Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Non Obstetric Surgery During Pregnancy 2013
Cargado por
christietwongDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Non Obstetric Surgery During Pregnancy 2013
Cargado por
christietwongCopyright:
Formatos disponibles
Imelda Odibo, MD
2
nd
-Year Maternal-Fetal Medicine Fellow
Division of Maternal-Fetal Medicine
Department of Obstetrics and Gynecology
University of Arkansas for Medical Sciences
Non-Obstetric Surgery
During Pregnancy
Objectives
Describe the role of the obstetrician in the diagnosis and
management of patients requiring non-obstetric surgery
during pregnancy
Outline common indications for non-obstetric surgery in
the parturient
Discuss anesthetic considerations, optimal timing and
surgical approach to non-obstetric surgery during
pregnancy
Discuss indications for tocolytics, antenatal steroids,
progesterone and the guidelines on fetal monitoring when
non-obstetric surgery is performed during pregnancy
Discuss effect of anesthesia and surgery on maternal and
fetal outcome after non-obstetric surgery
Introduction
Non-obstetric surgery during pregnancy
Performed in 1.5-2% of all pregnancies
More than 75,000 women in the US each year
Diagnosis and management complicated by altered anatomy and
physiology
Difficulty of conducting large-scale, randomized clinical
trials in this population
Information based on observational studies, expert
opinion, and extrapolation from trials in non pregnant
individuals
ACOG: Insufficient data to allow for specific
recommendations
Role of the Obstetrician
ACOG
Obstetric consultation prior to performing non-obstetric surgery
and some invasive procedures (cardiac catheterization,
colonoscopy) during pregnancy
Multi-disciplinary approach
Obstetricians uniquely qualified to discuss aspects of maternal
physiology and anatomy which may affect maternal-fetal well-being
Obstetrician must be well informed on
Influence of surgical disorders on pregnancy and vice versa
Risk of diagnostic and therapeutic procedures
Management of preterm labor in immediate postoperative period
Indications for Non-Obstetric
Surgery in Pregnancy
Indications for Non-Obstetric Surgery
in Pregnancy
Abdominal diseases and disorders
Appendicitis
Biliary disease: Cholecystitis and Cholelithiasis
Acute pancreatitis
Peptic ulcer disease
Acute intestinal obstruction
Spontaneous hepatic and splenic rupture
Ruptured splenic artery aneurysm
Pelvic diseases and disorders
Ovarian masses
Torsion of the adnexa
Solid ovarian tumors
Carcinoma of the ovary
Leiomyomas
Indications for Non-Obstetric Surgery
in Pregnancy
Cancer in pregnancy
Breast cancer
Cervical cancer
Lymphomas and leukemias
Malignant melanoma
Cardiac disease
Neurologic disease
Hemorrhoids
Trauma
Fetal and Maternal
Considerations
General Maternal Considerations
Hematologic/CVS
30-50% increase in plasma volume CO drug distribution/lab
test results
Plasma volume more than red cell mass Physiologic anemia
Colloid osmotic pressure increased interstitial fluid-edema
Systolic and diastolic BPs in the 2
nd
trimester, return to baseline
by term
SVR
General Maternal Considerations
Respiratory
FRC due to limitation of diaphragmatic excursion
MV due to TV and RR
Compensated mild respiratory alkalosis
Renal
Renal blood flow GFR, serum Cr, BUN
GI
GI motility , gastric emptying and constipation
Anatomic
Enlarging uterus alters anatomic relationship among different
organs
When supine enlarged uterus compresses vena cava hypotensive
vena cava compression syndrome
Fetal Considerations
Assessment of risk to fetus challenging and should include
risks associated with
Maternal disease
Diagnostic radiologic procedure
Therapeutic drugs
Anesthesia
Surgery
Fetal loss
Preterm labor/delivery
Fetal Considerations: Diagnosis
Rely more on careful review of medical history, signs and
symptoms and comprehensive physical exam
Lab values often have altered normal values during
pregnancy
Imaging: Use abdominal shield whenever feasible
Adverse effects varies with GA and is dose dependent
Current evidence suggests no increased structural or developmental
fetal risks with dose <5 rad
<8w: radiation induced IUGR
8-15W: MR, 4% risk at 10 rad, 60% at 150 rad
10 rad: microcephaly, MR, IUGR, eye abnormalities
In utero exposure risk of childhood neoplasm-dose
related
Fetal exposure of 1-2 rad translates to RR 1.5-2.0 for childhood
leukemia
Fetal Considerations: ACOG Guidelines
Regarding Radiation Exposure in Pregnancy
Counseling; <5 rad, no increased risk for fetal anomalies or
pregnancy loss
Concern for radiation exposure should not prevent medically
indicated diagnostic procedure when appropriate
US and MRI are not associated with known adverse fetal effects
so consider when appropriate
Consult expert in dosimetry calculation to help estimated fetal
dose in case of multiple radiologic studies
Radioactive isotopes of iodine- avoid diagnostic or therapeutic
use in pregnancy; Avoid Iodinated contrast agents due to risk of
neonatal hypothyroidism
Radiopaque and paramagnetic contrast agents - unlikely to
cause harm and may be of diagnostic benefit, use in pregnancy
only if the potential benefit justifies potential fetal risk
Pregnancy Outcomes After
Non-Obstetric Surgery
Maternal and Fetal Outcome
After Surgery
The indications for surgery and its timing are major
determinants of maternal and fetal outcome
No evidence that surgery during pregnancy increases
background risk for miscarriage (8-16% at < 13w for
clinically recognized pregnancies, 2-4% at 13-20w)
Pregnancy Outcome After
Non-Obstetrical Surgical Intervention
Cohen-Kerem et al, Pregnancy outcome following non-
obstetric surgical intervention. Am J Surg. 2005
Sep;190(3):467-73
Literature review of 54 papers including 12,452 subjects
Maternal death was rare .006% (<1/10,000)
Miscarriage rate was 5.8%; 10.5% in the first trimester (# difficult to
interpret - no matched controls)
Elective termination 1.3%
Preterm labor 3.5% (specifically following appendectomy)
Fetal loss 2.5%
Preterm delivery 8.2%
Pregnancy Outcome After
Non-Obstetrical Surgical Intervention
Major birth defects in women who had surgery in 1st trimester 3.9%
(1-3% in gen pop)
Sub-analysis of papers reporting on appendectomy during
pregnancy revealed a high rate (4.6%) of surgery-induced labor
Fetal loss associated with appendectomy was 2.6%; however, this
rate was increased when peritonitis was present (10.9%)
Surgery in the first trimester does not appear to increase
major birth defects and should not be delayed when
indicated; Acute appendicitis with peritonitis is associated
with higher risk to the mother and fetus
Surgery is not generally recommended
during the first trimester due to potential
for pregnancy loss and teratogenicity
Early to mid 2
nd
trimester is optimal
Timing of Surgery
Timing of Surgery
Pregnancy loss
Cohen-Kerem et al reported 10.5% in 1
st
trimester
Some other studies have reported higher rates
Considerations include
Inherent rate of pregnancy loss is higher in 1
st
trimester
Surgical procedure
Underlying maternal condition (infection, high fever)
Maternal characteristics/comorbidities (smoking, AMA)
Exposure to teratogens
First 2 wks of gestation - all or none effect
3-8w during organogenesis - may cause major structural organ
abnormalities
Exposure at >8w - functional changes or growth retardation,
structural abnormalities rare
Timing of Surgery
Advanced gestation
Difficulty maneuvering around gravid uterus
Difficulty managing airway
Increased chance of uterine irritability, preterm contractions and
PTL
ACOG
A pregnant woman should never be denied indicated surgery,
regardless of trimester
Elective surgery should be postponed until after delivery
If possible, non urgent surgery should be performed in the second
trimester when preterm contractions and spontaneous abortion are
least likely
Location for Surgical Procedure
Perform at institution with neonatal and pediatric services
An obstetric care provider with cesarean delivery privileges
should be readily available
Data shows laparoscopy for non-
obstetric surgery during pregnancy is
as safe as laparotomy
Surgical approach should be based on
skill of the surgeon and availability of
appropriate staff and equipment
Laparoscopy vs. Laparotomy
Laparotomy
Incision
Depends on surgical procedure and GA
In general, vertical incision recommended as GA advances - better
exposure, allows for extension if necessary
Laparoscopy
Increasing use during pregnancy in the past decade
Most common uses
Exploration and treatment of adnexal masses
Appendectomy
Cholecystectomy
Advantages
Decreased postoperative morbidity
Less pain
Shorter hospital stay and postoperative recovery time
Drawbacks
Risk of injury to gravid uterus
Technical difficulty with exposure
Increased co2 absorption by mother and fetus
Decreased uterine blood blow due to excessive intra-abdominal
pressure
Laparoscopy vs. Laparotomy
Reedy MB, Klln B, Kuehl TJ. Laparoscopy during
pregnancy: a study of five fetal outcome parameters with
use of the Swedish health registry. Am J Obstet Gynecol.
1997;177:673679
Swedish study covering 2,015,000 deliveries from 1973-
1993
2181 laparoscopies and 1522 laparotomies performed at
4-20w gestation for non-obstetric surgical indications
during pregnancy
Increased risk of preterm delivery prior to 37w, birth
weight <2500g and IUGR in both groups compared with
total population
No difference in five fetal outcome variables, birth weight,
gestational duration, growth restriction, infant survival up
to 1 year, fetal malformations among laparoscopy and
laparotomy groups
Laparoscopy vs. Laparotomy
Rollins et al, Laparoscopy for appendicitis and cholelithiasis
during pregnancy: a new standard of care. Surg Endosc.
2004 Feb;18(2):237-41
Retrospective review of open or laparoscopic
cholecystectomy or appendectomy cases between 1998
and 2002; The outcomes were compared with the authors'
previous data
The laparoscopic management of symptomatic
cholelithiasis and appendicitis during pregnancy increased
from 54% to 97%
No significant differences in PTD rates, birth weights, or 5-
min Apgar scores were found between the two periods; No
birth defects or uterine injuries occurred
Laparoscopy vs. Laparotomy
Cohen-Kerem et al, Pregnancy outcome following non-
obstetric surgical intervention. Am J Surg. 2005
Sep;190(3):467-73
Evaluated the effects of non-obstetric surgical procedures
on maternal and fetal outcome
Literature review of 54 papers including 12,452 subjects; 9
studies focused laparoscopic
None of the studies came to the conclusion that laparoscopic
procedures were harmful to the mother or fetus
In general, the most common conclusion was that laparoscopic
surgery was safe and may benefit with the patient when compared
to open procedures
Laparoscopy vs. Laparotomy
Koo et al Laparotomy vs. laparoscopy for the treatment of
adnexal masses during pregnancy, ANJZOG 2012; 52: 34
38
Retrospective analysis of 262 pregnant women -
laparotomy or laparoscopic surgery between 200-2009;
174 (66.4%) laparotomies, 88 (33.6%) laparoscopies
The laparoscopy group
Shorter mean operative time (60.7 27.1 vs. 69.7 24.4 min, P =
0.002)
Shorter mean hospital stay (4.7 1.7 vs. 6.6 1.3 days, P < 0.001)
No significant difference between the two groups in
obstetric outcomes, including PTD and miscarriage rate,
after adjusting for GA at surgery, emergency surgery and
mass size
Conclusions: Laparoscopic approach appears to offer a
suitable alternative to laparotomy
Type determined primarily by
planned surgical procedure
(indication, nature, site)
Choose technique which requires
minimal quantity of drugs and
minimizes fetal exposure (e.g.
regional) that is appropriate for
surgical procedure and patients
condition
Anesthesia for Non-Obstetric
Surgery in Pregnancy
Anesthesia for Non-Obstetric
Surgery in Pregnancy
Regional anesthesia has better safety profile for mother so
is preferred over GETA
However, most Non-obstetric surgeries in pregnancy are
performed via laparoscopy or urgent exploratory
laparotomy so GETA is utilized
Major anesthesia concerns
Inherent increased risk associated with surgery and anesthesia
during pregnancy
Teratogenesis
Untoward reaction to anesthetic agents
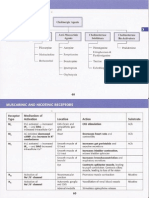
System Physiological change Anesthetic implications
Cardiovascular CO up to 50%
Uterine perfusion to 10% of CO Uterine perfusion not auto regulated
SVR, PVR, AP
Hypotension common under regional and
general anesthesia
Aortocaval compression from 13 weeks
Supine hypotensive syndrome requires left
lateral tilt
Respiratory Minute ventilation Faster inhalation induction
Respiratory alkalosis (Pa
co
2
3.74.2 kPa) Maintain Pa
co
2
at normal pregnancy levels
ERV, RV, FRC
V/Q mismatch
Oxygen consumption
Upward displacement of diaphragm
Potential hypoxaemia in the supine and
Trendelenburg positions
Thoracic diameter
Breathing more diaphragmatic than
thoracic
Mucosal edema
Difficult laryngoscopy and intubation;
bleeding during attempts
CNS Epidural vein engorgement Bloody tap more common
Epidural space volume More extensive local anesthetic spread
Sensitivity to opioids and sedatives
Hematological Red cell volume 30%, WCC
Plasma volume 50% Dilutional anemia
Coagulation factors
Thromboembolic complications (DVT
prophylaxis)
Albumin and colloid osmotic pressure edema, decreased protein binding of drugs
Gastrointestinal Intragastric pressure Aspiration risk
Barrier pressure
Antacid prophylaxis, RSI after 18 weeks
gestation
Renal Renal plasma flow, GFR
Normal urea and creatinine may mask
impaired renal function
Reabsorptive capacity Glycosuria and proteinuria
General Anesthesia
Issues related to GETA in pregnancy
Risk of difficult intubation
Risk of desaturation
Risk of aspiration
Risk of hemodynamic instability
Effects of mechanical ventilation (failure to account for physiologic
respiratory alkalosis during GETA can result in hypoventilation
respiratory acidosis)
Optimizes maternal and fetal oxygenation, reduces
intraoperative uterine irritability
Regional Anesthesia
Highly desirable when feasible
Avoids problems related to GETA except HYPOTENSION
Obesity and edema can obscure landmarks, hormonal
effect on interspinal ligaments epidural loss of
resistance techniques
Spread of local anesthetic in spinal or epidural space ,
lower doses needed (mechanical effect of enlarging uterus,
hormonal changes, increased sensitivity to local
anesthetics)
Sympathetic activity in pregnancy, sympathetic block
maternal hypotension in the presence of hypovolemia
Treat hypotension with Left lateral tilt/vasoconstrictor
administration/IVF
Teratogenicity
Despite general safety of anesthetic agents; concern
remains regarding teratogenicity in early gestation
Study of 572 women, operated at 4-5w gestation suggests possible
increase in NTDs
All but emergent surgery should be postponed until 2
nd
trimester
No evidence of adverse effect on human brain
development or risk of learning disabilities later in life
? Increased risk of miscarriage in health care professionals
with chronic exposure to nitrous oxide; Adverse effects of
acute exposure has not been established
Teratogenicity
All commonly used induction agents, opioids, neuromuscular
blocking agents, and volatile anesthetics can be used in
pregnancy; They are not teratogenic when used in clinical
concentrations and when maternal physiology is maintained
ACOG: No currently used anesthetic agents have been shown
to have any teratogenic effects in humans when using standard
concentrations at any gestational age
Tocolytic effect: Potent inhalational agents decrease uterine
tone
Anesthesia for Non-Obstetric
Surgery in Pregnancy
Swedish population based study
720,000 patients, 5405 patients underwent Non-obstetric surgery
using general anesthesia during pregnancy
Specific types of anesthesia not associated with adverse outcome
Adverse effects including LBW( due to prematurity and IUGR) early
neonatal death( within 7 days) increased in the surgery group. This
increased risk thought to correlate with underlying condition that
necessitated the surgical procedure rather than type of anesthesia
Rate of congenital malformations and unexplained stillbirths similar
in women who underwent surgery requiring anesthesia when
compared to those who did not suggests surgery and anesthesia are
not associated with adverse effects in early pregnancy
Efficacy during non-obstetric surgery is
unproven and prophylactic use is
controversial given potential maternal
side-effects
Tocolytic Therapy
Tocolytic Therapy
Prophylactic therapy can be considered in the 3
rd
trimester
in patients undergoing lower abdominal or pelvic surgery
for inflammatory conditions
Efficacy unproven, use controversial
The use of volatile anesthetic agents has been advocated
as they relax the uterus, although high concentrations can
cause undesirable hypotension
Reduction of uterine manipulation during surgery
Monitor uterine activity following surgery, if premature
labor occurs, tocolysis will be necessary to preserve the
pregnancy
Whitecar et al; Adnexal masses in pregnancy: A review of
130 cases undergoing surgical management, Am J Obstet
Gynecol 181:19-24,1999
Prophylactic tocolysis administered to 13 patients who had
surgery in 2
nd
and 3
rd
trimester
6/13 had preterm delivery, only 2 delivered within 2 weeks
of laparotomy
Potential for preterm delivery unresponsive to tocolysis
Tocolytic Therapy
Antenatal Steroid Administration
Given negligible risk of steroids and potential for preterm
delivery consideration should be given to prophylactic
course of steroids for FLM if surgery performed between
24-34 weeks
Consider the increase in patients risk of PTB due to
underlying disease and planned surgery
Avoid in setting of systemic infection such as sepsis or
ruptured appendix
Thromboprophylaxis
Pregnancy hyper-coagulable state
Protective against excessive blood loss while increasing risk
for thromboembolic event in postsurgical period
Place pneumatic compression devices on all women
undergoing surgery during pregnancy
Pharmacologic thrombo-prophylaxis should be
individualized based on
Additional risk factors for VTE
Length of procedure
Scope of procedure
Antibiotic Prophylaxis
Depends on specific procedure
Cephalosporins, penicillins, erythromycin, azithromycin,
clindamycin- Good safety profile
Aminoglycosides- relatively safe- risk of fetal and maternal
ototoxicity and nephrotoxicity
Doxycycline- generally avoided other tetracyclines
associated with transient suppression of bone growth and
staining of developing teeth
Trimethroprim- dihydrofolate reductase inhibitor affects
folic acid metabolism- avoid during first trimester-
potential increase in incidence of congenital malformation
Fluoroquinolones- avoid during pregnancy and lactation-
toxic to developing cartilage in animal studies. Has not
been documented in humans
Individualize Based On
GA
Type of surgery
Facilities available
Fetal Monitoring
Fetal Monitoring
Previable fetus
FHR by Doppler before and after procedure.
In rare cases, intraop fetal monitoring may be performed for a previable
fetus to facilitate positioning and oxygenation intervention
Intraop FHR more sensitive assessment of maternal cardiorespiratory status
than vital signs
Viable fetus
Cardiotocographic monitoring before and after procedure
Continuous CTG or Doppler US
Decreased FHR variability and baseline( remains within normal range) with
general anesthesia
Continuous intraoperative CTG monitoring if
It is physically possible to perform( TVS if feasible)
Provider with appropriate skills is available and willing to intervene during the
surgical procedure for fetal indication
Patient signs informed consent for emergency CD
Nature of surgery allows for safe interruption or alteration to provide access for
CD
Progesterone Supplementation
Csapo et al; 1972, Scott et al 1991
Removal of the corpus luteum up to 47 days of pregnancy (dating by
LMP) resulted in a high rate of abortion
Removal after 61 days only resulted in a transient decrease in
progesterone, without a high rate of abortion
Supplement if corpus luteum is removed at 7-9 w gestation
Luteal placental shift starts at about 9 weeks
Progesterone 50 to 100 mg vaginal suppository every 8 to 12 hours
OR
Daily intramuscular injection of 1 mL [50 mg] progesterone in oil
Oral progesterone appears to be less effective
Post-Op Pain Management
Short term postop use of narcotic analgesic agents
acetaminophen or NSAID generally appears to produce no
adverse fetal effects
Avoid NSAID use after 32w- risk of premature closure of DA
if given for >48hrs
Epidural analgesia- effective and reasonable alternative.
risk of opioid induced hypoventilation when compared
to IV OPIOIDS
Reserve CD for Obstetric Indications
Mode of Delivery
References
Crowhurst JA. Anaesthesia for non-obstetric surgery during pregnancy. Acta Anaesthesiol Belg
2002;53:2957.
Cohen-Kerem R, Railton C, Oren D, Lishner M, Koren G. Pregnancy outcome following non-obstetric
surgical intervention. Am J Surg 2005;190:46773.
Van De Velde M, De Buck F. Anaesthesia for non-obstetric surgery in the pregnant patient. Minerva
Anestesiol 2007;73:23540.
Fatum M, Rojansky N. Laparoscopic surgery during pregnancy. Obstet Gynecol Surv. 2001
Jan;56(1):50-9.
Rollins MD, Chan KJ, Price RR: Laparoscopy for appendicitis and cholelithiasis during pregnancy: A
new standard of care. Surg Endosc 2004;18:237
Fatum M, Rojansky N: Laparoscopic surgery during pregnancy. Obstet Gynecol Surv 2001;56:50
Reedy MB, Klln B, Kuehl TJ. Laparoscopy during pregnancy: a study of five fetal outcome
parameters with use of the Swedish health registry. Am J Obstet Gynecol. 1997;177:673679.
Wilcox AJ, Weinberg CR, O'Connor JF, et al. Incidence of early loss of pregnancy. N Engl J Med 1988;
319:189.
Boklage CE. Survival probability of human conceptions from fertilization to term. Int J Fertil 1990;
35:75, 79.
Griffen WO Jr., Dilts PV Jr., Roddick JW Jr.. Non-obstetric surgery during pregnancy. Curr Probl Surg
1969;6:156.
Crowhurst JA. Anaesthesia for non-obstetric surgery during pregnancy. Acta Anaesthesiol Belg
2002;53:2957.
Cohen-Kerem R, Railton C, Oren D, Lishner M, Koren G. Pregnancy outcome following non-obstetric
surgical intervention. Am J Surg 2005;190:46773.
Van De Velde M, De Buck F. Anaesthesia for non-obstetric surgery in the pregnant patient. Minerva
Anestesiol 2007;73:23540.
Reedy MB, Kallen B, Kuehl TJ. Laparoscopy during pregnancy: a study of five fetal outcome
parameters with use of the Swedish Health Registry. Am J Obstet Gynecol 1997;177:6739.
Fanzago E. Anaesthesia for non-obstetric surgery in pregnant patients. Minerva Anestesiol
2003;69:41627.
Kuczkowski KM. The safety of anaesthetics in pregnant women. Exp Opin Drug Saf 2006;5:25164.
Mazze RI, Kallen B. Reproductive outcome after anesthesia and operation during pregnancy: a
registry study of 5405 cases. Am J Obstet Gynecol 1989;161:117885.
Gin T, Mainland P, Chan MT, Short TG. Decreased thiopental requirements in early pregnancy.
Anesthesiology 1997;86:738.
Higuchi H, Adachi Y, Arimura S, Kanno M, Satoh T. Early pregnancy does not reduce the C
50
of
propofol for loss of consciousness. Anesth Analg 2001;93:15659.
Datta S, Crocker S, Alper MH. Muscle pain following administration of suxamethonium to pregnant
and non-pregnant patients undergoing laparoscopic tubal ligation. Br J Anaesth 1977;49:6258.
De-Kun L, Liyan L, Odouli R. Exposure to non-steroidal anti-inflammatory drugs during pregnancy and
risk of miscarriage: population based cohort study. Br Med J 2003;324:368.
References
También podría gustarte
- The Careers Paths of Doctorate HoldersDe EverandThe Careers Paths of Doctorate HoldersAún no hay calificaciones
- Non Obstetric Surgery During PregnancyDocumento64 páginasNon Obstetric Surgery During PregnancyHareen ReddyAún no hay calificaciones
- Anaesthesia For Non Obstetric Surgery in PregnancyDocumento71 páginasAnaesthesia For Non Obstetric Surgery in PregnancyVaibhav JainAún no hay calificaciones
- Low Peh Hueh International Medical University, MalaysiaDocumento19 páginasLow Peh Hueh International Medical University, MalaysiaChaitanya Venkata SattiAún no hay calificaciones
- Heparin Induced ThrombocytopeniaDocumento17 páginasHeparin Induced ThrombocytopeniaTafsir arefin100% (1)
- Bladder IrrigationDocumento9 páginasBladder IrrigationWelas_Riyanto_9968Aún no hay calificaciones
- Ch12 - LN Culinary SoupsDocumento14 páginasCh12 - LN Culinary Soupsamitjoshi78Aún no hay calificaciones
- B Lynch SuturingDocumento32 páginasB Lynch SuturingDoru Draghici67% (3)
- Bladder IrrigationDocumento3 páginasBladder IrrigationRuth GunjalAún no hay calificaciones
- CTGDocumento20 páginasCTGjaya ruban100% (1)
- Menu EngineeringDocumento11 páginasMenu EngineeringAnel BadenhorstAún no hay calificaciones
- Menu EngineeringDocumento37 páginasMenu EngineeringWai-Yan HauAún no hay calificaciones
- Necrotizing Enterocolotis (NEC)Documento2 páginasNecrotizing Enterocolotis (NEC)JDRN14Aún no hay calificaciones
- Pre Eclampsia ManualDocumento48 páginasPre Eclampsia ManualFilipa Pimenta de MatosAún no hay calificaciones
- Games Trainers PlayDocumento1 páginaGames Trainers PlayRudy Susanto100% (1)
- Donor Milk Banking and Breastfeeding in NorwayDocumento6 páginasDonor Milk Banking and Breastfeeding in NorwayFrieta Diaz AstutiAún no hay calificaciones
- Assessment of Fetal Well BeingDocumento46 páginasAssessment of Fetal Well BeingAumrin Fathima100% (1)
- លិខិតរដ្ឋបាលDocumento1 páginaលិខិតរដ្ឋបាលChanveasna RosAún no hay calificaciones
- Neonatal SubgalealDocumento6 páginasNeonatal SubgalealIrenLayAún no hay calificaciones
- Pediatric Newborn Medicine Clinical Practice GuidelinesDocumento15 páginasPediatric Newborn Medicine Clinical Practice GuidelinesJosselle Sempio CalientaAún no hay calificaciones
- Neonatal ResuscitationDocumento7 páginasNeonatal ResuscitationJavier López García100% (1)
- Heart & Hemodynamics NotesDocumento8 páginasHeart & Hemodynamics NotesBrandice BradleyAún no hay calificaciones
- Shoulder DystociaDocumento14 páginasShoulder Dystociarake sardevaAún no hay calificaciones
- Handbook Peads SurgDocumento88 páginasHandbook Peads Surgsedaka26Aún no hay calificaciones
- Approach To Sick NeonateDocumento47 páginasApproach To Sick NeonateblitheleevsAún no hay calificaciones
- Complicated Labor and DeliveryDocumento226 páginasComplicated Labor and Deliveryrhimineecat71100% (1)
- MK Fetal Lie and Presentation (OBGY)Documento9 páginasMK Fetal Lie and Presentation (OBGY)Moses Jr KazevuAún no hay calificaciones
- Bleeding in Early Late PregnancyDocumento46 páginasBleeding in Early Late PregnancyAndrada Catrinoiu100% (2)
- Non Communicable DiseaseDocumento13 páginasNon Communicable DiseaseClancy Anne Garcia Naval100% (1)
- Examination of The Newborn A Practical Guide PDFDocumento2 páginasExamination of The Newborn A Practical Guide PDFSick0% (1)
- Neonatal Resuscitation New GuidelinesDocumento11 páginasNeonatal Resuscitation New GuidelinesJl AAún no hay calificaciones
- Bladder Irrigation & InstallationDocumento12 páginasBladder Irrigation & InstallationSui NarcanAún no hay calificaciones
- MonsterABG LectureDocumento12 páginasMonsterABG LectureDanielleJalisaAún no hay calificaciones
- Free Paper Abstract BookDocumento1047 páginasFree Paper Abstract Bookkukadiya100% (1)
- Acute Fatty Liver Versus HELLPDocumento44 páginasAcute Fatty Liver Versus HELLPrainmaker77771121100% (1)
- Menu EngineeringDocumento4 páginasMenu Engineeringsebijoseph97Aún no hay calificaciones
- Fluid and Electrolyte TherapyDocumento39 páginasFluid and Electrolyte TherapyrikarzAún no hay calificaciones
- LeukemiaDocumento51 páginasLeukemiaCres Padua QuinzonAún no hay calificaciones
- Biopsy/Cytology/Exploratory ProceduresDocumento19 páginasBiopsy/Cytology/Exploratory ProceduresPrincewill SeiyefaAún no hay calificaciones
- (New) Early Pregnancy Complications RDocumento51 páginas(New) Early Pregnancy Complications RMesk Banat100% (2)
- AnestesiDocumento15 páginasAnestesiayang rasheldaAún no hay calificaciones
- Labour Ward HandbookDocumento29 páginasLabour Ward Handbookglow28Aún no hay calificaciones
- Medication ErrorsDocumento11 páginasMedication ErrorsJayson V Caranto RN100% (1)
- Fetal Growth Restriction - ACOG 2019Documento23 páginasFetal Growth Restriction - ACOG 2019Adhitya Yudha MaulanaAún no hay calificaciones
- Menopause Concept MapDocumento1 páginaMenopause Concept MapBritanny NelsonAún no hay calificaciones
- Update in AnaesthesiaDocumento52 páginasUpdate in AnaesthesiaRoy AAún no hay calificaciones
- Neo BFHI Core Document 2015 EditionDocumento71 páginasNeo BFHI Core Document 2015 EditionGastón FalconiAún no hay calificaciones
- Management of Epilepsy During PregnancyDocumento24 páginasManagement of Epilepsy During PregnancyClaudio UdjajaAún no hay calificaciones
- Evaluation of The Neonate With Seizures 2020Documento7 páginasEvaluation of The Neonate With Seizures 2020Eduardo Rios DuboisAún no hay calificaciones
- Benign Prostatic Hyperplasia (BPH) : By, Ms. Ekta. S. Patel, I Yr M.SC NursingDocumento71 páginasBenign Prostatic Hyperplasia (BPH) : By, Ms. Ekta. S. Patel, I Yr M.SC NursingannisanabilaasAún no hay calificaciones
- Chapter 15 The Peripheral Vascular System and Lymphatic SystemDocumento4 páginasChapter 15 The Peripheral Vascular System and Lymphatic SystemKhanh Hoang100% (1)
- Hospital Management System SoftwareDocumento11 páginasHospital Management System SoftwareNikesh Solanki50% (2)
- Acid Base DisordersDocumento5 páginasAcid Base DisordersMillenial VoiceAún no hay calificaciones
- RCOG Cardiac Disease and Pregnancy PDFDocumento18 páginasRCOG Cardiac Disease and Pregnancy PDFSteven SetioAún no hay calificaciones
- Nursing Family Community Wellness Diagnoses SuttonDocumento6 páginasNursing Family Community Wellness Diagnoses SuttonMaria LpzAún no hay calificaciones
- Pediatric Abdominal Assessment: Hind Al-SuwaisDocumento20 páginasPediatric Abdominal Assessment: Hind Al-SuwaisHINDAún no hay calificaciones
- Surgival Diseases in PregnancyDocumento4 páginasSurgival Diseases in PregnancyZeynep YılmaztürkAún no hay calificaciones
- Cholecystitis & Pregnancy - KSherafganDocumento41 páginasCholecystitis & Pregnancy - KSherafganIsharajul ShahAún no hay calificaciones
- Management of The Critically Ill Obstetric Patient: ReviewDocumento9 páginasManagement of The Critically Ill Obstetric Patient: ReviewAripinSyarifudinAún no hay calificaciones
- Preventive Medicine in Obstetrics Regarding Pregnancy Loss: Dr. Mohammed Abdalla Domiat General HospitalDocumento44 páginasPreventive Medicine in Obstetrics Regarding Pregnancy Loss: Dr. Mohammed Abdalla Domiat General HospitalCosmina Alina MoscuAún no hay calificaciones
- Core Clinical Cases in ObstetricsDocumento193 páginasCore Clinical Cases in Obstetricsshafijan100% (10)
- Ob-Gyn OsceDocumento2 páginasOb-Gyn Oscechristietwong100% (1)
- Past Years OSCE Answers - 2012Documento30 páginasPast Years OSCE Answers - 2012christietwongAún no hay calificaciones
- OBOSCEDocumento3 páginasOBOSCEchristietwongAún no hay calificaciones
- 35 HIVAntretroviralsDocumento15 páginas35 HIVAntretroviralschristietwongAún no hay calificaciones
- Cholinergic AgentsDocumento30 páginasCholinergic AgentschristietwongAún no hay calificaciones
- Physics MCAT Formula SheetDocumento35 páginasPhysics MCAT Formula Sheetthrowaway864Aún no hay calificaciones
- Lecture Reviews - Neuro ReviewsDocumento2 páginasLecture Reviews - Neuro ReviewschristietwongAún no hay calificaciones
- General PE Case Write-Up - Doctoring IIIDocumento5 páginasGeneral PE Case Write-Up - Doctoring IIIchristietwongAún no hay calificaciones
- Clerkship Handbook (Final)Documento89 páginasClerkship Handbook (Final)christietwongAún no hay calificaciones
- Exercise Physiology That Can Help Treat Patients With Cardiovascular Coronary Heart Disease in Patients Younger That 15Documento3 páginasExercise Physiology That Can Help Treat Patients With Cardiovascular Coronary Heart Disease in Patients Younger That 15christietwongAún no hay calificaciones
- Clerkship Handbook (Final)Documento89 páginasClerkship Handbook (Final)christietwongAún no hay calificaciones
- ChristieTWong - Comp Lication of Acute MI NotesDocumento60 páginasChristieTWong - Comp Lication of Acute MI NoteschristietwongAún no hay calificaciones
- Lecture Reviews - OrthoDocumento1 páginaLecture Reviews - OrthochristietwongAún no hay calificaciones
- Patho Logy C V Anat Omy and Histo LogyDocumento11 páginasPatho Logy C V Anat Omy and Histo LogychristietwongAún no hay calificaciones
- Chest Pain Case Write-Up - Doctoring IIIDocumento4 páginasChest Pain Case Write-Up - Doctoring IIIchristietwongAún no hay calificaciones
- Written Documentation Case Example Fall 2013 - Doctoring IIIDocumento3 páginasWritten Documentation Case Example Fall 2013 - Doctoring IIIchristietwongAún no hay calificaciones
- Written Documentation Skills I Fall 2013 - Doctoring IIIDocumento84 páginasWritten Documentation Skills I Fall 2013 - Doctoring IIIchristietwong100% (1)
- Chapterand 38Documento6 páginasChapterand 38wraith324Aún no hay calificaciones
- Antepartum HemorrhageDocumento5 páginasAntepartum Hemorrhagecode-24Aún no hay calificaciones
- A Reflective JournalDocumento4 páginasA Reflective JournallalaineAún no hay calificaciones
- Final FACT SHEET-SataraDocumento11 páginasFinal FACT SHEET-SataraChaitanya PawarAún no hay calificaciones
- Nursing-Care-Plan Case 1 LaquihonDocumento2 páginasNursing-Care-Plan Case 1 LaquihonRuby Jane LaquihonAún no hay calificaciones
- Anemia Mukt Bharat Brochure EnglishDocumento6 páginasAnemia Mukt Bharat Brochure EnglishAchint KumarAún no hay calificaciones
- Non Inmune Fetal Hydrops Oct 2013 PDFDocumento14 páginasNon Inmune Fetal Hydrops Oct 2013 PDFMariana González DíazAún no hay calificaciones
- NCPDocumento4 páginasNCPShella CondezAún no hay calificaciones
- Obesity and Diabetes Genetic Variants Associated With Gestational Weight GainDocumento17 páginasObesity and Diabetes Genetic Variants Associated With Gestational Weight GainEgie Nugraha Fitriyan ApriyadiAún no hay calificaciones
- CMAM Community Based Management ofDocumento18 páginasCMAM Community Based Management ofZia BalochAún no hay calificaciones
- Artículo 7000 PalabrasDocumento8 páginasArtículo 7000 PalabrasEmalaith BlackburnAún no hay calificaciones
- Drug Therapy in Pregnancy (Soal)Documento6 páginasDrug Therapy in Pregnancy (Soal)Yola FebriyantiAún no hay calificaciones
- STD PregnancyDocumento44 páginasSTD Pregnancymacybnz100% (1)
- Ebook Case Files Pediatrics 6E Oct 6 2021 - 126047495X - Mcgraw Hill PDF Full Chapter PDFDocumento67 páginasEbook Case Files Pediatrics 6E Oct 6 2021 - 126047495X - Mcgraw Hill PDF Full Chapter PDFserafina.rios491100% (26)
- Effectiveness of Nutrition Education of Adolescent GirlDocumento29 páginasEffectiveness of Nutrition Education of Adolescent GirlBushra FaridiAún no hay calificaciones
- Maternal and Child Health NSG SummaryDocumento2 páginasMaternal and Child Health NSG SummaryAshley Jane MacapayadAún no hay calificaciones
- Ao 2016-0035Documento9 páginasAo 2016-0035Donna Miranda100% (5)
- Adolescencents Pregnanncy in Baranggay Kimadzil, Carmen, CotabatoDocumento9 páginasAdolescencents Pregnanncy in Baranggay Kimadzil, Carmen, CotabatoRonnie OmarAún no hay calificaciones
- Induction of LabourDocumento45 páginasInduction of LabourVidya RamanathanAún no hay calificaciones
- Travatan (Travoprost Ophthalmic Solution) 0.004% SterileDocumento7 páginasTravatan (Travoprost Ophthalmic Solution) 0.004% SterileSyed Shariq AliAún no hay calificaciones
- Shoulder DystociaDocumento20 páginasShoulder DystociaDanielle Francis Hirang0% (1)
- Advantages (Pros) of AbortionDocumento3 páginasAdvantages (Pros) of AbortionKatrina BalimbinAún no hay calificaciones
- OGDocumento385 páginasOGMin MawAún no hay calificaciones
- Obat TeratogenikDocumento24 páginasObat TeratogenikHidayat BazeherAún no hay calificaciones
- 1 Maternal High Risk Intro Pregestational ConditionsDocumento90 páginas1 Maternal High Risk Intro Pregestational ConditionsKaren Joy Jacinto Ello100% (2)
- Michigan Adoption Resource Guide: - 2nd EditionDocumento20 páginasMichigan Adoption Resource Guide: - 2nd EditionAmy Jayne HawkinsAún no hay calificaciones
- PAHAL Quarterly Newsletter 10th Issue Apr June 2021Documento8 páginasPAHAL Quarterly Newsletter 10th Issue Apr June 2021Sriram ChandramohanAún no hay calificaciones
- FHIS Version 2014Documento254 páginasFHIS Version 2014Sphero Castillo100% (1)
- Obstetric ExaminationDocumento4 páginasObstetric ExaminationSusan GeorgeAún no hay calificaciones
- Gynecology Amp Obstetrics Bahavar Medicine LibraryDocumento9 páginasGynecology Amp Obstetrics Bahavar Medicine Librarykukadiya0% (1)