Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Urinary Diversion Following Cystectomy: EAU Update Series
Cargado por
moetazDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Urinary Diversion Following Cystectomy: EAU Update Series
Cargado por
moetazCopyright:
Formatos disponibles
EAU
Update Series
EAU Update Series 3 (2005) 129137
Urinary Diversion Following Cystectomy
Udo Nagele*, Karl-Dietrich Sievert, Axel S. Merseburger,
Aristotelis G. Anastasiadis, Arnulf Stenzl
Department of Urology, University of Tuebingen, Hoppe-Seyler-Str. 3, Tuebingen 72076, Germany
Abstract
Urinary diversion is an essential component of the surgical procedure after cystectomy. Replacement with an
orthotopic ileal neobladder should be the first choice if external urethral sphincter sparing surgery is possible,
offering good long-term function, quality of life and patients acceptance with few complications.
The possible use of a variety of alternative intestinal segments widen the horizon of the reconstructive surgeon,
allowing him or her to be prepared for unusual cases.
Contraindications for orthotopic neobladder reconstruction include tumour location, reduced renal, liver,
intestinal function, intellectual ability and physical handicaps.
It is therefore important to custom tailor the appropriate mode of diversion for individual patients with a variety of
options available, including ureterocutaneous stomas, intestinal conduits and continent catheterizable reservoirs and
orthotopic neobladders. All these techniques require detailed knowledge of the possible metabolic problems
encountered by using gastrointestinal segments and how they react in contact with urine. Modern surgical
techniques such as nerve sparing surgery have the ability to preserve postoperative continence with voluntarily
micturition as well as sexual function. In addition, preliminary experimental data hold great promise that the off
shelf bladder substitute may become a technique of choice in the future, avoiding common problems encountered
using current technqiues.
# 2005 Elsevier B.V. All rights reserved.
Keywords: Urinary diversion; Bladder substitute; Conduit; Neobladder; Continent catheterizable reservoir
1. History
In 1852, Simon first reported a urinary diversion
using intestinal segments [26]. In 1888, the first orthotopic diversion in an animal study was performed by
Tizzoni and Foggi [39]. Coffey introduced uretreosigmoidostomy in 1911, which became the standard technique, although the ileal conduit was reported by Zaayer
in the same year [22]. It took another 40 years, in which
many patients died because of hyperchloremic acidosis
(suffered by 80% of all patients with ureterosigmoidostomy) until Bricker established the ileal conduit as a
diversion of first choice in 1950 [5].
* Corresponding author. Tel. +49 7071 2986615;
Fax: +49 7071 2985092.
E-mail address: Udo.Nagele@med.uni-tuebingen.de (U. Nagele).
The first use of detubularized reconfigured ileal
segments in bladder augmentation as a low pressure
reservoir was described by Goodwin 1959. This technique was able to increase bladder capacity with
minimal pressure peaks [10,11].
Since then, many different continent catheterizable
reservoirs and neobladders were introduced. However,
urologists have not been able to overcome problems
related to the use of bowel such as resorption of urinary
contents, mucus production, and abnormal peristalsis
instead of detrusor-like contractions. In many centers
of excellence worldwide, a continent reservoir, preferably connected to the urethra is the urinary diversion
of choice today. For the creation of such reservoirs,
ileal segments are preferred, because of their lower
intraluminal pressure peaks, and their ease of surgical
handling.
1570-9124/$ see front matter # 2005 Elsevier B.V. All rights reserved.
doi:10.1016/j.euus.2005.07.003
130
U. Nagele et al. / EAU Update Series 3 (2005) 129137
2. Urinary reservoirs - which
gastrointestinal segment?
2.1. Stomach
Metabolic acidosis and its related adverse effects are
seen with ileal and colonic diversions, especially
among younger patients. Gastric reservoirs have been
recommended by several authors with a variety of
outcomes [14,21]. Short term follow-up demonstrated
favourable results [24,27] with reduced mucus production and prevention of hyperchloremic acidosis by the
acidic milieu of the urine. To overcome the disadvantages of haematuria-dysuria syndrome, a so-called
composite urinary reservoir, combining gastric
and ileal or colonic segments were favoured [4,6].
The idea is to combine a segment with proton secretion
with an absorbing one. Therefore, metabolic acidosis
and its sequelae, which are inherent to ileal and colonic
segments, can be prevented. Furthermore, composite
reservoirs may be an option in patients with renal
insufficiency, which is a relative contraindication to
continent urinary diversion. However, our knowledge
of ion interactions of the gastric and lower intestinal
segments remains limited [29].
2.2. Ileum
The authors of the largest series of continent urinary
diversion prefer a re-configured low-pressure ileal reservoir, according to the principle of the Goodwin cup
patch technique [28,37]. Good medium term results with
acceptable ileum-related morbidity continue to be
reported among those using the ileal low pressure
reservoir [37]. The ileum is important for vitamin B
12 and bile acid absorption. Resection of up to 60 cm
does appear to cause significant side-effects regarding
absorption, if the terminal ileum is preserved. Fat-soluble vitamin malabsorbtion, biliary salt loss and
increased oxalate absorption are of major concern, if
over 100 cm of ileum are resected, but in the majority of
cases a 4060 cm long segment is adequate.
Using ileum as urinary diversion causes a impairment
in renal acid and salt regulation. Hyperkalaemic, hypochloraemic acidosis, and osteoporosis and osteomalacia
can occur in the long term. Mild acidosis is common
postoperatively and can be controlled with administration of oral sodium bicarbonate. The absorptive capacity
of the bowel segment decreases 8-fold with time, resulting in less re-absorption and metabolic problems [15].
2.3. Ileocoecal valve
The ileocaecal valve is important for controlling the
transport of ileal contents into the colon. Resection of
the valve with the terminal ileum may lead to rapid
bowel propulsion, resulting in soft stools, diarrhoea
and malabsorbtion [3].
In a group of patients with a Mainz pouch, using the
ileocaecal valve and terminal ileum, 32% and 11% of
patients demonstrated decreased vitamin B12 and folic
acid levels respectively. More than 30% of this cohort
had a metabolic acidosis, in addition to an increased
risk of developing renal, and/or gallbladder stones [37].
2.4. Colon
The sigmoid colon is redundant in many patients.
With its large diameter compared to the small bowel and
its relative mobility, it can easily be brought down to the
urethra and allows a relatively easy anti-reflux ureteral
implantation. Vitamin B12 malabsorbtion and biliary salt
loss are minor compared to the terminal ileum. Despite
these advantages and even after detubularization and
reconfiguration, patients with a sigmoid colon neobladder have a more frequent night-time voiding pattern.
This may be due to enhanced peristaltic activity and
higher pressure of the large bowel [12]. Initially reported
results suggest a high acceptance rates by patients, but
long-term follow-up, especially regarding the upper
urinary tract is warranted and the technique requires
further evaluation [9].
2.5. Appendix
The appendix is routinely removed during anterior
exenteration in some centres. However, it might be
quite useful to create a catheterizable nipple for a
continent cutaneous diversion. Some surgeons use
the appendix as the intestinal segment of choice in
forming a continence mechanism [8]. Surprisingly, a
continent ileocaecal diversion can be achieved with an
unaltered appendix conduit [7,25] and obviating more
complicated tunnelling techniques. Whenever the
appendix is not present or is inadequate, transversely
tubularized ileal segments by using the Monti principle
may be used as an alternative to create the efferent
continence mechanism of urinary pouches [38].
3. Preparation of the ureters for urinary
diversion
Irrespective of the type of urinary diversion used,
postoperative ureteral anastomotic stricture is a recognised complication. Ischemia of the distal ureter is
avoidable, by taking note of its vascular supply with its
common variations [32] and preserving the periureteral
adventitial tissue - even below the level of ureteral
dissection. This reduces the risk of ischemia and
strictures. The left ureter should be moved across
U. Nagele et al. / EAU Update Series 3 (2005) 129137
131
4.2. Ileal and colonic conduits
In contrast to a cutaneous stoma, the ileal conduit
has no risk of stenosis at the skin level, because of the
short gut segment interposed between the skin and the
ureters. Usually, a 1012 cm segment of terminal ileum
approximately 20 cm proximal of the ileocecal valve is
used. For a low pressure diversion it is important to pay
caution to a short, straight conduit without kinking and
a sufficient wide fascial opening (usually x-type incision). The segment is used in an isoperistaltic fashion.
Ureteric implantation can be carried out in three
ways:
Fig. 1. Anatomical specimen of a female pelvis outlining the arterial
vascularization of the distal ureter. The arrow depicts a common iliac
arterial branch which, apart from the vesical arteries, is the only other major
supply of the distal ureter.
the retroperitoneum above the level of the inferior
mesenteric artery to the contralateral retroperitoneal
space in order to maximise length and avoid unnecessary kinking (Fig. 1).
A: The Bricker and Nesbit technique: Both ureters are
implanted individually in an end-to-side technique
[5].
B: Wallace 66 parallel oriented ureters; both spatulated at the distal end for a distance slightly longer
than the diameter of the ileum. The posterior plate
is sutured and anastomosed in a side-to-end fashion
to the ileal stump [41] (Fig. 5).
C: Wallace 69 - end to end oriented ureters; both
spatulated and sutured to a ureteral plate anastomosed in a side-to-end fashion to the ileal stump.
4. Incontinent urinary diversion
4.1. (Transuretero-) Ureterocutaneostomy
Cutaneous ureterostomy is the least desirable form of
urinary diversion, but despite its disadvantages it is a
valid option in selected cases, e.g. after palliative
cystectomy in elderly frail patients, in patients with
incurable malignancies or pelvic complications, as
(temporary) diversion in situations when gastrointestinal diversion is not possible or whenever the bladder
needs to be diverted because of fistulae or haemorrhage.
The ureters are carefully mobilised to the bladder,
with minimal disruption to their blood supply, ligated
and divided. After creating a retroperitoneal tunnel
cranial to the inferior mesenteric artery, the less dilated
left or right ureter is transposed to the contralateral
side. A V- or U- shaped skin incision is made in the
skin, and a track is developed through the abdominal
wall in the most direct line. The ureter with the largest
diameter is pulled through the track without tension
and angulations and spatulated. A 4/0 or 5/0 absorbable
suture is placed through the apex of the skin flap into
the apex of the ureteral spatulation.
The dilated ureter is then incised longitudinally for
approximately 2 cm and anastomosed to the other
ureter without any tension, using and end-to-side configuration to complete the transureteroureterostomy.
An omental flap can be used to secure both anastomoses and the abdominal tunnel.
Of greatest importance is the position of the stoma.
Improper preoperative selection for the stoma location
causes urinary leakage underneath the stomal plate
because of skin folds or interference with the waist
belt. The location should be above or below the waistband and not too close to the umbilicus, the edge of the
rectus muscle, a bony prominence or a scar, and must
be tested with the patient and marked pre-operatively.
For decades the ileal conduit has been the procedure
of choice for urinary diversion. It remains a valid
option or even a better alternative than a continent
urinary diversion in many cases. The short gut segment
limits metabolic changes and is therefore recommended in patients with renal insufficiency (creatinine > 2 mg/dl) or severe hepatic dysfunction, and when
a postoperative radiation might be necessary. Contraindications, among others, are short bowel syndrome,
radiation disease of the terminal ileum and ascites. In
cases of severe radiation disease in the pelvis, a
transverse colon conduit may be an alternative option.
5. Continent urinary diversion
5.1. Reservoir construction
The reservoir is a compromise between good capacity, low pressure storage and metabolic issues, partially caused by the re-absorptive surface of the pouch.
132
U. Nagele et al. / EAU Update Series 3 (2005) 129137
A spherical reservoir stands for maximum volume
and minimum re-absorptive surface. To minimize pressure peaks caused by coordinated bowel contractions,
detubularization of the used bowel segment is mandatory. In addition, according to Laplaces law (pressure = tension/radius) a spherical reservoir has a low endfilling pressure with maximum radius. Despite the
mathematical advantages of an M or a W folded
reservoir, we prefer a cross folded U [11] because of
its simplicity, and its documented low intraluminal
pressures due to the so called wind chamber effect.
5.2. Continent catheterizable reservoir
A catheterizable reservoir is indicated whenever
external urethral sphincter sparing surgery is not possible, or in patients with urethral malformations, spinal
injuries or other complex neurological defects. Patient
compliance is of outmost importance because of the
need for regular intermittent self-catheterisation. However, due to the lack of an overflow valve there is a
certain danger that catheterisation difficulties may lead
to perforation and even bladder rupture, if regular
reservoir evacuation is delayed. Several different continence mechanisms have been described. Nowadays
mostly the appendix, tapered ileum, or intussucepted
ileal nipples are used.
The catheterizable stoma is the main source of problems and complications in these patients. The reported
re-operation rate varies from 22% to 49 % [30] with
stomal stenosis ranging from 4% to 15% [23,37], an
overall incontinence rate of 3,2% [37], and ureteral
stenosis in 8% of patients [2]. Using the ileocaecal valve
and terminal ileum for a continent catheterizable reservoir carries the potential risks of diarrhoea, hyperchloraemic acidosis and malabsorbtion. Metabolic and
clinical work-up, with regular check-up of serum parameters for inflammation, renal and hepatic function,
metabolic acidosis, electrolyte disorders and hydration
is important. Adequate oral sodium bicarbonate supplementation is often necessary.
5.3. Orthotopic neobladder
The orthotopic neobladder continues to gain popularity. Quality of life issues including physical integrity, near normal voiding and continence are important
factors that many patients consider important, after
cure from their cancer. Contraindications are listed in
Table 1. The patients continence and external urethral
sphincter must be intact pre-operatively. To rule out
cancer infiltration and possibly positive margins, preoperative cystoscopic biopsies of the bladder neck/
prostatic urethra as well as intraoperative frozen sections of the resected margins are mandatory.
Table 1
General contraindications to continent urinary diversions
1.
2.
3.
4.
5.
6.
Chronic renal failure with serum creatinine exceeding 2 mg/dl
without acute hydronephrosis. In doubtful cases percutaneous
drainage is indicated preoperatively in an attempt to normalise
renal function.
Severe hepatic failure.
Compromised intestinal function especially caused by radiation
or inflammatory bowel disease.
The presence of histologically proven cancer at the prostatic
apex (male) or bladder neck (female)
Lack of patient motivation and/or intellect to follow a strict
postoperative voiding regime, to accept possible incontinence
(mainly nocturnal) in the early post-operative phase and
sometimes in the long-term.
Pelvic floor disorders such as detrusor sphincter dis-synergia
or neurourological diseases.
From the oncological standpoint there are no significant differences in cancer-specific survival between
ileal conduits and contemporary bladder substitutes
[42]. The low local tumor recurrence rate of 11%
and the recurrence rate of 25% in the urethra support
the trend towards orthotopic urinary diversion [13,18]
and demonstrate that safe patient selection for an
orthotopic neobladder is possible.
After decades of searching for the ideal gastrointestinal segment, many surgeons favour nowadays
the ileal neobladder, because of easy harvesting and
handling as well as low intraluminal pressures [15,36].
Approximately 40 cm of ileum are necessary to create
an adequate volume reservoir. Key points with every
neobladder are the connections cranially to the ureters
and caudally to the urethra.
5.3.1. Afferent anastomosis: Reflux prevention how
and when to do it
5.3.1.1. Technique of reflux prevention
5.3.1.2. Camey - Le Duc. A channel is created on the
posterior intestinal wall by incising the mucosa longitudinally for 33.5 cm all the way to the muscularis.
At the proximal end, the obliquely cut the ureter
penetrates into the lumen of the neobladder and is
fixed at the distal end of the channel. The Camey-Le
Duc ureteroileal anastomosis must be considered historical now. It has been widely abandoned due to its
high complication rate.
5.3.1.3. Intussusceptive ileal nipple.The Hemi-Kock
type of intussusceptive ileal nipple with both ureters
implanted at the proximal end of the nipple creates a
good intraluminal valve, but there is considerable risk
of long-term obstruction (Fig. 2).
5.3.1.4. Serosa-lined extramural tunnel implantation (Abol-Enein, Stein). After detubularization, the
ileum it is arranges as a W, M, or double-folded
U. Nagele et al. / EAU Update Series 3 (2005) 129137
133
Fig. 2. The Herni-Kock intussusceptive ileal nipple.
U. The serosa is anastomosed approximately 2 cm
from the medial edges of the cut flaps on each wing
with running sutures, thus forming two troughs. The
spatulated and joined ureters or a tapered 1012 cm
segment of ileum to which the ureters are anastomosed
proximally, placed into the trough and anastomosed to
the bowel mucosa at the distal end (Fig. 3). The tunnel
is closed above the ureters by a running suture forming
an extramural serosa lined tunnel which serves as a
volume dependent antireflux mechanism.
5.3.1.5. Isoperistaltic tubular limb. Ureters are
implanted in an end-to-side fashion into the proximal
end of a 15 to 20 cm long afferent tubular segment,
where antireflux protection is achieved by coordinated
peristalsis [19].
Fig. 4. Preparation of the ileal segment.
continence range between 87% and 98%, and 72% and
95% respectively [1,16,17,20,40]. Incomplete bladder
emptying with the need to perform intermittent self
catheterisation is seen in up to 15% of females [35] and
in 4% of male patients [13].
Precise preparation of the urethra is essential. Urethro-ileal anastomosis is performed at the most caudal
point of the neobladder (determined digitally), either
by leaving a small opening at the end of the ventral
suture line forming a spout (our preferred technique in
male patients) (Fig. 5) or by making a 0.5 cm opening
into the ileal wall close to the mesentery (female
patients). It is important in female patients not to
5.3.2. Efferent anastomosis
Good voiding function is mandatory to achieve good
quality of life with an orthotopic neobladder substitution. In recently reported series, daytime and night time
Fig. 3. Serosa-lined extramural tunnel implantation with tapered ileum.
Fig. 5. Wallace 66 ureteral anastomosis.
134
U. Nagele et al. / EAU Update Series 3 (2005) 129137
Fig. 6. U-shaped isolated ileum segment with ileal trough.
Fig. 8. Reconstructed neobladder with spout shaped afferent opening.
use the corner of the pouch, as this may lead to kinking
later on and difficulties with voiding.
5.3.3. Neobladder
The neobladder described here appears to be economic with regards to bowel length utilisation, efficient in reflux protection of the upper urinary tract, and
less time consuming than other methods. The left ureter
is transposed as mentioned above. Both ureters are
spatulated and conjoined to a ureteral plate.
40 cm of terminal ileum (Fig. 4) are isolated and
the ileal tube is arranged as a U. Starting 23 cm
from the endings, a running seromuscular suture of
approximately 10 cm at the mesenterial insertion
forms a so called ileal trough (Fig. 6). The ileum
is opened at its antimesenteric border in its entire
length. The conjoined ureters are placed into the ileal
trough, sutured to the distal end of the trough and
buried by closing the ileal flaps over both ureters.
Two mono-J stents are placed into the ureters, the
ileal bladder is completed with a running suture line,
cross folded, and closed on the left side. The mono-J
stents are brought through the side wall of the neobladder (Fig. 7).
In male patients the right side is closed leaving a
small opening at the distal end where the bladder is
anastomosed with the urethra with 6 stay sutures over a
2022 Fr catheter (Figs. 8 and 9).
In female patients the right side is closed completely and a small separate opening serves as the neobladder neck where the urethra is anastomosed with 6
sutures.
At the end of the procedure, a J-shaped omentum
flap is brought down and led around the bottom part of
the pouch. Alternatively, portions of the ileal bladder
are fixed to the pelvic wall, obstruction caused by ileal
Fig. 7. Detubularised neobladder with afferent anastomosis, during crossfolding.
Fig. 9. Neobladder in situ.
U. Nagele et al. / EAU Update Series 3 (2005) 129137
135
Table 2
Advantages of the orthotopic technique described
1.
2.
3.
4.
Economic with regards to bowel length utilised.
Cross folded U (Goodwins cup-patch principle) combines low
pressure with simplicity and short suture lines.
Serosa lined extramural tunnel implantation achieves an antireflux
mechanism with volume depended closure and has a low
stricture rate.
Wallace implantation in the middle of the posterior neobladder
wall facilitates endourological, especially ureteroscopic
procedures and follow up if necessary.
folds and a pouchocele = descent can thus be
avoided in addition to securing the urethrointestinal
junction [31,33]. Advantages, postoperative follow-up
and illustrations of the technique are shown in Table 2
and Fig. 10, respectively.
5.4. Uretero (ileo-) sigmoidostomy
Ureterosigmoidostomy, though still performed, has
been largely replaced by other techniques because of
metabolic acidosis, renal failure, and tumourigenesis
typically with adenocarcinoma at the site of the anastomosis years after implantation [9] (Fig. 11). By
detubularisation of the sigmoid, ileal interposition,
and antireflux implantation of the ureters, some of
the complications of this technique can be reduced.
Major disadvantages are bacterial reflux causing pyelonephritis and stenosis of the ureteral implantation,
which causes considerable renal damage, leading to reoperation. In contrast to the ileal neobladder, reabsorbtion and metabolic problems are higher, result in an
increased need for permanent sodium bicarbonate
substitution and, interference with future systemic
chemotherapy.
Fig. 10. Bladder replacement: postoperative management.
Fig. 11. Ureteroileorectosigmoidostomy.
6. Conclusion
In the 21st century, in both male and female patients
with bladder cancer requiring cystectomy, an orthotopic bladder substitution should be the first choice of
urinary diversion whenever the urethra can be spared
safely, without compromising the oncological aim of
the procedure. Refinements of surgical techniques such
as autonomic nerve preservation and improved afferent
(ureteral) and efferent (urethral) anastomoses result in
excellent functional outcomes and improved quality of
life. Understanding the structural transformation of the
ileal mucosa and metabolic changes as well as the
functional principle of the neobladder results in a
structured follow-up, and avoids postoperative complications. Other types of continent and incontinent
urinary diversion remain valid and time-tested options,
whenever an orthotopic bladder replacement is not
possible. Using careful selection criteria, the type of
136
U. Nagele et al. / EAU Update Series 3 (2005) 129137
urinary diversion used does not appear to impact on
cancer specific survival.
Future concepts, including tissue engineering techniques, show promising results in the laboratory. This
is however outside the scope of the current article,
and several hurdles need to be overcome before the
first off-the-shelf neobladder can be used in our
patients.
References
[1] Abol-Enein H, Ghoneim MA. Functional results of orthotopic ileal
neobladder with serous-lined extramural ureteral reimplantation:
experience with 450 patients. J Urol 2001;165:142732.
[2] Albers P. Urinary diversion after cystectomy. Urologe A 2004;43:997
1009 quiz 1010.
[3] Ashken MH. An appliance-free ileocaecal urinary diversion: preliminary communication. Br J Urol 1974;46:6318.
[4] Austin PF, DeLeary G, Homsy YL, Persky L, Lockhart JL. Long-term
metabolic advantages of a gastrointestinal composite urinary reservoir.
J Urol 1997;158:17047 discussion 17071708.
[5] Bricker EM. Bladder substitution after pelvic evisceration. Surg Clin
North Am 1950;30:151121.
[6] Chiang PH, Huang YS, Wu WJ, Chiang CP. The gastroileal neobladder
for renal insufficiency. J Urol 1997;158:19056.
[7] English SF, Pisters LL, McGuire EJ. The use of the appendix as a
continent catheterizable stoma. J Urol 1998;159:7479.
[8] Gerharz EW, Kohl U, Weingartner K, Melekos MD, Bonfig R,
Riedmiller H. Complications related to different continence mechanisms in ileocecal reservoirs. J Urol 1997;158:170913.
[9] Gittes RF. Carcinogenesis in ureterosigmoidostomy. Urol Clin North
Am 1986;13:2015.
[10] Goodwin WE, Winter CC. Technique of sigmoidocystoplasty. Surg
Gynecol Obstet 1959;108:3702.
[11] Goodwin WE, Winter CC, Barker WF. Cup-patch technique of
ileocystoplasty for bladder enlargement or partial substitution. Surg
Gynecol Obstet 1959;108:2404.
[12] Grasset D, Delbos O, Muir GH, Robert M, Guiter J. Orthotopic bladder
substitution by detubularized sigmoid using a new method of neovesico-urethral anastomosis. Br J Urol 1998;81:6237.
[13] Gschwend JE. Bladder substitution. Curr Opin Urol 2003;13:
47782.
[14] Hauri D. Can gastric pouch as orthotopic bladder replacement be used
in adults? J Urol 1996;156:9315.
[15] Hautmann RE. Urinary diversion: ileal conduit to neobladder. J Urol
2003;169:83442.
[16] Hautmann RE, Simon J. Ileal neobladder and local recurrence of
bladder cancer: patterns of failure and impact on function in men. J
Urol 1999;162:19636.
[17] Kessler TM, Burkhard FC, Perimenis P, Danuser H, Thalmann GN,
Hochreiter WW, et al. Attempted nerve sparing surgery and age have a
significant effect on urinary continence and erectile function after
radical cystoprostatectomy and ileal orthotopic bladder substitution. J
Urol 2004;172:13237.
[18] Madersbacher S, Hochreiter W, Burkhard F, Thalmann GN, Danuser
H, Markwalder R, et al. Radical cystectomy for bladder cancer today
a homogeneous series without neoadjuvant therapy. J Clin Oncol
2003;21:6906.
[19] Mann F, Bollmann J. A method for making a satisfactory fistula at any
level of the gastrointestinal tract. Ann Surg 1931;93:7947.
[20] Mansson A, Henningsohn L, Steineck G, Mansson W. Neutral third
party versus treating institution for evaluating quality of life after
radical cystectomy. Eur Urol 2004;46:1959.
[21] Nguyen DH, Mitchell ME. Gastric bladder reconstruction. Urol Clin
North Am 1991;18:64957.
[22] Pannek J, Senge T. History of urinary diversion. Urol Int 1998;60:1
10.
[23] Pantuck AJ, Han KR, Perrotti M, Weiss RE, Cummings KB. Ureteroenteric anastomosis in continent urinary diversion: long-term results
and complications of direct versus nonrefluxing techniques. J Urol
2000;163:4505.
[24] Shamsa A. Gastric neobladder for treatment of tuberculosis cystitis. J
Urol 1998;159:202.
[25] Simforoosh N, Razzaghi MR, Danesh AK, Sharifi FA, Gholamrezaie
HR, Mousavi H. Continent ileocecal diversion with an unaltered in situ
appendix conduit. J Urol 1998;159:11768.
[26] Simon J. Ectopia vesicae: operation for directing the orifices of the
ureters into the rectum: temporary succes; subsequent death; autopsy.
Lancet 1852;2:56870.
[27] Singla A, Galloway N. Early experience with the use of gastric
segment in lower urinary tract reconstruction in adult patient population. Urology 1997;50:6305.
[28] Skinner DG, Stein JP, Lieskovsky G, Skinner EC, Boyd SD, Figueroa
A, et al. 25-year experience in the management of invasive bladder
cancer by radical cystectomy. Eur Urol 1998;33(Suppl 4):256.
[29] Stampfer DS, McDougal WS, McGovern FJ. The use of in bowel
urology. Metabolic and nutritional complications. Urol Clin North Am
1997;24:71522.
[30] Stein JP, Stenzl A, Esrig D, Freeman JA, Boyd SD, Lieskovsky G, et al.
Lower urinary tract reconstruction following cystectomy in women
using the Kock ileal reservoir with bilateral ureteroileal urethrostomy:
initial clinical experience. J Urol 1994;152:14048.
[31] Stenzl A, Colleselli K, Bartsch G. Update of urethra-sparing
approaches in cystectomy in women. World J Urol 1997;15:1348.
[32] Stenzl A, Hobisch A, Strasser H, Bartsch G. Ureteroileal anastomosis
in orthotopic urinary diversion: how much or how little is necessary?
Tech Urol 2001;7:18895.
[33] Stenzl A, Janetschek G, Bartsch G, Hofer C, Hartung R. Report of
experience in reconstruction of the lower urinary tract in the man and
woman. Urologe A 1994;33:914.
[35] Stenzl A, Strasser H, Hobisch A, Bartsch G. VIchoosing the right
reconstruction for your female patients. Semin Urol Oncol 2001;19:9
17.
[36] Studer UE, Danuser H, Merz VW, Springer JP, Zingg EJ. Experience
in 100 patients with an ileal low pressure bladder substitute combined
with an afferent tubular isoperistaltic segment. J Urol 1995;154:4956.
[37] Studer UE, Zingg EJ. Ileal orthotopic bladder substitutes What we
have learned from 12 years experience with 200 patients. Urol Clin
North Am 1997;24:78193.
[38] Sugarman ID, Malone PS, Terry TR, Koyle MA. Transversely tubularized ileal segments for the Mitrofanoff or Malone antegrade colonic
enema procedures: the Monti principle. Br J Urol 1998;81:2536.
[39] Tizzoni G, Foggi A. Die Wiederherstellung der Harnblase. Zentralbl
Chir 1888;15:921.
[40] Vallancien G, Abou El Fettouh H, Cathelineau X, Baumert H, Fromont
G, Guillonneau B. Cystectomy with prostate sparing for bladder
cancer in 100 patients: 10-year experience. J Urol 2002;168:24137.
[41] Wallace DM. Ureteric diversion using a conduit: a simplified technique. Br J Urol 1966;38:5227.
[42] Yossepowitch O, Dalbagni G, Golijanin D, Donat SM, Bochner BH,
Herr HW, et al. Orthotopic urinary diversion after cystectomy for
bladder cancer: implications for cancer control and patterns of disease
recurrence. J Urol 2003;169:17781.
U. Nagele et al. / EAU Update Series 3 (2005) 129137
137
CME questions
Please visit www.uroweb.org/updteseries to answer
these CME question on-line. The CME credits will
then be attributed automatically.
1. A catheterizable reservoir is not indicated:
A. if an external urethral sphincter sparing surgery
is not possible
B. in patients with urethral malformations
C. in the incompliant patient
D. in complex neurourological defects
2. Which of the following techniques of reflux prevention has been abandoned due to its high complication rates?
A. Camey-LeDuc
B. Intussusceptive ileal nipple
C. Serosa-lined extramural tunnel implatation
D. Isoperistaltic tubular limb
3. which of the following principles of reservoir construction is false?
A. A spherical reservoir stands for minimum reabsorptive surface
B. A spherical reservoir has low end-filling pressure with maximum radius
C. Pressure peaks are minimized by the use of
isoperistaltic gut segments
D. A cross folded U reservoir uses the wind
chamber effect
4. Ureterocutaneostomy is:
A. performed, when continent urinary diversion is
possible
B. used, when gastrointestinal diversion is possible
C. indicated in patients with serum creatinin
exceeding 2 mg/dl
D. not associated with the risk of stenosis at the
skin level
También podría gustarte
- The Ileoanal Pouch: A Practical Guide for Surgery, Management and TroubleshootingDe EverandThe Ileoanal Pouch: A Practical Guide for Surgery, Management and TroubleshootingJanindra WarusavitarneAún no hay calificaciones
- Los Terrybles Book TeamDocumento9 páginasLos Terrybles Book TeamWildor Herrera GuevaraAún no hay calificaciones
- Liver Transplantation For Biliary Atresia : Thomas E. Starz), M.D., Ph.D. Carlos O. Esquivel, M.D., PH.DDocumento8 páginasLiver Transplantation For Biliary Atresia : Thomas E. Starz), M.D., Ph.D. Carlos O. Esquivel, M.D., PH.DPratita Jati PermatasariAún no hay calificaciones
- Surgery For Duodenal Ulcer PDFDocumento10 páginasSurgery For Duodenal Ulcer PDFRuel P. AgustinAún no hay calificaciones
- Difficult Acute Cholecystitis: Treatment and Technical IssuesDe EverandDifficult Acute Cholecystitis: Treatment and Technical IssuesAún no hay calificaciones
- IleostomyDocumento7 páginasIleostomyPavan KumarAún no hay calificaciones
- Mainz II Surgery IllustratedDocumento25 páginasMainz II Surgery IllustratedPurvi ParikhAún no hay calificaciones
- Ileal Neobladder and Its Variants: Georgios Gakis, Arnulf StenzlDocumento9 páginasIleal Neobladder and Its Variants: Georgios Gakis, Arnulf StenzlRara Aulia IIAún no hay calificaciones
- Colecistogastrostomia-Biopsia de HigadoDocumento8 páginasColecistogastrostomia-Biopsia de HigadoWildor Herrera GuevaraAún no hay calificaciones
- Laparoscopic Cholecystectomy - StatPearls - NCBI BookshelfDocumento1 páginaLaparoscopic Cholecystectomy - StatPearls - NCBI BookshelfOmar HamwiAún no hay calificaciones
- Hepatico JDocumento4 páginasHepatico Jcharie2Aún no hay calificaciones
- Urinary DiversionDocumento44 páginasUrinary Diversionminnalesri100% (1)
- Small Nowel Emergency SurgeryDocumento8 páginasSmall Nowel Emergency SurgerySurya Nirmala DewiAún no hay calificaciones
- Pi Is 2213576614000049Documento3 páginasPi Is 2213576614000049Ditha FadhilaAún no hay calificaciones
- Remove Them Within A Week. Mainz Neobladder: Chapter 189: Supravesical Urinary DiversionDocumento1 páginaRemove Them Within A Week. Mainz Neobladder: Chapter 189: Supravesical Urinary DiversioncesaliapAún no hay calificaciones
- Basics of Intestinal Surgery: Anatomy, Pathophysiology, Instrumentation & SuturingDocumento8 páginasBasics of Intestinal Surgery: Anatomy, Pathophysiology, Instrumentation & SuturingakreditasirsurAún no hay calificaciones
- Urinary DiversionDocumento11 páginasUrinary Diversionvlad910Aún no hay calificaciones
- Argh - Ms.id.555581, DR Muhammad Zafar Mengal ArticlesDocumento4 páginasArgh - Ms.id.555581, DR Muhammad Zafar Mengal ArticlesMuhammad Zafar MengalAún no hay calificaciones
- Wormuth 2006Documento12 páginasWormuth 2006DH SiriruiAún no hay calificaciones
- DTSCH Arztebl Int-109-0617Documento7 páginasDTSCH Arztebl Int-109-0617Carlos PalaciosAún no hay calificaciones
- Oesophagocoloplasty For Corrosive Oesophageal Stricture: AbstractDocumento12 páginasOesophagocoloplasty For Corrosive Oesophageal Stricture: AbstractSpandan KadamAún no hay calificaciones
- B - Bile Duct Injuries in The Era of Laparoscopic Cholecystectomies - 2010Documento16 páginasB - Bile Duct Injuries in The Era of Laparoscopic Cholecystectomies - 2010Battousaih1Aún no hay calificaciones
- Laparoscopic Gastrointestinal SurgeryDocumento22 páginasLaparoscopic Gastrointestinal SurgeryRoxana BoloagaAún no hay calificaciones
- CholecystectomyDocumento2 páginasCholecystectomyHiylie MartinezAún no hay calificaciones
- Cholelithiasis Treatment & ManagementDocumento8 páginasCholelithiasis Treatment & ManagementRayhanun MardhatillahAún no hay calificaciones
- ZollingerDocumento5 páginasZollingerSantiago Xicotencatl MendezAún no hay calificaciones
- Ureteral ReconstructionDocumento6 páginasUreteral ReconstructiongumAún no hay calificaciones
- Assessment TN MasrukhiDocumento3 páginasAssessment TN MasrukhiAngger SatriaAún no hay calificaciones
- Urushihara 10.1007 s00383-015-3779-8Documento4 páginasUrushihara 10.1007 s00383-015-3779-8CherAún no hay calificaciones
- Case ReportDocumento5 páginasCase ReportAmmar magdyAún no hay calificaciones
- Surgery Illustrated - Focus - Tapering of The MegaureterDocumento5 páginasSurgery Illustrated - Focus - Tapering of The MegauretermoetazAún no hay calificaciones
- Safe CholecystectomyDocumento60 páginasSafe CholecystectomyCarlos Reyes100% (1)
- Equine Abdominal SurgeryDocumento76 páginasEquine Abdominal SurgeryasheneyAún no hay calificaciones
- PancreaticoduodenectomyDocumento2 páginasPancreaticoduodenectomymarkfernandoeAún no hay calificaciones
- Bakshi 2017Documento7 páginasBakshi 2017DH SiriruiAún no hay calificaciones
- Closure of Loop Ileostomy Potentially ADocumento7 páginasClosure of Loop Ileostomy Potentially Ashah hassaanAún no hay calificaciones
- Cholecystectomy: Cholecystectomy (Pronounced / Kɒləsɪs Tɛktəmi/, Plural: Cholecystectomies) Is TheDocumento3 páginasCholecystectomy: Cholecystectomy (Pronounced / Kɒləsɪs Tɛktəmi/, Plural: Cholecystectomies) Is Thejosias_jorgio1Aún no hay calificaciones
- Cholecystectomy: Navigation SearchDocumento4 páginasCholecystectomy: Navigation SearchMohammed OmerAún no hay calificaciones
- 54.the Gallbladder and Bile DuctsDocumento19 páginas54.the Gallbladder and Bile DuctsAdenegan Adesola RaymondAún no hay calificaciones
- T Tube by Daldoul2012Documento7 páginasT Tube by Daldoul2012Suhenri SiahaanAún no hay calificaciones
- Sleeve-Gastrectomy 2011 BrethauerDocumento15 páginasSleeve-Gastrectomy 2011 BrethauerDavid Schnettler RodriguezAún no hay calificaciones
- Overview: 1.1 BackgroundDocumento12 páginasOverview: 1.1 BackgroundAndika Dwiputra DjajaAún no hay calificaciones
- Choice of Enterostoma: Feeding JejunostomyDocumento4 páginasChoice of Enterostoma: Feeding JejunostomyFikranaya SalimAún no hay calificaciones
- International Journal of Surgery Case ReportsDocumento5 páginasInternational Journal of Surgery Case ReportsJuan Eduardo Rios RodriguezAún no hay calificaciones
- Colonic Interposition For Benign DiseaseDocumento18 páginasColonic Interposition For Benign DiseaseOhana S.Aún no hay calificaciones
- Open Cholecystectomy ReportDocumento7 páginasOpen Cholecystectomy ReportjosephcloudAún no hay calificaciones
- BiliaryDocumento41 páginasBiliaryayundyawibowoAún no hay calificaciones
- Colostomy & Colostomy CareDocumento56 páginasColostomy & Colostomy Careapi-3722454100% (31)
- Cirugía y Cirujanos: Gallstone Ileus After Endoscopic Retrograde CholangiopancreatographyDocumento4 páginasCirugía y Cirujanos: Gallstone Ileus After Endoscopic Retrograde CholangiopancreatographyMuhammad Fuad MahfudAún no hay calificaciones
- Partial CholelithiasisDocumento4 páginasPartial CholelithiasisSyamsulBahriANAún no hay calificaciones
- Final EditDocumento43 páginasFinal EditMary Rose LinatocAún no hay calificaciones
- Laparoscopic Splenectomy: Standardized ApproachDocumento9 páginasLaparoscopic Splenectomy: Standardized ApproachLauraAún no hay calificaciones
- Cholecystectomy (: Laparoscopic GallstonesDocumento4 páginasCholecystectomy (: Laparoscopic GallstonesAlexia BatungbacalAún no hay calificaciones
- 012011SCNA3Documento14 páginas012011SCNA3mariafmhAún no hay calificaciones
- Video DigestDocumento18 páginasVideo Digestsahirwar02Aún no hay calificaciones
- Intestinal Stomas PDFDocumento12 páginasIntestinal Stomas PDFRye Asri Mashudy Dhasry100% (1)
- Blumgart Anastomosis For Pancreaticojejunostomy Minimizes Severe Complications After Pancreatic Head ResectionDocumento10 páginasBlumgart Anastomosis For Pancreaticojejunostomy Minimizes Severe Complications After Pancreatic Head ResectionRegina UgarteAún no hay calificaciones
- Buccal Mucosa Urethroplasty For Adult Urethral Strictures - PMCDocumento13 páginasBuccal Mucosa Urethroplasty For Adult Urethral Strictures - PMCEllya Syahfitri 2108125983Aún no hay calificaciones
- IPSS QuizDocumento2 páginasIPSS QuizmoetazAún no hay calificaciones
- Uro Embryology Cunha 2004Documento16 páginasUro Embryology Cunha 2004moetazAún no hay calificaciones
- Surgery Illustrated - Focus - Tapering of The MegaureterDocumento5 páginasSurgery Illustrated - Focus - Tapering of The MegauretermoetazAún no hay calificaciones
- Anatomy of The Anterior Abdominal Wall & Groin PDFDocumento4 páginasAnatomy of The Anterior Abdominal Wall & Groin PDFmoetazAún no hay calificaciones
- Rusch Urology BroschureDocumento72 páginasRusch Urology BroschuremoetazAún no hay calificaciones
- Post Graduate 2013Documento4 páginasPost Graduate 2013moetazAún no hay calificaciones
- Modified Gibson Incision - WikipediaDocumento1 páginaModified Gibson Incision - WikipediamoetazAún no hay calificaciones
- TJW Neurogenic BladderDocumento8 páginasTJW Neurogenic BladdermoetazAún no hay calificaciones
- Nej Mic M 1308004Documento1 páginaNej Mic M 1308004moetazAún no hay calificaciones
- Cadmium in VXDocumento12 páginasCadmium in VXmoetazAún no hay calificaciones
- Active Surveillance For Prostate Cancer AUA Update 33 2008Documento8 páginasActive Surveillance For Prostate Cancer AUA Update 33 2008moetazAún no hay calificaciones
- Digital Rectal Examination (Prostate Exam) - WWW - Urology-TextbookDocumento2 páginasDigital Rectal Examination (Prostate Exam) - WWW - Urology-TextbookmoetazAún no hay calificaciones
- Histo Lab Exercise #14Documento4 páginasHisto Lab Exercise #14Gela ReyesAún no hay calificaciones
- Cholecystectomy (Gallbladder Removal)Documento6 páginasCholecystectomy (Gallbladder Removal)Katleen Calang AlagAún no hay calificaciones
- MD II Material Pentru 10.03.2020Documento4 páginasMD II Material Pentru 10.03.2020Irina Panciu StefanAún no hay calificaciones
- Assignment Structure of Oral CavityDocumento4 páginasAssignment Structure of Oral CavityNarjis BatoolAún no hay calificaciones
- Peptic Ulcer LP PDF FreeDocumento8 páginasPeptic Ulcer LP PDF FreeAвнιѕнєĸ BαjpαιAún no hay calificaciones
- Gastrointestinal: Metastatic Melanoma of The TractDocumento5 páginasGastrointestinal: Metastatic Melanoma of The TractCristi PopescuAún no hay calificaciones
- Lab 13 Digestive SystemDocumento11 páginasLab 13 Digestive SystemMary Dominique D. TambienAún no hay calificaciones
- Las Science 8 m1Documento9 páginasLas Science 8 m1Diamond CrsktAún no hay calificaciones
- The Microbiota in Cirrhosis and Its Role in Hepatic Decompensation. 2020Documento15 páginasThe Microbiota in Cirrhosis and Its Role in Hepatic Decompensation. 2020mafe.z.solarte87Aún no hay calificaciones
- Quiz Biology Pre Igcse 3Documento17 páginasQuiz Biology Pre Igcse 3eric sivaneshAún no hay calificaciones
- Cholecystitis BelgradeDocumento52 páginasCholecystitis BelgradeLazar VučetićAún no hay calificaciones
- Lesions Portal Gastritis Congestive Gastropathy?: Gastric in Hypertension: InflammatoryDocumento7 páginasLesions Portal Gastritis Congestive Gastropathy?: Gastric in Hypertension: InflammatoryAnisa SafutriAún no hay calificaciones
- What Is Colonoscopy and Its PurposeDocumento6 páginasWhat Is Colonoscopy and Its PurposeGrape JuiceAún no hay calificaciones
- GI Tract Histology SummaryDocumento5 páginasGI Tract Histology SummaryFluffy_iceAún no hay calificaciones
- Repuestos MaterialDocumento18 páginasRepuestos MaterialCristhian Andree Lucar MonzonAún no hay calificaciones
- Hubungan Asupan Serat Makanan Dan Cairan Dengan Kejadian Konstipasi Fungsional Pada Remaja Di Sma Kesatrian 1 SemarangDocumento10 páginasHubungan Asupan Serat Makanan Dan Cairan Dengan Kejadian Konstipasi Fungsional Pada Remaja Di Sma Kesatrian 1 SemarangHanifAún no hay calificaciones
- Hepatic, Pancreatic, and Rare Gastrointestinal Complications of Immune Checkpoint Inhibitor Therapy - UpToDateDocumento29 páginasHepatic, Pancreatic, and Rare Gastrointestinal Complications of Immune Checkpoint Inhibitor Therapy - UpToDatemayteveronica1000Aún no hay calificaciones
- GIT Abnormality in Infant/Children On Radiology Imaging Which Need Surgery CorrectionDocumento48 páginasGIT Abnormality in Infant/Children On Radiology Imaging Which Need Surgery Correctiondr fikriAún no hay calificaciones
- Growth Inhibition of Probiotics On The Growth of Streptococcus MutansDocumento4 páginasGrowth Inhibition of Probiotics On The Growth of Streptococcus MutansSi EllaAún no hay calificaciones
- QT4 - Science 8Documento3 páginasQT4 - Science 8joseph mampustiAún no hay calificaciones
- GIDocumento196 páginasGIswagmasterAún no hay calificaciones
- Biology Grade 8-Quarter 4: He Stomach Muscles Mix The Food and Liquid With Digestive JuicesDocumento6 páginasBiology Grade 8-Quarter 4: He Stomach Muscles Mix The Food and Liquid With Digestive Juicesleah jane malinaoAún no hay calificaciones
- Biliary AtresiaDocumento25 páginasBiliary Atresiajulius billiAún no hay calificaciones
- Ceklist Harian Alat Laparotomy Merk RudolfDocumento4 páginasCeklist Harian Alat Laparotomy Merk RudolfDiahAún no hay calificaciones
- 11th Zoology Ps Answer Key For Quarterly Exam 2019 Question Paper Shri Krishna English MediumDocumento11 páginas11th Zoology Ps Answer Key For Quarterly Exam 2019 Question Paper Shri Krishna English Mediumsri thamizhanAún no hay calificaciones
- CP On Calculous CholelithiasisDocumento102 páginasCP On Calculous Cholelithiasiskathy100% (3)
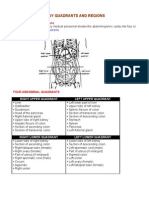
- Organs in The Body Quadrants and RegionsDocumento3 páginasOrgans in The Body Quadrants and RegionsDavid HosamAún no hay calificaciones
- PHS 222/225 Git PhysiologyDocumento32 páginasPHS 222/225 Git PhysiologyDurchessAún no hay calificaciones
- Colostomy Care ReviseDocumento6 páginasColostomy Care ReviseMeryl Mae RamosAún no hay calificaciones
- Colonoscopy: Dr. Aditya Hans Suwignjo, M.HDocumento18 páginasColonoscopy: Dr. Aditya Hans Suwignjo, M.HRenaa PujiiAún no hay calificaciones