Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Chapter 18 - The Heart Study Guide: Save Date: Wednesday, March 25, 2009 4:18:00 PM
Cargado por
Bettina RosuTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Chapter 18 - The Heart Study Guide: Save Date: Wednesday, March 25, 2009 4:18:00 PM
Cargado por
Bettina RosuCopyright:
Formatos disponibles
Chapter 18 The Heart Study Guide Part 1
Wednesday March 25, 2009
Page 1 of 7
Chapter 18 The Heart
Study Guide
Location of the heart
Mediastinum is the body cavity between the lungs where the heart lies
About two-thirds of the heart is to the left of the midline
Apex of the heart points to the left hip and contacts the chest wall. This is where
it is easiest to feel the heart beat.
Structures around the heart
Fibrous pericardium dense connective tissue layer protects and anchors the heart and
prevents overfilling
Serous pericardium double-walled membranes within the fibrous pericardium
Serous fluid is between the layers
Inflammation between the layers can create painful adhesions
Excess fluid from inflammation can actually inhibit pumping. This is
cardiac tamponade
The heart is a pair of pumps working in a coordinated way
The right side pumps blood to the lungs - pulmonary circuit
The left side pumps blood to the body - systemic circuit
Cardiac muscle
cells are interconnected by connective tissue fibers that form a fibrous skeleton of
the heart. The fibers and muscles are arranged in spiraling bundles. This
arrangement creates a wringing action of the heart when it contracts.
Wringing action of the ventricles ejects blood superiorly into the arteries leaving
the ventricles
Chambers of the heart
Atria deoxygenated blood from the body enters the right atrium. Oxygenated blood
from the lungs enters the left atrium. The two atria are relatively small and have
relatively thin walls.
Ventricles the right ventricle pumps blood to the lungs and is relatively thin-walled
The left ventricle pumps blood to the body and is much more thick-walled.
C:\Documents and Settings\adele.cunningham\My Documents\APII spring 09\lectures
and study guides APII spring 09\study guides APII spring 09\BIOL2112-Chapter18Heart-StudyGuide01.doc
Save date: Wednesday, March 25, 2009 4:18:00 PM
Chapter 18 The Heart Study Guide Part 1
Wednesday March 25, 2009
Page 2 of 7
Valves
Tricuspid or right atrioventricular valve connects the right atrium to the right
ventricle
Left atrioventricular valve is also called the bicuspid or mitral valve. It
connects the left atrium to the left ventricle.
Semilunar valves - have three cusps or cup-like structures
Pulmonary semilunar valve - leads from the right ventricle to the
pulmonary trunk (artery)
Aortic semilunar valve - leads from the left ventricle to the body
Definitions of artery and vein
Artery takes blood away from the chambers of the heart
Vein - brings blood back to the chambers of the heart
When you look at the heart as it beats, contraction of the two sides is almost
simultaneous (left side leads slightly)
The two atria fill with blood
When pressure increases enough the AV valves open
Ventricles begin to fill with blood
Contraction of the atria sends more blood through
The valves close
There is a pause that
Gives the atrioventricular valves time to close
And is the hearts only chance to rest
The ventricles contract and propel blood into the large blood vessels at the heart
Trace the path of a single drop of blood through the heart
Dont lose sight of the overall purpose to send oxygenated blood to the body.
The heart collects blood from the body (both above and below the heart), sends it
to the lungs for oxygen, and then distributes it to the body.
Deoxygenated blood from the superior and inferior vena cava enter the right
atrium
When there is enough pressure, the tricuspid valve opens and lets blood flow
into the right ventricle.
The right atrium contracts to push more blood through.
Papillary muscles connected to chordae tendinae pull the tricuspid valve
closed
The right ventricle contracts and sends blood through the pulmonary semilunar valves to the pulmonary artery and to the lungs. As the ventricle relaxes,
pressure drops and blood flows backwards through the pulmonary artery to
close the semilunar valve.
C:\Documents and Settings\adele.cunningham\My Documents\APII spring 09\lectures
and study guides APII spring 09\study guides APII spring 09\BIOL2112-Chapter18Heart-StudyGuide01.doc
Save date: Wednesday, March 25, 2009 4:18:00 PM
Chapter 18 The Heart Study Guide Part 1
Wednesday March 25, 2009
Page 3 of 7
Blood returns from the lungs through the pulmonary veins
The pulmonary veins empty into the left atrium
When there is enough pressure, the bicuspid (mitral) valve opens and lets blood
flow into the left ventricle.
The left atrium contracts to push more blood through.
Papillary muscles connected to chordae tendinae pull the bicuspid valve
closed.
The left ventricle contracts, forcing blood through the aortic semilunar valve to
the aorta and to the body. As the ventricle relaxes, pressure drops and blood
flows backwards through the aorta to close the semilunar valve.
Note for study: For the lecture test, you are responsible for all the information
above. For the quiz on tracing a single drop of blood through the heart, the
minimum you must include to avoid losing points is the structures below.
1. Begin with blood returning from the body through the superior and
inferior vena cavae
2. right atrium
3. tricuspid valve (or right atrioventricular valve)
4. right ventricle
5. pulmonary semilunar valve
6. pulmonary trunk (artery)
7. pulmonary veins
8. left atrium
9. bicuspid (mitral or left atrioventricular valve)
10. left ventricle
11. aortic semilunar valve
12. aorta
Diastole and Systole
Diastole is a general term for relaxation of either atria or ventricles.
Systole is a general term for contraction of either atria or ventricles.
When speaking of diastolic and systolic pressure of the heart, these terms refer to the
ventricles.
Ventricular diastole is diastolic blood pressure.
Ventricular systole produces the systolic blood pressure.
C:\Documents and Settings\adele.cunningham\My Documents\APII spring 09\lectures
and study guides APII spring 09\study guides APII spring 09\BIOL2112-Chapter18Heart-StudyGuide01.doc
Save date: Wednesday, March 25, 2009 4:18:00 PM
Chapter 18 The Heart Study Guide Part 1
Wednesday March 25, 2009
Page 4 of 7
Cardiac output
Some blood remains in the ventricle after it contracts
The cardiac output is the difference between the amount of blood that enters (end
diastolic) and the amount that is left (end systolic)
Usually, output is constant
Factors that affect output
Exercise because it returns more blood to the right atrium
Strength of cardiac muscle contraction is strongest
when cardiac muscle is stretched (because contractile
proteins have the most overlap at a certain level of
stretching)
Anything that increases resistance to flow especially back
pressure due to stiff valves or arteriosclerosis at the aorta
Anything that increases heart rate without increasing the
strength of a contraction, especially heart arrhythmias
The heart itself must be supplied with blood
Right and left coronary arteries branch at the base of the aorta and become
Anterior and posterior interventricular coronary arteries supply blood to the heart itself.
The coronary sinus is a vein that drains blood from the myocardium into the right atrium.
Angiogenesis the creation of new blood vessels - can occur to compensate for poor
flow
Importance of stress tests
Stress tests can find blockage before it kills
A radiotracer such as thallium can reveal blockage
Abnormal flow that only appears during exercise is
probably blockage
Abnormal flow appearing during rest and exercise may
be due to scar tissue
Angina pectoris transient insufficient oxygen may be due to stress- induced
spasms of arteries, physical exertion
Myocardial infarction oxygen deficit kills some cells. Heart cells are probably
amitotic. Noncontractile scar tissue forms.
Layers of the heart wall (under the fibrous pericardium)
The visceral layer of the serous pericardium
Endocardium epithelial tissue covers valves too and is continuous with epithelial
lining of the blood vessels leaving the heart
Myocardium the muscular layer
Intercalated discs consist of two kinds of junctions
Desmosomes are protein rivets that help distribute stress
Gap junctions connect muscle cells with protein tunnels and help the heart act as
a coordinated unit
C:\Documents and Settings\adele.cunningham\My Documents\APII spring 09\lectures
and study guides APII spring 09\study guides APII spring 09\BIOL2112-Chapter18Heart-StudyGuide01.doc
Save date: Wednesday, March 25, 2009 4:18:00 PM
Chapter 18 The Heart Study Guide Part 1
Wednesday March 25, 2009
Page 5 of 7
Anatomy of nodes autorhythmic or pacemaker cardiac cells
All muscle cells of the heart are excitable. They communicate by action potentials
- nerve impulses. Some specialized noncontractile cells the nodes set the rhythm of
contractions. Pacemakers are autorhythmic and not contractile. That is they
spontaneously go through depolarization and repolarization at a certain pace.
Depolarization when a cardiac muscle cell is stimulated by another cardiac cell or by
the nervous system, it becomes very permeable to sodium and calcium. This influx of
sodium and calcium makes the cell membrane more positive. This influx of sodium and
calcium spreads from cell to cell it is the way cardiac muscle cells communicate. When
the membrane reaches a threshold positive charge, the membrane becomes more
permeable to potassium and repolarization occurs - potassium flows out of the cell
making it more negative until the muscle cell reaches its resting charge.
In the heart, it takes a little longer to initiate a new influx of sodium and calcium. That is,
the heart has a longer refractory period when it can not initiate a new impulse at the
same point. This slowness helps coordinate contractions.
SA node sinoatrial node is located in the right atrium near the superior vena cava. It
determines heart rate normally. Normal rhythm is called sinus rhythm.
AV node is located in the right atrium just above the tricuspid valve near the septum
between atria.
Bundle of His (AV bundle) located superiorly between the ventricles
Purkinje fibers complete the path through the interventricular septum and then turn
superiorly into the ventricular walls
Sequence of activation of pacemaker cells
Beat starts at SA node in the right atrial wall just inferior to superior vena cava.
Excitation (depolarization) spreads across the two atria.
The AV in the inferior part of interatrial septum delays the impulse allowing atria to
finish contracting before ventricles contract. The AV has smaller fibers and fewer gap
junctions.
Bundle of His superior part of interventricular septum distributes to lower ventricle
Bundle of His (atrioventricular bundle) divides into two branches that travel down the
septum. Excitation follows the two branches of the bundle of His (bundle branches) and
travels to the apex of the heart.
Purkinje distribute the signal up the ventricles from the apex.
EKG electrocardiogram or ECG (K is from the Greek kardia) This is a graph that
represents the overall, net electrical changes in the heart due to changes of ions (action
potentials).
The P wave represents depolarization of the atria - depolarization immediately precedes
contraction.
The QRS wave represents depolarization of the ventricles.
The T wave represents repolarization of the ventricles.
Repolarization of the atria is masked by the larger QRS wave.
C:\Documents and Settings\adele.cunningham\My Documents\APII spring 09\lectures
and study guides APII spring 09\study guides APII spring 09\BIOL2112-Chapter18Heart-StudyGuide01.doc
Save date: Wednesday, March 25, 2009 4:18:00 PM
Chapter 18 The Heart Study Guide Part 1
Wednesday March 25, 2009
Page 6 of 7
In the case of a defective SA node, the AV node, which has a much slower intrinsic beat
may direct the rhythm of the heart. Or an ectopic (in the wrong place) node may develop.
Ectopic nodes can develop even when the SA node is functioning
Damage to the AV node is called heart block because the AV node is the only point of
communication between the atria and the ventricles.
Arrhythmias
Atrial flutter an ectopic pacemaker in the right atrium results in about 300 beats/min
for atria and about 150/min for the ventricles. Atrial flutter may be the result of heart
damage such as congestive heart failure or may occur in an otherwise healthy heart.
Chances of having atrial flutter increase with age. Atrial flutter can be treated with drugs
- beta blockers or calcium blockers - or by ablating the abnormal circuit.
Atrial fibrillation is a dangerous condition that renders the heart useless as a pump.
An electric shock is used to depolarize the entire myocardium and to re-establish normal,
or sinus rhythm.
Factors that affect the heart rate and/or strength of contractions
Notice that these two factors are normally inter-related. If you increase heart rate
without increasing the strength of contractions, then the cardiac output (volume of blood
leaving the heart with each beat) is less with each beat.
The main factor that affects strength of contraction and heart rate is the amount of
blood returning to the heart. Normally, this increase in blood flowing into the heart
occurs during exercise. Stretching the heart muscle slightly causes it to contract with
greater force.
Bainbridge effect is a sympathetic nervous system response to increased venous
return and atrial stretching. Atrial stretch receptors activate the
sympathetic
nervous system and increase both heart rate and the strength of
contractions.
Sympathetic and parasympathetic nervous systems
Both stimulate the heart continuously
Sympathetic increases and parasympathetic decreases heart rate.
The parasympathetic usually dominates and slows the SA node to about
75 beats/min. When the vagus nerve, a parasympathetic nerve, is cut, the
heart beats at about 100 beats/min
The heart is said to have vagal tone because the vagus nerve of the
parasympathetic nervous system usually regulates heart beat
Epinephrine - from the adrenal medulla - and norepinephrine - from the
sympathetic nervous system - increase heart rate and the strength of contractions
Thyroxine increases the effect of epinephrine and norepinephrine on the heart
Chronic hyperthyroidism leads to a weakened heart.
C:\Documents and Settings\adele.cunningham\My Documents\APII spring 09\lectures
and study guides APII spring 09\study guides APII spring 09\BIOL2112-Chapter18Heart-StudyGuide01.doc
Save date: Wednesday, March 25, 2009 4:18:00 PM
Chapter 18 The Heart Study Guide Part 1
Wednesday March 25, 2009
Page 7 of 7
Ion concentrations affect heart
Calcium is involved in action potentials and as a signal for contraction
within individual cells
Potassium - potassium outflow occurs during repolarization
Too little or too much of either can lead to weak or irregular heart beats
Back pressure from the aorta, for instance due to arteriosclerosis, reduces stroke
volume and the heart compensates by increasing contractility and heart rate.
Heat
Higher body temperatures increase heart rate by increasing metabolic
rates of cardiac cells. A high fever produces a rapid, weak heart beat.
Abnormally fast heart rate is tachycardia - over 100 beats/min
Slow heart rate under 60 beats/minute is bradycardia - can be due to cold or due to
endurance exercise
Normal heart rate 72 -80 beats/min for women and slightly slower for men
Congestive heart failure
Normally, equal volumes of blood are pumped by the right and left heart
Failure of one side results in fluid build-up of the other system.
Failure of the right side results in systemic fluid build-up and swollen ankles, feet and
fingers
Failure of left side results in pulmonary congestion
C:\Documents and Settings\adele.cunningham\My Documents\APII spring 09\lectures
and study guides APII spring 09\study guides APII spring 09\BIOL2112-Chapter18Heart-StudyGuide01.doc
Save date: Wednesday, March 25, 2009 4:18:00 PM
También podría gustarte
- Cardiovascular System - Transportation 1Documento28 páginasCardiovascular System - Transportation 1Louise Mica Lee100% (1)
- Clinical MedicineDocumento18 páginasClinical MedicineRishikesh AsthanaAún no hay calificaciones
- Faith HealingDocumento23 páginasFaith Healingcreamyfrappe0% (1)
- AP Chapter 16BDocumento35 páginasAP Chapter 16BJay Patel100% (1)
- Cardiovascular DiseaseDocumento22 páginasCardiovascular DiseaseSunday JamesAún no hay calificaciones
- Anatomy and Physiology ASCVDDocumento9 páginasAnatomy and Physiology ASCVDAlvheen JoaquinAún no hay calificaciones
- Cardiovascular SystemDocumento14 páginasCardiovascular SystemAthena Huynh100% (1)
- Cardiovascular SystemDocumento34 páginasCardiovascular Systemurooj100% (1)
- AMCA Study Guide PhlebotomyDocumento34 páginasAMCA Study Guide Phlebotomyayoonia100% (1)
- Anatomy and Physiology of HeartDocumento69 páginasAnatomy and Physiology of HeartRitu Arun Kaushik100% (1)
- Textbook of Forensic Medicine & Toxicology (VV Pillay)Documento513 páginasTextbook of Forensic Medicine & Toxicology (VV Pillay)s.misbaunnisa26100% (3)
- Cardiogenic ShockDocumento14 páginasCardiogenic ShockZellanien hdAún no hay calificaciones
- Cardiac PhysiologyDocumento102 páginasCardiac PhysiologyPeter Larsen100% (1)
- Assignment On Anatomy and Physiology of Heart: Submitted By: Submitted To: Jayita Gayen Madam S. PoddarDocumento10 páginasAssignment On Anatomy and Physiology of Heart: Submitted By: Submitted To: Jayita Gayen Madam S. PoddarJayita Gayen DuttaAún no hay calificaciones
- HeartDocumento6 páginasHeartAhmed OmaarAún no hay calificaciones
- Anatomy & Physiology of Heart: BY: Mr. Anurag Lecturer College of Nursing DMC & H, LudhianaDocumento56 páginasAnatomy & Physiology of Heart: BY: Mr. Anurag Lecturer College of Nursing DMC & H, Ludhianapreet kaurAún no hay calificaciones
- Cardio Vascular SystemDocumento8 páginasCardio Vascular SystemguptaasitAún no hay calificaciones
- Cardiovascular SystemDocumento32 páginasCardiovascular SystemAugustus Alejandro ZenitAún no hay calificaciones
- Cardiovascular System: Presented by DR Aparna Ramachandran Mds 1 Dept of Public Health DentistryDocumento73 páginasCardiovascular System: Presented by DR Aparna Ramachandran Mds 1 Dept of Public Health DentistryAparna RamachandranAún no hay calificaciones
- Microdosing Mushrooms: Fruiting Bodies Introduction ToDocumento12 páginasMicrodosing Mushrooms: Fruiting Bodies Introduction ToPaulo Das Nuvens100% (2)
- Non-Alcoholic Fatty Liver DiseaseDocumento15 páginasNon-Alcoholic Fatty Liver DiseaseKurnia pralisaAún no hay calificaciones
- Bob Beck Lecture - Take Back Your PowerDocumento42 páginasBob Beck Lecture - Take Back Your Powerprobiermalaus100% (1)
- Clinical Case Study Guide - Cardiopulmonary Physical Therapy 3ed PDFDocumento245 páginasClinical Case Study Guide - Cardiopulmonary Physical Therapy 3ed PDFraquelbibi0% (1)
- CHAPTER 3 GcsDocumento14 páginasCHAPTER 3 GcsNurse NotesAún no hay calificaciones
- Anatomy of The HeartDocumento8 páginasAnatomy of The HeartAbigail BrillantesAún no hay calificaciones
- Managing The Risk of FatigueDocumento26 páginasManaging The Risk of Fatiguenapinnvo100% (1)
- Chapter 19 Heart Marie BDocumento29 páginasChapter 19 Heart Marie BomarAún no hay calificaciones
- Medical Nutrition Therapy: Burn Patients: Amy GabrielsonDocumento33 páginasMedical Nutrition Therapy: Burn Patients: Amy GabrielsonImam HakikiAún no hay calificaciones
- Chapter I - Cardiovascular System: HeartDocumento2 páginasChapter I - Cardiovascular System: HeartIndranil SinhaAún no hay calificaciones
- Understanding How Your Heart FunctionsDocumento4 páginasUnderstanding How Your Heart FunctionsthenameisvijayAún no hay calificaciones
- HUMAN ANATOMY AND PHYSIOLOGY LABORATORY Cardiovascular SystemDocumento12 páginasHUMAN ANATOMY AND PHYSIOLOGY LABORATORY Cardiovascular SystemZaira MangalimanAún no hay calificaciones
- Cardiac Control CentreDocumento8 páginasCardiac Control CentregeorgeloxdaleAún no hay calificaciones
- Our Heart BeatsDocumento7 páginasOur Heart BeatsferyAún no hay calificaciones
- HeartDocumento7 páginasHeartKaryll AguilaAún no hay calificaciones
- Exam 4 Study Guide (1386)Documento11 páginasExam 4 Study Guide (1386)S. MartinezAún no hay calificaciones
- Circulatory System IIDocumento13 páginasCirculatory System IIsmbdy tbhhhAún no hay calificaciones
- Cardiovascular SystemDocumento5 páginasCardiovascular SystemDrexel DalaygonAún no hay calificaciones
- Project BioDocumento18 páginasProject Bioyanshu falduAún no hay calificaciones
- Basics of The Heart: Katee Beaudry MS 2 - Penn State University College of MedicineDocumento24 páginasBasics of The Heart: Katee Beaudry MS 2 - Penn State University College of MedicineAlkhnsa CaifAún no hay calificaciones
- The HeartDocumento11 páginasThe HeartElisa TapalesAún no hay calificaciones
- The Heart: Basis of Life .?Documento94 páginasThe Heart: Basis of Life .?Diksha AgrawalAún no hay calificaciones
- احلام 1 PDFDocumento7 páginasاحلام 1 PDFEhab Alaa Abd Al-AmeerAún no hay calificaciones
- Anatomy of The HeartDocumento5 páginasAnatomy of The HeartxXjhmXxAún no hay calificaciones
- Cardio 1Documento4 páginasCardio 1Liam Jacque LapuzAún no hay calificaciones
- Heart by Aritra SahaDocumento15 páginasHeart by Aritra SahaAritra SahaAún no hay calificaciones
- Lecture 5 (Heart)Documento10 páginasLecture 5 (Heart)Άγγελος ΧαβέλαςAún no hay calificaciones
- Oral RevDocumento6 páginasOral RevjjolaguerAún no hay calificaciones
- Cardio Vascular SystemDocumento22 páginasCardio Vascular SystemdeborahAún no hay calificaciones
- Common Cardiac Anomalies Seen Within The Cardiac Catheterization LabDocumento23 páginasCommon Cardiac Anomalies Seen Within The Cardiac Catheterization Labapi-356406300Aún no hay calificaciones
- القلبDocumento11 páginasالقلبNajwa AbdualgaderAún no hay calificaciones
- Cardiovascular System - Lecture IDocumento4 páginasCardiovascular System - Lecture IpragantraAún no hay calificaciones
- Cardiovascular SystemDocumento2 páginasCardiovascular Systemmitsuki_sylphAún no hay calificaciones
- Clinical PaperDocumento18 páginasClinical Paperapi-356406300Aún no hay calificaciones
- Anatomy of The HeartDocumento28 páginasAnatomy of The HeartHerman DjawaAún no hay calificaciones
- Bio 12 Ch12 Cardiovascular Sys Notes PackageDocumento16 páginasBio 12 Ch12 Cardiovascular Sys Notes Packagekw2533Aún no hay calificaciones
- Pedrajeta-Heart and Neck Vessels AssessmentDocumento4 páginasPedrajeta-Heart and Neck Vessels AssessmentAndrei PedrajetaAún no hay calificaciones
- Cardiovascularsystem 090820055728 Phpapp02Documento75 páginasCardiovascularsystem 090820055728 Phpapp02muhammad ijazAún no hay calificaciones
- Anaphysio of The HeartDocumento6 páginasAnaphysio of The HeartChamCham AquinoAún no hay calificaciones
- B2U3 CirculationNotesDocumento15 páginasB2U3 CirculationNotesVanusha Azzriel100% (1)
- Chapter 13 - HeartDocumento5 páginasChapter 13 - Heartbussniesm05Aún no hay calificaciones
- Biology Grade 9 - Lesson NoteDocumento9 páginasBiology Grade 9 - Lesson NotemicahxAún no hay calificaciones
- 2 Days Training Module 1Documento36 páginas2 Days Training Module 1ArumAún no hay calificaciones
- 81: Mammalian Heart and Its RegulationDocumento75 páginas81: Mammalian Heart and Its RegulationIt's Ika100% (1)
- Anatomy and Physiology of The Heart: Dr. N. PraveenDocumento56 páginasAnatomy and Physiology of The Heart: Dr. N. Praveenamjad khan100% (1)
- NR 161:cardiology Study Guide Cardiology Study GuideDocumento6 páginasNR 161:cardiology Study Guide Cardiology Study GuideApril Danielle TeschAún no hay calificaciones
- Cardiovascular SystemDocumento101 páginasCardiovascular SystemBanessa Mae GarcianoAún no hay calificaciones
- Management of Clients With Problems of The Cardiovascular SystemDocumento7 páginasManagement of Clients With Problems of The Cardiovascular Systemjerry smatt dumtoAún no hay calificaciones
- Cardio Notes 1Documento8 páginasCardio Notes 1Lindsay Grace MandarioAún no hay calificaciones
- Salcedo ANPH111 The Cardiovascular System23Documento46 páginasSalcedo ANPH111 The Cardiovascular System23ajline.esto23Aún no hay calificaciones
- How To Rid The Body of CandidaDocumento2 páginasHow To Rid The Body of Candidaradio53fingerAún no hay calificaciones
- DkaDocumento32 páginasDkanatheAún no hay calificaciones
- B.SC Nursing - 2019 - 2 - Aug Sept - Pharmacology Pathology andDocumento1 páginaB.SC Nursing - 2019 - 2 - Aug Sept - Pharmacology Pathology andshubham vermaAún no hay calificaciones
- Burns Secret TestDocumento2 páginasBurns Secret TestChin ChanAún no hay calificaciones
- CestodesDocumento39 páginasCestodesNachiket Vijay PotdarAún no hay calificaciones
- 2022 - ACLS - Handbook 1 30 13 30 PDFDocumento18 páginas2022 - ACLS - Handbook 1 30 13 30 PDFJefferson MoraAún no hay calificaciones
- Barium Swallow (Esophagram) :: Positions and Barium Images PurposeDocumento3 páginasBarium Swallow (Esophagram) :: Positions and Barium Images PurposeAaron SmithAún no hay calificaciones
- No-Scar Transoral Thyroglossal Duct Cyst Excision in ChildrenDocumento21 páginasNo-Scar Transoral Thyroglossal Duct Cyst Excision in ChildrenMishel Rodriguez GuzmanAún no hay calificaciones
- HACCP Carbonated Soft DrinksDocumento9 páginasHACCP Carbonated Soft DrinksmubdiantiAún no hay calificaciones
- MudrasDocumento8 páginasMudrasKishore CheralaAún no hay calificaciones
- ER Technician Competency ProfileDocumento6 páginasER Technician Competency Profileplanedude86Aún no hay calificaciones
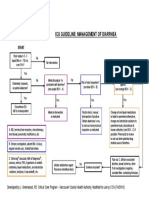
- Icu Guideline: Management of Diarrhea: StartDocumento1 páginaIcu Guideline: Management of Diarrhea: StartGracia VionaAún no hay calificaciones
- Capstone OutlineDocumento3 páginasCapstone Outlineapi-395468231Aún no hay calificaciones
- Guideline On Good Pharmacovigilance Practices (GVP) Module XV Safety Communication (Rev 1)Documento20 páginasGuideline On Good Pharmacovigilance Practices (GVP) Module XV Safety Communication (Rev 1)Salló TivadarAún no hay calificaciones
- Significance of The Structure of Human SkeletonDocumento5 páginasSignificance of The Structure of Human SkeletonTodirenche LarisaAún no hay calificaciones
- Final Letter To NLM Re - IJOEH Nov 2017Documento35 páginasFinal Letter To NLM Re - IJOEH Nov 2017Celeste MonfortonAún no hay calificaciones
- End-Of-Life Care in The Icu: Supporting Nurses To Provide High-Quality CareDocumento5 páginasEnd-Of-Life Care in The Icu: Supporting Nurses To Provide High-Quality CareSERGIO ANDRES CESPEDES GUERREROAún no hay calificaciones
- Anaphy (Lab) ReviewerDocumento3 páginasAnaphy (Lab) ReviewerAgatha Cristie AndradaAún no hay calificaciones
- Contoh Soal Pas BingDocumento8 páginasContoh Soal Pas BingAnnisa AuliaAún no hay calificaciones
- Paroxysmal Nocturnal Hemoglobinuria: Section 13Documento2 páginasParoxysmal Nocturnal Hemoglobinuria: Section 13MANGAún no hay calificaciones