Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Comparison of Two Diff Erent Right-Sided Double-Lumen Tubes With Diff Erent Designs
Cargado por
Linto JohnTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Comparison of Two Diff Erent Right-Sided Double-Lumen Tubes With Diff Erent Designs
Cargado por
Linto JohnCopyright:
Formatos disponibles
Original Article
Turk J Med Sci
2012; 42 (6): 1063-1069
TBTAK
E-mail: medsci@tubitak.gov.tr
doi:10.3906/sag-1201-46
Comparison of two different right-sided double-lumen tubes
with different designs
Hilal SAZAK1, Uur GKTA2, Ali ALAGZ1, ilsem SEVGEN DEMRBA1, zlem GVEN1,
Eser AVKILIOLU1
Aim: To compare usage of 2 right-sided double-lumen tubes (RDLTs) with different designs in thoracic anesthesia.
Although the left-sided double-lumen tube (DLT) is preferred, the RDLT is necessary in some circumstances.
Materials and methods: A total of 40 patients undergoing left thoracotomy were divided into 2 groups receiving a
Rsch or Sheridan RDLT. The position of the RDLT was verified by clinical evaluation. It was also checked by fiberoptic
bronchoscope (FOB). When malposition was detected, it was corrected using the FOB. The correct installation time of
the RDLT, frequency of bronchoscopy, and left lung collapse time were recorded.
Results: According to the bronchoscopic assessment, the rates of patients with a misplaced RDLT in the supine (40% vs.
50%) and lateral decubitis position (35% vs. 30%) were similar between the groups (P > 0.05). Ratios of total malpositions
to total bronchoscopies were similar. The most frequent malposition types were displacement of RDLTs proximally or
distally. Correct RDLT installation time (262 vs. 291 s) and collapse time of the left lung (215 vs. 234 s) were comparable
between the groups (P > 0.05).
Conclusion: With the aid of bronchoscopic evaluation, our data suggest that Rsch and Sheridan RDLTs are not superior
to each other in one-lung ventilation. They were similar in terms of malpositions.
Key words: One-lung ventilation, right-sided double-lumen tube, fiberoptic bronchoscopy
Introduction
Endobronchial intubation and one-lung ventilation
(OLV) are the most important practices in thoracic
anesthesia (1). Today, Robertshaw type doublelumen tubes (DLTs) are frequently used in patients
undergoing thoracic surgery (2-4). The margin of
safety is the margin in which the location is still
correct despite the displacement of the DLT (2).
Both in right and left thoracotomies, the left-sided
DLTs are usually preferred to the right-sided DLTs
(RDLTs), which have a lower margin of safety (5,6)
and higher risk of right upper lobe collapse and
obstruction (2).
In particular, anatomical features of the right
upper lobe division render the use of the RDLT more
difficult compared to the left-sided DLT. It is stated
that the use of RDLTs only with clinical assessment,
without confirming the location via fiberoptic
bronchoscope (FOB), is unacceptable (7,8). All RDLTs
have an additional opening, allowing ventilation
of the right upper lobe, in their endobronchial
lumen. Failure to fit this opening onto the bronchial
lumen of the right upper lobe can lead to some
complications such as atelectasis and hypoxia (9).
Although the design of the RDLT has been modified
many times in order to facilitate correct installation
Received: 17.01.2012 Accepted: 15.06.2012
1
Department of Anesthesiology and Reanimation, Atatrk Chest Disease and Thoracic Surgery Education and Research Hospital, Ankara - TURKEY
2
Department of Anesthesiology and Reanimation, Faculty of Medicine, Yznc Yl University, Van - TURKEY
Correspondence: Hilal SAZAK, Department of Anesthesiology and Reanimation, Atatrk Chest Disease and Thoracic Surgery Education and Research Hospital, Ankara - TURKEY
E-mail: hilalgun@yahoo.com
1063
Comparison of two right-sided double-lumen tubes
and to allow ventilation of the right upper lobe, the
optimal DLT design has not yet been found. Various
brands of RDLTs with different bronchial balloon
configurations and locations are currently available.
Both the size and the place of the right upper lobe
ventilation openings are also different from each
other in these RDLTs (8). It has been reported that
the incidence of malposition detected by FOB varies
between 73% and 89%, when a right-sided RDLT
is placed without the use of a FOB (10-12). In this
study, we aimed to compare the effectiveness of
the Rsch and Sheridan brands of RDLTs having
different configurations of endobronchial balloon
and upper lobe ventilation openings. We compared
their clinical usage evaluating installation into the
right main bronchus, intraoperative misplacements,
and collapse of the operated lung.
Materials and methods
This prospective, randomized and single-blinded
study was performed with approval of the institutional
human investigation ethics committee and written
informed consent obtained from all patients.
The study was performed in accordance with the
principles of the Declaration of Helsinki. Forty adult
patients (28 males, 12 females) undergoing elective
left-sided thoracotomy were allocated into 2 groups.
Patients with destroyed lung, emphysematous lung
disease, or endobronchial lesions in the right main
bronchus or intermediary bronchus were excluded
from the study.
Rsch (Rschelit, Bronchopart, Willy Rsch AG,
Kernen, Germany) and Sheridan (Sher-i-bronch,
Hudson Respiratory Care Inc., Temecula, CA, USA)
brand of RDLTs were placed in Group R (n = 20)
and Group S (n = 20), respectively. The size of the
DLT was 35-37 French (Fr) in females, while it was
39-41 Fr in males. In the conventional intubation
method, the endobronchial cuff passed the vocal
cords with direct laryngoscopy, as the distal concave
angle of DLT faced the anterior. The RDLT was
installed by pushing the tube with a 90 rotation
towards the right side. The stylet was pulled as soon
as the endobronchial cuff passed the vocal cords.
The tracheal and endobronchial cuffs were inflated
consecutively until no leak was observed. The
placement of the DLT was assessed clinically with
manual ventilation, inspection, and auscultation
of the chest by clamping the lumens of the DLT
individually. The position of the DLT was recorded as
appropriate or inappropriate based on a clinical
evaluation. In the supine position, correct placement
of the DLT was verified using a FOB (Olympus LF
DP, Olympus Medical System Corp., Tokyo, Japan)
by another anesthetist. Inappropriately located DLTs
were positioned in the expected place via the FOB.
After bronchoscopic evaluation, if the DLT had to be
moved more than 0.5 cm to correct its position, this
condition was defined as malposition.
In the operating room, following pre-oxygenation,
anesthesia was induced with propofol (2.5 mg/kg
I.V.), fentanyl citrate (2 g/kg I.V.), and vecuronium
bromide (0.1 mg/kg I.V.). Anesthesia was maintained
with isoflurane (1%-1.5%), fentanyl citrate, and
vecuronium bromide. Oxygen 100% was used during
OLV and a routine OLV procedure was performed
throughout this study. Electrocardiography,
peripheral oxygen saturation (SpO2), invasive arterial
pressure, and end-tidal carbon dioxide (ETCO2) were
monitored. The arterial blood gases were analyzed
hourly during the operation.
The bronchoscopic criteria of correct RDLT
installation were described as follows: observation
of the carina and direction of the endobronchial
lumen towards the right when examining from the
tracheal lumen, and observation of the right upper
lobe bronchus orifice at the level of right upper
lobe ventilation opening when checking from the
bronchial lumen of the DLT. When the right upper
lobe ventilation opening of the DLT was not placed
at the level of right upper lobe bronchus orifice, the
position of the DLT was corrected by turning and
pushing or pulling it along by FOB. The correct
installation time was regarded as the time beginning
from the passage of the endobronchial cuff between
the vocal cords to the moment that the DLTs position
was decided to be appropriate using a FOB.
All patients were intubated with a Robertshaw
type, disposable RDLT using the conventional
method by the same thoracic anesthesia specialist.
The position of the DLT was also assessed via
FOB in the lateral decubitis position and throughout
the operation every 30 min. In the event of DLT
1064
H. SAZAK, U. GKTA, A. ALAGZ, . SEVGEN DEMRBA, . GVEN, E. AVKILIOLU
malposition it was corrected immediately. Additional
bronchoscopies were performed whenever a difficulty
existed in the operated lung collapse or dependent
lung ventilation. Total number of bronchoscopies,
and the number and types of malpositions were
recorded. The malposition types are defined in Table
1. The surgeon was asked to evaluate the left lung
collapse as good surgical view, partial collapse, or
no collapse. The time beginning from the initiation
of OLV to complete collapse of the operated lung was
recorded as lung collapse time.
The descriptive statistics were defined as mean
and standard deviation for continuous variables.
Categorical variables were defined as numbers
and percentages. The Pearson chi-square test and
Fishers exact test were used for determination of the
relationships between categorical variables.
Results
The groups were similar with respect to patient
characteristics (P > 0.05) (Table 2). In clinical
assessment, DLT malpositions were significantly
lower in Group R compared to Group S (P = 0.05) in
the patients in the supine position. However, there was
no significant difference between the groups in the
assessment of DLT placement via FOB (Table 3). No
significant difference was found between the groups
in terms of malposition types determined using FOB
in the patients in the supine and lateral decubitis
positions (Table 4). During the operation, including
additional bronchoscopies, DLTs were found to be
displaced proximally in 8 and 7 patients in Group R
and Group S, respectively. DLTs were observed to be
displaced distally in 3 patients in each group. This
difference was not statistically significant (P > 0.05).
Table 1. Description of malposition types.
Malposition types
Type 1
Protrusion of the bronchial balloon into the carina and inadequate visualization of the right upper lobe orifice from the
upper lobe ventilation opening in the bronchial lumen (proximal displacement of DLT)
Type 2
Nonvisualization of the upper margin of the bronchial balloon at the entrance of the main bronchus and inadequate
visualization of the right upper lobe orifice from the upper lobe ventilation opening in the bronchial lumen (distal
displacement of DLT)
Type 3
Both lumens of DLT are in the trachea
Type 4
Intubation of the left main bronchus
DLT: double-lumen tube.
Table 2. Patient characteristics.
Group R (n = 20)
Group S (n = 20)
Age (year)
50.5 12.8
48.8 17.9
0.74
Weight (kg)
68.40 9.70
66.80 12.80
0.65
Height (cm)
166.9 5.4
168.4 7.6
0.30
Female/Male
6/14
6/14
1.00
177.15 56.62
177.15 34.40
1.00
Operation time (min)
Surgical procedures
0.251
Pneumonectomy
Lobectomy
12
Wedge resection
Cystotomy
1065
Comparison of two right-sided double-lumen tubes
Table 3. Clinical assessment and bronchoscopic evaluation of the tube placement in the patient in supine
position.
Group R
(n = 20)
Group S
(n = 20)
11 (55%)
5 (25%)
0.05
Malposition with FOB
3 (27%)
0 (0%)
0.228
No malposition with FOB
8 (73%)
5 (100%)
0.638
9 (45%)
15 (75%)
0.05
Malposition with FOB
5 (56%)
10 (67%)
0.678
No malposition with FOB
4 (44%)
5 (33%)
0.678
DLT placement
Clinically correct
Clinically incorrect
DLT: double-lumen tube, FOB: fiberoptic bronchoscope.
Table 4. Malposition types by bronchoscopic evaluation in the patient in supine and lateral decubitis position.
Supine
LDP
Group R
(n = 20)
Group S
(n = 20)
No
10
0.523
Type 1
0.677
Type 2
0.462
Type 3
0.305
Type 4
1.000
No
0.735
Type 1
0.203
Type 2
0.065
Type 3
1.000
Type 4
1.000
When the patient turned to the lateral decubitis position (LDP)
The data for DLT placement by bronchoscopic
evaluation are given in Table 5. There was no
significant difference between the groups in terms
of correct installation time or left lung collapse time
(P > 0.05). The ratios of total malpositions to total
bronchoscopies were 26/152 (17.1%) and 26/146
(17.8%) in Group R and Group S, respectively
(P > 0.05). The number of patients without DLT
malpositions was 8 (40%) and 9 (45%) in Group
R and Group S, respectively, in all bronchoscopic
checks (Table 5).
1066
The surgeon evaluated the left lung collapse
as good in 18 and 17 patients in Group R and
Group S, respectively, whereas it was defined as
partial in 2 and 3 patients in Group R and Group
S, respectively. There was no statistically significant
difference between the groups with regard to surgical
assessment of the left lung collapse (P > 0.05). The
installation of the DLT and FOB handling were
managed uneventfully in the present study. Arterial
blood gases and ETCO2 values were within the
normal physiological ranges. Hypoxemia (SaO2 <
90%) was not seen at any stage of our study.
H. SAZAK, U. GKTA, A. ALAGZ, . SEVGEN DEMRBA, . GVEN, E. AVKILIOLU
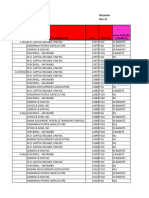
Table 5. Data of DLT placement by bronchoscopic evaluation.
Group R
(n = 20)
Group S
(n = 20)
Patients with DLT malposition in supine position
8 (40%)
10 (50%)
0.523
Patients with DLT malposition in LDPa
7 (35%)
6 (30%)
0.735
5/7 (71.4%)
4/6 (66.7%)
0.853
3/13 (23%)
3/14 (21.4%)
0.918
Patients without DLT malposition
8 (40%)
9 (45%)
0.749
Malpositions in routine bronchoscopy during operation
9 (45%)
6 (30%)
0.080
Total malpositions
26
26
0.635
Routine bronchoscopies
150
142
Additional bronchoscopies
0.36
Correct installation time (s)
262.25 108.62
291.5 126.75
0.270
Lung collapse time (s)
215.1 127.89
234 69.83
0.537
Patients with intraoperative DLT malposition/with DLT malposition in LDPa
a
Patients with intraoperative DLT malposition/without DLT malposition in LDP
DLT: double-lumen tube, FOB: fiberoptic bronchoscope.
When the patient turned to the lateral decubitis position (LDP)
Discussion
Although a left-sided DLT is usually preferred during
OLV in patients undergoing right or left thoracotomy,
the placement of a RDLT might be mandatory in
some conditions. Benumof (2) summarized these
conditions as follows: the presence of a lesion in the
left main bronchus, torsion of the left main bronchus
due to external pressure, destruction of the tracheabronchial tree, and special operations such as sleeve
resections. In fact, in many studies, a RDLT has been
found to be as safe and effective as a left-sided DLT
in the presence of FOB (4,6). Ehrenfeld et al. (13)
stated that the idea that a left-sided DLT is safer than
RDLT is not true when hypoxemia, hypercapnia,
and high airway pressure are considered as criteria.
However, blind (without FOB) installation of the
RDLT might lead to significant problems such as
atelectasis in the upper lobe, shunt, and hypoxia.
When the RDLT is placed blindly, the incidence of
malposition is high with the guidance of a FOB. In
previous studies, when checked by FOB, the rates of
DLT malpositions were 89%, 83%, and 73% (10-12).
Interestingly, the positions were thought to be correct
with auscultation.
In one case, Van Dyck and Astiz (14) reported that
the bronchial lumen of the Sheridan RDLT caused
an acute ventilation problem by twisting during
the intubation and entering the right upper lobe
bronchus. They concluded that with the Sheridan
RDLT the right upper lobe ventilation opening is
placed between the 2 bronchial balloons, and is
longer and wider than the Rsch. These factors might
have contributed to the bronchial lumens kink in the
Sheridan RDLT. In a prospective study, Hurford et al.
(15) found that the incidence of malposition leading
to insufficient lung isolation was higher with the
Sheridan RDLT than with the Rsch.
In our study, we found a significant difference
between the groups in terms of clinical malpositions
in the supine position of 45% in Group R and 75% in
Group S. We suggest that this can arise from incorrect
auscultation findings (reflected sound), displacement
of the tube during bronchoscopy, or insufficient
inflation of the bronchial cuff.
The mean margin of safety, which explains
the vulnerability of the RDLT to malposition, is
one third that of the left-sided DLT (5,7,12). It has
been stated that the use of RDLTs with only clinical
1067
Comparison of two right-sided double-lumen tubes
assessment, without confirmation using FOB, is
not appropriate (7,8). In our study, the groups were
similar in terms of the number of malpositions found
in the first assessment with FOB. The malpositions
were detected with FOB in approximately one fifth
of all DLTs whose position was clinically assessed as
correct. This shows the necessity of bronchoscopy
during the installation of a RDLT.
An optimal RDLT design facilitating the correct
installation towards the right main bronchus and
allowing ventilation of the right upper lobe has
not been found yet. Failure to fit the upper lobe
ventilation opening to the right upper lobe bronchus
lumen during right endobronchial intubation leads
to serious complications. It is stated that this problem
is rarely encountered if the ventilation opening is
wider and longer (9). The endobronchial balloons of
the Rsch and Sheridan RDLTs are in different forms
and locations despite having similar basic features
(7,8). The Rsch RDLT has a single bronchial balloon
and the upper lobe ventilation opening is placed in
that area (Figure 1), whereas the Sheridan RDLT has
2 bronchial balloons and the upper lobe ventilation
opening is between them (Figure 2).
Campos et al. (6) reported that DLT malpositions
often occurred when the patient was turned to the
lateral decubitis position from the supine position.
Figure 1. Endobronchial segment of Rsch right-sided doublelumen tube.
1068
The DLT can be displaced distally or proximally by
head and neck movements of the patient (16). The
tolerance of RDLTs to head movements is lower than
that of left-sided DLTs. When a small tube is used, the
DLT could be pushed cephalad with a high volume of
the endobronchial cuff (2).
When the patient turned to the lateral decubitis
position from the supine position, we observed
malpositions in approximately one third of
the patients in both groups. The probability of
malposition during OLV was found to be higher in
patients having DLT malposition when turned to the
lateral decubitis position (17). In our study, the ratio
of patients with intraoperative DLT malposition to
the patients having DLT malposition when turned
to the lateral decubitis position was 71.4% in Group
R and 66.7% in Group S. Moreover, the ratio of the
patients with intraoperative DLT malposition to the
patients not having DLT malposition when turned to
the lateral decubitis position was 23% and 21.4% in
Group R and Group S, respectively.
In the present study, displacement of the DLT
proximally or distally was the most common
malposition type in both groups. Surgeons did not
define any insufficient collapse of the left lung during
OLV.
The use of a RDLT with assessment of its
placement via FOB is recommended in the anesthesia
Figure 2. Endobronchial segment of Sheridan right-sided
double-lumen tube.
H. SAZAK, U. GKTA, A. ALAGZ, . SEVGEN DEMRBA, . GVEN, E. AVKILIOLU
curriculum (7,8,18). In a previous study, which was
performed on anesthetists with limited experience
in thoracic surgery, the endobronchial intubation
time was long and the malposition rates were high.
Consequently, that result was attributed to insufficient
knowledge of FOB usage (19). Routine FOB use
provides anesthesiologists increased expertise in
positioning DLTs (20). We think that training on
RDLT usage with the aid of a FOB is essential as a part
of the residency program in thoracic anesthesiology
in order to provide the skills for conditions requiring
a RDLT. We agree with previous authors (21,22)
on the point that the clinician should be familiar
with the available devices to provide OLV and safe
management of patients.
In conclusion, with the aid of bronchoscopic
evaluation, the present study indicates that Rsch
and Sheridan RDLTs are not superior to each other
in OLV. Despite their different bronchial structures,
both Rsch and Sheridan RDLTs were safe and similar
in terms of malpositions during thoracic surgery.
Handling the RDLT and FOB is a challenging issue in
thoracic anesthesia practice. Therefore, experienced
anesthesia staff should be available in such a center
performing thoracic surgery and OLV.
References
12.
Klein U, Karzai W, Bloos F, Wohlfarth M, Gottschall R, Fritz
H et al. Role of fiberoptic bronchoscopy in conjunction
with the use of double-lumen tubes for thoracic anesthesia.
Anesthesiology 1998; 88: 346-50.
13.
Benumof JL, Alfery DD. Anesthesia for Thoracic Surgery. In:
Miller RD, editor. Anesthesia. 5th ed. Philadelphia: ChurchillLivingstone; 2000. p. 1665-752.
Ehrenfeld JM, Walsh JL, Sandberg WS. Right and left-sided
Mallinckrodt double-lumen tubes have identical clinical
performance. Anesth Analg 2008; 106: 1847-52.
14.
Campos JH, Massa FC. Is there a better right-sided tube for
one-lung ventilation? A comparison of the right-sided doublelumen tube with the single-lumen tube with right-sided
enclosed bronchial blocker. Anesth Analg 1998; 86: 696-700.
Van Dyck MJ, Astiz I. Kinking of a right-sided double-lumen
tube in the right upper lobe bronchus. Anesthesiology 1994;
80: 1410-1.
15.
Hurford WE, Alfille PH. A quality improvement study of the
placement and complications of double-lumen endobronchial
tubes. J Cardiothorac Vasc Anesth 1993; 7: 517-20.
1.
Gothard JWW. Anaesthetic equipment for thoracic surgery.
Anaesthesia and Intensive Care Medicine 2005; 6: 425-7.
2.
Benumof JL. Separation of the two lungs (double-lumen tube
and bronchial blocker intubation). In: Benumof JL, editor.
Anesthesia for thoracic surgery. Philadelphia: WB Saunders;
1995. p. 330-89.
3.
4.
5.
Benumof JL, Partridge BL, Salvatierra C, Keating J. Margin
of safety in positioning modern double-lumen endotracheal
tubes. Anesthesiology 1987; 67: 729-38.
16.
Saito S, Dohi S, Naito H. Alteration of double-lumen
endobronchial tube position by flexion and extension of the
neck. Anesthesiology 1985; 62: 697-8.
6.
Campos JH, Massa FC, Kernstine KH. The incidence of right
upper-lobe collapse when comparing a right-sided doublelumen tube versus a modified left double-lumen tube for leftsided thoracic surgery. Anesth Analg 2000; 90: 535-40.
17.
Inoue S, Nishimine N, Kitaguchi K, Furuya H, Taniguchi S.
Double lumen tube location predicts tube malposition and
hypoxaemia during one lung ventilation. Br J Anaesth 2004;
92: 195-201.
7.
Cohen E. Double-lumen tube position should be confirmed
by fiberoptic bronchoscopy. Curr Opin Anaesthesiol 2004; 17:
1-6.
18.
Ramsay MAE. Right-sided double-lumen endobronchial tubes
for left-sided thoracic surgery. Anesth Analg 2000; 91: 762.
8.
Cohen E. Methods of lung separation. Curr Opin Anaesthesiol
2002; 15: 69-78.
19.
Campos JH, Hallam EA, Natta TV, Kernstine KH. Devices for
lung isolation used by anesthesiologists with limited thoracic
experience. Anesthesiology 2006; 104: 261-6.
9.
Campos JH. Current techniques for perioperative lung
isolation in adults. Anesthesiology 2002; 97: 1295-301.
20.
10.
McKenna MJ, Wilson RS, Botelho RJ. Right upper lobe
obstruction with right-sided double-lumen endobronchial
tubes: a comparison of two tube types. J Cardiothorac Anesth
1988; 2: 734-40.
Bussires JS, Slinger P. Correct positioning of double-lumen
tubes. Can J Anesth 2012; 59: 431-6.
21.
Cohen E. Methods of lung separation. Minerva Anestesiol
2004; 70: 313-8.
22.
11.
Alliaume B, Coddens J, Deloof T. Reliability of auscultation
in positioning of double-lumen endobronchial tubes. Can J
Anaesth 1992; 39: 687-90.
Hoten T, Topu S. The importance of bronchoscopic anatomy
for anesthesiologists. Tuberk Toraks 2011; 59: 416-26.
1069
También podría gustarte
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (894)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- DMF360 Tandem Lift With ForkliftDocumento4 páginasDMF360 Tandem Lift With Forkliftreda mesbahAún no hay calificaciones
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- Research BulletsDocumento18 páginasResearch BulletsVong Albios DogomeoAún no hay calificaciones
- Aeration PaperDocumento11 páginasAeration PapersehonoAún no hay calificaciones
- Matrix Structural Analysis of BeamsDocumento28 páginasMatrix Structural Analysis of BeamsKristine May Maturan0% (1)
- 2.2 X 2 Feet Macgd3 Cake DesignDocumento1 página2.2 X 2 Feet Macgd3 Cake DesignLinto JohnAún no hay calificaciones
- 1 S-Adenosyl-L-methionine Synthetase and Phospholipid Methyltransferase Are Inhibited in Human Cirrhosis. Hepatology 1988 8:65-8Documento2 páginas1 S-Adenosyl-L-methionine Synthetase and Phospholipid Methyltransferase Are Inhibited in Human Cirrhosis. Hepatology 1988 8:65-8Linto JohnAún no hay calificaciones
- Pathophysiology and Therapy of Myocardial Ischaemia/reperfusion SyndromeDocumento14 páginasPathophysiology and Therapy of Myocardial Ischaemia/reperfusion SyndromeLinto JohnAún no hay calificaciones
- HF GuidelinesDocumento76 páginasHF GuidelinesLinto JohnAún no hay calificaciones
- Neutrophil Stunning by Metoprolol Reduces Infarct Size: ArticleDocumento15 páginasNeutrophil Stunning by Metoprolol Reduces Infarct Size: ArticleLinto JohnAún no hay calificaciones
- Exacerbations GoldDocumento10 páginasExacerbations GoldLinto JohnAún no hay calificaciones
- Metoprolol in The Treatment of Cardiovascular Disease: A Critical ReappraisalDocumento19 páginasMetoprolol in The Treatment of Cardiovascular Disease: A Critical ReappraisalLinto JohnAún no hay calificaciones
- Evidences On SAMe in Liver DiseasesDocumento1 páginaEvidences On SAMe in Liver DiseasesLinto JohnAún no hay calificaciones
- Same Eliminates Free Radicals, Protects LiverDocumento1 páginaSame Eliminates Free Radicals, Protects LiverLinto JohnAún no hay calificaciones
- Evolving Therapies For Myocardial Ischemia-Reperfusion InjuryDocumento18 páginasEvolving Therapies For Myocardial Ischemia-Reperfusion InjuryLinto JohnAún no hay calificaciones
- Clopidogrel Versus Ticagrelor o Prasugrel en Pacientes de 70 Años o Más Con Síndrome Coronario Agudo Sin Elevación Del Segmento ST (POPular AGE)Documento8 páginasClopidogrel Versus Ticagrelor o Prasugrel en Pacientes de 70 Años o Más Con Síndrome Coronario Agudo Sin Elevación Del Segmento ST (POPular AGE)Frank Antony Arizabal GaldosAún no hay calificaciones
- Restenosis After Coronary and Peripheral Intervention: Efficacy and Clinical Impact of CilostazolDocumento8 páginasRestenosis After Coronary and Peripheral Intervention: Efficacy and Clinical Impact of CilostazolLinto JohnAún no hay calificaciones
- GINA Flare UpsDocumento15 páginasGINA Flare UpsLinto JohnAún no hay calificaciones
- Airway Inflammation Induced SputumDocumento2 páginasAirway Inflammation Induced SputumLinto JohnAún no hay calificaciones
- Pharma MarketingDocumento167 páginasPharma MarketingLinto JohnAún no hay calificaciones
- Exacerbations GoldDocumento10 páginasExacerbations GoldLinto JohnAún no hay calificaciones
- Viral Infection in Community-Acquired Pneumonia: A Systematic Review and Meta-AnalysisDocumento11 páginasViral Infection in Community-Acquired Pneumonia: A Systematic Review and Meta-AnalysisLinto JohnAún no hay calificaciones
- Final Evolution in Respiratory Medicine - Copy1Documento49 páginasFinal Evolution in Respiratory Medicine - Copy1Linto JohnAún no hay calificaciones
- A New Strategy in Reliever Therapy Budesonide/Formoterol Maintenance PlusDocumento13 páginasA New Strategy in Reliever Therapy Budesonide/Formoterol Maintenance PlusLinto JohnAún no hay calificaciones
- Air Pollution A Big Killer in India: Source: World Health OrganisationDocumento1 páginaAir Pollution A Big Killer in India: Source: World Health OrganisationLinto JohnAún no hay calificaciones
- For Uncontrolled Asthma Despite ICS: Tiotropium Add-On TXDocumento1 páginaFor Uncontrolled Asthma Despite ICS: Tiotropium Add-On TXLinto JohnAún no hay calificaciones
- What Is CopdDocumento4 páginasWhat Is CopdLinto JohnAún no hay calificaciones
- Coming SoonDocumento1 páginaComing SoonLinto JohnAún no hay calificaciones
- StatusasthmaticusDocumento40 páginasStatusasthmaticusLinto JohnAún no hay calificaciones
- Coming SoonDocumento1 páginaComing SoonLinto JohnAún no hay calificaciones
- Potential Drug That Could Help Treat Cystic Fibrosis Identified by ResearchersDocumento2 páginasPotential Drug That Could Help Treat Cystic Fibrosis Identified by ResearchersLinto JohnAún no hay calificaciones
- Zero Day REspi Test PaperDocumento3 páginasZero Day REspi Test PaperLinto JohnAún no hay calificaciones
- Coming SoonDocumento1 páginaComing SoonLinto JohnAún no hay calificaciones
- Recent Advances in Asthma ManagementDocumento6 páginasRecent Advances in Asthma ManagementLinto JohnAún no hay calificaciones
- AutohalerDocumento51 páginasAutohalerLinto JohnAún no hay calificaciones
- Nov. AbwDocumento50 páginasNov. Abwjbyarkpawolo70Aún no hay calificaciones
- 3 - Molecules and Compounds: Practice TestDocumento2 páginas3 - Molecules and Compounds: Practice Testfamily_jvcAún no hay calificaciones
- Fulltext PDFDocumento454 páginasFulltext PDFVirmantas JuoceviciusAún no hay calificaciones
- Kitchen Chemistry ExperimentDocumento7 páginasKitchen Chemistry ExperimentMss FaixaAún no hay calificaciones
- 03 Correcao Exercicios FixacaoDocumento3 páginas03 Correcao Exercicios FixacaoRodrigoAún no hay calificaciones
- Formulas For Thermodynamics 1Documento2 páginasFormulas For Thermodynamics 1Stefani Ann CabalzaAún no hay calificaciones
- TVL CSS11 Q4 M1Documento12 páginasTVL CSS11 Q4 M1Richard SugboAún no hay calificaciones
- UMTS Chap6Documento33 páginasUMTS Chap6NguyenDucTaiAún no hay calificaciones
- TM View Software User - S ManualDocumento190 páginasTM View Software User - S ManualLuis SánchezAún no hay calificaciones
- Matriculation Chemistry Introduction To Organic Compound Part 1 PDFDocumento24 páginasMatriculation Chemistry Introduction To Organic Compound Part 1 PDFiki292Aún no hay calificaciones
- Timer Counter ArduinoDocumento8 páginasTimer Counter ArduinoKietDangAún no hay calificaciones
- Alcohols, Phenols and Ethers Worksheet Answer Grade 12Documento6 páginasAlcohols, Phenols and Ethers Worksheet Answer Grade 12sethu100% (1)
- MCB and ELCB PDFDocumento35 páginasMCB and ELCB PDFChris AntoniouAún no hay calificaciones
- Chapter 2Documento2 páginasChapter 2LolmasterAún no hay calificaciones
- A Git Cheat Sheet (Git Command Reference) - A Git Cheat Sheet and Command ReferenceDocumento14 páginasA Git Cheat Sheet (Git Command Reference) - A Git Cheat Sheet and Command ReferenceMohd AzahariAún no hay calificaciones
- TP 03: Technique D'optimisation PSODocumento3 páginasTP 03: Technique D'optimisation PSOCEM Yelle N centreAún no hay calificaciones
- Design of RivetsDocumento20 páginasDesign of RivetsRavishanker BaligaAún no hay calificaciones
- Lectures Accompanying The Book - Solid State Physics - An (PDFDrive)Documento148 páginasLectures Accompanying The Book - Solid State Physics - An (PDFDrive)Raza Ali RazaAún no hay calificaciones
- Chapter 1: Introduction: 1.1 Background TheoryDocumento36 páginasChapter 1: Introduction: 1.1 Background TheoryBe-fit Be-strongAún no hay calificaciones
- Multi-Band Booster With HRLB - In-Band Routed DCN Solution GuideDocumento26 páginasMulti-Band Booster With HRLB - In-Band Routed DCN Solution GuideAchintha AluthmanageAún no hay calificaciones
- Alkali Boil Out ProcedureDocumento7 páginasAlkali Boil Out Procedureismail karmanaAún no hay calificaciones
- Mediburn 30Documento35 páginasMediburn 30Vsee EnkoAún no hay calificaciones
- Bio Inorganic ChemistryDocumento2 páginasBio Inorganic ChemistryMeghna KumarAún no hay calificaciones
- Mammography View ChapterDocumento60 páginasMammography View ChapterSehar GulAún no hay calificaciones
- Prepare and Interpret Technical DrawingDocumento5 páginasPrepare and Interpret Technical DrawingDwin Rosco75% (4)
- EWDLEWML Servo Motor DriverDocumento14 páginasEWDLEWML Servo Motor DriverWaleed LemsilkhiAún no hay calificaciones