Documentos de Académico
Documentos de Profesional
Documentos de Cultura
tmp95F5 TMP
Cargado por
FrontiersDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
tmp95F5 TMP
Cargado por
FrontiersCopyright:
Formatos disponibles
Malaysian J Pathol 2013; 35(1) : 71 76
ORIGINAL ARTICLE
Review of patients with Strongyloides stercoralis infestation in a
tertiary teaching hospital, Kelantan
AZIRA NMS,*,**ABDEL RAHMAN MZ* and ZEEHAIDA M*
*Department of Medical Microbiology and Parasitology, Universiti Sains Malaysia, and **Cluster of
Pathology and Laboratory Medicine, Faculty of Medicine, Universiti Teknologi Mara, Malaysia.
Abstract
Strongyloides stercoralis is an intestinal nematode infecting humans. The actual prevalence of
infestation with this parasite in our setting is not well established. Thus, this study was conducted
to determine the age, sex and co-morbid conditions among patients with S. stercoralis infestation as
well as to study the common manifestations of strongyloidiasis in our patients. Records of patients
with positive S. stercoralis larvae from January 2000 to December 2012 in Hospital Universiti Sains
Malaysia, Kubang Kerian, Kelantan were reviewed. Ten patients were male and two were female.
Their ages ranged from 19 to 78 years old. The majority (92%) of cases, presented with intestinal
symptoms and 50% with moderate to severe anaemia. Thirty percent of cases had extraintestinal
manifestations such as cough, sepsis and pleural effusion. Ninety-two percent of the patients had
a comorbid illness. Most patients were immunocompromised, with underlying diabetes mellitus,
retroviral disease, lymphoma and steroid therapy contributing to about 58% of cases. Only 58%
were treated with anti-helminthic drugs. Strongyloidiasis is present in our local setting, though the
prevalence could be underestimated.
Key words: Strongyloides stercoralis, diarrhoea, abdominal discomfort
INTRODUCTION
Strongyloides stercoralis is a widespread, soiltransmitted intestinal helminth, which infects
millions of people worldwide.1 It was first
described in 1876 from stool specimens obtained
from soldiers who had returned from Vietnam and
were suffering from severe diarrhoea and other
gastrointestinal symptoms.2 Human infection
occurs in endemic areas when the infective
filariform larvae in contaminated soil actively
penetrate the intact skin of the feet sole or hand
palm; or the rhabditiform larva are ingested
with contaminated food.3 Low socioeconomic
backgrounds and habits that facilitate parasitic
transmission are known to be the major risk
factors for acquiring the primary infection.2,4
The disease is generally asymptomatic in an
immunocompetent person. It commonly manifests
as intestinal symptoms, frequently diarrhoea,
fever and abdominal pain. Some patients
present with cough, dyspnoea or constipation.5
Complications include autoinfection which may
lead to hyperinfection syndrome (HS) which is
a potentially serious life-threatening condition
in immunocompromised and immunosupressed
patients. 3 Generally, most of the patients
have underlying co-morbidities for instance
malnutrition, corticosteroid therapy, chronic
obstructive airway disease, chronic liver disease
or cirrhosis and peptic ulcer disease.5
The actual prevalence of infestation with this
parasite in our setting is not well identified. The
commonly associated risk factors for acquiring
this parasitic infestation include traveling into an
endemic area, working in the agriculture sector
and gardening as well as visiting contaminated
beaches.6
Current estimates indicate that at least 30-100
million people are infected with S. stercoralis
in 70 countries, and the risk for developing
advanced clinical complications is high in patients
with certain underlying clinical conditions.2,7
However, the present global estimation for the
prevalence of strongyloidiasis is not precise
and accurate, since the infection is sometimes
Address for correspondence and reprint requests: Dr. Nurul Azira Mohd Shah, Cluster of Pathology and Laboratory Medicine, Faculty of Medicine,
Universiti Teknologi Mara, 47000, Sungai Buloh, Selangor, Malaysia. Email: nazlizainuddin@yahoo.com
71
Malaysian J Pathol
misdiagnosed or difficult to detect because of the
poor sensitivity of the usual applied diagnostic
tests and the absence of reference standard (gold
standard) that provides an absolute evidence
for diagnosis.8,9 Therefore, S. stercoralis is
considered to be the most neglected among
soil-transmitted helminths infections.4
The disease has been studied among schoolage children10,11, travelers and immigrants,12,13
in tropical countries, 14 subjects with low
socioeconomic status and unhygienic habits,15-17
cancer patients,18 immunosuppressed patients,19
haematopoietic stem cell transplantation,19 and
in HTLV-1-infected patients.20 In addition, there
are case reports of acute, relapsed and fatal
strongyloidiasis.21-24
The occurrence of strongyloidiasis varies
widely among different countries, localities,
and socioeconomic backgrounds.6 The disease is
endemic in tropical, temperate and heavy rainfall
areas.3
The prevalence of strongyloidiasis in Southeast
Asia was determined as 11%.25 In Malaysia, the
prevalence of strongyloidasis among cancer
patients of all age groups who were treated with
various chemotherapeutic regimes was reported
as 5.7% (unpublished data). Rahmah et al.,16
had reported a prevalence of up to 1.2% among
aborigine children. The epidemiology of S.
stercoralis infection has been studied in much
more detail in Thailand, especially among school
children26 and was noted as 1.8%, this being 6-30
times greater than previous reports reported in
the same country.10
Infection with S. stercoralis is frequently
imported to non-endemic areas by travelers
and immigrants.27 In Spain, the epidemiology
of strongyloidiasis in the Mediterranean was
described as 0.9% among patients who were
elderly men and farmers who had walked
barefooted. 9 In the USA, 347 cases of
strongyloidiasis-associated deaths occurred
within a period of 15 years studied.28 In the
same country, it was found that half of cancer
patients who had strongyloidiasis had solid organ
malignancy and the remaining had haematologic
malignancy.18 Meanwhile in Columbia, 3.6% of
immunocompromised patients were found to be
infected with S. stercoralis.29
This study was conducted to determine the sex,
age, geographical area and co-morbid conditions
among patients with S. stercoralis infestation as
well as to study the clinical manifestations of
strongyloidiasis in our patients.
72
June 2013
MATERIALS AND METHODS
Records of patients with positive S. stercoralis
larvae from January 2000 to December
2012 in Hospital Universiti Sains Malaysia,
Kubang Kerian, Kelantan were reviewed. A
total of 15,155 of stool samples were received
within this study period. Single direct stool
microscopical examination was conducted. Wet
mount preparation of stool concentrate with
normal saline was done prior to microscopical
examination of the larvae. The morphology of the
larvae seen was described. Patients demographic
data such as age, sex, geographic area, co-morbid
conditions and clinical manifestations were
collected using a checklist. Data were analyzed
and presented as descriptive statistics.
RESULTS
Only twelve cases were detected in 13-year
period from year 2000 to 2012. The overall
prevalence of Strongyloides stercoralis infection
determined by the above method was 0.08%
(12/15,155). Ten patients (83.3%) were male
whereas two (16.7%) were female. Nine patients
were aged more than 60 years old while three
were less than 60. Most of the patients were
from Bachok (4), followed by Terengganu
(3), Kota Bharu (2), Pasir Putih (2) and Kuala
Lumpur (1).
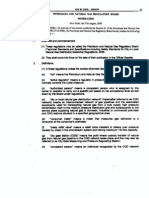
Ninety-two percent of the patients had
a co-morbid illness. Patients were mainly
immunocompromised patients, with underlying
diabetes mellitus (DM), retroviral disease,
lymphoma, chronic renal failure and steroid
therapy contributing 58% of cases (7 out of
12) (Figure 1). Concurrent illness such as
chronic obstructive airway disease (COAD),
hypertension (HPT) and chronic rheumatic heart
disease (CRHD) were also observed.
Our findings showed that most patients had
intestinal manifestations which were mainly
diarrhoea and abdominal discomfort (Table 1).
Less than half of the patients had extra-intestinal
manifestations. Twenty-five percent of patients
most probably had developed secondary bacterial
infections which lead to septicaemia.
Fifty-eight percent (7 out of 12) of patients
were treated with albendazole. In terms of
outcome, 11 patients survived while 1 died as
a result of secondary septicaemia.
STRONGYLOIDES STERCORALIS
Note: DM- Diabetes mellitus; HIV: Human Immunodeficiency Virus; COAD; Chronic Obstructive airway Disease;
HPT; Hypertensian;CRHD: Chronic Rheumatic Heart Disease, CRF; Chronic Renal Failure
FIG. 1: Percentage distribution of underlying co-morbidities in patients with Strongyloides stercoralis
infestation.
DISCUSSION
Strongyloides stercoralis is an important
intestinal helminthic infestation. It is endemic
mainly in rural areas in Malaysia but the actual
prevalence is not determined.
From our review of these strongyloidiasis
patients, males are more prone to infestation
compared to females. In our series, most of
the male patients were farmers. Male gender
has been attributed with higher prevalence
of strongyloidiasis. This could be due to
occupational exposure as most of the cases
reviewed here are farmers. In addition, the
cure rate of the infection in man is lower than
that in female, and this condition is marked by
the persistent elevation of serum IgG4.3,30 This
finding was reported in previous studies.9,7
Our centre is a referral centre for haematological
malignancies such as lymphoma and leukaemia
as well as solid organ cancers such as breast
cancer. In this review, the majority of patients
were immunocompromised. Although most
patients had intestinal symptoms, some
presented with extraintestinal symptoms such
as pleural effusion. Immunocompromised and
immunosuppressed conditions are identified as
common risks associated with this infestation
as well as contributing factors for developing
hyperinfection syndrome (HS). Autoinfection
can become amplified into a potentially fatal HS,
characterized by increased numbers of infective
filariform larvae in stool and sputum. Systemic
manifestations attributable to increase parasite
burden and migration, include gastrointestinal
bleeding and respiratory distress.3
TABLE 1: Clinical manifestations in patients with Strongyloides stercoralis infestation
Symptoms/ signs
Intestinal symptoms
Diarrhea
Constipation
Abdominal discomfort
Anorexia
Number (%)
11 (92)
9 (75)
1 ( 8)
7 (58)
5 (42)
Extraintestinal symptoms
Cough
Pleural effusion
Sepsis
4 (33)
2 (17)
2 (17)
3 (25)
Others
Moderate to severe anaemia
Fever
Weight loss
6 (50)
6 (50)
1 ( 8)
73
Malaysian J Pathol
In disseminated strongyloidiasis, bacteraemia
may develop as a result of translocation of
enteric bacteria through the tract created by
invading filariform larvae or bacteria itself can
be carried on the larva. This stage is found not
to be uncommon in the reviewed cases.3
There is no standard agreement on the
screening of S. stercoralis in suspected patients.
Routine diagnosis of strongyloidiasis is made
by a combination of stool direct microscopy,
concentration method, and culture method. Thus,
there are many reasons that can explain a very
low prevalence of strongyloidiasis among our
patients in this study. The diagnosis of chronic
strongyloidiasis from stool samples can be
difficult and insufficiently sensitive to be used
alone for screening because of intermittent larval
output in stool31,32 which lead to a low yield
of detection.33 The low sensitivity of routine
microscopical method may further contribute
to the low prevalence of detected infection.
In addition, the possibility of other unreported
cases may contribute to the overall low prevalence.
Most patients especially immunocompetent
patients are asymptomatic.33 Thus, such patients
were not presented to our setting.
On the other hand, the detection rate by direct
stool microscopy is found to be increased during
acute infection and hyperinfection as the result of
increased larval output as reported previously.34-36
However, it is extremely uncommon to see acute
infection or hyperinfection in routine clinical
practice or in surveys, since most of the positive
cases, if presented, are in the chronic phase
of the infection. Therefore, direct microscopy
alone is not useful in routine screening of
strongyloidiasis unless it is combined with other
detection methods or when the chronic disease
turns into active hyperinfection.6
The detection of parasitic DNA in faecal
samples using PCR-based methods proved
to be a sensitive and specific method for the
diagnosis of strongyloidiasis in individuals with
or without clinical symptoms at all infection
stages.37,38 Recent studies and case reports using
Strongyloides-real-time PCR reported increased
detection rates when compared with other stoolbased procedures.39 However, this method is not
widely available and is expensive, limiting its
use in developing countries.
Serological tests have shown a correlation
between S. stercoralis infection and antibody
level at all stages including acute, chronic,
hyperinfection, after treatment (treatment followup), and cure.6,40 In addition, serodiagnosis using
74
June 2013
ELISA appear to be useful in the diagnosis of
strongyloides infection in immunosuppressed
and immunocompetent patients.18 However,
there are some limitations for ELISA that may
affect results including: cross-reactions with
other nematode infections; variable sensitivity
and specificity; lack of a gold standard; and
inability to differentiate between acute or
chronic infections.2,41 In addition, the sensitivity
of serology is good in individuals with chronic
infection but is lower in those infected after
travelling to endemic areas.38,42
Albendazole is the preferred anti-helminthic
in this setting in view of its single dosing which
provides better compliance. Albendazole at
400 mg orally twice a day for 3 days has been
shown to clear stools of S. stercoralis larvae in
38% to 45% and normalize serology in 75% of
chronically infected individuals in whom larvae
were not detectable.3
As most of the reviewed cases were
immunocompromised patients, extra attention
should be made in providing screening tests to
those who are immunocompromised particularly
those presenting with symptoms of chronic
strongyloidisis, steroid therapy, diabetic, HIV
and patients with malignancy. This may help
in reducing the risk of hyperinfection and
disseminated strongyloidiasis. Screening of at
risk individiuals has also being suggested by
Keiser et al.3
In conclusion, Strongyloidiasis is present
in our local setting. However, as the current
available method which is microscopy has
low sensitivity, the actual prevalence of
strongyloidiasis might be underestimated. Thus,
other more sensitive methods such as molecular
methods may help in determining the actual
prevalence in this region. The infection should
be looked for especially in immunosuppressed
patients as its treatment would improve morbidity
and mortality.
ACKNOWLEDGEMENTS
The authors would like to thank Mr. Nik Zairi
Zakaria and Mr. Zulnuhisham Suhaimi from
the Medical Microbiology and Parasitology
Laboratory, School of Medical Sciences,
Universiti Sains Malaysia for their technical
assistance.
REFERENCES
1. Weinstein D, Lake-Bakaar G. Strongyloides
stercoralis infection presenting with severe
STRONGYLOIDES STERCORALIS
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
malabsorption and arthritis in an immune competent
host. Internet J Rheumatology. 2006; 2(2). doi:
10.5880/13e9.
Siddiqui AA, Berk SL. Diagnosis of Strongyloides
stercoralis infection. Clin Infect Dis. 2001; 33(7):
1040-7.
Keiser PB, Nutman TB. Strongyloides stercoralis
in the immunocompromised population. Clin
Microbiol Rev. 2004; 17(1): 208-17.
Olsen A, van Lieshout L, Marti H, et al.
Strongyloidiasis - the most neglected of the
neglected tropical diseases? Trans R Soc Trop Med
Hyg. 2009; 103(10): 967-72.
Tsai HC, Lee SS, Liu YC, et al. Clinical
manifestations of strongyloidiasis in southern
Taiwan. J Microbiol Immunol Infect. 2002; 35(1):
29-36.
Marcos LA, Terashima A, Dupont HL, Gotuzzo
E. Strongyloides hyperinfection syndrome: an
emerging global infectious disease. Trans R Soc
Trop Med Hyg. 2008; 102(4): 314-8.
Yori PP, Kosek M, Gilman RH, et al. Seroepidemiology
of strongyloidiasis in the Peruvian Amazon. Am J
Trop Med Hyg. 2006; 74(1): 97-102.
Lindo JF, Lee MG. Strongyloides stercoralis and S.
fulleborni. In: Gillespie SH, Pearson RD, editors.
Principles and practice of clinical parasitology. 1st
ed. New York: John Wiley & Sons; 2001. p. 47992.
Snchez PR, Guzman AP, Guillen SM, et al. Endemic
strongyloidiasis on the Spanish Mediterranean coast.
QJM. 2001; 94(7): 357-63.
Anantaphruti MT, Nuamtanong S, Muennoo
C, Sanguankiat S, Pubampen S. Strongyloides
stercoralis infection and chronological changes of
other soil-transmitted helminthiases in an endemic
area of southern Thailand. Southeast Asian J Trop
Med Public Health. 2000; 31(2): 378-82.
Dada-Adegbola HO, Bakare RA. Strongyloidiasis
in children five years and below. West Afr J Med.
2004; 23(3): 194-7.
Loutfy MR, Wilson M, Keystone JS, Kain KC.
Serology and eosinophil count in the diagnosis and
management of strongyloidiasis in a non-endemic
area. Am J Trop Med Hyg. 2002; 66(6): 749-52.
Sudarshi S, Stmpfle R, Armstrong M, et al.
Clinical presentation and diagnostic sensitivity
of laboratory tests for Strongyloides stercoralis
in travellers compared with immigrants in a nonendemic country. Trop Med Int Health. 2003; 8(8):
728-32.
Vannachone B, Kobayashi J, Nambanya S, Manivong
K, Inthakone S, Sato Y. An epidemiological survey
on intestinal parasite infection in Khammouane
Province, Lao PDR, with special reference to
Strongyloides infection. Southeast Asian J Trop
Med Public Health. 1998; 29(4): 717-22.
Huminer D, Symon K, Groskopf I, et al.
Seroepidemiologic study of toxocariasis and
strongyloidiasis in institutionalized mentally
retarded adults. Am J Trop Med Hyg. 1992; 46(3):
278-81.
Rahmah N, Ariff RH, Abdullah B, Shariman MS,
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
Nazli MZ, Rizal MZ. Parasitic infections among
aborigine children at Post Brooke, Kelantan,
Malaysia. Med J Malaysia. 1997; 52(4): 412-5.
Machado ER, Teixeira EM, de Paula FM,
Gonalves-Pires MRF, Ueta MT, Costa-Cruz JM.
Immunoparasitological diagnosis of Strongyloides
stercoralis in garbage collectors in Uberlndia, MQ
Brazil. Parasitol Latinoam. 2007; 62(3-4): 180-2.
Safdar A, Malathum K, Rodriguez SJ, Husni
R, Rolston KV. Strongyloidiasis in patients at a
comprehensive cancer center in the United States.
Cancer. 2004; 100(7): 1531-6.
Schaffel R, Nucci M, Carvalho E, et al. The
value of an immunoenzymatic test (enzymelinked immunosorbent assay) for the diagnosis of
strongyloidiasis in patients immunosuppressed by
hematologic malignancies. Am J Trop Med Hyg.
2001; 65(4): 346-50.
Hirata T, Uchima N, Kishimoto K, et al. Impairment
of host immune response against strongyloides
stercoralis by human T cell lymphotropic virus
type 1 infection. Am J Trop Med Hyg. 2006; 74(2):
246-9.
Abdelrahman MZ, Zeehaida M, Rahmah N,
et al. Fatal septicemic shock associated with
Strongyloides stercoralis infection in a patient with
angioimmunoblastic T-cell lymphoma: a case report
and literature review. Parasitol Int. 2012; 61(3):
508-11.
Norsarwany M, Abdelrahman Z, Rahmah N, et al.
Symptomatic chronic strongyloidiasis in children
following treatment for solid organ malignancies:
case reports and literature review. Trop Biomed.
2012; 29(3): 479-88.
Prendki V, Fenaux P, Durand R, Thellier M,
Bouchaud O. Strongyloidiasis in man 75 years after
initial exposure. Emerg Infect Dis. 2011; 17(5):
931-2.
Win TT, Sitiasma H, Zeehaida M. Strongyloides
stercoralis induced bilateral blood stained pleural
effusion in patient with recurrent Non-Hodgkin
lymphoma. Trop Biomed. 2011; 28(1), 64-7.
Genta RM. Global prevalence of strongyloidiasis:
critical review with epidemiologic insights into the
prevention of disseminated disease. Rev Infect Dis.
1989; 11(5): 755-67.
Steinmann P, Zhou XN, Du ZW, et al. Occurrence
of Strongyloides stercoralis in Yunnan Province,
China, and comparison of diagnostic methods. PLoS
Negl Trop Dis. 2007; 1(1): e75.
van Doorn HR, Koelewijn R, Hofwegen H, et
al. Use of enzyme-linked immunosorbent assay
and dipstick assay for detection of Strongyloides
stercoralis infection in humans. J Clin Microbiol.
2007; 45(2): 438-42.
Croker C, Reporter R, Redelings M, Mascola L.
Strongyloidiasis-related deaths in the United States,
1991-2006. Am J Trop Med Hyg. 2010; 83(2):
422-6.
Botero JH, Castao A, Montoya MN, Ocampo
NE, Hurtado MI, Lopera MM. A preliminary
study of the prevalence of intestinal parasites in
immunocompromised patients with and without
75
Malaysian J Pathol
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
76
gastrointestinal manifestations. Rev Inst Med Trop
Sao Paulo. 2003; 45(4): 197-200.
Walzer PD, Milder JE, Banwell JG, Kilgore G,
Klein M, Parker R. Epidemiologic features of
Strongyloides stercoralis infection in an endemic
area of the United States. Am J Trop Med Hyg.
1982; 31(2): 313-9.
Marty FM. Strongyloides hyperinfection syndrome
and transplantation: a preventable, frequently fatal
infection. Transpl Infect Dis. 2009; 11(2): 97-9.
Wirk B, Wingard JR. Strongyloides stercoralis
hyperinfection in hematopoietic stem cell
transplantation. Transpl Infect Dis. 2009; 11(2):
143-8.
Mora CS, Segami MI, Hidalgo JA. Strongyloides
stercoralis hyperinfection in systemic lupus
erythematosus and the antiphospholipid syndrome.
Semin Arthritis Rheum. 2006; 36(3): 135-43.
Kia EB, Rahimi HR, Mirhendi H, et al. A
case of fatal strongyloidiasis in a patient with
chronic lymphocytic leukemia and molecular
characterization of the isolate. Korean J Parasitol.
2008; 46(4): 261-3.
Azira NM, Zeehaida M. Strongyloides stercoralis
hyperinfection in a diabetic patient: case report.
Trop Biomed. 2010; 27(1): 115-9.
Stewart DM, Ramanathan R, Mahanty S, Fedorko
DP, Janik JE, Morris JC. Disseminated Strongyloides
stercoralis infection in HTLV-1-associated adult
T-cell leukemia/lymphoma. Acta Haematol. 2011;
126(2): 63-7.
ten Hove RJ, van Esbroeck M, Vervoort T, van
den Ende J, van Lieshout L, Verweij JJ. Molecular
diagnostics of intestinal parasites in returning
travellers. Eur J Clin Microbiol Infect Dis. 2009;
28(9): 1045-53.
Verweij JJ, Canales M, Polman K, et al. Molecular
diagnosis of Strongyloides stercoralis in faecal
samples using real-time PCR. Trans R Soc Trop
Med Hyg. 2009; 103(4): 342-6.
Basuni M, Muhi J, Othman N, et al. A pentaplex realtime polymerase chain reaction assay for detection
of four species of soil-transmitted helminths. Am J
Trop Med Hyg. 2011; 84(2): 338-43.
Rodrigues RM, de Oliveira MC, Sopelete MC, et al.
IgG1, IgG4, and IgE antibody responses in human
strongyloidiasis by ELISA using Strongyloides ratti
saline extract as heterologous antigen. Parasitol Res.
2007; 101(5): 1209-14.
Boulware DR, Stauffer WM, Hendel-Paterson BR,
et al. Maltreatment of Strongyloides infection: case
series and worldwide physicians-in-training survey.
Am J Med. 2007; 120(6): 545. e1-8.
Marcos LA, Terashima A, Canales M,
Gotuzzo E. Update on strongyloidiasis in the
immunocompromised host. Curr Infect Dis Rep.
2011; 13(1): 35-46.
June 2013
También podría gustarte
- tmp80F6 TMPDocumento24 páginastmp80F6 TMPFrontiersAún no hay calificaciones
- tmpCE8C TMPDocumento19 páginastmpCE8C TMPFrontiersAún no hay calificaciones
- tmp3CAB TMPDocumento16 páginastmp3CAB TMPFrontiersAún no hay calificaciones
- Tmpa077 TMPDocumento15 páginasTmpa077 TMPFrontiersAún no hay calificaciones
- tmpF178 TMPDocumento15 páginastmpF178 TMPFrontiersAún no hay calificaciones
- tmp6F0E TMPDocumento12 páginastmp6F0E TMPFrontiersAún no hay calificaciones
- tmpEFCC TMPDocumento6 páginastmpEFCC TMPFrontiersAún no hay calificaciones
- Tmp1a96 TMPDocumento80 páginasTmp1a96 TMPFrontiersAún no hay calificaciones
- tmp72FE TMPDocumento8 páginastmp72FE TMPFrontiersAún no hay calificaciones
- tmpF407 TMPDocumento17 páginastmpF407 TMPFrontiersAún no hay calificaciones
- tmpF3B5 TMPDocumento15 páginastmpF3B5 TMPFrontiersAún no hay calificaciones
- tmpE3C0 TMPDocumento17 páginastmpE3C0 TMPFrontiersAún no hay calificaciones
- tmpE7E9 TMPDocumento14 páginastmpE7E9 TMPFrontiersAún no hay calificaciones
- tmpFFE0 TMPDocumento6 páginastmpFFE0 TMPFrontiersAún no hay calificaciones
- tmp6382 TMPDocumento8 páginastmp6382 TMPFrontiersAún no hay calificaciones
- tmp60EF TMPDocumento20 páginastmp60EF TMPFrontiersAún no hay calificaciones
- tmpB1BE TMPDocumento9 páginastmpB1BE TMPFrontiersAún no hay calificaciones
- tmpC30A TMPDocumento10 páginastmpC30A TMPFrontiersAún no hay calificaciones
- tmp8B94 TMPDocumento9 páginastmp8B94 TMPFrontiersAún no hay calificaciones
- tmp998 TMPDocumento9 páginastmp998 TMPFrontiersAún no hay calificaciones
- tmp3656 TMPDocumento14 páginastmp3656 TMPFrontiersAún no hay calificaciones
- tmp37B8 TMPDocumento9 páginastmp37B8 TMPFrontiersAún no hay calificaciones
- tmpD1FE TMPDocumento6 páginastmpD1FE TMPFrontiersAún no hay calificaciones
- tmpC0A TMPDocumento9 páginastmpC0A TMPFrontiersAún no hay calificaciones
- tmp4B57 TMPDocumento9 páginastmp4B57 TMPFrontiersAún no hay calificaciones
- tmp9D75 TMPDocumento9 páginastmp9D75 TMPFrontiersAún no hay calificaciones
- tmp27C1 TMPDocumento5 páginastmp27C1 TMPFrontiersAún no hay calificaciones
- tmp2F3F TMPDocumento10 páginastmp2F3F TMPFrontiersAún no hay calificaciones
- tmpA0D TMPDocumento9 páginastmpA0D TMPFrontiersAún no hay calificaciones
- Tmp75a7 TMPDocumento8 páginasTmp75a7 TMPFrontiersAún no hay calificaciones
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Buffer System - Group 3Documento5 páginasBuffer System - Group 3Rameen QadirAún no hay calificaciones
- TATA PROJECTS LIMITED Tilting & Drum Transfer Unit Technical SpecificationDocumento6 páginasTATA PROJECTS LIMITED Tilting & Drum Transfer Unit Technical SpecificationSridhar VedulaAún no hay calificaciones
- AnimalDocumento3 páginasAnimalSyamiminajwa RizanAún no hay calificaciones
- Songs BookDocumento38 páginasSongs BookАнастасія ЯщукAún no hay calificaciones
- Waterways Summer 2013Documento76 páginasWaterways Summer 2013Waterways MagazineAún no hay calificaciones
- Rosen 48V 200AH LiFePo4 Battery-PowerwallDocumento5 páginasRosen 48V 200AH LiFePo4 Battery-Powerwallgihan_maAún no hay calificaciones
- Pra Ukp 1-1Documento34 páginasPra Ukp 1-1Evantius TariganAún no hay calificaciones
- Technical Standards PNGRBDocumento44 páginasTechnical Standards PNGRBRashid HussainAún no hay calificaciones
- Hazard Management in Contracts Guidelines: Petroleum Development Oman L.L.CDocumento13 páginasHazard Management in Contracts Guidelines: Petroleum Development Oman L.L.Csatish20ntrAún no hay calificaciones
- 2020-Botao NHS Gad Budget-RevisedDocumento5 páginas2020-Botao NHS Gad Budget-RevisedJoseph Caballero CruzAún no hay calificaciones
- Epidemiology of Chlamydia Trachomatis InfectionsDocumento20 páginasEpidemiology of Chlamydia Trachomatis InfectionsAmbarAún no hay calificaciones
- Genome Browser ExerciseDocumento5 páginasGenome Browser ExerciseyukiAún no hay calificaciones
- Overtime Pay-DOLEDocumento1 páginaOvertime Pay-DOLEJun CanilloAún no hay calificaciones
- Art of Focused ConversationsDocumento8 páginasArt of Focused Conversationsparaggadhia100% (1)
- Ecological Solid Waste Management Survey at Barangay 41 BogtongDocumento3 páginasEcological Solid Waste Management Survey at Barangay 41 BogtongRab Baloloy100% (1)
- School and Community RelationsDocumento8 páginasSchool and Community RelationsWendell HernandezAún no hay calificaciones
- Vaccination List: Name Anti-Hbs Vaccine To GIVE Hepa-B (PHP 340/dose)Documento10 páginasVaccination List: Name Anti-Hbs Vaccine To GIVE Hepa-B (PHP 340/dose)Manuel Florido ZarsueloAún no hay calificaciones
- General EcologyDocumento152 páginasGeneral Ecologykidest100% (2)
- Life Skills Curriculum - Secondary 1Documento546 páginasLife Skills Curriculum - Secondary 1Jeff Zacker100% (2)
- The Hunters: Anthropologists' Misconceptions of the !Kung PeopleDocumento4 páginasThe Hunters: Anthropologists' Misconceptions of the !Kung PeopleSimba GlynAún no hay calificaciones
- Chapter 7 - Products, Services - Brands-Building Customer ValueDocumento48 páginasChapter 7 - Products, Services - Brands-Building Customer ValuexuetingAún no hay calificaciones
- Tinjauan Penjelasan General Consent Di Pendaftaran Rawat Inap Rs Medika Permata HijauDocumento6 páginasTinjauan Penjelasan General Consent Di Pendaftaran Rawat Inap Rs Medika Permata HijauAgnesthesiaAún no hay calificaciones
- MCPS FBA Form 2016Documento4 páginasMCPS FBA Form 2016Nzinga WardAún no hay calificaciones
- Mark-Recapture Lab: BIOL 3370LDocumento2 páginasMark-Recapture Lab: BIOL 3370Lapi-475993899Aún no hay calificaciones
- Soal I KUNCIDocumento4 páginasSoal I KUNCIAyie Sharma100% (1)
- ChoiDocumento19 páginasChoiLuciana RafaelAún no hay calificaciones
- Red Cabbage IndicatorDocumento2 páginasRed Cabbage IndicatorgadbloodAún no hay calificaciones
- S9S12HA32CLLDocumento1 páginaS9S12HA32CLLAutotronica CaxAún no hay calificaciones
- ADEC - Al Khalil International School 2016-2017Documento19 páginasADEC - Al Khalil International School 2016-2017Edarabia.comAún no hay calificaciones
- English Debate Competition 558b213e259d1Documento22 páginasEnglish Debate Competition 558b213e259d1Mutiara MaulinaAún no hay calificaciones