHMED AMIRAAún no hay calificaciones
- ICT Backup Procedure PolicyDocumento8 páginasICT Backup Procedure PolicySultan BatoorAún no hay calificaciones
- Should A Christian Believer Wear An ANKH?: Luxury Art By: Ketu'Rah GloreDocumento4 páginasShould A Christian Believer Wear An ANKH?: Luxury Art By: Ketu'Rah GloreMyk Twentytwenty NBeyondAún no hay calificaciones
- Climate Change ReactionDocumento2 páginasClimate Change ReactionAngelika CotejoAún no hay calificaciones
- Atestat EnglezaDocumento29 páginasAtestat EnglezaAdrianaAún no hay calificaciones
- Cp-117-Project EngineeringDocumento67 páginasCp-117-Project Engineeringkattabomman100% (1)
- Deepali Bhartiya: TCI Express Limited Gurgaon Assistant Manager Prateek Group Noida Senior ExecutiveDocumento3 páginasDeepali Bhartiya: TCI Express Limited Gurgaon Assistant Manager Prateek Group Noida Senior ExecutiveThe Cultural CommitteeAún no hay calificaciones
- Alcatel 350 User Guide FeaturesDocumento4 páginasAlcatel 350 User Guide FeaturesFilipe CardosoAún no hay calificaciones
- Nestle CompanyDocumento5 páginasNestle CompanymehakAún no hay calificaciones
- Checking battery control unitDocumento3 páginasChecking battery control unitjuanAún no hay calificaciones
- Mahabharata Book 9 Shalya ParvaDocumento413 páginasMahabharata Book 9 Shalya Parvaavacdis1969Aún no hay calificaciones