Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Imanieh - TC Sign in Detection of BA
Cargado por
romeoenny41540 calificaciones0% encontró este documento útil (0 votos)
13 vistas4 páginasTC sign, i.e., triangular structure located cranial to the portal vein bifurcation on ultrasonographic examination, is suggestive of BA in suspected cases. Hepatobiliary scintigraphy had 80% sensitivity, 72.9% specificity, and 74.1% accuracy.
Descripción original:
Título original
Imanieh_TC Sign in Detection of BA
Derechos de autor
© © All Rights Reserved
Formatos disponibles
PDF, TXT o lea en línea desde Scribd
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoTC sign, i.e., triangular structure located cranial to the portal vein bifurcation on ultrasonographic examination, is suggestive of BA in suspected cases. Hepatobiliary scintigraphy had 80% sensitivity, 72.9% specificity, and 74.1% accuracy.
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PDF, TXT o lea en línea desde Scribd
0 calificaciones0% encontró este documento útil (0 votos)
13 vistas4 páginasImanieh - TC Sign in Detection of BA
Cargado por
romeoenny4154TC sign, i.e., triangular structure located cranial to the portal vein bifurcation on ultrasonographic examination, is suggestive of BA in suspected cases. Hepatobiliary scintigraphy had 80% sensitivity, 72.9% specificity, and 74.1% accuracy.
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PDF, TXT o lea en línea desde Scribd
Está en la página 1de 4
ORI GI NAL ARTI CLE
Triangular Cord Sign in Detection of Biliary Atresia:
Is It a Valuable Sign?
Mohammad Hadi Imanieh Seyed Mohsen Dehghani Mohammad Hadi Bagheri
Vahid Emad Mahmood Haghighat Mozhgan Zahmatkeshan
Hamid Reza Forutan Ali Reza Rasekhi Farshid Gheisari
Received: 10 October 2008 / Accepted: 12 January 2009 / Published online: 20 February 2009
Springer Science+Business Media, LLC 2009
Abstract Background Early detection of biliary atresia
(BA) has a vital role in prevention of liver cirrhosis in these
patients. There are some evidences that triangular cord
(TC) sign, i.e., triangular structure located cranial to the
portal vein bifurcation on ultrasonographic examination, is
suggestive of BA in suspected cases. The aim of this study
is to evaluate and compare the sensitivity, specicity, and
accuracy of TC sign with other methods of diagnosis such
as hepatobiliary scan. Methods Fifty-eight infants referred
to pediatric gastroenterology ward with diagnosis of
infantile cholestasis from March 2004 to March 2008 were
evaluated to nd the cause of cholestasis. Diagnosis was
made by means of history, clinical examination, hepatob-
iliary scan, and liver biopsy. Ultrasonographic examination
was focused on presence of TC sign in patients. If the
diagnosis was in favor of BA, patient was sent for direct
cholangiography as a gold-standard test for conrmation of
the diagnosis. The sensitivity, specicity, and accuracy of
the tests were compared with golden standard. Results
Among 58 infants with infantile cholestasis, BA was
diagnosed and conrmed in 10 infants (17.2%). Hepatob-
iliary scintigraphy had 80% sensitivity, 72.9% specicity,
and 74.1% accuracy. TC sign had 70% sensitivity, 95.8%
specicity, and 91.3% accuracy. Conclusion TC sign is
more accurate than hepatobiliary scan and has acceptable
sensitivity and specicity for diagnosis of BA.
Keywords Biliary atresia Triangular cord sign
Accuracy
Introduction
Early detection of infantile cholestasis is the most impor-
tant factor for determination of prognosis, especially in
biliary atresia (BA) [1]. In 70% of cases, differentiation
between neonatal hepatitis and BA is a working diagnosis
[2]. The diagnosis of BA in infants is based on hepatobil-
iary scintigraphy, sonography, percutaneous liver biopsy,
and intraoperative cholangiography.
Stable general condition of BA patients is one of the
factors that delay referral to gastroenterologist.
Another factor is invasiveness of diagnostic methods,
which are also time consuming and costly.
In 1996, Choi et al. [1] reported a new sonographic
nding in BA patients, called triangular cord (TC) sign. It
is a triangular structure, composed of brous tissue located
cranial to the portal vein bifurcation. Although some
studies reported 100% accuracy of TC sign in detection of
BA [3], most studies report accuracy of 7090% for this
sign [4].
M. H. Imanieh S. M. Dehghani (&) V. Emad M. Haghighat
Gastroenterohepatology Research Center, Nemazee Hospital,
Shiraz University of Medical Sciences, Shiraz 71937-11351, Iran
e-mail: dehghanism@sums.ac.ir
M. H. Imanieh S. M. Dehghani M. Haghighat
M. Zahmatkeshan
Department of Pediatric Gastroenterology, Nemazee Hospital,
Shiraz University of Medical Sciences, Shiraz, Iran
M. H. Bagheri A. R. Rasekhi
Department of Radiology, Nemazee Hospital,
Shiraz University of Medical Sciences, Shiraz, Iran
H. R. Forutan
Department of Pediatric Surgery, Nemazee Hospital,
Shiraz University of Medical Sciences, Shiraz, Iran
F. Gheisari
Department of Nuclear Medicine, Nemazee Hospital,
Shiraz University of Medical Sciences, Shiraz, Iran
1 3
Dig Dis Sci (2010) 55:172175
DOI 10.1007/s10620-009-0718-3
In this study we investigate the accuracy of TC sign
compared with hepatobiliary scintigraphy, liver biopsy,
and cholangiography in diagnosis of BA.
Patients and Methods
Participants in this study were infants referred to pediatric
gastroenterology ward afliated to Shiraz University of
Medical Sciences with diagnosis of infantile cholestasis
from March 2004 to March 2008. After preliminary
examination and blood tests, liver and biliary system
sonography was performed after at least 4 h fasting using
General Electric Logic 7 equipped with 7-MHz linear
transducer for all patients. The ultrasonographic examina-
tion focused on presence or absence of TC sign at the porta
hepatis as mentioned above. Hepatobiliary scintigraphy
was also performed for all patients. Percutaneous liver
biopsy was the next step of diagnosis and differentiating
between neonatal hepatitis and BA. The diagnosis of BA in
liver biopsy was suggested by presence of bile duct pro-
liferation, bile rosette, or other features suggestive of
extrahepatic obstruction. If the diagnosis was in favor of
BA, patient was sent for direct cholangiography for con-
rmation of the diagnosis. Kasai operation was done for
BA patients.
Presence of TC sign was investigated in patients con-
sidering the denite diagnosis by means of liver biopsy and
cholangiography.
Results
Of 58 patients recruited for the study, 25 patients were
female (43.1%) and 33 patients were male (56.9%) with
mean age of 46 14 days (range 30120 days). The
beginning onset of the symptoms in infants ranged from 1
to 120 days old (mean 32.4 33.5 days).
Among 58 infants with infantile cholestasis, BA was
diagnosed and conrmed in 10 infants (17.2%). Other
causes of cholestasis are shown in Table 1.
From ten infants with denite diagnosis of BA, hepa-
tobiliary scintigraphy was positive in eight patients
(sensitivity = 80%).
Thirteen patients had positive hepatobiliary scan for BA
but further workups conrmed other diagnoses [specic-
ity = 72.9%, positive predictive value (PPV) = 38.1%,
negative predictive value (NPV) = 94.5%] (Table 2).
From ten patients with conrmed BA, seven patients
(70%) had TC sign in their ultrasonographic examination
(sensitivity = 70%).
Two patients had TC sign in the ultrasonographic
examination but further workups revealed the diagnosis of
neonatal hepatitis (specicity = 95.8%).
Presence of TC sign in ultrasonographic examination
was signicantly correlated with diagnosis of BA in
infants, with PPV of 77.8% and NPV of 93.9%.
(P = 0.0002) (Table 3).
In the validity study, the percentage agreement between
ultrasonographic nding of TC sign and gold standard
(accuracy of the test) was 91.3%. The calculated accuracy
for hepatobiliary scan was 74.2%. Combination of hepa-
tobiliary scan and TC sign in ultrasonography showed that
nine of ten conrmed BA patients had at least one positive
result for these diagnostic methods (sensitivity 90%). The
number of false-positive and false-negative results of
combination diagnosis was 12 and 1, respectively (speci-
city = 79.9%, PPV = 40.9%, NPV = 97.2%).
Table 1 Final diagnosis of patients referred for infantile cholestasis
Idiopathic
neonatal
hepatitis
Biliary
atresia
Progressive
familial
intrahepatic
cholestasis
Biliary
sludge
Cystic
brosis
Galactosemia Cytomegalovirus
hepatitis
Glycogen
storage
disease
Alagille
syndrome
Niemann
Pick
disease
23
(39.6%)
10
(17.2%)
7
(12.1%)
4
(6.9%)
3
(5.2%)
3
(5.2%)
2
(3.4%)
2
(3.4%)
2
(3.4%)
2
(3.4%)
Table 3 Comparison of the results of ultrasonography and
cholangiography
Positive
TC sign
Negative
TC sign
Cholangiogram in favor of BA 7 3
Cholangiogram against BA 2 46
Table 2 Comparison of the results of hepatobiliary scintigraphy and
cholangiography
Hepatobiliary
scan in favor
of BA
Hepatobiliary
scan against
BA
Cholangiogram in favor of BA 8 2
Cholangiogram against BA 13 35
Dig Dis Sci (2010) 55:172175 173
1 3
Discussion
Immediate treatment of BA has vital role in prevention of
liver cirrhosis. Accurate and early diagnosis is important
for early treatment.
Invasive and expensive methods of diagnosis of BA are
two major factors that delay the process of diagnosis in
golden time.
Liver biopsy is a valuable procedure to differentiate
neonatal hepatitis from BA [5]. Although liver biopsy is
safe, it is still an invasive procedure and needs hemody-
namic and coagulation system stability. Impaired liver
function in patients sometimes leads to coagulopathies that
delay the process of liver biopsy. It will be advantageous
for patients to nd a noninvasive method to replace liver
biopsy for diagnosis of BA.
In the study, performed in our center between 2003 and
2006, sensitivity, specicity, PPV, and NPV of different
diagnostic methods was evaluated and compared with
direct cholangiography as the gold-standard method for
diagnosis of BA [5]. Ultrasonography, which is noninva-
sive, nonionizing, less expensive, and produces real-time
images, is still a preferable tool for evaluation of hepa-
tobiliary tree, especially in infants and neonates who need
sedation for magnetic resonance imaging. Reported accu-
racies of the hepatobiliary scintigraphy and ultraso-
nography (not on the basis of TC sign) for detection of BA
were 58.5% and 69.2%, respectively [5].
After reports of Choi et al. [1] and Park et al. [68]
about the sensitivity and specicity of TC sign in diagnosis
of BA, it became a major interest to evaluate and stan-
dardize the accuracy of this sign in diagnosis of BA.
Our research showed 70% sensitivity and 95.8% speci-
city of TC sign in diagnosis of BA.
The specicity of TC sign (95.8%) is much higher
compared with hepatobiliary scintigraphy (72.9%). The
PPV of TC sign is two times higher than hepatobiliary
scintigraphy (77.8% versus 38.1%). To improve the accu-
racy of ultrasonographic imaging in the diagnosis of BA,
Park et al. [6] proposed combining TC sign with gallbladder
imaging. Positive TC sign coupled with abnormal gall-
bladder length improves PPV value to 100% in the
diagnosis of BA. Recent study showed PPV and NPV in the
diagnosis of BA of 98 and 100%, respectively, if positive
TC sign was combined with either abnormal size or
abnormal contractility of the gallbladder [9]. Our study
showed that TC sign has much higher accuracy compared
with hepatobiliary scan. Statistical analysis showed agree-
ment of 73.6% between TC sign and hepatobiliary scan.
Also Wongsawasdi et al. [10] suggested that TC sign is a
noninvasive and easily available test when combined with
acholic stool and gammaglutamyl transpeptidase level.
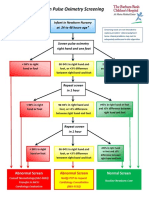
It seems that positive TC sign in ultrasonography is
accurate enough to bypass liver biopsy and to candidate
patient for intraoperative cholangiography, but in case of
clinical suspicion of BA and negative TC sign, liver biopsy
is essential to conrm the diagnosis. The suggested algo-
rithm for evaluation of suspicious infant to have BA is
shown in Fig. 1.
References
1. Choi SO, Pare WH, Lee HJ, Woo S. Triangular cord: a sono-
graphic nding applicable in the diagnosis of biliary atresia. J
Pediatr Surg. 1996;31:363366. doi:10.1016/S0022-3468(96)
90739-3.
2. A-Kader HH, Balistreri WF. Neonatal hepatobiliary disease. Se-
min Gastrointest Dis. 1994;5:115.
3. Kotb MA, Kotb A, Sheba MF, et al. Evaluation of the triangular
cord sign in the diagnosis of biliary atresia. Pediatrics.
2001;108:416420. doi:10.1542/peds.108.2.416.
4. Kanegawa K, Yoshinobu A, Kitamura E, et al. Sonographic
diagnosis of biliary atresia in pediatric patients using the
Patient presenting with cholestasis
Ultrasonography
Triangular
cord sign
positive
Triangular
cord sign
negative
Biliary
atresia
Neonatal
hepatitis
Intraoperative
cholangiography
Liver
biopsy
Fig. 1 Suggested algorithm for diagnosis and management of infants
with cholestasis
174 Dig Dis Sci (2010) 55:172175
1 3
Triangular cord sign versus gallbladder length and contraction.
AJR Am J Roentgenol. 2003;181:13871390.
5. Dehghani SM, Haghighat M, Imanieh MH, Geramizadeh B.
Comparison of different diagnostic methods in infants with
cholestasis world. J Gastroenterol. 2006;12(36):58935896.
6. Park WH, Choi SO, Lee HJ, Kim SP, Zeon SK, Lee SK. A new
diagnostic approach to Biliary atresia with emphasis on the
ultrasonographic triangular cord sign: comparison of ultraso-
nography, hepatobiliary scintigraphy, and liver needle biopsy in
the evaluation of infantile cholestasis. J Pediatr Surg.
1997;32:15551559. doi:10.1016/S0022-3468(97)90451-6.
7. Park WH, Choi SO, Lee HJ. The ultrasonographic triangular
cord coupled with gallbladder images in diagnostic prediction of
biliary atresia from infantile intrahepatic cholestasis. J Pediatr
Surg. 1999;34(11):17061710. doi:10.1016/S0022-3468(99)90
650-4.
8. Park WH, Choi SO, Lee HJ. Technical innovation for noninva-
sive and early diagnosis of biliary atresia: the ultrasonographic
triangular cord sign. J Hepatobiliary Pancreat Surg.
2001;8:337341. doi:10.1007/s005340170005.
9. Takamizawa S, Zaimaa A, Muraji T, et al. Can biliary atresia be
diagnosed by ultrasonography alone? J Pediatr Surg.
2007;42(12):20932096. doi:10.1016/j.jpedsurg.2007.08.032.
10. Wongsawasdi L, Ukarapol N, Visrutaratna P, Singhavejsakul J,
Kattipattanapong V. Diagnostic evaluation of infantile cholesta-
sis. J Med Assoc Thai. 2008;91(3):345349.
Dig Dis Sci (2010) 55:172175 175
1 3
También podría gustarte
- DD Viral ExantemDocumento4 páginasDD Viral Exantemsiska_mariannaAún no hay calificaciones
- List of Allergens: Skin Prick Test Allergens 01/29/2016Documento3 páginasList of Allergens: Skin Prick Test Allergens 01/29/2016romeoenny4154Aún no hay calificaciones
- Contoh ReviewDocumento6 páginasContoh Reviewromeoenny4154Aún no hay calificaciones
- 51 Allergens Patch Test SetDocumento2 páginas51 Allergens Patch Test Setromeoenny4154Aún no hay calificaciones
- Dizziness in PaedDocumento7 páginasDizziness in Paedromeoenny4154Aún no hay calificaciones
- HemophiliaDocumento2 páginasHemophiliaromeoenny4154Aún no hay calificaciones
- Ulceration Slides 090331Documento62 páginasUlceration Slides 090331mumutdwsAún no hay calificaciones
- Pneumonia and Respiratory Tract Infections in ChildrenDocumento37 páginasPneumonia and Respiratory Tract Infections in ChildrenjayasiinputAún no hay calificaciones
- PolyarthritisDocumento6 páginasPolyarthritisromeoenny4154Aún no hay calificaciones
- Bronchiolitis Clinical Guideline2014Documento2 páginasBronchiolitis Clinical Guideline2014romeoenny4154Aún no hay calificaciones
- Febrile Seizure GuidelineDocumento1 páginaFebrile Seizure GuidelinesmileyginaaAún no hay calificaciones
- Clinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls BackgroundDocumento5 páginasClinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls Backgroundromeoenny4154Aún no hay calificaciones
- Clinical guideline for evaluation and treatment of febrile neonatesDocumento1 páginaClinical guideline for evaluation and treatment of febrile neonatesromeoenny4154Aún no hay calificaciones
- Acute Fever in Children and InfantDocumento26 páginasAcute Fever in Children and Infantromeoenny4154Aún no hay calificaciones
- Congenital Heart Disease 2014Documento1 páginaCongenital Heart Disease 2014romeoenny4154Aún no hay calificaciones
- Children Perio DiseasesDocumento9 páginasChildren Perio Diseasesdr parveen bathlaAún no hay calificaciones
- Common Anemia in Pediatric BRM - PM - V1P4 - 03Documento12 páginasCommon Anemia in Pediatric BRM - PM - V1P4 - 03romeoenny4154Aún no hay calificaciones
- Common Anemia in Pediatric BRM - PM - V1P4 - 03Documento12 páginasCommon Anemia in Pediatric BRM - PM - V1P4 - 03romeoenny4154Aún no hay calificaciones
- Calvin K.W. Tong Approach To A Child With A Cough: General PresentationDocumento5 páginasCalvin K.W. Tong Approach To A Child With A Cough: General Presentationromeoenny4154Aún no hay calificaciones
- Afebrile SeizuresDocumento11 páginasAfebrile SeizuresMai Hunny100% (1)
- Approach To Acute Arthritis in Kids: Allyson Mcdonough, MD Baylor Scott & White Health Department of RheumatologyDocumento35 páginasApproach To Acute Arthritis in Kids: Allyson Mcdonough, MD Baylor Scott & White Health Department of Rheumatologyromeoenny4154Aún no hay calificaciones
- Acute Stridor Diagnostic Challenges in Different Age Groups Presented To The Emergency Department 2165 7548.1000125Documento4 páginasAcute Stridor Diagnostic Challenges in Different Age Groups Presented To The Emergency Department 2165 7548.1000125romeoenny4154Aún no hay calificaciones
- Clinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls BackgroundDocumento5 páginasClinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls Backgroundromeoenny4154Aún no hay calificaciones
- Common Anemia in Pediatric BRM - PM - V1P4 - 03Documento12 páginasCommon Anemia in Pediatric BRM - PM - V1P4 - 03romeoenny4154Aún no hay calificaciones
- Adhd Scoring ParentDocumento3 páginasAdhd Scoring Parentromeoenny4154Aún no hay calificaciones
- DD Viral ExantemDocumento4 páginasDD Viral Exantemsiska_mariannaAún no hay calificaciones
- Guidelines Clinical Management Chikungunya WHODocumento26 páginasGuidelines Clinical Management Chikungunya WHOFábio CantonAún no hay calificaciones
- GinggivostomatitisDocumento6 páginasGinggivostomatitisromeoenny4154Aún no hay calificaciones
- Asthma ED Clinical Guideline2014Documento5 páginasAsthma ED Clinical Guideline2014romeoenny4154Aún no hay calificaciones
- Croup GuidelineDocumento17 páginasCroup Guidelineromeoenny4154Aún no hay calificaciones
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Machine Learning Predicts 5-Chloro-1 - (2 - Phenylethyl) - 1h-Indole-2,3-Dione As A Drug Target For Fructose Bisphosphate Aldolase in Plasmodium FalciparumDocumento7 páginasMachine Learning Predicts 5-Chloro-1 - (2 - Phenylethyl) - 1h-Indole-2,3-Dione As A Drug Target For Fructose Bisphosphate Aldolase in Plasmodium FalciparumInternational Journal of Innovative Science and Research TechnologyAún no hay calificaciones
- (Doi 10.1016/j.ijpharm.2015.01.022) T. Loftsson - Excipient Pharmacokinetics and ProfilingDocumento7 páginas(Doi 10.1016/j.ijpharm.2015.01.022) T. Loftsson - Excipient Pharmacokinetics and ProfilingRia DeviAún no hay calificaciones
- Ejercicios DBT (TDC)Documento4 páginasEjercicios DBT (TDC)vanessa_lm_Aún no hay calificaciones
- Firstaid ModuleDocumento143 páginasFirstaid Moduleretni wulandariAún no hay calificaciones
- Daftar Obat High AlertDocumento2 páginasDaftar Obat High Alertayu aAún no hay calificaciones
- Unit 5 Hospital EquipmentDocumento3 páginasUnit 5 Hospital EquipmentALIFIAAún no hay calificaciones
- High Level Technical Meeting On Health Risks at The Human-Animal-Ecosystems Interfaces Mexico City, Mexico 15-17 November 2011Documento7 páginasHigh Level Technical Meeting On Health Risks at The Human-Animal-Ecosystems Interfaces Mexico City, Mexico 15-17 November 2011d3bd33pAún no hay calificaciones
- Rhubarb April 2017Documento17 páginasRhubarb April 2017ISADD LietuvaAún no hay calificaciones
- Population Health ManagementDocumento25 páginasPopulation Health ManagementVitreosHealthAún no hay calificaciones
- Benefits of Equality ToolkitDocumento64 páginasBenefits of Equality ToolkitBasic Rights OregonAún no hay calificaciones
- Klasifikasi Penyebab KomaDocumento19 páginasKlasifikasi Penyebab KomaNoni JacksonAún no hay calificaciones
- Appendix2 Full Reccomendations Afac205Documento138 páginasAppendix2 Full Reccomendations Afac205julietaAún no hay calificaciones
- CBTDocumento21 páginasCBTsavvy_as_98Aún no hay calificaciones
- Cebu Normal University College of NursingDocumento7 páginasCebu Normal University College of NursingGwyn RosalesAún no hay calificaciones
- Chester V Afshar (2005) 1 A.C. 134Documento33 páginasChester V Afshar (2005) 1 A.C. 134V100% (1)
- Niyog-Niyogan - Quisqualis Indica Herbal Medicine-Health Benefits-Side Effects PDFDocumento4 páginasNiyog-Niyogan - Quisqualis Indica Herbal Medicine-Health Benefits-Side Effects PDFJikka RodriguezAún no hay calificaciones
- 110 TOP SURGERY Multiple Choice Questions and Answers PDF - Medical Multiple Choice Questions PDFDocumento11 páginas110 TOP SURGERY Multiple Choice Questions and Answers PDF - Medical Multiple Choice Questions PDFaziz0% (1)
- Dimensional Modeling Basics For HealthcareDocumento27 páginasDimensional Modeling Basics For Healthcareduwayne_willettAún no hay calificaciones
- Medication Error Reporting FormDocumento2 páginasMedication Error Reporting Formahmad ganieAún no hay calificaciones
- FIP PharmabridgeDocumento2 páginasFIP PharmabridgeInternational Pharmaceutical Students' Federation (IPSF)Aún no hay calificaciones
- Dental instruments for extracting teethDocumento18 páginasDental instruments for extracting teethKateryna BondarenkoAún no hay calificaciones
- Overcoming Low Self-Esteem Extract PDFDocumento40 páginasOvercoming Low Self-Esteem Extract PDFMarketing Research0% (1)
- Staff Nurse Interview Questions 2Documento3 páginasStaff Nurse Interview Questions 2daciana_ilie100% (2)
- Introduction To Dental Anatomy: DR - Yad Raouf BDS, Efb, MrcsedDocumento27 páginasIntroduction To Dental Anatomy: DR - Yad Raouf BDS, Efb, MrcsedRabarAún no hay calificaciones
- CPM14th DIABETES Food GuideDocumento21 páginasCPM14th DIABETES Food GuideXhiariwen Bayro0% (1)
- ICU protocol 2015 قصر العيني by mansdocsDocumento227 páginasICU protocol 2015 قصر العيني by mansdocsWalaa YousefAún no hay calificaciones
- You Can Grow Your IntelligenceDocumento6 páginasYou Can Grow Your IntelligenceSoniaAún no hay calificaciones
- Assessment Gestational AgeDocumento61 páginasAssessment Gestational Ageleaslim100% (1)
- Range of Motion PresentationDocumento27 páginasRange of Motion Presentationsathish100% (1)
- Anderson2008 Levofloxasin A ReviewDocumento31 páginasAnderson2008 Levofloxasin A ReviewFazdrah AssyuaraAún no hay calificaciones