Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Topical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDF
Cargado por
Treesna OuwpolyDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Topical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDF
Cargado por
Treesna OuwpolyCopyright:
Formatos disponibles
Nikhil et al
IJRPC 2012, 2(2)
ISSN: 22312781
INTERNATIONAL JOURNAL OF RESEARCH IN PHARMACY AND CHEMISTRY
Review Article
Available online at www.ijrpc.com
TOPICAL LIPOSOMAL GEL: A NOVEL DRUG DELIVERY SYSTEM
Nikhil Argan*, SL. Harikumar and Nirmala
Rayat and Bahra Institute of Pharmacy, Sahauran, District Mohali, Punjab, Chandigarh, India.
ABSTRACT
Liposomes established themselves as a promising novel drug delivery vehicle in several different
basic sciences and as a viable alternative in several applications. Liposomes are microscopic
spheres with an aqueous core surrounded by one or more outer shells consisting of lipids
arranged in a bilayer configuration. Liposomes are acceptable and superior carriers having
ability to encapsulate hydrophilic and lipophilic drugs and protect them from degradation. It also
has affinity to keratin of horny layer of skin and can penetrate deeper into skin and hence give
better absorption. Applied on the skin, liposomes may act as a solublizing matrix for poorly
soluble drugs, penetration enhancer as well as local depot at the same time diminishing the side
effects of these drugs. Topical liposome formulations could be more effective and less toxic than
conventional formulations. The liposome gel formulations could perform therapeutically better
effects than the conventional formulations, as prolonged and controlled release topical dosage
forms, which may lead to improved efficiency and better patient compliance.
the opposite end is water insoluble. Watersoluble medications added to the water were
trapped inside the aggregation of the
hydrophobic ends; fat-soluble medications
were incorporated into the phospholipid
layer10-11.
Topical drug delivery is an attractive route for
12
local and systemic treatment .Liposomes are
acceptable and superior carriers and have
ability to encapsulate hydrophilic and lipophilic
13-14
drugs
and protect them from degradation. It
also has affinity to keratin of horny layer of skin
and can penetrate deeper into skin and hence
give better absorption. In the formulation of
topical dosage forms, attempts are being
made to utilize drug carriers that ensure
adequate localization or penetration of drug
within or through the skin in order to enhance
the local and minimize the systemic effects or
to
ensure
adequate
percutaneous
absorption15. Applied on the skin, liposomes
may act as a solublizing matrix for poorly
soluble drugs, penetration enhancer as well as
local depot at the same time diminishing the
side effects of these drugs. Topical liposome
formulations could be more effective and less
toxic than conventional formulations. Skin has
been considered as a promising route for the
administration of drugs because of its
accessibility and large surface area.
Transdermal drug delivery system, designed to
deliver a variety of drugs to the body through
INTRODUCTION
Liposomes
Liposomes are microscopic spheres with an
aqueous core surrounded by one or more
outer shell(s) consisting of lipids arranged in a
bilayer configuration. The potential use of
liposomes as drug carriers was recognized
more than 25 years ago and, since that time,
liposomes have been used in a broad range of
1
pharmaceutical applications.
They present many advantages since they can
be used as carriers for both hydrophilic and
lipophilic molecules, as well as drug delivery
systems for controlled drug delivery for
2-5
different
therapeutical
purposes .An
important aspect of liposomes is the protection
that they afford as an encapsulating agent
against potentially damaging conditions in
external environments. Liposomes are also an
important system in their own right in medical,
cosmetic,
and
industrial
applications67
.Liposomes can substantially improve drug
loading, drug delivery and sustained release,
thereby offering clear-cut advantages over
8
traditional dosage forms .Liposomes were first
produced in England in 1961 by Alec D.
Bangham, who was studying phospholipids
and blood clotting9. It was found that
phospholipids
combined
with
water
immediately formed a sphere because one
end of each molecule was water soluble, while
383
IJRPC 2012, 2(2)
Nikhil et al
diffusion across the skin layers, is appealing
for several reasons including avoidance of the
variable absorption and metabolic breakdown
associated with oral treatments, drug
administration can be continuous, and minimal
intestinal irritation can be avoided. Liposome is
has been used in transdermal drug delivery
system because of its much higher diffusivity
16in skin compared to most bare drugs
18
.Liposomal formulations are widely used in
the pharmaceutical field as drug delivery
systems due to their versatility and clinical
efficacy and they have been used to
administer drugs by several routes such as the
oral, parenteral, and topical. Among these,
topical delivery of drugs carried by liposomes
exhibits interesting applications, not only for
promoting dermal delivery of drugs which have
to act topically, such as local anaesthetics, but
also for enhancing transdermal delivery of
drugs intended for systemic use, thus more
effectively
exploiting
this
non-invasive
alternative route to oral administration. Due to
the forementioned advantages, in this study
liquid-state liposomes were chosen to serve as
19-20
the
drug
delivery
system
.Although
liposomes
demonstrated
promise
for
Transdermal drug delivery, the practical
application of these formulations onto the skin
is less. However, these can be incorporated
into the gels than can apply onto the skin. It
has been found that liposomes incorporate into
21-22
the gels are stable
.Hydrogels are clinically
acceptable
systems
that
offer
many
advantages, such as suitable rheological
properties, good tissue compatibility and
convenience in handling and ease of
application. Carbopol gels are approved for
pharmaceutical use in several different
administration routes. Cutaneous use of these
gels is advantageous as they possess good
rheological properties resulting in long residue
times at the site of administration and they
provide
higher
and
sustained
skin
concentrations of drugs compared to
conventional gels and creams. Moreover,
carbopol gels are anionic hydrogels with good
buffering capacity, which may contribute to the
23-24
maintenance of the desired pH
.
ISSN: 22312781
Advantages
1. Precipitation at the injection site and in the
blood circulation can be prevented.
2. Phospholipids are one of the few
solubilizers that are well tolerated
intravenously.
3. Provide selective passive targeting to
tumour tissues.
4. Increase safety and therapeutic index.
5. Increase stability via encapsulation
6. Site avoidance effect.
Methods of preparation of liposomes
A) Multilamellar Liposomes (MLV)
26
1.
Lipid hydration method
This is the most widely used method for the
preparation of MLV. The methodinvolves
drying a solution of lipids so that a thin film is
formed at the bottom of roundbottom flask and
then hydrating the film by adding aqueous
buffer and vortexing thedispersion for some
time. The hydration step is done at a
temperature above the gel-liquidcrystalline
transition temperature Tc of the lipid or above
the Tc of the highest meltingcomponent in the
lipid mixture. The compounds to be
encapsulated are added either toaqueous
buffer or to organic solvent containing lipids
depending upon their solubilities.MLV are
simple to prepare by this method and a variety
of substances can beencapsulated in these
liposomes. The drawbacks of the method are
low
internal
volume,low
encapsulation
efficiency and the size distribution is
heterogeneous.
2.
Solvent Spherule Method27
A method for the preparation of MLVs of
homogeneous size distribution .The process
involved dispersing in aqueous solution the
small spherules of volatile hydrophobic solvent
in which lipids had been dissolved. MLVs were
formed when controlled evaporation of organic
solvent occurred in a water bath.
B) Small Unilamellar Liposomes (SUV)
28
1. Sanitation Method
Here MLVs are sonicated either with a bath
type sonicator or a probe sonicator under an
inert atmosphere. The main drawbacks of this
method
are
very
low
internal
volume/encapsulation
efficiency,
possibly
degradation of phospholipids and compounds
to be encapsulated, exclusion of large
molecules, metal contamination from probe tip
and presence of MLV along with SUV.
Classification of liposomes based on
25
structure parameters
1. Multilamellar Large vesicles > 0.5um
2. Oligolamellar vesicles 0.1-1um
3. Unilamellar vesicles (All size range)
a) Small unilamellar vesicles 20-100nm
b) Medium sized unilamellar vesicles
c) Large unilamellar vesicles >100nm
d) Giant unilamellar vesicles >1um
4. Multivesicular vesicles >1um
29
2. French Pressure Cell Method
The method involves the extrusion of MLV at
20,000 psi at 4C through a smallorifice. The
384
Nikhil et al
IJRPC 2012, 2(2)
method has several advantages over
sonication method. The method issimple rapid,
reproducible and involves gentle handling of
unstable materials. The resulting liposomes
are somewhat larger than sonicated SUVs.
The drawbacks of the method are that the
temperature is difficult to achieve and the
working volumes are relatively small (about 50
mL maximum).
ISSN: 22312781
These conditions may possibly result in the
denaturation of some proteins or breakage of
DNA strands. We get a heterogeneous sized
dispersion of vesicles by this method. Modified
Reverse Phase Evaporation Method was
presented and the main advantage of the
method is that the liposomes had high
encapsulation efficiency (about 80%). The
Reverse Phase Evaporation has also been
modified to entrap plasmids without damaging
DNA strands.
C) Large Unilamellar Liposomes (LUV)
They have high internal volume/encapsulation
efficiency and are now days being used for the
encapsulation of drugs and macromolecules.
1. Solvent Injection Methods
30
a) Ether Infusion Method
A solution of lipids dissolved in diethyl ether or
ether/methanol mixture is slowly injected to an
aqueous solution of the material to be
encapsulated at 55-65C or under reduced
pressure. The subsequent removal of ether
under vacuum leads to the formation of
liposomes. The main drawbacks of the method
are that the population is heterogeneous (70190 nm) and the exposure of compounds to be
encapsulated to organic solvents or high
temperature.
d) Calcium-Induced Fusion Method35
This method is used to prepare LUV from
acidic phospholipids. The procedure is based
on the observation that calcium addition to
SUV induces fusion and results in the
formation of multilamellar structures in spiral
configuration (Cochleate cylinders). The
addition of EDTA to these preparations results
in the formation of LUVs. The main advantage
of this method is that macromolecules can he
encapsulated under gentle conditions. The
resulting liposomes are largely unilamellar,
although of a heterogeneous size range. The
chief disadvantage of this method is that LUVs
can
only
be
obtained
from
acidic
phospholipids.
b) Ethanol Injection Method31
A lipid solution of ethanol is rapidly injected to
a vast excess of buffer. The MLVs are
immediately formed. The drawbacks of the
method are that
the
population is
heterogeneous (30-110 nm), liposomes are
very dilute, it is difficult to remove all ethanol
because it forms azeotrope with water and the
possibility of various biologically active
macromolecules to inactivation in the presence
of even low amounts of ethanol.
e) Freeze-Thaw Method37
SUVs are rapidly frozen and followed by slow
thawing. The brief sonication disperses
aggregated materials to LUV. The formation of
unilamellar vesicles is due to the fusion of SUV
during the processes of freezing and
orthawing. This type of fusion is strongly
inhibited by increasing the ionic strength of the
medium and by increasing the phospholipid
concentration. The encapsulation efficiencies
from 20 to 30% were obtained.
32-34
38
c) Reserves Phase Evaporation Method
First water in oil emulsion is formed by brief
sonication of a two phase system containing
phospholipids in organic solvent (diethylether
or isopropylether or mixture of isopropyl ether
and chloroform) and aqueous buffer. The
organic solvents are removed under reduced
pressure, resulting in the formation of a
viscous gel. The liposomes are formed when
residual solvent is removed by continued
rotary evaporation under reduced pressure.
With this method high encapsulation efficiency
up to 65% can be obtained in a medium of low
ionic strength for example 0.01 M NaCl. The
method has been used toencapsulate small,
large and macromolecules. The main
disadvantage of the method is the exposure of
the materials to be encapsulated to organic
solvents and to brief periods of sonication.
(D) Giant Liposomes
(i) The procedure for the formation of giant
liposomes involves the dialysis, of a methanol
solution of phosphatidylcholine in the presence
of methylglucoside detergent against an
aqueous solution containing up to 1 M NaCl.
The liposomes range in diameter from 10 to
100 mm.
39
Preparation of Liposomal Gel
Gel was prepared using carbopol 934NF (1,
1.5 and 2%). The appropriate quantity of
carbopol 934 powder was dispersed into
distilled water under constant stirring with a
glass rod, taking care to avoid the formation of
indispersible lumps and allowed to hydrate for
24 h at room temperature for swelling. Topical
liposome gel formulations were prepared by
incorporation of liposome's containing drug
385
Nikhil et al
IJRPC 2012, 2(2)
(separated from the unentrapped drug) were
mixed into the carbopol gel with a mechanical
stirrer (25 rpm, 2 m). The dispersion was
neutralized using triethanolamine (0.5% w/w).
Control gels were made under the same
conditions.
ISSN: 22312781
Skin was excised from rat with scalpel and
fattylayer was removed by keeping the skin in
warm water at 60c. After 2 m, fatty layer was
peeled off gently and skinwas washed with
water and kept for saturation inphosphate
buffer saline pH 7.4 for about 30 m before
itwas used for permeation studies. Fresh skin
was usedevery time. Skin permeation studies
with drug containing liposome formulations
were carried out usingabdominal rat skin,
employing modified Franz-diffusion cells. The
results obtained were compared with that
ofnon-liposomal formulations of drug. The skin
wasprepared by mounting on the receptor
2
chamber withcross-sectional area of 3.91 cm
exposed to the receptorcompartment. The
receptor compartment was filled with(22 ml)
phosphate buffer pH 7.4. It was jacketed to
maintain the temperature 37 + 0.5C and was
kept stirring at 50 rpm. Prior to application of
formulations, the skin was allowed to
equilibrate at this condition for 1 h. Liposomal
or
non-liposomal
formulation
(amount
equivalent to 5 mg of drug) was applied
uniformly on the dorsal side of skin. Aliquots of
2 ml were withdrawn periodically and replaced
with same amount of saline solution to
maintain the receptor phase volume at a
constant level. The samples were quantified
spectrophotometrically. For determination of
drug deposited in skin, cell was dismantled
after a period of 8 h and skin was carefully
removed from the cell. The formulation applied
on skin surface was swabbed first with
phosphate buffer pH 7.4 and then with
methanol. The procedure was repeated twice
to ensure no traces of formulation are left onto
skin surface. The skin was then cutinto small
pieces and drug present in skin was extracted
in phosphate buffer pH 7.4
Chracterization of Topical Liposomal
Formulation
40
Size distribution
Prepared liposomal batches were monitored
for their morphological attributes using optical
microscope. Mean vesicle size and size
distribution profile of liposome was determined
by using Malvern particle size analyzer model
SM 2000, which follows Mie's theory of light
scattering. Diluted liposome suspension was
added to the sample dispersion unit containing
stirrer and stirredat 2000 rpm in order to
reduce the interparticle aggregation, and laser
obscuration range was maintained between
10-20%. The average particle size was
measured after performing the experiment in
triplicate.
41
Entrapment efficiency
Drug associated with liposome was separated
from unentrapped drug using centrifugation
method. Liposomes were centrifuged at 20000
rpm for 1 h at controlled temperature of 4 C.
Supernatant containing unentrapped drug was
withdrawn
and
measured
UV
spectrophotometrically against phosphate
buffer saline (pH 7.4). The amount of drug
entrapped in liposome was determined as
follow
EE (%) = [(CdCf )/Cd] 100
Where Cd is concentration detected of total
f
drug and C is concentration of free drug. The
entrapment efficiency was obtained by
repeating the experiment in triplicate and the
values were expressed as mean standard
deviation.
43,44
Rheological studies
While considering the stable liposome
dispersion or any other delivery system they
usually need to beincorporated into convenient
dosage for to obtainformulation with desired
semisolid consistency for easein topical and
transdermal application. It is important
andcontrols the flow properties to ensure
product quality andeffectiveness of the
production. It helps in selection of
dermatological formulation that will progress to
clinical efficacy. In present study liposomal
gels were prepared using carbopol 934 as
gelling agent. Rheological analysis of liposome
loaded carbopol gels were performed using a
stress
control
rheometer
(Viscotech
Rheometer , Rheological Instruments AB,
Lund, Sweden), equipped with stress rheologic
basic software, version 5, using cone-plate
Zeta potential (z) determination42
Charge on empty and drug loaded vesicles
surface was determined using Zetasizer
300HSA (Malvern Instruments, Malvern, UK).
Analysis time was kept for 60 s and average
zeta potential and charge on the liposome was
determined.
Skin permeation and drug deposition
studies
Rat was sacrificed by exposing to excess
chloroform. Tothe abdominal skin, depilatory
(Anne French, India) wasapplied and kept for
10 m to remove the hair from theskin. After 10
m of application, skin was washed withwater.
386
Nikhil et al
IJRPC 2012, 2(2)
geometry with a diameter of the cone being 25
mm and a cone angle of 10, operating in the
oscillation and static mode. Rheological
analysis was performed at room temperature.
The following parameters were carried out for
rheology measurement.
ISSN: 22312781
and analysed for the drug content and particle
size for liposomal suspension and drug
deposition for liposomal gel in the manner
described under entrapment efficiency and
particle size distribution studies.
Drug Criteria for Topical Liposomal Drug
Delivery System
Which
groups of
substances are considered to be especially
interesting for liposomal encapsulation in
49,50
the field of dermatology?
1. There are drugs which are known to have
severe side-effects by the conventional
way of topical administration, e.g.
topicalglucocorticosteroids.
2. There are substances which normally are
effective by systemic application but not by
topical application, e.g. interferon.
3. There are drugs which only show
insufficient effects when applied topically.
E.g. hamamelis distillate.
45,46
Oscillation stress sweep
Dynamic oscillation stress sweep was
performed to determine the linear viscoelastic
region (LVR). LVR is the region where the
elastic modulus (G') was independent of
applied stress because destruction in
thestructure of gels occurs at high shear
stress. Analysis of viscoelastic material was
designed not to destroy the structure so that
measurement can provide the information
about intermolecular and interparticle forces in
the material. This test gives idea about the
critical stress beyond which the sample may
show significant structural changes, and
therefore the consequent choice of the stress
value to be used in other in other oscillation
tests. The samples were exposed to
increasing stress (0.5 to 150 Pa) at a constant
frequency of 0.1 Hz. The three main
parameters determined in this test were the
storage modulus G', loss modulus G and loss
tangent tan! The end point of the linear
viscoelastic region was determined as a
stress, when the G' value was dropped 10%
from the linear level that indicated a significant
change in the structure gel samples.
Marketed
Formulation
51
Liposome
of
Topical
a) Celadrin
1. Celadrin Topical Liposome Lotion- 4 oz.
2. Celadrin is a registered trademark of
Imagenetix, Inc.
b) Optisome
TM
Encapsulated Tetracaine.
TM
c) Lipo C Liposome -encapsulated Active
Vitamin C with Vitamin E and Zinc.
47
Oscillation frequency sweep
The samples were exposed to stepwise
increasing frequency (0.1 to 100 Hz) at a
constant stress in the field of LVR and elastic
moduli (G') as well as viscous modulus (G?)
were recorded against frequency.
d) Lipo-Gest Natural Balancing Cream
e) Liposome progesterone based cream.
CONCLUSION
Generally speaking Liposomes have some
advantages which make them look interesting
as drug carriers for topically applied drugs.
First, they are variable concerning size and
surface properties and Second, They can act
as sustained release depots, releasing
encapsulated drugs of half-lives ranging from
0.6 to 11 days. Moreover a new generation of
liposomes, the so-called collagen modified
liposomes can moderate the liposomeliposome and the liposome-cell interaction due
to their collagen surface properties. This
indeed might mean a greater possibility to
control the drug release. The topically applied
liposomal formulations, particularly those
prepared from lipid mixtures of composition
similar to the stratum corneum, would be an
effective delivery system for the treatment of
skin diseases. Since these liposomal
formulations provide sustained, enhanced
Drug content and content uniformity
The gel sample (100 mg) was withdrawn and
drug content was determined using UV
spectrophotometer. Similarly, the content
uniformity was determined by analyzing drug
Concentration in gel taken from 3 to 4 different
pointsfrom the container. In case of liposomal
gel, it was shaken with sufficient quantity of
methanol to extract the drug and then
analysed by using UV spectrophotometer.
Stability studies48
The ability of vesicles to retain the drug (i.e.,
drug retentive behaviour) was assessed by
keeping the liposomal suspensions and
liposomal gel at two different temperature
conditions, i.e., 4-8 C (Refrigerator; RF), 252
C (Room temperature; RT), for a period of 60
days. Samples were withdrawn periodically
387
Nikhil et al
IJRPC 2012, 2(2)
levels in deeper strata of the skin,they have
the capacity to meter a sufficient quantity of
drug into deeper tissue to treat the skin
symptomology. Such metering should also
ISSN: 22312781
reduce the incidence of undesirable side
effects arising from systemic administration, or
enhanced systemic absorption of drug.
Fig. 1: Structure of Liposomes
Fig. 2: Lipid Film Hydration Method
388
IJRPC 2012, 2(2)
Nikhil et al
ISSN: 22312781
Fig. 3:
REFRENCES
1. Arcadio Chonn and Pieter R Cullis.
Recent advances in liposomal drugdelivery systems year 1995;6:698-795.
2. A. Chonn, R. P. Cullis, Recent
advances in liposomal drug-delivery
systems,
Current
Opinion
in
Biotechnology, 6, 698708 (1995).
3. I. P. Kaur, A. Garg, A. K. Singla, D.
Aggarwal, Vesicular systems in ocular
drug delivery: an overview, Int.
J.Pharm., 269, 114 (2004).
4. M. Fresta, G. Puglisi, Application of
liposomes as potential cutaneous drug
delivery systems: in vitro and in vivo
investigation with radioactively labelled
vesicles, J. Drug Target., 4, 95101
(1996).
5. D. D. Lasic, Novel application of
liposomes, Trends Biotechnol., 16,
307321 (1998).
6. D.D. Lasic, Novel application of
liposomes. Tibtech, 1998, 16: 8-17
7. D.W. Osborne, A.H. Anann, Topical
Drug Delivery formulations, Marcel
Dekker Inc. 42, 468-477.
8. G. Storm, D. J. A. crommelin;
Liposomes: quo vadis
Research
focus. 1998; PSTT, 1, 1: 19-31.
9. Encyclopaedia of controlled release,
1: 461-485.
10. A.D. Sezer, A.L. Bas, and J. Akbuga
et al. Encapsulation of Enrofloxacin in
Liposomes I: Preparation and in vitro
characterization of LUV, J. Lipo. Res.,
2004, 14, 1 & 2: 77-86.
11. S.L. Law, K.J. Huang, V.H.Y. Chou, et
al. Stability of Desmopressin loaded in
Liposomes; J. Lipo. Res., 2003. 13, 3
& 4: 269277.
12. Schaeffer HE, Krohn DL. Liposomes in
topical
drug
delivery.
Invest.
13.
14.
15.
16.
17.
18.
19.
20.
389
Ophthalmol. Vis. Sci. 1982; 22:220227.
Mohamed MN. In vitro release of
hydrophilic and hydrophobic drugs
from liposomal dispersions and gels.
Act. Pharm. 2006; 56:311-324.
Kneep VM, Hinz RS, Szoka FSJr, Guy
RH.Controlled drug release from a
novel liposomal Delivery system I:
investigation of transdermal potential.
J. Control. Rel. 1988; 5:211-221.
Schmid MH, Korting HC. Therapeutic
progress with topical liposome drugs
for skin Disease. Adv. Drug Del. Rev.
1996; 18:335-342.
Barry BW. Novel mechanisms and
devices
to
enable
successful
transdermal drug Delivery. Eur J
Pharm Sci. 14: 10114(2001).
Cevc G. Lipid vesicles and other
colloids as drug carriers on the skin.
Adv Drug Deliv Rev. 56: 675711
(2004).
El Maghraby GM, Barry BW, Williams
AC. Liposomes and skin: From drug
delivery to model membranes. Eur J
pharm sci. 34: 20322(2008).
Grace J.Lim, Yozo Ishiuji, Aerlyn
Dawn, Benjamin Harrison, Do won
Kim, Anthony Atala, and Gil
Yosopovithch. In vitro and In vivo
Characterization of a Novel Liposomal
Butorphanol
Formulation
for
Treatment of Pruritus. Acta Derm
Venereol. 88: 327330 (2008).
Esposito E, Zanella C, Cortesi R,
Menegatti E, Nastruzzi C. Influence of
liposomal formulation parameters on
the in vitro absorption of methyl
nicotinate. Int J Pharm. 172: 25560
(1998).
IJRPC 2012, 2(2)
Nikhil et al
21. Shan-shan,
Qing
Du,
De-Ying
Cao.Preparation
of
liposomal
fluconazole gel and invitro transdermal
delivery. J Chinese Pharma Sci.
16:116-118 (2007).
22. Zeljka Pavelic, Natasa Skalko-Basnet,
Rolf Schubert. Liposomal gels for
vaginal drug delivery, Int J Pharm. 19:
139-149 (2001).
23. Zeljka Pavelc, Natasa Skalko Basnet,
Ivan Jalsenjak. Liposomal gel with
chloramphenicol: Characterisation and
in vitro release. Acta Pharm. 54: 319
330 (2004).
24. Beukelman CJ, van den Berg AJJ,
Hoekstra MJ, Uhl R, Reimer K,
Mueller
S.
Anti-inflammatory
properties of a liposomal hydrogel with
povidone-iodine (Repithel) for wound
healing in vitro, Burns. 34: 845-55
(2008).
25. Target and Controlled drug delivery
system chapter-5 by S.P Vyas and
R.K Khar.
26. Bangham A.D., Standish M.M. and
Watlins J.C. (1965). J. Mol. Biol. 13:
238.
27. Kim S., Turker M.S., Chi E.Y., Scla S.
and Martin G.M. (1983). Biochim.
Biophys. Acta. 728: 339.
28. Oezden M.Y. and Hasirci V.N. (1991).
Biochim. Biophys. Acta. 1075: 102.
29. Hamilton R.L. and Guo L.S.S. (1984).
In: Liposome Technology (Gregoriadis
G. ed.) CRC Press, Florida, Vol.1,
Chapter 4, p.37.
30. Deamer D. and Bangham A.D. (1976).
Biochim. Biophys. Acta. 443: 629.
31. Batzri S. and Korn E.D. (1973).
Biochim. Biophy. Acta. 298: 1015.
32. Szoka F. Jr. and Papahadjopoulos D.
(1978). Proc. Natl. Acad. Sci. USA. 75:
4194.
33. Handa T., Takeuchi H., Phokubo Y.
and Kawashima Y. (1987). Chem.
Pharm. Bull. 35: 748.
34. Naga N. and Yagi K. (1989). J. Clin.
Biochem. Nut,. 7: 175.
35. Papahadjopoulos D. and Vail W.J.
(1978). Ann. N.Y. Acad. Sci. 308: 259.
36. Pick U. (1981). Arch. Biochem.
Biophys. 212: 186.
37. Liu L. and Yonetaini T. (1994). J.
Microencapsulation. 11: 409.
38. Oku N., Scheerer J.F. and McDonald
R.C. (1982). Biochim. Biophys. Acta.
692: 384.
39. Pavelic Z. Liposomal gel with
chloramphenicol: characterization and
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
390
ISSN: 22312781
invitro release. Act. Pharm 2004;
54:319-330.
Du Plessis J, Ramchandran C, Weiner
N, Muller DG. The influence of particle
size of liposomes on the deposition of
drug into skin. Int. J. Pharm. 1994;
103:277-282.
Jia-You F, Yann-Lii L, Chia-Chun C,
Chia-Hsuan L, Yi-Hung T. Lipid
nano/submicron emulsion as vehicle
for topical flurbiprofen delivery. Drug
Del. 2004;11:97-105.
B.V Mitakari et al formulation and
evaluation of topical liposomal gel for
fluconazole Indian J.Pharm. Educ.
Res. 44(4), Oct - Dec, 2010.
Bayarri S, Duran L, Costell E.
Influence of sweetener on the
viscoelasticity of hydrocolloids gelled
systems. Food Hydrocolloids. 2004;
18:611- 619.
Calfors J, Edsman K, Petterson R.
Rheological evaluation of gelrite in situ
gels for ophthalmic use. Eur. J.
Pharm. Sci. 1998;6:113-119.
Kobayashi M, Ishikawa S, Samejima
M. Application of nonlinear viscoelastic
analysis by the oscillation method to
some pharmaceutical ointments in the
Japanese
Pharmacopeia.
Chem.
Pharm. Bull. 1982;30:4468-4478.
Thorgeirsdottira T, Kjoniksenb A,
Kenneth DK, Kristmundsdottira T,
Nystromb
B.
Viscoelastic
and
structural properties of pharmaceutical
hydrogels containing monocaprin. Eur.
J. Pharm. Biopharm. 2005; 59:333342.
Torres LG, Iturbe R, Snowdenb MJ,
Chowdhry
BZ,
Leharne
SA.
Preparation of o/w emulsions tabilized
by
solid
particles
and
their
characterization
by
oscillatory
rheology. Colloid Surfac. 2007;
302:439-448.
Goindi S, Aggarwal N. Preparation of
hydrogels of griseofulvin for dermal
application. Int. J. Pharm. 2006;
326:20-24.
Schmid MH and Korting HC.
Therapeutic progress with topical
liposome drugs for skin Disease.
Advanced Drug Delivery Reviews.
1996; 18:335-342.
Korting HC, Zienicke H, SchaferKorting M and Braun F. Liposome
encapsulation improves effcacy of
betamethasone dipropionate in atopic
eczema
but
not
in
psoriasis
IJRPC 2012, 2(2)
Nikhil et al
vulgaris.European Journal of Clinical
Pharmacology. 1991; 29:349-352.
51. Patel Meghana C et al Liposomes as a
topical
drug
delivery
system
international journal of pharmaceutical
and chemical sciences Vol. 1 (1) Jan
Mar 2012,
391
ISSN: 22312781
También podría gustarte
- RPh's Guide to Drug IncompatibilitiesDocumento27 páginasRPh's Guide to Drug IncompatibilitiesArk Olfato Parojinog100% (1)
- PST 04104 Pharmaceutical Dosage FormsDocumento17 páginasPST 04104 Pharmaceutical Dosage FormsambroceAún no hay calificaciones
- Vasquez, Julianne Gabrielle G. Pharmacology BSN 2-A-7 Course Task #1Documento6 páginasVasquez, Julianne Gabrielle G. Pharmacology BSN 2-A-7 Course Task #1PagodAún no hay calificaciones
- Formulation and Evaluation of Ketoconazole NiosomaDocumento7 páginasFormulation and Evaluation of Ketoconazole NiosomaKevin Nauval KarimAún no hay calificaciones
- Proniosomes Novel DdsDocumento11 páginasProniosomes Novel DdsArun DavesarAún no hay calificaciones
- NOVEL DRUG DELIVERY SYSTEMSDocumento20 páginasNOVEL DRUG DELIVERY SYSTEMSZainab ArshadAún no hay calificaciones
- Novel Drug Delivery SystemDocumento20 páginasNovel Drug Delivery SystemZainab ArshadAún no hay calificaciones
- Solid Lipid Nanoparticles 2Documento22 páginasSolid Lipid Nanoparticles 2هدي أبوعجورAún no hay calificaciones
- My Project ETHOSOMESDocumento26 páginasMy Project ETHOSOMESHaleema SultanAún no hay calificaciones
- Liposomes Drug Delivery 2013 KaurDocumento8 páginasLiposomes Drug Delivery 2013 Kaurnidus14Aún no hay calificaciones
- Semisolid Dosage Form: Contributed by Sanjay J DaharwalDocumento7 páginasSemisolid Dosage Form: Contributed by Sanjay J DaharwalMSKCAún no hay calificaciones
- 7-JBS3812Documento10 páginas7-JBS3812penjurisubhashAún no hay calificaciones
- Transfersomes for Transdermal Drug DeliveryDocumento5 páginasTransfersomes for Transdermal Drug DeliveryElla Masliana DewiAún no hay calificaciones
- Transfersomes for enhanced transdermal drug deliveryDocumento29 páginasTransfersomes for enhanced transdermal drug deliverySyedmohd SaimAún no hay calificaciones
- Microsponge Delivery System: Vikrant Chadawar and Jessy ShajiDocumento8 páginasMicrosponge Delivery System: Vikrant Chadawar and Jessy ShajiFatima MadrasAún no hay calificaciones
- Liposome Preparation Methods ReviewDocumento13 páginasLiposome Preparation Methods ReviewAshish GajeraAún no hay calificaciones
- Liposomes as Drug Delivery ReviewDocumento14 páginasLiposomes as Drug Delivery ReviewLeenusAún no hay calificaciones
- Emulgel ThisisDocumento11 páginasEmulgel ThisisVivek Patel Viks100% (1)
- Semisolid Dosage FormDocumento9 páginasSemisolid Dosage Formsayid saidAún no hay calificaciones
- Emulgel A ReviewDocumento11 páginasEmulgel A ReviewariAún no hay calificaciones
- Jurnal MikrospongeDocumento11 páginasJurnal MikrospongeMuthoh HaroAún no hay calificaciones
- Final Project 29-04-2010Documento38 páginasFinal Project 29-04-2010DRx Anuj ChauhanAún no hay calificaciones
- Nanoemulgel A Novel Nano Carrier As A Tool For TopDocumento28 páginasNanoemulgel A Novel Nano Carrier As A Tool For TopAdindaAún no hay calificaciones
- Liposome Assisted Drug Deliveryan Updated ReviewDocumento15 páginasLiposome Assisted Drug Deliveryan Updated ReviewvinayAún no hay calificaciones
- Transfersomes: New Dominants For Transdermal Drug Delivery: January 2012Documento22 páginasTransfersomes: New Dominants For Transdermal Drug Delivery: January 2012vallentpangalaAún no hay calificaciones
- Liposomes A Review of Manufacturing Techniques and Targeting StrategiesDocumento18 páginasLiposomes A Review of Manufacturing Techniques and Targeting StrategiesIrini Fountouli - LadopoulouAún no hay calificaciones
- Advantages of Pulmonary Drug DeliveryDocumento5 páginasAdvantages of Pulmonary Drug DeliveryYousab MKAún no hay calificaciones
- Microsponges: A Novel Strategy For Drug Delivery SystemDocumento14 páginasMicrosponges: A Novel Strategy For Drug Delivery Systemmunishahuja17Aún no hay calificaciones
- Lecture 1 Nanocosmetics PDFDocumento39 páginasLecture 1 Nanocosmetics PDFNura SadanyAún no hay calificaciones
- NDDSDocumento20 páginasNDDSAnonymous u5ICt3gLqLAún no hay calificaciones
- A Review On Liposomal Drug Delivery SystemDocumento9 páginasA Review On Liposomal Drug Delivery SystemInternational Journal of Innovative Science and Research TechnologyAún no hay calificaciones
- Oral Lipid Based DDSDocumento16 páginasOral Lipid Based DDSDyah Ayu NAún no hay calificaciones
- Lipozimi PDFDocumento9 páginasLipozimi PDFValentina PuiuAún no hay calificaciones
- Mucoadhesive Drug Delivery System - Project PaperDocumento43 páginasMucoadhesive Drug Delivery System - Project Papershafi_jp100% (1)
- Encapsulation PPT AkashDocumento18 páginasEncapsulation PPT AkashAkash PandayAún no hay calificaciones
- s2 The Role of Liposomes in Drug Delivery and Diagnostic Imaging 2003Documento8 páginass2 The Role of Liposomes in Drug Delivery and Diagnostic Imaging 2003Mirna MustapićAún no hay calificaciones
- Liposomes: Advantages of LiposomeDocumento9 páginasLiposomes: Advantages of LiposomeRavirajsinh GohilAún no hay calificaciones
- Abdul Muheem: - DR - Zeenat Iqbal - DR - Sushama Talegaonkar - DR - Yasmin SultanaDocumento34 páginasAbdul Muheem: - DR - Zeenat Iqbal - DR - Sushama Talegaonkar - DR - Yasmin SultanafaysalAún no hay calificaciones
- Emerging Trend of Microemulsion in PDFDocumento30 páginasEmerging Trend of Microemulsion in PDFrahmiadelianiAún no hay calificaciones
- Ijpab 2015 3 1 224 235 PDFDocumento12 páginasIjpab 2015 3 1 224 235 PDFDrAmit VermaAún no hay calificaciones
- AshishDocumento6 páginasAshishBaru Chandrasekhar RaoAún no hay calificaciones
- BuccalDocumento25 páginasBuccalAnushree pattajeAún no hay calificaciones
- Emulgel PreparationDocumento6 páginasEmulgel Preparationfirda rydAún no hay calificaciones
- LunguDocumento21 páginasLungutriagung setyoutomoAún no hay calificaciones
- JDD2011-591325 Metodos de ObtencionDocumento9 páginasJDD2011-591325 Metodos de ObtencionJose Carlos Solis SuarezAún no hay calificaciones
- Recent Advances in SemisolidsDocumento11 páginasRecent Advances in SemisolidsRajuAún no hay calificaciones
- 14 Nanostructure Lipid Carrier NLC The New Generation of Lipid NanoparticlesDocumento18 páginas14 Nanostructure Lipid Carrier NLC The New Generation of Lipid NanoparticlesRizqi ChairunnisaAún no hay calificaciones
- Noval Drug Delivery SystemDocumento82 páginasNoval Drug Delivery Systemzubairalam9720738045Aún no hay calificaciones
- Absorption of Drug From Non-Per Oral RoutesDocumento32 páginasAbsorption of Drug From Non-Per Oral Routesumamaheshwari33Aún no hay calificaciones
- LIPOSOMESDocumento53 páginasLIPOSOMESAlicia GarciaAún no hay calificaciones
- Semisolid Dosage FormDocumento12 páginasSemisolid Dosage Formdhananjay taumarAún no hay calificaciones
- Article 4 April June 2012Documento7 páginasArticle 4 April June 2012Sharn GillAún no hay calificaciones
- MicrospheresDocumento72 páginasMicrospheresTejas PatelAún no hay calificaciones
- Liposomes in Drug Delivery: A ReviewDocumento5 páginasLiposomes in Drug Delivery: A ReviewJuliaNofadiniAún no hay calificaciones
- Ocular Drug Delivery and PermeablityDocumento63 páginasOcular Drug Delivery and PermeablityDr AYAL TILAHUN MIHIRETIEAún no hay calificaciones
- Topical Dosage FormsDocumento19 páginasTopical Dosage FormscseoukienandanAún no hay calificaciones
- Nanoemulsions and Dermatological Diseases: Contributions and Therapeutic AdvancesDocumento7 páginasNanoemulsions and Dermatological Diseases: Contributions and Therapeutic AdvancesliliAún no hay calificaciones
- Wa0010Documento9 páginasWa0010Anonymous u8BdtFlAún no hay calificaciones
- Nanoemulgel 2Documento7 páginasNanoemulgel 2AdindaAún no hay calificaciones
- NANOTECHNOLOGY REVIEW: LIPOSOMES, NANOTUBES & PLGA NANOPARTICLESDe EverandNANOTECHNOLOGY REVIEW: LIPOSOMES, NANOTUBES & PLGA NANOPARTICLESAún no hay calificaciones
- Parenteral Products: The Preparation and Quality Control of Products for InjectionDe EverandParenteral Products: The Preparation and Quality Control of Products for InjectionAún no hay calificaciones
- Microneedle-mediated Transdermal and Intradermal Drug DeliveryDe EverandMicroneedle-mediated Transdermal and Intradermal Drug DeliveryAún no hay calificaciones
- Lagu AnakDocumento7 páginasLagu AnakTreesna OuwpolyAún no hay calificaciones
- Lagu AnakDocumento7 páginasLagu AnakTreesna OuwpolyAún no hay calificaciones
- Topical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFDocumento9 páginasTopical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFTreesna OuwpolyAún no hay calificaciones
- Topical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFDocumento9 páginasTopical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFTreesna OuwpolyAún no hay calificaciones
- Garuda Indonesia: Electronic Ticket ReceiptDocumento2 páginasGaruda Indonesia: Electronic Ticket ReceiptTreesna OuwpolyAún no hay calificaciones
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocumento8 páginasFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyAún no hay calificaciones
- HttpsDocumento1 páginaHttpsTreesna OuwpolyAún no hay calificaciones
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocumento8 páginasFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyAún no hay calificaciones
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocumento8 páginasFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyAún no hay calificaciones
- Topical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFDocumento9 páginasTopical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFTreesna OuwpolyAún no hay calificaciones
- Topical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFDocumento9 páginasTopical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFTreesna OuwpolyAún no hay calificaciones
- Topical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFDocumento9 páginasTopical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFTreesna OuwpolyAún no hay calificaciones
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocumento8 páginasFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyAún no hay calificaciones
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocumento8 páginasFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyAún no hay calificaciones
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocumento8 páginasFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyAún no hay calificaciones
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocumento8 páginasFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyAún no hay calificaciones
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocumento8 páginasFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyAún no hay calificaciones
- Topical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFDocumento9 páginasTopical Liposomal Gel A Novel Drug Delivery System (Kelompok V) PDFTreesna OuwpolyAún no hay calificaciones
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocumento8 páginasFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyAún no hay calificaciones
- Notes in PharmacologyDocumento96 páginasNotes in Pharmacologydmd_2dd50% (2)
- Shankar SwaminathanDocumento22 páginasShankar SwaminathanSurendar KesavanAún no hay calificaciones
- Product List W.E.F 01-01-2020 Tablets and CapsulesDocumento11 páginasProduct List W.E.F 01-01-2020 Tablets and CapsulesAmit BajpaiAún no hay calificaciones
- Design and Development of Ciclopirox Topical Nanoemulsion Gel For TheDocumento9 páginasDesign and Development of Ciclopirox Topical Nanoemulsion Gel For TheVenu Gopal NAún no hay calificaciones
- Public Assessment Report Scientific DiscussionDocumento8 páginasPublic Assessment Report Scientific Discussionlhthang1990Aún no hay calificaciones
- SemisolidDocumento17 páginasSemisolidzxvcazcfAún no hay calificaciones
- Seborrheic Dermatitis of The Scalp Etiology and TreatmentDocumento9 páginasSeborrheic Dermatitis of The Scalp Etiology and TreatmentAndi WahyuniAún no hay calificaciones
- Peritonitis GuiaDocumento28 páginasPeritonitis GuiaAndrea ClaudieAún no hay calificaciones
- Ludura Lulitec CreamDocumento1 páginaLudura Lulitec CreamGaurav NAún no hay calificaciones
- Egyptian OTC Drug ListDocumento6 páginasEgyptian OTC Drug ListDr HbAún no hay calificaciones
- Otomycosis: Yan Edward, Dolly IrfandyDocumento6 páginasOtomycosis: Yan Edward, Dolly IrfandyM Reza Kurnia AliAún no hay calificaciones
- About Darier's DiseaseDocumento5 páginasAbout Darier's DiseaseJuli SalgadoAún no hay calificaciones
- Pharmacology PDFDocumento109 páginasPharmacology PDFRanjit TharuAún no hay calificaciones
- 250 mcg = 0.250 mgStep 2: Determine the number of tabs needed. Each tab is 0.125 mg. To determine the number of tabs, divide the total dose by the dose per tabDocumento40 páginas250 mcg = 0.250 mgStep 2: Determine the number of tabs needed. Each tab is 0.125 mg. To determine the number of tabs, divide the total dose by the dose per tabAlison Gifford100% (1)
- Eczema HomeopathyDocumento4 páginasEczema Homeopathyruhul72Aún no hay calificaciones
- S102RA01Documento15 páginasS102RA01David LeeAún no hay calificaciones
- Dermatological DrugsDocumento46 páginasDermatological DrugsJai MurugeshAún no hay calificaciones
- 1 Intro To Pharmacology 2023Documento63 páginas1 Intro To Pharmacology 2023Hussain RazaAún no hay calificaciones
- TCL1 de 1Documento294 páginasTCL1 de 1Alvarin CsboyAún no hay calificaciones
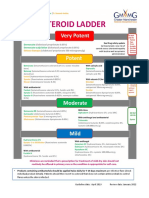
- GM Steroid LadderDocumento2 páginasGM Steroid LadderRenee McGuinnessAún no hay calificaciones
- Medicinal Plants & Extracts ITC Quarterly Report 2012Documento77 páginasMedicinal Plants & Extracts ITC Quarterly Report 2012didier1701Aún no hay calificaciones
- CCID 84765 Salicylic Acid As A Peeling Agent A Comprehensive Review - 082615Documento8 páginasCCID 84765 Salicylic Acid As A Peeling Agent A Comprehensive Review - 082615Wisnu Pangarso WibowoAún no hay calificaciones
- Balanitis UpdatesDocumento22 páginasBalanitis UpdatesUshal VeeriahAún no hay calificaciones
- Steroids PDFDocumento35 páginasSteroids PDFPratyusha VallamAún no hay calificaciones
- BioStine Hydroxide-GSA Powerpoint (En)Documento26 páginasBioStine Hydroxide-GSA Powerpoint (En)masumi.rndAún no hay calificaciones
- Dermovate™ 0.05% W/W Ointment: Package Leaflet: Information For The UserDocumento6 páginasDermovate™ 0.05% W/W Ointment: Package Leaflet: Information For The UsermahardiantooAún no hay calificaciones
- Pharmaceutical Standardization of Panchaguna Taila (Medicated Oil) .....Documento6 páginasPharmaceutical Standardization of Panchaguna Taila (Medicated Oil) .....Anonymous pqtS3tcu1Aún no hay calificaciones