Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Goljan Live Notes Day 1
Cargado por
Daniyal Azmat0 calificaciones0% encontró este documento útil (0 votos)
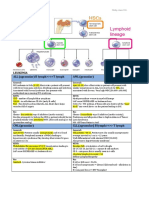
84 vistas5 páginas1. The document discusses oxygen transport and cellular respiration. Hemoglobin transports oxygen in red blood cells from the lungs to tissues, where oxygen is used in mitochondria to generate ATP through oxidative phosphorylation.
2. Several conditions that can impair oxygen transport and delivery are discussed, including hypoxia, carbon monoxide poisoning, methemoglobinemia, and anemia. Respiratory acidosis can also decrease oxygen levels in the blood.
3. When oxygen delivery is inadequate, anaerobic glycolysis is triggered to generate some ATP without oxygen, leading to a buildup of lactic acid and metabolic acidosis if the condition persists. This can cause cellular damage through various mechanisms.
Descripción original:
lecture notes!
Derechos de autor
© © All Rights Reserved
Formatos disponibles
DOCX, PDF, TXT o lea en línea desde Scribd
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documento1. The document discusses oxygen transport and cellular respiration. Hemoglobin transports oxygen in red blood cells from the lungs to tissues, where oxygen is used in mitochondria to generate ATP through oxidative phosphorylation.
2. Several conditions that can impair oxygen transport and delivery are discussed, including hypoxia, carbon monoxide poisoning, methemoglobinemia, and anemia. Respiratory acidosis can also decrease oxygen levels in the blood.
3. When oxygen delivery is inadequate, anaerobic glycolysis is triggered to generate some ATP without oxygen, leading to a buildup of lactic acid and metabolic acidosis if the condition persists. This can cause cellular damage through various mechanisms.
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como DOCX, PDF, TXT o lea en línea desde Scribd
0 calificaciones0% encontró este documento útil (0 votos)
84 vistas5 páginasGoljan Live Notes Day 1
Cargado por
Daniyal Azmat1. The document discusses oxygen transport and cellular respiration. Hemoglobin transports oxygen in red blood cells from the lungs to tissues, where oxygen is used in mitochondria to generate ATP through oxidative phosphorylation.
2. Several conditions that can impair oxygen transport and delivery are discussed, including hypoxia, carbon monoxide poisoning, methemoglobinemia, and anemia. Respiratory acidosis can also decrease oxygen levels in the blood.
3. When oxygen delivery is inadequate, anaerobic glycolysis is triggered to generate some ATP without oxygen, leading to a buildup of lactic acid and metabolic acidosis if the condition persists. This can cause cellular damage through various mechanisms.
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como DOCX, PDF, TXT o lea en línea desde Scribd
Está en la página 1de 5
Goljan Live Notes Day 1
Hypoxia inadequate oxygenation of tissue
Oxygen for oxygenation phosphorylation in mitochondria pathway ETC, last
reaction is oxygen is an electron acceptor. Protons are being kicked off the electron
transport system, going back to the membrane to form ATP.
ATP is mainly generated in the mitochondria
What carries oxygen? Hemoglobin is the most important times the oxygen
saturation plus partial pressure of arterial oxygen
Hemoglobin O2 to heme group saturation of O2 and partial pressure of arterial
oxygen
O2 content hemoglobin times O2 saturation plus Arterial Oxygen
Partial Pressure of oxygen Amount of oxygen dissolved in plasma
Iron has to be plus 2 to carry oxygen
If all 4 heme groups are occupied with red blood cells and oxygen the saturation is
100 percent
The oxygen flows in the following direction
1. Alveoli diffuses through the red blood cell membrane and attaches to the
heme group on red blood cell on the hemoglobin
2. If the partial pressure of oxygen decrease, o2 saturation is decreased as well
When you retain CO2 respiratory acidosis, P02 goes down
CO2 high = PO2 low
Acidosis = CO2 = PO2 down hypoxemia
Ventillation defect = RDS Hyaline membrane Disease
No ventilation, but there is perfusion
Recognize on exam patient on hypoxemia and given 100% oxygen but PO2
didnt increase because there is a shunt.
Intrapulmonary Shunting
Perfussion defects pulmonary embolis prolong flights.
Stasis from immobilization
Increases the dead space
Given 100% oxygen PO2 goes up!
Diffusion Defect Fibrosis halts oxygen transportation
Pulmonary Edema fluid restricts oxygen movement
Cardiac Failure fluid restricts the transportation of oxygen to vital regions
Fluid in interstitial of the lung causes irritation to the J receptors causing
dyspnea
Anemia Oxygen Content?
Decreased Hemoglobin, Normal Respiration P02 normal O2 saturation
is normal
Tissue hypoxia = exertional dyspnea exercise intolerance
Carbon Monoxide a heater in a wintertime, room heaters have combustible
material and inhaling can cause CO2 poisoning. House fire is another big cause of
CO2 poisoning. Another house fire related is cyanide poisoning from the insulation.
People in housefires have both cyanide and CO2 poisoning.
Co2 very high affinity for hemoglobin and highly diffusible, O2 saturation goes down
because CO2 is very high affinity to hemoglobin. It dissociates O2 from the heme
region because CO2 is taking up space on the HEME group. O2 saturation is down.
Treatment is 100% oxygen which increases O2 saturation.
Decrease of oxygen saturation = cyanosis. Why dont we see that in CO2 because
cherry red appearance masks it. The most common symptom is headache.
Methhemaglobin its iron in plus 3 state, oxygen cannot bind to it. Oxygen
saturation is decreased, chocolate colored blood because no O2 on heme groups.
The P02 is normal, the hemoglobin is normal.
RBC methemoglobin reductase system convert Fe iron in plus 3 state back to
plus 2 state.
Nitrites and Nitrates in drinking water are oxidizing agents, which oxidizes
hemoglobin and iron to plus 3 state, which causes methemoglobinemia, treatment is
IV blue.
Dapsone sulfur and nitro drugs produce methemoglobin and potential to
increase G6PD and hemolytic Anemia, oxidizing agents causing increase in peroxide
which destroys RBC.
Methemoglobenemia with HIV Treatment Pneumocystis carinii potential side
affects is methemoglobenemia
Right shift curve Hemoglobin with decrease affinity to oxygen, what moves
the curves to the right
2-3 BPG
o Fever
o Low Ph
o High altitude right shift curve, resp alkalosis, hyperventilate
o Decrease CO2 respiratory alkalosis = right shift because of high
altitude causes increase of 2-3 BPG
Left Shift
CO2
Methemoglobin
Decrease 2-3BPG
Alkalosis
Cytochrome Oxidase last enzyme before it transfers the electron to the oxygen
electron acceptor
Cyanide and CO2 inhibit Cyctochrome Oxidase
Uncoupling ability for the mitochondria to synthesize ATP Inner mitochondrial
membrane is permeable to protons, ATP synthase carrier is where proton is
suppose to travel to form ATP.
Dinitrophenol chemical to preserve wood
Alcohol protons to go right through the membrane and very little ATP generation
Uncoupling agents protons leaking out of the membrane pores without going
through the ATP synthase so there is no generation of ATP and therefore the
decrease of ATP causes severe energy depletion in the human body, all the reactions
start increase to make more NADPH and more electron transport chain to produce
more protons, the body can go into hyperthermia as compensation.
If youre an alcoholic on a hot day increases chances of heat stroke, because
alcoholics are so susceptible to heat stroke because they are already having
uncoupling agents destroy the mitochondria and therefore are very susceptible to
heat stroke.
Respiratory Acidosis hemoglobin is normal, oxygen saturation and PO2 decreased
Partial pressure of oxygen in arterial decreased
Anemia Oxygen saturation and PO2 is normal only hemoglobin conc is decreased
CO2 and Methemoglobenemia O2 saturation affected decreased, Hemoglobin is
normal and P02 is normal. Treatment 100% 02 for C02 and IV blue for
Methemoglbenemia and ascorbic acid.
Decrease in ATP tissue hypoxia Anaerobic Glycolysis triggered, end product is
Lactic Acid.
Pyruvate is converted to Lactic Acid due to increase in NADH.
Need to make NAD for feedback in the glycolytic cycle to make 2 more ATP
Mitochondria makes all ATP, one place where you can get 2 atp without going to
mitochondria is anaerobic glycolysis without oxygen.
Mitochondrial system shutdown anaerobic glycolysis forms only 2 ATP causes
buildup of Lactic Acid and increase anion gab metabolic acidosis, within a cell it
causes denature protein due to increase in acid. Denaturing is altering its
configuration and in terms of enzymes its denatured as well. The cell cant autodigest
itself because of buildup of enzymes and is caused coagulation necrosis.
Coagulation Necrosis Gross
Infarction through buildup of acid in the cell which denatures the structure and
enzymes of the cell. The ATPase pump is broken and Na/K pump is ineffective in
anaerobic glyclosis, Na comes into the cell and causes cellular swilling because
water comes into the cell with sodium
This is a reversible injury. Cellular swelling because of tissue hypoxia causes sodium
potassium pump causes sodium and water to into the cell and causes reversible
injury. Adding oxygen will remove sodium and bring cell back to natural healthy
state.
In mature red blood cells dont have mitochondria, so normally have anaerobic
glycolysis is always going on.
a cell without o2 is going to cause irreversible injury
Biggest agents is calcium, activates phospholipases in cell membrane and
causes damage to cell membrane
Activates enzyme in nucleus causes pyknosis and nuclear chromosome
disappears
Goes into mitochondria destroys the mitochondria
Hypercalcemia produces acute pancreatitis, activate pancreas enzyme.
Cell membrane damage is hallmark of irreversible damage, mitochondria the
energy producing factory destroyed is also irreversible.
Free radical injury Brownish Pigment in older people organ called atrophy
lipufushcin.
When you have free radical damage end product is lipufuschin, unbreakable
lipid.
what is a free radical?
A compound that has an unpaired electron
También podría gustarte
- Study Product 1Documento117 páginasStudy Product 1javibruinAún no hay calificaciones
- Nephrotic Syndrome WikipediaDocumento10 páginasNephrotic Syndrome WikipediaJohn KevlarAún no hay calificaciones
- Essential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsDocumento5 páginasEssential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsRika Ariyanti SaputriAún no hay calificaciones
- NSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saDocumento19 páginasNSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saAhmed HossamAún no hay calificaciones
- SYPHYLISDocumento1 páginaSYPHYLISkhadzxAún no hay calificaciones
- Patho CA - Acute PancreatitisDocumento1 páginaPatho CA - Acute PancreatitisKAún no hay calificaciones
- Abdominal Wall, Omentum, Mesentery, RetroperitoneumDocumento6 páginasAbdominal Wall, Omentum, Mesentery, RetroperitoneumMon Ordona De GuzmanAún no hay calificaciones
- Chronic Inflammatory Dermatoses Inflammatory Blistering DisordersDocumento4 páginasChronic Inflammatory Dermatoses Inflammatory Blistering DisordersspringdingAún no hay calificaciones
- Bacterial Infections of The SkinDocumento9 páginasBacterial Infections of The Skinbeia21Aún no hay calificaciones
- Pelvis and Perineum Clinical CorrelationDocumento4 páginasPelvis and Perineum Clinical CorrelationKeesha Mariel AlimonAún no hay calificaciones
- DermDocumento10 páginasDermyassrmarwaAún no hay calificaciones
- Renal SyndromeDocumento13 páginasRenal SyndromeAndreas KristianAún no hay calificaciones
- Commensal AmoebaDocumento2 páginasCommensal AmoebaCoy NuñezAún no hay calificaciones
- Histology Viscus Flow ChartDocumento1 páginaHistology Viscus Flow ChartNaser Hamdi ZalloumAún no hay calificaciones
- VQ - O2 GradientDocumento27 páginasVQ - O2 GradientIkbal NurAún no hay calificaciones
- 5 Cyto AbnormalDocumento9 páginas5 Cyto AbnormalMerli Ann Joyce CalditoAún no hay calificaciones
- MCB 252 Final Exam Study GuideDocumento62 páginasMCB 252 Final Exam Study GuideJay ZAún no hay calificaciones
- Kidney Physiology (Q & A)Documento28 páginasKidney Physiology (Q & A)ramadan100% (1)
- Histo Review 2Documento13 páginasHisto Review 2Coy NuñezAún no hay calificaciones
- The Immune System OhtDocumento6 páginasThe Immune System OhtKa-Shun Leung100% (1)
- PancreasDocumento35 páginasPancreasPaskalisAún no hay calificaciones
- NephroticDocumento8 páginasNephroticsangheetaAún no hay calificaciones
- Arterial Blood Gas Workshop Dr. Lanzona 12.06.07: Lala 3C-Med-09 1Documento4 páginasArterial Blood Gas Workshop Dr. Lanzona 12.06.07: Lala 3C-Med-09 1pramastutiAún no hay calificaciones
- Abdominal OrgansDocumento28 páginasAbdominal OrgansRS BuenavistaAún no hay calificaciones
- Handouts Integumentary Sys Sp11 B201Documento7 páginasHandouts Integumentary Sys Sp11 B201Kelly TrainorAún no hay calificaciones
- Abdominal Pain: No. Features Explanation Associated WithDocumento4 páginasAbdominal Pain: No. Features Explanation Associated WithNazmun LailahAún no hay calificaciones
- 1 11857 AnatomyDocumento5 páginas1 11857 Anatomykalyan2k5Aún no hay calificaciones
- Cytogenetics Note PDFDocumento14 páginasCytogenetics Note PDFMerjema Bahtanović100% (1)
- Kidney NewDocumento4 páginasKidney NewParth BhayanaAún no hay calificaciones
- Toxicology USMLE NotesDocumento15 páginasToxicology USMLE NotesDuncan JacksonAún no hay calificaciones
- Structural Biology of HIVDocumento31 páginasStructural Biology of HIVLaura TapiaAún no hay calificaciones
- Cardio Block 3Documento62 páginasCardio Block 3Maya LaPradeAún no hay calificaciones
- Disease PDFDocumento6 páginasDisease PDFJohn Christopher LucesAún no hay calificaciones
- Midterm Chapter7Documento43 páginasMidterm Chapter7Frances FranciscoAún no hay calificaciones
- Review For The 2° Semester Exam Alessandro Mo6a, UVVG, 3 YearDocumento9 páginasReview For The 2° Semester Exam Alessandro Mo6a, UVVG, 3 Yeardjxela89Aún no hay calificaciones
- Chapter 3 Genetic VariationDocumento21 páginasChapter 3 Genetic VariationAbdulkarimAún no hay calificaciones
- Actinic Keratosis: (Aka Bowen's Disease)Documento5 páginasActinic Keratosis: (Aka Bowen's Disease)fadoAún no hay calificaciones
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDocumento4 páginas4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaAún no hay calificaciones
- Renal Physiology IDocumento16 páginasRenal Physiology IJubilee Christiene AngAún no hay calificaciones
- Purine Metabolism de Novo Synthesis and Salvage Pathway, 2015Documento28 páginasPurine Metabolism de Novo Synthesis and Salvage Pathway, 2015Tehreem NadeemAún no hay calificaciones
- Complement SystemDocumento4 páginasComplement SystemFait HeeAún no hay calificaciones
- Casts inDocumento1 páginaCasts ingregoryvoAún no hay calificaciones
- Genitourinary System: Renal FailureDocumento6 páginasGenitourinary System: Renal FailureEn ConejosAún no hay calificaciones
- Clin Path Trans 3.05 Urinalysis (2b)Documento6 páginasClin Path Trans 3.05 Urinalysis (2b)Reymart FernandezAún no hay calificaciones
- NEUROHISTORYDocumento2 páginasNEUROHISTORYTom MallinsonAún no hay calificaciones
- Inguinal CanalDocumento4 páginasInguinal CanalspiraldaoAún no hay calificaciones
- Im-Ugib PudDocumento6 páginasIm-Ugib PudTrisAún no hay calificaciones
- Abnormal LFTsDocumento2 páginasAbnormal LFTsRenu RosyAún no hay calificaciones
- Acute Tubular NecrosisDocumento60 páginasAcute Tubular NecrosisYedesney C. LinaresAún no hay calificaciones
- Boards - Gen AnaDocumento26 páginasBoards - Gen AnaJoyce EbolAún no hay calificaciones
- LeukemiaDocumento2 páginasLeukemiaAyeshaArifAún no hay calificaciones
- General Features of The Immune SystemDocumento6 páginasGeneral Features of The Immune SystemMinerva Bautista RoseteAún no hay calificaciones
- The Complement SystemDocumento4 páginasThe Complement SystemExamville.com100% (1)
- Iron Metabolism: DR Mukhtiar BaigDocumento58 páginasIron Metabolism: DR Mukhtiar BaigdrmukhtiarbaigAún no hay calificaciones
- Infection of Skin Muscles, Bone FinalDocumento90 páginasInfection of Skin Muscles, Bone FinalNoelani-Mei Ascio100% (1)
- Gene Related DiseaseDocumento3 páginasGene Related Diseasevivek govardhanamAún no hay calificaciones
- Haemopoiesis: Composition of Whole Blood & Its ComponentsDocumento8 páginasHaemopoiesis: Composition of Whole Blood & Its ComponentsSafiya JamesAún no hay calificaciones
- Goljan Audio TranscriptDocumento234 páginasGoljan Audio TranscriptHuan Bien100% (4)
- Golijan, S Audio Lec NotesDocumento186 páginasGolijan, S Audio Lec NotesUsman100% (5)
- Goljan Audios Transcribed (Margaret)Documento216 páginasGoljan Audios Transcribed (Margaret)sean8phamAún no hay calificaciones
- Trauma HandbookDocumento321 páginasTrauma HandbookDaniyal AzmatAún no hay calificaciones
- 196-Apollo59-C - Person SpecificationDocumento10 páginas196-Apollo59-C - Person SpecificationDaniyal AzmatAún no hay calificaciones
- Plab PlanDocumento5 páginasPlab PlanDaniyal AzmatAún no hay calificaciones
- Trust Benefits Sept19Documento1 páginaTrust Benefits Sept19Daniyal AzmatAún no hay calificaciones
- Nformation ACK: Specialty Doctor in Anaesthetics and Intensive Care Post Reference 415-MP499-21Documento17 páginasNformation ACK: Specialty Doctor in Anaesthetics and Intensive Care Post Reference 415-MP499-21Daniyal AzmatAún no hay calificaciones
- 259-MED824447RLHNS - Job Description and Person Specification - Generic Non Specialist ACCU Clin Fellow JD 2016Documento8 páginas259-MED824447RLHNS - Job Description and Person Specification - Generic Non Specialist ACCU Clin Fellow JD 2016Daniyal AzmatAún no hay calificaciones
- 290 TDPB 394 B Job DescriptionDocumento11 páginas290 TDPB 394 B Job DescriptionDaniyal AzmatAún no hay calificaciones
- Pediatrics Modern Day AnalysisDocumento144 páginasPediatrics Modern Day AnalysisDaniyal AzmatAún no hay calificaciones
- Trust Doctor in Joint Reconstruction and Sarcoma Job Description Trust ProfileDocumento9 páginasTrust Doctor in Joint Reconstruction and Sarcoma Job Description Trust ProfileDaniyal AzmatAún no hay calificaciones
- 040-CF466-A - 040-CF466 - Job DescriptionDocumento7 páginas040-CF466-A - 040-CF466 - Job DescriptionDaniyal AzmatAún no hay calificaciones
- 213-UPACS-5584-A - Job Description & Person SpecificationDocumento4 páginas213-UPACS-5584-A - Job Description & Person SpecificationDaniyal AzmatAún no hay calificaciones
- 236-SCO-MD-010-2021 - FY1 LAS JD Person SpecDocumento9 páginas236-SCO-MD-010-2021 - FY1 LAS JD Person SpecDaniyal AzmatAún no hay calificaciones
- 358-2686264-ED-C - Job Description and Person Specification - PHEM 2020Documento14 páginas358-2686264-ED-C - Job Description and Person Specification - PHEM 2020Daniyal AzmatAún no hay calificaciones
- Enhanced Road Assessment FAQsDocumento3 páginasEnhanced Road Assessment FAQsDaniyal AzmatAún no hay calificaciones
- Drugs Affecting Respiratory SystemDocumento45 páginasDrugs Affecting Respiratory SystemDaniyal AzmatAún no hay calificaciones
- Medical Genetics-Q Bank-Set 2: - Select The Best AnswerDocumento34 páginasMedical Genetics-Q Bank-Set 2: - Select The Best AnswerDaniyal AzmatAún no hay calificaciones
- How To Pass The Usmle: by Dr. Adrienne HicksDocumento13 páginasHow To Pass The Usmle: by Dr. Adrienne HicksDaniyal AzmatAún no hay calificaciones
- 1 - Ethical IssuesDocumento33 páginas1 - Ethical IssuesDaniyal Azmat100% (1)
- Lower Limb Exam QuestionsDocumento57 páginasLower Limb Exam QuestionsDaniyal Azmat91% (68)
- Safety Protocol To Avoid Dehydration Overexertion 1Documento18 páginasSafety Protocol To Avoid Dehydration Overexertion 1thennek nalliv78% (87)
- Kelompok 8 Psi Abnormal ADocumento83 páginasKelompok 8 Psi Abnormal Acandle einAún no hay calificaciones
- ThrombophlebitisDocumento10 páginasThrombophlebitismardsz100% (3)
- 02 Mar 2021 PDFDocumento8 páginas02 Mar 2021 PDFVaibhav RamAún no hay calificaciones
- Soalan Topikal Kertas 1 Tingkatan 4Documento320 páginasSoalan Topikal Kertas 1 Tingkatan 4Nurul Abdul Halim100% (1)
- GCSE Biology - Homeostasis - WorksheetDocumento2 páginasGCSE Biology - Homeostasis - WorksheetalexAún no hay calificaciones
- Brosure Prosim3Documento6 páginasBrosure Prosim3priyanka choudhryAún no hay calificaciones
- Acidosis & AlkalosisDocumento29 páginasAcidosis & Alkalosiszaeem1993Aún no hay calificaciones
- SAS - Session 3 - PSY079 - Intro To Psychology-Pages-1,5-8Documento5 páginasSAS - Session 3 - PSY079 - Intro To Psychology-Pages-1,5-8Dayne BitonAún no hay calificaciones
- Final Review Worksheet 11thDocumento28 páginasFinal Review Worksheet 11thElec AzAún no hay calificaciones
- Brain Bee Sample QuestionsDocumento4 páginasBrain Bee Sample QuestionsThasaRatha100% (3)
- Lee, Thonylet E. Mabinta, Dianne Melad, Maria FeDocumento25 páginasLee, Thonylet E. Mabinta, Dianne Melad, Maria FeShivaveerakumar S. Chandrikimath100% (1)
- ACS ATLS 1993 Test #1 9: 5/16/17, 4G38 PM Page 1 of 11Documento11 páginasACS ATLS 1993 Test #1 9: 5/16/17, 4G38 PM Page 1 of 11Joshua Runtuwene100% (2)
- Als Pass 5Documento1 páginaAls Pass 5Hazel Brondial67% (3)
- Health Teaching PPT For HypertensionDocumento13 páginasHealth Teaching PPT For HypertensionJeym Quinny ClapanoAún no hay calificaciones
- CH161 Lecture 9-10 - GIKIDocumento42 páginasCH161 Lecture 9-10 - GIKIHabny ShaaAún no hay calificaciones
- Electrolytes and Related AbnormalitiesDocumento10 páginasElectrolytes and Related AbnormalitiesKyla CastilloAún no hay calificaciones
- Solution Manual For High Acuity Nursing 7th Edition WagnerDocumento35 páginasSolution Manual For High Acuity Nursing 7th Edition Wagnerheadman.infuser.tfoth100% (54)
- Intrinsic Frequencies of Carotid Pressure Waveforms Predict Heart Failure EventsDocumento9 páginasIntrinsic Frequencies of Carotid Pressure Waveforms Predict Heart Failure EventsSaionara FranciscoAún no hay calificaciones
- ANATOMY Study Lower Respiratory TractDocumento3 páginasANATOMY Study Lower Respiratory TractLP BenozaAún no hay calificaciones
- AnaPhyLc - 1.3 Necessary Life Functions and Survival NeedsDocumento19 páginasAnaPhyLc - 1.3 Necessary Life Functions and Survival NeedsKyarra MedenillaAún no hay calificaciones
- Life ProcessesDocumento2 páginasLife ProcessesSuganthiVasanAún no hay calificaciones
- Clinical ECG RoundsDocumento2 páginasClinical ECG RoundsKai Siang ChanAún no hay calificaciones
- Body Temperature: Physiology DepartmentDocumento17 páginasBody Temperature: Physiology DepartmentMaab AlrsheedAún no hay calificaciones
- Test Bank For Anatomy and Physiology 10th Edition Kevin T PattonDocumento24 páginasTest Bank For Anatomy and Physiology 10th Edition Kevin T PattonAaronBrownpnmb100% (47)
- Action Potential NotesDocumento2 páginasAction Potential NotesJohn OsborneAún no hay calificaciones
- Morphine: Oleh: Chau Febriani Kharisma 1971002014 Pembimbing: DR. Dr. Gede Budiarta Sp. An, KMNDocumento51 páginasMorphine: Oleh: Chau Febriani Kharisma 1971002014 Pembimbing: DR. Dr. Gede Budiarta Sp. An, KMNCecilia MonaAún no hay calificaciones
- Oxygen Therapy: Housemanship Training Programme Department of Anaesthesiology and Intensive CareDocumento55 páginasOxygen Therapy: Housemanship Training Programme Department of Anaesthesiology and Intensive CaretorreslysAún no hay calificaciones
- Management of Diabetes and Hyperglycemia in Hospitals: S C S S. B, M F. M, A A, E P. S, R G. S, I B. H, D H W CDocumento39 páginasManagement of Diabetes and Hyperglycemia in Hospitals: S C S S. B, M F. M, A A, E P. S, R G. S, I B. H, D H W CMarshell TendeanAún no hay calificaciones
- Nervous System WorksheetDocumento12 páginasNervous System WorksheetLeamae ObinaAún no hay calificaciones