Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Osteoporosis
Cargado por
Gheavita Chandra DewiDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Osteoporosis
Cargado por
Gheavita Chandra DewiCopyright:
Formatos disponibles
yen et al.
BMC Musculoskeletal Disorders 2011, 12:67
http://www.biomedcentral.com/1471-2474/12/67
RESEARCH ARTICLE
Open Access
Low bone mineral density is a significant risk factor
for low-energy distal radius fractures in middleaged and elderly men: A case-control study
Jannike yen1, Gudrun Rohde2,3, Marc Hochberg4, Villy Johnsen2 and Glenn Haugeberg2,5*
Abstract
Background: In general there is a lack of data on osteoporosis and fracture in men; this also includes low-energy
distal radius fractures. The objectives of this study were to examine BMD and identify factors associated with distal
radius fractures in male patients compared with controls recruited from the background population.
Methods: In a 2-year period, 44 men 50 years or older were diagnosed with low-energy distal radius fractures, all
recruited from one hospital. The 31 men who attended for osteoporosis assessment were age-matched with 35
controls. Demographic and clinical data were collected and BMD at femoral neck, total hip and spine L2-4 was
assessed by dual energy X-ray absorptiometry.
Results: Apart from weight and living alone, no significant differences were found between patient and controls
for demographic variables (e.g. height, smoking) and clinical variables (e.g. co-morbidity, use of glucocorticoids,
osteoporosis treatment, falls and previous history of fracture). However, BMD expressed as T-score was significant
lower in patients than in controls at all measurement sites (femoral neck: -2.24 vs. -1.15, p < 0.001; Total hip: -1.65
vs. -0.64, p < 0.001; Spine L2-4: -1.26 vs. 0.25, p = 0.002). Among the potential risk factors for fracture evaluated,
only reduced BMD was found to be significantly associated with increased risk for low-energy distal radius fractures
in men.
Conclusion: The results from our study indicate that reduced BMD is an important risk factor for low-energy distal
radius fracture in men. This suggests that improvement of BMD by both pharmacological and non-pharmacological
initiatives may be a strategy to reduce fracture risk in men.
Background
The incidence of distal radius fractures is lower in middle-aged and elderly men than in women. In a Norwegian study, the average annual incidence rate was 25.4/
10,000 in men compared with 109.8/10,000 in women
over the age of 50 years [1].
Compared to women there is a general lack of data on
distal radius fractures in men including data on prevalence of osteoporosis and risk factors [2-4]. In a few studies, osteoporosis has been reported to be more
frequent in male distal radius fracture patients compared to control subjects and reference populations
[2,5-7]. There is also a lack of data exploring the role of
* Correspondence: glenn.haugeberg@sshf.no
2
Department of Rheumatology, Srlandet Hospital, Kristiansand, Service box
416, 4604 Kristiansand, Norway
Full list of author information is available at the end of the article
bone mineral density (BMD) together with other possible risk factors for low-energy distal radius fractures in
men.
The objective of this prospective case-control study
was to compare BMD at spine and hip in male lowenergy distal radius fracture patients with age-matched
controls and to search for factors associated with
increased risk for distal radius fractures.
Methods
Study design and study population
The low-energy distal radius fracture patients (age 50
years) were all prospectively recruited from one hospital
located in southern Norway in the two year period January 2004 through December 2005. The hospital is the
only referral centre for orthopaedic trauma in the
region. The population of men aged 50 years and older
2011 yen et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
yen et al. BMC Musculoskeletal Disorders 2011, 12:67
http://www.biomedcentral.com/1471-2474/12/67
living in the recruitment area of the hospital is approximately 16,000 and the majority of the population lives
in urban areas.
According to routine procedures at the hospital, all
patients with fractures are identified by trained nurses
and invited for osteoporosis assessment and fracture
risk assessment at the osteoporosis centre. Patients with
obvious confusion or dementia or serious infections
were not invited for osteoporosis assessment. At the
osteoporosis centre, routine clinical data were collected
for fracture risk assessment, and BMD was measured
(see below).
A low-energy distal radius fracture was defined as a fracture resulting from minimal trauma falling from standing
height or less [8]. Patients with high-trauma fractures (e.g.,
occurring as the result of a motor vehicle accident) were
excluded. A distal radius fracture was defined as located
within 3 cm of the radio-carpal joint [9].
Age-matched controls were randomly identified in the
national registry for the hospital catchment area and
were invited by mail to participate in the study. We
aimed to include one control person, matched for age
and sex, for each patient. The controls were recruited
and examined in the time period between June 2004
and March 2006.
The study was approved by the National Data Inspectorate and the regional committees for medical research
ethics.
Demographic and clinical data and BMD measurements
The demographic and clinical characteristics of the
patients and controls are listed in table 1. The information was obtained partly by self-report questionnaire
and partly by interview and clinical examination.
BMD was measured at the femoral neck, total hip and
lumbar spine (L2-4), by four trained nurses using the
same dual energy X-ray absorptiometry (DXA) equipment (General Electric, Lunar Prodigy). The in-vitro
long term coefficient of variance (CV) for the spine
phantom was 0.62% for the entire study period. The
in-vivo CV for the measurement procedure was 1.68%
for right femoral neck, 1.56% for left femoral neck,
0.94% for the right total hip, 0.88% for the left total hip
and 1.26% for lumbar spine L2-4. We used the BMD
values for the left hip unless there was a history of previous fracture or surgery. Scans from the right hip were
used in three patients.
T-score calculations were derived from standardized
NHANES male reference population supplied by the
DXA manufacturer. We used the WHO cut point definition for osteoporosis (T-score -2.5 standard deviation (SD)), osteopenia (T-score > -2.5 SD and < -1.0
SD) and normal bone density (T-score -1.0 SD) (10).
Page 2 of 6
Fracture risk estimated by FRAX
We used the WHO fracture risk assessment tool FRAX
to investigate if the distal radius fracture patients had
higher fracture risk than the controls prior to their current distal radius fracture. In the absence of a Norwegian FRAX model, we used the Swedish FRAX model
to estimate the 10-year risk of hip fractures and any
major osteoporotic fractures (clinical spine, forearm,
hip, or shoulder). FRAX was calculated with and without femoral neck BMD (g/cm2) in the algorithm. The
clinical risk factors included in the FRAX model comprise information on race, age, sex, weight, height,
femoral neck BMD, a previous fracture, parental history
of hip fracture, current smoking, use of oral glucocorticoids for more than three months, rheumatoid arthritis,
other secondary causes of osteoporosis, and alcohol
intake of three or more units per day [11]. The FRAX
was calculated without taking the current distal radius
fractures into account, but earlier low-energy fractures
were registered.
Statistical analysis
Categorical variables were expressed as numbers and
percentages, and continuous variables as means with
SD or as medians with range. We used independentsamples t-test for continuous variables and chi-square
test for categorical variables in comparisons between
fracture patients and controls, and between distal radius
fracture patients attending and not attending for DXA.
Chi-square tests were used to explore for differences in
frequency of patients with distal radius fractures in
spring, summer, autumn and winter. Independentsamples t-test was also used to compare FRAX 10-year
probability for fracture between fracture patients and
controls.
The association between low-energy distal radius fractures as dependent variable and the variables included
in table 1 as independent variables were tested in conditional logistical regression analyses, unadjusted and
adjusted for age. The degree of association was
expressed as odds ratio (OR) with 95% confidence interval (CI). A two-tailed p-value < 0.05 was considered statistically significant. All analyses were performed using
SPSS software for Windows, version 15.0 (SPSS Inc.,
Chicago, Illinois).
Results
In the two-year period, a total of 44 men with lowenergy distal radius fractures resident in the geographic
area of the hospital were assessed and treated. Two
male tourists with low-energy distal radius fracture were
also treated at the hospital but excluded from the present analysis. Among the 44 resident patients, two were
yen et al. BMC Musculoskeletal Disorders 2011, 12:67
http://www.biomedcentral.com/1471-2474/12/67
Page 3 of 6
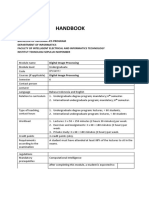
Table 1 Demographic variables, clinical characteristics and bone density measures in male distal radius fracture
patients and controls
Demographics
Patients (n = 31)
Controls (n = 35)
P-value
Age (years)
66.5 (11.6)
66.2 (10.1)
0.916
Height (cm)
175.3 (9.7)
176.2 (5.2)
0.666
Weight (kg)
Education > 13 years
77.3 (14.5)
8 (32.0)
84.7 (10.7)
18 (51.4)
0.020
0.188
Living alone
12 (38.7)
3 (8.6)
0.007
Current smoker
10 (33.3)
8 (22.9)
0.411
Alcohol abuse
0 (0.0)
0 (0.0)
Rheumatoid arthritis
1 (3.2)
0 (0.0)
0.470
Inflammatory diseases
1 (3.2)
1 (2.9)
1.000
Endocrine diseases
Cardiovascular diseases^
1 (3.2)
4 (12.9)
1 (2.9)
7 (20.0)
1.000
0.521
Diabetes
1 (3.2)
1 (2.9)
1.000
Ever
3 (11.5)
2 (5.9)
0.644
Current
2 (7.7)
0 (0.0)
0.184
3 months
2 (6.5)
2 (5.7)
1.000
Calcium supplement
3 (9.7)
3 (8.6)
1.000
12 (38.7)
2 (6.4)
14 (40.0)
1 (2.9)
1.000
0.597
Clinical characteristics
Glucocorticoids
Vitamin-D supplement
Bisphosphonate
Loss of height ( 3 cm)
6 (21.4)
6 (17.6)
0.755
Previous fracture
4 (12.9)
4 (12.9)
1.000
History of hip fracture in a parent
3 (10.3)
3 (9.1)
1.000
Falls ( 1 fall last year)
9 (40.9)
5 (18.5)
0.116
0.78 (0.14)
0.92 (0.14)
<0.001
0.84 (0.16)
1.08 (0.24)
1.01 (0.13)
1.27 (0.20)
<0.001
0.001
Bone mineral density
BMD femoral neck (g/cm2)
BMD total hip (g/cm2)
BMD L2-4 (g/cm2)
T-score femoral neck (SD)
-2.24 (1.05)
-1.15 (1.11)
<0.001
T-score total hip (SD)
-1.65 (1.04)
-0.64 (0.91)
<0.001
T-score L2-4 (SD)
-1.26 (2.05)
0.25 (1.69)
Femoral neck
Normal BMD
2 (6.9)
14 (40.0)
20 (69.0)
18 (51.4)
Osteoporosis
Total hip
7 (24.1)
3 (8.6)
Normal BMD
6 (23.1)
23 (65.7)
Osteopenia
15 (57.7)
12 (34.3)
Osteoporosis
7 (19.2)
0 (0.0)
Normal BMD
11 (35.5)
26 (74.3)
Osteopenia
Osteopenia
0.002
0.006**
<0.001**
Lumbar spine L2-4
0.002**
12 (38.7)
8 (22.9)
Osteoporosis
Normal BMD at all sites*
8 (25.8)
2 (6.5)
1 (2.9)
14 (40.0)
0.002
Osteopenia at 1 site but no osteoporosis*
20 (64.5)
17 (48.6)
0.222
Osteoporosis at 1 site*
9 (29.0)
5 (11.4)
0.120
Mean (SD) for continuous variables and numbers (%) for categorical variables.
SD: standard deviation. BMD: bone mineral density. Total numbers may vary between different variables according to different numbers of missing data.
Endocrine diseases included hyperparathyroidism, hypothyroidism and hyperthyroidism. ^Cardiovascular disease comprised angina pectoris and cardiac
infarction. Difference between present height and the given maximum adult height. Previous fracture before the current distal radius fracture defined as a
fracture of the distal radius, upper arm, rib, spine, hip, femur or lower leg from low-energy trauma after the age of 50. *Femoral neck, total hip, lumbar spine
L2-4. **Overall p-value for the actual categorised variable.
yen et al. BMC Musculoskeletal Disorders 2011, 12:67
http://www.biomedcentral.com/1471-2474/12/67
excluded due to dementia or confusion, and 11 patients
were unwilling to be assessed at the osteoporosis centre.
The final study sample comprised 31 patients, giving a
response rate among potentially eligible patients of
67.4%. For the age groups 50-59 years (n = 11), 60-69
years (n = 7) and 70 and above (n = 13) the response
rate was 84.6%, 63.6% and 65.0%, respectively. The median time between fracture and examination at the osteoporosis centre was 10.0 days (range 1-50 days).
Resident patients not assessed at the osteoporosis centre were on average 4.6 years older than patients
assessed at the osteoporosis centre (mean 71.1 years, SD
10.7 vs. 66.5 years, SD 11.6; p = 0.10).
A total of 65 potential control subjects were invited to
participate, of which 35 were willing to participate, giving a response rate of 54%.
Distal radius fracture prevalence and seasonal variations
No statistically significant difference in the distribution
across seasons was seen among the male distal radius
fracture patients; however, numerically more patients
had a fracture in winter (n = 16) than in spring (n =
11), summer (n = 7) and autumn (n = 10). There also
was no significant difference in the proportion of
patients with distal radius fractures with osteoporosis
between the seasons (spring 16.7%, summer 40.0%,
autumn 25.0% and winter 33.3%).
Distal radius fracture patients and age-matched controls
Demographic variables, clinical characteristics and BMD
values for patients assessed at the osteoporosis centre
and controls are shown in table 1. The patients had significant lower weight than the control subjects, and
more patients than controls were living alone. The
patients had significant lower BMD and T-scores than
the controls at all measurements sites. More patients
also had osteoporosis and osteopenia than controls. For
the other demographic and clinical variables listed in
table 1, no significant differences were seen between the
two groups.
Risk factors for distal radius fractures
ORs for the association of low BMD with distal radius
fractures were estimated in unadjusted and age-adjusted
analyses. As shown in table 2, both osteoporosis and
osteopenia were significantly associated with distal
radius fractures. Weight was found to be of borderline
significance in both unadjusted (OR = 0.95, 95% CI:
0.91-1.00, p = 0.053) and age-adjusted models (OR =
0.96, 95% CI: 0.91-1.00, p = 0.064). Living alone was no
longer significantly associated with fracture in unadjusted or age-adjusted models (data not shown).
When FRAX was calculated using femoral neck
BMD, a significant difference in 10-year risk for hip
Page 4 of 6
Table 2 Unadjusted and age adjusted odds ratios (OR*)
with 95% confidence interval (CI) for associations
between osteopenia and osteoporosis and low-energy
distal radius fracture in men
Unadjusted
Osteopenia
Adjusted for age
OR (95%) CI
p-value OR (95%) CI
p-value
5.95 (1.32-26.86)
0.020
0.023
Osteoporosis 10.48 (1.63-67.60) 0.013
5.82 (1.28-26.40)
10.02 (1.54-65.32) 0.016
*OR and 95% CI was calculated using conditional logistic regression analysis.
At femoral neck, total hip and/or lumbar spine L2-4 but no osteoporosis. At
femoral neck, total hip and/or lumbar spine L2-4.
fracture (9.6% vs. 4.7%, p = 0.039) and for any major
osteoporotic fracture (15.5% vs. 10.0%, p = 0.033) was
found between distal radius fracture patients and controls. However, when FRAX was calculated using
weight and height but without BMD, the differences in
FRAX between the two groups was no longer significant (hip fracture: 5.0% vs. 4.0%, p = 0.53; any major
osteoporotic fracture: 10.0% vs. 8.8%, p = 0.51).
Discussion
The most striking result from the present case-control
study is the demonstration of an approximately 15%
lower BMD at the hip and spine in men with distal
radius fractures compared with age-matched controls
and the apparently strength of the association between
low BMD and low-energy distal radius fracture in men.
This study adds evidence that reduced BMD is a major
risk factor for low-energy distal radius fracture in middle-aged and elderly men as previously has been shown
for women [12-14]. In the present study, no other risk
factors were found to be significantly associated with
low-energy distal radius fractures, although there was a
trend for low body weight. This most likely is related to
the low number of patients included in our study.
The strengths of this study are the prospective study
design for case acquisition over a 2-year period, high
participant rate (67.4% of all cases identified within a
single geographic region), the short time between
the occurrence of the fractures and the examination at
the osteoporosis centre (median 10 days) and use of
age-matched controls recruited randomly from the
population. We also identified all male patients with
low-energy distal radius fracture including patients not
attending DXA-measurements at the osteoporosis
centre. Further, we only included patients defined
according to the definition of low-energy fractures and
not high-energy trauma patients.
However, a limitation of this study is the rather low
number of fracture patients included. This may have
limited our ability to identify other important risk factors than reduced BMD for low-energy distal radius
fracture in men. Thus, our results should be interpreted
yen et al. BMC Musculoskeletal Disorders 2011, 12:67
http://www.biomedcentral.com/1471-2474/12/67
with caution. Furthermore, the response rate among
controls who were invited for assessment was only 54%.
This may have biased our results as the control group
may not reflect the true background population regarding distribution of risk factors for distal radius fracture.
In our study more male fracture patients than male
controls were living alone. In a recently published casecontrol study examining 214 female low-energy distal
radius fracture patients recruited from the same geographic area over the same two year period, we found
that living alone and current use of glucocorticoids in
addition to having osteoporosis were independently
associated with low-energy distal radius fracture in
women [14]. The explanation for this may be that behavioral and psychological factors associated with living
alone, might influence the risk of falls and fractures [15].
The discrepancy in numbers between men and women
in these two studies from the same geographic area is
reflected by the different age specific fracture rates of
approximately 1:4 reported for individuals aged 50
years with distal radius fracture in Norway [1].
Environmental factors may also contribute to an
increased risk of distal radius fracture. Previous studies
have shown that distal radius fractures occur more frequently in the winter months in both men and women
[4,16,17] and especially on days with snow and ice [18];
this probably is due to an increased risk of falling. In
our study, we also found a tendency to an increased risk
of distal radius fracture in men in winter as we previously have also shown for women [14].
Our study confirms the results from previous crosssectional studies which have reported DXA BMD at
heel, spine and hip to be lower in male distal radius
fracture patients than controls [2,6]. In the study by
Tuck et al that including men with high-energy distal
radius fracture, the magnitude of the difference in BMD
at lumbar spine (7%), total hip (8%) and femoral neck
(12%) was lower compared with that seen in our study
(~15% both at spine and hip) [2]. In that study, the
authors also reported that osteoporosis was independently associated with increased risk of distal radius
fracture after adjusting for age and body mass index
(BMI).
Among studies in men with distal radius fracture
without bone density data, one retrospective casecontrol study reported a history of previous fracture to
be the only independent risk factor for low-energy fracture [19], whereas another prospective study reported
increasing age and reduced BMI to be predictors of
increased forearm fracture risk [20]. In our study, mean
weight was significantly lower in men with distal radius
fracture; however, this was less strongly associated with
distal radius fracture than reduced BMD. Other tested
potential risk factors in our study including falls during
Page 5 of 6
the past year and previous low-energy fractures were
also not found to be statistical significantly associated
with an increased fracture risk. This again is most likely
due to the low number of patients included as in our
study.
In low-energy distal radius fracture patients, reduced
BMD has not only been shown to be related to an
increased fracture risk but also to be associated with an
increased severity of the distal radius fracture [21]. The
importance of reduced BMD as a risk factor for our
low-energy distal radius fracture patients is also demonstrated by the FRAX fracture risk analysis. We only
found a statistically significant difference in FRAX
between patients and controls when femoral neck BMD
was included in the FRAX algorithm but not when the
FRAX algorithm was calculated without BMD.
The results from the present study suggest that more
focus should be placed on improving bone strength and
reducing the risk of falling especially in winter time to
reduce low-energy distal radius fracture risk in men
above 50 years. Strategies to improve bone strength may
include changes in life style factors (e.g. modifying
drinking and smoking habits), improving nutrition
including calcium and vitamin D supplementation, and
medical treatment if indicated.
Conclusions
The results from the present study indicate that low
bone mineral density is an important modifiable risk
factor for low-energy distal radius fracture in men. This
suggests that strategies to improve bone strength should
include both pharmacological and non-pharmacological
initiatives. However, larger studies are needed to confirm our results as our study is limited by the low number of patients.
Acknowledgements
We gratefully appreciate the expert technical assistance and help with the
data collection of the osteoporosis nurses Lillann Krger Hstad, Hanne
Vestaby, Tove Kjstvedt, and se Birkedal. This work has been supported
and funded by the Competence Development Fund of Southern Norway
and Srlandet Hospital HF, Norway.
Author details
1
Department of Public Health and Primary Health Care, University of Bergen,
Bergen, Norway. 2Department of Rheumatology, Srlandet Hospital,
Kristiansand, Service box 416, 4604 Kristiansand, Norway. 3Faculty of Health
and Sport, University of Agder, Kristiansand, Norway. 4Departments of
Medicine and Epidemiology and Public Health, University of Maryland
School of Medicine, Baltimore, Maryland, USA. 5Department of Neuroscience,
Division of Rheumatology, Norwegian University of Science and Technology,
Trondheim, Norway.
Authors contributions
J contributed substantially to analyse and interpret the data and was
involved in drafting the manuscript. GR participated in acquisition of data,
interpretation of data and revising the manuscript critically for important
intellectual content. MH and VJ contributed substantially to the conception
yen et al. BMC Musculoskeletal Disorders 2011, 12:67
http://www.biomedcentral.com/1471-2474/12/67
and study design, interpreting the data and revising the manuscript critically
for important intellectual content. GH was the principal investigator and he
was involved in all steps of the study including conception of the study,
design of the study, acquisition of data, data analysing and interpretation of
data and drafting manuscript. All authors have given final approval of the
version to be published.
Competing interests
The authors declare that they have no competing interests.
Received: 2 November 2010 Accepted: 2 April 2011
Published: 2 April 2011
References
1. Lofthus CM, Frihagen F, Meyer HE, Nordsletten L, Melhuus K, Falch JA:
Epidemiology of distal forearm fractures in Oslo, Norway. Osteoporos Int
2008, 19:781-786.
2. Tuck SP, Raj N, Summers GD: Is distal forearm fracture in men due to
osteoporosis? Osteoporos Int 2002, 13:630-636.
3. Sharma S, Fraser M, Lovell F, Reece A, McLellan AR: Characteristics of
males over 50 years who present with a fracture: epidemiology and
underlying risk factors. J Bone Joint Surg Br 2008, 90:72-77.
4. Thompson PW, Taylor J, Dawson A: The annual incidence and seasonal
variation of fractures of the distal radius in men and women over 25
years in Dorset, UK. Injury 2004, 35:462-466.
5. Oyen J, Gjesdal CG, Brudvik C, Hove LM, Apalset EM, Gulseth HC,
Haugeberg G: Low-energy distal radius fractures in middle-aged and
elderly men and womenthe burden of osteoporosis and fracture risk: A
study of 1794 consecutive patients. Osteoporos Int 2010, 21:1257-1267.
6. Atroshi I, Ahlander F, Billsten M, Ahlborg HG, Mellstrom D, Ohlsson C,
Ljunggren O, Karlsson MK: Low calcaneal bone mineral density and the
risk of distal forearm fracture in women and men: a population-based
case-control study. Bone 2009, 45:789-793.
7. Oyen J, Brudvik C, Gjesdal CG, Tell GS, Lie SA, Hove LM: Osteoporosis as a
risk factor for distal radius fractures. A case-control study. J Bone Joint
Surg Am 2011, 93:348-356.
8. Cooper C, Melton LJ: Magnitude and impact of osteoporosis and
fractures. Academic Press, San Diego; 1996.
9. Rockwood CA, Green DP, Bucholz RW: Rockwood and Greens fractures in
adults. Lippincott William & Wilkins Philadelphia; 2006.
10. WHO Assessment of fracture risk and its application to screening for
postmenopausal osteoporosis. Geneva: World Health Organisation; 1994.
11. Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E: FRAX and the
assessment of fracture probability in men and women from the UK.
Osteoporos Int 2008, 19:385-397.
12. Kelsey JL, Browner WS, Seeley DG, Nevitt MC, Cummings SR: Risk factors
for fractures of the distal forearm and proximal humerus. The Study of
Osteoporotic Fractures Research Group. Am J Epidemiol 1992,
135:477-489.
13. Vogt MT, Cauley JA, Tomaino MM, Stone K, Williams JR, Herndon JH: Distal
radius fractures in older women: a 10-year follow-up study of
descriptive characteristics and risk factors. The study of osteoporotic
fractures. J Am Geriatr Soc 2002, 50:97-103.
14. Oyen J, Rohde GE, Hochberg M, Johnsen V, Haugeberg G: Low-energy
distal radius fractures in middle-aged and elderly women-seasonal
variations, prevalence of osteoporosis, and associates with fractures.
Osteoporos Int 2010, 21:1247-1255.
15. Peel NM, McClure RJ, Hendrikz JK: Psychosocial factors associated with
fall-related hip fractures. Age Ageing 2007, 36:145-151.
16. Falch JA: Epidemiology of fractures of the distal forearm in Oslo,
Norway. Acta Orthop Scand 1983, 54:291-295.
17. Solgaard S, Petersen VS: Epidemiology of distal radius fractures. Acta
Orthop Scand 1985, 56:391-393.
18. Jacobsen SJ, Sargent DJ, Atkinson EJ, OFallon WM, Melton LJ: Contribution
of weather to the seasonality of distal forearm fractures: a populationbased study in Rochester, Minnesota. Osteoporos Int 1999, 9:254-259.
19. Kelsey JL, Prill MM, Keegan TH, Tanner HE, Bernstein AL, Quesenberry CP Jr,
Sidney S: Reducing the risk for distal forearm fracture: preserve bone
mass, slow down, and dont fall! Osteoporos Int 2005, 16:681-690.
20. Holmberg AH, Johnell O, Nilsson PM, Nilsson J, Berglund G, Akesson K: Risk
factors for fragility fracture in middle age. A prospective population-
Page 6 of 6
based study of 33,000 men and women. Osteoporos Int 2006,
17:1065-1077.
21. Clayton RA, Gaston MS, Ralston SH, Court-Brown CM, McQueen MM:
Association between decreased bone mineral density and severity of
distal radial fractures. J Bone Joint Surg Am 2009, 91:613-619.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1471-2474/12/67/prepub
doi:10.1186/1471-2474-12-67
Cite this article as: yen et al.: Low bone mineral density is a significant
risk factor for low-energy distal radius fractures in middle-aged and
elderly men: A case-control study. BMC Musculoskeletal Disorders 2011 12:67.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color figure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
También podría gustarte
- Osteoporosis in Men PDFDocumento21 páginasOsteoporosis in Men PDFMihai GabrielaAún no hay calificaciones
- Current Calculator For Barrel Plating - Chlorize Zinc PlatingDocumento4 páginasCurrent Calculator For Barrel Plating - Chlorize Zinc PlatingARVINDA KUMARAún no hay calificaciones
- Christie Roadster S+20K Serial CommunicationsDocumento87 páginasChristie Roadster S+20K Serial Communicationst_wexAún no hay calificaciones
- Vertebral Fracture Risk (VFR) Score For Fracture Prediction in Postmenopausal WomenDocumento11 páginasVertebral Fracture Risk (VFR) Score For Fracture Prediction in Postmenopausal WomenAdhiatma DotAún no hay calificaciones
- F. Lapi, M. Simonetti, R. Michieli, A. Pasqua, M.L. Brandi, B. Frediani, C. Cricelli, G. MazzagliaDocumento6 páginasF. Lapi, M. Simonetti, R. Michieli, A. Pasqua, M.L. Brandi, B. Frediani, C. Cricelli, G. Mazzagliafirdha afghaniAún no hay calificaciones
- Stubbs 2014Documento17 páginasStubbs 2014sajith4457Aún no hay calificaciones
- 2020 Article 3188Documento9 páginas2020 Article 3188Abril SantiagoAún no hay calificaciones
- Osteoporosis Draft Evidence ReviewDocumento397 páginasOsteoporosis Draft Evidence ReviewChon ChiAún no hay calificaciones
- Mortensen 2020Documento9 páginasMortensen 2020sajith4457Aún no hay calificaciones
- Ymj 59 317Documento8 páginasYmj 59 317ItaloLozanoPalominoAún no hay calificaciones
- CMRN68 Ejcm - 132 569 573 2023Documento5 páginasCMRN68 Ejcm - 132 569 573 2023anant AgarwalAún no hay calificaciones
- Association Between Knee Osteoarthritis and Volumetric Bone Mineral DensityDocumento14 páginasAssociation Between Knee Osteoarthritis and Volumetric Bone Mineral Densitytranminhtri21062001Aún no hay calificaciones
- Fractura de CaderaDocumento9 páginasFractura de CaderaWendy Lorely Téllez HernándezAún no hay calificaciones
- Launonen 2015Documento5 páginasLaunonen 2015reginapriscillaAún no hay calificaciones
- Hi Per MobilityDocumento6 páginasHi Per MobilityMartín ZamoraAún no hay calificaciones
- FraktueDocumento8 páginasFraktueIA WulandaryAún no hay calificaciones
- MR KRISTIAN DAMGAARD LYNG (Orcid ID: 0000-0001-8668-691X) DR SINEAD HOLDEN (Orcid ID: 0000-0002-7314-2152)Documento18 páginasMR KRISTIAN DAMGAARD LYNG (Orcid ID: 0000-0001-8668-691X) DR SINEAD HOLDEN (Orcid ID: 0000-0002-7314-2152)Afifah Nur FauzaniAún no hay calificaciones
- J Spinee 2020 03 010Documento16 páginasJ Spinee 2020 03 010Victor CristianAún no hay calificaciones
- Osteoporosis in Men: An Endocrine Society Clinical Practice GuidelineDocumento21 páginasOsteoporosis in Men: An Endocrine Society Clinical Practice GuidelineChon ChiAún no hay calificaciones
- Passaretti 2017Documento8 páginasPassaretti 2017reginapriscillaAún no hay calificaciones
- Geriatria y OrtopediaDocumento28 páginasGeriatria y OrtopediaHector VallejosAún no hay calificaciones
- Fijcmr 650 May 31 2Documento3 páginasFijcmr 650 May 31 2khusnulAún no hay calificaciones
- Frailty Defined by 19 Items As A Predictor of Short-Term Functional Recovery in Patients With Hip FractureDocumento7 páginasFrailty Defined by 19 Items As A Predictor of Short-Term Functional Recovery in Patients With Hip FractureMirela Marina BlajAún no hay calificaciones
- Jcem1802osteoporosis in MenDocumento21 páginasJcem1802osteoporosis in MenSalmadiar RiskaAún no hay calificaciones
- Risk Factors For Refracture of The Femoral Shaft in Children After Removal of External FixationDocumento6 páginasRisk Factors For Refracture of The Femoral Shaft in Children After Removal of External FixationDita AldiniAún no hay calificaciones
- Osteoporosis in Men: An Endocrine Society Clinical Practice GuidelineDocumento21 páginasOsteoporosis in Men: An Endocrine Society Clinical Practice GuidelineChon ChiAún no hay calificaciones
- Alterations of Bone Microstructure and Strength in End-Stage Renal FailureDocumento12 páginasAlterations of Bone Microstructure and Strength in End-Stage Renal FailureDany AGarciaAún no hay calificaciones
- Jurnal MuskuloDocumento8 páginasJurnal MuskuloarvinelaAún no hay calificaciones
- Osteology 01 00018Documento10 páginasOsteology 01 00018Deddy ZulkarnaenAún no hay calificaciones
- Testicular Torsion and Risk Factors For Orchiectomy: Jonathan M. Mansbach, MD Peter Forbes, MA Craig Peters, MDDocumento5 páginasTesticular Torsion and Risk Factors For Orchiectomy: Jonathan M. Mansbach, MD Peter Forbes, MA Craig Peters, MDDiah Sukmawati HidayahAún no hay calificaciones
- Incidence of Mandibular FractureDocumento7 páginasIncidence of Mandibular FractureZaher ShAún no hay calificaciones
- Prevalence and Risk Factors For Lumbar Spondylosis and Its Association With Low Back Pain Among Rural Korean ResidentsDocumento8 páginasPrevalence and Risk Factors For Lumbar Spondylosis and Its Association With Low Back Pain Among Rural Korean Residentsrizky septiAún no hay calificaciones
- Traumatic Fracture of The Pediatric Cervical SpineDocumento11 páginasTraumatic Fracture of The Pediatric Cervical SpineVotey CHAún no hay calificaciones
- Operative Versus Nonoperative Treatments For Legg-Calve - Perthes Disease: A Meta-AnalysisDocumento9 páginasOperative Versus Nonoperative Treatments For Legg-Calve - Perthes Disease: A Meta-Analysisyarianna2Aún no hay calificaciones
- 1755 FullDocumento6 páginas1755 FullIbriana IbrahimAún no hay calificaciones
- FFFGVDocumento10 páginasFFFGVyundaAún no hay calificaciones
- Journal Reading: Dr. Firdaus RamliDocumento22 páginasJournal Reading: Dr. Firdaus RamliBell SwanAún no hay calificaciones
- Lewis Et Al - MrOS Fractures - JBMR2007Documento9 páginasLewis Et Al - MrOS Fractures - JBMR2007chuckc123Aún no hay calificaciones
- Assessment of Knowledge of Osteoarthritis Among Elderly PatientsDocumento7 páginasAssessment of Knowledge of Osteoarthritis Among Elderly PatientsMostafa ShabanAún no hay calificaciones
- Screening To Prevent Osteoporotic Fractures AnDocumento448 páginasScreening To Prevent Osteoporotic Fractures AnMayday FinishaAún no hay calificaciones
- A Practical Approach To Interpretation of Dual-Energy X-Ray Absorptiometry (DXA) For Assessment of Bone DensityDocumento12 páginasA Practical Approach To Interpretation of Dual-Energy X-Ray Absorptiometry (DXA) For Assessment of Bone DensityMuliaAún no hay calificaciones
- Review Article: The Role of Fibular Fixation in Distal Tibia-Fibula Fractures: A Meta-AnalysisDocumento9 páginasReview Article: The Role of Fibular Fixation in Distal Tibia-Fibula Fractures: A Meta-AnalysisGus AbellaAún no hay calificaciones
- Prevalence of Frailty in End Stage Renal DiseaseDocumento14 páginasPrevalence of Frailty in End Stage Renal Diseaseor1da2sa3Aún no hay calificaciones
- UTD 28 11 1634 1640hemaDocumento7 páginasUTD 28 11 1634 1640hemappdspkjuli23Aún no hay calificaciones
- Research ArticleDocumento10 páginasResearch ArticleastutikAún no hay calificaciones
- Prevalence and Risk Factors of Lumbar Spondylolisthesis in Elderly Chinese Men and WomenDocumento8 páginasPrevalence and Risk Factors of Lumbar Spondylolisthesis in Elderly Chinese Men and Womenrobert silitongaAún no hay calificaciones
- The Fracture Predictive Ability of A Musculoskeletal Composite Score in Old Men - Data From The Mros Sweden StudyDocumento6 páginasThe Fracture Predictive Ability of A Musculoskeletal Composite Score in Old Men - Data From The Mros Sweden StudyGio VandaAún no hay calificaciones
- Zhang2018Documento9 páginasZhang2018Rodrigo CarvachoAún no hay calificaciones
- Tennis Elbow JOSPT ArticleDocumento11 páginasTennis Elbow JOSPT ArticleHasan RahmanAún no hay calificaciones
- JMCP 2017 23 7 735Documento14 páginasJMCP 2017 23 7 735Sharan SahotaAún no hay calificaciones
- Exercises MMDocumento11 páginasExercises MMAna Luiza ToldoAún no hay calificaciones
- 10Documento6 páginas10cicelynara94Aún no hay calificaciones
- Nontraumatic Osteonecrosis of The Femoral Head: Ten Years LaterDocumento16 páginasNontraumatic Osteonecrosis of The Femoral Head: Ten Years LaterChristian OliveiraAún no hay calificaciones
- International Journal of Health Sciences and Research: Osteoporosis-Do We Need To Think Beyond Bone Mineral Density?Documento5 páginasInternational Journal of Health Sciences and Research: Osteoporosis-Do We Need To Think Beyond Bone Mineral Density?Ahmad Ghozi Al AkhmarAún no hay calificaciones
- Pereira 2015Documento9 páginasPereira 2015Amalia RosaAún no hay calificaciones
- 10.1007@s10067 020 04988 7Documento11 páginas10.1007@s10067 020 04988 7NyLa LibertyAún no hay calificaciones
- Ajinkya PaperDocumento20 páginasAjinkya Papervzxh5vqg8yAún no hay calificaciones
- Interpreting A DXA Scan in Clinical Practice: Rheumatology Department, Military Hospital Mohammed V, Rabat, MoroccoDocumento17 páginasInterpreting A DXA Scan in Clinical Practice: Rheumatology Department, Military Hospital Mohammed V, Rabat, MoroccoJaita SawettachaiAún no hay calificaciones
- Sciencedirect: Prevalence and Etiology of Midfacial Fractures: A Study of 799 CasesDocumento6 páginasSciencedirect: Prevalence and Etiology of Midfacial Fractures: A Study of 799 CasesSuci NourmalizaAún no hay calificaciones
- Romagna Et Al-2012-Journal of Clinical Periodontology PDFDocumento7 páginasRomagna Et Al-2012-Journal of Clinical Periodontology PDFChristine HacheAún no hay calificaciones
- Comparison of Femur Intertrochanteric Fracture Fixation With Hemiarthroplasty and Proximal Femoral Nail SystemsDocumento6 páginasComparison of Femur Intertrochanteric Fracture Fixation With Hemiarthroplasty and Proximal Femoral Nail SystemsBREEZE EVERARDINE SUXE TELLOAún no hay calificaciones
- Diagnostic Problems in Tumors of Central Nervous System: Selected TopicsDe EverandDiagnostic Problems in Tumors of Central Nervous System: Selected TopicsAún no hay calificaciones
- 80 (1) 40Documento7 páginas80 (1) 40Gheavita Chandra DewiAún no hay calificaciones
- TranslateDocumento3 páginasTranslateGheavita Chandra DewiAún no hay calificaciones
- K - 55 Hyperprolactinaemia H.HTPDocumento24 páginasK - 55 Hyperprolactinaemia H.HTPRuthra Devi NarayanasamyAún no hay calificaciones
- K - 55 Hyperprolactinaemia H.HTPDocumento24 páginasK - 55 Hyperprolactinaemia H.HTPRuthra Devi NarayanasamyAún no hay calificaciones
- Daftar Pustaka FixDocumento3 páginasDaftar Pustaka FixGheavita Chandra DewiAún no hay calificaciones
- K - 55 Hyperprolactinaemia H.HTPDocumento24 páginasK - 55 Hyperprolactinaemia H.HTPRuthra Devi NarayanasamyAún no hay calificaciones
- Doppler Ultrasound in The Assessment of Suspected Intra-Uterine Growth RestrictionDocumento10 páginasDoppler Ultrasound in The Assessment of Suspected Intra-Uterine Growth RestrictionGheavita Chandra DewiAún no hay calificaciones
- ReferenceDocumento4 páginasReferenceGheavita Chandra DewiAún no hay calificaciones
- Malaria Vaccine Questions and Answers October 2011Documento3 páginasMalaria Vaccine Questions and Answers October 2011Gheavita Chandra DewiAún no hay calificaciones
- Maternal Obesity, Gestational Hypertension, and Preterm DeliveryDocumento8 páginasMaternal Obesity, Gestational Hypertension, and Preterm DeliveryGheavita Chandra DewiAún no hay calificaciones
- Plasma, Urinary, and Salivary 8-Epi-Prostaglandin F Levels in Normotensive and Preeclamptic PregnanciesDocumento4 páginasPlasma, Urinary, and Salivary 8-Epi-Prostaglandin F Levels in Normotensive and Preeclamptic PregnanciesGheavita Chandra DewiAún no hay calificaciones
- Abnormalitas Irama JantungDocumento6 páginasAbnormalitas Irama JantungGheavita Chandra DewiAún no hay calificaciones
- Vitamin E in Preeclampsia: Lucilla Poston, Maarten Raijmakers, and Frank KellyDocumento7 páginasVitamin E in Preeclampsia: Lucilla Poston, Maarten Raijmakers, and Frank KellyGheavita Chandra DewiAún no hay calificaciones
- Daftar PustakaDocumento2 páginasDaftar PustakaGheavita Chandra DewiAún no hay calificaciones
- Assessment of Gestational Age in The First Trimester of Pregnancy by Maximum Fetal DiameterDocumento4 páginasAssessment of Gestational Age in The First Trimester of Pregnancy by Maximum Fetal DiameterGheavita Chandra DewiAún no hay calificaciones
- Gleeson 1993Documento2 páginasGleeson 1993Gheavita Chandra DewiAún no hay calificaciones
- Plasma, Urinary, and Salivary 8-Epi-Prostaglandin F Levels in Normotensive and Preeclamptic PregnanciesDocumento4 páginasPlasma, Urinary, and Salivary 8-Epi-Prostaglandin F Levels in Normotensive and Preeclamptic PregnanciesGheavita Chandra DewiAún no hay calificaciones
- Embryology-Nervous System DevelopmentDocumento157 páginasEmbryology-Nervous System DevelopmentGheavita Chandra DewiAún no hay calificaciones
- Fetal Development Chart OutlineDocumento1 páginaFetal Development Chart OutlineAnnapurna DangetiAún no hay calificaciones
- Research: Lateral Wedge Insoles For Medial Knee Osteoarthritis: 12 Month Randomised Controlled TrialDocumento9 páginasResearch: Lateral Wedge Insoles For Medial Knee Osteoarthritis: 12 Month Randomised Controlled TrialGheavita Chandra DewiAún no hay calificaciones
- ColonDocumento8 páginasColonGheavita Chandra DewiAún no hay calificaciones
- Rheumathoid ArthritisDocumento5 páginasRheumathoid ArthritisGheavita Chandra DewiAún no hay calificaciones
- OsteoporosisDocumento8 páginasOsteoporosisGheavita Chandra DewiAún no hay calificaciones
- OsteoporosisDocumento3 páginasOsteoporosisGheavita Chandra DewiAún no hay calificaciones
- Research: Lateral Wedge Insoles For Medial Knee Osteoarthritis: 12 Month Randomised Controlled TrialDocumento9 páginasResearch: Lateral Wedge Insoles For Medial Knee Osteoarthritis: 12 Month Randomised Controlled TrialGheavita Chandra DewiAún no hay calificaciones
- Down Syndrome DiagnosticDocumento13 páginasDown Syndrome DiagnosticGheavita Chandra DewiAún no hay calificaciones
- HelicobacterDocumento6 páginasHelicobacterGheavita Chandra DewiAún no hay calificaciones
- HelicobacterDocumento8 páginasHelicobacterGheavita Chandra DewiAún no hay calificaciones
- Nama: Fazlun Nisak NIM: 180170127 MK: Kecerdasan Buatan (A2) Tugas PerceptronDocumento8 páginasNama: Fazlun Nisak NIM: 180170127 MK: Kecerdasan Buatan (A2) Tugas PerceptronFazlun NisakAún no hay calificaciones
- Seatex DPS 132 User's ManualDocumento96 páginasSeatex DPS 132 User's ManualilgarAún no hay calificaciones
- Amt 113 - Weight and Balance LecDocumento67 páginasAmt 113 - Weight and Balance LecNino AngobAún no hay calificaciones
- NRC RG 1.99 Rev. 2 PDFDocumento10 páginasNRC RG 1.99 Rev. 2 PDFlalitAún no hay calificaciones
- Foot AbnormalityDocumento23 páginasFoot AbnormalityKezia PaneAún no hay calificaciones
- As-St300 - Day 1 - PLC WorkingDocumento16 páginasAs-St300 - Day 1 - PLC Workingashutosh123Aún no hay calificaciones
- Sachin BiradarDocumento2 páginasSachin Biradardecoo.cocooAún no hay calificaciones
- External Interface (XINTF)Documento38 páginasExternal Interface (XINTF)AlonsoAún no hay calificaciones
- Website Layout Design in Corel DrawDocumento111 páginasWebsite Layout Design in Corel DrawFathoni WangsadranaAún no hay calificaciones
- Mass Balance Equations For Deformable Porous MediaDocumento9 páginasMass Balance Equations For Deformable Porous MediaJonathan TeixeiraAún no hay calificaciones
- Exam Syllabus For Genius20Documento2 páginasExam Syllabus For Genius20Vaishali PandeyAún no hay calificaciones
- 1768 Compactlogix Controllers, Revision 20: Release NotesDocumento26 páginas1768 Compactlogix Controllers, Revision 20: Release NotesedeconsysAún no hay calificaciones
- Hydratight Flange Facing MachineDocumento30 páginasHydratight Flange Facing MachineDilipAún no hay calificaciones
- Codd's 12 Rules For Relational DatabasesDocumento5 páginasCodd's 12 Rules For Relational DatabasesArul VermanAún no hay calificaciones
- Summa Roll Cutters: S One - S Class 2 Series World Renowned Vinyl and Contour CuttersDocumento32 páginasSumma Roll Cutters: S One - S Class 2 Series World Renowned Vinyl and Contour CuttersPU PUAún no hay calificaciones
- IptablesDocumento3 páginasIptablessoomalikAún no hay calificaciones
- A.Van - Dam and Zegeling RobustFVM1DHyperbolicfromMagnetohydrodynamicsDocumento30 páginasA.Van - Dam and Zegeling RobustFVM1DHyperbolicfromMagnetohydrodynamicsSedanur Mazı GözenAún no hay calificaciones
- Determination of Hydrocarbons in Liquefied Petroleum (LP) Gases and Propane/Propene Mixtures by Gas ChromatographyDocumento11 páginasDetermination of Hydrocarbons in Liquefied Petroleum (LP) Gases and Propane/Propene Mixtures by Gas ChromatographyКарат центрAún no hay calificaciones
- 1.0 Intro To Aircon (Properties of Moist Air) With Sample ProblemDocumento10 páginas1.0 Intro To Aircon (Properties of Moist Air) With Sample ProblemRenneil De PabloAún no hay calificaciones
- 3tnv82a Bdsa2Documento2 páginas3tnv82a Bdsa2BaggerkingAún no hay calificaciones
- Mechatronics Eng 07 08 EtDocumento86 páginasMechatronics Eng 07 08 EtVenu Madhav ReddyAún no hay calificaciones
- Guide-Tone Space - Navigating Voice-Leading Syntax in Tonal JazzDocumento23 páginasGuide-Tone Space - Navigating Voice-Leading Syntax in Tonal JazzCacau Ricardo FerrariAún no hay calificaciones
- Assign N LabDocumento4 páginasAssign N LabMtende MosesAún no hay calificaciones
- g12 Module CapacitorsDocumento8 páginasg12 Module CapacitorsHarold Vernon MartinezAún no hay calificaciones
- IF184952 Digital Image ProcessingDocumento3 páginasIF184952 Digital Image Processingshela malaAún no hay calificaciones
- Danyar Et Al., 2020 - FinalDocumento24 páginasDanyar Et Al., 2020 - FinalSardar SaleemAún no hay calificaciones
- Long-Range DependenceDocumento3 páginasLong-Range Dependencewoodword99Aún no hay calificaciones
- 1979 IC MasterDocumento2398 páginas1979 IC MasterIliuta JohnAún no hay calificaciones