Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Zinc Supplementation Improve Dietary Intake
Cargado por
akochaDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Zinc Supplementation Improve Dietary Intake
Cargado por
akochaCopyright:
Formatos disponibles
Does Zinc Supplementation Improve
Dietary Intake, Symptoms of Eating
Problems, and Serum Zinc Levels in
Hemodialysis Patients?
Jamal Ghaemmaghami, MSc; Reza Mahdavi, PhD; Elnaz Faramarzi, PhD; Noshin Mohammadpour, MSc; Hassan Argani, MD
Drs. Mahdavi and Argani are with the Drug Applied Research Center, and Drs. Ghaemmaghami, Faramarzi and
N. Mohammadpour are with the Nutritional Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
Dr. Argani is also with the Division of Renal Transplant, Modarres Hospital, Shahid Beheshti University of Medical
Sciences, Tabriz, Iran.
OBJECTIVE: The objectives of this study were to determine the effects of zinc supplementation on dietary intake,
symptoms of eating problems, and serum zinc levels in hemodialysis patients.
METHODS: Thirty-nine patients who received chronic maintenance hemodialysis were randomized to experimental
(n 21) and placebo (n 18) groups given a daily supplement of 100 mg elemental zinc and corn starch, respectively, for 60 days. Dietary intake, body composition, and eating problems were assessed using 2-day dietary
records, bioelectric impedance tests, and a questionnaire, respectively. Serum zinc levels were determined by
atomic absorption before and after intervention.
RESULTS: The mean daily macro- and micronutrients intakes and percentage of body fat in the supplemented
group increased insignificantly. Administration of zinc improved appetite loss, dry mouth, nausea, and hypogeusia,
while incidence of these symptoms increased in control group. A significant increase (p 0.01) was observed in
the mean serum zinc levels in the experimental group (102 4 vs. 76 3 g/dL) while changes in the placebo
group were not significant.
CONCLUSIONS: Despite observed improvement in symptoms of eating problems and serum zinc levels in the
supplemented group, more study over a longer period must be carried out to achieve clearer results.
rotein-energy malnutrition (PEM)
is a comorbid condition and risk
factor for increased morbidity and
mortality in maintenance dialysis
patients. The prevalence of PEM in the
hemodialysis (HD) population varies from
25% to 70%.1-3 Numerous studies have
observed a positive relationship between
PEM and increased risk of morbidity and
mortality and low quality of life in this population.4-7 The pathogenesis of PEM among
these patients is multifactorial. Inadequate
nutrient intake, dialysis-related nutrient
losses, alterations in protein metabolism,
acidosis, and inflammation are considered
to be the major causes of PEM.8,9
In addition to PEM, other nutritional
abnormalities are frequently observed in
HD patients. These abnormalities may
include decreases in dietary intake and
dry body weight.3,4,7 Deficiencies of vita530 Dialysis & Transplantation December 2010
mins, minerals, and certain trace minerals
(particularly zinc) are also observed in the
malnourished HD patient.3,4
It is well known that trace element
disturbances can be a result of uremia, and
trace element metabolism can be affected
by reduced renal function, alteration of the
metabolic balance, special diet, medications, and dialysis treatment in renal insufficiency. Various trace element abnormalities in long-term HD patients have been
reported.10-12 Among the trace elements,
zinc (the second most abundant trace element in humans) is unique. Zinc plays three
well-known physiological rolescatalytic,
structural, and regulatory. Symptoms of zinc
deficiency are anorexia, impaired smell and
taste, growth retardation, hypogonadism,
skin lesions, and decreased cell-mediated
immunity.13,14 Some reports have indicated
that dysgeusia and poor food intake, which
are common problems of uremic patients,
may be improved by giving patients zinc
supplements.15 However, other studies have
not confirmed this.15 Controversy remains
in the literature as to the effects of zinc
deficiency on uremic patients undergoing
maintenance HD. Therefore, further studies
are needed to explore this issue.
Because of the low serum zinc concentrations in HD patients and the important
roles of zinc in the body,16 we evaluated the
effects of zinc supplementation on dietary
intake, eating problems, and serum zinc
levels in HD patients.
Patients and Methods
This prospective, double-blind study was
approved by the Ethics Committee of
Tabriz University of Medical Sciences. In
total, 45 patients undergoing HD in the
DOI: 10.1002/dat.20493
Hemodialysis Department of Sina Hospital
in Tabriz agreed to participate in the 60day study. Six patients did not complete
the study for reasons that included poor
compliance with study protocols, gastrointestinal disturbances, and/or death.
Thirty-nine patients (24 men and 15
women) completed the study. The 21 patients
in the supplemented group (8 women and 13
men; mean age 58 6 years) had been
receiving regular HD for 37 9 months.
The 18 patients in the control group (7
women and 11 men; mean age 52 4 years)
had been receiving regular HD for 49 11
months. The frequency of the therapy was
three times a week, with 4 hours of dialysis
per session. Selection criteria of patients to
participate in the study included: on HD
treatment for a minimum of 6 months, no
signs of gastrointestinal disorders, and not a
candidate for transplantation.
Patients were randomly selected to
receive two capsules each day containing either 220 mg zinc sulfate (100 mg
elemental zinc) or a cornstarch placebo,
to be taken without food or other medications, for 60 days. Height was measured
using a mounted tape with the patients
arm hanging freely at the side and was
recorded to the nearest 0.5 cm. Body
weight was measured barefoot and with
light clothing to the nearest 0.1 kg with
a Seca (Hanover, MD) scale. Body composition (total body water, free fat mass,
and body fat) was determined by means of
body impedance analysis (BIA; Human IM
Plus, DS Dietosystem, Milan, Italy) at day
0 and day 60.
Patients were instructed to keep 2day food records, including 1 dialysis
day and 1 non-dialysis day, at day 0 and
day 60 of the study. Both verbal and
written instructions were provided. The
records were analyzed by Nutritionist III
for Windows software (Axxya Systems,
Stafford, Texas). Information regarding
dietary intake of calories, total carbohydrate, total protein, total fat, and zinc was
obtained from the analysis.
Appetite, taste changes, nausea, and
dry mouth was assessed by questionnaire.
The questionnaire was completed before
and after HD at day 0 and day 60. Before
the questionnaire was administered, a reliability analysis was performed to determine
the extent to which items in the questionnaire were related to each other. The scale
of reliability was estimated with Cronbachs
alpha coefficient. The Cronbachs alpha reliability coefficient was 0.679, which showed
that the items were highly correlated.
Pre-dialysis blood samples for biochemical parameters were collected after
an overnight fast (12 hours) in tubes at the
onset of the study (day 0) and on day 60.
The samples were centrifuged at
2,000g for 15 minutes, and off-the-clot
serum samples without hemolysis were
removed with a micropipette. The serum
samples were kept at 32C until biochemical determinations.
Serum zinc levels were determined
by an atomic absorption spectrophotometer against standard references.17 Serum
albumin was measured by the colorimetric
method.18
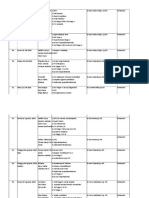
TABLE I. Mean SEM of body weight, body mass index (BMI),
body composition, and serum zinc and albumin levels at the onset
and end of study.
Zinc-Supplemented Group (n 21)
Control Group (n 18)
Before
After
Before
60 1.5
60 2.6
60 7
BMI
22 2.3
22 2.9
22 1.6 21.9 2
Total body water (%)
62 4
59 5
64 3
Body weight (kg)
After
59.5 5.5
60 1
Dry body weight (%)
38 7
41 4
36 2
40 3
Free fat mass (%)
78 1
77 2
79 1
78 1
Body fat (%)
21 1
22 1
21 4
21 4
Serum zinc (g/dL)
76 3
102 4*
77 4
80 6
Albumin (g/dL)
3.4 0.10
3.93 0.15*
* p 0.05 in comparison with before intervention, by paired t-test.
3.37 0.4 3.33 0.47
Statistical Analysis
Descriptive statistics were obtained for
all study variables for each study group.
McNemars test was used to compare
eating problems such as dry mouth and
loss of appetite before and after intervention. The differences among dietary intake,
anthropometric data, and serum zinc and
albumin concentrations before and after
intervention were compared by a paired
t-test. A p-value of 0.05 was considered
statistically significant.
Results
Thirty-nine participants completed the
study. There was no significant difference
in dietary intake (macronutrients and zinc
intakes) and body weight between the control and experimental groups at the beginning of the study.
Mean body weight, body mass index
(BMI), and body composition of patients
at the onset and the end of study are presented in Table I. As shown in the table,
in the zinc-supplemented group, the mean
body weight and BMI of patients did not
change before and after intervention. The
mean total body water and free fat mass
of patients in both groups had decreased
insignificantly at the end of study.
The means SEM of energy, macronutrients, and zinc intakes before and after
intervention in both groups are shown in
Table II. The mean energy intake in the
supplemented group increased from 1,709
120 kcal at the beginning of the study
to 1,875 112 kcal at the end of the
study, but the differences was not statistically significant. In the placebo group, the
mean energy intake decreased insignificantly from 1,706 105 kcal to 1,585
164 kcal. In the supplemented group, the
mean carbohydrate intake was significantly
(p 0.05) increased (about 35 g).
Changes in eating problems before
and after intervention are shown in
Table III. In the experimental group, eating
problems such as appetite loss, dry mouth,
nausea, and hypogeusia significantly
(p 0.05) decreased after intervention,
while these symptoms had increased in the
control group at the end of the study.
The means SEM of serum zinc and
albumin levels in the zinc-supplemented
December 2010 Dialysis & Transplantation 531
Zinc Supplementation in HD Patients
TABLE II. Mean SEM of energy, macronutrients, and zinc intakes
before and after intervention in both zinc-supplemented and placebo
groups.
Zinc-Supplemented Group (n 21)
Before
After
Placebo Group (n 18)
Before
After
1,709 120
1,875 112
Total protein (g)
56 6
57 9
54 5
50 8
High biological value
(HBV) protein (g)
25 3
27 1
26 1
23 3
Energy (kcal)
Total fat (g)
Total carbohydrate (g)
1,706 105 1,585 164
52 2
57 4
54 6
44 8
249 8
284 10*
251 14
247 11
42
31
31
31
Zinc (mg)
* p 0.05 in comparison with before intervention, paired t-test.
TABLE III. Comparison of eating problems before and after zinc
supplementation.
Eating problem
Zinc-Supplemented Group (n 21)
Control Group (n 18)
Before
After
Before
After
14.1
0*
5.6
22.2*
Dry mouth (%)
52
9.5*
33
44
Hypogeusia (%)
23.8
0*
39
39
57
28.6*
39
55.6
Appetite loss (%)
Nausea (%)
* p < 0.05 in comparison with before intervention, McNemars test.
and control groups are shown in Table I.
The initial mean serum zinc concentrations
in both the control group (77 4 g/dL)
and the zinc-supplemented experimental
group (76 3 g/dL) were in the lower
limit of the normal range (70-110 g/dL).19
At the end of the intervention, the mean
zinc concentrations in the supplemented
group had increased from 76 3 g/dL
to 102 4 g/dL, which was statistically
significant (p 0.05). At the onset of the
study in both groups, the mean serum
albumin levels were lower than the normal
range (3.5-5.2 g/dL).18 In the experimental
group, the mean serum albumin increased
significantly (p 0.05) compared with the
pre-treatment level (3.93 0.15 vs. 3.4
0.10 g/dL).
Discussion
The prevalence of malnutrition in patients on
HD is high (15-89%); the average is about
40%, and malnutrition in HD patients is a
significant predictor of mortality.20-22 Many
factors such as inadequate diet, anorexia,
abnormalities of taste, gastrointestinal prob532 Dialysis & Transplantation December 2010
lems, inflammation, and medications contribute to the PEM found in HD patients.23-25
After the intervention, in the zincsupplemented group the daily mean energy,
carbohydrate, protein, fat, and zinc intakes
had increased, but only the mean carbohydrate intake was increased significantly.
The results of previous studies showed
significant increases in energy and protein
intake after zinc supplementation.26-28 The
observed insignificant increase in dietary
intakes of these patients may be due to
the duration of the study (60 vs. 90 days).
Food records may affect patient dietary
intake,29 but in the present study intake
did not change significantly. Therefore we
assumed that food records did not cause a
bias in the eating habits of study participants.
In comparison with the control group,
the incidence of eating problems such as
dry mouth, loss of appetite, nausea, and
hypogeusia in the mouth was significantly
reduced after zinc supplementation. Several
studies have suggested that taste perception is abnormal in HD patients.27,30-33 One
proposed mechanism for the taste distur-
bance is zinc deficiency.26 Mahajan et al.32
observed improvement in taste acuity after
zinc supplementation, and Atkin-Thor et
al.27 observed improvement in taste acuity,
as well as an increase in energy and protein
intake when increased dietary zinc was
provided. The results of the present study
are consistent with those previous studies, which showed improvement in taste
perception after zinc supplementation.27,32
In the supplemented group, hypogeusia
improved after supplementation even when
zinc concentrations were within normal
ranges in serum. In a double-blind, placebo-controlled study, Yoshida et al.34 reported a therapeutic effect of zinc gluconate in
patients with idiopathic taste disorder and
normal serum zinc levels.
Mean body weights did not change
significantly for either group of patients,
which was in agreement with Chevalier et
al.28 and Mungua et al.,35 who reported
that dry body weight of HD patients did
not change after zinc supplementation.
After supplementation, serum zinc levels
increased from 76 3 to 102 4 g/dL
(within normal ranges). Our results are
compatible with those of Mungua et al.34
and Rashidi et al.,36 who showed that HD
patients with below-normal zinc concentrations had significant improvement in zinc
levels after supplementation.
At the onset of the study, the mean
serum albumin concentrations were lower
than the normal range (3.5-5.2 g/dL)
in both groups.18 Zinc supplementation
increased the mean serum albumin levels
in the supplemented group; the mean serum
albumin concentrations did not change in
control group.
Hypoalbuminemia occurs in a large
number of patients with end-stage renal
disease on chronic HD, and it is highly
associated with increased mortality risk
in this population.37 Possible causes of
hypoalbuminemia in these patients are
insufficient protein and calorie intakes, or
a discrete acute-phase response resulting
decreased in albumin synthesis by the liver
in favor of acute-phase protein.38 However,
albumin levels remain virtually unchanged
even in the presence of severe protein
calorie malnutrition in healthy individuals
until near terminal starvation.39 Thus low
albumin levels suggest that a more complex
etiology other than reduced protein intake
alone may contribute to hypoalbuminemia .
In this study, the dietary intake of the supplemented group did not change remarkably, so the increased levels of serum
albumin may be due to improvement of
antioxidant status and inflammation conditions in HD patients (data not shown) after
zinc supplementation.
The results of this study indicate that
symptoms of eating problem in HD patients
are positively influenced by zinc supplementation. In previous studies, it has been
suggested that zinc deficiency is a predominant factor underlying eating problems, especially hypogeusia, even when
zinc concentration are within normal ranges
in the serum. However, it may be prudent
to obtain a baseline measurement of serum
zinc concentrations in HD patients for monitoring abnormal values. We also suggest
that it would be worthwhile determining the
effects of zinc supplementation on other biochemical indicators that are more sensitive
to marginal zinc deficiency and that further
studies are needed with longer period of
supplementation to achieve clearer results.
Disclosures
Financial support from the Drug Applied
Research Center of Tabriz University of
Medical Sciences is gratefully acknowledged. D&T
References
1. Ikizler TA, Hakim R. Nutrition in end-stage renal
disease. Kidney Int. 1996;50:343-357.
2. Marcen R, Teruel JL, de la Cal MA, Gmez C. The
impact of malnutrition in morbidity and mortality in
stable haemodialysis patients. Nephrol Dial Transplant. 1997;12:2324-2331.
3. National Kidney Foundation: K/DOQI Clinical Practice Guidelines for Nutrition in Chronic Renal Failure. Am J Kidney Dis. 2000;35:S1-S104.
4. Kopple JD. Nutritional status as a predictor of
morbidity and mortality in maintenance dialysis
patients. ASIAO J. 1997;43:246-250.
5. Leavy SF, Strawderman RL, Jones CA, et al. Simple
nutritional indicators as independent predictors of
mortality in hemodialysis patients. Am J Kidney Dis.
1998;31:997-1006.
6. Goldstein DJ, Callahan C. Strategies for nutritional
intervention in patients with renal failure. Miner Electrolyte Metab. 1998;24:82-91.
23. Ahuja T, Mitch W. The evidence against malnutrition as a prominent problem for chronic dialysis
patients. Semin Dial. 2004;17:427-431.
7. Dwyer J, Larive B, Leung J, et al. Nutritional status
affects quality of life in hemodialysis (HEMO) study
patients at baseline. J Renal Nutr. 2002;12:213223.
24. Kalantar-Zadeh K, Block G, McAllister J, et al.
Appetite and inflammation, nutrition, anemia, and
clinical outcome in hemodialysis patients. Am J
Clin Nutr. 2004;80:299-307.
8. Locatelli F, Fouque D, Heimburger O, et al.
Nutritional status in dialysis patients: a
European consensus. Nephrol Dial Transplant.
2002;17:563-572.
25. Owen WF. Nutritional status and survival in endstage renal disease patients. Miner Electrolyte
Metab. 1998;24:72-81.
9. Bossola M, Muscaritoli M, Tazza L, et al. Malnutrition in hemodialysis patients: what therapy? Am J
Kidney Dis. 2005;46:371-386.
10. Tonelli M, Wiebe N, Hemmelgarn B, et al. Trace
elements in hemodialysis patients: a systematic review and meta-analysis. BMC Med.
2009;7:25.
11. Bogden JD, Oleske JM, Weiner B, et al. Elevated
plasma zinc concentrations in renal dialysis
patients. Am J Clin Nutr. 1980;33:1088-1095.
12. Navarro-Alarcon M, Reyes-Perez A, Lopez-Garcia
H, et al. Longitudinal study of serum zinc and
copper levels in hemodialysis patients and their
relation to biochemical markers. Biol Trace Elem
Res. 2006;113:209-222.
13. McCall KA, Huang C, Fierke CA. Function and mechanism of zinc metalloenzymes. J Nutr. 2000;130:
S1437-S1446.
14. Ibs KH , Rink L. Zinc-altered immune function. J
Nutr. 2003;133:S1452-S1456.
15. Kopple JD . Nutrition, diet and the kidney. In: Shils
ME, Shike M, Ross CA, Caballero B, Cousin SRJ,
eds. Modern Nutrition in Health and Disease.10th
ed. Philadelphia, PA: Lippincott Williams & Wilkins;
2006:1497.
16. Reilly C. The Nutritional Trace Metals. Boston, MA:
Blackwell; 2004:87.
17. Shenkin A, Baines M, Fell GS, Lyon TDG. Vitamins
and trace elements. In: Burtis CA, Ashwood ER,
Bruns DE, eds. Tietz Text Book of Clinical Chemistry and Molecular Diagnostics. 4th ed. Philadelphia, PA: WB Saunders; 2006:1121.
18. Johnson AM, Rohlfs EM, Silverman LM. Proteins.
In: Burtis CA, Ashwood ER, Bruns DE, eds. Tietz
Text Book of Clinical Chemistry and Molecular Diagnostics. 4th ed. Philadelphia, PA: WB Saunders;
2006:545-548.
19. Hargunow SA. Trace elements. In: Bishop ML,
Duben-Engelkirk JL, Fody EP, eds. Clinical Chemistry: Principles, Procedures, Correlations. 4th ed.
Philadelphia, PA: Lippincott Williams & Wilkins;
2000:323.
20. Owen WF, Lew NL, Yan Liu SM, et al. The urea
reduction ratio and serum albumin as predictors
of mortality inpatients undergoing hemodialysis.
N Engl J Med. 1993;329:1101-1106.
21. Qureshi AR, Alvestrand A, Danielsson A, et al.
Factors predicting malnutrition in hemodialysis
patients: a cross-sectional study. Kidney Int.
1998;53:773-782.
22. Collins AJ, Ma JZ, Umen A, Keshaviah P. Urea index
and other predictors of hemodialysis patient survival. Am J Kidney Dis. 1994;23:272-282.
26. Mahajan SK, Prasad AS, Rabbani P, et al. Zinc
deficiency: a reversible complication of uremia.
Am J Clin Nutr.1982;36:1177-1183.
27. Atkin-Thor E, Goddard BW, ONion J, et al. Hypogeusia and zinc depletion in chronic dialysis patients.
Am J Clin Nutr. 1978;31:1948-1951.
28. Chevalier CA, Liepa G, Murphy MD, et al. The
effects of zinc supplementation on serum zinc
and cholesterol concentrations in hemodialysis
patients. J Renal Nutr. 2002;12:183-189.
29. Freudehheim JL. A review of study designs and
methods of dietary assessment in nutritional epidemiology of chronic disease. J Nutr. 1993;123:401405
30. Vreman HJ, Venter C, Leegwater J, et al. Taste,
smell and zinc metabolism in patients with chronic
renal failure. Nephron.1980;26:163-170.
31. Fernstrom A, Hylander B, Rossner S. Taste acuity
in patients with chronic renal failure. Clin Nephrol.
1996;45:169-174.
32. Mahajan SK, Prasad AS, Lambujon J, et al. Improvement of uraemic hypogeusia by zinc: a double blind
study. Am J Clin Nutr. 1980;33:1517-1521.
33. Sprenger KBG, Bundschu D, Lewis K. Improvement of uraemic neuropathy and hypogeusia by
dialysate zinc supplementation: a double blind
study. Kidney Int. 1983;24:S315S318.
34. Yoshida S, Endo S, Tomita HA.A double-blind study
of the therapeutic efficacy of zinc gluconate on the
taste disorder. Auris Nasus Larynx.1991;18:153161.
35. Mungua C, Paniagua R, Avila-Daz M, et al. Effect
of zinc supplements on the nutritional status of
patients undergoing continuous ambulatory peritoneal dialysis. Rev Invest Clin. 2003;55:519-527
[Abstract].
36. Rashidi, AA, Salehi M, Piroozmand A, et al. Effects
of zinc supplementation on serum zinc and Creactive protein concentrations in hemodialysis
patients. J Renal Nutr. 2009;19:475-478.
37. Lowrie EG, Lew NL. Death risk in hemodialysis patients: the predictive value of commonly
measured variables and an evaluation of death
rate differences between facilities. Am J Kidney
Dis.1990;15:458-482.
38. Gali G, Tomi M, Gale K, et al. Hypoalbuminemia
and complication incidence in hemodialysed
uremic patients. Coll Antropol. 2009;33:559566.
39. Rigaud D, Hassid J, Meulemans A, et al. A paradoxical increase in resting energy expenditure in
malnourished patient near death: the king penguin syndrome. Am J Clin Nutr. 2000;72:355360.
December 2010 Dialysis & Transplantation 533
También podría gustarte
- Charity and Giving in Monotheistic ReligionDocumento431 páginasCharity and Giving in Monotheistic Religionakocha100% (1)
- Charity and Giving in Monotheistic ReligionDocumento431 páginasCharity and Giving in Monotheistic Religionakocha100% (1)
- Herrick and Heart DiseaseDocumento2 páginasHerrick and Heart DiseaseakochaAún no hay calificaciones
- Chad ScoreDocumento5 páginasChad ScoreakochaAún no hay calificaciones
- Bladder CancerDocumento18 páginasBladder CancerakochaAún no hay calificaciones
- ECG Reporting: The AtriaDocumento5 páginasECG Reporting: The AtriaakochaAún no hay calificaciones
- Torrent File - Wikipedia, The Free EncyclopediaDocumento5 páginasTorrent File - Wikipedia, The Free EncyclopediaakochaAún no hay calificaciones
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Acute Renal FailureDocumento12 páginasAcute Renal FailureElsa SimangunsongAún no hay calificaciones
- 2 UrinarySystemDocumento83 páginas2 UrinarySystemLemuel Lagasca Razalan IVAún no hay calificaciones
- Annisya Handini 1Documento15 páginasAnnisya Handini 1Hafidh Alyza RAún no hay calificaciones
- Effects of Lactulose and Neomycin On Urea Metabolism in Cirrhotic SubjectsDocumento5 páginasEffects of Lactulose and Neomycin On Urea Metabolism in Cirrhotic Subjectsnova adiAún no hay calificaciones
- 5.nervous System PDFDocumento88 páginas5.nervous System PDFMelancholy MedicineAún no hay calificaciones
- CRF TextbookDocumento5 páginasCRF TextbookThirdie LacorteAún no hay calificaciones
- Renal NursingDocumento11 páginasRenal NursingFreeNursingNotes100% (10)
- Chronic Kidney DiseaseDocumento41 páginasChronic Kidney DiseaseveraveroAún no hay calificaciones
- 240809-Data Penelitian Dan Publikasi IPDS Di IndonesiaDocumento22 páginas240809-Data Penelitian Dan Publikasi IPDS Di IndonesiaHasbiallah YusufAún no hay calificaciones
- Nursing Path o CardsDocumento194 páginasNursing Path o CardsDanielle Shull100% (1)
- Dr.M.Kannan MD DA Professor and HOD of Anaesthesiology Tirunelveli Medical CollegeDocumento26 páginasDr.M.Kannan MD DA Professor and HOD of Anaesthesiology Tirunelveli Medical CollegeAlina CiubotariuAún no hay calificaciones
- Non-Protein Nitrogen CompoundsDocumento6 páginasNon-Protein Nitrogen CompoundspixiedustAún no hay calificaciones
- Chronic Kidney Disease: Diagnosis and TherapyDocumento21 páginasChronic Kidney Disease: Diagnosis and TherapyLindsAún no hay calificaciones
- CRFDocumento50 páginasCRFKevin MontoyaAún no hay calificaciones
- PlabDocumento214 páginasPlabKarata SinghAún no hay calificaciones
- Diet Module 4 - 2019Documento90 páginasDiet Module 4 - 2019sourav.surAún no hay calificaciones
- Disorders of Hemostasis Associated in Chronic Kidney DiseaseDocumento7 páginasDisorders of Hemostasis Associated in Chronic Kidney DiseaseSandi AuliaAún no hay calificaciones
- Acute Renal Insufficiency Made Ridiculously Simple (Medicalstudyzone - Com)Documento73 páginasAcute Renal Insufficiency Made Ridiculously Simple (Medicalstudyzone - Com)charelle.33100% (2)
- Pathphysiology CurriculumDocumento14 páginasPathphysiology Curriculumapi-3728690Aún no hay calificaciones
- Pathophysiology of Chronic Renal Failure PDFDocumento4 páginasPathophysiology of Chronic Renal Failure PDFDewa Made Rendy SanjayaAún no hay calificaciones
- Renal Failure PresentationDocumento110 páginasRenal Failure PresentationMusa yohana100% (1)
- Acute-Renal-Failure Lecture OnlyDocumento17 páginasAcute-Renal-Failure Lecture OnlyeyesontheskyAún no hay calificaciones
- Chronic Kidney Disease Feb 2021Documento56 páginasChronic Kidney Disease Feb 2021ToyoAún no hay calificaciones
- Progression To End Stage Renal Disease in Post-Streptococcal Glomerulonephritis (PSGN) - Chandigarh StudyDocumento6 páginasProgression To End Stage Renal Disease in Post-Streptococcal Glomerulonephritis (PSGN) - Chandigarh StudyAubrey PerezAún no hay calificaciones
- Acute Kidney Injury Case Study FinalDocumento46 páginasAcute Kidney Injury Case Study FinalSalwa KaramanAún no hay calificaciones
- Jurnal Intra Dial ExercseDocumento70 páginasJurnal Intra Dial ExercseSutiknosaja CukupAún no hay calificaciones
- LEC-10-Non-Protein Nitrogen CompoundsDocumento12 páginasLEC-10-Non-Protein Nitrogen CompoundsBobbyAún no hay calificaciones
- Kidney Injury: AcuteDocumento14 páginasKidney Injury: AcuteRizkyaFarhanAún no hay calificaciones
- Acute Renal FailureDocumento19 páginasAcute Renal FailureUmmul HidayahAún no hay calificaciones
- Urinary Tract Disorders, PowerpointDocumento63 páginasUrinary Tract Disorders, Powerpointmutia mutia100% (4)