Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Malnutrition and Infection
Cargado por
sobanDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Malnutrition and Infection
Cargado por
sobanCopyright:
Formatos disponibles
DEFENCE AGAINST INFECTION
normally ingested together in food, macronutrient deficiency is
an indicator of likely micronutrient deficiency. The converse may
not be true, however; specific micronutrient deficiencies may arise
despite an adequate proteinenergy intake.
Malnutrition may be defined in several ways, of which weight
loss is the most common. Weight loss may be dynamic (I have lost
6 kg over 2 months), relative (I am 5 kg less than my usual body
weight) or static (I am badly underweight). Static measures are
best related to an absolute scale, but weight must be normalized for
body size before a meaningful comparison may be made, otherwise
small and wasted may be confused. In adults, normalization
is best achieved using BMI (span may be used if height is not
available), which has a normal range of 2025 kg/m2. Degrees of
malnutrition defined by BMI are shown in Figure 2. In children,
weight-for-height/length or height/length-for-age are alternative
indices.
Malnutrition and infection
Derek Macallan
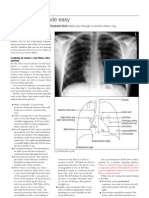
There are two aspects to the interaction between malnutrition and
infection (Figure 1):
the effect of nutritional state on susceptibility to and severity
of infective episodes
the effect of infection on metabolism and nutritional state.
Malnutrition is a major problem worldwide. Children are most
affected (see MEDICINE 31:4, 18), though this contribution focuses
on adults. The extent of malnutrition in hospitalized adult patients
in Western countries is largely unappreciated. In one study, about
40% of a sample of UK hospital patients were undernourished
on admission (body mass index, BMI < 20 kg/m2) and most
patients lost further weight during their stay (mean change
5.4%); weight loss was greatest in those who were initially most
undernourished.
Assessment of nutritional state
Assessment of nutritional state is easily neglected in the acute
medical setting. Appearances may be misleading, particularly
when oedema is present. For example, cushingoid patients may
have marked depletion of lean body tissue but not appear malnourished. Other parameters may be helpful in addition to weight
and BMI.
Anthropometric parameters include skin-fold thickness at
defined sites, muscle circumference and waist:hip ratio. Mid-upper
arm circumference (MUAC) is a useful indicator of malnutrition
that can be used in ill patients (normal MUAC > 23 cm in males,
> 22 cm in females).
Bioelectrical impedance analysis is an easy-to-use bedside test
that predicts the mass of different body compartments from resistance and reactance to the passage of a small alternating electric
current.
Dual-energy X-ray absorptiometry and CT may be used to
measure fat and lean compartments, but are essentially research
tools.
Malnutrition
Defining malnutrition
The term malnutrition refers primarily to deficiency of macronutrients (carbohydrate, protein and lipid), which manifests as
wasting, though it may also refer to specific deficiencies of vitamins
or trace elements. Because macronutrients and micronutrients are
Assessment in children: the most sensitive marker of nutritional
deprivation in children is failure to grow; this is because children
initially conserve energy and protein by slowing growth rather
than using reserves. Specific measures include weight-for-age and
Derek Macallan is Reader and Honorary Consultant in Infectious Diseases
at St Georges Hospital Medical School, London, UK.
Malnutrition and infection
Compromised barrier defences
Impaired cellular immunity
Impaired humoral immunity
Increased risk
Increased severity
Malnutrition
Infection
Negative energy balance
Anorexia
Increased
metabolic rate
Protein catabolism
Acute-phase response
MEDICINE 33:3
14
2005 The Medicine Publishing Company Ltd
DEFENCE AGAINST INFECTION
height-for-age. Severe proteinenergy malnutrition may result in
kwashiorkor with marked oedema.
Nutritional deficiency may turn a relatively mild illness into
a severe disease. In many developing countries, for example,
vitamin A deficiency dramatically increases the morbidity and
mortality caused by measles in children, and in China, Coxsackie
virus infection in children with selenium deficiency leads to severe
endemic juvenile cardiomyopathy (Keshan disease). Conversely,
acute infection can precipitate clinical deficiency in those with
borderline vitamin A status, resulting in visual loss.
Blood tests: measurement of blood nutrient levels is seldom a
good indicator of overall body status in patients with infection. The
main reason is the presence of the acute-phase response, which,
by sequestration of nutrients, may be an adaptive mechanism to
create an internal environment less conducive to the proliferation of invading organisms. For example, the increased levels of
iron-binding proteins and reduced availability of iron seen in the
acute-phase response may inhibit growth of some micro-organisms
with a high requirement for iron (e.g. malaria). In this situation,
improving iron status may exacerbate the pathology and increase
morbidity and mortality. Similarly, the up-regulation of circulating
lipid levels seen in infection may have a nonspecific binding effect
on both bacteria and viruses.
Albumin levels also contribute little to nutritional assessment.
Albumin is a negative acute-phase reactant, production of which
is specifically down-regulated as part of the acute-phase reaction.
Furthermore, albumin concentrations are profoundly affected
by changes in capillary permeability, which are common in
infection.
Effect of infection on nutrition
Chronic severe infection has been recognized for centuries as a
cause of wasting. Infection impinges on nutritional state in three
principal ways anorexia, increased metabolic rate and catabolism of protein.
Anorexia is a common feature of many infective processes and
is probably the most important contributor to the wasting that
accompanies chronic infections such as HIV and tuberculosis. Proinflammatory cytokines are thought to be the primary mediators
of such anorexia and probably act via neuropeptides such as NPY.
Resting (basal) energy expenditure is usually increased by acute
infection, partly as a consequence of fever. However, this increase
in energy expenditure is often more than offset by conservation of
energy as a consequence of reduced activity. Thus, total energy
expenditure may be reduced in sick, inactive patients, and energy
requirements are easily overestimated in such situations. Although
negative energy balance is common, the usual cause is reduced
intake, not increased expenditure.
Clinical assessment tools: several tools are available for clinical assessment of nutritional risk. The British Association for
Parenteral and Enteral Nutrition has recently produced a Malnutrition Screening Tool based largely on BMI.1
Relationship between nutritional state and infection
Protein metabolism: specific changes in protein metabolism occur
in infection. Net protein balance in muscle (the largest protein
reservoir in the body) is shifted towards protein breakdown, and
liberated amino acids are used partly to fuel the acute-phase
response. However, there is a net excess of breakdown over
utilization, resulting in increased nitrogen excretion, which may
exacerbate renal failure. The net effect on muscle is loss of functional tissue, resulting in weakness and fatiguability. This may
be sufficiently severe to compromise muscle groups essential for
respiration, coughing and posture, putting the patient at risk of
further infectious complications.
Malnutrition and susceptibility to infection
There are multiple mechanisms by which malnutrition increases
susceptibility to infection. The barrier functions of skin and mucosa
are the first line of defence against infection and are compromised
by malnutrition. Cellular and humoral immune function are markedly impaired in individuals with energy or protein deficiency.
These effects are more marked at the extremes of age. The perinatal
period is a crucial period when the developing immune system,
particularly the thymus, is susceptible to nutritional deprivation.
Elderly individuals may already have age-related immune dysfunction (immunosenescence) and are at greater risk of both infection
and malnutrition.
As a consequence, malnourished patients experience more
frequent and more severe infective episodes, as has been shown
for postoperative infective complications in malnourished patients
admitted for surgery.
Nutritional management
Macronutrients
The key approach to nutritional support in infection is provision
of adequate but not excessive nutrients. Processing of excess
Levels of malnutrition defined by body mass index
Normal
Marginal
Mild malnutrition
Moderate malnutrition
Severe malnutrition
BMI (kg/m2)
> 20
18.520
1718.5
1617
< 16
MEDICINE 33:3
15
2005 The Medicine Publishing Company Ltd
DEFENCE AGAINST INFECTION
nutrients may use essential substrates, and this may be the reason
why excessive nutritional support (hyperalimentation) can increase
morbidity and mortality in critically ill patients. Excess energy
tends to be accumulated as fat rather than useful lean tissue and
probably contributes little to the clinical outcome. Furthermore,
potent anabolic agents (e.g. growth hormone) increase mortality
in severely ill ICU patients, possibly by redirection of substrate
metabolism towards tissue anabolism and away from the acutephase response.
Inadequate nutrition leads to wasting, however, and such wasting increases morbidity, delays recovery, and predisposes patients
to further infective episodes. Dietary advice may be helpful and has
been the subject of a recent Cochrane review.2 When oral intake is
possible but inadequate, supplements may be helpful in achieving
weight gain or limiting weight loss. Enteral nutrition is the route
of choice whenever possible. In severely ill patients, energy is
usually provided at a rate of 2530 kcal/kg/day. Optimal protein
intakes are probably about 11.5 g/kg/day, though fixed-proportion
enteral feeds are often used, usually giving about 40 g protein per
1000 kcal energy. Protein losses associated with dialysis or drainage of ascites may demand greater protein intakes. Fluid volume,
electrolyte (particularly phosphate) and glycaemic control are also
of paramount importance in severely ill malnourished patients.
In famine situations, severely malnourished adults (BMI
< 13 kg/m2) have a very high mortality rate, primarily as a result
of infection. The presence of oedema, perhaps analogous to
kwashiorkor in children, is a poor prognostic sign, and mortality
in such patients is lower if the initial refeeding diet is relatively
low in protein.
Garrow J S, James W P T, Ralph A. Human nutrition and dietetics.
Edinburgh: Churchill Livingstone, 1999.
Macallan D C. Nutrition and immune function in human
immunodeficiency virus infection. Proc Nutr Socc 1999; 58: 7438.
(Review of interactions between HIV and nutrition, with particular
emphasis on mechanisms of wasting.)
McWhirter J P, Pennington C R. Incidence and recognition of malnutrition
in hospital. BMJJ 1994; 308: 9458.
Management of severe malnutrition: a manual for physicians and other
senior health workers. Geneva: WHO, 1999.
(Primarily focused on children and developing countries.)
Schwenk A, Macallan D C. Tuberculosis, malnutrition and wasting. Curr
Opin Clin Nutr Metab Care 2000; 3: 28591.
Villamor E, Fawzi W W. Vitamin A supplementation: implications for
morbidity and mortality in children. J Infect Dis 2000; 182: (Suppl. 1):
S12233.
Micronutrients
Micronutrients should be considered in all acutely unwell patients
who are unable to maintain adequate intake or are losing weight.
They may be given as part of complete nutritional formulas or
as separate supplements. Some nutrients (e.g. glutamine) may be
conditionally essential; that is, they become a requirement in
conditions of excessive demand. Use of specific nutrient formulations has been proposed for infective illnesses, but there is currently no evidence for this approach. However, future approaches
to nutritional management are likely to include disease-specific
supplementation or foodstuffs (so-called nutriceuticals).
Practice points
Measure weight regularly to predict malnutrition before it
becomes clinically apparent
Include a height measure or estimate to calculate BMI
Use a clinical malnutrition screening tool
Negative energy balance leads to wasting and must be
corrected whenever possible
Avoid excessive nutritional support it may harm rather than
benefit
Blood tests for nutrient status may be misleading in the
presence of infection
REFERENCES
1 British Association for Parenteral and Enteral Nutrition. Malnutrition
screening tool. www.bapen.org.uk/the-must.htm
2 Baldwin C, Parsons T, Logan S. Dietary advice for illness-related
malnutrition in adults. Cochrane Database Syst Revv 2001; 2:
CD002008. www.cochrane.org/cochrane/revsabstr/AB002008.htm
FURTHER READING
Calder P C, Field C J, Gill H S. Nutrition and immune function. Wallingford:
CABI, 2002.
(A comprehensive book on nutrient-immune interactions.)
MEDICINE 33:3
16
2005 The Medicine Publishing Company Ltd
También podría gustarte
- Palliative CareDocumento4 páginasPalliative CaresobanAún no hay calificaciones
- The Immunocompromised Patient Primary ImmunodeficienciesDocumento2 páginasThe Immunocompromised Patient Primary ImmunodeficienciessobanAún no hay calificaciones
- Rome III Diagnostic Criteria FGIDsDocumento14 páginasRome III Diagnostic Criteria FGIDsPutu Reza Sandhya PratamaAún no hay calificaciones
- Vulval PainDocumento3 páginasVulval PainsobanAún no hay calificaciones
- Medicolegal Issues and STIsDocumento3 páginasMedicolegal Issues and STIssobanAún no hay calificaciones
- Gastroenterology and AnaemiaDocumento5 páginasGastroenterology and Anaemiasoban100% (1)
- Urinary Tract ObstructionDocumento3 páginasUrinary Tract ObstructionsobanAún no hay calificaciones
- Acr Omega LyDocumento3 páginasAcr Omega LysobanAún no hay calificaciones
- Antineoplastic SDocumento20 páginasAntineoplastic SsobanAún no hay calificaciones
- Antiphospholipid SyndromeDocumento4 páginasAntiphospholipid SyndromesobanAún no hay calificaciones
- Autonomic & NeuromuscularDocumento20 páginasAutonomic & Neuromuscularzeina32Aún no hay calificaciones
- Adolescent NutritionDocumento1 páginaAdolescent NutritionsobanAún no hay calificaciones
- Disorders of PubertyDocumento2 páginasDisorders of PubertysobanAún no hay calificaciones
- The Wheezing InfantDocumento4 páginasThe Wheezing InfantsobanAún no hay calificaciones
- Cara Membaca Foto Thoraks Yang BaikDocumento2 páginasCara Membaca Foto Thoraks Yang BaikIdi Nagan RayaAún no hay calificaciones
- Neuro DegenerativeDocumento11 páginasNeuro DegenerativesobanAún no hay calificaciones
- Analgesic & AntimigraineDocumento12 páginasAnalgesic & AntimigraineChin ChanAún no hay calificaciones
- Case Scenarios Nutrition Growth and DevelopmentDocumento4 páginasCase Scenarios Nutrition Growth and DevelopmentsobanAún no hay calificaciones
- Neuro DegenerativeDocumento11 páginasNeuro DegenerativesobanAún no hay calificaciones
- What's New in Respiratory DisordersDocumento4 páginasWhat's New in Respiratory DisorderssobanAún no hay calificaciones
- Drugs That Damage The LiverDocumento5 páginasDrugs That Damage The LiversobanAún no hay calificaciones
- Non Epileptic Causes of Loss of ConsciousnessDocumento3 páginasNon Epileptic Causes of Loss of ConsciousnesssobanAún no hay calificaciones
- Haemo Chroma To SisDocumento4 páginasHaemo Chroma To SissobanAún no hay calificaciones
- Contraception: What's New in ..Documento4 páginasContraception: What's New in ..sobanAún no hay calificaciones
- What Is DiabetesDocumento2 páginasWhat Is DiabetessobanAún no hay calificaciones
- AppendixC NutrientChartDocumento5 páginasAppendixC NutrientChartArianne Nicole LabitoriaAún no hay calificaciones
- The Management of Acute Renal FailureDocumento4 páginasThe Management of Acute Renal Failuresoban100% (1)
- Whats New in Asthma and COPDDocumento3 páginasWhats New in Asthma and COPDsobanAún no hay calificaciones
- Renal Disease and PregnancyDocumento4 páginasRenal Disease and PregnancysobanAún no hay calificaciones
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- (15th June - 21st June) Weekly Webinars ScheduleDocumento1 página(15th June - 21st June) Weekly Webinars ScheduleSahil DhamijaAún no hay calificaciones
- Directed Writing and Essays On HealthDocumento8 páginasDirected Writing and Essays On HealthAtiqah AzmiAún no hay calificaciones
- Essential Oils Ancient Medicine-eBook PDFDocumento511 páginasEssential Oils Ancient Medicine-eBook PDFAlina Serban Leahu100% (20)
- Exam Patient Safety AwarenessDocumento5 páginasExam Patient Safety AwarenessidzniAún no hay calificaciones
- FNCPDocumento2 páginasFNCPJaylove CastilloAún no hay calificaciones
- Community & Public HealthDocumento3 páginasCommunity & Public HealthPark GwynethAún no hay calificaciones
- Critical Appraisal Untuk Artikel Terapi Scenario 1Documento7 páginasCritical Appraisal Untuk Artikel Terapi Scenario 1Sumendhe Hayuning SukmaraniAún no hay calificaciones
- Intrauterine Insemination (IUI)Documento21 páginasIntrauterine Insemination (IUI)Chanta MaharjanAún no hay calificaciones
- Gardasil Contract FDA Merck and Norwegian Government2Documento7 páginasGardasil Contract FDA Merck and Norwegian Government2Dustin EstesAún no hay calificaciones
- Covid-19 Crew Travel SafetyDocumento11 páginasCovid-19 Crew Travel SafetyВладимир Швец100% (1)
- Sample FNCP For InfectionDocumento3 páginasSample FNCP For InfectionAnonymous gHwJrRnmAún no hay calificaciones
- WebpdfDocumento461 páginasWebpdfTatiana RoaAún no hay calificaciones
- Pregnancy Nausea and Vomiting GuideDocumento16 páginasPregnancy Nausea and Vomiting Guidezakariah kamalAún no hay calificaciones
- Human Health & DiseaseDocumento58 páginasHuman Health & DiseaseSujay TewaryAún no hay calificaciones
- ICDSDocumento30 páginasICDSMadhu Ranjan100% (1)
- (EPI) 2.06 Community Diagnosis - DR - ZuluetaDocumento4 páginas(EPI) 2.06 Community Diagnosis - DR - ZuluetapasambalyrradjohndarAún no hay calificaciones
- Donning and Doffing Personal Protective Eqquipment (Ppe) : PreparationDocumento2 páginasDonning and Doffing Personal Protective Eqquipment (Ppe) : PreparationPam RuizAún no hay calificaciones
- Guide to Breech Presentation DeliveryDocumento13 páginasGuide to Breech Presentation DeliveryRahmawati Dianing PangestuAún no hay calificaciones
- Risk Assessment Template For Multi-Task Activities: Office Work ExampleDocumento4 páginasRisk Assessment Template For Multi-Task Activities: Office Work ExampleGorack ShirsathAún no hay calificaciones
- Scutchfield and Kecks Principles of Public Health Practice 4th Edition Erwin Solutions ManualDocumento3 páginasScutchfield and Kecks Principles of Public Health Practice 4th Edition Erwin Solutions Manuala710108653Aún no hay calificaciones
- The Relationship Between The Number of People With Immunity Against Covid-19 and Achieving Herd Immunity in Bangkok and The Vicinitiesareaof ThailandDocumento9 páginasThe Relationship Between The Number of People With Immunity Against Covid-19 and Achieving Herd Immunity in Bangkok and The Vicinitiesareaof ThailandIJAR JOURNALAún no hay calificaciones
- PreviewDocumento47 páginasPreviewRosario De La CruzAún no hay calificaciones
- COVID Business Liability BillDocumento42 páginasCOVID Business Liability BillMichelle Rindels100% (1)
- Microbiology of Water by Huzaifa FarooqDocumento16 páginasMicrobiology of Water by Huzaifa FarooqZaifi KhanAún no hay calificaciones
- NSO Level 1 Class 5 Question Paper 2019 Set B Part 11Documento4 páginasNSO Level 1 Class 5 Question Paper 2019 Set B Part 11Anubhuti GhaiAún no hay calificaciones
- Abnormal Labor - ClinicalKeyDocumento32 páginasAbnormal Labor - ClinicalKeyJunior KenAún no hay calificaciones
- VaccinationsDocumento31 páginasVaccinationsحامد يوسفAún no hay calificaciones
- Menstrual Hygiene Among Adolescent Girls Studying.34Documento6 páginasMenstrual Hygiene Among Adolescent Girls Studying.34riniandayaniAún no hay calificaciones
- Kevin Norbury in A Buggy Built For Him As A ChildDocumento6 páginasKevin Norbury in A Buggy Built For Him As A Childvaccine truthAún no hay calificaciones
- Urban HEP in Ethiopia XDocumento19 páginasUrban HEP in Ethiopia Xበተግባር ግዛቸውAún no hay calificaciones