Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Assessment of Eyes
Cargado por
Esha ReShaDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Assessment of Eyes
Cargado por
Esha ReShaCopyright:
Formatos disponibles
ASSESSMENT OF EYES
Tuesday, December 9, 2014
16:34
Visual Acuity
This is an essential part of the eye examination and a measure against which all
therapeutic outcomes are based.
The Snellen chart, which is composed of a series of progressively smaller rows of
letters, is used to test distance vision.
The fraction 20/20 is considered the standard of normal vision.
Most people can see the letters on the line designated as 20/20 from a distance
of 20 feet.
A person whose vision is 20/200 can see an object from 20 feet away that a
person with 20/20 vision can see from 200 feet away.
NOTE: ung first number ayun ung sayo, pero ung second number un ung sa
ibang tao. Meaning kapag 20/200 ikaw kailangan mong lumapit ng up to 20
feet para mabasa pero ung ibang tao nababasa nila un kahit 200 feet distance
Clients who wear corrective lenses other than for reading should have their vision
tested with the lens in place.
Confrontational test
The confrontational test is performed to examine visual fields or peripheral
vision.
The examiner and the client sit facing each other.
The client is asked to look directly into the eyes of the examiner throughout the
test.
The examiner covers his or her right eye while the client covers his or her left eye
(the client covers the eye directly opposite to the examiner's covered eye).
The examiner moves a finger from a nonvisible area into the client's line of vision.
The examiner and client should see the object at approximately the same time.
When the client sees the object coming into the line of vision, the client informs
the examiner.
The procedure is repeated on the opposite eye.
The test assumes that the examiner has normal peripheral vision.
Ishihara chart
The Ishihara chart consists of numbers composed of colored dots located within a
circle of colored dots.
The client is asked to read the numbers on the chart.
Each eye is tested separately.
Reading the numbers correctly indicates normal color vision
The test is sensitive for the diagnosis of red-green blindness but cannot detect
discrimination of blue.
Pupils
The pupils are round and of equal size.
Increasing light causes pupillary constriction.
Decreasing light causes pupillary dilation.
Constriction of both pupils is a normal response to direct light.
The client is asked to look straight ahead while the examiner quickly brings a
beam of light ( flashlight) in from the side and directs it onto the eye.
The constriction of the eye is a direct response to shining a light into that eye;
constriction of the opposite eye is known as a consensual response.
Sclera and cornea
Normal sclera color is white.
In a dark-skinned person, the sclera may normally appear yellow;
pigmented dots may be present.
A yellow color to the sclera may indicate jaundice or systemic problems.
The cornea is transparent, smooth, shiny, and bright.
Cloudy areas or specks on the cornea may be the result of an accident or eye
injury.
Ophthalmoscopy
The ophthalmoscope is an instrument used to examine the external structures
and the interior of the eye.
The room is darkened so that the pupil will dilate.
The instrument is held with the right hand when examining the right eye and
with the left hand when examining the left eye.
The client is asked to look straight ahead at an object on the wall.
The examiner should approach the client's eye from about 12 to 15 inches away
and 15 degrees lateral to the client's line of vision.
As the instrument is directed at the pupil, a red glare (red reflex) is seen in the
pupil.
The red reflex is the reflection of light on the vascular retina.
Absence of the red reflex may indicate opacity of the lens.
The retina, optic disk, optic vessels, fundus, and macula can be examined.
Tonometry
The test is used primarily to assess for an increase of intraocular pressure and
potential glaucoma.
Normal intraocular pressure is 10 to 21 mm Hg; intraocular pressure varies
throughout the day and is normally higher in the morning ( always document the
time of intraocular pressure measurement).
DISORDERS
Legally blind
The best visual acuity with corrective lenses in the better eye of 20/200 or less or
visual acuity of less than 20 degrees of the visual field in the better eye
NURSING INTERVENTIONS
When speaking to the client who has limited sight or is blind, the nurse uses a
normal tone of voice.
Alert the client when approaching.
Orient the client to the environment.
Use a focal point and provide further orientation to the environment from that
focal point.
Allow the client to touch objects in the room.
Use the clock placement of foods on the meal tray to orient the client.
Promote independence as much as is possible.
Provide radios, televisions, and clocks that give the time orally, or provide a
braille watch.
When ambulating, allow the client to grasp the nurse's arm at the elbow;
the nurse keeps his or her arm close to the body so that the client can
detect the direction of movement.
Instruct the client to remain one step behind the nurse when ambulating.
Instruct the client in the use of the cane for the blind, which is differentiated from
other canes by its straight shape and white color with red tip.
Instruct the client that the cane is held in the dominant hand several inches off
the floor.
Instruct the client that the cane sweeps the ground where the client's foot will be
placed next to determine the presence of obstacles.
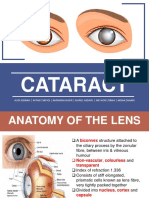
Cataract
is an opacity of the lens that distorts the image projected onto the retina and
that can progress to blindness.
Causes include the aging process (senile cataract), inherited (congenital
cataract), and injury (traumatic cataract s); cataract s also can result from
another eye disease (secondary cataract).
Intervention is indicated when visual acuity has been reduced to a level that
the client finds to be unacceptable or adversely affects his or her lifestyle.
ASSESSMENTS
Blurred v ision and decreased color perception are EARLY signs
Diplopia, reduced visual acuity, absence of the red reflex, and the presence of a
white pupil are LATE signs.
Loss of vision is gradual and painless
MEDICAL MANAGEMENT
No nonsurgical (medications, eyedrops, eyeglasses)
treatment cures cataracts or prevents age-related
cataracts.
In the early stages of cataract development, glasses, contact lenses, strong
bifocals, or magnifying lenses may improve vision.
SURGICAL MANAGEMENT
In general, if reduced vision from cataract does not interfere with normal
activities, surgery may not be needed.
In deciding when cataract surgery is to be performed, the patients functional and
visual status should be a primary
consideration.
Surgery is performed on an outpatient basis and usually takes less than 1 hour,
with the patient being discharged in 30 minutes or less afterward.
Although complications from cataract surgery are uncommon, they can have
significant effects on vision.
When both eyes have cataracts, one eye is treated first, with at least several
weeks, preferably months, separating the two procedures.
RATIONALE: Because cataract surgery is performed to improve visual
functioning, the delay for the other eye gives time for the patient and the
surgeon to evaluate whether the results from the first surgery are adequate to
preclude the need for a second operation. The delay also provides time for the f
irst eye to recover; if there are any complications, the surgeon may decide to
perform the second procedure differently.
POSTOPERATIVE INTERVENTION
Elevate the head of the bed 30 to 45 degrees.
Turn the client to the back or nonoperative side.
Maintain an eye patch as prescribed (usually for the first 24 hours adter the
surgery)
Orient the client to the environment.
Position the client's personal belongings to the nonoperative side.
Use side rails for safety.
Assist with ambulation.
HOME CARE
Advise the client to avoid the following activities, because these activities can
increase the IOP which can disrupt the sutures and can lead to Retrobulbar
hemorrhage
The nurse also explains that there should be minimal discomfort after surgery and
instructs the patient to take a mild analgesic agent, such as acetaminophen, as
needed. Antibiotic, anti-inflammatory, and corticosteroid eye drops or ointments
are prescribed postoperatively.
Advise the client to contact the physiciqn if the following is observed:
NURSING ALERT! If nausea occurs advised the client to call the physician
immediately as this is a sign of increase IOP
To prevent accidental rubbing or poking of the eye, the patient wears a protective
eye patch for 24 hours after surgery, followed by eyeglasses worn during the day
and a metal shield worn at night for 1 to 4 weeks.
Sunglasses should be worn while outdoors during the day because the eye is
sensitive to light.
Slight morning discharge, some redness, and a scratchy feeling may be expected
for a few days. A clean, damp washcloth may be used to remove slight morning
eye discharge.
Because cataract surgery increases the risk of retinal detachment, the patient
must know to notify the surgeon if new floaters (dots) in vision, flashing lights,
decrease in vision, pain, or increase in redness occurs.
The eye patch is removed after the first follow-up appointment.
The patient may experience blurring of vision for several days to weeks.
Vision gradually improves as the eye heals.
Vision is stabilized when the eye is completely healed, usually within 6 to 12
weeks.
Glaucoma
The term glaucomais used to refer to a group of ocular conditions characterized
by optic nerve damage due to increase IOP.
NORMAL PHYSIOLOGY
The eye normally produce fluid to nourish the cornea andlens. These fluilds are
known as the AQUEOUS HUMOR.
The Aqueous humor is produced by the cillary body.
These fluids will then drain through the TRABECULAR MESHWORK to th canal of
Schlemm and will then be reproduced by the cilliary body ( cycle sya kung baga)
GLAUCOMA PHYSIOLOGY
Open angle glaucoma
In this type of glaucoma, the production of aqueous humor is rapid and the the
cyle is slow.
This can lead to increase IOP
Pressure by the increase IOP impedes the microcirculation in the optic nerve
If the blood supply in the optic nerve is impeded by the pressure, this can lead to
gradual loss of vission.
Close angle glaucoma (pupillary block)
In this type of glaucoma, the production of the aqueous humor is normal,
however, the trabecular meshwork is block/obstructed due to thick iris
This can lead to increase IOP
Pressure by the increase IOP impedes the microcirculation in the optic nerve
If the blood supply in the optic nerve is impeded by the pressure, this can lead to
gradual loss of vission.
TYPES
MANIFESTATION
Open-Angle Glaucoma
Optic nerve damage
Visual field defects(loss of peripheral vission) IOP 21
mm Hg.
May have fluctuating IOPs.
Usually no symptoms but possible ocular pain,
headache, and halos.
NOTE: not that painful as compare to angle-
closure glaucoma
Angle-Closure ( Pupillary Rapidly progressive visual impairment,
Periocular pain
Block) Glaucoma
Conjunctival hyperemia, and congestion.
NOTE: Pain may be associated with nausea,
vomiting, bradycardia, and profuse sweating.
DIAGNOSTIC
Four major types of examinations are used in glaucoma evaluation, diagnosis, and
management:
Tonometry to measure the IOP
Ophthalmoscopy to inspect the optic nerve, gonioscopy to examine the filtration
angle of the anterior chamber, and perimetry to assess the visual fields. The
changes in the optic nerve related to glaucoma are pallor and cupping of the optic
nerve disc. The pallor of the optic nerve is caused by a lack of blood supply that
results from cellular destruction. Cupping is characterized by exaggerated
bending of the blood vessels as they cross the optic
MEDICAL MANAGEMENT
The aim of all glaucoma treatment is prevention of optic nerve damage.
Lifelong therapy is almost always necessary because glaucoma cannot be cured.
Treatment focuses on pharmacologic therapy, laser procedures, surgery, or a
combination of these approaches, all of which have potential complications and
side effects.
Although treatment cannot reverse optic nerve damage, further damage can be
controlled. The goal is to maintain an IOP within a range unlikely to cause further
damage.
PHARMACOLOGIC MANAGEMENT
MEDICATIO
N
ACTION
SIDE EFFECT
NURSING
INTERVENTION
Cholinergics
(miotics)
(pilocarpine,
carbachol)
Increases
Periorbital pain
Caution patients
Blurry vision
aqueous fluid
about diminished
Difficulty seeing in the dark
outflow by
vision in dimly lit
contracting the
areas.
Advise the client
ciliary muscle and
causing miosis
to qcoid complex
(constriction of
activitirs (driving,
the pupil) and
operating a
opening of
machine)
trabecular
meshwork
Adrenergic
agonists
(dipivefrin,
epinephrine)
Reduces
production of
aqueous humor
and increases
outflow
Eye redness and burning
Teach patients
Can have systemic effects,
punctal occlusion
including palpitations,
to limit systemic
elevated blood pressure,
effects ( Check
tremor, headaches, and
picture below)
anxiety
Beta-
blockers
(betaxolol,
timolol)
Decreases
aqueous humor
production
Can have systemic effects, Contraindicated in
including bradycardia,
patients with
exacerbation of pulmonary asthma, chronic
disease, and hypotension
obstructive
pulmonary
disease, second-
or third-degree
heart block,
bradycardia, or
cardiac failure
Teach patients
punctal occlusion
to limit systemic
effects.
Carbonic
anhydrase
inhibitors
(acetazolami
de,
methazolami
de,
dorzolamide)
Decreases
aqueous humor
production due its
diuretic effect
Oral medications
(acetazolamide and
methazolamide) associated
with serious side effects,
including anaphylactic
reactions, electrolyte loss,
depression, lethargy,
gastrointestinal upset,
impotence, and weight loss;
side effects of topical form
(dorzolamide) include
topical allergy
Do not administer
to patients with
sulfa allergies;
Monitor
electrolyte levels.
NOTE: PUNCTUAL OCCLUSION to prevent systemic absorprion of optic medication
SURGICAL MANAGEMENT
In laser trabeculoplastyfor glaucoma, laser burns are applied to the inner surface
of the trabecular meshwork to open the intratrabecular spaces and widen the
canal of Schlemm, thereby promoting outflow of aqueous humor and decreasing
IOP. The procedure is indicated when IOP is inadequately controlled by
medications, and it is contraindicated when the trabecular meshwork cannot be
fully visualized because of narrow angles. (LASER TRABECULOPLASTY is for OPEN
ANGLE GLAUCOMA ONLY)
In laser iridotomy for pupillary block glaucoma, an opening is made in the iris
to eliminate the pupillary block. Laser iridotomy is contraindicated in patients
with corneal edema, which interferes with laser targeting and strength.
NURSING INTERVENTIONS
Instruct the client on the importance of medication. ( CHECK THE TABLE ABOVE)
Instruct the client of the need for lifelong medication use.
Instruct the client to wear a Medic Alert bracelet. Instruct the client to avoid
anticholinergic medications (atropine sulfate, this medication can cause
increase IOP by dilating the pupil)
Instruct the client to report eye pain, halos around the eyes, and changes in vision
to the physician.
Instruct the client that when maximal medical therapy has failed to halt the
progression of visual field loss and optic nerve damage, surgery will be
recommended.
Prepare the client for trabeculoplasty or laser iridectomy as prescribed to
facilitate aqueous humor drainage.
Retinal detachment
Detachment or separation of the retina from the epithelium
Retinal detachment occurs when the layers of the retina separate because of the
accumulation of fluid between them, or when both retinal layers elevate away
from the choroid as a result of a tumor.
Partial detachment becomes complete if untreated.
When detachment becomes complete, blindness occurs.
ASSESSMENTS
Flashes of light
Floaters or black spots (signs of bleeding)
Increase in blurred vision
Sense of a curtain being drawn over the eye
Loss of a portion of the visual field
IMMEDIATE INTERVENTIONS
Provide bed rest.
Cover both eyes with patches as prescribed to prevent further detachment.
Speak to the client before approaching.
Position the client's head as prescribed. If the detachment is on the right side
of the eye ball position the client's head on the right side also to prevent
further detachment
Protect the client from injury.
Avoid jerky head movements.
Minimize eye stress.
Prepare the client for a surgical procedure as prescribed. ( SCLERAL BUCKLING)
POSTOPERATIVE INTERVENTIONS
Maintain eye patches as prescribed.
Monitor for hemorrhage.
Prevent nausea and vomiting and monitor for restlessness, which can cause
hemorrhage
Monitor for sudden, sharp eye pain (notify the physician).
Encourage deep breathing but avoid coughing.
Provide bed rest for 1 to 2 days as prescribed.
Position the client as prescribed ( positioning depends on the location of the
detachment).
Administer eye medications as prescribed.
Assist the client with activities of daily living.
Avoid sudden head movements or anything that increases intraocular pressure.
Instruct the client to limit reading for 3 to 5 weeks.
Instruct the client to avoid squinting, straining and constipation, lifting
heavy objects, and bending from the waist.
Instruct the client to wear dark glasses during the day and an eye patch at night.
Encourage follow-up care because of the danger of recurrence or occurrence in
the other eye.
Contusion
Bleeding into the soft tissue as a result of an injury.
A contusion causes a black eye; the discoloration disappears in about 10 days.
Pain, photophobia, edema, and diplopia may occur.
INTERVENTIONS
Place ice on the eye immediately.
Instruct the client to receive a thorough eye examination.
Penetrating objects
An eye injury in which an object penetrates the eye
INTERVENTIONS
NEVER remove the object because it may be holding ocular structures in place;
the object must be removed by the physician.
Cover the object with a cup. Both eyes shouls be covered
Do not allow the client to bend over.
Do not place pressure on the eye.
Client is to be seen by a physician immediately.
X-rays and CT scans of the orbit are usually obtained.
Magnetic resonance imaging (MRI) is contraindicated because of the possibility
of metal-containing projectile movement during the procedure.
Chemical burn
An eye injury in which a caustic substance enters the eye
INTERVENTIONS
Treatment should begin immediately.
Flush the eyes at the scene of the injury with water for at least 15 to 20
minutes.
At the scene of the injury, obtain a sample of the chemical involved.
At the emergency room, the eye is irrigated with normal saline solution or an
ophthalmic irrigation solution for at least 10 minutes.
The solution is directed across the cornea and toward the lateral canthus.
Prepare for visual acuity assessment.
Apply an antibiotic ointment as prescribed.
Cover the eye with a patch as prescribed.
También podría gustarte
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (72)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Visual Perception: The 5 Stages of SightDocumento12 páginasVisual Perception: The 5 Stages of SightfewjkhvbjkhlckvsjdbAún no hay calificaciones
- Chapter 8-SPECIAL SENSESDocumento5 páginasChapter 8-SPECIAL SENSESrishellemaepilonesAún no hay calificaciones
- Myopia Management & Refractive ErrorsDocumento11 páginasMyopia Management & Refractive ErrorsSubramaniam KrishnamoorthiAún no hay calificaciones
- Hyperthiroidism NouDocumento58 páginasHyperthiroidism NouAlina Pirtac100% (1)
- Imtiaz Notes Main-1-1Documento8 páginasImtiaz Notes Main-1-1Dr Afzal HussainAún no hay calificaciones
- Color and Color Psychology 2015Documento76 páginasColor and Color Psychology 2015Chaz PolicarpioAún no hay calificaciones
- Visual Impairment: By: Michael Ron Francis D. DimaanoDocumento16 páginasVisual Impairment: By: Michael Ron Francis D. DimaanoMichael Ron DimaanoAún no hay calificaciones
- Visual Outcomes and Barriers in Children with Low VisionDocumento4 páginasVisual Outcomes and Barriers in Children with Low VisionshishichanAún no hay calificaciones
- Schedule CIOMDocumento16 páginasSchedule CIOMBonita AsyigahAún no hay calificaciones
- Key To Eye Diagnosis by Tashfeen NasiraDocumento8 páginasKey To Eye Diagnosis by Tashfeen Nasiralakshay sharmaAún no hay calificaciones
- MCQ 05 OpticsDocumento14 páginasMCQ 05 OpticsAmr Abdulradi0% (1)
- Intermittent Exotropia: Management Options and Surgical OutcomesDocumento4 páginasIntermittent Exotropia: Management Options and Surgical OutcomesPierre A. RodulfoAún no hay calificaciones
- Lista Plugin-Uri Premiere ProDocumento2 páginasLista Plugin-Uri Premiere ProelbrusneoAún no hay calificaciones
- Color Psychology: How Hues Impact EmotionsDocumento24 páginasColor Psychology: How Hues Impact EmotionsChetna BhansaliAún no hay calificaciones
- Management of Giant Retinal TearsDocumento6 páginasManagement of Giant Retinal TearsAlejandro LondoñoAún no hay calificaciones
- Upsc SCDocumento65 páginasUpsc SCmadhujayaraj100% (1)
- Differences Between Ophthalmologist, and OpticianDocumento2 páginasDifferences Between Ophthalmologist, and OpticianLay EcanAún no hay calificaciones
- Visual Acuity Test TEMPLATEDocumento9 páginasVisual Acuity Test TEMPLATEJuriel Elohim GolvinAún no hay calificaciones
- A Guide For Supporting Visually Impaired Adults and Children in AthleticsDocumento19 páginasA Guide For Supporting Visually Impaired Adults and Children in AthleticsalexandreAún no hay calificaciones
- Understanding Ocular Motility and Strabismus ExamsDocumento35 páginasUnderstanding Ocular Motility and Strabismus ExamsDavid Wong Chao ShengAún no hay calificaciones
- NEURO Ch. 1-5 Quiz 1 NotesDocumento31 páginasNEURO Ch. 1-5 Quiz 1 NotesMelissa OrtizAún no hay calificaciones
- Material Downloaded From - 1 / 6Documento6 páginasMaterial Downloaded From - 1 / 6Jagpreet SinghAún no hay calificaciones
- Visual Development Milestones and Visual Acuity Assessment in ChildrenDocumento2 páginasVisual Development Milestones and Visual Acuity Assessment in ChildrenNikhil Maha DevanAún no hay calificaciones
- Doora Drishti - A Paravartajanya Vikara (Hypermetropia) - A Case StudyDocumento4 páginasDoora Drishti - A Paravartajanya Vikara (Hypermetropia) - A Case StudyAdvanced Research PublicationsAún no hay calificaciones
- POCUS 101 Ocular Ultrasound Pocket CardDocumento1 páginaPOCUS 101 Ocular Ultrasound Pocket CardEduardoAún no hay calificaciones
- Cataract: Audi Adibah - Affan Syafiqi - Amanina Nasir - Nurul Hidayu - Nik Nor Liyana - Arina ZahariDocumento57 páginasCataract: Audi Adibah - Affan Syafiqi - Amanina Nasir - Nurul Hidayu - Nik Nor Liyana - Arina ZaharivictorssideAún no hay calificaciones
- Anatomy and Function of The Eye: Henry J. KaplanDocumento7 páginasAnatomy and Function of The Eye: Henry J. KaplanCucută Alexandru-DanielAún no hay calificaciones
- The Eye: OphthalmologyDocumento12 páginasThe Eye: OphthalmologyAshley DayagAún no hay calificaciones
- 13-2 Ciuffreda PDFDocumento3 páginas13-2 Ciuffreda PDFirijoaAún no hay calificaciones
- Anterior Segment OctDocumento53 páginasAnterior Segment OctA.c. RaghuAún no hay calificaciones