Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Acute Post-Op Pain Management
Cargado por
1234chocoTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Acute Post-Op Pain Management
Cargado por
1234chocoCopyright:
Formatos disponibles
OKA5301 NPS APOP EVC.
qxd
16/2/07
3:13 PM
Page 1
Acute postoperative
pain management
Optimal postoperative pain management
begins in the preoperative period
Measure pain regularly using a validated
pain assessment tool
Pain is subjective and each individual patients experience of pain is different.
Reasons for these differences include:
Regular and routine assessment of pain will result in improved pain management.1
age
The patients own assessment of pain is the most reliable and should be used
when possible.1
co-morbidities including chronic pain
Use a pain measurement tool appropriate to patients mental status, age and language.
concurrent medication and other substance intake
Measure pain scores both at rest and on movement/function to assess the impact
on functional activity.13
mechanisms of pain nociceptive, neuropathic
Re-assess pain regularly and before/after administering analgesia or other pain
management strategies.
modifying factors e.g. mood, cognition, coping strategies
genetics.
Document pain assessment measurements as part of routine observations.
Conduct preoperative patient evaluation:
Validated pain assessment tools
Ask the patient and/or their carers to help establish pain history (consider the above).
Patient measures
Document in the patients medical record, otherwise state that there are
no relevant factors.
Visual analogue scale (VAS; figure 1).
Numerical rating scale (NRS; figure 2).
Discuss pain management strategies and expectations in the preoperative period.
Verbal descriptor scale e.g. none/mild/moderate/severe.
WongBaker faces scale (figure 3).
Observer measures
Behavioural pain scale.3
Fig 1: Visual analogue scale
Fig 2: Numerical rating scale
Fig 3: WongBaker faces scale
PAIN SCORE 0 10 NUMERICAL RATING
010 Numerical Rating Scale
No
Pain
Worst
Pain Ever
No
Pain
4
5
6
Moderate Pain
Worst
Possible
10 Pain
10
No Hurt
Hurts
Little Bit
Hurts
Little More
Hurts
Even More
Hurts
Whole Lot
Hurts
Worst
WongBaker FACES Pain Rating Scale, from Wong DL et al.: Whaley and
Wongs Essentials of Pediatric Nursing, 5th edition, St. Louis, 2001, Mosby, p. 1301.
http://www.mosbysdrugconsult.com/WOW/facesReproductions.html (accessed 31 January 2007).
APOP Project
OKA5301 NPS APOP EVC.qxd
16/2/07
3:13 PM
Page 2
Ensure all postoperative patients receive safe and effective analgesia
When prescribing analgesia
Routes of administration:
Use a variety of approaches (multimodal analgesia) to improve analgesia and decrease
doses of individual agents.4
Paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) are valuable components
of multimodal analgesia.1
Use intermittent intravenous (IV) opioids to gain initial control of severe pain,
as IV administration provides rapid and reliable drug absorption.1
(Note: prescription of nurse-administered IV opioids is not recommended for
ongoing analgesia on general wards.)
When using analgesics on a regular basis have additional prn medication available for
breakthrough pain.
Consider subcutaneous route for ongoing parenteral opioids, avoid intramuscular route
(painful and less predictable absorption).1
Use individualised doses of analgesic(s) administered at appropriate dose intervals and
titrate to patient response.4
Once the oral route has been established, use when possible.1
Drug class
Considerations
Selected precautions
Paracetamol
Useful adjunctive analgesic agent
Provide clear directions when prescribing >1 paracetamol-containing preparation
Consider regular order rather than prn
When combined with opioids, increases pain relief1
Maximum 4 g daily dose usually recommended in healthy adults;
reduce dose in malnourished, underweight patients
Regular (1 g every 46 hours) use can reduce opioid requirements by 2030%1
Avoid in severe liver dysfunction
Only prescribe IV (avoid rectal) if oral is inappropriate1
NSAIDs
(e.g. conventional: ibuprofen,
COX-2 selective: celecoxib)
Tramadol
Opioids
(e.g. morphine,
oxycodone, fentanyl, hydromorphone,
pethidine, dextropropoxyphene)
Adjunctive analgesics for use with opioids
and/or paracetamol1
Adverse effects of NSAIDs are significant; may limit use1
Inadequate for severe pain when given alone,
but can reduce opioid requirements1
Modify dose or avoid in congestive heart failure, those at risk of renal effects
(renal disease, hypovolaemia, hypotension, concurrent use of other nephrotoxic
agents), the elderly
Limit prescription to two to three days then review4
Lower risk of GI bleeding or ulcers with COX-2 selective NSAIDs1
Weak opioid with serotonergic and noradrenergic effects, as effective as morphine
for some types of moderate postoperative pain, less so for severe acute pain5
Avoid in patients with history of seizures
Less risk of respiratory depression and constipation1,5
Be aware of rare, but potentially serious, drug interactions with SSRIs, TCAs,
pethidine, warfarin, St Johns wort
Prescribe opioid dose based on age, use lower initial dose in the elderly
and titrate upwards5
Prescribing multiple opioids via multiple routes increases risk of opioid overdose
and is generally not recommended
Be aware of potential for prescribing and administration errors with immediate
and sustained-release preparations
Do not use morphine or pethidine in severe renal impairment5
Be aware of factors that may increase risk of opioid overdose (e.g. concurrent
sedatives, opioid nave, sepsis)
Use with caution in severe renal impairment and the elderly
Avoid pethidine (accumulation of toxic metabolite norpethidine, drug interactions)
and dextropropoxyphene (unsafe in overdose, ceiling effect)
Abbreviations: ACEI = angiotensin-converting enzyme inhibitors, NSAIDs = non-steroidal anti-inflammatory drugs, SSRIs = selective serotonin reuptake inhibitors, TCAs = tricyclic antidepressants.
OKA5301 NPS APOP EVC.qxd
16/2/07
3:13 PM
Page 3
Monitor and manage adverse events
Monitoring respiratory depression and sedation
(patients on opioids sedatives)
Respiratory rate alone as an indicator of respiratory depression is of limited value
and hypoxaemic episodes may occur in the absence of a reduced respiratory rate.1
Sedation scores are a more reliable indicator respiratory depression is almost always
preceded by sedation.6 The sedation score measures the patients level of wakefulness
and their ability to respond appropriately to verbal command. A four-point scale3
(box 1) is recommended.
Box 1: Sedation scoring
Sedation score
Suggested action
Awake, alert
Mild sedation
1S
Asleep
Moderate sedation, easy to rouse
but unable to stay awake
Monitoring nausea and vomiting
Easy to rouse
Effective antiemetics in the postoperative period include 5HT3 antagonists, droperidol
and dexamethasone.4
Consider co-prescribing more than one antiemetic, each with a different mechanism
of action, with instructions to add a drug from a different class if the first agent is
ineffective.7
Monitoring for other adverse events
Regular review will reduce the risk of serious side effects developing and will allow
for adjustment of doses, dosage interval and alteration of analgesics as necessary.
Side effects for the following include:
Continue routine monitoring
Consider reducing analgesic dose,
increase frequency of monitoring
If respiratory rate < 8 breaths per minute,
withhold opioid, administer naloxone
and notify medical officer
Difficult to rouse, unable to stay awake
Withhold opioid, administer naloxone
and notify medical officer
Note that naloxone should be administered
IV in divided doses of not greater than
100 micrograms
Opioids constipation (consider prescribing of prophylactic laxatives),
urinary retention, itch, confusion and postural hypotension.
NSAIDs GI (peptic ulceration), renal (monitor renal function e.g. in renally impaired
patients, and those being treated with ACEIs, diuretics and aminoglycoside antibiotics),
bronchospasm, platelet inhibition (increased blood loss).1 Risk and severity of side effects
is generally increased in the elderly.1
APOP Project
OKA5301 NPS APOP EVC.qxd
16/2/07
3:13 PM
Page 4
Communicate ongoing pain management plan to both patients
and primary healthcare professionals at discharge
There is evidence of gaps in discharge planning leading to significant harm.8
A pain management plan, as a component of discharge planning, should be clearly
communicated to the patient and/or their carer, general practitioner and other communitybased health professionals.
Management action:
A pain management plan is essential for patients at increased risk of pain after discharge
(see below). This is likely to improve the patients post-discharge pain experience, utilisation
of outpatient services and prevent surgical complications.9
Prescribe drugs for symptomatic relief of side effects where necessary
(e.g. antiemetics and laxatives).
Review analgesia requirements and consider relevant risk factors 24 hours
before discharge.
If prescribing a strong opioid, consider limiting quantity prescribed.
Pain management plan8 at discharge includes:
Factors associated with increased risk of pain and/or complexity of analgesic
requirements post-discharge*:
Patient characteristics5 age, debilitated, cognitive impairment, severe liver disease, renal
impairment, peptic ulcer disease, chronic pain or low pain threshold, multiple admissions
for pain, obstetric patients.
Surgery types1 thoracic, abdominal surgery, surgery involving major disruption of
muscle, bone or nervous tissue, bone grafts.
Concurrent medicines5 opioid antagonists, chronic opioids, SSRIs, monoamine oxidase
inhibitors, central nervous system depressants, warfarin, St Johns wort, ACEIs, diuretics.
*Consult Acute Pain Service or Pain Specialist where necessary (if available).
A list of all analgesics, with dosage and administration times.
Instructions on anticipated/intended duration of therapy and reducing/ceasing therapy
where appropriate.
Important consumer-specific medicines information (e.g. adverse reactions including
allergies, drug interactions, ceased medicines).
For paracetamol-containing analgesics, give (written) information about safe use,
including maximum daily dose of paracetamol.
Instructions for monitoring and managing side effects.5
Methods to improve function while recovering including non-pharmacological methods
for relieving pain.
Contact person for pain problems (uncontrolled or persistent pain) and other
postoperative concerns (e.g. bleeding and infections).
References:
1.
Australian and New Zealand College of Anaesthetists (ANZCA).
Acute pain management: Scientific evidence, 2nd edition. ANZCA, 2005.
http://www.anzca.edu.au/publications/acutepain.htm (accessed 31 January 2007).
3.
Acute pain management performance toolkit. Melbourne: Victorian Quality Council, 2007.
http://www.health.vic.gov.au/qualitycouncil/activities/acute.htm
(accessed 31 January 2007)
2.
Clinical practice guideline for the management of postoperative pain. Version 1.2.
Washington, DC: Department of Defense, Veterans Health Administration, 2002.
http://www.guideline.gov/summary/summary.aspx?doc_id=3284
(accessed 31 January 2007).
4.
Therapeutic Guidelines: Analgesic, Version 4. 2002.
5.
Australian Medicines Handbook, 2007.
6.
Macintyre PE, Schug SA. Acute Pain ManagementA Practical Guide, 3rd edition, 2007
(in press).
7.
Habib AS, Gan TJ. Evidence-based management of postoperative nausea and vomiting:
a review. Can J Anaesth 2004;51:32641.
8.
Australian Pharmaceutical Advisory Council. Guiding principles to achieve continuity
in medication management. Canberra: Department of Health and Ageing, 2005.
http://www.health.gov.au/internet/wcms/publishing.nsf/Content/nmp-guiding
(accessed 31 January 2007)
9.
Kable A, Gibberd R, Spigelman A. Complications after discharge for surgical patients.
ANZ J Surg 2004;74:9297.
Drug Use Evaluation project conducted by the APOP study group: Victorian Department of Human Services/Victorian Drug Usage Evaluation Group; UMORE, Tasmanian School of Pharmacy, University of Tasmania;
South Australian Therapeutic Advisory Group/Department of Health; School of Pharmacy, University of Queensland; New South Wales Therapeutic Advisory Group. Funded and supported by the National Prescribing Service Limited (02 8217 8700).
For more information on the management of postoperative pain refer to ANZCA Acute Pain Management: Scientific Evidence, 2nd edition, 2005, and Therapeutic Guidelines: Analgesic, Version 4, 2002.
The information contained in this material is derived from a critical analysis of a wide range of authoritative evidence. Any treatment decisions based on this information should be made in the context of the individual clinical
circumstances of each patient. Reviewed by: Dr C Roger Goucke, Dr Jane Trinca, Dr Pamela E Macintyre, Professor Stephan A Schug, Faculty of Pain Medicine, Australian and New Zealand College of Anaesthetists.
February 2007
NPSE0396_FEB_2007
También podría gustarte
- Treatment of Resistant and Refractory HypertensionDocumento21 páginasTreatment of Resistant and Refractory HypertensionLuis Rodriguez100% (1)
- Dr. Alurkur's Book On Cardiology - 2Documento85 páginasDr. Alurkur's Book On Cardiology - 2Bhattarai ShrinkhalaAún no hay calificaciones
- Getting the Hospital Job: A Step-by-Step Guide to Applying for Your First PositionDocumento41 páginasGetting the Hospital Job: A Step-by-Step Guide to Applying for Your First Position1234chocoAún no hay calificaciones
- Intravenous Fluid Therapy in Adults in Hospital Algorithm Poster Set 191627821Documento5 páginasIntravenous Fluid Therapy in Adults in Hospital Algorithm Poster Set 191627821crsscribdAún no hay calificaciones
- Managing Psychiatric Patients in The EDDocumento28 páginasManaging Psychiatric Patients in The EDfadiAún no hay calificaciones
- Opioid Analgesics: Mechanisms of Action and Clinical UsesDocumento20 páginasOpioid Analgesics: Mechanisms of Action and Clinical UsesRichard100% (1)
- Sinus ArrhythmiaDocumento6 páginasSinus ArrhythmiaVincent Maralit MaterialAún no hay calificaciones
- Prescribing Medicine in Pregnancy, by Australian Drug Evaluation CommitteeDocumento90 páginasPrescribing Medicine in Pregnancy, by Australian Drug Evaluation Committee徐承恩100% (1)
- Peripheral Artery Occlusive Disease: What To Do About Intermittent Claudication??Documento46 páginasPeripheral Artery Occlusive Disease: What To Do About Intermittent Claudication??Dzariyat_Azhar_9277100% (1)
- Anti-Anginal DrugsDocumento39 páginasAnti-Anginal Drugspoonam rana100% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDe EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsAún no hay calificaciones
- Drugs in Cardiac EnmergenciesDocumento94 páginasDrugs in Cardiac EnmergenciesVijayan VelayudhanAún no hay calificaciones
- Metoprolol Teaching PlanDocumento18 páginasMetoprolol Teaching Planapi-419091662Aún no hay calificaciones
- Pain Management in Infants - Children - AdolescentsDocumento9 páginasPain Management in Infants - Children - AdolescentsOxana Turcu100% (1)
- Clinical Handover Ian ScottDocumento26 páginasClinical Handover Ian ScottYwagar YwagarAún no hay calificaciones
- Psychiatric and Behavioral Aspects of Epilepsy: Nigel C. Jones Andres M. Kanner EditorsDocumento352 páginasPsychiatric and Behavioral Aspects of Epilepsy: Nigel C. Jones Andres M. Kanner EditorsDAVID100% (1)
- TLS FinalDocumento69 páginasTLS FinalGrace Arthur100% (1)
- Cyanotic Spell: Dr. Shirley L A, Sp. A 12 April 2011Documento6 páginasCyanotic Spell: Dr. Shirley L A, Sp. A 12 April 2011Kahfi Rakhmadian KiraAún no hay calificaciones
- USMLE Flashcards: Anatomy - Side by SideDocumento190 páginasUSMLE Flashcards: Anatomy - Side by SideMedSchoolStuff100% (3)
- Hypertension Treatment Steps For HypertensionDocumento15 páginasHypertension Treatment Steps For Hypertensionfreelancer08100% (1)
- Howlett and Ramesh Educational Policy ModelDocumento11 páginasHowlett and Ramesh Educational Policy ModelJaquelyn Montales100% (1)
- FIRST AID by Dr. Qasim AhmedDocumento80 páginasFIRST AID by Dr. Qasim AhmedFaheem KhanAún no hay calificaciones
- Antifungal Drugs: - Polyene Antibiotics: Amphotericin B, Nystatin - Antimetabolites: 5-Fluorocytosine - AzolesDocumento18 páginasAntifungal Drugs: - Polyene Antibiotics: Amphotericin B, Nystatin - Antimetabolites: 5-Fluorocytosine - AzolesgopscharanAún no hay calificaciones
- Hypertensive Crisis: Megat Mohd Azman Bin AdzmiDocumento34 páginasHypertensive Crisis: Megat Mohd Azman Bin AdzmiMegat Mohd Azman AdzmiAún no hay calificaciones
- Fluid N Electrolyte BalanceDocumento60 páginasFluid N Electrolyte BalanceAnusha Verghese67% (3)
- Pain ManagementDocumento78 páginasPain ManagementKiran100% (1)
- At2-Bsbsus411 (2) Done 29Documento15 páginasAt2-Bsbsus411 (2) Done 29DRSSONIA11MAY SHARMAAún no hay calificaciones
- ECMO and Right Ventricular FailureDocumento9 páginasECMO and Right Ventricular FailureLuis Fernando Morales JuradoAún no hay calificaciones
- Language of PreventionDocumento9 páginasLanguage of Prevention1234chocoAún no hay calificaciones
- Working Like A Scientist Grade 8Documento26 páginasWorking Like A Scientist Grade 8Therese D'Aguillar100% (1)
- Asthma 160424141552Documento54 páginasAsthma 160424141552almukhtabir100% (1)
- Standard Treatment GuidelinesDocumento5 páginasStandard Treatment Guidelinesbournvilleeater100% (1)
- Intravenous Fluid Therapy - Knowledge For Medical Students and PhysiciansDocumento6 páginasIntravenous Fluid Therapy - Knowledge For Medical Students and PhysiciansNafiul IslamAún no hay calificaciones
- Intravenous FluidsDocumento3 páginasIntravenous FluidsKristine Artes AguilarAún no hay calificaciones
- Maged 2015Documento185 páginasMaged 2015engy6nagyAún no hay calificaciones
- Standard Treatment WorkflowsDocumento75 páginasStandard Treatment WorkflowsIndranil DuttaAún no hay calificaciones
- 2020 Intravenous Fuid TherapyDocumento19 páginas2020 Intravenous Fuid TherapyDaniela MéndezAún no hay calificaciones
- Management of Hypertension in CKD 2015Documento9 páginasManagement of Hypertension in CKD 2015Alexander BallesterosAún no hay calificaciones
- IPHS Guidelines Health Centres PDFDocumento92 páginasIPHS Guidelines Health Centres PDFAnuradha YadavAún no hay calificaciones
- Aldrete'sDocumento1 páginaAldrete'sKarlston LapnitenAún no hay calificaciones
- Essential HypertensionDocumento13 páginasEssential HypertensionIvan KurniadiAún no hay calificaciones
- PalliationDocumento16 páginasPalliationPartha ChakrabortyAún no hay calificaciones
- Rational Drug Prescribing Training CourseDocumento78 páginasRational Drug Prescribing Training CourseAhmadu Shehu MohammedAún no hay calificaciones
- Safety PharmacologyDocumento20 páginasSafety PharmacologyPranjal KothaleAún no hay calificaciones
- Advanced Cardiac Life SupportDocumento37 páginasAdvanced Cardiac Life SupportRoy Acosta GumbanAún no hay calificaciones
- Drug Compliance Among Hypertensive PatientsDocumento5 páginasDrug Compliance Among Hypertensive PatientsSyifa MunawarahAún no hay calificaciones
- Principles of Fluid ManagementDocumento17 páginasPrinciples of Fluid ManagementBrainy-Paykiesaurus LuminirexAún no hay calificaciones
- Makalah HypertensionDocumento6 páginasMakalah HypertensionFatin ZafirahAún no hay calificaciones
- Pharmacotherapy of StrokeDocumento37 páginasPharmacotherapy of StrokeAndykaYayanSetiawanAún no hay calificaciones
- ICU-Procedural 1st YearDocumento3 páginasICU-Procedural 1st YearNephrology On-DemandAún no hay calificaciones
- Neurologic Assessment RationaleDocumento16 páginasNeurologic Assessment RationaleflorenzoAún no hay calificaciones
- Drugs Affecting Myometrium1 PDFDocumento9 páginasDrugs Affecting Myometrium1 PDFЛариса ТкачеваAún no hay calificaciones
- Nurse PicuDocumento5 páginasNurse PicuDitto RezkiawanAún no hay calificaciones
- Medicine CPDocumento127 páginasMedicine CPDipesh ShresthaAún no hay calificaciones
- Critical Care Update PDFDocumento25 páginasCritical Care Update PDFHugo PozoAún no hay calificaciones
- World Journal of Pharmacy and Pharmaceutical Sciences Review ArticleDocumento12 páginasWorld Journal of Pharmacy and Pharmaceutical Sciences Review Articlevikas vermaAún no hay calificaciones
- Hypertensive Emergencies (ESC 2019)Documento10 páginasHypertensive Emergencies (ESC 2019)Glen LazarusAún no hay calificaciones
- Cardiac ValveDocumento12 páginasCardiac ValveHellen WestgroveAún no hay calificaciones
- Intravenous (IV) InfusionDocumento16 páginasIntravenous (IV) InfusionSiti Rukayah100% (1)
- Biostatistics Community Medicine Gomal Medical College NotesDocumento22 páginasBiostatistics Community Medicine Gomal Medical College Notesjay_p_shah0% (1)
- Acute vs Chronic Pain: Key DifferencesDocumento20 páginasAcute vs Chronic Pain: Key DifferencessukunathAún no hay calificaciones
- Coagulation: Bleeding TimeDocumento6 páginasCoagulation: Bleeding TimeimperiouxxAún no hay calificaciones
- Ayurvedic Insights of Avascular Necrosis of Femoral HeadDocumento4 páginasAyurvedic Insights of Avascular Necrosis of Femoral HeadIJAR JOURNALAún no hay calificaciones
- Safeguards for Reducing Errors with High Alert MedicationsDocumento27 páginasSafeguards for Reducing Errors with High Alert MedicationsnovitalumintusariAún no hay calificaciones
- Managing Acute Pain in Opioid-Tolerant PatientsDocumento6 páginasManaging Acute Pain in Opioid-Tolerant PatientsHendrikus Surya Adhi PutraAún no hay calificaciones
- Pemantauan Dan Penanganan Nyeri Pasca BedahDocumento42 páginasPemantauan Dan Penanganan Nyeri Pasca BedahAkbar Muitan LantauAún no hay calificaciones
- Pokemon Theme Song 22Documento4 páginasPokemon Theme Song 221234chocoAún no hay calificaciones
- # 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in EDDocumento7 páginas# 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in ED1234chocoAún no hay calificaciones
- Code Geass - StoriesDocumento5 páginasCode Geass - Stories1234chocoAún no hay calificaciones
- Blue Veins Sub Theme TVBDocumento4 páginasBlue Veins Sub Theme TVB1234chocoAún no hay calificaciones
- Topical Steroids (Sep 19) PDFDocumento7 páginasTopical Steroids (Sep 19) PDF1234chocoAún no hay calificaciones
- Mbs Quick Guide: JULY 2020Documento2 páginasMbs Quick Guide: JULY 20201234chocoAún no hay calificaciones
- QLD Rail Traim PDFDocumento1 páginaQLD Rail Traim PDF1234chocoAún no hay calificaciones
- Fairy Tail - Main ThemeDocumento3 páginasFairy Tail - Main Theme1234chocoAún no hay calificaciones
- Osteo Infographic FinalDocumento1 páginaOsteo Infographic Final1234chocoAún no hay calificaciones
- Doctor Talk: Communication Practice Role PlaysDocumento6 páginasDoctor Talk: Communication Practice Role Plays1234chocoAún no hay calificaciones
- Fluids ElectrolytesDocumento2 páginasFluids Electrolytes1234chocoAún no hay calificaciones
- Blue BirdDocumento7 páginasBlue Bird1234chocoAún no hay calificaciones
- Topical Steroids (Sep 19) PDFDocumento7 páginasTopical Steroids (Sep 19) PDF1234chocoAún no hay calificaciones
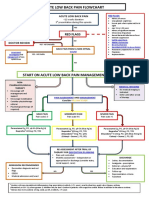
- Acute Low Back Pain Flowchart January 2017Documento1 páginaAcute Low Back Pain Flowchart January 20171234chocoAún no hay calificaciones
- PBM Module1 MTP Template 0Documento2 páginasPBM Module1 MTP Template 01234chocoAún no hay calificaciones
- VTE GuidelinesDocumento11 páginasVTE Guidelines1234chocoAún no hay calificaciones
- Managing Mental Illness in Patients From CALD Backgrounds: PsychiatryDocumento5 páginasManaging Mental Illness in Patients From CALD Backgrounds: Psychiatry1234chocoAún no hay calificaciones
- Taking a Social and Cultural History: A Biopsychosocial ApproachDocumento3 páginasTaking a Social and Cultural History: A Biopsychosocial Approach1234chocoAún no hay calificaciones
- 2016 Applicant Guide Web V2Documento83 páginas2016 Applicant Guide Web V21234chocoAún no hay calificaciones
- Metro South Intern Training Form (Logan)Documento3 páginasMetro South Intern Training Form (Logan)1234chocoAún no hay calificaciones
- FLOWCHART - ARC Adult Cardiorespiratory ArrestDocumento1 páginaFLOWCHART - ARC Adult Cardiorespiratory Arrest1234chocoAún no hay calificaciones
- The Effects of Social Networks On Disability in Older AustraliansDocumento22 páginasThe Effects of Social Networks On Disability in Older Australians1234chocoAún no hay calificaciones
- Herd Immunity'' A Rough Guide PDFDocumento6 páginasHerd Immunity'' A Rough Guide PDF1234chocoAún no hay calificaciones
- ImprovingMedAdherenceOlderAdultslyer Final 508CDocumento2 páginasImprovingMedAdherenceOlderAdultslyer Final 508CKumar PatilAún no hay calificaciones
- Clinical Contributions To Addressing The Social Determinants of HealthDocumento5 páginasClinical Contributions To Addressing The Social Determinants of Health1234chocoAún no hay calificaciones
- Defining and Assessing Risks To Health PDFDocumento20 páginasDefining and Assessing Risks To Health PDF1234chocoAún no hay calificaciones
- A Conceptual Framework For HealthDocumento1 páginaA Conceptual Framework For Health1234chocoAún no hay calificaciones
- Frcpath Part 1 Previous Questions: Document1Documento11 páginasFrcpath Part 1 Previous Questions: Document1Ali LaftaAún no hay calificaciones
- Limulus Amebocyte Lysate Test (LAL)Documento16 páginasLimulus Amebocyte Lysate Test (LAL)Shahriar ShamimAún no hay calificaciones
- De Luyen Thi TNTHPT (6) - HsDocumento5 páginasDe Luyen Thi TNTHPT (6) - HsPhương Quang Nguyễn LýAún no hay calificaciones
- Male, Masculinities Methodologies and MethodsDocumento40 páginasMale, Masculinities Methodologies and MethodsMarco Rojas VAún no hay calificaciones
- GSGMC Department Vacancies by SpecialtyDocumento6 páginasGSGMC Department Vacancies by SpecialtyRajaAún no hay calificaciones
- Reasons for Conducting Qualitative ResearchDocumento12 páginasReasons for Conducting Qualitative ResearchMa. Rhona Faye MedesAún no hay calificaciones
- Healing Wonders AppDocumento18 páginasHealing Wonders AppJoanna Atrisk C-LealAún no hay calificaciones
- Speech by SakiDocumento2 páginasSpeech by Sakiapi-516439363Aún no hay calificaciones
- 3710Documento9 páginas3710Asad KhanAún no hay calificaciones
- Dialysis Report - NURS 302Documento3 páginasDialysis Report - NURS 302AmalAún no hay calificaciones
- COBADocumento222 páginasCOBArendiAún no hay calificaciones
- Google CL Ebony ThomasDocumento2 páginasGoogle CL Ebony Thomasebony thomasAún no hay calificaciones
- Task 2 Case Notes: James Hutton: Time AllowedDocumento3 páginasTask 2 Case Notes: James Hutton: Time AllowedKelvin Kanengoni0% (1)
- Sublingual Sialocele in A Cat: Jean Bassanino, Sophie Palierne, Margaux Blondel and Brice S ReynoldsDocumento5 páginasSublingual Sialocele in A Cat: Jean Bassanino, Sophie Palierne, Margaux Blondel and Brice S ReynoldsTarsilaRibeiroMaiaAún no hay calificaciones
- Full Download Contemporary Nutrition A Functional Approach 4th Edition Wardlaw Solutions ManualDocumento36 páginasFull Download Contemporary Nutrition A Functional Approach 4th Edition Wardlaw Solutions Manualalojlyhol3100% (33)
- WiproDocumento14 páginasWipromalla srujanaAún no hay calificaciones
- Sports Injuries - StrainDocumento10 páginasSports Injuries - StrainChris SinugbojanAún no hay calificaciones
- Stress Eating: A Phenomenological StudyDocumento24 páginasStress Eating: A Phenomenological StudyGauis Laurence CaraoaAún no hay calificaciones
- Goal Planning and Neurorehabilitation: The Wolfson Neurorehabilitation Centre ApproachDocumento13 páginasGoal Planning and Neurorehabilitation: The Wolfson Neurorehabilitation Centre ApproachMiguelySusy Ramos-RojasAún no hay calificaciones
- The Nigerian National Health Policy and StructureDocumento24 páginasThe Nigerian National Health Policy and StructureofficialmidasAún no hay calificaciones
- TLE8 Q0 Mod5 Cookery v2Documento14 páginasTLE8 Q0 Mod5 Cookery v2Lauro Jr. AtienzaAún no hay calificaciones
- History of Movement EducationDocumento4 páginasHistory of Movement EducationMark FernandezAún no hay calificaciones
- Folder - Farming Insects - 2Documento2 páginasFolder - Farming Insects - 2Paulin NanaAún no hay calificaciones
- Pediatric Concept MapDocumento6 páginasPediatric Concept Mapapi-507427888Aún no hay calificaciones
- KHDA - Dar Al Marefa School 2016-2017Documento27 páginasKHDA - Dar Al Marefa School 2016-2017Edarabia.comAún no hay calificaciones
- RS5312 Assignment Analyzes Low Back Pain Case Using GuidelinesDocumento9 páginasRS5312 Assignment Analyzes Low Back Pain Case Using GuidelinesCelina Tam Ching LamAún no hay calificaciones