Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Aesthetic Lip Splits
Cargado por
rajtanniruDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Aesthetic Lip Splits
Cargado por
rajtanniruCopyright:
Formatos disponibles
TECHNICAL NOTE
Aesthetic lip splits
J. P. Hayter, E. D. Vaughan, J. S. Brown
Maxillofacial
Unit, Walton Hospital, Liverpool, UK
SUMMARY. Both upper and lower lip splits, usually with osteotomy of the underlying jaw, improve access to
the deep structures of the head and neck. A simple modification to the midline lip split is to incorporate a chevron
in both the peri-oral skin and vermilion margin. The advantages are: accurate wound closure, no straight line
contracture and a broken line of the peri-oral scar. This improves the aesthetic result of the healed lip.
INTRODUCTION
LOWER LIP
The lip splitting incision improves oral access to
pathological conditions of the maxillofacial region.
The lower lip split with mandibulotomy displays the
oral cavity, pharynx and upper cervical spine. The
upper lip split displays the maxilla. If the disarticulated maxilla is pedicled to the cheek flap, the paranasal sinuses, the nasopharynx and the base of skull
become readily accessible.
The final cosmetic result is optimised by restoring
the normal anatomical position of the maxilla and
mandible with stable fixation and careful approximation of the soft tissues. Transfacial approaches
incorporating lip splits attempt to use anatomical
landmarks and good principles of incision design to
hide the resultant scar line.3,4 However, the commonly used straight line incision across the lip skin
and vermilion margin can be the most obvious section
of the final scar, clearly indicating the surgical
approach used.
This paper describes a simple modification to the
design of both upper and lower lip splitting incisions
to improve the aesthetic result of the healed lip.
ROUXITROTTER
MCGREGOR
ROBSON
INCISIONS
Lower lip
1. Roux/Trotter
A midline split of the lower lip and mandible in the
surgical approach to tumours of the anterior tongue
was first described by Roux in 18395 (Fig. I). Trotter6
extended this approach by dividing the tongue in the
midline to expose tumours of the posterior tongue
and pharynx. This midline incision lies in a relaxed
skin tension line4 and minimises injury to the muscles,
vessels and nerves of the lower lip. However, both
contracture of this straight line scar over the lower
lip below the vermilion border together with a
Fig. 1 - Lower
432
lip splitting
incisions.
Aesthetic
depression of the vertical line over the chin prominence may combine to produce an unsightly scar.
lip splits
Upper lip
I. Webrr-Ferguson
The incision Weber described to expose the maxilla
made a midline split of the upper lip to the base of
2. McGregor
McGregor modified the midline lip splitting incision
to follow the outline of the labiomental groove and
chin prominence (Fig. 1). This modification breaks
up the straight line of the scar and attempts to
conceal the incision in the skin crease. However, the
semi-circular incision around the chin prominence
crosses vertical relaxed skin tension lines along much
of its course with the potential to produce a more
noticeable scar. Contracture of the straight midline
scar over the lower lip below the vermilion border
may still occur.
AESTHETIC
MODIFICATION
UPPER LIP
3. Robson
The incision described by Robson descends in a
relaxed skin tension line beginning just medial to the
lateral commissure. An incision placed in this line
should produce an unobtrusive scar. However, this
lateral approach will damage the terminal branches
of the facial and mental nerves.
LOWER LIP
UPPER LIP
Fig. 3 - Standard
WEBER-FERGUSON
lip splitting
incisions
with chevron
modification.
ALTEMIR
Fig. 2 - Upper
433
lip splitting
incisions.
Fig. 4 - (A,B)
Operative
planning
of aesthetic
lip splits
434
British
Journal
of Oral
and Maxillofacial
Surgery
Fig. 5 - Postoperative results 8 months (top) and 5 years (bottom) following lower lip split. The peri-oral scar is virtually imperceptible.
The semi-circular labiomental groove scar is noticeable where it crosses the relaxed skin tension lines.
the columella and then deviated to follow the nasal
contour to the medial canthus on the side to be
exposed. Fergusong described an infra-orbital lateral
extension of the incision from the medial canthus to
enhance exposure of the maxilla (Fig. 2). Although
this incision lies in a line of relaxed skin tension,
the straight vertical scar across the upper lip and
convexity of the vermilion margin may be noticeable, even if the vermilion border is carefully
apposed.
2. Altemir
Altemir described a straight line lip split along the
philtral crest which is then extended as for the WeberFerguson incision (Fig. 2). Access is provided, by
both this incision and also a palatal incision, for
osteotomy cuts to allow mobilisation of the maxilla
pedicled on the cheek soft tissues. The incision
through the lip follows a line of relaxed skin tension
but again the vertical straight scar across the lip and
vermilion margin may be noticeable.
Aesthetic
Fig. 6 - ( A,B) Postoperative
results 9 months
unobtrusive
broken hne of the peri-oral
scar.
after
Altemir
approach
__
METHODS
We routinely use a simple modification of both the
Weber-Ferguson incision to split the upper lip and
McGregor incision to split the lower lip. A chevron
is incorporated into both the vermilion margin and
midline lip incisions (Figs 3 & 4) and extended to
the obicularis oris which is divided in the midline.
The wounds are closed in layers with accurate apposition of the vermilion border.
DISCUSSION
There are three main advantages provided by this
simple modification
to the lip splitting incision.
Firstly, there are more landmarks for accurate wound
closure. Secondly, the line of the scar is elongated
with several alterations in orientation which avoids
straight line contracture, especially across the perioral skin. Finally, the stigmatising appearance of a
lip split is avoided by the broken line of the peri-oral
scar (Figs 5 & 6).
Previous descriptions of lip splits all share the
advantage of improving access to deep facial structures and often make use of similar anatomical features to help hide the scar line. However, they also
share the disadvantage of a straight line incision
across the vermilion margin and peri-oral skin which
may produce an unsatisfactory scar. The described
modification extends the attempts of existing incision
designs to conceal the resulting facial scars. The
prime benefit of this simple modification is to disguise
the peri-oral scar to improve the aesthetic result.
Acknowledgements
The authors
thank
Miss Tracey
Boyle, Medical
Artist
and Mr
Richard
Hancock,
Medical
Photographer
for preparing
the illustrations
and Miss Deborah
Noonan,
Medical Secretary
for preparing the manuscript.
with
radial
forearm
flap reconstruction
of the palate.
lip splits
Note
435
the
References
1. Gooris PJJ, Worthington
P, Evans JR. Mandibulotomy:
a
surgical approach
to oral and pharyngeal
lesions. Int J Oral
Maxillofac
Surg 1989; 18: 3599364.
2. Altemir
FH. Transfacial
access to the retromaxillary
area.
J Maxillofac
Surg 1986; 14: 1655170.
3_ Kraissl CJ. The selection of appropriate
lines for elective
surgical incisions.
Plast Reconstr
Surg 195 I; 8: I-14.
4. Borges AF, Alexander
JE. Relaxed skin tension lines,
Z-plasties
on scars, and fusiform
excision
of lesions. Br J Plast
Surg 1961; 15: 2422254.
Roux PJ. Cited in: Butlin HT, Spencer GJ eds. Diseases of the
tongue. London:
Cassell, 1900: 359.
Trotter W. Operations
for malignant
diseases of the pharynx.
Br J Surg 1929; 16: 485-495.
McGregor
IA. McDonald
DG. Mandibular
osteotomy
in the
approach
to the oral cavity. Head Neck Surg 1983; 5: 457-462.
Robson MC. An easy access incision for the removal
of some
intraoral
malignant
tumours.
Plast Reconstr
Surg 1979; 64:
8344835.
9. Weber 0. Vorstellung
einer kranken
mit Resection
des
Unterkiefers
Verhdndhmgen
des naturhist
--med Vereins z
Heidelberg
1845; 4: 80--82.
10. Ferguson
W. In operation
of the upper jaw. A System of
Practical
Surgery.
Edinburgh:
John Churchill.
1842: 484.
The Authors
J. P. Hayter FRCS, FDSRCS
Senior Registrar
E. D. Vaughan FRCS, FDSRCS
Consultant
J. S. Brown FRCS, FDSRCS
Consultant
Maxillofacial
Unit
Walton Hospital
Liverpool
L9 1AE, UK
Correspondence
and requests
Paper received 16 May
Accepted
18 July 1995
1995
for offprints
to J. P. Hayter
También podría gustarte
- Cleft Lip and Palate Management: A Comprehensive AtlasDe EverandCleft Lip and Palate Management: A Comprehensive AtlasRicardo D. BennunAún no hay calificaciones
- Nasolabial Flap For Oral Cavity ReconstructionDocumento10 páginasNasolabial Flap For Oral Cavity ReconstructionJamesAún no hay calificaciones
- Fat Removal: Invasive and Non-invasive Body ContouringDe EverandFat Removal: Invasive and Non-invasive Body ContouringMathew AvramAún no hay calificaciones
- The Open Brow LiftDocumento8 páginasThe Open Brow LiftdoctorbanAún no hay calificaciones
- Cases Surgery For Non-Melanoma Skin Cancers: bcc, scc, mcc.De EverandCases Surgery For Non-Melanoma Skin Cancers: bcc, scc, mcc.Aún no hay calificaciones
- A Classification System of DefectsDocumento12 páginasA Classification System of DefectsPrana SkyaAún no hay calificaciones
- Atlas of Topographical and Pathotopographical Anatomy of the Head and NeckDe EverandAtlas of Topographical and Pathotopographical Anatomy of the Head and NeckAún no hay calificaciones
- Asian Rhinoplasty1Documento19 páginasAsian Rhinoplasty1drbantmAún no hay calificaciones
- Mandibular ReconstructionDocumento26 páginasMandibular ReconstructiontalmordanielAún no hay calificaciones
- Aesthetic Surgery of The Orbits and EyelidsDocumento31 páginasAesthetic Surgery of The Orbits and EyelidsdoctorbanAún no hay calificaciones
- Facial Analysis LRDocumento36 páginasFacial Analysis LRdestiAún no hay calificaciones
- The Five-Step Rhinoplasty Dead Space Closure TechniqueDocumento2 páginasThe Five-Step Rhinoplasty Dead Space Closure TechniqueAdRiaNa JuLIetH LoZaDa PaTiÑoAún no hay calificaciones
- Medical Rhinoplasty: Injectables Aesthetic Feature 0Documento17 páginasMedical Rhinoplasty: Injectables Aesthetic Feature 0alejandro GonzàlezAún no hay calificaciones
- The Composite Spreader FlapDocumento11 páginasThe Composite Spreader FlapameliAún no hay calificaciones
- Liposuccion Cervical Haack2006Documento7 páginasLiposuccion Cervical Haack2006ever renteriaAún no hay calificaciones
- The Use of The Buccal Fat Pad Flap For Oral Reconstruction: Review Open AccessDocumento9 páginasThe Use of The Buccal Fat Pad Flap For Oral Reconstruction: Review Open Accessmehak malhotraAún no hay calificaciones
- Controversies in Maxillofacial Trauma PDFDocumento9 páginasControversies in Maxillofacial Trauma PDFFabian Camelo OtorrinoAún no hay calificaciones
- Ethnic and Gender Considerations in The Use of Facial Injectables: Male PatientsDocumento4 páginasEthnic and Gender Considerations in The Use of Facial Injectables: Male PatientsLuiggi FayadAún no hay calificaciones
- Abdominoplasty Classic Principles and TechniqueDocumento18 páginasAbdominoplasty Classic Principles and TechniqueJonathan Zenteno JiménezAún no hay calificaciones
- TULUA Lipoabdominoplasty Transversal Aponeurotic.12Documento14 páginasTULUA Lipoabdominoplasty Transversal Aponeurotic.12Carolina Ormaza Giraldo100% (1)
- Rhinoplasty: Edited by Michael J. BrennerDocumento158 páginasRhinoplasty: Edited by Michael J. BrennerSang TrầnAún no hay calificaciones
- Septal Extension Graft ArticlesDocumento7 páginasSeptal Extension Graft Articlesjose orlando sturla pelleranoAún no hay calificaciones
- (Lip Factor) The Lip Lift Stanley PDFDocumento7 páginas(Lip Factor) The Lip Lift Stanley PDFFelipeGuzanskyMilaneziAún no hay calificaciones
- Spare Roof Technique: A New Technique For Hump Removal-The Step-by-Step GuideDocumento4 páginasSpare Roof Technique: A New Technique For Hump Removal-The Step-by-Step GuideLeonardo SeveroAún no hay calificaciones
- Facial PlasticsDocumento116 páginasFacial Plasticssyed imdadAún no hay calificaciones
- Local and Regional Flaps in Head and Neck Cancer / Orthodontic Courses by Indian Dental AcademyDocumento56 páginasLocal and Regional Flaps in Head and Neck Cancer / Orthodontic Courses by Indian Dental Academyindian dental academyAún no hay calificaciones
- Rhinoplasty Experience SheenDocumento33 páginasRhinoplasty Experience SheenmadmaxpsuAún no hay calificaciones
- Endoscopic DacryocystorhinostomyDocumento17 páginasEndoscopic Dacryocystorhinostomyapi-19500641Aún no hay calificaciones
- Gox 1 E07 PDFDocumento2 páginasGox 1 E07 PDFUmer HussainAún no hay calificaciones
- Subbrow Blepharoplasty For Upper Eyelid Rejuvenation in AsiansDocumento5 páginasSubbrow Blepharoplasty For Upper Eyelid Rejuvenation in AsiansdoctorbanAún no hay calificaciones
- Lip LiftDocumento14 páginasLip LiftGuilherme BergantonAún no hay calificaciones
- Stefan Danilla - Selected Topics in Plastic Reconstructive Surgery (2012, InTech)Documento243 páginasStefan Danilla - Selected Topics in Plastic Reconstructive Surgery (2012, InTech)Ramona PaulaAún no hay calificaciones
- Lip and Cheek ReconstructionDocumento108 páginasLip and Cheek Reconstructionthanhtrimd100% (1)
- Alar Base Reduction and Alar-Columellar RelationshipDocumento9 páginasAlar Base Reduction and Alar-Columellar RelationshipFabian Camelo OtorrinoAún no hay calificaciones
- Flap Selection in Head and Neck Cancer ReconstructionDocumento14 páginasFlap Selection in Head and Neck Cancer ReconstructionFerry RusdiansaputraAún no hay calificaciones
- Postoperative Care RhinoplastyDocumento4 páginasPostoperative Care RhinoplastySunayan BGAún no hay calificaciones
- Asianrhinoplasty: Dean M. Toriumi,, Colin D. PeroDocumento18 páginasAsianrhinoplasty: Dean M. Toriumi,, Colin D. PerodrbantmAún no hay calificaciones
- Nasal Dorsal AugmentationDocumento9 páginasNasal Dorsal AugmentationAnonymous O9x3NDAún no hay calificaciones
- Management of Orbital FracturesDocumento12 páginasManagement of Orbital FracturesMarisol Gallego DuqueAún no hay calificaciones
- Smile Restoration After Facial PalsyDocumento6 páginasSmile Restoration After Facial PalsyJimmie CooperAún no hay calificaciones
- Retaining Ligaments of The Face: Review of Anatomy and Clinical ApplicationsDocumento14 páginasRetaining Ligaments of The Face: Review of Anatomy and Clinical ApplicationsMariel IslasAún no hay calificaciones
- Surgical Approaches To The Facial Skeleton Mandible and TMJDocumento24 páginasSurgical Approaches To The Facial Skeleton Mandible and TMJRagavi VijayaragavanAún no hay calificaciones
- Eyelidreconstruction 130801074705 Phpapp02 PDFDocumento15 páginasEyelidreconstruction 130801074705 Phpapp02 PDFEcaterina Borovic-PavlovschiAún no hay calificaciones
- 2022 Surek. Deep Plane Anatomy For The Facelift Surgeon A Comprehensi...Documento10 páginas2022 Surek. Deep Plane Anatomy For The Facelift Surgeon A Comprehensi...Vivekanand ChandrashekarAún no hay calificaciones
- Aging Facial Skeleton PrsDocumento10 páginasAging Facial Skeleton PrsJorge TreviñoAún no hay calificaciones
- "No-Touch" Technique For Lip EnhancementDocumento11 páginas"No-Touch" Technique For Lip EnhancementClaudia Antonia Ortiz Peralta0% (1)
- History of RhinoplastyDocumento9 páginasHistory of RhinoplastySyamsul RizalAún no hay calificaciones
- Sec 4 - Techniques 2Documento31 páginasSec 4 - Techniques 2Karem TubeAún no hay calificaciones
- Massry - Management of Postblepharoplasty Lower Eyelid RetractionDocumento10 páginasMassry - Management of Postblepharoplasty Lower Eyelid RetractionLuiggi Fayad100% (1)
- Bahan Local FlapDocumento72 páginasBahan Local FlapChandrawati PramanaAún no hay calificaciones
- Nasal ReconstructionDocumento14 páginasNasal ReconstructionNovia Chrisnawati100% (1)
- Changing Role of Septal Extension Versus Columellar Grafts in Modern RhinoplastyDocumento5 páginasChanging Role of Septal Extension Versus Columellar Grafts in Modern RhinoplastyDanielBallesterosAún no hay calificaciones
- The Anatomy of The Aging FaceA ReviewDocumento8 páginasThe Anatomy of The Aging FaceA ReviewDoctores Duarte BarrosAún no hay calificaciones
- Annals of Plastic and Reconstructive SurgeryDocumento10 páginasAnnals of Plastic and Reconstructive SurgeryLuiggi Fayad100% (2)
- Ricketts 1968Documento18 páginasRicketts 1968Claudia Gamboa FerrerAún no hay calificaciones
- BJPS 1984 Cormack Classification of FlapsDocumento8 páginasBJPS 1984 Cormack Classification of FlapsS EllurAún no hay calificaciones
- Centrofacial Rejuvenation (PDFDrive)Documento416 páginasCentrofacial Rejuvenation (PDFDrive)sousourimeAún no hay calificaciones
- Deep Plane LiftDocumento5 páginasDeep Plane LiftNéstor Ariel CecconiAún no hay calificaciones
- A Novel Technique of Asian Tip Plasty by Dr. Man Koon, Suh From JW Plastic SurgeryDocumento9 páginasA Novel Technique of Asian Tip Plasty by Dr. Man Koon, Suh From JW Plastic SurgeryJWPlasticsurgeryAún no hay calificaciones
- The Functional Anatomy of The Deep Facial Fat Compartments: A Detailed Imaging-Based InvestigationDocumento11 páginasThe Functional Anatomy of The Deep Facial Fat Compartments: A Detailed Imaging-Based InvestigationFernanda RibeiroAún no hay calificaciones
- The Homoeopathy Central Council Act, 1973: Reliminary EctionsDocumento19 páginasThe Homoeopathy Central Council Act, 1973: Reliminary EctionsrajtanniruAún no hay calificaciones
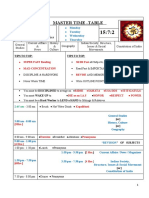
- Master Time - Table: 2 Hrs. - News 4 Hrs. - Revision 9 Hrs. - New TopicsDocumento2 páginasMaster Time - Table: 2 Hrs. - News 4 Hrs. - Revision 9 Hrs. - New TopicsrajtanniruAún no hay calificaciones
- Master Time - Table: 2 Hrs. - News 4 Hrs. - Revision 9 Hrs. - New TopicsDocumento3 páginasMaster Time - Table: 2 Hrs. - News 4 Hrs. - Revision 9 Hrs. - New TopicsrajtanniruAún no hay calificaciones
- Sarvai PapannaDocumento3 páginasSarvai Papannarajtanniru0% (1)
- Master Time - Table: 2 Hrs. - News 4 Hrs. - Revision 9 Hrs. - New TopicsDocumento3 páginasMaster Time - Table: 2 Hrs. - News 4 Hrs. - Revision 9 Hrs. - New TopicsrajtanniruAún no hay calificaciones
- VISHNUKUNDINSDocumento2 páginasVISHNUKUNDINSrajtanniruAún no hay calificaciones
- Social and Cultural Condition Under The Mauryan, Satavahanas and GuptasDocumento40 páginasSocial and Cultural Condition Under The Mauryan, Satavahanas and Guptasrajtanniru100% (2)
- PRAYER Is A Tool To Prepare Us For Religious Pursuits. It Is A Means To Prepare Us ForDocumento2 páginasPRAYER Is A Tool To Prepare Us For Religious Pursuits. It Is A Means To Prepare Us ForrajtanniruAún no hay calificaciones
- Agricultural Distress in IndiaDocumento10 páginasAgricultural Distress in IndiarajtanniruAún no hay calificaciones
- Children's Bill of Rights: Included in Class VIII Social Science Text Books For NCERTDocumento2 páginasChildren's Bill of Rights: Included in Class VIII Social Science Text Books For NCERTrajtanniruAún no hay calificaciones
- Mouth AnatomyDocumento12 páginasMouth AnatomyGeorgi GugicevAún no hay calificaciones
- Magee 6th Edition - OPA - 4 Temporomandibular JointDocumento30 páginasMagee 6th Edition - OPA - 4 Temporomandibular JointRonny Araya AbarcaAún no hay calificaciones
- Endo Gi QuestionerDocumento26 páginasEndo Gi QuestionerRymmus Asuncion100% (1)
- Ossicles: The Malleus, The Incus, and The StapesDocumento6 páginasOssicles: The Malleus, The Incus, and The StapesLili M.Aún no hay calificaciones
- Bhopal (M.P.) : Microteaching On TongueDocumento7 páginasBhopal (M.P.) : Microteaching On TongueamitAún no hay calificaciones
- Ophtha SIM 2nd EdDocumento250 páginasOphtha SIM 2nd EdRalphAún no hay calificaciones
- Kindergarten: Quarter 1: Week 6 Learning ExperiencesDocumento27 páginasKindergarten: Quarter 1: Week 6 Learning ExperiencesHanzel NietesAún no hay calificaciones
- Identify The Part of The BrainDocumento2 páginasIdentify The Part of The BrainClement Mar ClimacoAún no hay calificaciones
- Spinal CordDocumento4 páginasSpinal CordMabel LynAún no hay calificaciones
- Multiple Choice Questions: This Activity Contains 20 QuestionsDocumento5 páginasMultiple Choice Questions: This Activity Contains 20 QuestionsHUAWEI HUAWEIAún no hay calificaciones
- Surgical Anatomy of The Facial NerveDocumento37 páginasSurgical Anatomy of The Facial NerveAbel AbrahamAún no hay calificaciones
- Ophtha Quiz - NeurophthalmologyDocumento2 páginasOphtha Quiz - NeurophthalmologyadiAún no hay calificaciones
- Cerebral Aerobics: Alveolar Process of The MaxillaDocumento2 páginasCerebral Aerobics: Alveolar Process of The MaxillaJo Hn VengzAún no hay calificaciones
- Radiol Clin N Am 2007 - Oral Cavity and Oropharynx TumorDocumento20 páginasRadiol Clin N Am 2007 - Oral Cavity and Oropharynx Tumorgina2535Aún no hay calificaciones
- 8EM PHYSoundDocumento18 páginas8EM PHYSoundsreekanthkataAún no hay calificaciones
- A Study of Artificial Cranial Deformation in New BritainDocumento24 páginasA Study of Artificial Cranial Deformation in New BritainSlavica JovanovicAún no hay calificaciones
- Pediatric in ReviewDocumento10 páginasPediatric in ReviewkafosidAún no hay calificaciones
- HypothalamusDocumento47 páginasHypothalamusHira SultanAún no hay calificaciones
- Ent - MCQ ExamDocumento41 páginasEnt - MCQ ExamAhmed Noori100% (1)
- Anatomic Localization in Clinical Neurology: GeneralitiesDocumento11 páginasAnatomic Localization in Clinical Neurology: GeneralitiesChennieWong100% (1)
- Em Swedenborg The FIVE SENSES Being Part Three of The Animal Kingdom 1744 Enoch S Price Swedenborg Scientific Association 1914Documento352 páginasEm Swedenborg The FIVE SENSES Being Part Three of The Animal Kingdom 1744 Enoch S Price Swedenborg Scientific Association 1914francis batt100% (2)
- A Practical Review of The Muscles of Facial Mimicry With Special Emphasis On The Superficial Musculoaponeurotic SystemDocumento8 páginasA Practical Review of The Muscles of Facial Mimicry With Special Emphasis On The Superficial Musculoaponeurotic SystemDr. Frederico NevesAún no hay calificaciones
- Treatment of Prominent Ears and Otoplasty 2015 DBDocumento6 páginasTreatment of Prominent Ears and Otoplasty 2015 DBcirugia plastica uisAún no hay calificaciones
- Fronto-Ethmoidal Meningoencephalocele: A Case Report: TAF. Benitaryani, PD. UtomoDocumento1 páginaFronto-Ethmoidal Meningoencephalocele: A Case Report: TAF. Benitaryani, PD. UtomotrifoniastriAún no hay calificaciones
- 8509 30087 1 PBDocumento5 páginas8509 30087 1 PBWilson Quispe AlanocaAún no hay calificaciones
- Mandibular Anatomical LandmarksDocumento14 páginasMandibular Anatomical LandmarksKishor Chindam100% (4)
- HES 101 - Lesson 11-SensesDocumento4 páginasHES 101 - Lesson 11-SensesLAGUERTA, JOHN MICHAEL A.Aún no hay calificaciones
- M10-MED - Cleft Lip, Alveolus and Palate (CLAP) - Team02Documento5 páginasM10-MED - Cleft Lip, Alveolus and Palate (CLAP) - Team02abeer alrofaeyAún no hay calificaciones
- Douglas Stanley On The Jaw & MouthDocumento12 páginasDouglas Stanley On The Jaw & MouthNick Enriquez SchollAún no hay calificaciones
- Eyes and Ears AssessmentDocumento20 páginasEyes and Ears AssessmentMonica JoyceAún no hay calificaciones
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionCalificación: 4 de 5 estrellas4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDCalificación: 5 de 5 estrellas5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityCalificación: 4 de 5 estrellas4/5 (29)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeCalificación: 2 de 5 estrellas2/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossDe EverandThe Obesity Code: Unlocking the Secrets of Weight LossCalificación: 4 de 5 estrellas4/5 (6)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Calificación: 3 de 5 estrellas3/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisCalificación: 4.5 de 5 estrellas4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedCalificación: 5 de 5 estrellas5/5 (81)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAún no hay calificaciones
- The Comfort of Crows: A Backyard YearDe EverandThe Comfort of Crows: A Backyard YearCalificación: 4.5 de 5 estrellas4.5/5 (23)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Calificación: 4.5 de 5 estrellas4.5/5 (110)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsCalificación: 5 de 5 estrellas5/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessCalificación: 4.5 de 5 estrellas4.5/5 (328)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceDe EverandTo Explain the World: The Discovery of Modern ScienceCalificación: 3.5 de 5 estrellas3.5/5 (51)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityCalificación: 4 de 5 estrellas4/5 (5)
- Troubled: A Memoir of Foster Care, Family, and Social ClassDe EverandTroubled: A Memoir of Foster Care, Family, and Social ClassCalificación: 4.5 de 5 estrellas4.5/5 (27)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeCalificación: 4.5 de 5 estrellas4.5/5 (253)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisCalificación: 4 de 5 estrellas4/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisCalificación: 3.5 de 5 estrellas3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsCalificación: 4 de 5 estrellas4/5 (4)
- The Marshmallow Test: Mastering Self-ControlDe EverandThe Marshmallow Test: Mastering Self-ControlCalificación: 4.5 de 5 estrellas4.5/5 (59)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsCalificación: 4.5 de 5 estrellas4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryCalificación: 4 de 5 estrellas4/5 (45)