Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Cardiac Excitation
Cargado por
JayricDepalobosDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Cardiac Excitation
Cargado por
JayricDepalobosCopyright:
Formatos disponibles
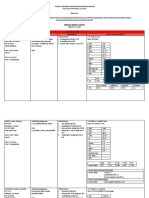
ELEMENTS OF CARDIAC EXCITATION
I) CARDIAC ACTION POTENTIAL
PHAS
E
4
FAST RESPONSE
SLOW RESPONSE
Resting membrane potential
due to outward diffusion of
potassium
Depolarization due to influx
of sodium via fast sodium
channels
Initial repolarization due to
transient efflux of potassium
Plateau due to entry of
calcium
Repolarization due to efflux
of potassium
Slow
depolarization/automaticity
due to inward movement of
sodium (via funny channels)
and Ca (via T channels)
Depolarization caused by
increased inward calcium
current
None
1
2
3
None
Repolarization due to efflux
of potassium
** RESTORATION OF IONIC CONCENTRATIONS via Na-K-ATPse pump
and 3Na-1Ca antiporter
** Check out Figures 16-1 and 16-3, Berne and Levy
CLINICAL CORRELATION:
1. Class Ia antiarrhythmics control heart rate by blocking Na
influx
2. Class II (beta blockers) and Class IV (calcium-channel blockers
like verapamil and diltiazem) antiarrhythmics block calcium
entry
3. With myocardial ischemia or infarction, activity of Na-K-ATPse
pump is impaired
FACTORS AFFECTING CONDUCTION VELOCITY
1. Amplitude of action potential: the greater the action potential
amplitude, the more rapidly is the wave of depolarization
propagated
2. Rate of change of potential during phase 0: the more gradual the
rate of change of potential in phase 0, more time required to reach
threshold, slower conduction velocity
3. resting membrane potential (RMP): the more negative the RMP,
the harder it is to reach threshold, decreases amplitude of action
potential and slope of upstroke, slower conduction velocity
CARDIAC EXCITABILITY
1. Absolute or effective refractory period: another action
potential cannot be generated; prevents sustained, tetanic
contraction of cardiac muscle
2. Relative refractory period (RRP): another action potential can
be generated in presence of stronger stimulus; the later in the
RRP that the fiber is stimulated, the greater the increase in
amplitude of response and slope of upstroke, thus the
propagation velocity also increases
** Check out Figure 16-15
II) CARDIAC CONDUCTION
- one-way conduction: SA node to AV node to AV bundle to right
and left bundle branches to Purkinje fibers
- Spread of depolarization is from endocardium to epicardium,
apex to base
- Automaticity self-excitation; ability to initiate its own beat
- Rhythmicity regularity of pacemaking activity
1. SA node
a. Pacemaker of the heart- controls rate of beating of the
entire heart
b. With greatest automaticity and rhythmicity
2. AV node: Delay in impulse conduction at the AV node to allow
complete emptying of blood from atria to ventricles; with
constant ERP protecting ventricle from excessive firing even in
the presence of premature excitations of atria
3. Ventricular conduction: via bundle branches and Purkinje
fibers; rapid transmission of action potential for synchronized
and immediate contraction of thick-walled ventricles
CLINICAL CORRELATION
1.Sympathetic effect: increased permeability to Na and Ca thus
increasing slope of slow diastolic depolarization
- More positive RMP of SA node
- Increased rate of SA node discharge
- Increased rate of conduction and excitability of A-V node
- Increased force of contraction
2. Parasympathetic effect/ increased vagal activity: increased
permeability to potassium thus hyperpolarizing pacemaker cell
membrane and reducing slope of slow diastolic depolarization
3. Quinidine and procainamide (antiarrhythmics) raise threshold
value to less negative values
** Check out Figure 16-18
ECTOPIC PACEMAKERS
- regions in the heart other than SA node initiating beats
-Mechanisms:
1. Enhanced own rhythmicity
2. Depressed rhythmicity of higher-order pacemakers
3. Block in pathways between ectopic focus and pacemaker
III) ELECTROCARDIOGRAPHY
1. P wave - atrial depolarization
2. PR interval: measures time from onset of atrial activation to onset
of ventricular activation
3. QRS ventricular depolarization
4.QT interval: time it takes for impulse to spread through ventricles
and for repolarization to occur; electrical systole of ventricles
5. T wave ventricular repolarization
6. J point point at which all parts of the ventricles are depolarized
CARDIAC VECTOR
- vector sum of all cardiac electrical activity at any moment
- orientation of vector represents mean electrical axis of the heart in
the frontal plane
AXIS
QRS in LEAD I
QRS in
LEAD II
QRS in
LEAD III
Normal axis ( -30 to
+100)
Left axis deviation (more
negative than -30)
Right axis deviation
(more positive than
+100)
CLINICAL CORRELATION: Ventricular hypertrophy shifts the axis
towards the hypertrophied side
IV) ARRHYTHMIAS
Arrhythymia
Sinus bradycardia
Pathophysiology
decreased SA node firing
Sinus tachycardia
increased SA node firing
First Degree AV
block
Second-degree AV
block
prolonged PR interval
Third degree AV
block/complete
heart block
Premature
depolarizations
(atrial/ventricular)
Fibrillation (Atrial
atria are depolarized at a high rate but only a
fraction of the atrial impulses are conducted to
ventricles; protects ventricles from excessive
contraction
none of the atrial impulses reaches ventricle;
atrial and ventricular rhythms are entirely
independent
excitation occurs at some ectopic focus
reentry phenomenon; premature impulse
or ventricular)
arrives during vulnerable period of cardiac
cycle ( downslope of T wave); during this
period, excitability of cardiac cells varies
( some in ERP, others fully recovered, others
able to conduct impulses). As region of cardiac
cells becomes excitable again, it is ultimately
reentered by one of the wave fronts travelling
around chamber, hence process is selfsustaining
V) CARDIAC CYCLE
Ventricular Filling
1. Rapid ventricular filling: AV valves open due to higher pressures
in atria; ventricular volumes start to increase rapidly
2. Diastasis or reduced ventricular filling: reduced ventricular filling
since increasing volume in ventricles results to equilibrating
pressures in atria and ventricles
3. Atrial systole: ventricular pressures start to increase greater than
atrial pressures, thus atria have to contract to empty remaining
blood in atria into ventricles
Isovolumic Contraction
- Increasing ventricular pressure
- Closure of A-V valves
- Tension is increasing but there is no emptying (WHY???)
- Ventricular volume remains constant (isovolumic, same volume)
Period of Ejection
- LV pressure is at its maximum
- Semilunar valves open
- Blood pours out of ventricles
Isovolumic Relaxation
- Decreasing intraventricular pressure
- Increased pressure in large arteries
- Closure of semilunar valves
- Ventricles relax, no change in ventricular volume
- Atria start to fill with blood
Left atrial pressure curve
1. a wave rise in pressure caused by atrial contraction
2. c wave - caused by impact of common carotid artery with
adjacent jugular vein and to some extent by abrupt closure of
the tricuspid valve in early ventricular systole
3. v wave rise in pressure associated with atrial filling
** Check out Figure 16-40
**Check out the following websites for Cardiac Cycle animations:
1.
http://highered.mcgrawhill.com/sites/0072495855/student_view0/ch
apter22/animation_the_cardiac_cycle_quiz_1_.html
2. http://anatimation.com/cardiac/intro.html
3. http://library.med.utah.edu/kw/pharm/hyper_heart1.html
DETERMINANTS OF Myocardial Contractility
1. Preload force that stretches relaxed muscle fibers
2. Afterload force against which contracting muscle must
overcome
*INDEX OF CONTRACTILITY: Ejection fraction
También podría gustarte
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Computer ModuleDocumento8 páginasComputer ModuleJayricDepalobosAún no hay calificaciones
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- FWD: Schedule Change AdvisoryDocumento2 páginasFWD: Schedule Change AdvisoryJayricDepalobosAún no hay calificaciones
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The LightDocumento2 páginasThe LightJayricDepalobosAún no hay calificaciones
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- Bill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341Documento1 páginaBill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341JayricDepalobosAún no hay calificaciones
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- FWD: Schedule Change AdvisoryDocumento2 páginasFWD: Schedule Change AdvisoryJayricDepalobosAún no hay calificaciones
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- The Church Must Stand TogetherDocumento7 páginasThe Church Must Stand TogetherJayricDepalobosAún no hay calificaciones
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Shipping Confirmation 1264941Documento1 páginaShipping Confirmation 1264941JayricDepalobosAún no hay calificaciones
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocumento13 páginasConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosAún no hay calificaciones
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocumento13 páginasConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosAún no hay calificaciones
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocumento13 páginasConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosAún no hay calificaciones
- Medical Ward 1 Service 2 CensusDocumento13 páginasMedical Ward 1 Service 2 CensusJayricDepalobosAún no hay calificaciones
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- WWW SlidDocumento1 páginaWWW SlidJayricDepalobosAún no hay calificaciones
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- Chapter 01 ChoicesDocumento9 páginasChapter 01 ChoicesJayricDepalobosAún no hay calificaciones
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Medical Ward 1 Service 2 CensusDocumento13 páginasMedical Ward 1 Service 2 CensusJayricDepalobosAún no hay calificaciones
- Acquaintance Party ParticipantsDocumento1 páginaAcquaintance Party ParticipantsJayricDepalobosAún no hay calificaciones
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- CAA Concert ProgramDocumento2 páginasCAA Concert ProgramJayricDepalobosAún no hay calificaciones
- What's in A Birthday?: I. We Can Be Mixed Blessings To OthersDocumento2 páginasWhat's in A Birthday?: I. We Can Be Mixed Blessings To OthersJayricDepalobosAún no hay calificaciones
- Sample Child Dedication ProgramDocumento1 páginaSample Child Dedication ProgramJayricDepalobos100% (2)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- "Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."Documento3 páginas"Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."JayricDepalobosAún no hay calificaciones
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- YHH Strategic Plan 2016-2017Documento5 páginasYHH Strategic Plan 2016-2017JayricDepalobosAún no hay calificaciones
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- Census TemplateDocumento3 páginasCensus TemplateJayricDepalobosAún no hay calificaciones
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Psalm 23 SermonDocumento5 páginasPsalm 23 SermonJayricDepalobosAún no hay calificaciones
- General Anesthesia in Caesarean SectionDocumento7 páginasGeneral Anesthesia in Caesarean SectionJayricDepalobosAún no hay calificaciones
- Thalassemia: Presentor: Don Jayric DepalobosDocumento19 páginasThalassemia: Presentor: Don Jayric DepalobosJayricDepalobosAún no hay calificaciones
- Tally Sheeth Per 10 HouseholdsDocumento14 páginasTally Sheeth Per 10 HouseholdsJayricDepalobosAún no hay calificaciones
- Clinical Pastoral OrientationDocumento3 páginasClinical Pastoral OrientationJayricDepalobos100% (1)
- Teen Parenting Brochure AssignmentDocumento1 páginaTeen Parenting Brochure AssignmentJayricDepalobosAún no hay calificaciones
- Peer Evaluation For Group 5Documento1 páginaPeer Evaluation For Group 5JayricDepalobosAún no hay calificaciones
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- Pneumonia Antibiotics PDFDocumento1 páginaPneumonia Antibiotics PDFRudy KurniawanAún no hay calificaciones
- Tally Sheeth Per 10 HouseholdsDocumento14 páginasTally Sheeth Per 10 HouseholdsJayricDepalobosAún no hay calificaciones
- Complete DentureDocumento57 páginasComplete Denturedr_ahmad_zuhdi100% (3)
- Bleak House - Book ThreeDocumento36 páginasBleak House - Book ThreeNicklaus Adam Rhodes100% (1)
- How Does Global Warming Affect Our Living?Documento19 páginasHow Does Global Warming Affect Our Living?Minahil QaiserAún no hay calificaciones
- 150 Years of PharmacovigilanceDocumento2 páginas150 Years of PharmacovigilanceCarlos José Lacava Fernández100% (1)
- Microbiology With Diseases by Taxonomy 6Th Edition Full ChapterDocumento37 páginasMicrobiology With Diseases by Taxonomy 6Th Edition Full Chapterjoelle.yochum318100% (25)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2102)
- CKD PrognosisDocumento8 páginasCKD PrognosisAlfred YangaoAún no hay calificaciones
- Prune Belly SyndDocumento11 páginasPrune Belly SyndnadiaryAún no hay calificaciones
- MCQ ChoDocumento31 páginasMCQ Choامجد حسين جواد كاظمAún no hay calificaciones
- Grape Growing in TennesseeDocumento28 páginasGrape Growing in TennesseeDbaltAún no hay calificaciones
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Flacourtia IndicaDocumento5 páginasFlacourtia IndicaGiffaria HafizhaAún no hay calificaciones
- Mangosteen ManualDocumento46 páginasMangosteen Manualherow999980% (5)
- Chi Cards 1Documento43 páginasChi Cards 1SwordAceAún no hay calificaciones
- Neuromuscular Blocking AgentsDocumento89 páginasNeuromuscular Blocking Agentslorenzo08Aún no hay calificaciones
- An Overview of Methods Used For Estimation of Time Since Death PDFDocumento12 páginasAn Overview of Methods Used For Estimation of Time Since Death PDFFajar SodiqiAún no hay calificaciones
- Dysrhythmia Advance Content Outline A1 - 2020.1.2Documento3 páginasDysrhythmia Advance Content Outline A1 - 2020.1.2Kimberly Whiteside50% (2)
- WHO International Standards For Drinking Water PDFDocumento204 páginasWHO International Standards For Drinking Water PDFAnonymous G6ceYCzwt100% (1)
- Return Permit For Resident Outside UAEDocumento3 páginasReturn Permit For Resident Outside UAElloyd kampunga100% (1)
- 10.1055s 0039 1688815 - CompressedDocumento15 páginas10.1055s 0039 1688815 - CompressedYolanda Gómez LópezAún no hay calificaciones
- Piriformis Syndrome: The Clinical Syndrome Signs and SymptomsDocumento5 páginasPiriformis Syndrome: The Clinical Syndrome Signs and SymptomsDewi IrfanAún no hay calificaciones
- MenopauseDocumento21 páginasMenopauseDr K AmbareeshaAún no hay calificaciones
- Cardiology UQU 2022Documento29 páginasCardiology UQU 2022Elyas MehdarAún no hay calificaciones
- Blood Pressure ChartDocumento7 páginasBlood Pressure ChartsolomwanAún no hay calificaciones
- Brain Edema XVI - Translate Basic Science Into Clinical Practice by Richard L Applegate, Gang Chen, Hua Feng, John H. ZhangDocumento376 páginasBrain Edema XVI - Translate Basic Science Into Clinical Practice by Richard L Applegate, Gang Chen, Hua Feng, John H. ZhangAjie WitamaAún no hay calificaciones
- REKAPITULASI PASIEN CA PENIS NewDocumento51 páginasREKAPITULASI PASIEN CA PENIS Newagus sukarnaAún no hay calificaciones
- Armstrong 2017 Diabetic Foot Ulcers and Their RecurrenceDocumento11 páginasArmstrong 2017 Diabetic Foot Ulcers and Their Recurrencefebyan yohanesAún no hay calificaciones
- HCM Treatment Italy Ammirati2016Documento13 páginasHCM Treatment Italy Ammirati2016xy manAún no hay calificaciones
- Columbian Exchange Graphic OrganizerDocumento2 páginasColumbian Exchange Graphic Organizerapi-327452561100% (1)
- 2016 PAD ACC+AHA SlidesDocumento74 páginas2016 PAD ACC+AHA SlidesPonpimol Odee BongkeawAún no hay calificaciones
- VECTOR BIOLOGY FOR IRS PROGRAM - Javan Chanda - 2018Documento16 páginasVECTOR BIOLOGY FOR IRS PROGRAM - Javan Chanda - 2018Luo MiyandaAún no hay calificaciones
- MSDS ThievesDocumento11 páginasMSDS ThievesATOMY KESEHATANAún no hay calificaciones
- The Obesity Code: Unlocking the Secrets of Weight LossDe EverandThe Obesity Code: Unlocking the Secrets of Weight LossCalificación: 4 de 5 estrellas4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityCalificación: 4 de 5 estrellas4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAún no hay calificaciones
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeCalificación: 2 de 5 estrellas2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDCalificación: 5 de 5 estrellas5/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionCalificación: 4 de 5 estrellas4/5 (404)