Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Prolonged Fever Occurring During Treatment of Pulmonary Tuberculosis - An Investigation of 40 Cases
Cargado por
সোমনাথ মহাপাত্র0 calificaciones0% encontró este documento útil (0 votos)
41 vistas3 páginasProlonged fever in pulmonary tuberculosis under treatment
Título original
ibrt01i3p147
Derechos de autor
© © All Rights Reserved
Formatos disponibles
PDF, TXT o lea en línea desde Scribd
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoProlonged fever in pulmonary tuberculosis under treatment
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PDF, TXT o lea en línea desde Scribd
0 calificaciones0% encontró este documento útil (0 votos)
41 vistas3 páginasProlonged Fever Occurring During Treatment of Pulmonary Tuberculosis - An Investigation of 40 Cases
Cargado por
সোমনাথ মহাপাত্রProlonged fever in pulmonary tuberculosis under treatment
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PDF, TXT o lea en línea desde Scribd
Está en la página 1de 3
Original Article
Ind. J. Tub. 2001,48, 147
PROLONGED FEVER OCCURRING DURING TREATMENT OF
PULMONARY TUBERCULOSIS - AN INVESTIGATION OF 40 CASES
Deepak Rosha*
(Received on 22.8.2000; Accepted on 6.2.2001)
Summary : A study that investigated the causes of prolonged fever or onset of fever during anti-tuberculosis treatment
(ATT) in sputum smear positive, HIV negative patients admitted in a TB sanatorium is reported. A total of 40 patients
were studied. All were males with ages ranging between 22 and 55 years (mean 43 years). There were 28(70%) patients who
had evidence of extra-pulmonary disease. It was found that fever occurred because of direct complications of tuberculosis
in 22.5%, tuberculous cold abscess in 12.5%, drug resistance in 10% and drug reaction in 22.5%. Other diseases were the
cause of fever in 32.5%. These included superaddcd lung infection, malaria, filariasis and amoebic liver abscess.
Key Words : Pulmonary Tuberculosis, Prolonged Fever, Treatment
INTRODUCTION
Fever occurs in 60-85% of patients afflicted
with tuberculosis. As a rule, every case of active
pulmonary tuberculosis may exhibit some degree of
pyrexia because it is one of the important signs of
disease activity
2
. Fever usually resolves by the
second week of starting chemotherapy
3
. Modern day
chemotherapy can achieve cure in virtually all
compliant patients
4
. However, there are patients who
remain febrile beyond a reasonable period of time or
develop fever during treatment. Such cases raise
issues such as quality of diagnosis, development of
drug resistance or associated cryptic disease
5
. This
study has been carried out to investigate the causes
of fever in such patients.
MATERIAL AND METHODS
The study was carried out in a tuberculosis
sanatorium where only male patients are admitted.
Only fresh sputum positive cases were eligible for
entry into the study, if they remained febrile for more
than 2 weeks after starting chemotherapy or if they
developed fever for 7 days while on treatment. Fever
was defined as mouth temperature >100 degrees
Fahrenheit at least once in 24 hours. The study
commenced on 1 December 1999 and ended on 30
September 2000. All patients were given standard
chemotherapy (2SHRZ/2EHRZ + 4HR), modified as
recommended
6
(for patients above 40 years of age
Ethambutol containing regimen, for those below 40
ears the Streptomycin regimen). All dosages were y
standardised for weight, as recommended
7
. Once
inducted into the study, the patients were examined
at least 3 times a week for development of any fresh
clinical finds, recorded weekly. Clinical examination
included palpation of liver, spleen, all sites of lymph
nodes, caecal area, spine, and fundoscopy. A high
calorie diet was provided (50 Kcal/kg) along with
high proteins (2g/kg) and vitamin supplements to all.
Sputum smears were examined once a week, serial
review of chest X-rays (CXR) and laboratory tests
as indicated in Table 1 carried out.
All the patients were classified according to
radiological extent of disease , evidence of extra-
pulmonary involvement and presence of toxemia as
follows:
1. Radiological extent:
a) Focal disease, minimal, where less than one
zone involved with non-cavitary disease on
CXR or severe if cavitation present.
b) Moderate disease, where more than one but
.less than 3 zones involved with non-cavitary
disease.
c) Extensive disease, where cavitation involved
more than one zone or non-cavitary disease
involving more than three zones.
2. Disseminated disease:
Defined as showing clinical, sonological,
radiological and/or laboratory evidence of
*Classified Specialist (Medicine & Respiratory Medicine) Military Hospital, Namkum. Ranchi, Jharkhand
Correspondence : Dr. Deepak Rosha, A-1/167. Safdarjung Enclave. New Delhi 110029
The Indian Journal of Tuberculosis
148
DI-EPAK ROSHA
involvement of extra-pulmonary organs excluding
pleura.
3. Toxemia:
Defined as presence of : (a) less than 90% of
expected body weight (b) serum albumin <3.5g%
(c) serum sodium <130 meqL (d) t uber cul i n
test(ITU) <5mm (e) normocytic normochromic
anemia with haemoglobin <8.0g%.
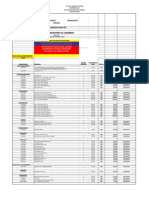
Table 1: Protocol for investigation of fever during
treatment for pulmonary tuberculosis
1. Complete blood counts done weekly
2. Peripheral blood smears for toxic granulation, type
of anemia, haemoparasites, abrormal cells etc.
3. Bone marrow studies*
4. Blood culture
5. Urine for pyogenic and M.tuberculosis cultures
6. Sputum smear examination
7. Tuberculin test (1TU)
8. Serial review of Chest X-Rays
9. Ultrasound of chest wall and abdomen
10. Anti-nuclear antibodies examination*
11. Cerebrospinal fluid examination*
12. CT Scan of chest and/or abdomen*
13. Bronchoscopy, bronchoalveolar lavage, biopsy*
14. Eliminate drug suspected of causing reaction
15. Repeated detailed clinical examination
* where indicated
RESULTS
A total of 40 patients were studied; all were
males, sputum smear positive for acid fast bacilli,
and HIV negative. Their ages ranged from 22 to 55
years with mean age, 43 years. Four patients had
diabetes mellitus, 2 had cirrhosis of liver and one
had dilated cardiomyopathy. There were 14 smokers
and 3 known cases of alcohol abuse.
There were 22 pat i ent s who had
radiologically extensive disease, 20 of these had
disease di ssemi nat i on to ot her organs and 12
had additional toxemia (Table 2). In all, 28(70%)
patients had extra-pulmonary involvement with the
disease.
Table 2: Classification of pulmonary tuberculosis cases
havi ng prolonged fever accordi ng to
radiological extent and di ssemination of
disease
Radiological
Not diss- Diss- Toxemia Total
extent eminated eminated &
disse-
mination
Extensive 2 8 12 22
Moderate 5 4 0 9
Focal Severe 2 2 0 4
Focal Minimal 3 2 0 5
12 16 12 40
The causes of fever as determined are given
in Table 3.
Table 3 : Causes of fever in patients of pulmonary
tuberculosis undergoing chemotherapy
Cause Number %
Direct complication of tuberculosis 9 22.5
Dissemination with toxemia alone 4
Potts disease with abscess 2
Loculatcd empyema 2
Tuberculous arthritis of hip with 1
abscess
Cold abscess 5 12.5
Mediastinal 2
Retroperitoneal 2
Retropectoral 1
Drug resistance 4 10.0
Drug reaction 9 22.5
Other illnesses 13 32.5
Pyogenic lung infection 6
Malaria 3
Others 4
It was seen that 9 patients had fever due to
direct complications of tuberculosis, i ncl udi ng
asymptomatic Potts disease wi t h para-spi nal
abscess in 2 patients and loculated empyema found
by ultra-sonography of the chest in 2 patients. One
patient had a minimally symptomatic tuberculous
arthritis of hip with peri-articular abscess. Cold
abscesses were seen in 5 patients, 2 mediastinal
abscesses detected by CT scan, and 2 retro pectoral
abscess by ultra sound. Drug resistance was seen
in 4 cases and these had multi drug resistance.
The Indian Journal of Tuberculosis
PROLONGED FEVER DURING TREATMFNT OF PULMONARY TUBERCULOSIS
149
Fever due to drug hypersensitivity reaction
was seen in 9 cases; perhaps Strepromycin associated
in 7 cases but without rash or eosinophilia and
Isoniazid induced lupus in 2 cases. There were 13
patients who had fever due to associated illnesses.
Of these, 6 patients had super-added pyogenic lung
infection and 3 patients had malaria.
DISCUSSION
The febrile response of body is to combat
infecting microbes. The response is generated by
the release of cytokines, notably interleukin-1 alpha
and tumor necrosis factor which are released in large
amounts in mycobacterial infections. Although short
term fevers may be beneficial, prolonged fevers cause
depletion of muscle mass and essentml nutrients
8
leading to malnutrition that ultimately weakens the
immune system. Thus, it is necessary to correctly
identify the underlying cause of fever and treat it
effectively.
When a patient of pulmonary tuberculosis
cont i nues to have fever despi t e t r eat ment or
developed fever during treatment, one has to consider
drug resistance and add second line drugs, or think
of hypersensitivity reaction producing fever and add
glucocorticoids. This study shows that both options
may be inappropriate since only 10% fevers were
due to dr ug resistance and 12.5% due to
hypersensitivity reaction (from cold abscess). The
more common cause of the fevers was concomitant
diseases (32.5%), of whi ch superadded l ung
infection formed the major part(15%). In such
situations, reliance has to be placed on sputum as
well as blood count studies. Search has to be made
for other causes diligently. Drug reaction was the
cause of fever in 22.5% of the cases as reported by
others
9
. In two patients (5%), Isoniazid induced
lupus was the cause of fever. These patients had
severe anaemia, hepatosplenomegaly and worsening
shadows on chest X-ray. Both the patients were
sputum negative, at this stage, and strongly positive
for anti-nuclear antibodies. There was marked
improvement after withdrawal of Isoniazid. This
phenomenon should be borne in mind as it might be
confused with drug resistance
10
.
There were 9(22.5%) fever cases due to
direct complications of tuberculosis. In 4 cases no
cause other than toxemia of tuberculosis could be
found and the fever resolved gradually. But in others,
a diligent search succeeded in locating the real cause.
This study shows that fevers developing
or persisting in patients undergoing treatment
for pulmonary tuberculosis require careful,
repeated clinical examination and detailed
investigations and should not be attributed to
tuberculosis alone, or the emergence of drug
resistance. Locally prevalent associated diseases
should be ruled out at first. Liberal use of
ultrasound should be made to detect pus
collections in the pleura, chest wall,
mediastinum, and retroperitoneal areas.
REFERENCES
1. Kiblawi SSO, Say SJ, Stondnll RB ct al. Fever response of
patients on therapy for pulmonary tuberculosis. Am Rev
RespDis 1981; 123:20
2. Barbes PF, Chan LS, Wong SF, The course ol lever during
treatment of pulmonary tuberculosis luhi-nlc 1987,
68:255
3. Tsao TC, Tsai YH, Lan RS, et al. l-ever characteristics in
tuberculosis-clinical observation of 597 cases, Chang Keng
I Hsueh Tsa Chih 1989; 12:81
4. Gryzybowski S. Fnarson DA, Kesul K in pul monar j
tuberculosis patients under various treatment programme
conditions. Bull Inl Tuherc 1978; 53:70
5. Mahmoudi A, Iseman MD. Pitfalls in care of patients with
tuberculosis. Common errors and their association with the
acquisition of drug resistance. JAMA 1993; 270:65
6. American Thoracic Society: Treatment of tuberculosis and
tuberculosis infections in adults and children. An official
statement of American Thoracic Society and Centres for
Disease Control and Prevention. Am J Resp Cril Care
Med
1994; 144:1359
7. Maher D, Chaulet P, Spi naci S, et al, Treatment of
tuberculosis: Guidelines for national programmes, Geneva,
WHO 1997:59
8. Atkins E, Fever. Historical aspects in Int erl euki n-l ,
Inflammation and Disease in Romford R, Henderson B,
Eds. New York, Elsevier Science, 1989; 3
9. Pitts FW, Tuberculosis,: Prevention and therapy, in Hook
EW, Mandell GL, Gwatlcney B, et al, Eds. In Current
concepts in infectious disease. New York, John Wiley, 1977;
181
10. Rothfield NF, Bierer WF-, Garfield JW, Isoniazid induction
of anti-nuclear antibodies Ann Inl Med 1978; 88
.
650
The Indian Journal of Tuberculosis
También podría gustarte
- Clinical Cases in PsychiatryDocumento161 páginasClinical Cases in PsychiatryAna Roman100% (35)
- Five Content Areas and Percent of Scored Test Items (Range) in Each AreaDocumento5 páginasFive Content Areas and Percent of Scored Test Items (Range) in Each Areaসোমনাথ মহাপাত্রAún no hay calificaciones
- Crohn's DiseaseDocumento46 páginasCrohn's Diseaseuttarasingh100% (3)
- Why GILD Remdesivir Is The Only Relevant Coronavirus DrugDocumento8 páginasWhy GILD Remdesivir Is The Only Relevant Coronavirus Drugjulia skripka-serry100% (2)
- Gastrointestinal Quiz AnswersDocumento5 páginasGastrointestinal Quiz AnswersFranciskhokhyx III100% (5)
- Paleopathology PDFDocumento14 páginasPaleopathology PDFRodrigo MictlanAún no hay calificaciones
- Infectious Disease Questions/Critical Care Board ReviewDocumento5 páginasInfectious Disease Questions/Critical Care Board ReviewAzmachamberAzmacareAún no hay calificaciones
- UWORLD Biostatistics Book Review PDFDocumento93 páginasUWORLD Biostatistics Book Review PDFসোমনাথ মহাপাত্র50% (2)
- Neuro Tract Lesions Ps230114Documento16 páginasNeuro Tract Lesions Ps230114সোমনাথ মহাপাত্রAún no hay calificaciones
- LeukoplakiaDocumento60 páginasLeukoplakiadimasahadiantoAún no hay calificaciones
- Thyroid Function Tests (TFTS)Documento27 páginasThyroid Function Tests (TFTS)ธิติวุฒิ แสงคล้อยAún no hay calificaciones
- Necrotizing PneumoniaDocumento7 páginasNecrotizing PneumoniaMahdalenaSyahAún no hay calificaciones
- NCP RHDocumento3 páginasNCP RHKirstie Durano Goc-ong0% (1)
- Overall Merit List MD Ms Jan2018 PUBLDocumento440 páginasOverall Merit List MD Ms Jan2018 PUBLসোমনাথ মহাপাত্র0% (1)
- Fast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlDe EverandFast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlAún no hay calificaciones
- Acute Bronchitis Case StudyDocumento6 páginasAcute Bronchitis Case Studyulka0750% (2)
- USMLE Step 1 NBME Top Concepts 2021Documento475 páginasUSMLE Step 1 NBME Top Concepts 2021dalia khamoAún no hay calificaciones
- PRADEEP'S - Brain TumorDocumento32 páginasPRADEEP'S - Brain TumorPRADEEPAún no hay calificaciones
- Manuscript Case Report Addison's Disease Due To Tuberculosis FinalDocumento22 páginasManuscript Case Report Addison's Disease Due To Tuberculosis FinalElisabeth PermatasariAún no hay calificaciones
- Difficulties in Diagnosis of Psittacosis or Ornithosis: A Case ReportDocumento4 páginasDifficulties in Diagnosis of Psittacosis or Ornithosis: A Case ReportYusrinabillaAún no hay calificaciones
- A Case of Typhoid Fever Presenting With Multiple ComplicationsDocumento4 páginasA Case of Typhoid Fever Presenting With Multiple ComplicationsCleo CaminadeAún no hay calificaciones
- Penggunaan Heparin Dosis Tinggi Pada Pasien COVID-19 Dengan ARDS Dan Hipertensi Di Unit Perawatan Intensif (ICU)Documento8 páginasPenggunaan Heparin Dosis Tinggi Pada Pasien COVID-19 Dengan ARDS Dan Hipertensi Di Unit Perawatan Intensif (ICU)Vicky LumalessilAún no hay calificaciones
- 51 Uysal EtalDocumento4 páginas51 Uysal EtaleditorijmrhsAún no hay calificaciones
- Pulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of LiteratureDocumento5 páginasPulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of Literatureamelya asryAún no hay calificaciones
- Orthinosis Query FeverDocumento6 páginasOrthinosis Query Feversomebody_maAún no hay calificaciones
- Unusual Cause of Fever in A 35-Year-Old Man: ECP YuenDocumento4 páginasUnusual Cause of Fever in A 35-Year-Old Man: ECP YuenhlAún no hay calificaciones
- Final SCRUB TYPHUS AS DIFFERENTIAL DIAGNOSIS OF COVIDDocumento6 páginasFinal SCRUB TYPHUS AS DIFFERENTIAL DIAGNOSIS OF COVIDDr Gaurav SinghAún no hay calificaciones
- Typhoid Fever and Viral Hepatitis in A g6pd DeficientDocumento2 páginasTyphoid Fever and Viral Hepatitis in A g6pd DeficientLoy GarikAún no hay calificaciones
- Neumonia Anciano 2014Documento8 páginasNeumonia Anciano 2014Riyandi MardanaAún no hay calificaciones
- Jurnal Maju DR ArifDocumento6 páginasJurnal Maju DR ArifRefta Hermawan Laksono SAún no hay calificaciones
- Case Report COVID-19 and Pulmonary Mycobacterium Tuberculosis CoinfectionDocumento4 páginasCase Report COVID-19 and Pulmonary Mycobacterium Tuberculosis CoinfectionNindie AulhieyaAún no hay calificaciones
- Pneumonia: V. Mandang, M.DDocumento44 páginasPneumonia: V. Mandang, M.DMeggy SumarnoAún no hay calificaciones
- A Rare Cause of Endocarditis: Streptococcus PyogenesDocumento3 páginasA Rare Cause of Endocarditis: Streptococcus PyogenesYusuf BrilliantAún no hay calificaciones
- Overview of Neutropenic Fever SyndromesDocumento16 páginasOverview of Neutropenic Fever Syndromesnon_zenseAún no hay calificaciones
- Pulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (ARDS) : A Case Report and Review of LiteratureDocumento5 páginasPulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (ARDS) : A Case Report and Review of LiteratureCimol AgustinaAún no hay calificaciones
- CONTINUATIONDocumento6 páginasCONTINUATIONBHAVANA VNAún no hay calificaciones
- Fever of Unknown Origin (Fuo) : DR Budi Enoch SPPDDocumento23 páginasFever of Unknown Origin (Fuo) : DR Budi Enoch SPPDRoby KieranAún no hay calificaciones
- Harrison's Infectious Diseases, Second EditionDocumento16 páginasHarrison's Infectious Diseases, Second EditionTorrecillas Luna María de los ÁngelesAún no hay calificaciones
- Management Booklet Coronavirus Disease MOHP - 2019 - 28marchDocumento22 páginasManagement Booklet Coronavirus Disease MOHP - 2019 - 28marchSanaa SbdelghanyAún no hay calificaciones
- BY DR Muhammad Akram M.C.H.JeddahDocumento32 páginasBY DR Muhammad Akram M.C.H.JeddahMuhammad Akram Qaim KhaniAún no hay calificaciones
- A Case of Lupus Pneumonitis Mimicking As Infective PneumoniaDocumento4 páginasA Case of Lupus Pneumonitis Mimicking As Infective PneumoniaIOSR Journal of PharmacyAún no hay calificaciones
- Ijcr 4045 20230703 V1Documento3 páginasIjcr 4045 20230703 V1haryatiAún no hay calificaciones
- Case LimaDocumento2 páginasCase LimaAnonymous 00nQE0Aún no hay calificaciones
- Acute Fulminent Leptospirosis With Multi-Organ Failure: Weil's DiseaseDocumento4 páginasAcute Fulminent Leptospirosis With Multi-Organ Failure: Weil's DiseaseMuhFarizaAudiAún no hay calificaciones
- Penggunaan Heparin Dosis Tinggi Pada Pasien COVID-19 Dengan ARDS Dan Hipertensi Di Unit Perawatan Intensif (ICU)Documento11 páginasPenggunaan Heparin Dosis Tinggi Pada Pasien COVID-19 Dengan ARDS Dan Hipertensi Di Unit Perawatan Intensif (ICU)Ariqa AzzhraAún no hay calificaciones
- Disseminated Tuberculosis in An AIDS/HIV-Infected Patient: AbstractDocumento3 páginasDisseminated Tuberculosis in An AIDS/HIV-Infected Patient: AbstractAmelia Fitria DewiAún no hay calificaciones
- Case Study 1 RRLDocumento4 páginasCase Study 1 RRLMae Arra Lecobu-anAún no hay calificaciones
- Case Report Typhoid Fever Complicated by Acute ResDocumento5 páginasCase Report Typhoid Fever Complicated by Acute ResVAMSHI LOCALAún no hay calificaciones
- COVID-19 and HELLP: Overlapping Clinical Pictures in Two Gravid PatientsDocumento4 páginasCOVID-19 and HELLP: Overlapping Clinical Pictures in Two Gravid PatientsDra Sandra VèlezAún no hay calificaciones
- Fever of Unknown Origin: The Journal of The Association of Physicians of India May 2004Documento6 páginasFever of Unknown Origin: The Journal of The Association of Physicians of India May 2004Sony NeovAún no hay calificaciones
- Respiratory Medicine CME: Lancelot Mark Pinto, Arpan Chandrakant Shah, Kushal Dipakkumar Shah, Zarir Farokh UdwadiaDocumento3 páginasRespiratory Medicine CME: Lancelot Mark Pinto, Arpan Chandrakant Shah, Kushal Dipakkumar Shah, Zarir Farokh UdwadiaLintang SuroyaAún no hay calificaciones
- Fever of Unknown OriginDocumento26 páginasFever of Unknown OriginFiona Yona Sitali100% (1)
- Work-Upforfeverduring Neutropeniaforboththe Stemcelltransplantrecipient Andthehematologicmalignancy PatientDocumento17 páginasWork-Upforfeverduring Neutropeniaforboththe Stemcelltransplantrecipient Andthehematologicmalignancy PatiententannabilakasdyAún no hay calificaciones
- Pneumonia Mimics: Pearls and Pitfalls: MAY 26TH, 2016Documento11 páginasPneumonia Mimics: Pearls and Pitfalls: MAY 26TH, 2016Marcel DocAún no hay calificaciones
- Jurnal Bahasa InggrisDocumento12 páginasJurnal Bahasa InggrisVanessa Angelica SitepuAún no hay calificaciones
- 68 JMSCRDocumento3 páginas68 JMSCRVani Junior LoverzAún no hay calificaciones
- Nonclostridial MyonecrosisDocumento9 páginasNonclostridial MyonecrosisTony Santos'sAún no hay calificaciones
- A 45-Year-Old Man With Shortness of Breath, Cough, and Fever BackgroundDocumento7 páginasA 45-Year-Old Man With Shortness of Breath, Cough, and Fever BackgroundFluffyyy BabyyyAún no hay calificaciones
- Jurnal Kedokteran Dan Kesehatan Indonesia: Indonesian Journal of Medicine and HealthDocumento6 páginasJurnal Kedokteran Dan Kesehatan Indonesia: Indonesian Journal of Medicine and HealthAimar rfAún no hay calificaciones
- 08 Pneumonia Review ofDocumento4 páginas08 Pneumonia Review ofMonika Margareta Maria ElviraAún no hay calificaciones
- A Young Traveller Presenting With Typhoid Fever After Oral Vaccination: A Case ReportDocumento9 páginasA Young Traveller Presenting With Typhoid Fever After Oral Vaccination: A Case ReportMarscha MaryuanaAún no hay calificaciones
- Cardiac Leptospirosis: Iralphuaborque Md14thbatch Hds DocharlabardaDocumento15 páginasCardiac Leptospirosis: Iralphuaborque Md14thbatch Hds DocharlabardaJr. CesingAún no hay calificaciones
- Lapsus Tifoid + DengueDocumento10 páginasLapsus Tifoid + DengueM.ThaufiqurrakhmanAún no hay calificaciones
- Value of Widal Test in The Diagnosis of Typhoid Fever: Original ArticleDocumento5 páginasValue of Widal Test in The Diagnosis of Typhoid Fever: Original ArticleguemadiAún no hay calificaciones
- Comparison of Clinical and Pathological Features of Lymph Node Tuberculosis and Histiocytic Necrotizing LymphadenitisDocumento8 páginasComparison of Clinical and Pathological Features of Lymph Node Tuberculosis and Histiocytic Necrotizing LymphadenitisfavorendaAún no hay calificaciones
- Adult Still's Disease and Respiratory Failure in A 74 Year Old WomanDocumento3 páginasAdult Still's Disease and Respiratory Failure in A 74 Year Old WomanEduardo Romero StéfaniAún no hay calificaciones
- IM GRP 3Documento11 páginasIM GRP 3Dale Maninantan De DiosAún no hay calificaciones
- A 65-Year-Old Man Came To The Emergency Department Via Ambulance - Relatives Accompanied The Patient and Described A 1-Day History of FeverDocumento43 páginasA 65-Year-Old Man Came To The Emergency Department Via Ambulance - Relatives Accompanied The Patient and Described A 1-Day History of FeverandriopaAún no hay calificaciones
- H (HBOT) (AD) : Olish Yperbaric EsearchDocumento6 páginasH (HBOT) (AD) : Olish Yperbaric EsearchervinstyaAún no hay calificaciones
- Case Study District Hospital - EtdDocumento7 páginasCase Study District Hospital - EtdWan AmeeramirulzamanAún no hay calificaciones
- TID 9999 E13413Documento5 páginasTID 9999 E13413saraabolghasemi1Aún no hay calificaciones
- Assignment On: SK Ahasanur Rahman Ashiq 1935043681, EMPH Fall 2020Documento15 páginasAssignment On: SK Ahasanur Rahman Ashiq 1935043681, EMPH Fall 2020Sk Ahasanur Rahman 1935043681Aún no hay calificaciones
- H (HBOT) (AD) : Olish Yperbaric EsearchDocumento6 páginasH (HBOT) (AD) : Olish Yperbaric EsearchVera MHAún no hay calificaciones
- Poster Discussion Room C1c - 10:45-12:45Documento5 páginasPoster Discussion Room C1c - 10:45-12:45aderina9032Aún no hay calificaciones
- CBT 15 1029Documento13 páginasCBT 15 1029সোমনাথ মহাপাত্রAún no hay calificaciones
- BD Biosciences Support - Protocols - Intracellular Staining of Human Red Blood CellsDocumento1 páginaBD Biosciences Support - Protocols - Intracellular Staining of Human Red Blood Cellsসোমনাথ মহাপাত্রAún no hay calificaciones
- Brandtzaeg 1981Documento14 páginasBrandtzaeg 1981সোমনাথ মহাপাত্রAún no hay calificaciones
- Account Statement As of 04-05-2020 19:48:27 GMT +0530Documento11 páginasAccount Statement As of 04-05-2020 19:48:27 GMT +0530সোমনাথ মহাপাত্রAún no hay calificaciones
- 1201020895PL IMillerDocumento26 páginas1201020895PL IMillerসোমনাথ মহাপাত্রAún no hay calificaciones
- Immune Recognition of Self Nucleic Acids Driven by Endogenous Antimicrobial Peptides: Role in AutoimmunityDocumento176 páginasImmune Recognition of Self Nucleic Acids Driven by Endogenous Antimicrobial Peptides: Role in Autoimmunityসোমনাথ মহাপাত্রAún no hay calificaciones
- Chapter 3 Haemoglobin Pattern Analysis: 3.1. Chromatographic Methods (For Hba Determination)Documento27 páginasChapter 3 Haemoglobin Pattern Analysis: 3.1. Chromatographic Methods (For Hba Determination)সোমনাথ মহাপাত্রAún no hay calificaciones
- DHR-ICMR Funded Workshops FormatDocumento3 páginasDHR-ICMR Funded Workshops Formatসোমনাথ মহাপাত্রAún no hay calificaciones
- 149 FullDocumento10 páginas149 Fullসোমনাথ মহাপাত্রAún no hay calificaciones
- Cell-Cell Interactions: Concept OutlineDocumento18 páginasCell-Cell Interactions: Concept Outlineসোমনাথ মহাপাত্রAún no hay calificaciones
- Icmr Talent FormDocumento2 páginasIcmr Talent Formসোমনাথ মহাপাত্রAún no hay calificaciones
- ElectivesDocumento5 páginasElectivesসোমনাথ মহাপাত্র100% (1)
- Observership Application ST - VincentsDocumento2 páginasObservership Application ST - Vincentsসোমনাথ মহাপাত্রAún no hay calificaciones
- Boards and Beyound Step 2 Cs PalpitationsDocumento4 páginasBoards and Beyound Step 2 Cs Palpitationsসোমনাথ মহাপাত্রAún no hay calificaciones
- Griffin Observership ApplicationDocumento7 páginasGriffin Observership Applicationসোমনাথ মহাপাত্রAún no hay calificaciones
- Visiting Scholar ChecklistDocumento9 páginasVisiting Scholar Checklistসোমনাথ মহাপাত্রAún no hay calificaciones
- PRISMA 2009 Flow Diagram PDFDocumento1 páginaPRISMA 2009 Flow Diagram PDFসোমনাথ মহাপাত্রAún no hay calificaciones
- Oral Halitosis: Definitions: Breath Malodor, Defined As Foul or Offensive Odor of Expired Air, May BeDocumento7 páginasOral Halitosis: Definitions: Breath Malodor, Defined As Foul or Offensive Odor of Expired Air, May BeSnowAún no hay calificaciones
- Spontaneous Intracerebral HaemorrhageDocumento3 páginasSpontaneous Intracerebral Haemorrhageselvie87Aún no hay calificaciones
- Assess Appropriateness For Clinical Condition. Heart Rate Typically 50/min If BradyarrhythmiaDocumento1 páginaAssess Appropriateness For Clinical Condition. Heart Rate Typically 50/min If BradyarrhythmiaatikaAún no hay calificaciones
- READINGDocumento21 páginasREADINGdiya baby100% (1)
- Pleural EffusionDocumento23 páginasPleural EffusionYousra ShaikhAún no hay calificaciones
- Hydatidiform Mole Study GuideDocumento4 páginasHydatidiform Mole Study GuideCarl Elexer Cuyugan AnoAún no hay calificaciones
- Script For Gradderall XVDocumento4 páginasScript For Gradderall XVapi-273399286Aún no hay calificaciones
- ESC Guideline 2018Documento84 páginasESC Guideline 2018Ganjar AdityoAún no hay calificaciones
- GlaucomaDocumento15 páginasGlaucomaAmalliaPradisthaAún no hay calificaciones
- K10 - ISK AtasDocumento39 páginasK10 - ISK AtasfelixAún no hay calificaciones
- Andrés Felipe Cardona: Eduardo Obando)Documento3 páginasAndrés Felipe Cardona: Eduardo Obando)Zarit Diseños CaliAún no hay calificaciones
- Anxiety and Hypertension Is There A Link A LiteratDocumento8 páginasAnxiety and Hypertension Is There A Link A LiteratDr. Mohammad Tanvir IslamAún no hay calificaciones
- 16/09/2015 1 Mujtaba AshrafDocumento44 páginas16/09/2015 1 Mujtaba Ashrafதீரன் சக்திவேல்Aún no hay calificaciones
- PancretitisDocumento44 páginasPancretitisMohammad Husni BanisalmanAún no hay calificaciones
- PLAGUE: Medical Management and Countermeasure Development.Documento52 páginasPLAGUE: Medical Management and Countermeasure Development.Dmitri PopovAún no hay calificaciones
- Brain Tumor New 1Documento6 páginasBrain Tumor New 1Tiiffanyy Faiith PadillaAún no hay calificaciones
- Colonic Carcinoma Case StudyDocumento23 páginasColonic Carcinoma Case StudyGlaiza Claire Am-amlan OlayanAún no hay calificaciones
- 02VBL PemphigusDocumento48 páginas02VBL PemphigusRaniya ZainAún no hay calificaciones
- Fragile X SyndromeDocumento5 páginasFragile X SyndromeAdam LechnerAún no hay calificaciones
- Malaria in Pregnancy. NewDocumento23 páginasMalaria in Pregnancy. Newgloriashirima8Aún no hay calificaciones
- ScenarioDocumento3 páginasScenarioporo rowAún no hay calificaciones