Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Jurnal TBC
Cargado por
Lorinsya OllinTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Jurnal TBC
Cargado por
Lorinsya OllinCopyright:
Formatos disponibles
International Journal of Mycobacteriology
H O S T E D BY
x x x ( 2 0 1 5 ) x x x x x x
Available at www.sciencedirect.com
ScienceDirect
journal homepage: www.elsevier.com/locate/IJMYCO
Diagnosis of pediatric pulmonary tuberculosis
with special reference to polymerase chain reaction
based nucleic acid amplification test
Shreshtha Tiwari
a
b
a,b
, Gita Nataraj
a,*
,
Swapna Kanade a, Preeti Mehta
Department of Microbiology, Seth GSMC & KEM Hospital, Parel, Mumbai 400012, India
AIIMS Bhopal, India
A R T I C L E I N F O
A B S T R A C T
Article history:
Objective: To determine the utility of polymerase chain reaction (PCR) for diagnosing pedi-
Received 7 November 2014
atric pulmonary tuberculosis (PPTB).
Accepted 17 November 2014
Method: A prospective cross-sectional study was carried out on 100 children less than
Available online xxxx
14 years of age, with strong clinical suspicion and radiological evidence suggestive of pulmonary tuberculosis (TB). Sputum samples/gastric lavage were collected. Direct smears
Keywords:
and culture on Lowenstein Jensen (LJ) media were performed. DNA extraction and amplifi-
Pediatric pulmonary tuberculosis
cation was performed using GeneiTM Amplification Reagent set for Mycobacterium tuberculosis
PCR
(MTB) (by Genei, Bangalore, India). This test is based on the principle of single-tube nested
PCR which amplifies the repetitive insertion sequence IS6110.
Results: When compared with culture, sensitivity and specificity of PCR was 93.55% and
92.75%, respectively. The PPV was 85.29% and the NPV was 96.97%. When intention to treat
(ITT) was used as the standard, sensitivity, specificity, PPV and NPV of PCR was 47.88%,
93.1%, 94.4%, and 42.19%, respectively, and that of culture was 40.85%, 100%, 100% and
40.85%, respectively. Against response to treatment (RTT), PCR demonstrated sensitivity,
specificity, PPV and NPV of 50.9%, 93.1%, 93.33% and 50%, respectively, and for culture it
was 43.64%, 100%, 100% and 48.33%, respectively.
Conclusion/recommendation: The present study reinforces better case detection rate with
PCR-based nucleic acid amplification test as compared with microscopy and culture in
pediatric pulmonary TB. PCR showed a higher correlation with clinical diagnosis as compared with microscopy and solid culture. Hence, a molecular platform should be the test
of choice for detecting PPTB.
2015 Asian-African Society for Mycobacteriology. Published by Elsevier Ltd. All rights
reserved.
* Corresponding author at: Department of Microbiology, 5th floor, New building, Seth G.S. Medical College and KEM Hospital, Parel,
Mumbai 400012, Maharashtra, India.
E-mail addresses: shreshtha.tiwari@gmail.com (S. Tiwari), gitanataraj@gmail.com (G. Nataraj), swapnakanade71@gmail.com
(S. Kanade), prm.kem@gmail.com (P. Mehta).
http://dx.doi.org/10.1016/j.ijmyco.2014.11.063
2212-5531/ 2015 Asian-African Society for Mycobacteriology. Published by Elsevier Ltd. All rights reserved.
Please cite this article in press as: S Tiwari et al. Diagnosis of pediatric pulmonary tuberculosis with special reference to polymerase chain reaction
based nucleic acid amplication test. Int. J. Mycobacteriol. (2015), http://dx.doi.org/10.1016/j.ijmyco.2014.11.063
International Journal of Mycobacteriology
Introduction
Pediatric pulmonary tuberculosis (PPTB) remains a major
cause of morbidity and mortality worldwide, particularly in
developing countries [1]. In India, it is estimated that 514%
of tuberculosis [TB] cases occur in children [2], and in Mumbai, the incidence was 9% in 2010 [3].
A major challenge to PPTB is establishing an accurate diagnosis. Children less than 5 years rarely expectorate sputum
for evaluation, and the disease is paucibacillary with a smear
positivity rate of <15% and a culture positivity rate of 3040%
[4]. Gastric lavage and induced sputum only marginally
improve sensitivity [5]. Rapid culture systems with their
improved yield and reduced turnaround time still require a
period of 10 days in most cases and may not be cost effective
[6]. Most cases are diagnosed based on clinical presentations,
radiographic abnormalities, contact history and tuberculin
skin test results, all of which suffer from low specificity [7].
The development of polymerase chain reaction (PCR)based assays for the detection of mycobacterial DNA in clinical specimens has proved to be a diagnostic boon. The role of
nucleic acid amplification tests (NAAT) has been well established worldwide [8]. Most NAAT assays use the mycobacterial
insertion element IS6110 as the target for detecting Mycobacterium tuberculosis (MTB) complex organisms. The reported sensitivity in pediatric pulmonary specimens ranges from 95% to
100% in culture-positive cases and 50% to 60% in culture-negative cases [9]. For resource-constrained settings, the limitations of NAATs include the expensive equipment, the high
cost per test and the need to obtain multiple specimens in
smear-negative patients to improve sensitivity. Hence, there
is an urgent need for a rapid, reliable and affordable diagnostic test.
This study was carried out to determine the utility of a
PCR-based NAAT for diagnosing PPTB.
Materials and methods
Institutional ethics committee permission was obtained prior
to commencing the study. A prospective, cross-sectional study
was carried out on 100 children less than 14 years of age, with
strong clinical suspicion of pulmonary tuberculosis (PTB),
radiological evidence suggestive of PTB and whose parents/
guardians provided written informed consent. Symptoms that
were likely to suggest a diagnosis of PTB included: cough
P2 weeks duration and/or weight loss of at least 10% of
healthy body weight or no weight gain in 3 months and/or
fever for P2 weeks or one measured temperature above
38.5 C [10]. Children who were on anti-TB therapy (ATT) for
pulmonary/extra-pulmonary TB or those who had received
ATT within the last 6 months were excluded from the study.
From children older than 5 years of age and who could
expectorate, two sputum specimens (as per the Revised
National Tuberculosis Control Programme, RNTCP, protocol)
were collected in sterile, wide-mouthed, screw-capped containers [11]. In younger children and those who could not
expectorate, gastric lavage (GL) was collected by the
pediatrician on 3 consecutive days in sterile, wide-mouthed,
x x x ( 2 0 1 5 ) x x x x x x
screw-capped containers. The pH was immediately adjusted
to neutral with sodium bicarbonate [12].
Microbiology workup
All processing was carried out in Biological Safety Cabinet
(BSC) Type II, and level 2 biosafety practices were followed.
Microscopy
Direct smears were prepared from each of the specimens and
stained by Ziehl Neelsen method. The results were read and
recorded as per RNTCP protocol. Irrespective of the number
of sputum or GL specimens submitted per case, detection of
acid fast bacilli (AFB) in any one or all of the specimens submitted was considered as positive for that child.
Isolation and identification of MTB complex
All specimens were decontaminated with N-acetyl-L-Cysteine
(NALC) NaOH method and concentrated by centrifuging at
3000g for 15 min [13]. Two loopsful of the sediment were inoculated on two Lowenstein Jensen (LJ) media. One was incubated aerobically at 37 C and the other at room
temperature (25 C) [13]. All cultures were read daily for the
first week for detecting contamination or rapid growers and
then weekly thereafter for eight weeks or until growth was
detected, whichever was later. If mycobacterial growth was
detected in any one or all of the two/three specimens submitted, it was considered as positive for that child. The isolates
were identified as MTBC using SD BIOLINE TB Ag MPT 64
Rapid immunochromatography assay after confirming their
acid-fast nature [14].
NAAT (PCR based)
DNA extraction and amplification was performed using GeneiTM Amplification Reagent set for MTB (by Genei, Bangalore,
India) as per manufacturers instructions with minimal modifications [15]. The samples were decontaminated with NALC
NaOH instead of using modified Petroffs method, and the pellets of all the specimens of a single patient were pooled so as
to get a single pellet on which NAAT was performed. 3 ll of a
DNA sample was added to 9 ll of the first amplification premix. This test is based on the principle of a single-tube-nested
PCR which amplifies the repetitive insertion sequence IS6110.
It is a two-step sequential assay. In the first step, the IS region
of the MTB complex DNA sequence, a 220 bp, is amplified by
specific external primers.
The external primer sequence was as follows:
695 to 724 (5 0 -CGGGACCACCCGCGGCAAAGCCCGCAGGAC3 0 ) and
885 to 914 (5 0 -CATCGTGGAAGCGACCCGCCAGCCCAGGAT-3 0 )
The first amplification reaction profile consisted of a cycle
of an initial denaturation step at 22 C for 10 min and 94 C for
5 min, followed by 20 cycles at 94 C for 30 s (denaturation),
Please cite this article in press as: S Tiwari et al. Diagnosis of pediatric pulmonary tuberculosis with special reference to polymerase chain reaction
based nucleic acid amplication test. Int. J. Mycobacteriol. (2015), http://dx.doi.org/10.1016/j.ijmyco.2014.11.063
International Journal of Mycobacteriology
68 C for 1 min (annealing) and 72 C for 1 min (extension),
and a final extension cycle of 70 C for 7 min. The vials were
removed from the thermal cycler when samples reached
4 C and then centrifuged at 10,000 rpm for 30 s before opening to avoid aerosol contamination.
After the first PCR cycling was completed, 15 ll of the second amplification master-mix was added to each tube and the
second NAAT was performed. The inner primers were used to
further amplify a 123 bp amplification product.
The inner primer sequence was as follows:
Primer IS1 [5 0 -CCTGCGAGCGTAGGCGTCGG-3 0 ] and
Primer IS2 [5 0 -CTCGTCCAGCGCCGCTTCGG-3 0 ]
The cycling parameters consisted of an initial cycle at
94 C for 5 min, followed by 30 cycles at 94 C for 30 s (denaturation), 68 C for 30 s (annealing) and 72 C for 30 s (extension),
and a cycle of final extension at 72 C for 7 min. The kit also
includes an internal control DNA. The amplified products
were analyzed using gel electrophoresis. A band of 340 bp is
the amplification product of the internal control DNA. An
amplification product of size 123 bp is indicative of the presence of MTBC. Results were considered as positive if there
was a band both at 123 bp and 340 bp or a band only at
123 bp. The presence of only one band at 340 bp was considered negative. The DNA extraction was to be repeated if there
was no band at all as it indicated either that the sample contained inhibitors or the DNA extraction had failed. Reprocessing of such samples was to be carried out by repeating the
extraction procedure with 100 ll of the DNA.
Data recording
Clinical details, radiological findings and relevant laboratory
investigations, where available, and the treatment initiated
were recorded. Contact number of the patients caregiver
was also recorded for follow-up. Each child was followed up
and the response to treatment (RTT) was noted at the end
of 2 weeks for those receiving antibiotics only and at
6 months for those receiving anti-tuberculosis treatment
(ATT). A probable case, confirmed case, cured, treatment completed, death and treatment failure were defined as er RNTCP
guidelines [16].
Statistical analysis
100 clinically suspected PPTB cases were included. Data was
entered in the SPSS version 15.0. Performance of PCR-based
x x x ( 2 0 1 5 ) x x x x x x
NAAT was reported in terms of sensitivity and specificity at
95% confidence interval. Three reference standards were used
for comparison; intention to treat (ITT), response to ATT and
culture positivity.
Results (Table 1)
Of 100 consecutive, clinically suspected PPTB cases included
in the study, 36 were less than 5 years of age. Gender ratio
was observed to be equal. GL was obtained from 41 children
and expectorated sputum from 59 children.
Of the 241 specimens (123 GL and 118 sputa) tested by
microscopy and culture, and 100 pooled specimens from an
equal number of suspect children tested by PCR, PCR was
positive in 36 children, culture was positive in 31 and microscopy was positive in 13. In clinically suspected cases of PPTB,
the sensitivity of NAAT, culture and microscopy was 36%, 31%
and 13%, respectively. All the isolates were identified as MTBC
by SD Bioline MPT 64 Rapid test.
Concordant results by PCR-NAAT and culture (Table 1) were
observed in 93 children with 29 testing positive both by culture
and PCR and 64 testing negative by both. Discordance was
observed in 7 of which 5 were PCR-positive and culture-negative and 2 were PCR-negative and culture-positive. When compared with culture, sensitivity and specificity of PCR-NAAT
was 93.55% (95% CI: 78.5499.02%) and 92.75% (95% CI: 83.88
97.58%), respectively. The PPV was 85.29% (95% CI: 68.93
94.99%) and NPV was 96.97% (95% CI: 89.4699.54%).
Of the 100 children enrolled in the study, 29 received only
antibiotics (Amoxicillin or Cloxacillin and/or Amikacin) and
responded. Of these, none were acid-fast microscopy positive
or culture positive. However, 2 of these were NAAT positive. 71
children received ATT; NAAT was positive in 34 of these cases,
while culture was positive in 31 and microscopy in 13. When
ITTwas used as the standard, NAAT had a sensitivity, specificity, PPV and NPV of 47.88% (95% CI: 35.8860.08%), 93.1% (95%
CI: 77.1998.95%), 94.4% (95% CI: 81.3399.16%), and 42.19%
(95% CI: 29.9455.18%). All that were positive by microscopy
were also positive by culture and PCR. The sensitivity, specificity, PPV and NPV of culture against ITT was 40.85% (95%
CI: 29.3253.16%), 100% (95% CI: 87.94100%), 100% (95% CI:
87.94100%) and 40.85% (95% CI: 29.3253.16%), respectively.
Of the 71 children initiated on ATT, 5 were lost to follow-up
and excluded from analysis. Of the remaining 66, treatment
completion was achieved in 55 (83.3%). Eleven children had
an adverse outcome of which 10 died during treatment and
1 was a treatment failure with culture-positive result. PCR
was positive in 28 and culture in 24 of the 55 patients who
Table 1 Comparison of Microscopy, culture and NAAT.
Culture positive (n = 31)
Culture negative (n = 69)
Total (n = 100)
Sensitivity (%)
Specificity (%)
Microscopy
Positive
Negative
13
18
0
69
13
87
41.9
100
NAAT
Positive
Negative
29
2
5
64
34
66
93.55
92.75
Please cite this article in press as: S Tiwari et al. Diagnosis of pediatric pulmonary tuberculosis with special reference to polymerase chain reaction
based nucleic acid amplication test. Int. J. Mycobacteriol. (2015), http://dx.doi.org/10.1016/j.ijmyco.2014.11.063
International Journal of Mycobacteriology
completed their treatment and responded. Against response
to treatment, NAAT demonstrated a sensitivity, specificity,
PPV and NPV of 50.9% (95% CI: 37.0764.64%), 93.1% (95% CI:
77.1998.95%), 93.33% (95% CI: 77.8998.99%) and 50% (95%
CI: 36.0863.92%), respectively. Culture demonstrated a sensitivity, specificity, PPV and NPV of 43.64% (95% CI: 30.31
57.68%), 100% (95% CI: 87.94100%), 100% (95% CI: 85.62
100%) and 48.33% (95% CI: 35.2361.6%), respectively.
Discussion
The conventional methods of diagnosis which include acidfast stained microscopy and culture perform poorly in PPTB.
In the present study on 100 children with clinical presentation
strongly suggestive of TB, performance of PCR-based NAAT
has been evaluated against culture on LJ medium, intention
to treat with ATT and RTT. This is one of the few studies
which included ITT and RTT as standards for defining performance of the different diagnostic tests.
The results observed in the present study reinforce previous published data with reference to sensitivity, specificity
and rapidity of PCR-based assays [1719]. In those 71 children
who received ATT, the sensitivity of PCR, culture and microscopy was 47.8%, 43.6% and 18.3%, respectively. Higher sensitivities have been reported in literature [2022]. However,
these have compared the performance of PCR against culture.
The higher sensitivity of any NAAT can be attributed to the
technology itself which amplifies the original load of DNA
more than a million times and in the present study, the use
of LJ medium instead of the recommended liquid culture systems (MGIT 960). PCR was positive in all 13 cases which were
smear-positive. In addition, PCR was also positive in 21 cases
which were smearnegative and 3 cases which were culturenegative. In smear-negative cases, PCR is reported to have a
lower sensitivity as compared with liquid culture [2325].
PCR was negative in two smear-negative but culture-positive cases. False negative NAAT may be due to the presence of
inhibitors not detected by the control amplification or nonhomogenous distribution of bacteria in the specimen so that
the fraction tested does not contain mycobacteria or a low
number of bacilli in the specimen. Both these reasons do
not apply to the present study. The following precautions
were taken to avoid false negative results. A recombinant
plasmid DNA was provided as an internal control during the
DNA extraction procedure to validate extraction protocol.
Absence of an internal control band at 340 bp indicated either
the presence of inhibitors or the failure of DNA extraction,
and the process of DNA extraction was to be repeated as
per manufacturers instructions. This was not observed in
any of the runs. All specimens were homogenized and concentrated before processing to improve the quality of specimen and to concentrate the bacillary load.
Five children were culture-negative and PCR-NAAT positive. Three of these were initiated on ATT and showed symptomatic improvement. Hence, these were considered as cases
of TB. The remaining 2 children had a history of TB one year
prior. These children, however, responded to antibiotic treatment and PCR may be false-positive. False-positive NAATs
can be due to multiple reasons. Carryover of amplicons from
x x x ( 2 0 1 5 ) x x x x x x
previous reactions is considered a major limitation of PCRbased assays. To avoid false positivity arising from cross-contamination, DNA extraction and NAAT were done in two separate laboratory areas away from the culture laboratory. PCR
workstation and dedicated equipment were used for reagent
preparation. Disposable plastic ware and filter-blocked tips
were used, and frequent changing of gloves was practiced.
Uracil DNA glycosylase (UDG) was added to the master mix
to minimize previous amplicon contamination and not more
than five samples were processed in a day. The other reason
for false positivity could be the amplification of DNA from
dead bacilli in the respiratory secretions following successful
ATT. Since DNA-based NAATs can also detect dead bacilli, the
results of NAAT should be used in conjunction with clinical
presentation and the pretest probabilities.
In the present study, culture positivity was 43.66% (31/71).
Studies from India have reported culture positivity ranging
from 32% to 37.7% [2628]. A higher culture positivity has been
reported by Petrovi et al. (Serbia, 2005, 43%) [29] and Jeena
et al. (South Africa, 2002, 88%) [30]. Higher rates in these studies have been attributed to the use of a combination of
induced sputum and gastric lavage as specimens, as well as
the use of a combination of one solid and one liquid medium.
Though culture is highly specific for the diagnosis of TB, it is
relatively insensitive for pediatric TB when evaluated against
the clinical reference standard [31,32].
The comparatively lower yield with culture may be attributed to the use of only solid medium for culture. Liquid culture systems with continuous monitoring for mycobacterial
growth (such as MB/BacT) and mycobacterial growth indicator tube (MGIT) provide a significantly higher yield than solid
culture and in half the time [6]. Microscopic observation drug
susceptibility (MODS) is a potentially low-cost alternative to
MGIT with comparable sensitivity [33].
In the present study, microscopy could detect only 18.3%
(13/71) of cases. The yield of acid-fast microscopy of respiratory samples in children has been found to be low, ranging
from 12% to 17.2% [2628]. The inherent reasons for the low
sensitivity of microscopy in children has been attributed to
the paucibacillary nature of the disease and to the fact that
often the child lacks post-tussive expulsive force to bring
out a good quality sputum.
Excluding drop-outs and deaths, successful treatment outcome was achieved in a total of 55 out of 66 children initiated
on ATT (83.3%). Though there is a wide margin for improving
treatment outcome, this would need an early diagnosis and
require the use of more accurate and rapid tests.
A mortality of 14.1% (10/71) was observed in the present
study. Oeltmann et al. reported 10.5% mortality (Botswana,
2008, 10.5%) [34], and Harries et al. reported 17% (Malawi,
2002) [35]. Death in young children can be attributed to the
rapid progression and dissemination of the disease.
Children usually acquire TB from adults. Thus, TB in children reflects the ongoing transmission in the community and
indirectly reflects on the performance of national programs.
This emphasizes the need for early and accurate diagnosis
of the disease in children to benefit both the affected child
and the community. For a long time, RNTCP has emphasized
acid-fast microscopy for the diagnosis of PTB. The present
Please cite this article in press as: S Tiwari et al. Diagnosis of pediatric pulmonary tuberculosis with special reference to polymerase chain reaction
based nucleic acid amplication test. Int. J. Mycobacteriol. (2015), http://dx.doi.org/10.1016/j.ijmyco.2014.11.063
International Journal of Mycobacteriology
study, like many before, reinforces the poor sensitivity of
microscopy and a better case detection rate with PCR-based
NAAT. Recent standards on TB care recommend that in all
children suspected of having pulmonary TB, microbiological
confirmation should be sought through examination of a
respiratory specimen for smear microscopy, Xpert MTB/RIF
assay and/or culture [36]. The GeneXpert MTB/RIF assay with
its simple procedure, rapid results, decreased turnaround
time and almost no expertise needed, is expectedly a better
option for detecting pediatric TB. The same is now recommended by RNTCP [37].
This study has some limitations. The collection of specimens were dependent on the pediatrician. Thus, there was
no control over the quality of the specimens and the transport
to the laboratory. Smear preparation after concentration of
the specimen and the use of fluorescent/LED microscopy
could have increased smear positivity. The use of liquid culture systems might have improved the culture yield.
All the three test modalities used in the present study
yielded sensitivity lower than that observed in adults. PCRNAAT showed a higher correlation with clinical diagnosis as
compared with microscopy and solid culture. Hence, a molecular platform should be the test of choice for detecting PPTB.
However, culture would still be required for effective case
management.
Conflict of interest
[9]
[10]
[11]
[12]
[13]
[14]
[15]
[16]
[17]
[18]
None declared.
Acknowledgement
[19]
The authors would like to acknowledge the operational
research Grant of RNTCP and funds from DJST.
[20]
[21]
R E F E R E N C E S
[22]
[1] P. Eamranond, E. Jaramillo, Tuberculosis in children:
reassessing the need for improved diagnosis in global control
strategies, Int. J. Tuberc. Lung Dis. 5 (7) (2001 Jul) 594603.
[2] TB India 2014 TB Control India. Available @ <www.tbcindia.
nic.in/pdfs/TB%20INDIA%202014.pdf>.
[3] RNTCP Status Report; Annual Report 2013. Available from:
URL: <planningcommission.nic.in/reports/genrep/health/
RNTCP_2013.pdf>
[4] Soumya Swaminathan, Banu Rekha, Pediatric tuberculosis:
global overview and challenges, Clin. Infect. Dis. 50 (S3) (2010)
S184S194.
[5] P. Hepple, N. Ford, R. McNerney, Microscopy compared to
culture for the diagnosis of tuberculosis in induced sputum
samples: a systematic review, Int. J. Tuberc. Lung Dis. 16 (5)
(2012 May) 579588.
[6] B.J. Marais, M. Pai, New approaches and emerging
technologies in the diagnosis of childhood tuberculosis,
Paediatr. Respir. Rev. 8 (2007) 124133.
[7] Diagnosis of Tuberculosis in Children. Available from: <www.
nc.cdc.gov/eid/article/1/4/pdfs/95-0402.pdf>.
[8] Centers for Disease Control and Prevention (CDC), Update
guidelines for the use of nucleic acid amplification tests in
[23]
[24]
[25]
[26]
x x x ( 2 0 1 5 ) x x x x x x
the diagnosis of tuberculosis, MMWR Morb. Mortal. Wkly.
Rep. 58 (1) (2009 Jan 16) 710.
H.S. Schaaf, B.J. Marais, A. Whitelaw, A.C. Hesseling, B. Eley,
G.D. Hussey, et al, Culture-confirmed childhood tuberculosis
in Cape Town, South Africa: a review of 596 cases, BMC Infect.
Dis. 7 (2007) 140.
Working Group on Tuberculosis, Indian Academy of
Pediatrics (IAP), Indian Pediatr. 47 (2010) 4155.
Central TB Division, Directorate General of Health Services,
Revised National Tuberculosis Control Programme, Manual
for Laboratory Technicians, Smear Microscopy for Detection
of Acid-Fast Bacilli.
P.T. Kent, G.P. Kubica, Public Health Mycobacteriology,
Centers for Disease Control, Atlanta, GA, 1985.
Revised National TB Control Programme Manual of Standard
Operating Procedures (SOPs) Culture of Mycobacterium
tuberculosis and Drug Susceptibility Testing on Solid Medium.
TB Antigen MPT 64 Rapid. Available from <www.standardia.
com/en/home/product/rapid/infectiousdisease/TB_Ag_
MPT64.html> (last accessed 01.10.14).
GeneiTM Amplification Reagent set for MTB (by Genei,
Bangalore, India). Available from <www.merckindiawebapps.
com/merckindiawebsites/merckmillipore/index.html#/128/>
(last accessed 01.10.14).
Central TB Division, Directorate General of Health Services.
RNTCP at a Glance. <tbcindia.nic.in/pdfs/RNTCP%20at%20a%
20Glance.pdf>.
H.J. Zar, L. Workman, W. Isaacs, et al, Rapid molecular
diagnosis of pulmonary tuberculosis in children using
nasopharyngeal specimens, Clin. Infect. Dis. 55 (8) (2012)
10881095.
S.H. Montenegro, R.H. Gilman, P. Sheen, et al, Improved
detection of Mycobacterium tuberculosis (MTB) in Peruvian
children using a nested IS6110-PCR assay, Clin. Infect. Dis. 36
(2003) 1623.
S.K. Jatana, M.N. Nair, K.K. Lahiri, N.P. Sarin, Polymerase
chain reaction in the diagnosis of tuberculosis, Indian
Paediatr. 37 (4) (2000 Apr) 375382.
S.G. Gulec et al, Description of pediatric tuberculosis
evaluated in a referral center in Istanbul Turkey, Yonsei Med.
J. 53 (6) (2012) 11761182.
R. Lolekha et al, Childhood TB epidemiology and treatment
outcomes in Thailand: a TB active surveillance network, 2004
to 2006, BMC Infect. Dis. 8 (2008) 94.
S. Khalilzadeh, M. Hassanzad, N. Baghaiee, M.R. Bloorsaz,
A.A. Velayati, Evaluation of tuberculosis diagnostic criteria in
children, Afr. J. Microbiol. Res. 6 (26) (2012) 54405444.
L.E. Scott, K. McCarthy, N. Gous, M. Nduna, et al, Comparison
of Xpert MTB/RIF with other nucleic acid technologies for
diagnosing pulmonary tuberculosis in a high HIV prevalence
setting: a prospective study, PLoS Med. 8 (7) (2011) e1001061,
http://dx.doi.org/10.1371/journal.pmed.1001061 (Epub 2011
Jul 26).
A.K. Maurya, S. Kant, V.L. Nag, R. Kushwaha, T.N. Dhole,
Detection of 123 bp fragment of insertion element IS6110
Mycobacterium tuberculosis for diagnosis of extrapulmonary
tuberculosis, Indian J. Med. Microbiol. 30 (2) (2012 AprJun)
182186, http://dx.doi.org/10.4103/0255-0857.96688.
A.L. Seagar, B. Neish, I.F. Laurenson, Comparison of two inhouse real-time PCR assays with MTB Q-PCR Alert and
GenoType MTBDRplus for the rapid detection of
mycobacteria in clinical specimens, J. Med. Microbiol. 61 (Pt.
10) (2012) 14591464, http://dx.doi.org/10.1099/jmm.0.0431660 (Epub 2012 Jul 12).
D. Vijayasekaran, R.A. Kumar, N.C. Gowrishankar, K.
Nedunchelian, S. Sethuraman, Mantoux and contact
positivity in tuberculosis, Indian J. Pediatr. 73 (11) (2006 Nov)
989993.
Please cite this article in press as: S Tiwari et al. Diagnosis of pediatric pulmonary tuberculosis with special reference to polymerase chain reaction
based nucleic acid amplication test. Int. J. Mycobacteriol. (2015), http://dx.doi.org/10.1016/j.ijmyco.2014.11.063
International Journal of Mycobacteriology
[27] M. Singh, N.V. Moosa, L. Kumar, M. Sharma, Role of gastric
lavage and broncho-alveolar lavage in the bacteriological
diagnosis of childhood pulmonary tuberculosis, Indian
Pediatr. 37 (9) (2000) 947951.
[28] N. Somu, S. Swaminathan, C.N. Paramasivan, D.
Vijayaserkaran, A. Chandrabhooshanam, V.K. Vijayan, et al,
Value of bronchoalveolar lavage and gastric lavage in the
diagnosis of pulmonary tuberculosis in children, Tuberc.
Lung Dis. 76 (4) (1995) 295299.
[29] S. Petrovic, Diagnostic value of certain methods for isolation
of Mycobacterium tuberculosis in children with suspected
pulmonary tuberculosis, Med. Pregl. 58 (56) (2005) 231235.
[30] P.M. Jeena, P. Pillay, T. Pillay, H.M. Coovadia, Impact of HIV-1
co-infection on presentation and hospital-related mortality
in children with culture proven pulmonary tuberculosis in
Durban, South Africa, Int. J. Tuberc. Lung Dis. 6 (8) (2002) 672
678.
[31] M.P. Nicol, H.J. Zar, New specimens and laboratory
diagnostics for childhood pulmonary TB: progress and
prospects, Paediatr. Respir. Rev. 12 (1) (2011 Mar) 1621.
x x x ( 2 0 1 5 ) x x x x x x
[32] R.A. Oberhelman, G. Soto-Castellares, R.H. Gilman, L.
Caviedes, M.E. Castillo, L. Kolevic, et al, Diagnostic
approaches for paediatric tuberculosis by use of different
specimen types, culture methods, and PCR: a prospective
casecontrol study, Lancet Infect. Dis. 10 (9) (2010) 612620.
[33] K. Limaye, S. Kanade, G. Nataraj, P. Mehta, Utility of
microscopic observation of drug susceptibility (MODS) assay
for Mycobacterium tuberculosis in resource constrained
settings, Indian J. Tuberc. 57 (4) (Oct 2010) 207212.
[34] J.E. Oeltmann et al, Reported childhood tuberculosis
treatment outcomes, Gaborone and Francistown, Botswana,
19982002, Int. J. Tuberc. Lung Dis. 12 (2) (2008) 186192.
[35] A.D. Harries, N.J. Hargreaves, S.M. Graham, et al, Childhood
tuberculosis in Malawi: nationwide case-finding and
treatment outcomes, Int. J. Tuberc. Lung Dis. 6 (5) (2002) 424
431.
[36] International Standards for Tuberculosis Care, third ed., 2014.
[37] Standards for Tb Care in India, WHO, 2014.
Please cite this article in press as: S Tiwari et al. Diagnosis of pediatric pulmonary tuberculosis with special reference to polymerase chain reaction
based nucleic acid amplication test. Int. J. Mycobacteriol. (2015), http://dx.doi.org/10.1016/j.ijmyco.2014.11.063
También podría gustarte
- Pedoman Nasional TBDocumento71 páginasPedoman Nasional TBwidya ningrumAún no hay calificaciones
- Timebomb:The Global Epidemic of Multi-Drug Resistant TuberculosisDe EverandTimebomb:The Global Epidemic of Multi-Drug Resistant TuberculosisCalificación: 3.5 de 5 estrellas3.5/5 (2)
- Kapita Selekta: Haryati Bagian Penyakit Paru FK Unlam-RSU D UlinDocumento45 páginasKapita Selekta: Haryati Bagian Penyakit Paru FK Unlam-RSU D UlinM. Ridho Bagus PratamaAún no hay calificaciones
- Pharmacogenomics: From Discovery to Clinical ImplementationDe EverandPharmacogenomics: From Discovery to Clinical ImplementationShowkat Ahmad GanieAún no hay calificaciones
- LEaflet TBCDocumento3 páginasLEaflet TBCatik mayasariAún no hay calificaciones
- Hubungan Antara TB Dan HIVDocumento52 páginasHubungan Antara TB Dan HIVNurlaela Eka RostariAún no hay calificaciones
- Kel 3 TPNDocumento32 páginasKel 3 TPNTriliantari Siregar0% (1)
- DR Hariadi - Transisi RegimentDocumento19 páginasDR Hariadi - Transisi RegimentFelly NovAún no hay calificaciones
- Capaian Program TB - 2019 - KasiDocumento31 páginasCapaian Program TB - 2019 - KasiMuhtar Angga LesmanaAún no hay calificaciones
- Seminar ISTC TB Feb 2016Documento12 páginasSeminar ISTC TB Feb 2016christine nathalia loupattyAún no hay calificaciones
- Comparison of Efficiency of Electromyography and Nerve Conduction Velocity Studies in Diagnosis of Diabetic NeuropathyDocumento5 páginasComparison of Efficiency of Electromyography and Nerve Conduction Velocity Studies in Diagnosis of Diabetic NeuropathyInternational Journal of Innovative Science and Research TechnologyAún no hay calificaciones
- Aloritma Terapi KandidiasisDocumento4 páginasAloritma Terapi KandidiasisMaemah TabriziAún no hay calificaciones
- Jurnal Gula Darah SewaktuDocumento9 páginasJurnal Gula Darah SewaktuIndra TeamRiotAún no hay calificaciones
- Dr. Dwi Sunarjadi, MKM Dr. Melania Dessy Savitri Dr. Dwi Sunarjadi, MKM Dr. Melania Dessy SavitriDocumento1 páginaDr. Dwi Sunarjadi, MKM Dr. Melania Dessy Savitri Dr. Dwi Sunarjadi, MKM Dr. Melania Dessy SavitriMelania Savitri100% (1)
- Congenital AnomaliDocumento59 páginasCongenital AnomaliFaqih Bawazir SAún no hay calificaciones
- Lembar Balik Keswa Final PDFDocumento28 páginasLembar Balik Keswa Final PDFDesy Putri CahyaniAún no hay calificaciones
- DEPKES RI NEW Pedoman Nasional Penanggulangan TBC 2011Documento110 páginasDEPKES RI NEW Pedoman Nasional Penanggulangan TBC 2011familyman8091% (11)
- TB-DM Di Fasyankes100615Documento38 páginasTB-DM Di Fasyankes100615david wyanto100% (1)
- Permintaan Pemeriksaan LaboratoriumDocumento1 páginaPermintaan Pemeriksaan LaboratoriumSMC KRIAún no hay calificaciones
- BHP IcuDocumento1 páginaBHP IcuSyamsul FahmiAún no hay calificaciones
- Dr. Bambang Pujo Semedi, SP An - Antibiotics in Critically Ill E4ED FinalDocumento46 páginasDr. Bambang Pujo Semedi, SP An - Antibiotics in Critically Ill E4ED FinalcittaarunikaAún no hay calificaciones
- APT Test (Fetal Hemoglobin)Documento11 páginasAPT Test (Fetal Hemoglobin)Diovic TanAún no hay calificaciones
- Perbandingan Naïve Bayes Dan Certainty Factor Pada Sistem Pakar Untuk Mendiagnosa Dini Penyakit GlaukomaDocumento9 páginasPerbandingan Naïve Bayes Dan Certainty Factor Pada Sistem Pakar Untuk Mendiagnosa Dini Penyakit GlaukomaJurnal JTIK (Jurnal Teknologi Informasi dan Komunikasi)Aún no hay calificaciones
- Pengenceran InjeksiDocumento6 páginasPengenceran InjeksiMaria Wiji PangestuAún no hay calificaciones
- Standar Operasional Prosedur Kids Amp Baby SpaDocumento34 páginasStandar Operasional Prosedur Kids Amp Baby SpaFegi mentari putrierlinaAún no hay calificaciones
- Contoh Jurnal K3 PDFDocumento10 páginasContoh Jurnal K3 PDFwendy weyAún no hay calificaciones
- Analisa SWOT Usaha Peternakan Ayam Ras PetelurDocumento9 páginasAnalisa SWOT Usaha Peternakan Ayam Ras PetelurPrawiro Indro BhaktiAún no hay calificaciones
- Diabetic Kidney Disease (DKD)Documento39 páginasDiabetic Kidney Disease (DKD)monpyitharAún no hay calificaciones
- Soal Praktek-EBM-THTKL-Daniel BramantyoDocumento20 páginasSoal Praktek-EBM-THTKL-Daniel BramantyoDaniel BramantyoAún no hay calificaciones
- TB Paru FK UncenDocumento66 páginasTB Paru FK UncenAndira Trianingrum TukanAún no hay calificaciones
- Tabel ICD 10 English Indonesia LengkapDocumento432 páginasTabel ICD 10 English Indonesia LengkaptwindaAún no hay calificaciones
- Patofisiologi HematuriaDocumento10 páginasPatofisiologi HematuriaNurunSalamanAún no hay calificaciones
- Form Monitoring Suhu Kulkas Fix 2Documento2 páginasForm Monitoring Suhu Kulkas Fix 2Farah Maestri DianiAún no hay calificaciones
- Kasus DM PDFDocumento22 páginasKasus DM PDFVidia AsriyantiAún no hay calificaciones
- Form Hasil Lab Nilai NormalDocumento4 páginasForm Hasil Lab Nilai NormalreniAún no hay calificaciones
- Nilai Normal LabDocumento18 páginasNilai Normal LabTata SalimAún no hay calificaciones
- Analisa SemenDocumento50 páginasAnalisa SemenwiwinAún no hay calificaciones
- Tuberkulosis (Batuk Darah) : Bagaimana Pengobatannya?Documento2 páginasTuberkulosis (Batuk Darah) : Bagaimana Pengobatannya?Wildan'z CreedAún no hay calificaciones
- Tensimeter - Erkameter EDocumento8 páginasTensimeter - Erkameter EeryAún no hay calificaciones
- Pedoman Nasional Penanggulangan TB Edisi 2 - 2007 - 2 PDFDocumento168 páginasPedoman Nasional Penanggulangan TB Edisi 2 - 2007 - 2 PDFPicha Luph PinkAún no hay calificaciones
- Resusitasi Jantung Paru Berkualitas: Dr. Ichwan Zuanto 3 FEBRUARI 2018 Rsia Setya BhaktiDocumento12 páginasResusitasi Jantung Paru Berkualitas: Dr. Ichwan Zuanto 3 FEBRUARI 2018 Rsia Setya BhaktiIchwan Zuanto SjamanAún no hay calificaciones
- Indeks Stres OksidatifDocumento9 páginasIndeks Stres OksidatifAnindya Wisastra Inggas AriawanAún no hay calificaciones
- Kuliah Kegawat Daruratan Respirasi (Dr. Yusup) 06.11.2013Documento76 páginasKuliah Kegawat Daruratan Respirasi (Dr. Yusup) 06.11.2013Ilham RamadhanAún no hay calificaciones
- Introp 1Documento5 páginasIntrop 1Rima RaisyiahAún no hay calificaciones
- Jurnal Meningitis TBDocumento5 páginasJurnal Meningitis TBPutri KartikaAún no hay calificaciones
- Peptostreptococcus Micros: Detection of DNA in Clinical Samples by PCRDocumento6 páginasPeptostreptococcus Micros: Detection of DNA in Clinical Samples by PCRjorgeAún no hay calificaciones
- And Evaluation of PCR For Diagnosis Of: Bordetella Parapertussis Pertussis BordetellaDocumento6 páginasAnd Evaluation of PCR For Diagnosis Of: Bordetella Parapertussis Pertussis BordetellaAsri RachmawatiAún no hay calificaciones
- Faring It IsDocumento8 páginasFaring It IsMuhammad sukronAún no hay calificaciones
- 1 BavejaDocumento9 páginas1 BavejaIJAMAún no hay calificaciones
- Genexpert For Diagnosis of Tubercular Meningitis: Clinical BriefDocumento3 páginasGenexpert For Diagnosis of Tubercular Meningitis: Clinical BriefYas MiineAún no hay calificaciones
- Carraro 2013 RSBMTV 46 N 2 P 161Documento5 páginasCarraro 2013 RSBMTV 46 N 2 P 161Emerson CarraroAún no hay calificaciones
- s10 PDFDocumento6 páginass10 PDFMARTIN FRANKLIN HUAYANCA HUANCAHUAREAún no hay calificaciones
- Penelitian AbstraktifDocumento9 páginasPenelitian AbstraktifYondi Piter PapulungAún no hay calificaciones
- Genexpert - On Body Fluid SpecimensDocumento4 páginasGenexpert - On Body Fluid Specimensramo G.Aún no hay calificaciones
- NMM N NNNNNNNNDocumento8 páginasNMM N NNNNNNNNKapil JhajhariaAún no hay calificaciones
- Application of PCR Technique Research PPRDocumento9 páginasApplication of PCR Technique Research PPRshiza habibAún no hay calificaciones
- ResistenciaDocumento12 páginasResistenciapaoandrealm123Aún no hay calificaciones
- Difficulties With The Implemented Xpert MTBRIF For Determining DiagnosisDocumento5 páginasDifficulties With The Implemented Xpert MTBRIF For Determining DiagnosisParluhutan DolliAún no hay calificaciones
- Diagnostic Accuracy of Xpert MTB/RIF On Bronchoscopy Specimens in Patients With Suspected Pulmonary TuberculosisDocumento6 páginasDiagnostic Accuracy of Xpert MTB/RIF On Bronchoscopy Specimens in Patients With Suspected Pulmonary TuberculosisMARTIN FRANKLIN HUAYANCA HUANCAHUAREAún no hay calificaciones
- Atlas RadiologiDocumento22 páginasAtlas RadiologiLorinsya OllinAún no hay calificaciones
- Journal Faringitis PDFDocumento8 páginasJournal Faringitis PDFGamaHariandaAún no hay calificaciones
- Glaucoma Medical StudentDocumento6 páginasGlaucoma Medical StudentLorinsya OllinAún no hay calificaciones
- 6 GlaucomaDocumento50 páginas6 GlaucomaKartika RezkyAún no hay calificaciones
- GlaucomeDocumento15 páginasGlaucomeLorinsya OllinAún no hay calificaciones
- A Critical Appreciation of Ode To NightingaleDocumento3 páginasA Critical Appreciation of Ode To NightingaleBaloch Karawan100% (2)
- Border Collie Training GuidelinesDocumento12 páginasBorder Collie Training GuidelinespsmanasseAún no hay calificaciones
- Marine Trans Owners Manual 1016313 RevH 0116 CDDocumento200 páginasMarine Trans Owners Manual 1016313 RevH 0116 CDMarco Aurelio BarbosaAún no hay calificaciones
- ArticleDocumento5 páginasArticleJordi Sumoy PifarréAún no hay calificaciones
- READING 4 UNIT 8 Crime-Nurse Jorge MonarDocumento3 páginasREADING 4 UNIT 8 Crime-Nurse Jorge MonarJORGE ALEXANDER MONAR BARRAGANAún no hay calificaciones
- DX340LC: Crawler ExcavatorDocumento20 páginasDX340LC: Crawler ExcavatorFeristha Meriani TabitaAún no hay calificaciones
- Comparative Pharmacology For AnesthetistDocumento162 páginasComparative Pharmacology For AnesthetistGayatri PalacherlaAún no hay calificaciones
- Minyak Atsiri Sereh WangiDocumento4 páginasMinyak Atsiri Sereh Wangicindy paraditha kasandraAún no hay calificaciones
- Tamilnadu Shop and Establishment ActDocumento6 páginasTamilnadu Shop and Establishment ActShiny VargheesAún no hay calificaciones
- Scope: Procter and GambleDocumento30 páginasScope: Procter and GambleIrshad AhamedAún no hay calificaciones
- Funding HR2 Coalition LetterDocumento3 páginasFunding HR2 Coalition LetterFox NewsAún no hay calificaciones
- Wisconsin Humane Society To Acquire Kenosha's Safe Harbor Humane Society - Press ReleaseDocumento3 páginasWisconsin Humane Society To Acquire Kenosha's Safe Harbor Humane Society - Press ReleaseTMJ4 NewsAún no hay calificaciones
- Inverter 1 KW ManualDocumento44 páginasInverter 1 KW ManualLeonardoAún no hay calificaciones
- Interviewing Skill Workshop (KAU)Documento54 páginasInterviewing Skill Workshop (KAU)DrKomal KhalidAún no hay calificaciones
- Mixed Topic Revision 4Documento18 páginasMixed Topic Revision 4YaakkwAún no hay calificaciones
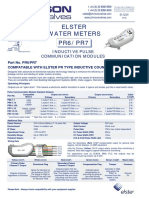
- Data Sheet No. 01.12.01 - PR6 - 7 Inductive Pulse ModuleDocumento1 páginaData Sheet No. 01.12.01 - PR6 - 7 Inductive Pulse ModuleThaynar BarbosaAún no hay calificaciones
- Registration Statement (For Single Proprietor)Documento2 páginasRegistration Statement (For Single Proprietor)Sherwin SalanayAún no hay calificaciones
- Hope Hospital Self Assessment ToolkitDocumento120 páginasHope Hospital Self Assessment Toolkitcxz4321Aún no hay calificaciones
- Terminologi AnatomiaDocumento49 páginasTerminologi AnatomiaLuluk QurrataAún no hay calificaciones
- Soil SSCDocumento11 páginasSoil SSCvkjha623477Aún no hay calificaciones
- Royal British College IncDocumento5 páginasRoyal British College IncLester MojadoAún no hay calificaciones
- Brief RESUME EmailDocumento4 páginasBrief RESUME Emailranjit_kadalg2011Aún no hay calificaciones
- Employee Final SettlementDocumento1 páginaEmployee Final SettlementZeeshan Mirza0% (1)
- Heat Transfer ExampleDocumento4 páginasHeat Transfer Examplekero_the_heroAún no hay calificaciones
- Inlet Manifold Pressure - Test: Testing and AdjustingDocumento2 páginasInlet Manifold Pressure - Test: Testing and AdjustingAbdoulaye Boua BERTHEAún no hay calificaciones
- Standards Spec Brochure ME WEBDocumento44 páginasStandards Spec Brochure ME WEBReza TambaAún no hay calificaciones
- Project Management A Technicians Guide Staples TOCDocumento5 páginasProject Management A Technicians Guide Staples TOCAnonymous NwnJNO0% (3)
- NG Teng Fong Discharge DocumentsDocumento14 páginasNG Teng Fong Discharge DocumentsAnonymous yGwMIPJRawAún no hay calificaciones
- Report On Analysis of TSF Water Samples Using Cyanide PhotometerDocumento4 páginasReport On Analysis of TSF Water Samples Using Cyanide PhotometerEleazar DequiñaAún no hay calificaciones
- Conference Version of SB 1Documento486 páginasConference Version of SB 1Paul MastersAún no hay calificaciones
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDCalificación: 5 de 5 estrellas5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityCalificación: 4 de 5 estrellas4/5 (28)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionCalificación: 4 de 5 estrellas4/5 (404)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeCalificación: 2 de 5 estrellas2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedCalificación: 5 de 5 estrellas5/5 (81)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- Gut: the new and revised Sunday Times bestsellerDe EverandGut: the new and revised Sunday Times bestsellerCalificación: 4 de 5 estrellas4/5 (393)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsCalificación: 5 de 5 estrellas5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisCalificación: 4.5 de 5 estrellas4.5/5 (42)
- The Obesity Code: Unlocking the Secrets of Weight LossDe EverandThe Obesity Code: Unlocking the Secrets of Weight LossCalificación: 4 de 5 estrellas4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAún no hay calificaciones
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsCalificación: 3.5 de 5 estrellas3.5/5 (3)
- The Comfort of Crows: A Backyard YearDe EverandThe Comfort of Crows: A Backyard YearCalificación: 4.5 de 5 estrellas4.5/5 (23)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDe EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningCalificación: 4 de 5 estrellas4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Aún no hay calificaciones
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityCalificación: 4 de 5 estrellas4/5 (4)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisCalificación: 3.5 de 5 estrellas3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryCalificación: 4 de 5 estrellas4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeCalificación: 4.5 de 5 estrellas4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Calificación: 4.5 de 5 estrellas4.5/5 (110)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisCalificación: 4 de 5 estrellas4/5 (1)
- The Marshmallow Test: Mastering Self-ControlDe EverandThe Marshmallow Test: Mastering Self-ControlCalificación: 4.5 de 5 estrellas4.5/5 (58)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsCalificación: 4.5 de 5 estrellas4.5/5 (170)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDe EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingCalificación: 4 de 5 estrellas4/5 (1138)