Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Propofol in Neurotrauma
Cargado por
Pekerja KesunyianDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Propofol in Neurotrauma
Cargado por
Pekerja KesunyianCopyright:
Formatos disponibles
Indian Journal of Neurotrauma (IJNT)
41
2008, Vol. 5, No. 1, pp. 41- 44
Drug Review
Propofol in Neurotrauma
TVSP Murthy MD
Prof and Senior Adviser, Neuroanesthesiology
Dept of Anesthesiology and Intensive Care
Army Hospital Research & Referral, Delhi Cantt 110010
Abstract : Propofol (2,6-diisopropylphenol) is one of the most popular agents used for induction of
anesthesia and long-term sedation, owing to its favorable pharmacokinetic profile, which ensures a
rapid recovery even after prolonged administration. Propofol is used widely as a sedative agent in
neurosurgical critical care because it is generally assumed that it has properties that are
advantageous to the injured brain. Propofol is believed to maintain, or even improve, cerebral
autoregulation, indeed even high doses of this drug do not obtund autoregulation or carbon dioxide
reactivity. A neuroprotective effect, beyond that related to the decrease in cerebral metabolic
rate for oxygen, has been shown to play an important role in the so-called multimodal neuroprotection,
a global strategy for the treatment of acute injury of the brain that includes preservation of
cerebral perfusion, temperature control, prevention of infections, and tight glycaemic control.
Keywords: propofol, neuroprotection, traumatic brain injury
INTRODUCTION
Propofol, like many other inhalational and intravenous
anesthetics shares some properties such as the reduction
in the cerebral metabolic rate for oxygen (CMRO2), the
inhibition of glutamate release, and the positive
modulation of GABA-A receptor function, which are
known to mitigate the detrimental effects of acute brain
injury and thus are typical of the ideal neuroprotective
drug1,2. Propofol is chemically unrelated to other clinically
used general anesthetics3. It has a structural analogy with
the antioxidant vitamin E, a fact that can partly explain
its antioxidant properties.
CLINICAL APPLICATION
The first report on the clinical use of Propofol dates
back to 1977 as an anesthesia induction agent 4 .
Subsequently, Propofol has been extensively employed
also for short-term sedation, as well as for long-term
sedation in intensive care unit patients 5.
Propofol exerts its sedative, hypnotic, and amnesic
effects by interacting with an allosteric site on the GABAA receptor, potentiating currents elicited by low
concentrations of GABA, increasing agonist efficacy, and
Address for correspondence:
Col TVSP Murthy MD
Prof and Senior Adviser, Neuroanesthesiology
Dept of Anesthesiology and Intensive Care
Army Hospital Research & Referral, Delhi Cantt 110010
Email : tvspmurthy@yahoo.com
at higher concentrations, directly opening the GABA-A
receptor Cl channel in the absence of GABA6. It also
inhibits excitatory glutamate release by a presynaptic
mechanism7. Interestingly, some of propofols effects such
as ant emesis, post recovery mood alterations, and
postoperative dreaming8, might rely on inhibition of the
cannabinoid degrading enzyme, with consequent
increases in anandamide (AEA) and 2-arachidonylglycerol
in the brain 9. Propofol is characterized by rapid
distribution from blood to tissues, an equally rapid
clearance of the molecule from the blood, and a slow
return of the drug from the deep compartments10, which
is responsible for the rapid onset, clear emergence, and
lack of cumulative effects observed in clinical use.
Adverse properties of Propofol include pain on
injection, apnea after induction, hypotension, and
bradycardia (especially when used with other vagotonic
drugs and in hypovolaemic patients). Decreases in blood
pressure induced by Propofol are generally dose and
infusion rate-dependent, and the effect is related to its
vagotonic activity and to decreases in peripheral vascular
resistance11. Other limitations and adverse effects of
Propofol include the risk of extraneous microbial
contamination of the emulsion formulation and lipidemia
induced by repeated administration of the agent over
time (infusions for periods exceeding 3 days produce
progressive increases in levels of serum lipids, particularly
triglycerides). The so-called propofol infusion syndrome,
characterized by metabolic acidosis and/or
rhabdomyolysis associated with progressive myocardial
failure, although rare, has been increasingly reported over
Indian Journal of Neurotrauma (IJNT), Vol. 5, No. 1, 2008
42
TVSP Murthy
the years12. The syndrome appears to be duration- and
dose-related (usually, doses >5 mg/kg/h for >48 h) and
more frequent in the pediatric population than in adults.
Hence, presently propofol is not indicated for long-lasting
sedation in children.
NEUROPROTECTION
The neuroprotective effects of propofol have been
investigated. Propofol has proved to be an efficacious
neuroprotective agent, but the results have not always
been consistent. Propofol has been postulated to be a
possible beneficial agent against cerebral ischemia based
on the assumption that it decreases cerebral blood flow
(CBF) (with a parallel reduction in CMRO2 and EEG
activity) and mitigates intracranial pressure (ICP), all
effects that are similar to those observed for barbiturates
and other intravenous neuroprotective anesthetic
agents1,2.
The effects on glucose metabolism have been addressed
in a study (13), who have shown that high doses of
propofol (60 mg/kg/h) attenuates both edema formation
and lactate accumulation . One recent study have
demonstrated neuroprotection with propofol also in a
rat model of permanent middle cerebral artery occlusion,
in which a short exposure to oxygen glucose deprivation
(OGD) induced selective neuronal injury, propofol
reduced pyramidal cell death, possibly by preventing an
increase in neuronal mitochondrial swelling14. Hence, it
appears that propofol may block early necrosis in vitro
but not subsequent apoptosis, which is in agreement
with the lack of long-term histological protection in vivo,
particularly if the ischemic insult is severe. However,
this postponement of neuronal death afforded by
propofol may be of importance to permit intervention
with other decisive pharmacologic strategies.
NEUROPROTECTION WITH PROPOFOL:
MECHANISM
As compared with studies in models of cerebral
ischemia, there are relatively fewer reports on the effects
of propofol in experimental traumatic brain injury. Most
anesthetic agents are neuroprotective because of their
ability to reduce the CMRO2, which has a beneficial
impact on the balance between brain energy supply and
demand, and because they increase neuronal tolerance
to hypoxic/ischemic injury. However, propofol has no
direct preconditioning effect and that cerebral metabolic
depression cannot entirely account for its effects in
Indian Journal of Neurotrauma (IJNT), Vol. 5, No. 1, 2008
experimental ischemia, suggesting that there might be
other mechanisms playing a key role in propofol-mediated
neuroprotection15.
Propofol has been proposed to attenuate glutamatemediated excitotoxic mechanisms by either decreasing
NMDA receptor activation, reducing glutamate release,
or recovering the function of transporters responsible
for glutamate uptake into neuronal and glial cells. Propofol
has been shown to modulate glutamate release. Propofol
does not alter high-affinity glutamate uptake by brain
synaptosomes under standard conditions16 but is able to
normalize glutamate transport in astrocytes during
oxidative stress17 and in cortical neurons exposed to
OGD18.
A mechanism that is known to be beneficial against
acute neuronal injury is the potentiation of GABAergic
neuronal activity, mainly due to its counteracting effects
on excitatory neurotoxicity.
Propofol directly activates GABA-A receptors 19,
leading to neuronal hyperpolarization and enhancement
of inhibitory synaptic transmission 16. Free radical
generation is an important component of neurologic
injury. Propofol has been assumed to possess antioxidant
activity because it bears a phenolic OH group like the
natural lipid peroxidation inhibitor -tocopherol (vitamin
E). Indeed, propofol has repeatedly been demonstrated
to inhibit free radical generation, prevent the initiation
of free radical chain reactions, and terminate their
propagation by scavenging highly reactive species and
inhibiting lipid peroxidation.
Following acute brain injury, oxidative stress can lead
to neuronal death by triggering a number of detrimental
cellular responses, including the loss of selective ion
permeability in mitochondria, which appears to be one
of the regulators of the apoptotic cascade 20.
Propofol has also been demonstrated to prevent
mitochondrial swelling caused by acute overload of Ca++
in isolated brain mitochondria or by OGD injury in
organotypic hippocampal slices14. Very recently, propofol
has been shown to interact with the endocannabinoid
system in the brain. This novel mechanism has been
associated with the sedative, psychomimetic, and
antiemetic properties of propofol, but there is
accumulating evidence that the endocannabinoid system
regulates the release of various neurotransmitters and
may also be involved in neuroprotection21.
43
Propofol in Neurotrauma
NEUROPROTECTION IN THE CLINICAL
SETTING
Even molecules that have shown to be dramatically
neuroprotective under experimental conditions may not
have clinical utility if they are endowed with negative
effects on cerebral physiology, especially on ICP and on
the coupling between CBF and CMRO2. The effects of
propofol on cerebral physiology are generally positive.
The effect on CBF is mostly mediated by the reduction
of CMRO2, even if a direct vasoconstrictor effect is also
thought to contribute, as the decrease in CBF is larger
than that in CMRO2. Propofol reduces ICP, a property
that is mandatory in case of intracranial hypertension
and is always favorable in cases of acute brain injury.
Cerebral autoregulation and CO2 responsiveness are
maintained during propofol anesthesia 22 , and an
anticonvulsant activity comparable to that of thiopental
has also been described23. Other specific advantages in
the use of propofol in neurosurgery include a rapid
recovery when intraoperative awake functional evaluation
is requested, a lower incidence of nausea and vomiting
as compared to volatile anesthetics, a lesser degree of
depression of electrophysiological brain activity as
compared to all the other anesthetic agents, which allows
better intraoperative monitoring24.
CONCLUSIONS
Taken as a whole, the available data appear to indicate
that propofol, has the potential of offering a certain
degree of neuroprotection, which is not exclusively due
to reduction of the CMRO2 but involves inhibition and/
or modulation of specific cellular pathways activated
following acute brain injury. At present, however, there
are no clinical data available to indicate that propofol
may have neuroresuscitative properties, as it occurs with
other anesthetic agents with the possible exception of
xenon25. It is probably quite nave to imagine that a single
anesthetic, given for a limited amount of time, might
offer long lasting protection against cerebral injuries for
which an evolution over days and months after the
primary insult occurs. However, propofol may share a
useful role with other anesthetics in the prevention of
intraoperative ischemic insults, which tend to be less
severe than spontaneous strokes. Undoubtedly, propofol
offers advantages during neurosurgery in which
intracranial hypertension is a menace, in that it allows
the surgeon to operate under safe and optimal conditions.
REFERENCES
1.
Kawaguchi M, Furuya H, Patel PM. Neuroprotective effects
of anesthetic agents.
J Anesth 2005; 19:1506.
2.
Koerner IP, Brambrink AM. Brain protection by anesthetic
agents.
Curr Opin Anaesthesiol 2006; 19:4816.
3.
James R, Glen JB. Synthesis, biological evaluation, and
preliminary structure-activity considerations of a series of
alkylphenols as intravenous anesthetic agents.
J Med Chem 1980; 23:13507.
4.
Kay B, Rolly G. I.C.I. 35868, a new intravenous induction
agent.
Acta Anaesthesiol Belg 1977; 28:3036.
5.
Borgeat A, Wilder-Smith O, Forni M, Suter PM. Adjuvant
propofol enables better control of nausea and emesis secondary
to chemotherapy for breast cancer.
Can J Anaesth 1994; 41:11179.
6.
Orser BA,Wang LY, Pennefather PS, MacDonald JF. Propofol
modulates activation and desensitization of GABAA receptors
in cultured murine hippocampal neurons.
J Neurosci 1994; 14:774760.
7.
Ratnakumari L, Hemmings HC, Jr. Effects of propofol on
sodium channel-dependent sodium influx and glutamate release
in rat cerebrocortical synaptosomes.
Anesthesiology 1997; 86:42839.
8.
Mortero RF, Clark LD, Tolan MM, Metz RJ, Tsueda K,
Sheppard RA. The effects of small-dose ketamine on propofol
sedation: Respiration, postoperative mood, perception,
cognition, and pain.
Anesth Analg 200; 92:14659.
9.
Patel P. No magic bullets: the ephemeral nature of anestheticmediated neuroprotection.
Anesthesiology 2004; 100:104951.
10. Kanto J, Gepts E. Pharmacokinetic implications for the clinical
use of propofol.
Clin Pharmacokinet 1989; 17:30826.
11. Bryson HM, Fulton BR, Faulds D. Propofol. An update of its
use in anaesthesia and conscious sedation.
Drugs 1995; 50:51359.
12. Wysowski DK, Pollock ML. Reports of death with use of
propofol (Diprivan) for nonprocedural (long-term) sedation
and literature review.
Anesthesiology 2006; 105:104751.
13. Ishii H, Arai T, Segawa H, Morikawa S, Inubushi T, Fukuda
K. Effects of propofol on lactate accumulation and oedema
formation in focal cerebral ischaemia in hyperglycaemic rats.
Br J Anaesth 2002; 88:4127.
14. Adembri C,Venturi L, Tani A, et al. Neuroprotective effects
of propofol in models of cerebral ischemia: Inhibition of
Indian Journal of Neurotrauma (IJNT), Vol. 5, No. 1, 2008
44
TVSP Murthy
mitochondrial swelling as a possible mechanism.
Anesthesiology 2006; 104:809.
15. Todd MM, Warner DS. A comfortable hypothesis reevaluated.
Cerebral metabolic depression and brain protection during
ischemia.
Anesthesiology 1992; 76:1614.
16. Nicol B, Rowbotham DJ, Lambert DG. Glutamate uptake is
not a major target site for anaesthetic agents.
Br J Anaesth 1995; 75:615.
17. Sitar SM, Hanifi-Moghaddam P, Gelb A, Cechetto DF,
Siushansian R, Wilson JX. Propofol prevents peroxide-induced
inhibition of glutamate transport in cultured astrocytes.
Anesthesiology 1999; 90:144653.
18. Velly LJ, Guillet BA, Masmejean FM, et al.. Neuroprotective
effects of propofol in a model of ischemic cortical cell cultures:
Role of glutamate and its transporters.
Anesthesiology 2003; 99:36875.
19. Williams DB, Akabas MH. Structural evidence that propofol
stabilizes different GABAA receptor states at potentiating and
activating concentrations.
J Neurosci 2002; 22:741724.
Indian Journal of Neurotrauma (IJNT), Vol. 5, No. 1, 2008
20. Mattson MP, Kroemer G. Mitochondria in cell death: novel
targets for neuroprotection and cardioprotection.
Trends Mol Med 2003; 9:196205.
21. Van Der Stelt M, Di Marzo, V. Cannabinoid receptors and
their role in neuroprotection.
Neuromol Med 2005; 7:3750.
22. Fox J, Gelb AW, Enns J, Murkin JM, Farrar JK, Manninen
PH. The responsiveness of cerebral blood flow to changes in
arterial carbon dioxide is maintained during propofol-nitrous
oxide anesthesia in humans.
Anesthesiology 1992; 77:4536.
23. Walder B, Tramer MR, Seeck M. Seizure-like phenomena
and propofol: A systematic review.
Neurology 2002; 58:132732.
24. Gupta A, Stierer T, Zuckerman R, Sakima N, Parker SD,
Fleisher LA. Comparison of recovery profile after ambulatory
anesthesia with propofol, isoflurane, sevoflurane and desflurane:
A systematic review.
Anesth Analg 2004; 98:63241.
25. Preckel B,Weber NC, Sanders RD, Maze M, SchlackW.
Molecular mechanisms transducing the anesthetic, analgesic,
and organ-protective actions of xenon.
Anesthesiology 2006; 105:18797.
También podría gustarte
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- Propofol in NeurotraumaDocumento4 páginasPropofol in NeurotraumaPekerja KesunyianAún no hay calificaciones
- Gcs CommentsDocumento6 páginasGcs CommentsTobyjohn Diapo GemoraAún no hay calificaciones
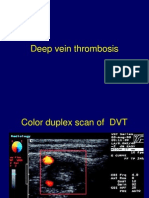
- 2 Deep Vein ThrombosisDocumento10 páginas2 Deep Vein ThrombosisLulu SupergirlAún no hay calificaciones
- Js 09036Documento5 páginasJs 09036Pekerja KesunyianAún no hay calificaciones
- Paul Ridolfi Upper-GIDocumento17 páginasPaul Ridolfi Upper-GIPekerja KesunyianAún no hay calificaciones
- Ccrs 21005Documento12 páginasCcrs 21005Pekerja KesunyianAún no hay calificaciones
- AspergillosisDocumento34 páginasAspergillosisvilla88Aún no hay calificaciones
- A Ann Lumbar SpineDocumento44 páginasA Ann Lumbar SpineAyu SartikaAún no hay calificaciones
- Ccpc13 20 Att2 CRC Slides ProvidersDocumento44 páginasCcpc13 20 Att2 CRC Slides ProvidersPekerja KesunyianAún no hay calificaciones
- 7 - Examination of The AbdomenDocumento48 páginas7 - Examination of The AbdomenPekerja KesunyianAún no hay calificaciones
- Ijav 2012 011-013Documento3 páginasIjav 2012 011-013Pekerja KesunyianAún no hay calificaciones
- Inflammation of the Peritoneal MembraneDocumento16 páginasInflammation of the Peritoneal MembranePekerja KesunyianAún no hay calificaciones
- Ccrs 21031Documento10 páginasCcrs 21031Pekerja KesunyianAún no hay calificaciones
- Ccrs 21023Documento8 páginasCcrs 21023Pekerja KesunyianAún no hay calificaciones
- 105 365 368Documento4 páginas105 365 368Pekerja KesunyianAún no hay calificaciones
- 95 97Documento3 páginas95 97Pekerja KesunyianAún no hay calificaciones
- Ijav 2012 011-013Documento3 páginasIjav 2012 011-013Pekerja KesunyianAún no hay calificaciones
- f167101a-b37b-4feb-b647-3ef5435d02cbDocumento5 páginasf167101a-b37b-4feb-b647-3ef5435d02cbPekerja KesunyianAún no hay calificaciones
- Js 09036Documento5 páginasJs 09036Pekerja KesunyianAún no hay calificaciones
- Daftar PustakaDocumento1 páginaDaftar PustakaPekerja KesunyianAún no hay calificaciones
- 4 - Gangguan - BrainDocumento36 páginas4 - Gangguan - BrainPekerja KesunyianAún no hay calificaciones
- Bone Regenerations - Current Concept and Future DirectionDocumento10 páginasBone Regenerations - Current Concept and Future DirectionPekerja KesunyianAún no hay calificaciones
- Gangguan Pernafasan: Bagian Anestesiologi Dan Reanimasi FK Unsyiah - Rsuza Banda AcehDocumento20 páginasGangguan Pernafasan: Bagian Anestesiologi Dan Reanimasi FK Unsyiah - Rsuza Banda AcehPekerja KesunyianAún no hay calificaciones
- Fracture Healing SsDocumento2 páginasFracture Healing SsIndra SyafaatAún no hay calificaciones
- Gangguan Sirkulasi: Bagian Anestesiologi Dan Reanimasi FK Unsyiah - RSUZA Banda AcehDocumento35 páginasGangguan Sirkulasi: Bagian Anestesiologi Dan Reanimasi FK Unsyiah - RSUZA Banda AcehPekerja KesunyianAún no hay calificaciones
- GmreadmeDocumento1 páginaGmreadmeAccap Aninam DimaraAún no hay calificaciones
- Fracture Healing - The Diamond ConceptDocumento4 páginasFracture Healing - The Diamond ConceptPekerja KesunyianAún no hay calificaciones
- Peritonitis and Intra-Abdominal Abscess Diagnosis TreatmentDocumento16 páginasPeritonitis and Intra-Abdominal Abscess Diagnosis TreatmentPekerja KesunyianAún no hay calificaciones
- 865Documento7 páginas865Pekerja KesunyianAún no hay calificaciones
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- AP PSYCHOLOGY EXAM REVIEW SHEETDocumento6 páginasAP PSYCHOLOGY EXAM REVIEW SHEETNathan HudsonAún no hay calificaciones
- Fruit and Vegetable Diseases PDFDocumento563 páginasFruit and Vegetable Diseases PDFgrigorasalexandru100% (1)
- 10th BIOLOGY PPT CH. NO. 8Documento13 páginas10th BIOLOGY PPT CH. NO. 8Aastha BorhadeAún no hay calificaciones
- Altitude PhysiologyDocumento41 páginasAltitude Physiologyshepherd jeremiahAún no hay calificaciones
- Chapter 4Documento7 páginasChapter 4R LashAún no hay calificaciones
- The Integumentary SystemDocumento11 páginasThe Integumentary SystemHamdy Pagilit DimaporoAún no hay calificaciones
- Blood Buffer SystemDocumento10 páginasBlood Buffer Systemmd hasib munsiAún no hay calificaciones
- Bulacan State University College of Nursing Final Exam ReviewDocumento7 páginasBulacan State University College of Nursing Final Exam ReviewDemiar Madlansacay QuintoAún no hay calificaciones
- NIOSH Investigation - CR 337 Fire LODDDocumento32 páginasNIOSH Investigation - CR 337 Fire LODDRamblingChiefAún no hay calificaciones
- B CellDocumento10 páginasB CellSonia Elizabeth SimonAún no hay calificaciones
- 201305283en Capsurefix 5076Documento2 páginas201305283en Capsurefix 5076Bian PurwaAún no hay calificaciones
- B2 Revision PIXLDocumento26 páginasB2 Revision PIXLtunmishetobilawalAún no hay calificaciones
- Science: Quarter 1 - Module 1Documento10 páginasScience: Quarter 1 - Module 1RUTH PIANGAún no hay calificaciones
- Chapter 6 Cell DivisionDocumento20 páginasChapter 6 Cell DivisionVinash Shka RaoAún no hay calificaciones
- Zoology: Zoology Previous Eamcet QuestionsDocumento8 páginasZoology: Zoology Previous Eamcet QuestionsGaganpreetSingh100% (1)
- UntitledDocumento89 páginasUntitledVladimir VešovićAún no hay calificaciones
- A New Furileusaurian Abelisaurid From La Invernada Upper Cretaceous Santonian Bajo de La Carpa Formation Northern Patagonia ArgentinaDocumento29 páginasA New Furileusaurian Abelisaurid From La Invernada Upper Cretaceous Santonian Bajo de La Carpa Formation Northern Patagonia ArgentinaStuff NewsroomAún no hay calificaciones
- Essential Ayurveda BookDocumento196 páginasEssential Ayurveda BookRoberto89% (9)
- C5 - Metabolism and Enzyme Part 1Documento20 páginasC5 - Metabolism and Enzyme Part 1Daniel LohAún no hay calificaciones
- Phylum Arthropoda - Why such abundance and diversityDocumento4 páginasPhylum Arthropoda - Why such abundance and diversitySHILAún no hay calificaciones
- Overview of Complications Occurring in The Post-Anesthesia Care UnitDocumento14 páginasOverview of Complications Occurring in The Post-Anesthesia Care UnitShahabuddin ShaikhAún no hay calificaciones
- ICSE Class 10 Biology Previous Year Question Paper 2011 PDFDocumento9 páginasICSE Class 10 Biology Previous Year Question Paper 2011 PDFmohammedAún no hay calificaciones
- The Management of Intra Abdominal Infections From A Global Perspective 2017 WSES Guidelines For Management of Intra Abdominal InfectionsDocumento34 páginasThe Management of Intra Abdominal Infections From A Global Perspective 2017 WSES Guidelines For Management of Intra Abdominal InfectionsJuan CastroAún no hay calificaciones
- Excretory System QuizDocumento17 páginasExcretory System QuizShadab HanafiAún no hay calificaciones
- Auxin Controls Seed Dormacy in Arabidopsis (Liu, Et Al.)Documento6 páginasAuxin Controls Seed Dormacy in Arabidopsis (Liu, Et Al.)Jet Lee OlimberioAún no hay calificaciones
- Wound CareDocumento14 páginasWound CareKirsten Padilla Chua100% (4)
- The Science of Laughing - Worksheet 3Documento3 páginasThe Science of Laughing - Worksheet 3Maria Alexandra PoloAún no hay calificaciones
- He History of ArticulatorsDocumento13 páginasHe History of ArticulatorsrekabiAún no hay calificaciones
- Nicotrol InhalerDocumento19 páginasNicotrol InhalerdebysiskaAún no hay calificaciones
- Circulatory System: Heart, Blood Vessels & Their FunctionsDocumento17 páginasCirculatory System: Heart, Blood Vessels & Their FunctionskangaanushkaAún no hay calificaciones