Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Journal Medicine: The New England
Cargado por
'Muhamad Rofiq Anwar'Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Journal Medicine: The New England
Cargado por
'Muhamad Rofiq Anwar'Copyright:
Formatos disponibles
Vol ume 336 Number 22
1541
The New England
Journal
of
Medicine
Copyr i ght, 1997, by t he Massachuset ts Medi cal Soci et y
VOLUME 336
M
AY
29, 1997
NUMBER 22
COMPARISON OF CONVENTIONAL ANTERIOR SURGERY AND LAPAROSCOPIC
SURGERY FOR INGUINAL-HERNIA REPAIR
M
IKE
S.L. L
IEM
, M.D., Y
OLANDA
VAN
DER
G
RAAF
, M.D., C
EES
J.
VAN
S
TEENSEL
, M.D., R
OELOF
U. B
OELHOUWER
, M.D.,
G
EERT
-J
AN
C
LEVERS
, M.D., W
ILLEM
S. M
EIJER
, M.D., L
AURENTS
P.S. S
TASSEN
, M.D., J
OHANNES
P. V
ENTE
, M.D.,
W
IBO
F. W
EIDEMA
, M.D., A
UGUSTINUS
J.P. S
CHRIJVERS
, P
H
.D.,
AND
T
HEO
J.M.V.
VAN
V
ROONHOVEN
, M.D.
A
BSTRACT
Background
Inguinal hernias can be repaired by
laparoscopic techniques, which have had better re-
sults than open surgery in several small studies.
Methods
We performed a randomized, multicenter
trial in which 487 patients with inguinal hernias were
treated by extraperitoneal laparoscopic repair and
507 patients were treated by conventional anterior
repair. We recorded information about postoperative
recovery and complications and examined the pa-
tients for recurrences one and six weeks, six months,
and one and two years after surgery.
Results
Six patients in the open-surgery group but
none in the laparoscopic-surgery group had wound
abscesses (P
0.03), and the patients in the laparo-
scopic-surgery group had a more rapid recovery
(median time to the resumption of normal daily
activity, 6 vs.10 days; time to the return to work, 14
vs. 21 days; and time to the resumption of athletic
activities, 24 vs. 36 days; P
0.001 for all compari-
sons). With a median follow-up of 607 days, 31 pa-
tients (6 percent) in the open-surgery group had re-
currences, as compared with 17 patients (3 percent)
in the laparoscopic-surgery group (P
0.05). All but
three of the recurrences in the latter group were with-
in one year after surgery and were caused by sur-
geon-related errors. In the open-surgery group, 15 pa-
tients had recurrences during the first year, and 16
during the second year. Follow-up was complete for
97 percent of the patients.
Conclusions
Patients with inguinal hernias who
undergo laparoscopic repair recover more rapidly and
have fewer recurrences than those who undergo open
surgical repair. (N Engl J Med 1997;336:1541-7.)
1997, Massachusetts Medical Society.
From the Department of Surgery, University Hospital Utrecht, Utrecht
(M.S.L.L., T.J.M.V.V.); the Department of Epidemiology and Public
Health, University of Utrecht, Utrecht (Y.G., A.J.P.S.); the Department of
Surgery, Ikazia Hospital, Rotterdam (C.J.S., R.U.B., W.F.W.); the Depart-
ment of Surgery, Diakonessenhuis, Utrecht (G.-J.C.); the Department of
Surgery, St. Clara Hospital, Rotterdam (W.S.M.); the Department of Sur-
gery, Reinier de Graaf Gasthuis, Delft (L.P.S.S.); and the Department of
Surgery, Hofpoort Hospital, Woerden (J.P.V.) all in the Netherlands.
Address reprint requests to Dr. Liem at the Department of General Sur-
gery, University Hospital Utrecht, G04.228, P.O. Box 85.500, 3508 GA
Utrecht, the Netherlands.
NGUINAL hernias are common, and although
the results of surgical repair are often satisfac-
tory, postoperative recovery may be slow, and
the hernia may recur. The period of recovery
after repair of inguinal hernia in patients with paid
recovery time is four to six weeks in most Western
countries.
1-4
Elimination of anxiety about resuming
work could shorten the recovery, but this possibility
has not been studied.
5
Recurrence rates have ranged from less than 1 per-
cent to more than 10 percent, with a follow-up of
more than five years.
4,6
These data should be viewed
with some caution, however, because follow-up data
are often incomplete and unreliable.
4,7
Indeed, the
overall recurrence rate in the Netherlands, the Unit-
ed Kingdom, and the United States and the results
of large, prospective, controlled studies suggest high-
er rates (up to 15 percent after five years).
3,7-9
Laparoscopic techniques for the repair of inguinal
hernias have recently been introduced,
10,11
and in
several small trials, these techniques proved superior
to open repair in terms of postoperative pain and re-
covery.
12,13
These studies were too small, however, to
detect differences in recurrence rates.
8,14-16
We conducted a multicenter, randomized study
to compare conventional anterior repair with extra-
peritoneal laparoscopic repair in terms of postoper-
I
The New England Journal of Medicine
Downloaded from nejm.org on April 19, 2013. For personal use only. No other uses without permission.
Copyright 1997 Massachusetts Medical Society. All rights reserved.
1542
May 29, 1997
The New Engl and Journal of Medi ci ne
ative recovery, complications, and recurrence rates
in patients with primary or first recurrent unilateral
hernias.
METHODS
We selected teaching and nonteaching hospitals in rural and ur-
ban regions for this study. The sex and age distributions of the
people living in these regions were similar to those in the Nether-
lands as a whole.
17
The surgeons in participating hospitals en-
rolled patients in the study. The study was approved by the ethics
committees at all the hospitals and by the Dutch Health Insur-
ance Council, and all patients gave informed consent.
Characteristics of the Patients
Patients over 20 years old who presented with clinically diag-
nosed, unilateral inguinal hernias (primary hernias or first recur-
rences) who were scheduled to undergo surgical repair with gen-
eral anesthesia were eligible for the study. Exclusion criteria were
an additional surgical intervention planned during the hernia re-
pair; a history of extensive lower abdominal surgery, severe local
inflammation, or radiotherapy; advanced pregnancy (
12 weeks
gestation); and previous participation in the study (contralateral
hernia). Patients who were mentally incompetent or not able to
speak Dutch were also excluded.
Base-Line Studies
A standardized history was obtained, and a physical examina-
tion performed. Before randomization, the patients were told
both orally and in writing that they should resume normal activ-
ity after surgery, including work and sports, when they felt able
to do so. It was emphasized that this recommendation applied to
both surgical techniques.
Random Assignment to Treatment Groups
The patients were randomly assigned to either conventional an-
terior repair or extraperitoneal laparoscopic repair, with the as-
signments made at a central office. Randomization was carried out
by telephone, according to a computer-generated list, in groups of
25 or 50 patients; within each of these groups, the maximal allow-
able difference in the number of patients assigned to the two treat-
ments was 4. To ensure an equal distribution of patients in the
two treatment groups, they were stratified according to the hos-
pital and the type of hernia (primary or first recurrent).
Surgical Techniques
All 87 surgeons and residents who performed hernia repairs us-
ing the conventional anterior approach were experienced in this
technique or were supervised by an experienced surgeon. The re-
pair consisted of a reduction of the hernia, ligation of the hernial
sac, if necessary, and reconstruction of the inguinal floor with
nonabsorbable sutures, if necessary. A mesh prosthesis was not
used unless adequate repair was otherwise not possible.
Of the 87 surgeons and residents, 23 also performed laparo-
scopic repairs. They had ample experience with other laparoscopic
procedures and acquired experience with this particular procedure
under the supervision of experienced surgeons before they were
allowed to participate in the trial.
The laparoscopic technique has been described elsewhere.
18
It
was usually performed with the patient under general anesthesia.
Balloon dissection was used to develop the preperitoneal space
without entering the abdominal cavity. Extensive lateral dissec-
tion was performed, with isolation and manipulation of the struc-
tures of the spermatic cord. A polypropylene mesh (10 cm by 15
cm) was placed over the myopectineal orifice. The mesh was not
split and was not fixed in place. Patients were catheterized only if
a full bladder was suspected. Prophylactic antibiotic therapy was
not commonly given in either group.
Data Collection and Follow-up
Standardized data collection was performed by the attending
resident or surgeon, and each patient was evaluated at the hospi-
tal monthly by a physician or data manager from the central study
office. The hernia was classified as type I, II, III (subtype A, B,
or C), or IV (subtype A, B, or C), according to the classification
of Nyhus.
19
The operation time was defined as the time from the
first incision to the placement of the last suture.
We collected information about multiple operative and postop-
erative complications. The operative complications were bleeding
from epigastric or testicular vessels, injury to the vas deferens,
nerve injuries, peritoneal defects or defects in the hernial sac,
pneumoscrotum, and technical defects of laparoscopic instru-
ments or equipment. Cardiovascular complications during sur-
gery were defined as a fall in the diastolic pressure to a level below
50 mm Hg or cardiac arrhythmia. Discontinuation of the original
laparoscopic procedure in favor of either a transperitoneal laparo-
scopic procedure or a conventional procedure was also recorded
as a complication.
6
Postoperatively, all potential complications, such as hematoma,
seroma, chronic pain, and wound infection, were assessed and
documented. A serious wound infection was defined as the pres-
ence of pus or sanguinopurulent discharge at the operative site.
A urinary tract infection or epididymitis was recorded only if an-
tibiotic treatment was prescribed. Urinary retention was defined
as an inability to urinate, requiring catheterization. Postoperative
bleeding was recorded if compression was required to control it.
The length of hospitalization, defined as the number of days in
the hospital after the day of surgery, was also recorded. Patients
were discharged from the hospital if there was no serious infec-
tion or bleeding, the patient was able to walk, and only oral an-
algesic therapy was required to manage pain.
The patients were requested to return to the outpatient clinic
at one and six weeks; at six months; and at one and two years for
a standardized history taking and physical examination by a resi-
dent and, in most cases, by the surgeon who had performed the
surgery. The patients were asked to assess the severity of pain at
the operative site every day for the first week and at two and six
weeks, with the use of a 100-mm visual-analogue scale (scores
ranged from 0, for no pain, to 100, for unbearable pain), and to
record the use of analgesic drugs. Oral analgesia, initially aceta-
minophen (500 mg) or a nonsteroidal antiinflammatory drug, was
given on request. Chronic pain was defined as pain in the groin,
scrotum, or medial part of the thigh that was serious enough for
the patient to mention at six months.
The activities of daily living were assessed with a questionnaire
from a Dutch health survey,
20
modified to include questions ap-
plicable to patients who had undergone inguinal-hernia repairs.
The scale ranged from 0 (worst score) to 100 (best score).
21
The
modified questionnaire was validated in 110 of the patients. The
testretest reliability was 0.89.
21,22
The questionnaire was admin-
istered one day and one, two, and six weeks after surgery. The pa-
tients were also asked to record in a diary the dates on which they
resumed normal daily activity at home, returned to work, and re-
sumed their usual athletic activities.
Since differences in advice about returning to work after in-
guinal hernia repair may affect the validity of this end point,
1,21,23
all study surgeons and other personnel were instructed to give the
same advice about the resumption of work and other activities.
In addition, the patients physicians received a letter explaining
the trial and stating that the patients should not limit their activ-
ities but do whatever they felt able to do.
5,21
All patients were
either visited or contacted by telephone by a member of the cen-
tral study office, who was unaware of the treatment assignments,
soon after discharge to explain the importance of keeping the di-
ary and answer any questions about the follow-up and resump-
tion of usual activities.
Home visits by experienced physicians were also conducted one
and two years postoperatively if patients were unable or did not
want to go to the hospital. Follow-up data were considered com-
The New England Journal of Medicine
Downloaded from nejm.org on April 19, 2013. For personal use only. No other uses without permission.
Copyright 1997 Massachusetts Medical Society. All rights reserved.
CONVENTI ONAL ANTERI OR SURGERY VERSUS LAPAROSCOPI C SURGERY FOR I NGUI NAL- HERNI A REPAI R
Vol ume 336 Number 22
1543
plete only if they included the results of follow-up physical exam-
inations by an experienced physician at the planned times.
End Points
The primary end point of the study was a recurrence of the her-
nia, defined as a clinically detectable swelling in the groin or a
clearly palpable defect of the abdominal wall in the groin, diag-
nosed by two physicians. If a physician was unsure whether there
was a recurrence, the physical examination was repeated or ultra-
sonography of the groin was performed.
The main secondary end point was time off from work, defined
as the number of days between the day of surgery and the first
day a patient returned to work, for all patients who were em-
ployed. All deaths were assessed in terms of immediate cause and
the relation of the death to the hernia operation. The resumption
of usual activities, the score on the activities-of-daily-living ques-
tionnaire, postoperative pain, and complications were additional
secondary end points.
Statistical Analysis
In the main analyses, we compared conventional open surgery
and laparoscopic surgery with respect to the interval between sur-
gery and the diagnosis of a recurrence or the return to work. Data
for all patients who were randomly assigned to a treatment group
and underwent surgery were analyzed on an intention-to-treat
basis. In this analysis, we did not include patients without hernias,
those who withdrew their consent before undergoing surgery,
those who at the time of surgery were found to be poor candi-
dates for general anesthesia, and those who did not undergo the
assigned operation because of a misunderstanding resulting in an
unplanned open or laparoscopic repair. No interim analyses were
performed.
Continuous, normally distributed data are expressed as means
SD; other continuous data are expressed as medians with inter-
quartile ranges. For the analysis of differences between groups, we
used two-tailed t-tests or, if the results were not normally distrib-
uted, nonparametric tests. Chi-square or Fishers exact tests were
used to compare proportions. An analysis of variance for repeated
measurements was performed to compare the pain scores for the
two groups. Recurrence-free survival and the time to the resump-
tion of normal activity (i.e., daily home activity, paid work, and
sports) were analyzed with KaplanMeier survival curves, and dif-
ferences between the two treatment groups were compared by
the log-rank test. All reported P values are two-tailed.
RESULTS
We enrolled 1051 patients in the study between
February 1994 and June 1995. During this time,
114 eligible patients were not enrolled: 74 refused
to participate, 27 could not understand the proto-
col, and 13 were not enrolled for a variety of rea-
sons. Of the 1051 enrolled patients, 31 (13 assigned
to the open-surgery group and 18 assigned to the
laparoscopic-surgery group) decided not to undergo
surgery, in most cases because of the absence of se-
rious symptoms. Only three of these patients have
subsequently undergone surgery.
Eighteen patients (8 in the open-surgery group
and 10 in the laparoscopic-surgery group) were ex-
cluded. Three of these patients had bilateral repairs,
four were considered to be poor candidates for gen-
eral anesthesia, and three were found not to have in-
guinal hernias at surgery. An additional eight with-
drew informed consent: two wanted open repairs,
three wanted laparoscopic repairs, two refused annu-
al follow-up, and one underwent surgery at another
hospital. In addition, eight patients did not undergo
the assigned procedure because of a misunderstand-
ing between the central office and the surgeon, with
six of the patients undergoing unplanned open re-
pairs and two undergoing unplanned laparoscopic
repairs.
Hence, our main analysis is based on data from
487 patients who underwent laparoscopic repairs
and 507 who underwent open repairs. Randomiza-
tion was successful, and the two groups were similar
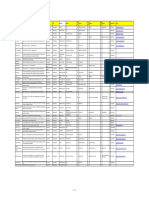
at base line (Table 1). A second analysis of recur-
rence rates included the 8 patients who did not un-
*Plusminus values are means
SD.
ADL denotes activities of daily living.
T
ABLE
1.
B
ASE
-L
INE
C
HARACTERISTICS
OF
994
P
ATIENTS
WITH
I
NGUINAL
H
ERNIAS
R
EPAIRED
WITH
O
PEN
OR
L
APAROSCOPIC
S
URGERY
.*
C
HARACTERISTIC
O
PEN
S
URGERY
(N
507)
L
APAROSCOPIC
S
URGERY
(N
487)
Age yr 55
15 55
16
Sex no. (%)
Male 485 (96) 461 (95)
Female 22 (4) 26 (5)
Height m 1.78
0.08 1.78
0.08
Weight kg 78.0
10.3 77.9
11.8
ADL score
Median
Interquartile range
94
83100
94
83100
Paid work no. (%) 278 (55) 266 (55)
Participation in sports
no. (%)
177 (35) 198 (41)
Primary hernia no. (%) 447 (88) 432 (89)
First recurrent hernia
no. (%)
60 (12) 55 (11)
History of contralateral
hernia no. (%)
14 (3) 28 (6)
Clinical presentation
no. (%)
Swelling in the groin 477 (94) 454 (93)
Discomfort or pain 423 (83) 416 (85)
Coincidental discovery 29 (6) 13 (3)
Potential risk factors for
recurrence no. (%)
Chronic obstructive
pulmonary disease
50 (10) 48 (10)
Benign hyperplasia of
the prostate
25 (5) 37 (8)
Constipation 25 (5) 26 (5)
Strenuous activity 122 (24) 103 (21)
Characteristics of hernia
no. (%)
Left-sided 245 (48) 243 (50)
Right-sided 262 (52) 244 (50)
Medial 267 (53) 259 (53)
Lateral 230 (45) 214 (44)
Unknown 10 (2) 13 (3)
Medial and lateral
(pantaloon)
12 (2) 8 (2)
Scrotal 17 (3) 24 (5)
The New England Journal of Medicine
Downloaded from nejm.org on April 19, 2013. For personal use only. No other uses without permission.
Copyright 1997 Massachusetts Medical Society. All rights reserved.
1544
May 29, 1997
The New Engl and Journal of Medi ci ne
dergo the assigned operation (for a total of 493 pa-
tients in the laparoscopic-surgery group and 509 in
the open-surgery group).
Perioperative and Early Postoperative Results
The mean time from randomization to surgery
was 33
36 days in the open-surgery group and
35
33 days in the laparoscopic-surgery group. In
the open-surgery group, a herniotomy with a high
ligation of the hernial sac was performed in 21 pa-
tients (4 percent). This procedure was combined
with a narrowing of the internal ring with sutures in
44 (9 percent), and a mesh prosthesis was inserted
and a so-called tension-free repair performed in 15
(3 percent). The remaining 427 patients underwent
hernioplasty, with a Bassini technique used in 147
patients (29 percent), a Shouldice technique in 112
(22 percent), a BassiniMcVay technique in 97 (19
percent), a McVay technique in 46 (9 percent), and
various other, less well known techniques in the oth-
er patients. The number of operations per surgeon
ranged from 1 to 33. In the laparoscopic-surgery
group, the range was 1 to 74.
The Nyhus classification of the hernias and the
operative and early postoperative complications in
the two groups are shown in Table 2. The median
duration of surgery was five minutes shorter for the
conventional repair than for the laparoscopic repair.
In the laparoscopic-surgery group, an open proce-
dure was used in 20 patients and a transabdominal
preperitoneal laparoscopic procedure was used in
4 (Table 3). During laparoscopic surgery, 115 pa-
tients (24 percent) had peritoneal tears, but in only
8 of these patients (7 percent) did the tear result in
loss of pneumopreperitoneum, requiring a switch to
another technique. In 15 patients (3 percent), the
epigastric vessels were ligated because they blocked
the view of the surgeon; in 2 patients, these vessels
were ligated after being injured during the insertion
of a trocar. After surgery, 64 patients had a pneumo-
scrotum (13 percent), which disappeared within one
day in all but 3 patients (Table 2). The most severe
postoperative complications were serious wound in-
fections in six patients in the open-surgery group
(Table 2); two of these patients had to be rehospi-
talized.
Postoperative Recovery
The visual-analogue pain scores after surgery were
lower in the laparoscopic-surgery group than in the
open-surgery group (P
0.001), although the differ-
ence diminished with time (Fig. 1). Seventeen pa-
tients in the laparoscopic-surgery group and 27 in
the open-surgery group did not record pain scores;
complete data were available for 90 percent of the
patients. On the day of surgery, 288 patients (59
percent) in the laparoscopic-surgery group did not
require any analgesic drugs for postoperative pain, as
compared with 165 patients (33 percent) in the
open-surgery group. The proportions of patients
not requiring analgesia were 88 and 82 percent, re-
spectively, at one week and 92 and 91 percent, re-
spectively, at six weeks.
The patients in the laparoscopic-surgery group
were able to resume normal activity sooner than the
patients in the open-surgery group (Table 4). Scores
*Type I is an indirect hernia with a normal internal abdominal ring. Type
II is an indirect hernia with an enlarged and distorted internal abdominal
ring and an intact posterior wall. Type III is a hernia with a posterior-wall
defect (A, direct; B, indirect [also pantaloon or scrotal]; or C, femoral).
Type IV is a recurrent hernia (A, direct; B, indirect [also pantaloon]; or
C, femoral).
T
ABLE
2.
C
HARACTERISTICS
OF
S
URGERY
AND
O
PERATIVE
AND
E
ARLY
P
OSTOPERATIVE
C
OMPLICATIONS
.
CHARACTERISTIC
OPEN SURGERY
(N507)
LAPAROSCOPIC
SURGERY
(N487)
P
VALUE
Operation time min
Median
Interquartile range
40
3045
45
3560
0.001
no. of patients (%)
Anesthesia
General 201 (40) 481 (99)
Spinal 306 (60) 6 (1)
Prophylactic antibiotics 16 (3) 7 (1)
Nyhus classification*
Type I 45 (9) 25 (5)
Type II 129 (25) 199 (41)
Type III
A 121 (24) 95 (20)
B 151 (30) 113 (23)
C 1 (1) 0
Type IV
A 36 (7) 24 (5)
B 23 (5) 30 (6)
C 1 (1) 0
Operative complications
Switch to another surgical
technique
24 (5)
Cardiovascular complica-
tions
1 (1) 2 (1) 0.62
Vas deferens injury 1 (1) 1 (1) 1.00
Arterial bleeding (clips or
ligatures required)
2 (1) 7 (1) 0.10
Balloon rupture during
dissection
6 (1)
Use of extra trocar 2 (1)
Broken instruments 0 2 (1) 0.24
Postoperative complications
Related death 0 0
Serious wound infection
(abscess)
6 (1) 0 0.03
Wound infection requiring
rehospitalization
2 (1) 0 0.50
Urinary tract infection 2 (1) 1 (1) 1.0
Epididymitis 2 (1) 3 (1) 0.68
Urinary retention 2 (1) 5 (1) 0.28
Bleeding 1 (1) 1 (1) 1.00
Chronic pain 70 (14) 10 (2) 0.001
Hematoma at 6 weeks 14 (3) 24 (5) 0.07
Seroma at 6 weeks 0 7 (1) 0.007
Pneumoscrotum at dis-
charge from hospital
3 (1)
The New England Journal of Medicine
Downloaded from nejm.org on April 19, 2013. For personal use only. No other uses without permission.
Copyright 1997 Massachusetts Medical Society. All rights reserved.
CONVENTI ONAL ANTERI OR SURGERY VERSUS LAPAROSCOPI C SURGERY FOR I NGUI NAL- HERNI A REPAI R
Vol ume 336 Number 22 1545
on the activities-of-daily-living questionnaire, which
were available for 98 percent of the patients, were
higher in the laparoscopic-surgery group at all times.
Complications and Recurrences
The median follow-up was 607 days (interquartile
range, 369 to 731). Recurrences were diagnosed in
31 patients (6 percent) in the open-surgery group
and 17 (3 percent) in the laparoscopic-surgery group
(P0.05) (Fig. 2). There were 11 deaths in the
open-surgery group and 6 in the laparoscopic-sur-
gery group, all of which were unrelated to the hernia
operation. All but 32 patients (3 percent) were ex-
amined in 1996.
Among the 17 patients in the laparoscopic-sur-
gery group who had recurrences, 10 (59 percent)
were operated on by surgeons who had just begun
to perform the operation independently. Six of these
10 patients were operated on by one surgeon, and
3 of his subsequent patients had recurrences. Four-
teen of the 17 recurrences (82 percent) in this group
occurred within the first year after surgery, whereas
in the open-surgery group 15 recurrences were di-
agnosed during the first year after surgery, and 16
during the second year. All but 12 of the 48 patients
with recurrences subsequently underwent additional
surgery, at which time the recurrence was con-
firmed.
The difference in the rates of recurrence between
the two groups was similar (P0.05) when the eight
patients who did not undergo the assigned operation
were included in the analysis.
DISCUSSION
The results of this study indicate that patients
with inguinal hernias recover more rapidly and have
fewer recurrences after laparoscopic repair than after
open repair. The duration of surgery was only slight-
ly longer (five minutes) with laparoscopic repair, pro-
viding little support for the widespread belief that
this procedure is more time-consuming than open
surgery. Nearly all the laparoscopic operations were
performed with general anesthesia, whereas 60 per-
cent of the open operations were performed with
spinal anesthesia. The use of general anesthesia might
be considered a disadvantage of laparoscopic repair.
Nevertheless, the patients in the laparoscopic-sur-
gery group were discharged from the hospital soon-
er and had less early and late postoperative pain than
the patients in the open-surgery group.
The difference in the rates of recurrence in the
two groups would appear to be clinically important.
With prolonged follow-up, more recurrences may be
expected in the open-surgery group,
9
and these late
recurrences may be prevented only by reinforcing
the groin region with additional support.
24
A late re-
currence after laparoscopic surgery may be uncom-
mon because mesh is used routinely to reinforce the
groin region from inside. The rationale for covering
the defect in the abdominal wall with mesh from in-
side is that the repair can better withstand the pres-
sure to which it is subjected, which originates inside
the abdomen.
25
The difference in recurrence rates in
the two groups can therefore be expected to increase
over time.
Early recurrences in general may be caused by
*TAPP denotes transabdominal preperitoneal lap-
aroscopy.
TABLE 3. REASONS FOR A SWITCH TO ANOTHER
SURGICAL TECHNIQUE DURING
LAPAROSCOPIC REPAIR IN 24 PATIENTS.
REASON TECHNIQUE USED
CONVEN-
TIONAL TAPP*
no. of patients
Loss of pneumopreperitoneum 6 2
Adhesions 3 2
Intubation impossible 2
Inadequate light 2
Arterial bleeding 2
Scrotal hernia 2
Hernial defect too large 1
Too much adipose tissue 1
Pain during spinal anesthesia 1
Figure 1. Mean (SE) Visual-Analogue Scores for Postopera-
tive Pain on the Day of Surgery, during the First 7 Days after
Surgery, and at 14 and 42 Days in Patients with Inguinal Herni-
as Repaired with Open or Laparoscopic Surgery.
A score of 0 denotes no pain, and a score of 100 unbearable
pain. Postoperative pain was less severe in the laparoscopic-
surgery group (P0.001).
0
100
0 1 2 3 4 5 6 7 14 42
80
60
40
20
Postoperative Day
V
i
s
u
a
l
-
A
n
a
l
o
g
u
e
P
a
i
n
S
c
o
r
e
Open surgery
Laparoscopic surgery
The New England Journal of Medicine
Downloaded from nejm.org on April 19, 2013. For personal use only. No other uses without permission.
Copyright 1997 Massachusetts Medical Society. All rights reserved.
1546 May 29, 1997
The New Engl and Journal of Medi ci ne
technical errors.
26
All but three recurrences in the
laparoscopic-surgery group occurred within one year
after surgery, and in most cases, the patients had lat-
eral hernias that had been overlooked. Insufficient
lateral preperitoneal dissection, resulting in furled
mesh, was another common mistake.
18
Ten of the re-
currences were in patients operated on by surgeons
who had limited experience with the laparoscopic
procedure, and a single surgeon was responsible for
9 of the 17 recurrences. These findings clearly illus-
trate the danger of underestimating the skill and ex-
perience required to master this technique.
Physical examination during follow-up is indis-
pensable for obtaining reliable data on rates of re-
currence, because follow-up by telephone or mail is
unreliable.
4,7,8
Virtually all our patients (97 percent)
had follow-up physical examinations performed by
two experienced physicians, who made home visits
to patients unable or unwilling to come to the hos-
pital for follow-up. Although others
4,7,27
have recog-
nized the importance of physical examination after
hernia repair, the percentages of patients examined
during follow-up have usually been lower than in
our study.
The patients returned to work sooner after laparo-
scopic repair than after open repair, as reported in
several smaller trials.
8,15
In our study, the difference
was appreciable (a median of seven days). This differ-
ence may be explained by the absence of an inguinal
incision, the absence of dissection of muscle in the
groin during laparoscopic repair, and the tension-free
repair, as well as by the lower complication rate.
It may be argued that a small group of surgeons
who are interested in a particular procedure will al-
ways perform better than those who do not have this
special interest and that different levels of experience
should be taken into account when comparing our
two groups of surgeons. Our surgeons were selected
broadly, and the initial errors made by several of them
indicate that they were not highly experienced. With-
in the group performing laparoscopic repairs and
within the group performing conventional repairs,
there were different levels of experience and skill.
Finally, the hospitals in our study were selected to
obtain a representative cross-section of patients and
surgeons in the Netherlands. This pragmatic approach
may provide an answer to the question of whether
the Dutch surgical community is capable of achiev-
ing better results overall with a laparoscopic ap-
proach than with the open approach currently used.
The results of our trial will be used by the govern-
ment to decide whether laparoscopic repair of in-
guinal hernias should be included as a reimbursable
procedure in our health care system. Given the su-
perior results of laparoscopic repair in terms of re-
covery and recurrence rates over time, and with the
lessons of the learning curve kept in mind, a gradual
introduction of laparoscopic hernia repair on a large
scale seems warranted, but only if the procedure is
supervised by experienced surgeons.
Supported by a grant (OG/011) from the Dutch Ministry of Health,
Welfare, and Sports.
*P0.001 for all comparisons.
ADL denotes activities of daily living.
TABLE 4. POSTOPERATIVE RECOVERY IN THE TWO
TREATMENT GROUPS.*
VARIABLE
OPEN
SURGERY
LAPAROSCOPIC
SURGERY
median (interquartile range)
Postoperative hospital stay
(days)
2 (12) 1 (12)
Time to resumption of
normal activity (days)
10 (616) 6 (410)
Time to return to work (days) 21 (1233) 14 (721)
Time to resumption of
athletic activities (days)
36 (2444) 24 (1438)
ADL score
At 1 day 39 (2256) 50 (3367)
At 1 week 72 (5683) 83 (7294)
At 2 weeks 83 (7294) 94 (83100)
At 6 weeks 83 (7294) 94 (83100)
Figure 2. KaplanMeier Curves for Recurrence-free Survival in
the Open-Surgery and Laparoscopic-Surgery Groups.
The median follow-up was 607 days (interquartile range, 369 to
731). The P value for the difference in the rates of recurrence
between the two groups was 0.05 by the log-rank test.
84
0
100
0 300 1200
96
92
88
600 900
Days after Surgery
P
a
t
i
e
n
t
s
F
r
e
e
o
f
R
e
c
u
r
r
e
n
c
e
s
(
%
)
NO. OF PATIENTS AT RISK
Laparoscopic surgery
Open surgery
Laparoscopic
surgery
Open
surgery
455
463
252
248
9
14
The New England Journal of Medicine
Downloaded from nejm.org on April 19, 2013. For personal use only. No other uses without permission.
Copyright 1997 Massachusetts Medical Society. All rights reserved.
CONVENTI ONAL ANTERI OR SURGERY VERSUS LAPAROSCOPI C SURGERY FOR I NGUI NAL- HERNI A REPAI R
Vol ume 336 Number 22 1547
We are indebted to the surgeons, residents, and staff at St. Clara
Hospital, Diakonessenhuis, Hofpoort Hospital, Ikazia Hospital,
Reinier de Graaf Gasthuis, and University Hospital Utrecht for
their help with this study; to Ms. C.G.M.M. Beckers, Ms. I.G.M. An-
nink, Ms. A.D.M. Schyns, and Drs. R.C. Zwart, I. Geurts, and
J.J.M. Heyligers of the Conventional Anterior versus Laparoscopic
Hernia Repair (COALA) Trial Office for data management and
secretarial support; to Drs. L.S. de Vries and I.M.C. Janssen for their
collaboration at the beginning of the trial; and to all our patients
for their willingness to participate in the study.
REFERENCES
1. Rider MA, Baker DM, Locker A, Fawcett AN. Return to work after in-
guinal hernia repair. Br J Surg 1993;80:745-6.
2. Salcedo-Wasicek MC, Thirlby RC. Postoperative course after herniorrha-
phy: a case-controlled comparison of patients receiving workers compensa-
tion vs. patients with commercial insurance. Arch Surg 1995;130:29-32.
3. Dutch Center for Health Care Information. Annual computer disk of
the hospitals, the annual of the hospitals. Utrecht, the Netherlands: SIG
Zorginformatie, 1995 (software). (In Dutch.)
4. Schumpelick V, Treutner KH, Arlt G. Inguinal hernia repair in adults.
Lancet 1994;344:375-9.
5. Shulman AG, Amid PK, Lichtenstein IL. Returning to work after her-
niorrhaphy: take it easy is the wrong advice. BMJ 1994;309:216-7.
6. Soper NJ, Brunt LM, Kerbl K. Laparoscopic general surgery. N Engl J
Med 1994;330:409-19.
7. Hay J-M, Boudet M-J, Fingerhut A, et al. Shouldice inguinal hernia re-
pair in the male adult: the gold standard? A multicenter controlled trial in
1578 patients. Ann Surg 1995;222:719-27.
8. Liem MSL, van Vroonhoven TJMV. Laparoscopic inguinal hernia repair.
Br J Surg 1996;83:1197-204.
9. Lichtenstein IL, Shulman AG, Amid PK. The cause, prevention,
and treatment of recurrent groin hernia. Surg Clin North Am 1993;73:
529-44.
10. McKernan JB, Laws HL. Laparoscopic repair of inguinal hernias using
a totally extraperitoneal prosthetic approach. Surg Endosc 1993;7:26-8.
11. Felix EL, Michas CA, Gonzales MH Jr. Laparoscopic hernioplasty:
TAPP vs. TEP. Surg Endosc 1995;9:984-9.
12. Stoker DL, Spiegelhalter DJ, Singh R, Wellwood JM. Laparoscopic
versus open inguinal hernia repair: randomised prospective trial. Lancet
1994;343:1243-5.
13. Payne JH Jr, Grininger LM, Izawa MT, Podoll EF, Lindahl PHJ, Bal-
four J. Laparoscopic or open inguinal herniorrhaphy? A randomized pro-
spective trial. Arch Surg 1994;129:979-81.
14. Vogt DM, Curet MJ, Pitcher DE, Martin DT, Zucker KA. Preliminary
results of a prospective randomized trial of laparoscopic onlay versus con-
ventional inguinal herniorrhaphy. Am J Surg 1995;169:84-90.
15. Lawrence K, McWhinnie D, Goodwin A, et al. Randomised controlled
trial of laparoscopic versus open repair of inguinal hernia: early results. BMJ
1995;311:981-5.
16. Barkun JS, Wexler MJ, Hinchey EJ, Thibeault D, Meakins JL. Laparo-
scopic versus open inguinal herniorrhaphy: preliminary results of a ran-
domized controlled trial. Surgery 1995;118:703-10.
17. Age distribution per municipality, 1 January 1994. Mndstat Bevolk
(CBS) 1994;10:24-32. (In Dutch.)
18. Liem MSL, van Steensel CJ, Boelhouwer RU, et al. The learning curve
for totally extraperitoneal laparoscopic inguinal hernia repair. Am J Surg
1996;171:281-5.
19. Nyhus LM. Individualization of hernia repair: a new era. Surgery
1993;114:1-2.
20. Picavet HSJ, van Sonsbeek JLA, van den Bos GAM. Health interview
surveys, the measurement of functional disabilities in the elderly by surveys.
Mndber Gezond (CBS) 1992;7:5-20. (In Dutch.)
21. Liem MSL, van der Graaf Y, Zwart RC, Geurts I, van Vroonhoven
TJMV. A randomized comparison of physical performance following lap-
aroscopic and open inguinal hernia repair. Br J Surg 1997;84:64-7.
22. Streiner DL, Norman GR. Health measurement scales: a practical
guide to their development and use. Oxford, England: Oxford University
Press, 1989.
23. Activity and recurrent hernia. BMJ 1977;2:3-4.
24. Lichtenstein IL, Shore JM. Exploding the myths of hernia repair. Am
J Surg 1976;132:307-15.
25. Stoppa RE. The treatment of complicated groin and incisional hernias.
World J Surg 1989;13:545-54.
26. Peacock EE Jr, Madden JW. Studies on the biology and treatment of
recurrent inguinal hernia. II. Morphological changes. Ann Surg 1974;179:
567-71.
27. Iles JDH. Specialisation in elective herniorrhaphy. Lancet 1965;1:751-
5.
MASSACHUSETTS MEDICAL SOCIETY REGISTRY ON CONTINUING MEDICAL EDUCATION
To obtain information about continuing medical education courses in New England, call
between 9 a.m. and 12 noon, Monday through Friday, (617) 893-4610, or in Massachusetts,
1-800-322-2303, ext. 1342.
The New England Journal of Medicine
Downloaded from nejm.org on April 19, 2013. For personal use only. No other uses without permission.
Copyright 1997 Massachusetts Medical Society. All rights reserved.
También podría gustarte
- Family Medicine Board Review - Pass Your ABFM Exam - CMEDocumento6 páginasFamily Medicine Board Review - Pass Your ABFM Exam - CMEa jAún no hay calificaciones
- Kelantan Obstetrics Shared Care Guideline Finale1 10 3Documento100 páginasKelantan Obstetrics Shared Care Guideline Finale1 10 3JashveerBedi0% (1)
- RCM: Revenue Cycle Management in HealthcareDocumento15 páginasRCM: Revenue Cycle Management in Healthcaresenthil kumar100% (5)
- Conservative Management of Perforated Peptic UlcerDocumento4 páginasConservative Management of Perforated Peptic UlcerAfiani JannahAún no hay calificaciones
- Hernia IngunalisDocumento7 páginasHernia IngunalisAnggun PermatasariAún no hay calificaciones
- Laparoscopic Appendectomy PostoperativeDocumento6 páginasLaparoscopic Appendectomy PostoperativeDamal An NasherAún no hay calificaciones
- Corto y Largo PlazoDocumento6 páginasCorto y Largo PlazoElard Paredes MacedoAún no hay calificaciones
- Reoperation For Dysphagia After Cardiomyotomy For Achalasia: Clinical Surgery-InternationalDocumento5 páginasReoperation For Dysphagia After Cardiomyotomy For Achalasia: Clinical Surgery-Internationalgabriel martinezAún no hay calificaciones
- Vrijland Et Al-2002-British Journal of SurgeryDocumento5 páginasVrijland Et Al-2002-British Journal of SurgeryTivHa Cii Mpuzz MandjaAún no hay calificaciones
- Laparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Documento5 páginasLaparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Juan Carlos SantamariaAún no hay calificaciones
- Perbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterDocumento7 páginasPerbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterAfiani JannahAún no hay calificaciones
- Nah Incarcerated HerniaDocumento4 páginasNah Incarcerated Herniafelix_the_meowAún no hay calificaciones
- Utd 04524 Clinical - Article KunduzDocumento5 páginasUtd 04524 Clinical - Article Kunduzzenatihanen123Aún no hay calificaciones
- Isj-5899 oDocumento5 páginasIsj-5899 oAbhiram MundleAún no hay calificaciones
- Stapled Rectal Mucosectomy vs. Close HemorrhoidectomyDocumento9 páginasStapled Rectal Mucosectomy vs. Close HemorrhoidectomyNadllely Garcia ZapataAún no hay calificaciones
- 268 2011 Article 1088 PDFDocumento6 páginas268 2011 Article 1088 PDFIoel Tovar TrovaAún no hay calificaciones
- Clinical Study: Delorme's Procedure For Complete Rectal Prolapse: A Study of Recurrence Patterns in The Long TermDocumento6 páginasClinical Study: Delorme's Procedure For Complete Rectal Prolapse: A Study of Recurrence Patterns in The Long TermAnonymous A1ycUQ9zVIAún no hay calificaciones
- Apendisitis MRM 3Documento8 páginasApendisitis MRM 3siti solikhaAún no hay calificaciones
- VolvulusDocumento10 páginasVolvuluswatsonmexAún no hay calificaciones
- Laparoscopic Surgery For DiverticulitisDocumento4 páginasLaparoscopic Surgery For DiverticulitisSigit SetiaWanAún no hay calificaciones
- Conventional Versus Laparoscopic Surgery For Acute AppendicitisDocumento4 páginasConventional Versus Laparoscopic Surgery For Acute AppendicitisAna Luiza MatosAún no hay calificaciones
- Incisional Hernia Mesh RepairDocumento5 páginasIncisional Hernia Mesh Repaireka henny suryaniAún no hay calificaciones
- Short- and Long-Term Outcomes of Laparoscopic vs Open Colorectal Cancer SurgeryDocumento7 páginasShort- and Long-Term Outcomes of Laparoscopic vs Open Colorectal Cancer SurgeryRegina SeptianiAún no hay calificaciones
- @medicinejournal European Journal of Pediatric Surgery January 2020Documento126 páginas@medicinejournal European Journal of Pediatric Surgery January 2020Ricardo Uzcategui ArreguiAún no hay calificaciones
- qt5kh1c39r NosplashDocumento12 páginasqt5kh1c39r NosplashSusieAún no hay calificaciones
- Brown 2014Documento8 páginasBrown 2014nelly alconzAún no hay calificaciones
- The Learning Curve For Hernia PDFDocumento5 páginasThe Learning Curve For Hernia PDFIgor CemortanAún no hay calificaciones
- Bun V34N3p223Documento6 páginasBun V34N3p223pingusAún no hay calificaciones
- Palliative Management of Malignant Rectosigmoidal Obstruction. Colostomy vs. Endoscopic Stenting. A Randomized Prospective TrialDocumento4 páginasPalliative Management of Malignant Rectosigmoidal Obstruction. Colostomy vs. Endoscopic Stenting. A Randomized Prospective TrialMadokaDeigoAún no hay calificaciones
- Reoperative Antireflux Surgery For Failed Fundoplication: An Analysis of Outcomes in 275 PatientsDocumento8 páginasReoperative Antireflux Surgery For Failed Fundoplication: An Analysis of Outcomes in 275 PatientsDiego Andres VasquezAún no hay calificaciones
- The Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014Documento7 páginasThe Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014alemago90Aún no hay calificaciones
- A Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerDocumento9 páginasA Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerFarizka Dwinda HAún no hay calificaciones
- Laparoscopic Versus Open Transhiatal Esophagectomy For Distal and Junction CancerDocumento6 páginasLaparoscopic Versus Open Transhiatal Esophagectomy For Distal and Junction CancerDea Melinda SabilaAún no hay calificaciones
- Esposito 2006Documento4 páginasEsposito 2006Fernando GarciaAún no hay calificaciones
- 1 Bjs 10662Documento8 páginas1 Bjs 10662Vu Duy KienAún no hay calificaciones
- Mid-Term Pneumatic Dilatation for AchalasiaDocumento3 páginasMid-Term Pneumatic Dilatation for AchalasiaLuis PerazaAún no hay calificaciones
- Recurrent Ureteropelvic Junction Obstruction Following Primary Treatment: Prevalence, Associated Factors, and Laparoscopic TreatmentDocumento9 páginasRecurrent Ureteropelvic Junction Obstruction Following Primary Treatment: Prevalence, Associated Factors, and Laparoscopic TreatmentPatricio G.Aún no hay calificaciones
- Monitoring Complications of MeDocumento8 páginasMonitoring Complications of Meaxl___Aún no hay calificaciones
- Umesh Singh. TLTK-47Documento5 páginasUmesh Singh. TLTK-47HẢI HOÀNG THANHAún no hay calificaciones
- Bariatric SurgeryDocumento4 páginasBariatric SurgeryCla AlsterAún no hay calificaciones
- DTSCH Arztebl Int-115 0031Documento12 páginasDTSCH Arztebl Int-115 0031Monika Diaz KristyanindaAún no hay calificaciones
- Management of Perforated Appendicitis in Children: A Decade of Aggressive TreatmentDocumento5 páginasManagement of Perforated Appendicitis in Children: A Decade of Aggressive Treatmentapi-308365861Aún no hay calificaciones
- Jo (2003)Documento5 páginasJo (2003)Елена КарпинскаяAún no hay calificaciones
- emil2006Documento5 páginasemil2006mia widiastutiAún no hay calificaciones
- Complicated AppendicitisDocumento4 páginasComplicated AppendicitisMedardo ApoloAún no hay calificaciones
- Protocol oDocumento8 páginasProtocol oCynthia ChávezAún no hay calificaciones
- Laparoscopic Vagotomy for Chronic Peptic Ulcer DiseaseDocumento4 páginasLaparoscopic Vagotomy for Chronic Peptic Ulcer Diseasepeter_mrAún no hay calificaciones
- Hernia Jur Nal 2000Documento12 páginasHernia Jur Nal 2000Hevi Eka TarsumAún no hay calificaciones
- Frazee 2016Documento10 páginasFrazee 2016Herpian NugrahadilAún no hay calificaciones
- Laparoscopic Appendectomy PDFDocumento4 páginasLaparoscopic Appendectomy PDFdydydyAún no hay calificaciones
- Inguinal HerniaDocumento9 páginasInguinal HerniaAmanda RapaAún no hay calificaciones
- Laparoscopic Versus Open Surgery For Gastric Gastrointestinal Stromal Tumors: A Propensity Score Matching AnalysisDocumento10 páginasLaparoscopic Versus Open Surgery For Gastric Gastrointestinal Stromal Tumors: A Propensity Score Matching AnalysisFerdian PriantoAún no hay calificaciones
- Surgical Outcome of Genito Urinary Fistula - RayazDocumento3 páginasSurgical Outcome of Genito Urinary Fistula - RayazRiaz Ahmed ChaudhryAún no hay calificaciones
- Closure Vs Nonclosure of PeritoneumDocumento6 páginasClosure Vs Nonclosure of PeritoneumFrancisco Xavier Beltrán Vallejo100% (1)
- Bar Dram 2000Documento6 páginasBar Dram 2000Prasetyö AgungAún no hay calificaciones
- General Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueDocumento3 páginasGeneral Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueRahul SinghAún no hay calificaciones
- Enhanced Recovery Protocol After Ileostomy ReversalDocumento4 páginasEnhanced Recovery Protocol After Ileostomy Reversalshah hassaanAún no hay calificaciones
- PICO InvaginasiDocumento4 páginasPICO InvaginasimutimutimutiAún no hay calificaciones
- A Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisDocumento5 páginasA Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisBenjamin PaulinAún no hay calificaciones
- Impact of Postoperative Morbidity On Long-Term Survival After OesophagectomyDocumento10 páginasImpact of Postoperative Morbidity On Long-Term Survival After OesophagectomyPutri PadmosuwarnoAún no hay calificaciones
- Damage Control in Trauma Care: An Evolving Comprehensive Team ApproachDe EverandDamage Control in Trauma Care: An Evolving Comprehensive Team ApproachJuan DuchesneAún no hay calificaciones
- Case Studies of Postoperative Complications after Digestive SurgeryDe EverandCase Studies of Postoperative Complications after Digestive SurgeryAún no hay calificaciones
- The SAGES Manual of Biliary SurgeryDe EverandThe SAGES Manual of Biliary SurgeryHoracio J. AsbunAún no hay calificaciones
- Kawasaki CPD Online 2014Documento47 páginasKawasaki CPD Online 2014'Muhamad Rofiq Anwar'Aún no hay calificaciones
- GigiDocumento10 páginasGigiIsmail Eko SaputraAún no hay calificaciones
- GNAPS Online Simpo Rev 2Documento19 páginasGNAPS Online Simpo Rev 2chlorooAún no hay calificaciones
- Hubungan Kepribadian Tipe D Dengan Kejadian HipertensiDocumento4 páginasHubungan Kepribadian Tipe D Dengan Kejadian HipertensiS'Herlina Ali SopiahAún no hay calificaciones
- Cutaneous Tuberculosis in Children PDFDocumento10 páginasCutaneous Tuberculosis in Children PDFMeryam SetiawanAún no hay calificaciones
- Chronic Migrainous VertigoDocumento5 páginasChronic Migrainous VertigoDyah Wulan RamadhaniAún no hay calificaciones
- Hemoroid LigationDocumento6 páginasHemoroid Ligation'Muhamad Rofiq Anwar'Aún no hay calificaciones
- STROKE HEMORAGIKDocumento20 páginasSTROKE HEMORAGIKFebrita PutriAún no hay calificaciones
- JurnalDocumento6 páginasJurnal'Muhamad Rofiq Anwar'Aún no hay calificaciones
- Overview Dermatitis AtopiDocumento9 páginasOverview Dermatitis Atopi'Muhamad Rofiq Anwar'Aún no hay calificaciones
- Cutaneous Tuberculosis in Children PDFDocumento10 páginasCutaneous Tuberculosis in Children PDFMeryam SetiawanAún no hay calificaciones
- 2013 Sa64 PDFDocumento13 páginas2013 Sa64 PDF'Muhamad Rofiq Anwar'Aún no hay calificaciones
- Overview Dermatitis AtopiDocumento9 páginasOverview Dermatitis Atopi'Muhamad Rofiq Anwar'Aún no hay calificaciones
- Hand Expressing Breast PubmedDocumento15 páginasHand Expressing Breast PubmedAsri HartatiAún no hay calificaciones
- The Pharmacist's Guide To Evidence-Based MedicineDocumento2 páginasThe Pharmacist's Guide To Evidence-Based MedicineDhanang Prawira NugrahaAún no hay calificaciones
- Clinical Dental Hygiene II 2021-2022 Course CatalogDocumento2 páginasClinical Dental Hygiene II 2021-2022 Course Catalogapi-599847268Aún no hay calificaciones
- Nutritional Content and Health Benefits of EggplantDocumento6 páginasNutritional Content and Health Benefits of Eggplantdhanashri pawarAún no hay calificaciones
- The Amazing Science of AuriculotherapyDocumento26 páginasThe Amazing Science of AuriculotherapyNatura888100% (13)
- Crma Unit 1 Crma RolesDocumento34 páginasCrma Unit 1 Crma Rolesumop3plsdn0% (1)
- Clinical Practice Guidelines On The Management of ChildrenDocumento17 páginasClinical Practice Guidelines On The Management of ChildrenRajithaHirangaAún no hay calificaciones
- Intensive-Care Unit: TypesDocumento2 páginasIntensive-Care Unit: TypesRavi KantAún no hay calificaciones
- Handbook On ICMR Ethical GuidelinesDocumento28 páginasHandbook On ICMR Ethical Guidelinessamkarmakar2002Aún no hay calificaciones
- Orthopedics P - Iv June15 PDFDocumento2 páginasOrthopedics P - Iv June15 PDFPankaj VatsaAún no hay calificaciones
- Name Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailDocumento8 páginasName Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailshrutiAún no hay calificaciones
- The Impact of Depression Among Students in Iplc Senior High School-1Documento3 páginasThe Impact of Depression Among Students in Iplc Senior High School-1Roxanne TongcuaAún no hay calificaciones
- Exercise in PregnancyDocumento7 páginasExercise in PregnancynirchennAún no hay calificaciones
- AFOMP Newsletter January 2022 Vol14 No.1 UpdatedDocumento48 páginasAFOMP Newsletter January 2022 Vol14 No.1 UpdatedparvezAún no hay calificaciones
- DR Avijit Bansal-My Experiences at UCMSDocumento6 páginasDR Avijit Bansal-My Experiences at UCMScholesterol200Aún no hay calificaciones
- Myocardial Infarction Case StudyDocumento9 páginasMyocardial Infarction Case StudyMeine Mheine0% (1)
- Danielle Nesbit: Work ExperienceDocumento4 páginasDanielle Nesbit: Work ExperienceNav SethAún no hay calificaciones
- Nutritional Needs of A Newborn: Mary Winrose B. Tia, RNDocumento32 páginasNutritional Needs of A Newborn: Mary Winrose B. Tia, RNcoosa liquorsAún no hay calificaciones
- Ap2 Safe ManipulationDocumento5 páginasAp2 Safe ManipulationDarthVader975Aún no hay calificaciones
- Donning A Sterile Gown and GlovesDocumento3 páginasDonning A Sterile Gown and GlovesVanny Vien JuanilloAún no hay calificaciones
- Barriers To NP Practice That Impact Healthcare RedesignDocumento15 páginasBarriers To NP Practice That Impact Healthcare RedesignMartini ListrikAún no hay calificaciones
- Motivation Letter - EmboDocumento1 páginaMotivation Letter - EmboFebby NurdiyaAún no hay calificaciones
- Altitude SicknessDocumento2 páginasAltitude Sicknessapi-367386863Aún no hay calificaciones
- Clinical Pharmacology Answers 2022Documento223 páginasClinical Pharmacology Answers 2022nancy voraAún no hay calificaciones
- StiDocumento12 páginasStiValentinaAún no hay calificaciones
- Cholelithiasis N C P BY BHERU LALDocumento1 páginaCholelithiasis N C P BY BHERU LALBheru LalAún no hay calificaciones
- 7-Postoperative Care and ComplicationsDocumento25 páginas7-Postoperative Care and ComplicationsAiden JosephatAún no hay calificaciones