Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Update On BCS
Cargado por
doccommieTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Update On BCS
Cargado por
doccommieCopyright:
Formatos disponibles
An update on management of Budd-Chiari syndrome.
, 2014; 13 (3): 323-326
CONCISE
REVIEW
323
May-June, Vol. 13 No. 3, 2014: 323-326
An update on management of Budd-Chiari syndrome
Andrea Mancuso
Medicina Interna 1, ARNAS Civico-Di Cristina-Benfratelli, Palermo, Italy.
Epatologia e Gastroenterologia, Ospedale Niguarda C Granda, Milano, Italy.
ABSTRACT
The topic of this paper is to report an update on management of Budd-Chiari syndrome (BCS). Actually, the
flow-chart of BCS management comes from experts opinion and is not evidence-based due to the rarity
of BCS. Management of BCS follows a step-wise strategy. Anticoagulation and medical therapy should be
the first line treatment. Revascularization or TIPS in case of no response to medical therapy. OLT as a
rescue therapy. Surgery has limited but important space, especially in cases with high inferior vena cava
obstruction not suitable for endovascular treatment. However, no clear indication can actually be given
about the timing of different treatments. Moreover, there is some concern about treatment of some
subgroup of patients, especially regarding the risk of recurrence after liver transplantation. This paper
propose a new algorithm of BCS management suggesting an earlier therapeutic approach when clinical
signs are evident.
Key words. Ascites. TIPS. Liver transplantation. Surgery. Outcome.
The aim of this paper is to propose a new algorithm of BCS management. In fact, as it will be discussed, evidence is lacking about BCS due to the
rarity of the syndrome. We will see that some data
argue against the actual expectant strategy of BCS
management and suggest a more interventional
approach.
The topic of this paper is to report an update on
management of Budd-Chiari syndrome (BCS). BCS
is a rare disease with a generally worsening outcome without intervention. Following experts opinion
coming from not evidence-based experiences, BCS
management should follow a step-wise management.
In fact, medical therapy (anticoagulation, treatment
of underlying disease, symptomatic therapy of portal
hypertension complications) should be the first-line
treatment, angioplasty/stenting the second-line (in
patients with short-length stenoses not responding
to medical therapy), TIPS the next step (in patients
not responding to medical therapy and in case of no
response to, or stenoses unsuitable for, angioplasty/
Correspondence and reprint request: Andrea Mancuso, M.D.
Medicina Interna 1, ARNAS Civico, Piazzale Liotti 4, 90100, Palermo, Italy.
Tel.: 00393298997893, Fax: 00390916090252
E-mail: mancandrea@libero.it
Manuscript received: February 16,2014.
Manuscript accepted: February 25, 2014.
stenting) and liver transplantation (LT) the last
chance when TIPS is not effective. 1-3 Step-wise
management suggests moving forward when no
response to therapy appears.1
A therapeutic approach limited to short-length
stenoses is angioplasty/stenting, with a good medium
term outcome reported in some experience.4-6 However, no data can argue against the use of TIPS also in
the subgroup with short-length stenoses. In fact a
prospective comparison between TIPS and angioplasty/stenting has not been performed. Probably,
such a therapeutic choice in this subgroup of patients
should be personalized and based on local expertise.
The most frequent treatment for BCS is surely
TIPS.1-3 TIPS has been shown to be effective as BCS
treatment in early experiences. 7-9 Moreover, TIPS
can be successful also in the technically difficult
case of extension of thrombosis to the portal vein
tree.10,11 Finally, a multi-center experience provided
long-term data on TIPS treatment for 147 BCS
patients not responding to medical treatment or
recanalization. TIPS was successful in 124 BCS
patients, who were followed for a median of 36.7
months. Overall, 16 (13%) died, 8 (6.5%) underwent
OLT. Main complications were hepatic encephalopathy
in 21% and TIPS dysfunction in 41%. The 10-year
survival was 69%.12
Apart from LT, surgical treatment is generally
not contemplated in the BCS management by recent
324
Mancuso A.
guidelines.1 In fact, the most used treatment for
BCS non responsive to medical therapy is TIPS, LT
is used as a rescue therapy, while surgical treatments are limited to a strict minority of patients.1-3
Surgical shunts for BCS can be very successful, but
have been associated with rapid decompensation and
in-hospital mortality can be high (about 25%), primarily due to the patients poor general condition.13-16
In the past years, a surgical approach has been traditionally considered the first choice. In some series,
an excellent outcome with long-term follow-up has
been reported (95% survival, 3 to 28-year followup).15 However, in this series, the SSPCS was used,
an approach that cannot be used in case of inferior
vena cava (IVC) thrombosis or significant compression. In the same series, the mortality rates of patients with IVC involvement were very high after
traditional surgery (mesoatrial shunts) and better
results were described with another technique
(SSPCS + cavoatrial shunt) in 18 patients, all surviving after a follow-up of 5-25 years.15 However,
outcome after surgical portosystemic shunt is variable
and worse results were reported by others.13,14,16
In most of the above series, patients with liver failure were not considered for surgery but for liver
transplantation.13-16
Patients with BCS due to a IVC obstruction near
to the atrium constitute a difficult to treat subgroup
of BCS patients, whose management can benefit
from endovascular dilatation/stenting or surgical
treatment. Because of obvious reasons, TIPS does
not by-pass IVC obstruction, resulting ineffective.
Although some study describes the possibility of endovascular management for patients with IVC obstruction near to the atrium as safe and with good
long-term patency, data are scanty and need confirmation on a larger scale.17
The widest experience with a surgical shunt
approach for BCS due to a IVC obstruction was
the above reported after a combination of SSPCS
and cavo-atrial shunt: 18 patients, all surviving
after a follow-up of 5-25 years.15 Other surgical
techniques reported in that and other series either had unacceptable or non reported outcomes.13,14,16
We recently described a patient with IVC obstruction near to the atrium and a previous severe complication of a trial of endovascular management,
who had an excellent outcome after the replacement
of the obstructed segment of the IVC with a caval
homograft.18
LT is the last chance for BCS syndrome non responsive to either medical therapy or recanalization/
, 2014; 13 (3): 323-326
decompression.19-24 A European multi-center study
reported long-term data on 248 patients who underwent LT for BCS between 1988 and 1999. MPD was
the underlying syndrome in 45%. LT was performed
electively in 55%, in emergency in 21%. Hepatocellular carcinoma was incidentally found in explanted
liver in 3. Before LT, 19% had portal vein thrombosis and 16% IVC thrombosis. Median follow-up was
48 months. Overall, 67 (27%) died (49% in the first
month). Causes of death were sepsis in 47%, graft
dysfunction or hepatic artery thrombosis in 19%, venous thrombosis in 12%, cardiac in 9% and brain
damage in 5%. There was a significantly increased
mortality if LT was shortly after SPSS or TIPS.
Thirty-seven patients underwent re-LT (4 twice).
The 10-year survival was 68%. After 1 year there
were 9 deaths, seven of which were in MPD patients. Causes were: 4 BCS recurrence, 1 leukaemia
(7 years post-LT), 1 ovarian cancer, 1 colangitis, 2
not known. Anticoagulation after LT was performed
by 200/235 (18 heparin or aspirin), suspended in 10,
all of which were believed to have a cause of BCS reversible after LT (antithrombin III and Protein C
deficiency); all had an uneventful outcome but one
who reported pulmonary embolization 1 year after,
when anti-phospholipid syndrome was discovered.
Complications post-OLT in the patients treated with
anticoagulation were thrombosis in 27 (11%), 11 of
whom (41%) died; recurrence of BCS in 6 (1 ReOLT, 1 TIPS, 4 death); bleeding in 27 (11%), 2 of
whom died (intracranial bleeding). Prognostic Factors were pre-OLT renal function and pre-OLT
SPSS/TIPS.23 However, the prognostic factor of a
previous shunt before LT has to be weighed cautiously because it can only reflect the fact that patients who underwent TIPS before LT had the most
severe liver disease. Moreover, a recent American
multi-center study found no negative effect of TIPS
on the following LT outcome.24 Finally, recent data
show promising results of living donor LT for
BCS.25
The possibility of BCS underlying disease progression is a concern, in particular the development
of leukaemia in MPD after LT. Preliminary multicenter studies failed to draw conclusions on this topic, given that long-term outcome was not correlated
to t h e t y p e o f u n d e r l y i n g d i s e a s e p r e d i s p o s ing to BCS.23,24 However, although not statistically
significant, 7 of the 9 patients who died after 1 year
post LT in the European study had MPD.23 The impact of Jak2 and MPL mutations on prognosis of
splanchnic vein thrombosis (either BCS or portal
vein thrombosis) was recently reported in 241 cases.
An update on management of Budd-Chiari syndrome.
, 2014; 13 (3): 323-326
325
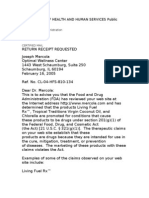
BCS diagnosis
Anticoagulation
Treatment of underlying disease
Ascites, esophageal/gastric varices and/or liver failure?
Yes
TIPS
Follow-up
Feasible and effective
Ineffective or
unfeasible
Consider angioplasty/
Stent or surgery
No
Feasible and effective
Liver transplant
Ineffective or unfeasible
In BCS, patients with the Jak2V617F mutation had
a significantly more severe disease (Child-Pugh, Clichy
PI, Rotterdam score). Moreover, event free survival
tended to be decreased, but not significantly, in
patients with Jak2V617F mutation and significantly
decreased in MPD. However, at a median follow
up of 3.9 years, overall survival was not influenced
by either Jak2V617F mutation or MPD.26
The outcome of BCS with currently available
treatment is described in a prospective multi-center
study in which 163 patients were followed for a median of 17 mo (range 1-31 mo); 18% also had portal
vein thrombosis, 84% had a thrombophilic syndrome, 46% of which a myeloproliferative disorder
(MPD). Overall, 29 died, 8 for liver failure, 2 multiple organ failure, 2 bleeding. The 24 mo survival
was 82%. Prognostic factors were sex (male), ascites
and creatinine. Importantly, about 1/3 of the patients remained on medical therapy only.27 However,
the follow-up was not long enough to eventually
show the consequences of a slowly progressing disease, possibly prevented by early recanalization/decompression, and to draw any definitive conclusion
about the exact timing of treatment.
The long-term outcome of the same multicenter
experience was recently reported. Interestingly, 20
of the 69 who received only medical therapy died, a
high rate considering the availability of further invasive treatments. The remaining 88 underwent
invasive treatment, mostly TIPS, 20 LT, and only 3
surgical shunt. Overall survival was 74% at 5 years.28
One of the main unsolved issue of BCS management is probably timing of treatment. In fact,
Figure 1. A proposal of a new
algorithm for the management of
Budd-Chiari syndrome (BCS).
although step-wise management suggests moving
forward when no response to therapy appears, definition for response to therapy was not stated1,2,29
and a proposal of such a definition needs validation.2 Moreover, because of the rarity of BCS, management guidelines come from expert opinion, are
empirical, and are not evidence based. Given that
benefit of treatments for BCS is not under debate,
anticipating invasive treatments, namely TIPS, before no response to medical therapy appears, could
perhaps decrease hepatic fibrosis development, disease progression, and finally improve outcome.29 In
conclusion, a proposal of a new algorithm of BCS
management suggesting early interventional therapy when clinical signs appear is reported (Figure 1).
FINANCIAL DISCLOSURE
I declare I have nothing to disclose
REFERENCES
1. DeLeve LD, Valla DC, Garcia-Tsao G. Vascular disorders of
the liver. Hepatology 2009; 49: 1729-64.
2. Plessier A, Sibert A, Consigny Y, Hakime A, Zappa M, Denninger MH, Condat B, et al. Aiming at minimal invasiveness
as a therapeutic strategy for Budd-Chiari syndrome. Hepatology 2006; 44: 1308-16.
3. Mancuso A. Budd-Chiari syndrome management: lights and
shadows. World J Hepatol 2011; 3: 262-4.
4. Bilbao JI, Pueyo JC, Longo JM, Arias M, Herrero JI, Benito
A, Barettino MD, et al. Interventional therapeutic techniques in Budd-Chiari syndrome. Cardiovasc Intervent Radiol
1997; 20: 112-19.
5. Fisher NC, McCafferty I, Dolapci M, Wali M, Buckels JA,
Olliff SP, Elias E. Managing Budd-Chiari syndrome: a retros-
326
Mancuso A.
pective review of percutaneous hepatic vein angioplasty
and surgical shunting. Gut 1999; 44: 568-74.
6. Eapen CE, Velissaris D, Heydtmann M, Gunson B, Olliff S,
Elias E. Favourable medium term outcome following hepatic vein recanalisation and/or transjugular intrahepatic
portosystemic shunt for Budd Chiari syndrome. Gut 2006;
55: 878-84.
7. Perell A, Garca-Pagn JC, Gilabert R, Surez Y, Moitinho
E, Cervantes F, Reverter JC, et al. TIPS is a useful longterm derivative therapy for patients with Budd-Chiari
syndrome uncontrolled by medical therapy. Hepatology
2002; 35: 132-9.
8. Mancuso A, Fung K, Mela M, Tibballs J, Watkinson A,
Burroughs AK, Patch D. TIPS for acute and chronic BuddChiari syndrome: a single-centre experience. J Hepatol
2003; 38: 751-4.
9. Rssle M, Olschewski M, Siegerstetter V, Berger E, Kurz K,
Grandt D. The Budd-Chiari syndrome: outcome after
treatment with the transjugular intrahepatic portosystemic shunt. Surgery 2004; 135: 394-403.
10. Mancuso A, Watkinson A, Tibballs J, Patch D, Burroughs
AK. Budd-Chiari syndrome with portal, splenic, and superior mesenteric vein thrombosis treated with TIPS: who
dares wins. Gut 2003; 52: 438.
11. Darwish MS, Valla DC, De Groen PC, Zeitoun G, Haagsma
EB, Kuipers EJ, Janssen HL. Pathogenesis and treatment
of Budd-Chiari syndrome combined with portal vein thrombosis. Am J Gastroenterol 2006; 101: 83-90.
12. Garcia-Pagn JC, Heydtmann M, Raffa S, Plessier A, Murad
S, Fabris F, Vizzini G, et al. TIPS for Budd-Chiari syndrome:
long-term results and prognostics factors in 124 patients.
Gastroenterology 2008; 135: 808-15.
13. Ringe B, Lang H, Oldhafer KJ, Gebel M, Flemming P, Georgii
A, Borst HG, et al. Which is the best surgery for BuddChiari syndrome: venous decompression or liver transplantation? A single-center experience with 50 patients.
Hepatology 1995; 21: 1337-44.
14. Hemming AW, Langer B, Greig P, Taylor BR, Adams R,
Heathcote EJ. Treatment of Budd-Chiari syndrome with
portosystemic shunt or liver transplantation. Am J Surg
1996; 171: 176-180; discussion 180-181.
15. Orloff MJ, Isenberg JI, Wheeler HO, Daily PO, Girard B.
Budd-Chiari syndrome revisited: 38 years experience
with surgical portal decompression. J Gastrointest Surg
2012; 16: 286-300; discussion 300.
16. Zhang Y, Zhao H, Yan D, Xue H, Lau WY. Superior mesenteric vein-caval-right atrium Y shunt for treatment of
Budd-Chiari syndrome with obstruction to the inferior
, 2014; 13 (3): 323-326
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
vena cava and the hepatic veins-a study of 62 patients. J
Surg Res 2011; 169: e93-e99.
Srinivas BC, Dattatreya PV, Srinivasa KH, Prabhavathi CN.
Inferior vena cava obstruction: long-term results of endovascular management. Indian Heart J 2012; 64: 162-9.
Mancuso A, Martinelli L, De Carlis L, Rampoldi AG, Magenta
G, Cannata A, Belli LS. A caval homograft for Budd-Chiari
syndrome due to inferior vena cava obstruction. World J
Hepatol 2013; 27: 292-5.
Halff G, Todo S, Tzakis AG, Gordon RD, Starzl TE. Liver
transplantation for the Budd-Chiari syndrome. Ann Surg
1990; 211: 43-9.
Rao AR, Chui AK, Gurkhan A, Shi LW, Al-Harbi I, Waugh R,
Verran DJ, et al. Orthotopic liver transplantation for
treatment of patients with Budd-Chiari syndrome: a Singecenter experience. Transplant Proc 2000; 32: 2206-207.
Ulrich F, Steinmller T, Lang M, Settmacher U, Mller AR,
Jonas S, Tullius SG, et al. Liver transplantation in patients
with advanced Budd-Chiari syndrome. Transplant Proc
2002; 34: 2278.
Srinivasan P, Rela M, Prachalias A, Muiesan P, Portmann B,
Mufti GJ, Pagliuca A, et al. Liver transplantation for BuddChiari syndrome. Transplantation 2002; 73: 973-7.
Mentha G, Giostra E, Majno PE, Bechstein WO, Neuhaus P,
OGrady J, Praseedom RK, et al. Liver transplantation for
Budd-Chiari syndrome: A European study on 248 patients
from 51 centres. J Hepatol 2006; 44: 520-8.
Segev DL, Nguyen GC, Locke JE, Simpkins CE, Montgomery
RA, Maley WR, Thuluvath PJ. Twenty years of liver transplantation for Budd-Chiari syndrome: a national registry
analysis. Liver Transpl 2007; 13: 1285-94.
Choi GS, Park JB, Jung GO, Chun JM, Kim JM, Moon JI,
Kwon CH, et al. Living donor liver transplantation in BuddChiari syndrome: a single-center experience. Transplant
Proc 2010; 42: 839-42.
Kiladjian JJ, Cervantes F, Leebeek FW, Marzac C, Cassinat B, Chevret S, Cazals-Hatem D, et al. The impact of
JAK2 and MPL mutations on diagnosis and prognosis
of splanchnic vein thrombosis: a report on 241 cases.
Blood 2008; 111: 4922-9.
Darwish MS, Plessier A, Hernandez-Guerra M, Fabris F,
Eapen CE, Bahr MJ, Trebicka J, et al. Etiology, management, and outcome of the Budd-Chiari syndrome. Ann Intern Med 2009; 151: 167-75.
Seijo S, Plessier A, Hoekstra J, DellEra A, Mandair D, Rifai
K, Trebicka J, et al. Good long-term outcome of Budd-Chiari syndrome with a step-wise management. Hepatology
2013; 57: 1962-8.
Mancuso A. Budd-Chiari Syndrome Management: Timing of
Treatment Is an Open Issue. Hepatology (IN PRESS).
También podría gustarte
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Trasturel 440mg Anti CancerDocumento3 páginasTrasturel 440mg Anti CancerRadhika ChandranAún no hay calificaciones
- Jurnal Asli PBL 3 Blok 9Documento6 páginasJurnal Asli PBL 3 Blok 9Annisa FadilasariAún no hay calificaciones
- Futuristic Nursing: - Sister Elizabeth DavisDocumento14 páginasFuturistic Nursing: - Sister Elizabeth DavisPhebeDimple100% (2)
- Counseling: Counseling Is A Wonderful Twentieth-Century Invention. We Live in A Complex, BusyDocumento21 páginasCounseling: Counseling Is A Wonderful Twentieth-Century Invention. We Live in A Complex, BusyAnitha KarthikAún no hay calificaciones
- HHHHHGGGDocumento7 páginasHHHHHGGGemrangiftAún no hay calificaciones
- 11th Bio Zoology EM Official Answer Keys For Public Exam Mhay 2022 PDF DownloadDocumento3 páginas11th Bio Zoology EM Official Answer Keys For Public Exam Mhay 2022 PDF DownloadS. TAMIZHANAún no hay calificaciones
- My Evaluation in LnuDocumento4 páginasMy Evaluation in LnuReyjan ApolonioAún no hay calificaciones
- DLL - Mapeh 6 - Q4 - W6Documento4 páginasDLL - Mapeh 6 - Q4 - W6Bernard Martin100% (1)
- Philhealth Circular 013-2015Documento12 páginasPhilhealth Circular 013-2015Kim Patrick DayosAún no hay calificaciones
- MLC Lean Bronze Prep ClassDocumento2 páginasMLC Lean Bronze Prep ClassSalaAún no hay calificaciones
- 50 Maternal and Child NCLEX QuestionsDocumento14 páginas50 Maternal and Child NCLEX QuestionsShengxy Ferrer100% (2)
- AM LOVE School Form 8 SF8 Learner Basic Health and Nutrition ReportDocumento4 páginasAM LOVE School Form 8 SF8 Learner Basic Health and Nutrition ReportLornaNirzaEnriquezAún no hay calificaciones
- Professional Self ConceptDocumento11 páginasProfessional Self Conceptgladz25Aún no hay calificaciones
- Nursing Exam Questions With AnswerDocumento7 páginasNursing Exam Questions With AnswerjavedAún no hay calificaciones
- Soy Estrogen Myth False - DR Mercola Caught by Federal Authorities Spreading False Health Info - (Soy Found Not To Contain Estrogen, Soy Does Not Lower Men's Testosterone, Fraudulent Claims)Documento10 páginasSoy Estrogen Myth False - DR Mercola Caught by Federal Authorities Spreading False Health Info - (Soy Found Not To Contain Estrogen, Soy Does Not Lower Men's Testosterone, Fraudulent Claims)FRAUDWATCHCOMMISSIONAún no hay calificaciones
- 5.3.1 Distinguish Between Learning and Performance: Skill in SportDocumento48 páginas5.3.1 Distinguish Between Learning and Performance: Skill in SportAiham AltayehAún no hay calificaciones
- July 7, 2017 Strathmore TimesDocumento28 páginasJuly 7, 2017 Strathmore TimesStrathmore TimesAún no hay calificaciones
- Export of SpicesDocumento57 páginasExport of SpicesJunaid MultaniAún no hay calificaciones
- What Is FOCUS CHARTINGDocumento38 páginasWhat Is FOCUS CHARTINGSwen Digdigan-Ege100% (2)
- Using The Childrens Play Therapy Instrument CPTIDocumento12 páginasUsing The Childrens Play Therapy Instrument CPTIFernando Hilario VillapecellínAún no hay calificaciones
- Q3-Las-Health10-Module 3-Weeks 6-8Documento6 páginasQ3-Las-Health10-Module 3-Weeks 6-8MA TEODORA CABEZADAAún no hay calificaciones
- Know About Dengue FeverDocumento11 páginasKnow About Dengue FeverKamlesh SanghaviAún no hay calificaciones
- A Smart Gym Framework: Theoretical ApproachDocumento6 páginasA Smart Gym Framework: Theoretical ApproachciccioAún no hay calificaciones
- Net Jets Pilot & Benefits PackageDocumento4 páginasNet Jets Pilot & Benefits PackagedtoftenAún no hay calificaciones
- A Study To Assess The Effectiveness of Selected Teaching Strategies Knowledge Regarding Drug Calculation Among B.Sc. N Students in Selected College at ChennaiDocumento3 páginasA Study To Assess The Effectiveness of Selected Teaching Strategies Knowledge Regarding Drug Calculation Among B.Sc. N Students in Selected College at ChennaiEditor IJTSRDAún no hay calificaciones
- 2011 Member Handbook English UHCCPforAdults NYDocumento52 páginas2011 Member Handbook English UHCCPforAdults NYpatsan89Aún no hay calificaciones
- Module 11 Rational Cloze Drilling ExercisesDocumento9 páginasModule 11 Rational Cloze Drilling Exercisesperagas0% (1)
- Pitbull StatementDocumento4 páginasPitbull StatementThe Citizen NewspaperAún no hay calificaciones
- R4 HealthfacilitiesDocumento332 páginasR4 HealthfacilitiesCarl Joseph BarcenasAún no hay calificaciones
- 2011 Urine Therapy J of NephrolDocumento3 páginas2011 Urine Therapy J of NephrolCentaur ArcherAún no hay calificaciones