Documentos de Académico
Documentos de Profesional
Documentos de Cultura
79
Cargado por
Nejc KvacDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
79
Cargado por
Nejc KvacCopyright:
Formatos disponibles
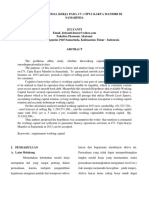
172 Respiratory Physiology
CLINICAL CORRELATE
Respiratory Distress Syndrome of the Newborn
Immediately after delivery, a newborn takes its rst breath. Nega-
tive pressure of 40 to 100 cm H
2
O is required to draw air into the
collapsed airways and inate the alveoli. During this rst breath,
in a healthy, normal, term infant, surfactant stored in type II
alveolar epithelial cells is released and forms a mononuclear layer
at the air-uid interface of the small airways and alveoli. By the
third breath, only a small negative pressure is required to inate
the lung. Respiratory distress syndrome (previously known as
hyaline membrane disease) is the most common cause of death in
premature infants, and is caused by a lack of surfactant produc-
tion. Without surfactant, the negative pressure required to inate
the lungs remains high (CL is low) and portions of the lung col-
lapse, leading to respiratory distress and potentially respiratory
failure and death. Treatment consists of ventilatory support and
surfactant therapy through the breathing tube.
Negative pressure of 40 to 100
cm H
2
O needed to inflate sac
(alveolus) with air.
Monomolecular layer of surfactant
lining fluid layer on surface of
terminal sac (alveolus)
The initial inflation of the collapsed lungs of a neonate requires large negative pressure (40 to 100 cm H
2
0), but surface tension is reduced in
subsequent breaths as surfactant lines the alveoli and small airways, reducing the work required to inflate the lungs. Premature birth is often
associated with surfactant deficiency and respiratory distress.
Drop of water with surface tension
of 72 dynes/cm forms a globule
Drop of water mixed with household
detergent; surface tension reduced to 20
dynes/cm and thus water spreads out
Glass sheets
Radius 25 Radius 100 Radius 25
Surfactant
absent
Surfactant
present
Fluid-filled
airway
Terminal sac
(alveolus) Air Fluid
Air Fluid Collapsed terminal sac
(alveolus)
Negative pressure of 40 to 100 cm H
2
O
needed to inflate sac (alveolus) with air.
Inflated terminal
sac (alveolus)
During 1st breath After 3rd breath
Radius 25 Radius 100 Radius 50
Fluid-filled airway
Surfactant stored in type II
cells of terminal sac (alveolus)
Air Fluid
Air Fluid
Surfactant
Inflated terminal
sac (alveolus)
Before 1st breath
Minimum surface tension is 50 dynes/cm.
As much as 20 cm H
2
O of negative pressure
needed to inflate sac (alveolus) during fourth
and subsequent breaths.
Surface tension is 5 dynes/cm or less. Negative
pressure of only 2 cm H
2
O needed to inflate
sac (alveolus) to maximum diameter during
fourth and subsequent breaths.
Diabetes mellitus
(maternal)
Prematurity
Birth wt. 2.5 kg; RDS not likely
Birth wt. 2.5 kg; likelihood of
RDS increases in relation to
lower wt. (if viable)
A. Risk factors for development of respiratory distress syndrome (RDS) of newborn
B. Surfactant effects during lung inflation in the neonate
Cesarean birth
Perinatal asphyxia
(2nd born of twins
more susceptible)
During normal, quiet breathing, pleural pressure is always
negative. However, during active expiration, contraction of
expiratory muscles results in elevation of pleural pressure
above atmospheric pressure (see Fig. 14.7). Under these cir-
cumstances, during expiration, alveolar pressure is the sum of
the positive pleural pressure and the elastic recoil pressure
of the lungs. Pressure in the airways falls between the alveoli
and the opening of the mouth, reaching atmospheric pressure
at the mouth. Thus, at some point downstream from the
alveoli, an equal pressure point is reached, at which airway
También podría gustarte
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Mouth Tongue and Salivary GlandsDocumento52 páginasMouth Tongue and Salivary GlandsIrfan FalahAún no hay calificaciones
- Practice 3Documento7 páginasPractice 3NinhAún no hay calificaciones
- Kebutuhan Modal Kerja Pada Cv. Cipta Karya Mandiri Di SamarindaDocumento7 páginasKebutuhan Modal Kerja Pada Cv. Cipta Karya Mandiri Di SamarindaHerdi VhantAún no hay calificaciones
- Chapter One A CellDocumento46 páginasChapter One A CellLeon MarkoAún no hay calificaciones
- RSC SCST Programme Briefing For Factories enDocumento4 páginasRSC SCST Programme Briefing For Factories enmanikAún no hay calificaciones
- (Promotion Policy of APDCL) by Debasish Choudhury: RecommendationDocumento1 página(Promotion Policy of APDCL) by Debasish Choudhury: RecommendationDebasish ChoudhuryAún no hay calificaciones
- Vdocuments - MX - Sri Thiruppugal Vidhana Shodasa Upachara Puja PDFDocumento73 páginasVdocuments - MX - Sri Thiruppugal Vidhana Shodasa Upachara Puja PDFDomnick WilkinsAún no hay calificaciones
- Brochure For New HiresDocumento11 páginasBrochure For New HiresroseAún no hay calificaciones
- We Don't Need No MBADocumento9 páginasWe Don't Need No MBAsharad_khandelwal_2Aún no hay calificaciones
- SOAL ASSEMEN PAKET A BAHASA INGGRIS NewDocumento3 páginasSOAL ASSEMEN PAKET A BAHASA INGGRIS Newmtsn4 clpAún no hay calificaciones
- TDS 39987 Easycoat Profile Decor 3MM Euk GBDocumento3 páginasTDS 39987 Easycoat Profile Decor 3MM Euk GBp4pubgwalyAún no hay calificaciones
- Family Advent Devotions 1Documento3 páginasFamily Advent Devotions 1collingdalenazAún no hay calificaciones
- Making Electric Vehicles ProfitableDocumento18 páginasMaking Electric Vehicles ProfitablevjslkumarAún no hay calificaciones
- ADVOCATE ACT - Smart Notes PDFDocumento30 páginasADVOCATE ACT - Smart Notes PDFAnonymous n7rLIWi7100% (2)
- Softwash ComparatorDocumento5 páginasSoftwash ComparatorFaheem MushtaqAún no hay calificaciones
- Solved MCQS For Mid Terms Papers Solved by JUNAID MALIK and TeamDocumento23 páginasSolved MCQS For Mid Terms Papers Solved by JUNAID MALIK and TeamUrwa RiazAún no hay calificaciones
- A Study of Absenteeism of Workers in Nutrine Confectionery Company LTD ChittoorDocumento69 páginasA Study of Absenteeism of Workers in Nutrine Confectionery Company LTD ChittoorShoaib MohammedAún no hay calificaciones
- ICT Authority Legal NoticeDocumento13 páginasICT Authority Legal NoticeICT AUTHORITYAún no hay calificaciones
- SQL Interview QuestionsDocumento89 páginasSQL Interview QuestionsVaneet Arora100% (2)
- Homeless Class ActionDocumento36 páginasHomeless Class ActionMichael_Lee_RobertsAún no hay calificaciones
- Aci - The Financial Markets Association: Examination FormulaeDocumento8 páginasAci - The Financial Markets Association: Examination FormulaeJovan SsenkandwaAún no hay calificaciones
- Fish Immune System and Vaccines-Springer (2022) - 1Documento293 páginasFish Immune System and Vaccines-Springer (2022) - 1Rodolfo Velazco100% (1)
- Ps 202PET Manual enDocumento7 páginasPs 202PET Manual enStiv KisAún no hay calificaciones
- Case Study1: Partnering For Success: Working Together: How Biotech Firms and Large Drug Companies Bring Pharmaceutical Products To MarketDocumento2 páginasCase Study1: Partnering For Success: Working Together: How Biotech Firms and Large Drug Companies Bring Pharmaceutical Products To MarketLakhan SinghAún no hay calificaciones
- Automatic Water Level Indicator and Controller by Using ARDUINODocumento10 páginasAutomatic Water Level Indicator and Controller by Using ARDUINOSounds of PeaceAún no hay calificaciones
- Definition of CultureDocumento14 páginasDefinition of CultureRenee Louise CoAún no hay calificaciones
- Different Varieties of English C1 WSDocumento5 páginasDifferent Varieties of English C1 WSLaurie WAún no hay calificaciones
- The Til Pat YearsDocumento1 páginaThe Til Pat Yearsrajkumarvpost6508Aún no hay calificaciones
- How To Install Linux, Apache, MySQL, PHP (LAMP) Stack On Ubuntu 16.04Documento12 páginasHow To Install Linux, Apache, MySQL, PHP (LAMP) Stack On Ubuntu 16.04Rajesh kAún no hay calificaciones
- International Banking & Foreign Exchange ManagementDocumento4 páginasInternational Banking & Foreign Exchange ManagementAnupriya HiranwalAún no hay calificaciones