Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Neurocisticercosis 2005
Cargado por
adzlDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Neurocisticercosis 2005
Cargado por
adzlCopyright:
Formatos disponibles
Review
Introduction
Neurocysticercosis is an old disease. Known in ancient
Greece as a disease of swine and since the 17th century
as a human ailment, neurocysticercosis was not
considered a public health problem until the second half
of the 20th century, when British investigators
recognised the disease among soldiers returning from
India. Since then, hundreds of studies have described
the epidemiological characteristics and the clinical
manifestations of neurocysticercosis.
1,2
During the past
three decades, the introduction of modern diagnostic
tools and potent cysticidal drugs has allowed accurate
diagnosis and improved the prognosis for many
patients.
1,3
Despite these advances in diagnosis and therapy,
neurocysticercosis remains endemic in most low-
income countries, where it represents one of the most
common causes of acquired epilepsy.
1
WHO has
calculated that over 50 000 deaths are due to
neurocysticercosis each year, and many times this
number of people have active epilepsy, with all the social
and economic consequences that this implies.
4
Neurocysticercosis is being diagnosed with increasing
frequency in high-income countries because of
increased migration of people with the disease
5
or
tapeworm carriers,
5,6
and because of tourism and travel
to endemic areas. It is also one of a few conditions
included in a list of potentially eradicable infectious
diseases of public-health importance,
7
and control or
eradication programmes are urgently needed to reduce
its effect.
Life cycle of Taenia solium
Although the pig is the usual intermediate host of the
tapeworm Taenia solium, human cysticercosis occurs
when the eggs, which are excreted in the faeces of an
individual carrying the parasite, are ingested. A common
misconception is that one can acquire neurocysticercosis
by eating pork. However, ingestion of infected pork only
causes adult tapeworm infestation (taeniasis), because
infected pork contains the larval cysts that develop into
adult worms in human intestine, and does not contain
the eggs that cause cysticercosis. Transmission was
previously thought to be by indirect means, such as by
the ingestion of vegetables irrigated with water
contaminated with human faeces and thus T solium
eggs. However, recent epidemiological evidence
suggests that the most common source of infective eggs
is a symptom-free tapeworm carrier in the household.
8,9
Therefore, cysticercosis should be seen as a disease
mostly transmitted from person to person, whereas the
role of infected pigs is to perpetuate the infection. In the
usual cycle of transmission of T solium, pigs have access
to contaminated human stools by their coexistence with
human beings in the domestic setting and the lack of
household sewage or sanitary facilities. Pig-to-pig
transmission has been recently described,
10
but its effect
on transmission pressure is not yet known.
Figure 1 shows the larval cysts in the meat of an
infected pig. The cyst consists of a scolex, or head, of the
future tapeworm surrounded by a vesicle formed by the
extension of the parasites tegument (vesicular wall).
11
T solium is a 24 m atworm that lives in the human
upper small intestine, most often without noticeable
symptoms. It excretes eggs and proglottids irregularly,
which if ingested cause cysticercosis. After ingestion,
eggs hatch and liberate the embryos or oncospheres into
the intestine. Oncospheres actively cross the intestinal
Lancet Neurol 2005; 4: 65361
Cysticercosis Unit, Institute of
Neurological Sciences, Lima,
and Department of
Microbiology, Universidad
Peruana Cayetano Heredia,
Lima, Peru (H H Garcia MD);
Department of Clinical
Neurosciences, Hospital-Clinica
Kennedy, Guayaquil, Ecuador
(O H Del Brutto MD)
Correspondence to:
Dr Hector H Garcia, Cysticercosis
Unit, Instituto de Ciencias
Neurolgicas, Jr Ancash 1271,
Barrios Altos, Lima 1, Peru
hgarcia@jhsph.edu
http://neurology.thelancet.com Vol 4 October 2005 653
Neurocysticercosis: updated concepts about an old disease
Hector H Garcia, Oscar H Del Brutto, for The Cysticercosis Working Group in Peru
Neurocysticercosis, the infection of the human brain by the larvae of Taenia solium, is a major cause of acquired
epilepsy in most low-income countries. Cases of neurocysticercosis are becoming more common in high-income
countries because of increased migration and travel. Diagnosis by neuroimaging and serological assessment has
greatly improved over the past decade, and the natural progression of the disease and response to antiparasitic drugs
is now much better understood. Neurocysticercosis is potentially eradicable, and control interventions are underway
to eliminate this infection. Meanwhile, updated information on diagnosis and management of neurocysticercosis is
required, especially for clinicians who are unfamiliar with its wide array of clinical presentations.
Figure 1: Infected pork showing multiple viable cysticerci
Review
wall, enter the bloodstream, and are carried into the
tissues of the host where they develop into larval cysts.
These cysts are rapidly destroyed by the hosts immune
system in most circumstances, except for those located
in immunologically privileged sites such as the eye and
the nervous system.
12
Natural history
There is little information on the natural history of
human cysticercosis or neurocysticercosis. Data from
pigs show that cysts reach their maximum size in
23 months,
13
and that while alive they trigger little
perilesional inammation.
14
However, most pigs are
slaughtered at about 9 months of age and thus this
model only reects the early stages of the infection.
15
In
human beings, the initial perspective of neuro-
cysticercosis (based on the few cases diagnosed by
radiography, and a series of cases attending surgery or
with the disease detected only at necropsy) was that of a
lethal, aggressive disease, mostly causing intractable
epilepsy and progressive intracranial hypertension.
16
Two natural epidemiological scenarios helped to
understand the dynamics of infection and disease, at
least in part. Early in the 20th century, British troops
were sent on duty to India for dened periods of time.
Many (up to 450) of them or their direct relatives had
seizures and were studied by a special unit of the British
Army, which was able to nd evidence of neuro-
cysticercosis in up to 75% of those with seizures.
16,17
More importantly, the onset of neurological symptoms
was recorded according to the date of return to the UK (a
cysticercosis-free country), and most individuals had
their initial seizure 25 years after their return,
suggesting a long latent stage. In a second, unrelated
episode in 1968, the King of Bali sent pigs as a pre-
electoral gift to the peasants of Papua New Guinea, an
island that was free of cysticercosis. 2 years later, a
sudden epidemic of burns was caused by people falling
into their bonres because of seizures that occurred
while sleeping close to the re. Necropsy studies of some
of these people conrmed neurocysticercosis as the
cause of the seizure disorder.
18
These bouts of
neurocysticercosis, in cases for which the date of
infection could be traced, were evidence against
symptoms appearing at the time of initial exposure.
The introduction of CT and MRI unveiled a whole
spectrum of mild infections in symptom-free individuals
or in patients with sporadic seizures, which changed the
denition of neurocysticercosis from a fatal or severe
disease, to a less aggressive one. For example, in India,
most individuals with neurocysticercosis present with a
single degenerating cysticercus, whereas in Latin
America and China a substantial proportion of infected
individuals present with a few viable brain cysts.
19
Recently, several studies with CT in endemic villages of
Latin America have found that 1020% of symptom-free
villagers have one or more intraparenchymal brain
calcications.
2024
We have hypothesised that in most mild
exposures the parasite dies in its early stages by action of
the hosts immune system, whereas a small subgroup of
infections (probably those with heavier egg challenges)
become established and survive as viable cysts.
9
654 http://neurology.thelancet.com Vol 4 October 2005
Figure 2: Diverse presentations of neurocysticercosis
Multiple viable cysts (vesicular stage; A); single enhancing lesion (degenerating cysts; B); multiple intraparenchymal calcications (C); intraventricular cyst (D); basal
subarachnoid cysticercosis (extraparenchymal neurocysticercosis; E); cysticercotic encephalitis (extraparenchymal neurocysticercosis; F); ocular cysticercosis (G); and
muscle cysticercosis (H).
Review
General features of neurocysticercosis
Clinical description
Although neurocysticercosis can cause almost any
neurological symptom, late-onset epilepsy and
intracranial hypertension are its most common clinical
manifestations.
25,26
Symptomatic neurocysticercosis
results from a combination of factors, including the
number, stage, and localisation of the parasites within
the nervous system, as well as the severity of the hosts
immune response against the parasites (gure 2).
Seizures occur in up to 70% of patients.
26
Patients may
also present with intracranial hypertension that can be
associated with seizures, dementia, or focal signs.
Hydrocephalus, related to arachnoiditis, granular
ependymitis, or ventricular cysts, is the most common
cause of this syndrome.
27
Intracranial hypertension also
occurs in patients with giant cysts and in those with the
rare form of cysticercotic encephalitis (resulting from
infection with many cysticerci inducing a severe
immune response from the host).
28
Various focal
neurological ndings may also occur in patients with
neurocysticercosis. Whereas focal signs usually follow a
subacute or chronic course, some patients present with
acute focal signs due to the occurrence of a
cerebrovascular event.
29
Patients are likely to have
transient and eeting focal neurological decits that may
either be postictal or are elicited by acute inammatory
responses to parasites.
Diagnosis
Diagnosis of neurocysticercosis is typically made on the
basis of neuroimaging studies and conrmatory
serological analysis. The most common neuroimaging
examination done in endemic areas is CT. The latest
generation of CT machines have fairly good diagnostic
sensitivity, although some small lesions, especially
those in the posterior fossa, close to the bone, or those
inside the ventricles or basal cisterns, may be missed.
30
MRI has better accuracy, although it may miss some
small calcications, and has the important pitfall of
being much more expensive and less available in areas
where the disease is endemic. Several serological assays
to detect specic antibodies have been used for decades
with different and somewhat conicting results.
31,32
Currently, most centres use an enzyme-linked
immunoelectrotransfer blot (EITB) with puried
glycoprotein antigens (western blot),
33
which can be
done in serum samples or in CSF or use ELISAs in CSF
samples. An advantage of EITB is that its sensitivity in
serum samples is equal to or better than that in CSF
samples.
34
Although EITB has 100% specicity and an
overall sensitivity of 98%, a major problem is that
approximately 30% of patients with a single brain
parasite may test negative.
35
An interesting new
development is the introduction of antigen-detection
ELISA, although no concrete data on sensitivity and
specicity are yet available.
36
A set of diagnostic criteria has recently been proposed
to help clinicians and health workers with the diagnosis
of neurocysticercosis.
37
Proper interpretation of these
criteria permit two degrees of diagnostic certainty,
denitive or probable (panel).
Treatment
Treatment should be tailored according to the type of
neurocysticercosis (table).
38
Physicians in charge of
patients with neurocysticercosis should always
remember that therapy includes a combination of
symptomatic and antiparasitic measures, including
analgesics, antiepileptic drugs (AEDs), cysticidal drugs,
surgical resection of lesions, and placement of
ventricular shunts.
The main point of controversy has been over the use of
cysticidal drugs, used since 1979.
3941
Praziquantel is most
often used at doses of 50 mg/kg/day for 15 days, but the
drug has been given in regimens of 10100 mg/kg for
321 days,
42
or even as a single-day regimen (based on
exposing cysticerci to very high concentrations of
http://neurology.thelancet.com Vol 4 October 2005 655
Panel: Proposed diagnostic criteria for neurocysticercosis
Absolute
1 Histological demonstration of the parasite from biopsy of a brain or spinal-cord lesion
2 Cystic lesions showing the scolex on CT or MRI
3 Direct visualisation of subretinal parasites by funduscopic examination
Major
1 Lesions highly suggestive of neurocysticercosis on neuroimaging studies (ie, CT or MRI
showing cystic lesions without scolex, enhancing lesions, or typical parenchymal brain
calcications)
2 Positive serum EITB (with puried extracts of T soliumantigens) for the detection of
anticysticercal antibodies (assay developed by the Centers for Disease Control and
Prevention, Atlanta, GA, USA)
3 Resolution of intracranial cystic lesions after therapy with albendazole or praziquantel
4 Spontaneous resolution of small single enhancing lesions (ie, solitary ring-enhancing
lesions measuring less than 20 mm in diameter in patients presenting with seizures, a
normal neurological examination, and no evidence of an active systemic disease)
Minor
1 Lesions compatible with neurocysticercosis on neuroimaging studies (ie, CT or MRI
showing hydrocephalus or abnormal enhancement of the leptomeninges, and
myelograms showing multiple lling defects in the column of contrast medium)
2 Clinical manifestations suggestive of neurocysticercosis (ie, seizures, focal neurological
signs, intracranial hypertension, and dementia)
3 Positive CSF ELISA for detection of anticysticercal antibodies or cysticercal antigens
4 Cysticercosis outside the CNS (ie, histologically conrmed subcutaneous or muscular
cysticercosis, plain radiographic lms showing cigar-shaped soft-tissue calcications,
or direct visualisation of cysticerci in the anterior chamber of the eye)
Epidemiological
1 Evidence of a household contact with T soliuminfection
2 Individuals coming from or living in an area where cysticercosis is endemic
3 History of frequent travel to disease-endemic areas
Reproduced with permission from Lippincott Williams and Wilkins.
37
Review
praziquantel, by giving three doses of 2530 mg/kg at 2 h
intervals).
43
As a drawback, serum concentrations of
praziquantel decrease when steroids are also used.
44
Albendazole was initially given at doses of 15 mg/kg/day
for 1 month.
40
Further studies showed that at similar
doses, the length of therapy could be shortened to 1 week
without lessening the effectiveness of the drug.
45,46
In
general, albendazole has higher parasiticidal effect than
does praziquantel.
40
Cysticidal drug therapy has been
harshly criticised by some clinicians because treatment-
associated parasite death leads to an acute, severe
inammatory reaction in the surrounding brain tissue,
increasing intracranial hypertension and potentially
leading to the death of the patient.
47
Another major
argument against the use of cysticidal drugs has been that
there was no evidence that killing the parasites would lead
to fewer seizures during follow-up.
48
However, as noted
below, current evidence favours their use in patients with
viable intraparenchymal or extraparenchymal parasites.
49,50
The administration of a single rst-line AED results
in seizure control in most patients with
neurocysticercosis-related epilepsy.
26
However, the
optimum duration of antiepileptic drug therapy in these
patients has not been settled. Up to 50% of those
patients who remain seizure free for 2 years while on
AEDs will have relapses after AED withdrawal,
suggesting that intracranial cysticerci are permanent
substrates for seizures and may be reactivated when the
inhibitory inuences of AEDs are absent.
51
Prognostic
factors associated with seizure recurrence include the
development of parenchymal brain calcications, and
the presence of recurrent seizures and multiple brain
cysts before the institution of therapy.
52
Although some
clinicians have proposed that AEDs could be
discontinued after 3 months of resolution of a single
brain-enhancing lesion,
53
controlled data supporting
this afrmation are still required.
5355
Corticosteroids are the main form of therapy for
cysticercotic encephalitis, angiitis, and chronic meningitis
that causes progressive entrapment of cranial nerves
56
(particularly for extraparenchymal neurocysticercosis).
Simultaneous administration of corticosteroids
ameliorates the secondary effects of headache and
vomiting that may occur during cysticidal drug therapy.
Such manifestations are not associated with the toxic
effects of the drugs but to the destruction of parasites
within the brain, and are reliable indicators of drug
efcacy. In patients with giant subarachnoid cysticerci,
ventricular cysts, spinal cysts, and multiple parenchymal
brain cysts, corticosteroids must be given before, during,
and even some days after the course of cysticidal drugs to
avoid the risk of cerebral infarcts, acute hydrocephalus,
spinal-cord swelling, or massive brain oedema.
56
The most common surgical indication in
neurocysticercosis is ventricular shunting to resolve
hydrocephalus.
57
Hydrocephalus secondary to neurocys-
ticercosis is associated with high rates of shunt
dysfunction; indeed, it is common for these patients to
have protracted courses of disease and high mortality,
correlated with the number of surgical interventions to
revise the shunt.
58
Twice weekly prednisone treatment
reduces the risk of shunt dysfunction.
59
Other surgical
indications include the excision of giant cysts or
intraventricular cysts.
Location of neurocysticercosis
One of the main problems in analysing the abundant
literature on neurocysticercosis is the generalisation of
concepts while ignoring the differences between the
disease types. Mixing different types of neuro-
cysticercosis leads to confusing assessments of accuracy
of diagnostic tests, therapeutic approaches, and
prognosis. To avoid the risks of unwarranted
generalisation, we have categorised the main clinical
presentations of neurocysticercosis, and describe their
associated clinical manifestations and specics of
diagnosis, therapy, and prognosis. A major factor is
whether parasites are in the brain parenchyma or in
extraparenchymal structures.
Intraparenchymal cysts
Pathophysiology
Once established, the larval cysts actively evade the
hosts immune response through several mechanisms,
including inhibition of complement, cytokine release,
and masking with host immunoglobulins.
60,61
Thus, only
656 http://neurology.thelancet.com Vol 4 October 2005
Treatment
Parenchymal neurocysticercosis
Vesicular cysts
Single Albendazole 15 mg/kg/day for 1 week, steroids used only if side-effects
occur; or praziquantel 100 mg/kg in three equal doses
Moderate infections Albendazole 15 mg/kg/day for 1 week, with simultaneous use of steroids.
Heavy infections (100 or more cysts) Albendazole 15 mg/kg/day for 1 week with high doses of steroids
Degenerating (colloidal) cysts
Single lesions Albendazole 15 mg/kg/day for 1 week, steroids used only if side-effects
occur; or no antiparasitic treatment
Moderate infections Albendazole 15 mg/kg/day for 1 week with steroids
Heavy infections (encephalitis) No antiparasitic treatment, high doses of steroids, osmotic diuretics
(mannitol)
Calcications
Single or multiple No antiparasitic treatment
Extraparenchymal neurocysticercosis
Subarachnoid neurocysticercosis
Giant cyst (usually in Sylvian ssure) Albendazole 15 mg/kg/day for 1 month, with high doses of steroids;
or surgical excision
Basal subarachnoid (racemose) Albendazole 15 mg/kg/day for 1 month, with high doses of steroids.
Ventricular cysts Endoscopic aspiration or surgical resection, use of antiparasitic drugs is
controversial
Hydrocephalus No antiparasitic treatment, ventricular shunt
Arachnoiditis, angiitis No antiparasitic treatment, high doses of steroids for 1 month
Ependymitis No antiparasitic treatment, ventricular shunt if indicated, high doses of
steroids
Other forms of neurocysticercosis
Spinal cysts Surgical resection, albendazole may be used
Ocular cysts Surgical resection
Table: Treatment guidelines for the diverse forms of neurocysticercosis
Review
scarce inammatory changes are seen in the
surrounding tissues. In this vesicular stage, parasites
look healthy and have a clear vesicular uid (gure 2).
Viable cysticerci may remain alive for years, and a
substantial proportion of even those lesions with signs
of inammation do not die for several months. At some
point, the hosts immune system and the inammatory
response overcome the immune evasion mechanisms,
resulting in the death of the parasite.
60,61
The rst stage of involution of cysticerci is the colloidal
stage, in which the vesicular uid becomes turbid, and
the scolex shows early signs of degeneration. Colloidal
cysticerci are surrounded by a thick collagen capsule and
the surrounding brain parenchyma shows astrocytic
gliosis and diffuse oedema.
62
Thereafter, the wall of the
cyst thickens and the scolex is transformed into coarse
mineralised granules; this is called the granular stage. A
single brain cyst in the colloidal or granular stage
compose the so-called single enhancing lesions,
common in Indian patients.
63,64
Finally, in the calcied
stage parasite remnants appear as a mineralised nodule.
When parasites enter the granular and calcied stages,
the oedema subsides, but astrocytic changes in the
vicinity of the lesions become more intense than in the
preceding stages.
11,65
Imaging
On CT, viable cysts appear as hypodense, rounded, cystic
lesions. Some may enhance after administration of
contrast. The scolex can be occasionally seen as a
hyperintense dot in the interior of the cyst. On MRI, the
cysts are hypointense in T1 and FLAIR sequences, but
hyperintense in T2 sequences. MRI is better than CT to
show small cysts or those close to the skull or in the
posterior fossae. Degenerating cysts appear as contrast-
enhancing rings or nodules surrounded by areas of
brain oedema (gure 2). The scolex is not usually seen
using CT or MRI, creating some diagnostic confusion
with other infections or even with intracranial
neoplasms. FLAIR or diffusion-weighted MRI may allow
the visualisation of the scolex in some degenerating
cysts, facilitating the correct diagnosis in these cases
(gure 3). One of the most important (and difcult)
differential diagnoses of a single degenerating
cysticercus is a tuberculoma. Rajshekhar and Chandy
66
have suggested that lesions measuring 20 mm or less
without a shift of the midline structures due to the
surrounding oedema are most probably due to
cysticercosis. Magnetic resonance spectroscopy seems to
detect a peak of lipids in tuberculomas
67
not present in
degenerating cysticerci. Calcied cysts appear as
punctate hyperdense dots on CT, or as areas of
subtracted signal on MRI. Because of this, old MRI
methods had poor sensitivity to detect calcied
neurocysticercosis. At the time of a symptomatic relapse,
a third to a half of patients with calcied lesions only
may show oedema around at least one calcied lesion.
68,69
Because most cases of neurocysticercosis are already
calcied or will eventually resolve and become calcied,
this mechanism may be the main reason for morbidity
in neurocysticercosis.
Treatment
A single course of albendazole or praziquantel kills
6085% of viable brain cysts.
40,45,46,50
A recent
randomised, blinded, controlled trial with albendazole
showed the clinical benet of decreased numbers of
seizures and enhanced resolution of cysts after
treatment, providing evidence for the use of cysticidal
drugs in patients with viable intracranial cysts.
50
Several
randomised trials in Indian patients with single
enhancing lesions
7074
showed a non-signicant but
consistent trend towards fast radiological resolution of
lesions and decreased likelihood of seizure relapse
(gure 4). Fast radiological resolution after cysticidal
treatment may be helpful in the management of
patients with single enhancing lesions, thus avoiding
diagnostic pitfalls.
75
However, in most patients with
single enhancing lesions, the lesions disappear
spontaneously.
76
Patients with cysticercotic encephalitis
should not receive cysticidal drugs because they may
exacerbate the intracranial hypertension observed in
this form of the disease.
38
Finally, patients with
calcications alone should not receive cysticidal drugs
because these lesions represent dead parasites (table).
Extraparenchymal neurocysticercosis
Extraparenchymal disease varies in its symptoms or
prognosis according to whether the parasites are located
in the convexity of the cerebral hemispheres, in the basal
subarachnoid space, in the sylvian ssure, or in the
ventricles. Intracranial hypertension is a common
manifestation of extraparenchymal neurocysticercosis
and may be due to mass effect, distortion of the normal
anatomy of CSF pathways, direct obstruction of the
ventricular system by a cyst, or inammatory reaction in
http://neurology.thelancet.com Vol 4 October 2005 657
Figure 3: New MRI techniques that may improve diagnostic accuracy for cysticercosis
FLAIR (left) and MRI with inversion recovery (right).
Review
the meninges leading to arachnoiditis.
27,77
Cysts in the
convexity of the cerebral hemispheres behave as
intraparenchymal cysts. The other locations are
discussed separately below.
Basal subarachnoid neurocysticercosis or cysticercosis of the
sylvian ssure
When cysts are located outside the brain parenchyma
they tend to grow irregularly and trigger a more severe
inammatory response. Giant cysts typically develop in
areas where more space is available, like the sylvian
ssure or the CSF cisterns at the base of the brain, and
mostly behave as benign tumours due to their persisting
growth.
49
By far the worst prognosis is associated with
basal subarachnoid neurocysticercosis, in which vesicles
in CSF cisterns grow in a very disorganised way,
inltrate neighbouring structures, and are associated
with a severe local inammatory response with high
protein concentrations and cell counts in the CSF.
78
Other less common manifestations include basal
meningitis, ventriculitis, angiitis, or hydrocephalus with
no discernible cysts (commonly associated with
inammatory CSF and strong seropositivity). These
conditions seem to correspond to residual pathology
from old, resolved infections, although the reason for
the chronic inammatory CSF response is unclear.
MRI is more accurate than CT for the diagnosis of
most cases of extraparenchymal neurocysticercosis.
30
Coronal and sagittal sections allow better assessment of
areas infected by the parasites. Lesions may rst appear
as multilobed cysts occupying the full space of the CSF
cistern. With further growth, the anatomy of that cistern
is disturbed and adjacent parenchymal structures get
compressed (gure 2). Cerebral infarctions may also be
imaged by either CT or MRI in patients with
cysticercotic arachnoiditis when an artery at the base of
the brain is occluded as the result of the inammatory
reaction surrounding the parasites.
79
Subarachnoid or sylvian neurocysticercosis will progress
if not treated with cysticidal drugs. However, physicians
should be aware that the management of intracranial
hypertension, when present, is the priority. In patients
with both hydrocephalus and intracranial cysts, cysticidal
drugs should be used only after a ventricular shunt has
been placed to avoid further increases of the intracranial
pressure as a result of drug therapy. Cysticidal drugs must
be used with caution in patients with giant subarachnoid
cysts because the inammatory reaction developed by the
host in response to the destruction of parasites may
occlude leptomeningeal vessels surrounding the cyst.
80
In
such cases, treatment with steroids is mandatory to avoid
the hazard of a cerebral infarct.
Ventricular cysticercosis
The manifestation of intraventricular cysts depends on
the involved ventricle, and is more severe if the fourth
ventricle is occupied.
81
Contrast-enhanced MRI is the
examination of choice to rule out the existence of live
cysts in the ventricles or basal cisterns. Hydrocephalus
can develop when CSF transit is blocked by parasitic
membranes.
30
In patients with ventricular cysts, the
therapeutic approach with cysticidal drugs should be
personalised. Although albendazole successfully
destroys many ventricular cysts, the inammatory
reaction surrounding those cysts may cause acute
hydrocephalus.
81
Neuroendoscopic excision is a
promising alternative in cysticercosis of the lateral or
third ventricles,
8284
although it is used less in fourth
ventricle cysts, for which microsurgery or antiparasitic
treatment are still used in most centres. In the absence
of ependymitis, ventricular shunts are not needed after
removal of a ventricular cyst in most cases. By contrast,
shunt placement should follow or even precede the
excision of ventricular cysts associated with ependymitis.
658 http://neurology.thelancet.com Vol 4 October 2005
Padma
70
Odds ratio
Odds ratio
Baranwal
71
Kalra
72
*
Gogia
73
Singhi
74
Baranwal
71
Kalra
72
*
Gogia
73
Singhi
74
0 1 2 3 4
0 2 4 6 8 10
Figure 4: Treatment of neurocysticercosis with ABZ
Odds ratios for lesion disappearance (top) and seizure relapse (bottom) in randomised trials in patients with single
enhancing lesions treated with ABZ compared to placebo (three trials) or prednisone (three trials, one had both
types of controls). *Included some patients with two enhancing lesions; data for patients with a single enhancing
lesion only.
Review
Other locations
Patients with intrasellar cysticerci present with
ophthalmic and endocrinological disturbances similar to
those produced by pituitary tumours.
85
Spinal
cysticercosis, mostly extramedullary, presents with root
pain or motor and sensory decits that vary according to
the level of the lesion,
86
and is most common in the
cervical segments.
8789
Ophthalmic cysticercosis is not
rare in endemic countries and is found in any of the eye
chambers (most commonly the retina or vitreous),
causing a decrease of visual acuity or visual eld
defects.
90,91
Massive cysticercal infection of striated
muscles may produce generalised weakness associated
with progressive muscle enlargement.
1,92
Epidemiology and control
Despite occasional scepticism,
93
most clinicians agree
that neurocysticercosis is the main cause of acquired
epilepsy in low-income countries and probably in the
world.
9496
The prevalence of epilepsy in endemic
countries is clearly higher than in North America or
Europe, although this could be due to other factors
including prenatal and delivery care, or other
infections.
94
Recently, several articles from different
countries in South and Central America consistently
showed an association between around 30% of all
seizures and cysticercosis.
23,24,97
Neurocysticercosis is potentially eradicable, and
several attempts to control it in eld conditions have
been tried.
15,98103
Farmers use the examination of the
tongue of the pigs, a time-honoured technique that
detects most animals with heavy infections, to take them
to clandestine meat commercialisation circuits
(bypassing formal slaughterhouse systems).
15
Mass
human chemotherapy to eliminate the tapeworm stage
has been tried in Ecuador, Mexico, Guatemala,
Honduras, Peru, and other countries.
99103
Most of these
programmes achieved only a temporal decrease in the
prevalence of cysticercosis (measured in the pig
population, which is the most sensitive and practical
indicator),
15
and returned to preintervention levels soon
after the control pressure was interrupted. A wide-based
programme to eliminate cysticercosis in a province of
Peru is underway, funded by the Bill and Melinda Gates
Foundation. Major obstacles include the lack of basic
sanitary facilities in endemic areas, the extent of
domestic pig raising, the costs of the interventions, and
most importantly, their cultural acceptability.
Conclusions
Cysticercosis is a major cause of epileptic seizures in
most developing countries. Although there is little
information on its natural history, most types and
presentations of neurocysticercosis (depending on the
stage, number, location and size of the parasites, as well
as on the immune response of the host) are well dened.
For example, on the Indian subcontinent, most patients
have a single degenerating cysticercus, whereas in Latin
America multiple viable cysts are common. To dene
and to recognise these main clinical presentations is
central to the understanding of results of serological
tests and to appropriate medical and surgical treatment.
Appropriate management of intracraneal hypertension
or epileptic syndromes is the main aim of management
of patients with neurocysticercosis. Current evidence
favours the use of antiparasitic drugs in most patients
with viable or degenerating lesions, although in patients
with cysticercotic encephalitis this approach is counter-
indicated and in those with calcied lesions it is
unnecessary. In rural endemic communities, neuro-
cysticercosis seems to be symptomatic in only a few
cases, but the disease is an important cause of seizures
because the prevalence of infection is so high.
Neurocysticercosis is potentially eradicable, and control
or eradication programmes are urgently needed to
reduce the burden of this disease.
Acknowledgments
Research grants P01 AI51976, U01 AI35894, and TW05562 from the
US National Institutes of Health, 01107 from the US Food and Drug
Administration, 063109 from The Wellcome Trust, UK, and 23981 from
The Bill and Melinda Gates Foundation, USA, funded other
cysticercosis research by one of the authors (HHG). The sponsors had
no role in the design or writing of this manuscript. Figure 1 was kindly
provided by Dr A E Gonzalez.
Authors contribution
Both authors contributed equally.
Conicts of interest
We have no conicts of interest.
References
1 Garcia HH, Gonzalez AE, Evans CAW, Gilman RH, The
Cysticercosis Working Group in Peru. Taenia soliumcysticercosis.
Lancet 2003; 362: 54756.
2 Del Brutto OH, Sotelo J, Roman GC. Neurocysticercosis: a clinical
handbook. Lisse: Swets and Zeitliger, 1997.
3 Garcia HH, Del Brutto OH, Nash TE, White AC Jr, Tsang VC,
Gilman RH. New concepts in the diagnosis and management of
neurocysticercosis (Taenia solium). Am J Trop Med Hyg 2005;
72: 39.
4 Roman G, Sotelo J, Del Brutto O, et al. A proposal to declare
neurocysticercosis an international reportable disease.
Bull World Health Organ 2000; 78: 399406.
5 Ong S, Talan DA, Moran GJ, et al. Neurocysticercosis in
radiographically imaged seizure patients in US emergency
departments. Emerg Infect Dis 2002; 8: 60813.
http://neurology.thelancet.com Vol 4 October 2005 659
Search strategy and selection criteria
References for this review were identied by searches of
MEDLINE between 1969 and 2005, Old-MEDLINE since
1949, and references from relevant articles; numerous articles
were also identied through searches of the extensive les of
the authors. The search terms cysticercosis,
neurocysticercosis, Taenia solium, albendazole,
praziquantel, and epilepsy were used. Papers published in
English, Spanish, or Portuguese were reviewed. The nal
reference list was generated on the basis of originality and
relevance to the topics covered in the review.
Review
6 Schantz PM, Moore AC, Munoz JL, et al. Neurocysticercosis in an
Orthodox Jewish community in New York City. N Engl J Med 1992;
327: 69295.
7 International Task Force for Disease Eradication. Recommendations
of the International Task Force for Disease Eradication.
MMWR Morb Mortal Wkly Rep 1993; 42 (RR-16): 138.
8 Garcia HH, Gilman RH, Gonzalez AE, et al. Hyperendemic human
and porcine Taenia solium infection in Peru. Am J Trop Med Hyg
2003; 68: 26875.
9 Garcia HH, Gonzalez AE, Gilman RH, The Cysticercosis Working
Group in Peru. Diagnosis, treatment and control of Taenia solium
cysticercosis. Curr Opin Infect Dis 2003; 16: 41119.
10 Gonzalez AE, Lpez-Urbina T, Tsang BY, et al, for The Cysticercosis
Working Group in Peru. Secondary transmission in porcine
cysticercosis: description and their potential implications for control
sustainability. Am J Trop Med Hyg (in press).
11 Escobar A, Weidenheim KM. The pathology of neurocysticercosis.
In: Singh G, Prabhakar S, eds. Taenia solium cysticercosis. From
basic to clinical science. Wallingford: CABI Publishing,
2002: 289305.
12 Evans CAW, The Cysticercosis Working Group in Peru. The
immunology of the host-parasite relationship in Taenia solium
cysticercosis: implications for prevention and therapy. In:
Garcia HH, Martinez SM, eds. Taenia solium taeniasis/cysticercosis,
2nd edn. Lima: Ed Universo, 1999: 2537.
13 Yoshino K. Studies on the post-embryonal development of
Taenia solium: III. On the development of cysticercus cellulosae
within the denitive intermediate host. J Med Assoc Formosa 1933;
32: 16669.
14 Aluja AS, de Martinez JJ, Villalobos A. Taenia solium cysticercosis in
young pigs: age at rst infection and histological characteristics.
Vet Parasitol 1998; 76: 7179.
15 Gonzalez AE, Garcia HH, Gilman RH, Tsang VCW, The
Cysticercosis Working Group in Peru. Control of Taenia solium.
Acta Tropica 2003; 87: 10309.
16 McArthur WP. Cysticercosis as seen in the British Army with
special reference to the production of epilepsy.
Trans R Soc Trop Med Hyg 1934; 27: 34363.
17 Dixon HB, Lipscomb FM. Cysticercosis: an analysis and follow-up
of 450 cases. London: Medical Research Council, 1961.
18 Gajdusek DC. Introduction of Taenia solium into west New Guinea
with a note on an epidemic of burns from cysticercus epilepsy in
the Ekari people of the Wissel Lakes area. P N G Med J 1978;
21: 32942.
19 Singh G. Neurocysticercosis in South-Central America and the
Indian subcontinent. A comparative evaluation. Arq Neuropsiquiatr
1997; 55: 34956.
20 Cruz ME, Schantz PM, Cruz I, et al. Epilepsy and neurocysticercosis
in an Andean community. Int J Epidemiol 1999; 28: 799803.
21 Sanchez AL, Lindback J, Schantz PM, et al. A population-based,
case-control study of Taenia solium taeniasis and cysticercosis.
Ann Trop Med Parasitol 1999; 93: 24758.
22 Garcia-Noval J, Moreno E, de Mata F, et al. An epidemiological
study of epilepsy and epileptic seizures in two rural Guatemalan
communities. Ann Trop Med Parasitol 2001; 95: 16775.
23 Del Brutto OH, Santibanez R, Idrovo L, et al. Epilepsy and
neurocysticercosis in Atahualpa: a door-to-door survey in rural
coastal Ecuador. Epilepsia 2005; 46: 58387.
24 Medina MT, Duron RM, Martinez L, et al. Prevalence, incidence,
and etiology of epilepsies in rural Honduras: the Salama Study.
Epilepsia 2005; 46: 12431.
25 Del Brutto OH, Sotelo J. Neurocysticercosis: an update.
Rev Infect Dis 1988; 10: 107587.
26 Del Brutto OH, Santibanez R, Noboa CA, Aguirre R, Diaz E,
Alarcon TA. Epilepsy due to neurocysticercosis: analysis of
203 patients. Neurology 1992; 42: 38992.
27 Estanol B, Kleriga E, Loyo M, et al. Mechanisms of hydrocephalus
in cerebral cysticercosis: implications for therapy. Neurosurgery
1983; 13: 11923.
28 Rangel R, Torres B, Del Bruto O, Sotelo J. Cysticercotic
encephalitis: a severe form in young females. Am J Trop Med Hyg
1987; 36: 38792.
29 Del Brutto OH. Cysticercosis and cerebrovascular disease: a review.
J Neurol Neurosurg Psychiatry 1992; 55: 25254.
30 Garcia HH, Del Brutto OH. Imaging ndings in neurocysticercosis.
Acta Trop 2003; 87: 7178.
31 Arambulo PV 3rd, Walls KW, Bullock S, Kagan IG. Serodiagnosis of
human cysticercosis by microplate enzyme-linked immunospecic
assay (ELISA). Acta Trop 1978; 35: 6367.
32 Ramos-Kuri M, Montoya RM, Padilla A, et al. Immunodiagnosis of
neurocysticercosis. Disappointing performance of serology (enzyme-
linked immunosorbent assay) in an unbiased sample of neurological
patients. Arch Neurol 1992; 49: 63336.
33 Tsang VC, Brand JA, Boyer AE. An enzyme-linked immunoelectro-
transfer blot assay and glycoprotein antigens for diagnosing human
cysticercosis (Taenia solium). J Infect Dis 1989; 159: 5059.
34 Garcia HH, Martinez M, Gilman R, et al. Diagnosis of cysticercosis
in endemic regions. The Cysticercosis Working Group in Peru.
Lancet 1991; 338: 54951.
35 Prabhakaran V, Rajshekhar V, Murrell KD, Oommen A.
Taenia soliummetacestode glycoproteins as diagnostic antigens for
solitary cysticercus granuloma in Indian patients.
Trans R Soc Trop Med Hyg 2004; 98: 47884.
36 Garcia HH, Gonzalez AE, Gilman RH, et al. Circulating parasite
antigen in patients with hydrocephalus secondary to
neurocysticercosis. Am J Trop Med Hyg 2002; 66: 42730.
37 Del Brutto OH, Rajshekhar V, White AC Jr, et al. Proposed
diagnostic criteria for neurocysticercosis. Neurology 2001;
57: 17783.
38 Garcia HH, Evans CA, Nash TE, et al. Current consensus guidelines
for treatment of neurocysticercosis. Clin Microbiol Rev 2002;
15: 74756.
39 Robles C, Chavarria M. Report of a clinical case of cerebral
cysticercosis treated medically with a new drug: praziquantel.
Salud Publica Mex 1979; 21: 60318.
40 Sotelo J, del Brutto OH, Penagos P, et al. Comparison of therapeutic
regimen of anticysticercal drugs for parenchymal brain cysticercosis.
J Neurol 1990; 237: 6972.
41 Del Brutto OH. Medical treatment of cysticercosis: effective.
Arch Neurol 1995; 52: 10204.
42 Bittencourt PR, Gracia CM, Gorz AM, Mazer S, Oliveira TV. High-
dose praziquantel for neurocysticercosis: efcacy and tolerability.
Eur Neurol 1990; 30: 22934.
43 Corona T, Lugo R, Medina R, Sotelo J. Single-day praziquantel
therapy for neurocysticercosis. N Engl J Med 1996; 334: 125.
44 Vazquez ML, Jung H, Sotelo J. Plasma levels of praziquantel
decrease when dexamethasone is given simultaneously. Neurology
1987; 37: 156162.
45 Sotelo J, Penagos P, Escobedo F, Del Brutto OH. Short course of
albendazole therapy for neurocysticercosis. Arch Neurol 1988;
45: 113033.
46 Garcia HH, Gilman RH, Horton J, et al. Albendazole therapy for
neurocysticercosis: a prospective double-blind trial comparing
7 versus 14 days of treatment. Cysticercosis Working Group in Peru.
Neurology 1997; 48: 142127.
47 Kramer LD. Medical treatment of cysticercosis: ineffective.
Arch Neurol 1995; 52: 10102.
48 Carpio A, Santillan F, Leon P, Flores C, Hauser WA. Is the course of
neurocysticercosis modied by treatment with antihelminthic
agents? Arch Intern Med 1995; 155: 198288.
49 Proano JV, Madrazo I, Avelar F, Lopez-Felix B, Diaz G, Grijalva I.
Medical treatment for neurocysticercosis characterized by giant
subarachnoid cysts. N Engl J Med 2001; 345: 87985.
50 Garcia HH, Pretell EJ, Gilman RH, et al. A trial of antiparasitic
treatment to reduce the rate of seizures due to cerebral cysticercosis.
N Engl J Med 2004; 350: 24958.
51 Nash TE, Del Brutto OH, Butman JA, et al. Calcic
neurocysticercosis and epileptogenesis. Neurology 2004;
62: 193438.
52 Del Brutto OH. Prognostic factors for seizure recurrence after
withdrawal of antiepileptic drugs in patients with neurocysticercosis.
Neurology 1994; 44: 170609.
53 Carpio A, Hauser WA. Prognosis for seizure recurrence in patients
with newly diagnosed neurocysticercosis. Neurology 2002;
59: 173034.
54 Thussu A, Arora A, Prabhakar S, Lal V, Sawhney IM. Acute
symptomatic seizures due to single CT lesions: how long to treat
with antiepileptic drugs? Neurol India 2002; 50: 14144.
660 http://neurology.thelancet.com Vol 4 October 2005
Review
55 Gupta M, Agarwal P, Khwaja GA, et al. Randomized prospective
study of outcome of short term antiepileptic treatment in small
single enhancing CT lesion in brain. Neurol India 2002; 50: 14547.
56 Del Brutto OH, Sotelo J, Roman GC. Therapy for neurocysticercosis:
a reappraisal. Clin Infect Dis 1993; 17: 73035.
57 Madrazo I, Proao J. Tratamiento quirurgico de la
neurocisticercosis. In: Arriagada C, Nogales-Gaete J, Apt W, eds.
Neurocysticercosis. Santiago: Arrynog Ediciones, 1997: 299322.
58 Sotelo J, Marin C. Hydrocephalus secondary to cysticercotic
arachnoiditis. A long-term follow-up review of 92 cases. J Neurosurg
1987; 66: 68689.
59 Suastegui Roman RA, Soto-Hernandez JL, Sotelo J. Effects of
prednisone on ventriculoperitoneal shunt function in hydrocephalus
secondary to cysticercosis: a preliminary study. J Neurosurg 1996;
84: 62933.
60 Flisser A. Taeniasis and cysticercosis due to Taenia solium.
Prog Clin Parasitol 1994; 4: 77116.
61 Flisser A, Correa D, Evans CAW. Taenia soliumcysticercosis: new
and revisited immunological aspects. In: Singh G, Prabhakar S, eds.
Taenia soliumcysticercosis: from basic to clinical science.
Wallingford: CABI Publishing, 2002: 1524.
62 Escobar A. The pathology of neurocysticercosis. In: Palacios E,
Rodriguez-Carbajal J, Taveras JM, eds. Cysticercosis of the central
nervous system. Springeld: Charles C Thomas, 1983: 2754.
63 Rajshekhar V, Abraham J. Disappearing CT lesions in Indian
patients with epilepsy. J Neurol Neurosurg Psychiatry 1990;
53: 81819.
64 Chandy MJ, Rajshekhar V, Ghosh S, et al. Single small enhancing
CT lesions in Indian patients with epilepsy: clinical, radiological and
pathological considerations. J Neurol Neurosurg Psychiatry 1991;
54: 70205.
65 Pittella JE. Neurocysticercosis. Brain Pathol 1997; 7: 68193.
66 Rajshekhar V, Chandy MJ. Validation of diagnostic criteria for
solitary cerebral cysticercus granuloma in patients presenting with
seizures. Acta Neurol Scand 1997; 96: 7681.
67 Pretell EJ, Martinot C Jr, Garcia HH, Alvarado M, Bustos JA,
Martinot C. Differential diagnosis between cerebral tuberculosis and
neurocysticercosis by magnetic resonance spectroscopy.
J Comput Assist Tomogr 2005; 29: 11214.
68 Nash TE, Patronas NJ. Edema associated with calcied lesions in
neurocysticercosis. Neurology 1999; 53: 77781.
69 Nash TE, Pretell J, Garcia HH. Calcied cysticerci provoke
perilesional edema and seizures. Clin Infect Dis 2001; 33: 164953.
70 Padma MV, Behari M, Misra NK, Ahuja GK. Albendazole in single
CT ring lesions in epilepsy. Neurology 1994; 44: 134446.
71 Baranwal AK, Singhi PD, Khandelwal N, Singhi SC. Albendazole
therapy in children with focal seizures and single small enhancing
computerized tomographic lesions: a randomized, placebo-
controlled, double blind trial. Pediatr Infect Dis J 1998; 17: 696700.
72 Kalra V, Dua T, Kumar V. Efcacy of albendazole and short-course
dexamethasone treatment in children with 1 or 2 ring-enhancing
lesions of neurocysticercosis: a randomized controlled trial. J Pediatr
2003; 143: 11114.
73 Gogia S, Talukdar B, Choudhury V, Arora BS. Neurocysticercosis in
children: clinical ndings and response to albendazole therapy in a
randomized, double-blind, placebo-controlled trial in newly
diagnosed cases. Trans R Soc Trop Med Hyg 2003; 97: 41621.
74 Singhi P, Jain V, Khandelwal N. Corticosteroids versus albendazole
for treatment of single small enhancing computed tomographic
lesions in children with neurocysticercosis. J Child Neurol 2004;
19: 32327.
75 Del Brutto OH, Quintero LA. Cysticercosis mimicking brain tumor:
the role of albendazole as a diagnostic tool. Clin Neurol Neurosurg
1995; 97: 25658.
76 Rajshekhar V, Jeyaseelan L. Seizure outcome in patients with a
solitary cerebral cysticercus granuloma. Neurology 2004; 62: 223640.
77 Lobato RD, Lamas E, Portillo JM, et al. Hydrocephalus in cerebral
cysticercosis. Pathogenic and therapeutic considerations. J Neurosurg
1981; 55: 78693.
78 Bickerstaff ER, Cloake PCP, Hughes B, Smith WT. The racemose
form of cerebral cysticercosis. Brain 1952; 75: 116.
79 Barinagarrementeria F, Cantu C. Frequency of cerebral arteritis in
subarachnoid cysticercosis: an angiographic study. Stroke 1998;
29: 12325.
80 Woo E, Yu YL, Huang CY. Cerebral infarct precipitated by
praziquantel in neurocysticercosis: a cautionary note.
Trop Geogr Med 1988; 40: 14346.
81 Cuetter AC, Garcia-Bobadilla J, Guerra LG, Martinez FM, Kaim B.
Neurocysticercosis: focus on intraventricular disease. Clin Infect Dis
1997; 24: 15764.
82 Psarros TG, Zouros A, Coimbra C. Neurocysticercosis: a
neurosurgical perspective. South Med J 2003; 96: 101922.
83 Psarros TG, Krumerman J, Coimbra C. Endoscopic management
of supratentorial ventricular neurocysticercosis: case series and
review of the literature. Minim Invasive Neurosurg 2003; 46: 33134.
84 Bergsneider M, Holly LT, Lee JH, King WA, Frazee JG. Endoscopic
management of cysticercal cysts within the lateral and third
ventricles. J Neurosurg 2000; 92: 1423.
85 Del Brutto OH, Guevara J, Sotelo J. Intrasellar cysticercosis.
J Neurosurg 1988; 69: 5860.
86 Homans J, Khoo L, Chen T, Commins DL, Ahmed J, Kovacs A.
Spinal intramedullary cysticercosis in a ve-year-old child: case
report and review of the literature. Pediatr Infect Dis J 2001;
20: 90408.
87 Kim KS, Weinberg PE. Spinal cysticercosis. Surg Neurol 1985;
24: 8082.
88 Sheehan JP, Sheehan JM, Lopes MB, Jane JA. Intramedullary
cervical spine cysticercosis. Acta Neurochir (Wien) 2002;
144: 106163.
89 Mathuriya SN, Khosla VK, Vasishta RK, Tewari MK, Pathak A,
Prabhakar S. Intramedullary cysticercosis: MRI diagnosis.
Neurol India 2001; 49: 7174.
90 Chang GY, Keane JR. Visual loss in cysticercosis: analysis of
23 patients. Neurology 2001; 57: 54548.
91 Pushker N, Bajaj MS, Chandra M, Neena. Ocular and orbital
cysticercosis. Acta Ophthalmol Scand 2001; 79: 40813.
92 Sawhney BB, Chopra JS, Banerji AK, Wahi PL. Pseudohypertrophic
myopathy in cysticerosis. Neurology 1976; 26: 27072.
93 Carpio A, Escobar A, Hauser WA. Cysticercosis and epilepsy: a
critical review. Epilepsia 1998; 39: 102540.
94 Commission on Tropical Diseases of the International League
Against Epilepsy. Relationship between epilepsy and tropical
diseases. Epilepsia 1994; 35: 8993.
95 White AC Jr. Neurocysticercosis: a major cause of neurological
disease worldwide. Clin Infect Dis 1997; 24: 10113.
96 Schantz PM, Wilkins PP, Tsang VCW. Immigrants, imaging and
immunoblots: the emergence of neurocysticercosis as a signicant
public health problem. In: Scheld WM, Craig WA, Hughes JM,
eds. Emerging infections 2. Washington: ASM Press, 1998: 21341.
97 Montano SM, Villaran MV, Ylquimiche L, et al, for The
Cysticercosis Working Group in Peru. Neurocysticercosis:
association between seizures, serology and brain CT in rural Peru.
Neurology 2005; 65: 22933.
98 Gilman R, Garcia HH, Gonzalez AE, Dunleavy M, Verastegui M,
Evans C, The Cysticercosis Working Group in Peru. Short cuts to
development: methods to control the transmission of cysticercosis
in developing countries. In: Garcia HH, Martinez SM, eds.
Taenia solium taeniasis/cysticercosis (2nd edn). Lima: Ed Universo,
1999: 31326.
99 Sarti E, Schantz PM, Avila G, Ambrosio J, Medina-Santillan R,
Flisser A. Mass treatment against human taeniasis for the control
of cysticercosis: a population-based intervention study.
Trans R Soc Trop Med Hyg 2000; 94: 8589.
100 Allan JC, Velasquez-Tohom M, Fletes C, et al. Mass chemotherapy
for intestinal Taenia solium infection: effect on prevalence in
humans and pigs. Trans R Soc Trop Med Hyg 1997; 91: 59598.
101 Diaz Camacho SP, Candil Ruiz A, Suate Peraza V, et al.
Epidemiologic study and control of Taenia solium infections with
praziquantel in a rural village of Mexico. Am J Trop Med Hyg 1991;
45: 52231.
102 Cruz M, Davis A, Dixon H, Pawlowski ZS, Proano J. Operational
studies on the control of Taenia solium taeniasis/cysticercosis in
Ecuador. Bull World Health Organ 1989; 67: 40107.
103 Keilbach NM, de Aluja AS, Sarti-Gutierrez E. A programme to
control taeniasis-cysticercosis (T. solium): experiences in a Mexican
village. Acta Leiden 1989; 57: 18189.
http://neurology.thelancet.com Vol 4 October 2005 661
También podría gustarte
- Basic Science Quick Facts Step1Documento31 páginasBasic Science Quick Facts Step1Hannah Jackson100% (20)
- Pediatric Infectious Disease - A Practically Painless Review (2015)Documento213 páginasPediatric Infectious Disease - A Practically Painless Review (2015)Fajrin Ashari100% (2)
- Acute Headache in The ED Evidence-Based Evaluation and Treatment OptionsDocumento32 páginasAcute Headache in The ED Evidence-Based Evaluation and Treatment OptionsSasi KumarAún no hay calificaciones
- Water QualityDocumento34 páginasWater QualitySarim ChAún no hay calificaciones
- K - 18 Infection of The CNS (Neurologi)Documento137 páginasK - 18 Infection of The CNS (Neurologi)Vera AristaAún no hay calificaciones
- 12-Cytokines 2020-2Documento26 páginas12-Cytokines 2020-2Rami AlhilliAún no hay calificaciones
- Vaccination a Delusion: Its Penal Enforcement a Crime: Proved by the Official Evidence in the Reports of the Royal CommissionDe EverandVaccination a Delusion: Its Penal Enforcement a Crime: Proved by the Official Evidence in the Reports of the Royal CommissionAún no hay calificaciones
- Pathophysiology of Leptospirosis and Dengue FeverDocumento5 páginasPathophysiology of Leptospirosis and Dengue FeverKenneth Lagman100% (1)
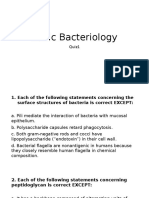
- Microbiology Quiz1 (Basic Bacteriology)Documento26 páginasMicrobiology Quiz1 (Basic Bacteriology)ROHITAún no hay calificaciones
- C PerfringensDocumento2 páginasC PerfringensArifin R HidayatAún no hay calificaciones
- Approach To An Unconscious PatientDocumento62 páginasApproach To An Unconscious Patientangiolikkia80% (5)
- A Novel of Typhoid Mary: FEVER by Mary Beth KeaneDocumento16 páginasA Novel of Typhoid Mary: FEVER by Mary Beth KeaneSimon and Schuster95% (19)
- Clinical symptoms, diagnosis, and treatment of neurocysticercosisDocumento15 páginasClinical symptoms, diagnosis, and treatment of neurocysticercosisIngVictorHuertaAún no hay calificaciones
- 1.1 BackgroundDocumento13 páginas1.1 BackgroundmayawjyAún no hay calificaciones
- Neuro Cystic Er Cos IsDocumento14 páginasNeuro Cystic Er Cos IsAndreaAún no hay calificaciones
- Mehu131 - U1 - T6 - Clinical Symptoms, Diagnosis, and Treatment of NeuricysticercosisDocumento14 páginasMehu131 - U1 - T6 - Clinical Symptoms, Diagnosis, and Treatment of NeuricysticercosisGabriel OlivaresAún no hay calificaciones
- Neurocisticercosis: Neurología - InfectologíaDocumento7 páginasNeurocisticercosis: Neurología - Infectologíasanti gamer mAún no hay calificaciones
- Neurocisticercosis PDFDocumento7 páginasNeurocisticercosis PDFFiorella Alexandra HRAún no hay calificaciones
- Nihms 985420Documento30 páginasNihms 985420Frank Harry LampardAún no hay calificaciones
- Pathogens 11 01212Documento13 páginasPathogens 11 01212Bapa akuAún no hay calificaciones
- Cabasso, 1958. Hepatitis en PerrosDocumento17 páginasCabasso, 1958. Hepatitis en PerrosJavi CarrilloAún no hay calificaciones
- 06 Neurocisticercosis Actualidad y AvancesDocumento7 páginas06 Neurocisticercosis Actualidad y Avancesfeliecheverria11Aún no hay calificaciones
- Accepted Manuscript: Acta TropicaDocumento24 páginasAccepted Manuscript: Acta TropicaakshayajainaAún no hay calificaciones
- Jurnal Kedokteran Dan Kesehatan Indonesia: Current Trends of Diagnosis and Management of NeurocysticercosisDocumento8 páginasJurnal Kedokteran Dan Kesehatan Indonesia: Current Trends of Diagnosis and Management of NeurocysticercosisMagfira HermanAún no hay calificaciones
- Oral Cysticercosis: Case Report and Review of The LiteratureDocumento4 páginasOral Cysticercosis: Case Report and Review of The LiteraturePeiterGozaliAún no hay calificaciones
- The Pathogenesis of Acute Viral Encephalitis and Postinfectious EncephalomyelitisDocumento6 páginasThe Pathogenesis of Acute Viral Encephalitis and Postinfectious EncephalomyelitisBill RajagukgukAún no hay calificaciones
- Sistiserkosis Taenia Solium PDFDocumento10 páginasSistiserkosis Taenia Solium PDFOgix HilandoAún no hay calificaciones
- Enterovirus DR - MiraDocumento28 páginasEnterovirus DR - MiraPranudiah Yulianti NingtiasAún no hay calificaciones
- Cox Sack I e VirusesDocumento3 páginasCox Sack I e VirusesRuba IjraiwiAún no hay calificaciones
- Neurocysticercosis. A Frequent Cause of Seizures, Epilepsy, and OtherDocumento12 páginasNeurocysticercosis. A Frequent Cause of Seizures, Epilepsy, and OtherMaria Lucero Jinés TapiaAún no hay calificaciones
- Operational Manual - Newcastle DiseaseDocumento36 páginasOperational Manual - Newcastle DiseasePrasai SaiAún no hay calificaciones
- NCC HG2021Documento7 páginasNCC HG2021RENZO ALEJANDRO ACUÑA FLORESAún no hay calificaciones
- Rickettsial Infections of The Central Nervous SystemDocumento18 páginasRickettsial Infections of The Central Nervous SystemMarilupe Perez GonzalezAún no hay calificaciones
- Neurocysticercosis - an neglected disease in ChileDocumento10 páginasNeurocysticercosis - an neglected disease in ChileDavidAlvarezTerronesAún no hay calificaciones
- Hookworm: Ancylostoma Duodenale and Necator AmericanusDocumento18 páginasHookworm: Ancylostoma Duodenale and Necator AmericanusPutri AmandaAún no hay calificaciones
- Echinococcosis Review: Causes, Symptoms, and TreatmentDocumento9 páginasEchinococcosis Review: Causes, Symptoms, and TreatmentAmalia Nur LatifahAún no hay calificaciones
- CoccocidiopsisDocumento10 páginasCoccocidiopsisMoises PinedaAún no hay calificaciones
- Whitley 2005Documento7 páginasWhitley 2005Firah Triple'sAún no hay calificaciones
- Proceeding of The SEVC Southern European Veterinary ConferenceDocumento4 páginasProceeding of The SEVC Southern European Veterinary ConferenceHartina SamosirAún no hay calificaciones
- Calcific Neurocysticercosis and EpileptogenesisDocumento7 páginasCalcific Neurocysticercosis and EpileptogenesiskreizztelAún no hay calificaciones
- Clinical Microbiology and Infection: A. Mailles, J.-P. Stahl, K.C. BlochDocumento7 páginasClinical Microbiology and Infection: A. Mailles, J.-P. Stahl, K.C. BlochgugicevdzoceAún no hay calificaciones
- Cryptococcosis ManualDocumento3 páginasCryptococcosis Manualnassem54Aún no hay calificaciones
- Chikungunya Virus InfectionDocumento7 páginasChikungunya Virus InfectionWalter Tejada ChaurraAún no hay calificaciones
- Herpes Simplex: Encephalitis Children and Adolescents: Richard J. Whitley, MD, and David W. Kimberlin, MDDocumento7 páginasHerpes Simplex: Encephalitis Children and Adolescents: Richard J. Whitley, MD, and David W. Kimberlin, MDFirah Triple'sAún no hay calificaciones
- Licensed vaccines section details tetanus toxoidDocumento1 páginaLicensed vaccines section details tetanus toxoidRaulimar Hernandez RamosAún no hay calificaciones
- 839 PDFDocumento3 páginas839 PDFRicardo RakaAún no hay calificaciones
- Doi10.1046j.1469 0691.2002.00485.XpdfDocumento7 páginasDoi10.1046j.1469 0691.2002.00485.XpdfRaluca ChiruAún no hay calificaciones
- Topic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"Documento26 páginasTopic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"deekshit dcAún no hay calificaciones
- Leptospirosis - Clinical Aspects - PMCDocumento9 páginasLeptospirosis - Clinical Aspects - PMCJhimy Eraldo Alfaro LopezAún no hay calificaciones
- Arthropod-Borne Encephalitides - UpToDateDocumento21 páginasArthropod-Borne Encephalitides - UpToDateBhargav YagnikAún no hay calificaciones
- Meningitis: According To International Journal of Infection, Among 53 Patients With Meningitis (47%Documento5 páginasMeningitis: According To International Journal of Infection, Among 53 Patients With Meningitis (47%Yzza Mae CabanaAún no hay calificaciones
- PoliomilitisDocumento9 páginasPoliomilitisEko YSAún no hay calificaciones
- PlagueDocumento20 páginasPlagueHemanth G.Aún no hay calificaciones
- Human MonkeypoxDocumento17 páginasHuman MonkeypoxJessica C. S.Aún no hay calificaciones
- Escleritis EpiescleritisDocumento16 páginasEscleritis EpiescleritisAngeloCarpioAún no hay calificaciones
- Journal of Clinical Microbiology-2018-Garcia-JCM.00424-18.fullDocumento23 páginasJournal of Clinical Microbiology-2018-Garcia-JCM.00424-18.fullTolean AndreeviciAún no hay calificaciones
- Taenia SoliumDocumento2 páginasTaenia SoliumGlazy Kim SecoAún no hay calificaciones
- Human Monkeypox Epidemiologic and Clinical Characteristics, Diagnosis, and PreventionDocumento17 páginasHuman Monkeypox Epidemiologic and Clinical Characteristics, Diagnosis, and PreventionVeronicaSanJoséAún no hay calificaciones
- Ecthyma Contagiosum (Human Orf)Documento2 páginasEcthyma Contagiosum (Human Orf)Deba P SarmaAún no hay calificaciones
- Jurnal 1 Treatment and Management of Scleral DisordersDocumento16 páginasJurnal 1 Treatment and Management of Scleral DisordersIndikator SulSelAún no hay calificaciones
- Granulosus and E. Multilocularis (Hydatid) .: Tenia Solium or T. Saginata (Teniasis)Documento7 páginasGranulosus and E. Multilocularis (Hydatid) .: Tenia Solium or T. Saginata (Teniasis)moosAún no hay calificaciones
- Hemolytic-Uremic Syndrome in ChildrenDocumento17 páginasHemolytic-Uremic Syndrome in ChildrenYuri vanessa Ortiz hAún no hay calificaciones
- Toxoplasma GondiiDocumento7 páginasToxoplasma Gondiiأحمد المسيريAún no hay calificaciones
- Case Report Pasteurella Multocida Septicemia in A Patient With CirrhosisDocumento4 páginasCase Report Pasteurella Multocida Septicemia in A Patient With CirrhosisSilviyah MujionoAún no hay calificaciones
- Leptospirosis: Zoonotic Disease Caused by Pathogenic SpirochetesDocumento4 páginasLeptospirosis: Zoonotic Disease Caused by Pathogenic SpirochetesniabustamAún no hay calificaciones
- 2011 Virulence 0059 RDocumento9 páginas2011 Virulence 0059 RHervi LaksariAún no hay calificaciones
- Echinococcosis 1Documento38 páginasEchinococcosis 1Nadine SellersAún no hay calificaciones
- West Nile virus causes fever, encephalitis, rarely fatalDocumento7 páginasWest Nile virus causes fever, encephalitis, rarely fatalkojerzooAún no hay calificaciones
- Mehu131 U1 T6 NeurocysticercosisDocumento16 páginasMehu131 U1 T6 NeurocysticercosisGabriel OlivaresAún no hay calificaciones
- Cryptococcosis - WikipediaDocumento35 páginasCryptococcosis - Wikipedianoveva cenoAún no hay calificaciones
- Fibroscan 01Documento8 páginasFibroscan 01AmiablePCAún no hay calificaciones
- Sick Building Syndrome: Is Mould The Cause?: Abba I Terr, MDDocumento54 páginasSick Building Syndrome: Is Mould The Cause?: Abba I Terr, MDddd79797Aún no hay calificaciones
- BioterrorismDocumento36 páginasBioterrorismMarfaaAún no hay calificaciones
- National EPI Policy & Strategic Guidelines Pakistan 2015Documento64 páginasNational EPI Policy & Strategic Guidelines Pakistan 2015Salman MinhasAún no hay calificaciones
- Solitaire Company ProfileDocumento71 páginasSolitaire Company ProfilesolitairepharmaciaAún no hay calificaciones
- Microbiology (Chapter - Medical Microbiology) Solved MCQs (Set-2)Documento5 páginasMicrobiology (Chapter - Medical Microbiology) Solved MCQs (Set-2)Sufiyan AbduramanAún no hay calificaciones
- The Latest:: Veg. Vs Non-VegDocumento44 páginasThe Latest:: Veg. Vs Non-VegedwincliffordAún no hay calificaciones
- 6-Moehring-SPICE-Antibiotic-use-2019 ANTIBIOTICS HAIS 2020Documento67 páginas6-Moehring-SPICE-Antibiotic-use-2019 ANTIBIOTICS HAIS 2020SIUSANTO HadiAún no hay calificaciones
- International Rice Research Newsletter Vol.7 No.4Documento20 páginasInternational Rice Research Newsletter Vol.7 No.4ccquintosAún no hay calificaciones
- Gastrointestinal Manifestations of HIV Http-::hivinsite - Ucsf.eduDocumento21 páginasGastrointestinal Manifestations of HIV Http-::hivinsite - Ucsf.edufitriAún no hay calificaciones
- Assignment 2Documento3 páginasAssignment 2Anonymous 9MDGo2jAún no hay calificaciones
- National Tuberculosis Management Guidelines 2019 NepalDocumento152 páginasNational Tuberculosis Management Guidelines 2019 NepalRam Maya ShresthaAún no hay calificaciones
- Rice Stink Bug (Oebalus Pugnax)Documento4 páginasRice Stink Bug (Oebalus Pugnax)Rizky Rajabillah PAún no hay calificaciones
- New Microsoft Office Word DocumentDocumento5 páginasNew Microsoft Office Word DocumentAvinash KashyapAún no hay calificaciones
- 2.4 Filarial Worms (PG 30-38)Documento38 páginas2.4 Filarial Worms (PG 30-38)Rj RiveraAún no hay calificaciones
- PROMETRA-UGANDA PROMOTES TRADITIONAL MEDICINEDocumento7 páginasPROMETRA-UGANDA PROMOTES TRADITIONAL MEDICINESekagya YahayaAún no hay calificaciones
- Staph Lecture MicrococcusDocumento30 páginasStaph Lecture Micrococcussophia salibaAún no hay calificaciones
- Morphology of Moulds/ Molds A. ThallusDocumento3 páginasMorphology of Moulds/ Molds A. ThallusJane LappaoAún no hay calificaciones
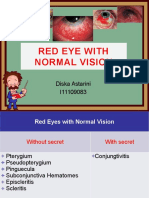
- Red Eye With Normal VisionDocumento58 páginasRed Eye With Normal VisionDiskaAstariniAún no hay calificaciones
- Part5 RespiratoryDiseasesDocumento4 páginasPart5 RespiratoryDiseasesAhmed HamdyAún no hay calificaciones