Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Community Integration and Satisfaction With Functioning After Intensive Cognitive Rehabilitation For Traumatic Brain Injury
Cargado por
Begoña MartinezTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Community Integration and Satisfaction With Functioning After Intensive Cognitive Rehabilitation For Traumatic Brain Injury
Cargado por
Begoña MartinezCopyright:
Formatos disponibles
943
Community Integration and Satisfaction With Functioning
After Intensive Cognitive Rehabilitation
for Traumatic Brain Injury
Keith D. Cicerone, PhD, Tasha Mott, PhD, Joanne Azulay, PhD, John C. Friel, PsyD
ABSTRACT. Cicerone KD, Mott T, Azulay J, Friel JC.
Community integration and satisfaction with functioning after
intensive cognitive rehabilitation for traumatic brain injury.
Arch Phys Med Rehabil 2004;85:943-50.
Objective: To evaluate the effectiveness of an intensive
cognitive rehabilitation program (ICRP) compared with standard neurorehabilitation (SRP) for persons with traumatic brain
injury (TBI).
Design: Nonrandomized controlled intervention trial.
Setting: Community-based, postacute outpatient brain injury rehabilitation program.
Participants: Fifty-six persons with TBI.
Interventions: Participants in ICRP (n27) received an
intensive, highly structured program of integrated cognitive
and psychosocial interventions based on principles of holistic
neuropsychologic rehabilitation. Participants in SRP (n29)
received comprehensive neurorehabilitation consisting primarily of physical therapy, occupational therapy, speech therapy,
and neuropsychologic treatment. Duration of treatment was
approximately 4 months for both interventions.
Main Outcome Measures: Community Integration Questionnaire (CIQ); and Quality of Community Integration Questionnaire assessing satisfaction with community functioning
and satisfaction with cognitive functioning. Neuropsychologic
functioning was evaluated for the ICRP participants.
Results: Both groups showed significant improvement on
the CIQ, with the ICRP group exhibiting a significant treatment
effect compared with the SRP group. Analysis of clinically
significant improvement indicated that ICRP participants were
over twice as likely to show clinical benefit on the CIQ (odds
ratio2.41; 95% confidence interval, 0.8 7.2). ICRP participants showed significant improvement in overall neuropsychologic functioning; participants with clinically significant improvement on the CIQ also showed greater improvement of
neuropsychologic functioning. Satisfaction with community
functioning was not related to community integration after
treatment. Satisfaction with cognitive functioning made a significant contribution to posttreatment community integration;
this finding may reflect the mediating effects of perceived
self-efficacy on functional outcome.
Conclusions: Intensive, holistic, cognitive rehabilitation is
an effective form of rehabilitation, particularly for persons with
TBI who have previously been unable to resume community
From the Cognitive Rehabilitation Department, JFK-Johnson Rehabilitation Institute, Edison, NJ.
Supported by the National Institute on Disability and Rehabilitation Research
(grant no. H133A020518).
No commercial party having a direct financial interest in the results of the research
supporting this article has or will confer a benefit on the author(s) or on any
organization with which the author(s) is/are associated.
Reprint requests to Keith D. Cicerone, PhD, JFK-Johnson Rehabilitation Institute,
2048 Oak Tree Rd, Edison, NJ 08820, e-mail: kcicerone@solarishs.org.
0003-9993/04/8506-8427$30.00/0
doi:10.1016/j.apmr.2003.07.019
functioning. Perceived self-efficacy may have significant impact on functional outcomes after TBI rehabilitation. Measures
of social participation and subjective well-being appear to
represent distinct and separable rehabilitation outcomes after
TBI.
Key Words: Brain injuries; Outcome and process assessment (health care); Quality of life; Rehabilitation.
2004 by the American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and
Rehabilitation
T IS GENERALLY well recognized that the cognitive and
psychosocial impairments after traumatic brain injury (TBI)
Icontribute
to chronic disability, and therefore, rehabilitation
must address these aspects of a persons functioning to be
effective. Neuropsychologic rehabilitation of persons with TBI
may best be achieved through a comprehensive, holistic approach to the treatment of cognitive, emotional, and functional
impairments and disability. In their review of postacute, outpatient brain injury rehabilitation, Malec and Basford1 noted
that comprehensive integrated treatment for persons with TBI
includes a neuropsychologic focus that addresses cognitive,
interpersonal, and affective concerns; group interventions that
address awareness, acceptance, and social skills; involvement
of significant others; and therapeutic trials to enhance vocational functioning and independent living skills. These programs are typically centered on the goals of fostering participants awareness of their functional potential; improving
personal organization and social skills; developing compensations for residual cognitive limitations; developing psychologic
coping skills for emotional and behavioral self-management;
participating in social, work, and leisure activities; and adapting to the chronic limitations imposed by their injury, to
alleviate disability in everyday activities and facilitate social
role functioning. Malec et al2 made explicit the distinction
between remedial interventions, which are intended to be restorative of cognitive abilities, and interventions designed to
develop alternative or compensatory behaviors to accomplish
the same goals through different means. Although treatment
may initially attempt to restore dysfunctional cognitive systemsan approach that can increase awareness of disabilities
and produce small changes in cognitive impairmentsthe emphasis on compensatory behavior and environmental restructuring for residual cognitive limitations increases over the
course of treatment.
In their discussion of the rationale for the holistic approach
to neuropsychologic rehabilitation, Ben-Yishay and Gold3 emphasized that the neurobehavioral manifestations after TBI are
dynamic and multidetermined. They stated that effective rehabilitation must systematically integrate interventions directed at
the remediation of cognitive deficits, functional skills, and
interpersonal functions. Improvements in functioning are typically accomplished by an improvement in the effective functional application of residual cognitive abilities rather than
restoration of the underlying cognitive deficits per se. Evidence
Arch Phys Med Rehabil Vol 85, June 2004
944
INTENSIVE COGNITIVE REHABILITATION FOR TBI, Cicerone
exists that holistic, integrated rehabilitation that includes both
individualized cognitive and psychosocial-interpersonal therapies produces the greatest overall improvements in functioning
by persons with TBI.4,5
Few studies of comprehensive integrated TBI rehabilitation
have assessed treatment effectiveness at the level of community integration and social participation. Malec6 reported improvements in social participation after comprehensive TBI
rehabilitation, assessed with the Mayo Portland Adaptability
Inventory, despite the fact that primary cognitive functions of
attention, memory, and novel problem solving improved least
frequently over the course of treatment. Sander et al,7 using the
Community Integration Questionnaire (CIQ), evaluated treatment effects for 24 persons with TBI who were admitted for
comprehensive integrated, postacute rehabilitation within 8
months of injury. They found significant improvements after an
average of 4 months of treatment on the CIQ total score and on
the 3 subscales measuring home integration, social integration,
and productivity. A subsequent analysis of 71 persons with TBI
who participated in this program again showed significant
improvements on all of the CIQ subscales.8 Participants who
were admitted for treatment less than 1 year after injury
showed greater improvement on the total CIQ and productivity
subscale but not the home integration or social integration
subscales, compared with participants admitted to treatment 1
to 5 years after injury. In addition to group analyses, individual
variability in response to rehabilitation was evaluated using
reliable change methodology. The analysis of clinically significant change for individual participants indicated that 46% of
the total sample improved on total CIQ scores from pretreatment to posttreatment, 49% did not make significant change,
and 4% showed clinically significant worsening. The participants who were less than 1 year after injury were more likely
to make clinically significant improvement on total CIQ (59%
vs 36%) and productivity (59% vs 23%) scores, consistent with
group analyses.
None of these studies included a comparison group, limiting
the interpretation of results. Further, measures of participation
like the CIQ assess neither effectiveness of functioning8 nor
persons satisfaction with their community functioning.9 In his
review of the CIQ as a measure of long-term outcomes after
TBI, Dijkers10 noted a particular need for research both to
assess CIQ change that occurs after interventions to improve
community functioning and to relate objective assessment of
community functioning with the CIQ to subjective quality of
life (QOL).
Several studies have found little relation between QOL after
TBI and injury-related variables,11-13 physical independence,14-17 or cognitive functioning.13,17,18 Several studies have
examined the relationship between subjective well-being and
the CIQ score.13,19-21 Heinemann and Whiteneck19 included
measures of impairment, disability, handicap, and life satisfaction among 758 individuals with TBI an average of 5 years
after injury. Global perception of life satisfaction was positively related to social integration and productivity (but not
home integration) on the CIQ. Corrigan et al13 also found a
relation between life satisfaction and CIQ social integration for
214 persons with TBI who were 2 years after injury (but not 1y
after injury). Life satisfaction was only modestly associated
with factors predictive of other aspects of outcome after TBI.
Burleigh et al20 examined the relation between global life
satisfaction and components of community integration on the
CIQ for 30 persons with TBI who were living in the community and were at least 8 years after injury. They found only a
marginal relation between life satisfaction and social integration and no relation with home integration, productivity, or
Arch Phys Med Rehabil Vol 85, June 2004
overall community integration scores. However, Smith et al21
failed to find a significant relation between life satisfaction and
total CIQ score on any of the subscale scores among 43 adults
with TBI who were living in the community an average of 7
years after injury. Overall, the studies that evaluated both
community integration and QOL several years after TBI found
a marginal relation, suggesting that these represent distinct
aspects of participants experience and separable aspects of
long-term outcome after rehabilitation for TBI.
Prior studies14,15,17 have emphasized the importance of understanding a persons perceptions of well-being, values, and
beliefs for providing effective, holistic rehabilitation. Although
several studies that examined life satisfaction after TBI included subjects who had received rehabilitation, we did not
identify a single study that directly assessed life satisfaction as
an outcome of TBI rehabilitation.
The purpose of our study was to compare the effectiveness
relative to community integration of a program of holistic,
intensive, cognitive rehabilitation with a more conventional
rehabilitation program for persons with TBI. We also assessed
participants satisfaction with their functioning after treatment
and examined the relations among neuropsychologic functioning, community integration, satisfaction with community functioning, and satisfaction with cognitive functioning.
METHODS
Participants
We examined treatment effectiveness for people with TBI
who participated in a comprehensive, postacute, outpatient,
brain injury rehabilitation program. Criteria for participation in
this program include being medically stable at the time of
admission; independent in basic self-care skills, such as feeding and toileting; and having the cognitive ability to participate
in treatment. Additional inclusion criteria for participants in the
current study included medical documentation of TBI, age of
18 years or older, and having adequate language expression
and comprehension to participate in verbally based interventions (ie, participants had to speak English and could not be
severely aphasic). Participants with a history of substance
abuse or psychiatric history were not excluded, although patients identified with current substance use or psychiatric disturbance that would preclude effective treatment for their cognitive deficits were not admitted to the postacute rehabilitation
program. Participants also had to have a family member or
person who could participate in treatment planning conferences
and support implementation of the treatment plan. Participants
provided informed consent to participate in treatment.
The participants in our study were 56 persons with TBI who
were admitted for treatment within a 2-year period from January 1997 through December 1998. We conducted a prospective analysis of 2 different intervention programs over this
time. The majority of participants (89%) had sustained moderate to severe TBI, with the remainder sustaining mild injuries. One group of 27 participants had been screened and
selected for an intensive cognitive rehabilitation program
(ICRP). These participants typically exhibited significant cognitive limitations and had been unable to resume their preinjury
activity levels and/or employment. Although these participants
were, in principle, considered to have some capacity to develop
a realistic awareness of their strengths and weaknesses, participants with significant impairments of self-awareness were
typically referred for the ICRP as the most likely means of
improving their functional abilities. Impaired self-awareness
was determined by the judgment of clinicians involved in the
patients care, typically based on a combination of clinical
INTENSIVE COGNITIVE REHABILITATION FOR TBI, Cicerone
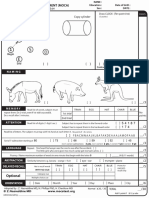
Table 1: Demographic Characteristics
n
Mean age SD (y)
Mean education SD (y)
Gender, n (%)
Men
Women
Preinjury employment status, n (%)
Competitively employed
Student
Unemployed
Moderate to severe injury (%)
Mean time after injury SD (mo)
Mean treatment length SD (mo)
ICRP
SRP
27
37.810.6
13.21.7
29
37.112.0
13.02.2
17 (63)
10 (37)
23 (79)
6 (21)
25 (92.6)
1 (3.7)
1 (3.7)
88.9
33.94.8
3.80.4
25 (86.2)
3 (10.3)
1 (3.5)
89.6
4.89.5*
3.92.5
Abbreviation: SD, standard deviation.
*P.05.
interview, discrepancies between the patients subjective report
and results of neuropsychologic evaluation, and responses to
feedback regarding the presence of cognitive deficits. There
were 29 participants who participated in a standard rehabilitation program (SRP) for brain injury. The 2 groups were equivalent with regard to age, education, and gender (table 1). Most
participants in both groups were productive before their injury,
with most engaged in full-time, competitive employment (table 1).
A systematic bias existed in the selection of participants,
based on time from injury at the admission to treatment.
Participants who were further postinjury and had chronic disability (including participants who had received prior postacute
rehabilitation and/or been unsuccessful in their attempts to
resume functioning) were more likely to be admitted to ICRP.
Participants who were admitted to the postacute rehabilitation
program relatively earlier after injury and who were considered
more likely to exhibit active neurologic recovery over the
course of treatment were more likely to receive SRP. As a
result, participants in SRP were significantly earlier postinjury
than participants in ICRP (see table 1). Twenty-eight of 29
(97%) of the SRP participants were 1 year or less after injury,
with 20 of 29 (69%) 3 months or less after injury. In contrast,
14 of the 27 (52%) ICRP participants were 1 year or less after
injury, and none were less than 4 months after injury.
One of the ICRP participants left treatment to enter a vocational training program 2 weeks before the completion of the
planned intervention. This patient returned to complete the
posttreatment evaluation as originally scheduled and is included in the current analysis. No SRP participants discontinued treatment, although the length of treatment could vary
based on therapists recommendations and participants preferences.
Interventions
The ICRP is a highly structured and integrated program
lasting 16 weeks. It is provided to small groups of 5 to 8
participants at a given time. The ICRP consisted of individual
and group cognitive remediation with an emphasis on increasing awareness and developing compensations for cognitive
deficits, small-group treatment for interpersonal and pragmatic
communication skills, individual and/or group psychotherapy,
family support, and therapeutic work trials and placement to
facilitate educational or vocational readiness. Some participants received a limited amount of physical or occupational
therapy for sensorimotor deficits, if necessary. Within the
945
ICRP, participants are expected to accept and to provide feedback to others, and interpersonal group process is emphasized
throughout all of the treatment components. The core treatment
program was conducted 4 days a week, 5 hours a day. All ICRP
participants received cognitive group treatment for 2 hours a
day, 3 days a week. Cognitive group treatment used a variety
of functional activities, with an emphasis on executive functioning (eg, planning, problem solving, adapting to unexpected
situations), metacognitive functioning (eg, self-monitoring,
cognitive self-appraisal, affect regulation), and interpersonal
group process (eg, giving and receiving feedback, achieving
consensual agreement). The final 20 to 30 minutes of cognitive
group treatment was devoted to reviewing the group process,
summarizing the activities of the group, and highlighting participants individual problems and progress. After each cognitive group, participants received 1 hour of individual cognitive
remediation directed toward their specific areas of impaired
cognitive functioning. An active effort was made to relate the
content of individual cognitive interventions to the areas of
cognitive difficulty observed in group treatments, as well as to
make explicit the relation between individual cognitive treatments and the participants everyday functioning. These sessions were also used to ensure participants agreement with the
goals of their treatment, to obtain their recommendations regarding appropriate treatment content, and to address any additional concerns. Group treatment of communication and interpersonal skills was conducted for an additional 3 hours a
week, to address participants pragmatic language skills, interpersonal communication style, perspective taking, and social
behavior. The interpersonal communication interventions incorporated role playing in varied functional and interpersonal
scenarios. It also incorporated interpersonal and videotaped
feedback, review of each participants communication style
and intent, and analysis of social interactions and interpersonal
interactions. Performance feedback and active self-appraisal
were encouraged throughout the group process. Participants
also received group treatment 1 hour a week to facilitate the
application of therapeutic gains in their daily lives. Although
the specific focus and methods of this group varied at different
times, typically reflecting the needs of different groups of
participants, the application of life skills (eg, note-taking),
self-management of emotional reactions that adversely impacted functioning, and instruction and modeling to facilitate
generalization of compensatory strategies were consistently
addressed. Participants received additional therapies within the
core program determined by their individual needs. ICRP participants typically received 15 hours a week of therapies in the
treatments described above.
In addition to these treatments, 1 day a week of the core
ICRP program was devoted to participation in individually
designed therapeutic work trials within the hospital or community. These trials were under the supervision of a vocational
therapist who could also provide on-site job coaching. For
participants expecting to return to school, this aspect of treatment was directed at reestablishing functional academic skills
and participating in structured coursework or educational training. Participants without active goals of returning to work or
school received treatment relevant to their discharge destination, such as management of home responsibilities or providing
volunteer services. The therapeutic work trials and related
activities provided an opportunity for participants to identify
their deficits, to practice compensatory strategies, and to improve their interpersonal communication skills in a realistic
environment. Throughout the program, families were scheduled to participate in a typical treatment day along with the
participants, to establish an ongoing connection among the
Arch Phys Med Rehabil Vol 85, June 2004
946
INTENSIVE COGNITIVE REHABILITATION FOR TBI, Cicerone
goals of the program, participants progress, observation of
family members and significant others, and reinforcement of
the use of compensatory strategies in the home and community.
The SRP consisted primarily of physical, occupational,
speech, and neuropsychologic therapies. Each participants
treatment content and duration were clinically determined in
accordance with participants individual needs, medically prescribed treatments, and the treatment teams clinical recommendations. Specific interventions directed at their cognitive
deficits were typically included within these therapies, according to the therapists individual assessments and treatment
plans, and all participants continued to be monitored by a staff
neuropsychologist throughout the course of their treatment.
Participants in SRP could also receive recreational therapy,
vocational or educational interventions, and psychologic counseling based on their individual needs. The SRP was delivered
within the same postacute brain injury rehabilitation setting as
the ICRP and incorporated many of the principles of comprehensive neuropsychologic rehabilitation,22 but the delivery of
treatment was less intensive and less structured. Participants in
the SRP were initially admitted for 15 hours a week of treatment; this was adjusted over the course of treatment to reflect
current needs and typically varied between 12 and 24 hours of
treatment a week for all of the SRP participants. Both groups
received approximately 4 months of treatment (see table 1).
Outcome Measures
The primary measure of the effectiveness of treatment was
improvement in community integration from before to after
treatment. QOL, based on a new measure of participants
satisfaction with their functioning, was also assessed at the
completion of treatment. For participants receiving ICRP, we
also evaluated changes in neuropsychologic functioning from
before to after treatment.
Community integration. Community integration was assessed with the CIQ, which was administered and scored
according to the original procedures.9 The primary measure of
interest was total CIQ score, although changes in home integration, social integration, and productivity subscales were also
examined. Effect sizes (ESs) were determined using the Cohen
d statistic, based on the pooled variance from pretreatment CIQ
scores.23 To evaluate the incidence of clinically significant
changes in community integration for individual participants,
we derived a reliable change index24 (RCI) for the total CIQ
score from the psychometric information for 341 persons with
TBI.9 Participants were classified as showing positive change,
no change, or negative change based on reliable change scores
exceeding the 90% confidence interval (CI) (5% in either
direction). Using this method to determine the 90% RCI resulted in a value of 4.2 for the total CIQ score, which is
essentially the same as the value derived by Seale et al.8
Satisfaction with functioning. No consensus exists on the
use of instruments to measure health-related QOL in a manner
that is relevant to persons with TBI.25,26 To evaluate participants satisfaction with their functioning after cognitive rehabilitation, we took a practical approach and developed a measure that complemented the CIQ. This instrument, which we
have referred to as the Quality of Community Integration
Questionnaire (QCIQ) queries 2 types of satisfaction: (1) individuals subjective satisfaction with their level of community
integration and (2) individuals satisfaction with their current
level of cognitive functioning as it affects their ability to
function in specific areas of their lives.
The initial portion of the QCIQ corresponds to the assessment of community integration with the CIQ, and consists of
questions related to the individuals satisfaction with commuArch Phys Med Rehabil Vol 85, June 2004
nity functioning (QCI scale). The home integration section
includes a satisfaction question for each of the 6 CIQ items; for
example, the CIQ question Who usually looks after your
personal finances, such as banking or paying bills? was accompanied by the question How satisfied are you with the way
in which your personal finances are managed? The social
integration section of the QCIQ incorporates 2 satisfaction
questions related to participants satisfaction with their leisure
life and satisfaction with their ability to get along with others.
The productivity section of the QCIQ included an additional
question related to satisfaction with current work situation,
school situation, and/or volunteer activities. Each of the satisfaction questions is rated on a 4-point scale (range: 1, very
dissatisfied to 4, very satisfied). Total possible scores on the
QCI scale range from 9 to 36.
We believe that an important aspect of QOL for persons
with TBI receiving cognitive rehabilitation is their satisfaction with their cognitive functioning. Therefore, the final section of the QCIQ addresses participants satisfaction with cognitive functioning (QCOG scale). Subjects are initially asked to
rate how important they consider their cognitive functioning to
their happiness, with responses ranging from not important
to very important. There are 6 subsequent questions asking
respondents, How satisfied are you with your cognitive functioning (1) as it affects your ability to carry out daily household
responsibilities (eg shopping, meal preparation, housework,
child care, personal financial management); (2) as means of
enabling you to be a contributing member of your family; (3)
as it enables you to engage in leisure activities; (4) as it impacts
on your ability to get along with others; (5) as it impacts on
your ability to be productive (being able to accomplish things
that are important to you in your everyday life); and (6) as a
source of feeling good about yourself? Each of the 6 questions
also was rated on a 4-point scale (range: 1, very dissatisfied to
4, very satisfied). Total possible scores on the QCOG range
from 6 to 24.
Properties of the QCIQ were evaluated in a sample of 80
patients with neurologic injury or illness on admission for
rehabilitation. This sample included the 56 patients with TBI
reported in our study, 16 stroke patients, and 8 patients with
other neurologic illnesses. Principal components analysis supported the interpretation of the QCI and QCOG scales as
discrete factors. Use of the QCIQ with this sample indicated
good internal reliability for both the scales measuring satisfaction with community functioning (Cronbach .85) and satisfaction with cognitive functioning (.93).
Neuropsychologic functioning. Before they began treatment, most participants underwent comprehensive baseline
evaluation that included neuropsychologic assessments as part
of their clinical evaluation. Neuropsychologic assessments
were readministered at the completion of treatment for all
ICRP participants. Complete pretreatment and posttreatment
neuropsychologic data were obtained on only 12 of the 29 SRP
participants. Neuropsychologic data were, therefore, only analyzed for ICRP participants. The primary variable of interest
was a composite index derived from 6 neuropsychologic measures. Attention and processing speed was evaluated with
Trail-Making Test27 Parts A (TMT-A) and B (TMT-B). Memory functioning was evaluated with the total acquisition score
from the California Verbal Learning Test28 (CVLT) and immediate-recall score from the Rey Complex Figure (RCF).29
Higher cognitive functioning was assessed with the Controlled
Oral Word Association Test30 (COWAT) and Category Test.27
All raw scores were converted to T scores that were demographically corrected for age (CVLT, RCF), or age and education (TMT-A, TMT-B, COWAT, Category Test). A compos-
947
INTENSIVE COGNITIVE REHABILITATION FOR TBI, Cicerone
Table 2: CIQ, QCIQ, and Neuropsychologic Scores
ICRP
Before
Community integration
CIQ
Home integration
Social integration
Productivity
Satisfaction with functioning
QCI
QCOG
Neuropsychologic functioning
Overall T score
SRP
After
Before
After
11.64.6
3.12.7
7.02.3
1.40.9
16.84.2
5.12.4
8.61.8
3.11.3
13.74.4
3.52.1
6.82.0
3.42.0
16.15.4*
4.52.7*
8.02.5
3.62.2
27.14.6
16.73.6
29.74.4
18.24.3
35.58.7
40.78.8
NOTE. Values are mean SD.
*Significant difference between groups, before versus after treatment (P.05).
Significant difference between groups, before versus after treatment (P.01).
Significant difference between groups (P.01)
Significant difference before versus after treatment (P.01)
ite score reflecting overall neuropsychologic functioning was
based on the mean T score. Five participants were missing 1
neuropsychologic data point; for these participants, the mean
value from each participants respective pretreatment or posttreatment measures was imputed for the missing values for
analysis of overall neuropsychologic functioning. For the analysis of individual neuropsychologic measures, cases with missing data were dropped from the analysis of that variable.
Analysis of change on the CIQ was evaluated with repeatedmeasures analyses of variance (ANOVAs) with program (ICRP
vs SRP) as a between-subjects factor and time (pretreatment vs
posttreatment) as a within-subjects factor. The difference between groups on the QCIQ scales after treatment was analyzed
with the Mann-Whitney U test. Spearman correlations were
obtained to evaluate the relations among measures. Linear
stepwise regression with probability equal to .05 or less to enter
variables and equal to .10 or greater to remove variables was
used to evaluate predictors and indicators of total CIQ and QCI
and QCOG scores at completion of treatment.
RESULTS
Effectiveness of Intervention
We found a significant main effect for time on total CIQ
scores (F1,5440.49, P.001) with both ICRP and SRP groups
improving from before to after treatment (table 2). There was
also a significant program by time interaction effect
(F1,545.66, P.021), suggesting that the participants in the
ICRP showed greater improvement from before to after treatment (table 3). The ICRP group exhibited over twice the
magnitude of treatment effect on total CIQ than the participants
receiving SRP did (ES, 1.20 vs 0.49).
Analysis of CIQ subscales showed significant pretreatment
versus posttreatment main effects for home integration
Table 3: ANOVA for Type of Treatment Program
and Before and After Treatment CIQ Scores
Source
Sum of
Squares
df
Mean
Square
Significance
CIQ
Program
CIQ by program
412.67
15.76
57.69
1
1
1
412.67
15.76
57.69
40.49
0.47
5.66
.000
.497
.021
.43
.01
.10
(F1,543.44, P.001), social integration (F1,5418.81,
P.001), and productivity (F1,5412.51, P.001). Significant
program by time interaction effects were found for home
integration (F1,544.08, P.048) and productivity (F1,548.29,
P.006) but not for social integration.
Among the participants receiving ICRP, 52% showed clinically significant improvement on the CIQ compared with 31%
of participants receiving SRP. Among SRP participants, 7%
showed clinically significant decline on the CIQ, whereas none
of the ICRP participants exhibited significant decline. Using
clinically significant improvement on the CIQ as the index of
a positive outcome, the ICRP treatment represents a relative
benefit of 68% and an odds ratio of 2.41 (95% CI, 0.8 7.2); in
other words, ICRP participants were almost 2.5 times more
likely than SRP participants to achieve a positive outcome.
Satisfaction with functioning after treatment. At completion of treatment, SRP participants expressed greater satisfaction with their community functioning than did ICRP participants (see table 2). There was a notable tendency for more SRP
participants to indicate that they were very satisfied with all
aspects of their community functioning; this was true of 6 SRP
participants (21%) but only 1 ICRP participant (4%). The
overall difference between groups on the QCI was statistically
significant (Mann-Whitney U240, P.03; ES.57). The
SRP participants also tended to report greater satisfaction with
their cognitive functioning (see table 2), but the overall difference between groups on the QCOG was not significant
(ES.38).
Neither total CIQ nor any of the CIQ subscales were related
to the QCI. However, the QCOG was significantly related to
posttreatment total CIQ (Spearman .42, P.001), home
integration (.41, P.002), and social integration (.36,
P.007), although not to productivity (.06). The relation
between posttreatment CIQ and QCOG scores was particularly
apparent for ICRP participants (.55, P.005) compared
with SRP participants (.36, P.051).
To evaluate what other factors were related to CIQ and
QCIQ outcomes, we conducted stepwise linear regressions
with pretreatment CIQ total score, age, education, gender, time
postinjury, and type of treatment as predictor variables and
posttreatment CIQ, QCI, and QCOG as concurrent indicator
variables. The CIQ outcome was best predicted by the QCOG
(P.001), initial CIQ (P.001), and treatment program
(P.02), with this model accounting for slightly more than one
Arch Phys Med Rehabil Vol 85, June 2004
948
INTENSIVE COGNITIVE REHABILITATION FOR TBI, Cicerone
third of the variance associated with CIQ outcomes (adjusted
R2.39). Satisfaction with community functioning (QCI) was
best predicted by time after injury in addition to QCOG score
(adjusted R2.32, P.001). A negative coefficient (.31)
existed between time after injury and QCI score, indicating that
more recent injury was associated with greater satisfaction with
community functioning. No additional variables contributed to
the prediction of satisfaction with cognitive functioning
(QCOG) after taking into consideration the significant relation
between the QCOG and the CIQ and QCI measures (adjusted
R2.36, P.001).
Neuropsychologic functioning for participants receiving
ICRP. Change in neuropsychologic functioning from before
to after treatment was evaluated for ICRP participants with
repeated-measures ANOVA, with significant CIQ change as a
between-subjects factor. Participants who received ICRP
showed significant improvement of their overall neuropsychologic functioning from before to after treatment (F48.39,
P.001; ES.60) (see table 2). Post hoc analyses of individual
measures were conducted using Bonferroni adjustments to
adjust the level of significance to P less than .008. These
analyses indicated significant improvements on the TMT-A
(P.002), CVLT (P.007), and RCF (P.002).
Improvement on overall neuropsychologic functioning (differences between pretreatment and posttreatment T scores) was
associated with improvement on total CIQ raw scores (.42,
P.03). We found a significant interaction between pretreatment and posttreatment neuropsychologic functioning and clinically significant CIQ change, with participants who showed
clinically significant improvement on the CIQ showing greater
improvement on overall neuropsychologic functioning
(F4.47, P.045) and TMT-B (F12.89, P.001).
Neither overall neuropsychologic functioning T score
(.15) nor change in neuropsychologic functioning T score
(.03) were related to participants subjective report of satisfaction with cognitive functioning.
DISCUSSION
Results of this prospective, observational study support the
effectiveness of an intensive, holistic, postacute program of
cognitive rehabilitation compared with an alternative program
of neurorehabilitation for persons with TBI. Although both
groups improved with treatment, the participants receiving
ICRP showed significantly greater improvements in community integration than participants receiving standard rehabilitation. Over half the ICRP participants showed clinically significant improvement in their community functioning, compared
with about one third of those who received standard neurorehabilitation. Those receiving ICRP were over twice as likely to
exhibit clinically significant improvement as those receiving
SRP. Participants receiving ICRP also showed significant improvement in their overall neuropsychologic functioning, particularly in the areas of attention and processing speed and
immediate-memory recall. Improvements in neuropsychologic
functioning were greater for those participants who showed
clinically significant improvement in their community integration over the course of treatment. Improvement on a measure of
complex attention and executive functioning was most directly
related to improvement in community integration, a relationship that has been suggested previously.31,32 The differential
benefit of ICRP on community integration was evident, despite
ICRP participants being further after injury and having lower
functioning before treatment. These 2 factors appear to be
potentially negative prognostic influences8,33 and might have
been expected to reduce the probability of finding a significant
treatment effect for the persons receiving ICRP.
Arch Phys Med Rehabil Vol 85, June 2004
Despite making greater improvements in community integration, participants who received ICRP did not report greater
satisfaction with their community functioning. In fact, there
was a tendency for SRP participants to report greater satisfaction, although this may be related to the fact that they were
earlier after injury. Many of the patients in the SRP were only
several months after injury and had limited experience resuming their preinjury responsibilities. In contrast, the persons in
the ICRP program were significantly further after injury, and
many had already experienced difficulty with their attempts to
resume functioning in their communities. During the acute
period of rehabilitation and recovery, patients with TBI are
more likely to recognize physical impairments than cognitive
impairments,34,35 and poorer awareness of impairments is associated with reports of greater life satisfaction.36 Thus, there
may be a general tendency for persons who are earlier after
injury, who have not fully experienced difficulties associated
with their impairments, to feel more satisfied with their level of
community functioning. Although self-reported cognitive difficulties are minimal initially after injury, they may increase
significantly over the first year of recovery from TBI as people
become more aware of their cognitive impairments.34
The relation between community functioning and satisfaction appears to become more complex over the postacute
course of recovery from TBI. Our results are consistent with
previous studies that have found a marginal relationship between community integration and QOL after TBI.13,19-21 The
dissociation between functional outcomes and subjective wellbeing has been noted, in particular, for persons with TBI who
are many years after injury.14,15 These findings again suggest
that community functioning and satisfaction with functioning
are distinct and separable aspects of participants experience
that must be considered in the design and evaluation of rehabilitation programs for persons with TBI.
Satisfaction with cognitive functioning was strongly related
to participants level of community integration after treatment,
and this relationship was most apparent for those who received
the ICRP. The relation between satisfaction with cognitive
functioning and community integration may reflect participants perceived self-efficacy regarding their functioning. Perceived self-efficacy refers to the individuals belief and judgments of his/her capability to accomplish a specific task or to
attain a designated level of performance and is mediated
through the process of cognitive self-appraisal.37 Both greater
perceived self-efficacy and greater subjective well-being appear to reflect the congruence of ones expectations and
achievements.38,39 Among patients with physical disease, functional disability is better predicted by perceived self-efficacy
than by the degree of actual physical impairment or duration of
illness.37,40-44 Perceived self-efficacy regarding cognitive abilities is also predictive of actual cognitive performance,45,46
including the degree of improvement in cognitive functioning
after training in compensatory strategies.47,48 In the current
study, improvements in neuropsychologic functioning and satisfaction with cognitive functioning were not related to each
other, but each contributed positively to community integration
after intensive cognitive rehabilitation. This finding again suggests that the relation between objective indices of severity of
TBI or impairments, functional outcomes, and QOL are moderated by the subjective meanings and values assigned by
patients. To be effective, rehabilitation after TBI must address
patients attitudes and beliefs in addition to their cognitive
abilities; remediation of cognitive abilities may have more
generalized effects if it increases self-efficacy beliefs as well as
trains cognitive skills.49 Perceived self-efficacy may be enhanced by interventions that facilitate an understanding of
INTENSIVE COGNITIVE REHABILITATION FOR TBI, Cicerone
environmental and task demands, provide training that improves individuals understanding of how to use their abilities
successfully, and provide feedback to correct inaccurate personal or causal attributions.50 The impact of self-efficacy beliefs on health-related outcomes is also mediated by selfregulatory processesself monitoring, goal setting, cognitive
self-appraisal, and affective self-evaluation.51 These are integral components of ICRP.
Our study has several limitations in its methods. The standard treatment condition in our study consisted of relatively
comprehensive, multidisciplinary, neuropsychologic rehabilitation. Therefore, our findings are likely to underestimate the
difference that would be found if we were to compare ICRP
with the type of services that may actually be available for
many persons with TBI. The interpretation and generalization
of results is also tempered by sampling limitations: specifically,
the confounding of time after injury with treatment condition.
That is, there was a systematic selection bias in enrolling, into
the more intensive, holistic treatment program, participants
who were further after injury with persistent disability, whereas
participants who were more recently injured and were expected
to make additional recovery received the more limited treatment regimen. The ICRP participants also exhibited slightly
worse community integration before treatment, but this difference was no longer apparent after treatment. Although the
difference in pretreatment CIQ scores was not significant, it
may have contributed to the finding of a differential treatment
effect in the ICRP group. As recently noted, time since injury
and level of disability appear to be important characteristics in
determining the appropriate form of postacute brain injury
rehabilitation.33 Although these differences limit the ability to
generalize our results, it is notable that this selection bias might
be expected to reduce the probability of observing a differential
benefit for those persons with TBI who received the ICRP. The
present findings suggest, at least, that persons with TBI who are
less recently injured and have experienced persisting disability
can be successfully treated, even many years after injury, with
a more intensive and holistic approach to cognitive rehabilitation.
The relation among neurocognitive impairment, functional
disability, and QOL after rehabilitation for TBI merits additional investigation. There is a need to validate measures of
QOL for persons with TBI and, specifically, to develop measures that are sensitive to the participants views of changes in
subjective well-being as a result of treatment. We did not
obtain systematic follow-up information as part of our study. In
the future, it will be important to assess the maintenance and
stability of community integration and QOL after TBI rehabilitation.7
CONCLUSIONS
The results of our controlled, observational study indicate
significant clinical benefit of ICRP for persons with TBI.
Although both groups improved, the participants receiving
ICRP were over twice as likely to show clinically significant
improvement in community integration as those receiving SRP,
despite being longer after injury and having slightly worse
community functioning before treatment. Participants QOL,
assessed by their satisfaction with community functioning, was
not related to level of community integration. Satisfaction with
cognitive functioning did not differ between groups but did
make a significant contribution to community integration, particularly for those participants receiving ICRP. The construct
of perceived self-efficacy has received limited attention in
relation to brain injury rehabilitation and may have considerable heuristic and explanatory value for understanding the
949
effective ingredients of interventions. Prospective controlled
studies are needed to compare the effectiveness of different
forms of cognitive rehabilitation and to assess the patient
characteristics and treatment ingredients that contribute to positive outcomes. Future efforts to assess cognitive functioning
and social participation after TBI rehabilitation also must consider that functional disability and subjective well-being represent distinct rehabilitation outcomes.
References
1. Malec JF, Basford JS. Post-acute brain injury rehabilitation. Arch
Phys Med Rehabil 1996;77:198-207.
2. Malec JF, Smigielski JS, DePompolo RW, Thompson JM. Outcome evaluation and prediction in a comprehensive-integrated
post-acute outpatient brain injury rehabilitation programme. Brain
Inj 1993;7:15-29.
3. Ben-Yishay Y, Gold J. Therapeutic milieu approach to neuropsychological rehabilitation. In: Woods RL, editor. Neurobehavioral
sequelae of traumatic brain injury. New York: Taylor & Francis;
1990. p 194-218.
4. Rattok J, Ben-Yishay Y, Ezrachi O, et al. Outcome of different
treatment mixes in a multidimensional neuropsychological rehabilitation program. Neuropsychology 1992;6:395-415.
5. Cicerone KD, Dahlberg C, Kalmar K, et al. Evidence-based cognitive rehabilitation: recommendations for clinical practice. Arch
Phys Med Rehabil 2000;81:1596-615.
6. Malec JF. Impact of comprehensive day treatment on societal
participation for persons with acquired brain injury. Arch Phys
Med Rehabil 2001;82:885-95.
7. Sander AM, Roebuck TM, Struchen M, Sherer M, High WM.
Long-term maintenance of gains obtained in postacute rehabilitation by persons with traumatic brain injury. J Head Trauma
Rehabil 2001;16:356-73.
8. Seale GS, Caroselli JS, High WM, Becker CL, Neese LE, Scheibel R. Use of the Community Integration Questionnaire (CIQ) to
characterize changes in functioning for individuals with traumatic
brain injury who participated in a post-acute brain injury rehabilitation programme. Brain Inj 2002;16:955-67.
9. Willer B, Rosenthal M, Kreutzer JS, Gordon WA, Rempel R.
Assessment of community integration following rehabilitation for
traumatic brain injury. J Head Trauma Rehabil 1993;8(2):75-87.
10. Dijkers M. Measuring the long-term outcomes of traumatic brain
injury: a review of Community Integration Questionnaire studies.
J Head Trauma Rehabil 1997;12(6):74-91.
11. Webb CR, Wrigley M, Yoels W, Fine PR. Explaining quality of
life for persons with traumatic brain injuries 2 years after injury.
Arch Phys Med Rehabil 1995;76:1113-9.
12. Corrigan JD, Smith-Knapp K, Granger CV. Outcomes in the first
5 years after traumatic brain injury. Arch Phys Med Rehabil
1998;79:298-305.
13. Corrigan JD, Bogner JA, Mysiw WJ, Clinchot D, Fugate L. Life
satisfaction after traumatic brain injury. J Head Trauma Rehabil
2001;16:543-55.
14. Bezner JR, Hunter DL. Wellness perception in persons with
traumatic brain injury and its relation to functional independence.
Arch Phys Med Rehabil 2001;82:787-92.
15. Koskinen S. Quality of life 10 years after a severe traumatic brain
injury (TBI): the perspective of the injured and the closest relative.
Brain Inj 1998;12:631-48.
16. Schalen W, Hansson L, Nordstom G, Nordstrom CH. Psychosocial outcome 5-8 years after severe traumatic brain lesions and the
impact of rehabilitation services. Brain Inj 1994;8:49-64.
17. Steadman-Pare D, Colantonio A, Ratcliff G, Chase S, Vernich L.
Factors associated with perceived quality of life many years after
traumatic brain injury. J Head Trauma Rehabil 2001;16:330-42.
18. Azouvi P, Mailhan L, Truelle JL, Dazor A. Quality of life 2 to 6
years after a severe traumatic brain injury. Paper presented at: The
4th World Congress on Brain Injury: 2001 May 59; Turin, Italy.
19. Heinemann AW, Whiteneck GG. Relationships among impairment, disability, handicap and life satisfaction in persons with
traumatic brain injury. J Head Trauma Rehabil 1995;10(4):54-63.
Arch Phys Med Rehabil Vol 85, June 2004
950
INTENSIVE COGNITIVE REHABILITATION FOR TBI, Cicerone
20. Burleigh SA, Farber RS, Gillard M. Community integration and
life satisfaction after traumatic brain injury: long-term findings.
Am J Occup Ther 1998;52:45-52.
21. Smith JL, Magill-Evans J, Brintnell A. Life satisfaction following
traumatic brain injury. Can J Rehabil 1998;11:131-40.
22. Bergquist T, Boll TJ, Corrigan JD, et al. Neuropsychological
rehabilitation: proceedings of a consensus conference. J Head
Trauma Rehabil 1994;9(4):50-61.
23. Zakzanis KK. Statistics to tell the truth, the whole truth, and
nothing but the truth: formulae, illustrative numerical examples,
and heuristic interpretation of effect size analyses for neuropsychological researchers. Arch Clin Neuropsychol 2001;16:653-67.
24. Jacobson NS, Truax P. Clinical significance: a statistical approach
to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991;59:12-9.
25. Bullinger M, Azouvi P, Brooks N, et al. Quality of life in participants with traumatic brain injury basic issues, assessment and
recommendations. Restor Neurol Neurosci 2002;20:111-24.
26. Johnston MV, Miklos CS. Activity-related quality of life in rehabilitation and traumatic brain injury. Arch Phys Med Rehabil
2002;83(Suppl 2):26-38.
27. Heaton RK, Grant I, Matthews CG. Comprehensive norms for an
expanded Halstead-Reitan battery. Odessa (FL): Psychological
Assessment Resources; 1991.
28. Delis DC, Kramer JH, Kaplan E, Ober BA. California Verbal
Learning Test, research edition: manual. New York: Psychological Corp; 1987.
29. Meyers JF, Meyers KR. Rey Complex Figure Test and Recognition Trial: professional manual. Odessa (FL): Psychological Assessment Resources; 1995.
30. Gladsjo JA, Schuman CC, Evans JD, Peavy BM, Miller SW,
Heaton RK. Norms for letter and category fluency: demographic
corrections for age, education and ethnicity. Assessment 1999;6:
147-78.
31. Millis SR, Rosenthal M, Lourie IF. Predicting community integration after traumatic brain injury with neuropsychological measures. Int J Neurosci 1994;79:165-7.
32. Hanks RA, Rapport LJ, Millis SR, Deshpande SA. Measures of
executive functioning as predictors of functional ability and social
integration in a rehabilitation sample. Arch Phys Med Rehabil
1999;80:1030-7.
33. Malec JF, Degiorgio L. Characteristics of successful and unsuccessful completers of 3 postacute brain injury rehabilitation pathways. Arch Phys Med Rehabil 2002;83:1759-64.
34. Powell JM, Machamer JE, Temkin NR, Dikmen SS. Self-report of
extent of recovery and barriers to recovery after traumatic brain
injury: a longitudinal study. Arch Phys Med Rehabil 2001;82:
1025-30.
Arch Phys Med Rehabil Vol 85, June 2004
35. Sherer M, Hart T, Nick TG, Whyte J, Nakese-Thompson R,
Yablon SA. Early impaired self-awareness after traumatic brain
injury. Arch Phys Med Rehabil 2003;84:168-76.
36. Evans C, Sherer M, Nakase-Thompson R, Novack T, Nick T.
Early impaired self-awareness, depression, and subjective wellbeing following TBI. J Int Neuropsychol Soc 2003;9:253-4.
37. Bandura A. Self-efficacy: the exercise of control. New York: WH
Freeman; 1997.
38. Dijkers M. Measuring quality of life. In: Fuhrer MJ, editor.
Assessing medical rehabilitation practices: the promise of outcomes research. Baltimore: PH Brookes; 1997. p 153-80.
39. Fuhrer MJ. Subjective well being: implications for medical rehabilitation outcomes and models of disablement. Am J Phys Med
Rehabil 1994;73:358-64.
40. Kohler CL, Fish L, Greene PG. The relationship of perceived
self-efficacy to quality of life in chronic obstructive pulmonary
disease. Health Psychol 2002;21:610-4.
41. Robinson-Smith G, Johnston MV, Allen J. Self-care self-efficacy,
quality of life, and depression after stroke. Arch Phys Med Rehabil 2000;81:460-4.
42. Holden G. The relationship of self-efficacy appraisals to subsequent health-related outcomes: a meta-analysis. Soc Work Health
Care 1991;16:53-93.
43. Holroyd KA, Penzien DB, Hursey KG, et al. Change mechanisms
in EMG biofeedback training: cognitive changes underlying improvements in tension headache. J Consult Clin Psychol 1984;52:
1039-53.
44. Schiaffiano KM, Revenson TA, Gibofshy A. Assessing the impact
of self-efficacy beliefs on adaptation to rheumatoid arthritis. Arthritis Care Res 1991;4:150-7.
45. Berry JM, West RL, Dennehey D. Reliability and validity of the
memory self-efficacy questionnaire. Dev Psychol 1989;25:701-13.
46. Lachman ME, Steinberg ES, Trotter SD. Effects of control beliefs
and attributions on memory self-assessments and performance.
Psychol Aging 1987;2:266-71.
47. Lachman ME, Weaver SL, Bandura MM, Elliott E, Lewkowicz
CJ. Improving memory and control beliefs through cognitive
restructuring and self-generated strategies. J Gerontol 1992;47:
P293-9.
48. Rebok GW, Balcerak LJ. Memory self-efficacy and performance
differences in young and old adults: the effect of mnemonic
training. Dev Psychol 1989;25:714-21.
49. Bandura A. Regulation of cognitive processes through perceived
self-efficacy. Dev Psychol 1989;25:729-35.
50. Gist M, Mitchell T. Self-efficacy: a theoretical analysis of its
determinants and malleability. Acad Manage Rev 1992;17:183211.
51. Bandura A. Health promotion from the perspective of social
cognitive theory. Psychol Health 1998;13:623-49.
También podría gustarte
- Multimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital DiversionDe EverandMultimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital DiversionAún no hay calificaciones
- Chapter 1 1Documento11 páginasChapter 1 1NICA ALFANTEAún no hay calificaciones
- Effects of Cognitive Remediation On Cognitive and Social Functions in Individuals With SchizophreniaDocumento14 páginasEffects of Cognitive Remediation On Cognitive and Social Functions in Individuals With SchizophreniaLu LopezAún no hay calificaciones
- Final Cat 2Documento20 páginasFinal Cat 2api-458845384Aún no hay calificaciones
- Fledderus 2010Documento7 páginasFledderus 2010VIMAún no hay calificaciones
- Occupational Therapy and Mental Health - Add Summary and Bullet PointsDocumento11 páginasOccupational Therapy and Mental Health - Add Summary and Bullet Pointsapi-339190475100% (1)
- Life Satisfaction After TBIDocumento3 páginasLife Satisfaction After TBIeva.mmAún no hay calificaciones
- Psychosocial Rehabilitation and Recovery: Exploring The RelationshipDocumento11 páginasPsychosocial Rehabilitation and Recovery: Exploring The RelationshipmariajoaomoreiraAún no hay calificaciones
- Predictors of Psych Intervention To Promote Health Behaviour Adherence in HF 2021Documento14 páginasPredictors of Psych Intervention To Promote Health Behaviour Adherence in HF 2021Bob JoeAún no hay calificaciones
- Evidence-Based Cognitive Rehabilitation: Updated Review of The Literature From 2003 Through 2008Documento12 páginasEvidence-Based Cognitive Rehabilitation: Updated Review of The Literature From 2003 Through 2008hsvm1989Aún no hay calificaciones
- SGRDGFGD FullDocumento9 páginasSGRDGFGD FullDidikPrasetyoSuliAún no hay calificaciones
- Mental Health First Aid Training: Review of Evaluation StudiesDocumento3 páginasMental Health First Aid Training: Review of Evaluation StudiesLiz RoxAún no hay calificaciones
- THE ROLE OF OCCUPATONAL THERAPY IN THE RECOVERY OF PATIENTS IN BUTABIKA HOSPITAL (AutoRecovered)Documento41 páginasTHE ROLE OF OCCUPATONAL THERAPY IN THE RECOVERY OF PATIENTS IN BUTABIKA HOSPITAL (AutoRecovered)samuelAún no hay calificaciones
- Mindfulness - Substance Abuse in A Therapeutic CommunityDocumento6 páginasMindfulness - Substance Abuse in A Therapeutic CommunityCarmo de SousaAún no hay calificaciones
- Chan Wu YiDocumento8 páginasChan Wu YiAlejandra SacanellAún no hay calificaciones
- Physical Therapy After Spinal Cord Injury: A Systematic Review of Treatments Focused On ParticipationDocumento10 páginasPhysical Therapy After Spinal Cord Injury: A Systematic Review of Treatments Focused On ParticipationInaauliahanAún no hay calificaciones
- Bedard Et Al 2003 MindfulnessDocumento11 páginasBedard Et Al 2003 MindfulnessMarta SanchezAún no hay calificaciones
- 1 s2.0 S0022399920301847 MainDocumento10 páginas1 s2.0 S0022399920301847 MainMaria SilaghiAún no hay calificaciones
- Article 1Documento2 páginasArticle 1api-308016174Aún no hay calificaciones
- RRL Chapter 3Documento4 páginasRRL Chapter 3Blescel AntongAún no hay calificaciones
- Cognitive Enhancement Therapy in Early SchizophreniaDocumento15 páginasCognitive Enhancement Therapy in Early SchizophreniaMohdshuaib SaifiAún no hay calificaciones
- Effects of Cognitive Remediation On Cognitive and SocialDocumento14 páginasEffects of Cognitive Remediation On Cognitive and SocialHarumy NakayamaAún no hay calificaciones
- MindfulnessDocumento14 páginasMindfulnessRosa SecoAún no hay calificaciones
- Mobile Health (Mhealth) Versus Clinic-Based Group Intervention For People With Serious Mental Illness: A Randomized Controlled TrialDocumento8 páginasMobile Health (Mhealth) Versus Clinic-Based Group Intervention For People With Serious Mental Illness: A Randomized Controlled TrialOlivia NasarreAún no hay calificaciones
- Ware 2003Documento9 páginasWare 2003DoniLeiteAún no hay calificaciones
- Neurorehab StrokeDocumento9 páginasNeurorehab StrokekapilphysioAún no hay calificaciones
- The Effect of A Community Mental Health Training Program For Multidisciplinary Staff PDFDocumento5 páginasThe Effect of A Community Mental Health Training Program For Multidisciplinary Staff PDFAzuan SalimAún no hay calificaciones
- Telerehabilitation 4Documento13 páginasTelerehabilitation 4Jerrin JacobAún no hay calificaciones
- Ariss 2019Documento11 páginasAriss 2019Vincent VeldmanAún no hay calificaciones
- The Impact of Therapeutic Community in The Perception of A Probationer in Quirino Province PhilippinesDocumento5 páginasThe Impact of Therapeutic Community in The Perception of A Probationer in Quirino Province PhilippinesMelissa BubosAún no hay calificaciones
- Implementing Recovery-Oriented EBPDocumento18 páginasImplementing Recovery-Oriented EBPLuigi BassoAún no hay calificaciones
- Occt 643 Cat Evidence Table Worksheet FinalDocumento22 páginasOcct 643 Cat Evidence Table Worksheet Finalapi-260120536Aún no hay calificaciones
- Mindfulnees Self Compassion WorkplaceDocumento9 páginasMindfulnees Self Compassion WorkplaceMarta Martínez PalmerAún no hay calificaciones
- Community Based Rehabilitation Special IssuesDocumento16 páginasCommunity Based Rehabilitation Special IssuesMike F MartelliAún no hay calificaciones
- Rheumatoid 4Documento14 páginasRheumatoid 4Mohamed AbozeidAún no hay calificaciones
- Web Link: Published: March 2016 Doi: Journal: Rejuvenation Research 19Documento6 páginasWeb Link: Published: March 2016 Doi: Journal: Rejuvenation Research 19sadia nadeemAún no hay calificaciones
- Rehabilitation of Social Communication Skills in PDocumento10 páginasRehabilitation of Social Communication Skills in Pt6zyhmkdbrAún no hay calificaciones
- Social Rehab Process in Long-Term ConditionsDocumento12 páginasSocial Rehab Process in Long-Term ConditionsClara PosadaAún no hay calificaciones
- Reflective Writing - Pgi ManimtimDocumento22 páginasReflective Writing - Pgi ManimtimKim Adarem Joy ManimtimAún no hay calificaciones
- Mancini 2008Documento8 páginasMancini 2008StelianAún no hay calificaciones
- Schizophr Bull 2009 Wunderink 362 9Documento8 páginasSchizophr Bull 2009 Wunderink 362 9kurniafniatiAún no hay calificaciones
- Cognitive-Behavioural Therapy For Personal Recovery of Patients With Schizophrenia: A Systematic Review and Meta-AnalysisDocumento13 páginasCognitive-Behavioural Therapy For Personal Recovery of Patients With Schizophrenia: A Systematic Review and Meta-AnalysisLydia AmaliaAún no hay calificaciones
- Harris Et Al., 2013 (BA - Depression - Physical Illness)Documento6 páginasHarris Et Al., 2013 (BA - Depression - Physical Illness)Alba EneaAún no hay calificaciones
- Occupational Therapy For People With Psychotic ConditionsDocumento29 páginasOccupational Therapy For People With Psychotic Conditionssaurav.das2030Aún no hay calificaciones
- Analisis Jurnal Metode Pico Rahman R AkubaDocumento20 páginasAnalisis Jurnal Metode Pico Rahman R AkubaKilinik MirahAún no hay calificaciones
- Guided Self-Help Works Randomized Waitlist Controlled Trial ofDocumento17 páginasGuided Self-Help Works Randomized Waitlist Controlled Trial ofMaria GabrielaAún no hay calificaciones
- Effects of Horticultural Therapy On Elderly ' Health: Protocol of A Randomized Controlled TrialDocumento10 páginasEffects of Horticultural Therapy On Elderly ' Health: Protocol of A Randomized Controlled Trialaldi9aAún no hay calificaciones
- A Systematic Review and Meta-Analysis of Randomised Controlled Trials of Peer Support For People With Severe Mental IllnessDocumento12 páginasA Systematic Review and Meta-Analysis of Randomised Controlled Trials of Peer Support For People With Severe Mental IllnessBryan PrasetyoAún no hay calificaciones
- Head and Neck CancerDocumento15 páginasHead and Neck CancerFlorinaAún no hay calificaciones
- Kobori Osamu Does Perfectionism Impact Adherence To 2019Documento5 páginasKobori Osamu Does Perfectionism Impact Adherence To 2019Sean EscalderonAún no hay calificaciones
- Optimism: The Biology of HopeDocumento6 páginasOptimism: The Biology of HopeNaga Raj SAún no hay calificaciones
- Technology-Enhanced 4active Intervention Impacting Psychological Well-Being and Physical Activity Among Older Adults: A Pilot StudyDocumento12 páginasTechnology-Enhanced 4active Intervention Impacting Psychological Well-Being and Physical Activity Among Older Adults: A Pilot StudySofía PinoAún no hay calificaciones
- Positive Psychology and HealthDocumento11 páginasPositive Psychology and HealthMónica GarzaAún no hay calificaciones
- Alzh 1 ART Intervenciones Psicosocial y Conductual en Demencia-BurnsDocumento5 páginasAlzh 1 ART Intervenciones Psicosocial y Conductual en Demencia-BurnsKitzia AveiriAún no hay calificaciones
- 1 s2.0 S109830152034465X MainDocumento10 páginas1 s2.0 S109830152034465X MainHesty YuliasariAún no hay calificaciones
- Evaluation of A Life Skills Group For Brain Injury Patients On An Acute Neurological Rehabilitation UnitDocumento1 páginaEvaluation of A Life Skills Group For Brain Injury Patients On An Acute Neurological Rehabilitation UnitJodiMBrownAún no hay calificaciones
- Patient and Family Member Factors Influencing Outcomes of Poststroke Inpatient RehabilitationDocumento9 páginasPatient and Family Member Factors Influencing Outcomes of Poststroke Inpatient RehabilitationAdelya YuzyAún no hay calificaciones
- Integrated Group Treatment For People Experiencing Mental Health-Substance Use Problems, Kathleen SciaccaDocumento14 páginasIntegrated Group Treatment For People Experiencing Mental Health-Substance Use Problems, Kathleen SciaccaKathleen Sciacca, MA - Sciacca Comprehensive Service Dev. Dual Diagnosis; Motivational Interviewing100% (1)
- Moore Ar Proposal FinalDocumento15 páginasMoore Ar Proposal Finalapi-604372078Aún no hay calificaciones
- The Effectiveness of A Feminist-Informed, Individualised Counselling Intervention For The Treatment of Eating Disorders: A Case Series StudyDocumento12 páginasThe Effectiveness of A Feminist-Informed, Individualised Counselling Intervention For The Treatment of Eating Disorders: A Case Series StudyJasmeen ParmarAún no hay calificaciones
- ESENER 2019 Policy Brief ENDocumento64 páginasESENER 2019 Policy Brief ENBegoña MartinezAún no hay calificaciones
- Misuse of Statistical Tests Inarchives of ClinicalNeuropsychologypublicationsDocumento7 páginasMisuse of Statistical Tests Inarchives of ClinicalNeuropsychologypublicationsBegoña MartinezAún no hay calificaciones
- Psychosocial Work Factors and Stress DisordersDocumento10 páginasPsychosocial Work Factors and Stress DisordersBegoña MartinezAún no hay calificaciones
- The Effectiveness of Mindfulness Based Programs In.4Documento9 páginasThe Effectiveness of Mindfulness Based Programs In.4Begoña MartinezAún no hay calificaciones
- 1 s2.0 S0887617704001209 MainDocumento6 páginas1 s2.0 S0887617704001209 MainBegoña MartinezAún no hay calificaciones
- A Review of Mushrooms in Human Nutrition and HealthDocumento14 páginasA Review of Mushrooms in Human Nutrition and HealthBegoña MartinezAún no hay calificaciones
- Better Safe Than Sorry: Methods For Risk Assessment of Psychosocial HazardsDocumento18 páginasBetter Safe Than Sorry: Methods For Risk Assessment of Psychosocial HazardsBegoña MartinezAún no hay calificaciones
- Occupational Stress Among Health Workers of A University HospitalDocumento6 páginasOccupational Stress Among Health Workers of A University HospitalBegoña MartinezAún no hay calificaciones
- Preventing Psychosocial Risks at Work: An Evaluation Study of Labour Inspectorate InterventionsDocumento8 páginasPreventing Psychosocial Risks at Work: An Evaluation Study of Labour Inspectorate InterventionsBegoña MartinezAún no hay calificaciones
- Tryptophan-Rich Diet Is Negatively Associated Withdepression and Positively Linked To Social CognitionDocumento7 páginasTryptophan-Rich Diet Is Negatively Associated Withdepression and Positively Linked To Social CognitionBegoña MartinezAún no hay calificaciones
- International Journal of Nursing Studies: ReviewDocumento14 páginasInternational Journal of Nursing Studies: ReviewBegoña MartinezAún no hay calificaciones
- Neuropsychologia: Andrew H. Bell, Janet H. BultitudeDocumento9 páginasNeuropsychologia: Andrew H. Bell, Janet H. BultitudeBegoña MartinezAún no hay calificaciones
- International Journal of Nursing Studies: Constanze Leineweber, Staffan Marklund, Gunnar Aronsson, Klas GustafssonDocumento9 páginasInternational Journal of Nursing Studies: Constanze Leineweber, Staffan Marklund, Gunnar Aronsson, Klas GustafssonBegoña MartinezAún no hay calificaciones
- Amigurumi White Rabbit Free Crochet Pattern - AmigurumiDocumento18 páginasAmigurumi White Rabbit Free Crochet Pattern - AmigurumiBegoña Martinez0% (1)
- 1 s2.0 S1556086415317809 MainDocumento7 páginas1 s2.0 S1556086415317809 MainBegoña MartinezAún no hay calificaciones
- Regulation ofN-Methyl-D-aspartic Acid (NMDA) Receptors Bymetabotropic Glutamate Receptor 7Documento11 páginasRegulation ofN-Methyl-D-aspartic Acid (NMDA) Receptors Bymetabotropic Glutamate Receptor 7Begoña MartinezAún no hay calificaciones
- 1 s2.0 S1059131116301595 MainDocumento8 páginas1 s2.0 S1059131116301595 MainLuisa FernandaAún no hay calificaciones
- Confounding Obscures Our View, Effect Modification Is Part of RealityDocumento2 páginasConfounding Obscures Our View, Effect Modification Is Part of RealityBegoña MartinezAún no hay calificaciones
- Baremos NeuronormaDocumento21 páginasBaremos NeuronormaDebbieAún no hay calificaciones
- Research in Developmental Disabilities: Matilde Taddei, Sara BulgheroniDocumento6 páginasResearch in Developmental Disabilities: Matilde Taddei, Sara BulgheroniBegoña MartinezAún no hay calificaciones
- A Motion To Exclude and The Fixed' Versus Flexible' Battery in Forensic' Neuropsychology: Challenges To The Practice of Clinical NeuropsychologyDocumento7 páginasA Motion To Exclude and The Fixed' Versus Flexible' Battery in Forensic' Neuropsychology: Challenges To The Practice of Clinical NeuropsychologyBegoña MartinezAún no hay calificaciones
- Forensic Neuropsychology: Are We There Yet?: Jim HomDocumento19 páginasForensic Neuropsychology: Are We There Yet?: Jim HomBegoña MartinezAún no hay calificaciones
- National Academy of Neuropsychology: President's Address The Future of NeuropsychologyDocumento12 páginasNational Academy of Neuropsychology: President's Address The Future of NeuropsychologyBegoña MartinezAún no hay calificaciones
- FBI (Frontal Behabioral InventoryDocumento2 páginasFBI (Frontal Behabioral InventoryBegoña Martinez100% (1)
- Karate Form 1 Hand PositionsDocumento7 páginasKarate Form 1 Hand PositionsBegoña MartinezAún no hay calificaciones
- Crochet Project Planner Download 1Documento1 páginaCrochet Project Planner Download 1Begoña MartinezAún no hay calificaciones
- Karate Form 1 Hand PositionsDocumento7 páginasKarate Form 1 Hand PositionsBegoña MartinezAún no hay calificaciones
- Montreal Cognitive Assessment Basic English FINAL VERSION 4 June 2014Documento2 páginasMontreal Cognitive Assessment Basic English FINAL VERSION 4 June 2014Begoña Martinez100% (1)
- MoCA-Test-English - 7 - 3 June - 13 PDFDocumento1 páginaMoCA-Test-English - 7 - 3 June - 13 PDFBegoña Martinez100% (2)
- MoCA B Instructions FinalDocumento5 páginasMoCA B Instructions FinalsequoyahAún no hay calificaciones
- Methodology 3.1 VideostudyDocumento6 páginasMethodology 3.1 VideostudyZuzana ŠimkováAún no hay calificaciones
- Joseph Sereño's Criminology ProfileDocumento2 páginasJoseph Sereño's Criminology ProfileRoelineRosalSerenoAún no hay calificaciones
- Movers Speaking Test OverviewDocumento57 páginasMovers Speaking Test OverviewThu HợpAún no hay calificaciones
- Holistic Teacher Development LAC SessionDocumento2 páginasHolistic Teacher Development LAC SessionfrancisAún no hay calificaciones
- Todorov The Notion of LiteratureDocumento15 páginasTodorov The Notion of LiteratureSiddhartha PratapaAún no hay calificaciones
- Newsletter June 18 2012Documento26 páginasNewsletter June 18 2012Ken StaynerAún no hay calificaciones
- LiteratureDocumento6 páginasLiteratureMohammed EcoAún no hay calificaciones
- Ranking of Honors 3rd 1 9 2020Documento56 páginasRanking of Honors 3rd 1 9 2020RachelleGomezLatrasAún no hay calificaciones
- First Day of Second GradeDocumento21 páginasFirst Day of Second Gradeapi-268706556Aún no hay calificaciones
- Nutritional AssessmentDocumento7 páginasNutritional AssessmentCm MacaliaAún no hay calificaciones
- AF - Agri-Crop Production NC II 20151119 PDFDocumento26 páginasAF - Agri-Crop Production NC II 20151119 PDFFidel B. Diopita100% (7)
- Mobile: 6303779851: CH - VasaviDocumento2 páginasMobile: 6303779851: CH - VasaviOmprakashAún no hay calificaciones
- Ecotourism's Impact and Sustainable Development in SurinameDocumento14 páginasEcotourism's Impact and Sustainable Development in SurinameMaylene TobyAún no hay calificaciones
- CUET Maths Domain Chapter Wise: MixedDocumento19 páginasCUET Maths Domain Chapter Wise: MixedDivyansh Singh BaghelAún no hay calificaciones
- Houran - Do Online Matchmaking Tests WorkDocumento21 páginasHouran - Do Online Matchmaking Tests Workyasirzaidi1Aún no hay calificaciones
- Introduction To Paralegalism Instructors ManualDocumento12 páginasIntroduction To Paralegalism Instructors Manualonerussian11% (9)
- Trends, Networks, and Critical Thinking in the 21st CenturyDocumento21 páginasTrends, Networks, and Critical Thinking in the 21st CenturyJessie May CaneteAún no hay calificaciones
- Fol Admissions 2021-22 FaqsDocumento14 páginasFol Admissions 2021-22 FaqsYash RajAún no hay calificaciones
- My Final NagidDocumento36 páginasMy Final NagidRenalene BelardoAún no hay calificaciones
- Math7 - q1 - Mod12 - Arranging Real Numbers On A Number Line - v3Documento25 páginasMath7 - q1 - Mod12 - Arranging Real Numbers On A Number Line - v3Vicente TrinidadAún no hay calificaciones
- Accounting Modular LearningDocumento21 páginasAccounting Modular LearningClarissa Rivera VillalobosAún no hay calificaciones
- William M.A. Grimaldi-Aristotle, Rhetoric I. A Commentary - Fordham University Press (1980)Documento368 páginasWilliam M.A. Grimaldi-Aristotle, Rhetoric I. A Commentary - Fordham University Press (1980)racoonic100% (3)
- 00 B1 Practice Test 1 IntroductionDocumento6 páginas00 B1 Practice Test 1 IntroductionsalvaAún no hay calificaciones
- Division of Misamis Occidental Training Design Action Research Seminar Workshop Venue: TBA Date: TBA Time: 8:00 AM - 4:30 PM A. RationaleDocumento6 páginasDivision of Misamis Occidental Training Design Action Research Seminar Workshop Venue: TBA Date: TBA Time: 8:00 AM - 4:30 PM A. RationaleDENMARK100% (1)
- Mapeh Module 1Documento44 páginasMapeh Module 1Elaica Nicole MalekchanAún no hay calificaciones
- Peter Ghosh - Max Weber and 'The Protestant Ethic' - Twin Histories-Oxford University Press (2014) PDFDocumento421 páginasPeter Ghosh - Max Weber and 'The Protestant Ethic' - Twin Histories-Oxford University Press (2014) PDFvkozaevaAún no hay calificaciones
- Statements of Purpose Guidelines and Sample EssaysDocumento51 páginasStatements of Purpose Guidelines and Sample Essaysyawnbot botAún no hay calificaciones
- Organizational Behavior: Stephen P. RobbinsDocumento35 páginasOrganizational Behavior: Stephen P. RobbinsPariManiyarAún no hay calificaciones
- Pass4sure 400-101Documento16 páginasPass4sure 400-101Emmalee22Aún no hay calificaciones
- Kindergarten Unit Module 4 Practice Pages For Math at HomeDocumento10 páginasKindergarten Unit Module 4 Practice Pages For Math at HomeSarah PhalenAún no hay calificaciones