Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Anestesia Espinal Preeclampsia Severa
Cargado por
Leonardo GuimelDescripción original:
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Anestesia Espinal Preeclampsia Severa
Cargado por
Leonardo GuimelCopyright:
Formatos disponibles
686 www.anesthesia-analgesia.
org September 2013
Volume 117
Number 3
Copyright 2013 International Anesthesia Research Society
DOI: 10.1213/ANE.0b013e31829eeef5
P
reeclampsia, which affects 5% to 7% of pregnancies,
is a signifcant cause of maternal and neonatal mor-
bidity and mortality
1
and was implicated in 54 of 569
maternal deaths in the United States in 2006.
2
Characterized
by hypertension and proteinuria after 20 weeks gestation,
the pathophysiologic basis of preeclampsia is deranged
angiogenesis with incomplete trophoblastic invasion lead-
ing to small, constricted myometrial spiral arteries with
exaggerated vasomotor responsiveness, superfcial pla-
centation, and placental hypoperfusion. Symptomatic pre-
eclampsia refects widespread endothelial dysfunction, in
which placenta-derived mediators cause multisystem organ
dysfunction.
3
Preeclamptic parturients whose hypertension has been
treated antepartum generally present for delivery with
contracted plasma volume, normal or increased cardiac
output, vasoconstriction, and hyperdynamic left ventricu-
lar function (although left ventricular systolic and diastolic
dysfunction may develop). Additional manifestations
include increased airway edema, decreased glomerular fl-
tration, platelet dysfunction, and a spectrum of hemostatic
derangements (typically accentuated hypercoagulability).
4,5
In severe preeclampsia, chronic placental hypoperfusion
is often signifcant. Since the uteroplacental circulation is
not autoregulated, further decreases in perfusion may be
poorly tolerated by the fetus. Primary peripartum goals in
the severely preeclamptic parturient are the optimization of
maternal blood pressure, cardiac output, and uteroplacental
perfusion and the prevention of seizures and stroke.
Historically, a pervasive belief that spinal anesthesia in
patients with severe preeclampsia causes severe hypoten-
sion and decreased uteroplacental perfusion prevented
the widespread use of spinal anesthesia in these patients.
However, studies show that parturients with severe pre-
eclampsia experience less frequent, less severe hypotension
than healthy parturients. Among patients with severe pre-
eclampsia, spinal anesthesia may cause a greater degree of
hypotension than epidural anesthesia; however, this hypo-
tension is typically easily treated and short lived, and no
studies have demonstrated clinically signifcant differences
in outcomes when spinal anesthesia is compared with epi-
dural or general anesthesia. Riskbeneft considerations
strongly favor neuraxial techniques over general anesthe-
sia for cesarean delivery in the setting of severe preeclamp-
sia as long as neuraxial anesthesia is not contraindicated.
Therefore, spinal anesthesia is a reasonable anesthetic
option in severe preeclampsia when cesarean delivery is
indicated, and there is no indwelling epidural catheter or
contraindication to spinal anesthesia.
SPINAL ANESTHESIA AND HYPOTENSION IN
SEVERE PREECLAMPSIA
Hypotension after spinal anesthesia in severely preeclamp-
tic patients may refect the rapid onset of sympathetic
blockade, underlying intravascular volume depletion, and
possible left ventricular dysfunction. Longstanding obsta-
cles to widespread use of spinal anesthesia for patients
with preeclampsia were concerns about (1) precipitous spi-
nal anesthesiainduced hypotension, superimposed on (2)
preexisting uteroplacental hypoperfusion and (3) the risk
of inducing hypertension or pulmonary edema with sub-
sequent efforts to correct the hypotension.
6
While there was
evidence as early as 1950 that preeclampsia actually attenu-
ates spinal anesthesiainduced hypotension,
7,8
it was not
until the mid-1990s, when clinical trials demonstrated the
safety of spinal and combined spinalepidural (CSE) anes-
thesia in this patient population,
911
that spinal anesthesia
gained acceptance as an alternative to epidural and general
anesthesia for preeclamptic patients.
Most trials assessing the severity of hypotension after
spinal anesthesia among severely preeclamptic parturients
exclude patients in active labor because labor itself attenu-
ates the frequency and severity of the hypotensive response
to neuraxial anesthesia during cesarean delivery.
12
Most
studies are relatively small (n < 150), and the details of pre-
operative antihypertensive and magnesium regimens vary.
Three prospective trials have demonstrated that pre-
eclamptic parturients experience less frequent and less
severe hypotension and require smaller doses of vasopres-
sors than normotensive controls after the initiation of spinal
Spinal anesthesia is widely regarded as a reasonable anesthetic option for cesarean delivery
in severe preeclampsia, provided there is no indwelling epidural catheter or contraindication to
neuraxial anesthesia. Compared with healthy parturients, those with severe preeclampsia expe-
rience less frequent, less severe spinal-induced hypotension. In severe preeclampsia, spinal
anesthesia may cause a higher incidence of hypotension than epidural anesthesia; however,
this hypotension is typically easily treated and short lived and has not been linked to clinically
signifcant differences in outcomes. In this review, we describe the advantages and limitations
of spinal anesthesia in the setting of severe preeclampsia and the evidence guiding intraopera-
tive hemodynamic management. (Anesth Analg 2013;117:68693)
Spinal Anesthesia in Severe Preeclampsia
Vanessa G. Henke, MD,* Brian T. Bateman, MD, and Lisa R. Leffert, MD
From the *Department of Anesthesia, Stanford University School of Medi-
cine, Stanford, California; and Department of Anesthesia, Critical Care and
Pain Medicine, Massachusetts General Hospital, Harvard Medical School,
Boston, Massachusetts.
Accepted for publication May 7, 2013.
Funding: Departmental.
The authors declare no conficts of interest.
Reprints will not be available from the authors.
Address correspondence to Vanessa G. Henke, MD, UCLA Department of
Anesthesiology, Ronald Reagan UCLA Medical Center, 757 Westwood Plaza,
Suite 3325, Los Angeles, CA 90095-7403. Address e-mail to vanessagiselle@
gmail.com.
E FOCUSED REVIEW
Spinal Anesthesia in Severe Preeclampsia
September 2013
Volume 117
Number 3 www.anesthesia-analgesia.org 687
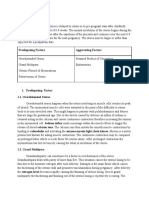
anesthesia (Table1). A potential limitation of an initial study
by Aya et al.
14
was that mean gestational age and fetal
weight were signifcantly lower in the severely preeclamp-
tic group compared with the normotensive group. Resulting
intergroup differences in degree of aortocaval compres-
sion could have contributed to the fnding that hypoten-
sion was less severe in the preeclamptic group. Similarly,
a study by Clark et al.
15
did not control for fetal weight or
gestational age. To correct for this limitation, a follow-up
study by Aya et al.
13
studied preterm parturients present-
ing for nonemergency cesarean delivery and matched the
normotensive and preeclamptic patients for gestational age
(neonatal and placental weights were also comparable). The
severely preeclamptic group experienced a lower incidence
of hypotension requiring treatment (25% vs 41%, P = 0.044)
and received a lower mean cumulative ephedrine dose (10
vs 16 mg, P = 0.031) compared with the normotensive con-
trol group. These fndings indicate that spinal anesthesia
can be safely administered to severely preeclamptic par-
turients undergoing nonemergency cesarean delivery and
that spinal anesthesiainduced hypotension can generally
be treated safely.
SPINAL VERSUS EPIDURAL ANESTHESIA IN
SEVERE PREECLAMPSIA
It was traditionally believed that epidural is safer than spi-
nal anesthesia in the setting of severe preeclampsia because
epidural anesthesia was expected to confer a lower risk of
clinically signifcant hypotension.
6
Studies are inconsistent
as to whether hypotension is more severe after spinal anes-
thesia as compared with epidural anesthesia. However,
the most rigorous study addressing this question, by
Visalyaputra et al.,
16
concluded that although severely pre-
eclamptic patients did experience more severe hypotension
after spinal anesthesia than after epidural anesthesia, that
difference was unlikely to be clinically signifcant.
Earlier studies had reported that vasopressor require-
ments for severely preeclamptic parturients were simi-
lar when comparing spinal with epidural anesthesia
11,17,18
(Table2) and when comparing CSE with epidural anesthesia
(Table 3).
9
Limitations of these early studies included small
sample size,
17
retrospective design
11,18
and heterogeneous
populations, and approaches to fuid
11,17,18
and vasopressor
11,18
administration. In contrast, Visalyaputra et al.
16
conducted
a larger, multicenter randomized controlled trial involving
100 severely preeclamptic parturients (Table2). Spinal anes-
thesia was associated with a higher incidence (51% vs 23%,
P < 0.001) of hypotension (defned as systolic blood pres-
sure <100 mm Hg) during the 20 minutes after induction of
anesthesia. However, the difference in median cumulative
ephedrine dose was small (epidural group: 6 mg vs spinal
group: 12 mg; P = 0.025). In both groups, hypotension was
easily treated and short lived, with the median duration of
hypotension 1 minute or less in both groups. Furthermore,
some of the intergroup differences may have been magnifed
by institutional differences in clinical practice and the ephed-
rine dosing scales that were used.
19
No study has reported
clinically signifcant differences in markers of neonatal well-
being, such as Apgar scores or umbilical artery pH.
9,1618
As emphasized by practice guidelines from the American
Society of Anesthesiologists (ASA)
20
and the American
T
a
b
l
e
1
.
P
r
o
s
p
e
c
t
i
v
e
T
r
i
a
l
s
C
o
m
p
a
r
i
n
g
H
e
m
o
d
y
n
a
m
i
c
C
h
a
n
g
e
s
i
n
S
e
v
e
r
e
l
y
P
r
e
e
c
l
a
m
p
t
i
c
w
i
t
h
N
o
r
m
o
t
e
n
s
i
v
e
P
a
r
t
u
r
i
e
n
t
s
A
u
t
h
o
r
,
s
t
u
d
y
t
y
p
e
S
a
m
p
l
e
s
i
z
e
S
p
i
n
a
l
d
o
s
e
E
p
h
e
d
r
i
n
e
d
o
s
e
F
l
u
i
d
m
a
n
a
g
e
m
e
n
t
C
o
n
c
l
u
s
i
o
n
s
I
m
p
o
r
t
a
n
t
c
h
a
r
a
c
t
e
r
i
s
t
i
c
s
A
y
a
e
t
a
l
.
,
1
3
p
r
o
s
p
e
c
t
i
v
e
c
a
s
e
-
c
o
n
t
r
o
l
S
e
v
e
r
e
l
y
p
r
e
e
c
l
a
m
p
t
i
c
(
n
=
6
5
)
;
n
o
r
m
o
t
e
n
s
i
v
e
(
n
=
7
1
)
H
y
p
e
r
b
a
r
i
c
b
u
p
i
v
a
c
a
i
n
e
(
8
1
2
m
g
)
+
s
u
f
e
n
t
a
n
i
l
(
3
g
)
+
m
o
r
p
h
i
n
e
(
1
0
0
g
)
F
o
r
S
B
P
<
7
0
%
o
f
b
a
s
e
l
i
n
e
,
o
r
(
f
o
r
h
e
a
l
t
h
y
g
r
o
u
p
)
f
o
r
S
B
P
<
1
0
0
m
m
H
g
:
e
p
h
e
d
r
i
n
e
6
m
g
(
e
v
e
r
y
2
m
i
n
b
e
f
o
r
e
,
e
v
e
r
y
5
m
i
n
a
f
t
e
r
d
e
l
i
v
e
r
y
)
1
.
5
2
.
0
L
c
r
y
s
t
a
l
l
o
i
d
p
r
e
l
o
a
d
L
o
w
e
r
i
n
c
i
d
e
n
c
e
o
f
h
y
p
o
t
e
n
s
i
o
n
(
2
5
%
v
s
4
1
%
,
P
=
0
.
0
4
)
a
n
d
l
e
s
s
e
p
h
e
d
r
i
n
e
u
s
e
d
(
1
0
5
v
s
1
6
6
m
g
,
P
=
0
.
0
3
)
i
n
s
e
v
e
r
e
l
y
p
r
e
e
c
l
a
m
p
t
i
c
v
e
r
s
u
s
h
e
a
l
t
h
y
g
r
o
u
p
M
a
t
c
h
e
d
f
o
r
g
e
s
t
a
t
i
o
n
a
l
a
g
e
D
i
f
f
e
r
e
n
t
e
p
h
e
d
r
i
n
e
d
o
s
i
n
g
c
r
i
t
e
r
i
a
f
o
r
e
a
c
h
g
r
o
u
p
A
y
a
e
t
a
l
.
,
1
4
p
r
o
s
p
e
c
t
i
v
e
c
o
h
o
r
t
S
e
v
e
r
e
l
y
p
r
e
e
c
l
a
m
p
t
i
c
(
n
=
3
0
)
;
n
o
r
m
o
t
e
n
s
i
v
e
(
n
=
3
0
)
S
a
m
e
d
o
s
e
s
a
s
i
n
R
e
f
.
1
3
S
a
m
e
e
p
h
e
d
r
i
n
e
d
o
s
e
c
r
i
t
e
r
i
a
a
s
i
n
R
e
f
.
1
3
1
.
5
2
.
0
L
c
r
y
s
t
a
l
l
o
i
d
p
r
e
l
o
a
d
L
o
w
e
r
i
n
c
i
d
e
n
c
e
o
f
h
y
p
o
t
e
n
s
i
o
n
r
e
q
u
i
r
i
n
g
t
r
e
a
t
m
e
n
t
i
n
p
r
e
e
c
l
a
m
p
t
i
c
g
r
o
u
p
(
1
7
%
v
s
5
3
%
,
P
=
0
.
0
0
6
)
a
n
d
l
e
s
s
e
p
h
e
d
r
i
n
e
g
i
v
e
n
(
6
0
v
s
1
3
7
m
g
,
P
=
0
.
0
0
3
)
S
i
g
n
i
f
c
a
n
t
l
y
l
o
w
e
r
g
e
s
t
a
t
i
o
n
a
l
a
g
e
i
n
p
r
e
e
c
l
a
m
p
t
i
c
g
r
o
u
p
v
e
r
s
u
s
h
e
a
l
t
h
y
g
r
o
u
p
(
3
2
3
v
s
3
8
2
w
k
;
P
<
0
.
0
0
0
1
)
D
i
f
f
e
r
e
n
t
e
p
h
e
d
r
i
n
e
d
o
s
i
n
g
c
r
i
t
e
r
i
a
f
o
r
e
a
c
h
g
r
o
u
p
C
l
a
r
k
e
t
a
l
.
,
1
5
p
r
o
s
p
e
c
t
i
v
e
c
a
s
e
-
c
o
n
t
r
o
l
P
r
e
e
c
l
a
m
p
t
i
c
(
n
=
2
0
)
;
n
o
r
m
o
t
e
n
s
i
v
e
(
n
=
2
0
)
H
y
p
e
r
b
a
r
i
c
b
u
p
i
v
a
c
a
i
n
e
1
3
m
g
+
f
e
n
t
a
n
y
l
1
3
g
F
o
r
<
8
0
%
b
a
s
e
l
i
n
e
S
B
P
,
o
r
f
o
r
n
a
u
s
e
a
/
v
o
m
i
t
i
n
g
:
e
p
h
e
d
r
i
n
e
5
m
g
e
v
e
r
y
2
m
i
n
2
5
0
m
L
c
r
y
s
t
a
l
l
o
i
d
L
e
s
s
e
p
h
e
d
r
i
n
e
u
s
e
d
i
n
s
e
v
e
r
e
l
y
p
r
e
e
c
l
a
m
p
t
i
c
v
e
r
s
u
s
h
e
a
l
t
h
y
g
r
o
u
p
(
1
6
1
5
v
s
2
8
1
2
m
g
;
P
<
0
.
0
1
)
L
o
w
e
r
g
e
s
t
a
t
i
o
n
a
l
a
g
e
i
n
p
r
e
e
c
l
a
m
p
t
i
c
v
e
r
s
u
s
h
e
a
l
t
h
y
g
r
o
u
p
:
3
5
3
.
0
v
s
3
9
1
.
2
w
k
D
a
t
a
a
r
e
p
r
e
s
e
n
t
e
d
a
s
i
n
c
i
d
e
n
c
e
(
%
)
,
m
e
a
n
S
D
.
S
B
P
=
s
y
s
t
o
l
i
c
b
l
o
o
d
p
r
e
s
s
u
r
e
.
688 www.anesthesia-analgesia.org ANESTHESIA & ANALGESIA
E FOCUSED REVIEW
T
a
b
l
e
2
.
P
r
o
s
p
e
c
t
i
v
e
T
r
i
a
l
s
C
o
m
p
a
r
i
n
g
S
p
i
n
a
l
A
n
e
s
t
h
e
s
i
a
w
i
t
h
E
p
i
d
u
r
a
l
A
n
e
s
t
h
e
s
i
a
i
n
S
e
v
e
r
e
l
y
P
r
e
e
c
l
a
m
p
t
i
c
P
a
r
t
u
r
i
e
n
t
s
A
u
t
h
o
r
,
s
t
u
d
y
t
y
p
e
S
a
m
p
l
e
s
i
z
e
S
p
i
n
a
l
d
o
s
e
E
p
i
d
u
r
a
l
d
o
s
e
P
r
e
h
y
d
r
a
t
i
o
n
E
p
h
e
d
r
i
n
e
d
o
s
i
n
g
C
o
n
c
l
u
s
i
o
n
s
I
m
p
o
r
t
a
n
t
c
h
a
r
a
c
t
e
r
i
s
t
i
c
s
V
i
s
a
l
y
a
p
u
t
r
a
e
t
a
l
.
,
1
6
p
r
o
s
p
e
c
t
i
v
e
r
a
n
d
o
m
i
z
e
d
S
p
i
n
a
l
(
n
=
5
3
)
;
e
p
i
d
u
r
a
l
(
n
=
4
7
)
H
y
p
e
r
b
a
r
i
c
b
u
p
i
v
a
c
a
i
n
e
1
1
m
g
+
p
r
e
s
e
r
v
a
t
i
v
e
-
f
r
e
e
m
o
r
p
h
i
n
e
2
0
0
g
L
i
d
o
c
a
i
n
e
2
%
w
i
t
h
e
p
i
n
e
p
h
r
i
n
e
1
:
4
0
0
,
0
0
0
(
1
8
2
3
m
L
)
+
f
e
n
t
a
n
y
l
5
0
g
(
T
6
l
e
v
e
l
)
;
a
f
t
e
r
d
e
l
i
v
e
r
y
,
p
r
e
s
e
r
v
a
t
i
v
e
-
f
r
e
e
m
o
r
p
h
i
n
e
3
m
g
5
0
0
m
L
c
o
l
l
o
i
d
o
v
e
r
2
0
m
i
n
F
o
r
S
B
P
1
0
0
1
2
0
m
m
H
g
:
e
p
h
e
d
r
i
n
e
3
m
g
;
f
o
r
S
B
P
<
1
0
0
m
m
H
g
:
e
p
h
e
d
r
i
n
e
6
m
g
(
e
v
e
r
y
2
m
i
n
)
H
i
g
h
e
r
i
n
c
i
d
e
n
c
e
o
f
h
y
p
o
t
e
n
s
i
o
n
(
S
B
P
<
1
0
0
m
m
H
g
)
a
n
d
l
a
r
g
e
r
m
e
d
i
a
n
e
p
h
e
d
r
i
n
e
d
o
s
e
s
i
n
s
p
i
n
a
l
a
n
e
s
t
h
e
s
i
a
g
r
o
u
p
(
5
1
%
v
s
2
3
%
,
P
<
0
.
0
0
1
;
e
p
h
e
d
r
i
n
e
6
m
g
[
r
a
n
g
e
:
0
4
2
m
g
]
v
s
1
2
m
g
[
r
a
n
g
e
:
0
6
0
m
g
]
P
=
0
.
0
2
5
)
I
n
b
o
t
h
g
r
o
u
p
s
,
t
h
e
m
e
d
i
a
n
d
u
r
a
t
i
o
n
o
f
h
y
p
o
t
e
n
s
i
o
n
(
S
B
P
<
1
0
0
m
m
H
g
)
w
a
s
1
m
i
n
N
o
p
a
t
i
e
n
t
h
a
d
S
B
P
8
0
m
m
H
g
f
o
r
>
1
m
i
n
S
h
a
r
w
o
o
d
-
S
m
i
t
h
e
t
a
l
.
,
1
7
p
r
o
s
p
e
c
t
i
v
e
r
a
n
d
o
m
i
z
e
d
S
p
i
n
a
l
(
n
=
1
1
)
;
e
p
i
d
u
r
a
l
(
n
=
1
0
)
H
y
p
e
r
b
a
r
i
c
0
.
5
%
b
u
p
i
v
a
c
a
i
n
e
1
4
m
g
L
i
d
o
c
a
i
n
e
8
0
m
g
,
t
h
e
n
b
u
p
i
v
a
c
a
i
n
e
(
u
p
t
o
8
0
m
g
)
t
o
a
c
h
i
e
v
e
T
5
l
e
v
e
l
)
f
e
n
t
a
n
y
l
7
5
g
2
5
0
m
L
c
r
y
s
t
a
l
l
o
i
d
F
o
r
S
B
P
<
7
0
%
o
f
b
a
s
e
l
i
n
e
,
o
r
n
a
u
s
e
a
,
v
o
m
i
t
i
n
g
,
o
r
d
i
z
z
i
n
e
s
s
:
e
p
h
e
d
r
i
n
e
6
m
g
e
v
e
r
y
2
m
i
n
S
i
m
i
l
a
r
i
n
c
i
d
e
n
c
e
o
f
h
y
p
o
t
e
n
s
i
o
n
a
n
d
m
e
a
n
e
p
h
e
d
r
i
n
e
d
o
s
e
i
n
g
r
o
u
p
s
r
e
c
e
i
v
i
n
g
e
p
i
d
u
r
a
l
a
n
d
s
p
i
n
a
l
a
n
e
s
t
h
e
t
i
c
s
N
o
n
e
m
e
r
g
e
n
t
d
e
l
i
v
e
r
i
e
s
o
n
l
y
;
n
o
P
-
v
a
l
u
e
s
r
e
p
o
r
t
e
d
;
i
n
f
e
r
i
o
r
a
n
a
l
g
e
s
i
a
i
n
t
h
e
e
p
i
d
u
r
a
l
g
r
o
u
p
D
a
t
a
a
r
e
p
r
e
s
e
n
t
e
d
a
s
m
e
d
i
a
n
[
r
a
n
g
e
]
o
r
i
n
c
i
d
e
n
c
e
(
%
)
.
S
B
P
=
s
y
s
t
o
l
i
c
b
l
o
o
d
p
r
e
s
s
u
r
e
.
T
a
b
l
e
3
.
P
r
o
s
p
e
c
t
i
v
e
T
r
i
a
l
C
o
m
p
a
r
i
n
g
C
S
E
A
n
e
s
t
h
e
s
i
a
w
i
t
h
E
p
i
d
u
r
a
l
A
n
e
s
t
h
e
s
i
a
a
n
d
G
e
n
e
r
a
l
A
n
e
s
t
h
e
s
i
a
A
m
o
n
g
S
e
v
e
r
e
l
y
P
r
e
e
c
l
a
m
p
t
i
c
P
a
r
t
u
r
i
e
n
t
s
A
u
t
h
o
r
,
s
t
u
d
y
t
y
p
e
S
a
m
p
l
e
s
i
z
e
C
S
E
d
o
s
e
E
p
i
d
u
r
a
l
/
G
A
d
o
s
e
s
P
r
e
h
y
d
r
a
t
i
o
n
E
p
h
e
d
r
i
n
e
d
o
s
i
n
g
P
e
r
t
i
n
e
n
t
c
o
n
c
l
u
s
i
o
n
s
I
m
p
o
r
t
a
n
t
c
h
a
r
a
c
t
e
r
i
s
t
i
c
s
W
a
l
l
a
c
e
e
t
a
l
.
,
9
p
r
o
s
p
e
c
t
i
v
e
r
a
n
d
o
m
i
z
e
d
C
S
E
(
n
=
2
7
)
;
e
p
i
d
u
r
a
l
(
n
=
2
7
)
;
g
e
n
e
r
a
l
(
n
=
2
6
)
H
y
p
e
r
b
a
r
i
c
b
u
p
i
v
a
c
a
i
n
e
1
1
m
g
,
e
p
i
d
u
r
a
l
b
u
p
i
v
a
c
a
i
n
e
(
1
5
m
g
d
o
s
e
s
)
a
s
n
e
e
d
e
d
E
p
i
d
u
r
a
l
:
l
i
d
o
c
a
i
n
e
2
%
o
r
c
h
l
o
r
o
p
r
o
c
a
i
n
e
3
%
(
1
8
2
3
m
L
)
,
T
4
l
e
v
e
l
;
G
A
:
p
e
n
t
o
t
h
a
l
4
5
m
g
/
k
g
,
l
i
d
o
c
a
i
n
e
1
.
5
m
g
/
k
g
,
s
u
c
c
i
n
y
l
c
h
o
l
i
n
e
1
.
5
m
g
/
k
g
,
e
n
d
-
t
i
d
a
l
i
s
o
f
u
r
a
n
e
(
0
.
7
5
%
)
,
n
i
t
r
o
u
s
o
x
i
d
e
(
5
0
%
)
G
A
g
r
o
u
p
:
4
0
0
8
0
m
L
;
C
S
E
:
9
9
0
6
0
m
L
;
e
p
i
d
u
r
a
l
:
1
0
2
0
6
0
m
L
F
o
r
S
B
P
<
1
0
0
m
m
H
g
:
e
p
h
e
d
r
i
n
e
5
m
g
a
n
d
/
o
r
c
r
y
s
t
a
l
l
o
i
d
E
p
h
e
d
r
i
n
e
g
i
v
e
n
t
o
2
2
%
p
a
t
i
e
n
t
s
i
n
C
S
E
g
r
o
u
p
,
3
0
%
i
n
e
p
i
d
u
r
a
l
g
r
o
u
p
,
a
n
d
n
o
p
a
t
i
e
n
t
s
i
n
G
A
g
r
o
u
p
(
s
i
g
n
i
f
c
a
n
t
d
i
f
f
e
r
e
n
c
e
P
=
0
.
0
0
9
)
C
S
E
:
i
n
t
r
a
t
h
e
c
a
l
d
o
s
e
s
c
o
m
p
a
r
a
b
l
e
w
i
t
h
s
p
i
n
a
l
d
o
s
e
s
i
n
o
t
h
e
r
s
t
u
d
i
e
s
c
o
m
p
a
r
i
n
g
s
p
i
n
a
l
w
i
t
h
e
p
i
d
u
r
a
l
a
n
e
s
t
h
e
s
i
a
.
E
p
h
e
d
r
i
n
e
d
o
s
e
s
n
o
t
r
e
p
o
r
t
e
d
D
a
t
a
a
r
e
p
r
e
s
e
n
t
e
d
a
s
m
e
a
n
S
D
o
r
i
n
c
i
d
e
n
c
e
(
%
)
.
C
S
E
=
c
o
m
b
i
n
e
d
s
p
i
n
a
l
e
p
i
d
u
r
a
l
;
G
A
=
g
e
n
e
r
a
l
a
n
e
s
t
h
e
s
i
a
;
S
B
P
=
s
y
s
t
o
l
i
c
b
l
o
o
d
p
r
e
s
s
u
r
e
.
Spinal Anesthesia in Severe Preeclampsia
September 2013
Volume 117
Number 3 www.anesthesia-analgesia.org 689
College of Obstetricians and Gynecologists (ACOG),
4
neur-
axial anesthetic techniques, when feasible, are strongly pre-
ferred to general anesthesia for preeclamptic parturients.
Early epidural catheter placement in laboring preeclamptic
parturients is encouraged, since it secures a means of deliv-
ering neuraxial anesthesia (avoiding the risks of general
anesthesia) in the event that an emergency cesarean delivery
is required. Additional benefts of epidural labor analgesia
are reduced oxygen consumption and minute ventilation
during the frst and second stages of labor
21
and, in pre-
eclamptic parturients, improved intervillous blood fow
22
(provided that hypotension is avoided) and decreased
maternal plasma catecholamines.
23
Consequently, for com-
plicated cases such as parturients with preeclampsia, the
ASA practice guideline recommends early epidural or spi-
nal catheter placement, which may even precede onset of
labor or the patients request for analgesia.
20
In preeclampsia, spinal anesthesia is generally consid-
ered for cesarean delivery when there is no indwelling
epidural catheter or there is a contraindication to neuraxial
anesthesia (e.g., coagulopathy, eclampsia with persistent
neurologic defcits). Spinal anesthesia affords quicker onset
of anesthesia than epidural or CSE anesthesia, which is a
critical advantage in emergency situations. In the setting
of severe hemodynamic instability or if a particularly long
operative time is anticipated, an alternative titratable neur-
axial technique such as epidural, CSE, or continuous spinal
anesthesia should be considered.
SPINAL VERSUS GENERAL ANESTHESIA
For most of the severely preeclamptic population, the risk
beneft profles of spinal anesthesia and general anesthesia
strongly favor the use of spinal anesthesia when feasible.
Important factors to consider are the risks of clinically sig-
nifcant maternal hemodynamic derangements, diffcult air-
way management, stroke, spinal/epidural hematoma, and
adverse neonatal outcomes. As described earlier, in severely
preeclamptic patients, spinal anesthesiainduced hypoten-
sion is typically easily treated, the risk of spinal/epidural
hematoma is low, and there is no evidence that neonatal
outcomes are compromised. In contrast, potential compli-
cations of general anesthesia, such as hypertensive crisis,
stroke, and diffcult airway management, are leading causes
of morbidity and mortality in the preeclamptic population.
Therefore, in the majority of severely preeclamptic patients,
who are not coagulopathic or thrombocytopenic, the risk of
diffcult or failed airway management and delayed recogni-
tion of maternal stroke during a general anesthetic are felt to
exceed the risk of adverse outcomes from spinal anesthesia
induced hypotension or spinal/epidural hematoma.
19
Peripartum pharyngeal and glottic edema are accen-
tuated in preeclamptic parturients,
24
and the risks of dif-
fcult/failed laryngoscopy and intubation are greater
among preeclamptic parturients than healthy parturients.
25
Traumatic laryngoscopy may trigger pharyngeal or hypo-
pharyngeal bleeding, further obscuring visualization of the
airway. Although the absolute risks of general anesthesia
(failed/diffcult airway management, hypertension with
direct laryngoscopy, delayed recognition of stroke under
general anesthesia, and aspiration) are low even among
preeclamptic parturients, the risk of diffcult airway man-
agement is a compelling reason to favor neuraxial anesthe-
sia. Closed claims analysis from the United Kingdom from
2006 to 2008 identifed poor management of preeclampsia
as one of the main categories in which poor perioperative
management may have contributed to maternal death.
26
Severe preeclampsia is also a leading cause of peripar-
tum hemorrhagic stroke.
27
During direct laryngoscopy and
intubation, severely preeclamptic parturients experience
signifcantly larger increases in arterial blood pressure and
middle cerebral artery velocity compared with healthy par-
turients.
28
Cerebral hypertension may, in turn, precipitate
hemorrhagic stroke. Hemorrhagic stroke was the leading
direct cause of mortality in patients with severe preeclamp-
sia according to the most recent analysis by the United
Kingdom Center for Maternal and Child Enquiries.
29
If gen-
eral anesthesia is necessary, equipment should be immedi-
ately available to manage a diffcult airway, and every effort
should be made to blunt the hemodynamic response to
laryngoscopy (e.g., via a bolus of an antihypertensive drug
or remifentanil).
30,31
One study has been designed to detect differences in
maternal or neonatal outcomes associated with the use
of spinal anesthesia compared with general anesthesia
in severe preeclampsia. Dyer et al.
32
prospectively com-
pared umbilical arterial fetal base defcit and other mark-
ers of maternal and neonatal well-being in 70 preeclamptic
patients undergoing cesarean delivery due to nonreassuring
fetal heart rate tracings, randomized to receive either spinal
or general anesthesia (Table4). The study was powered to
detect an intergroup difference in the primary outcome,
the incidence of umbilical arterial base defcit >8 mEq/L.
In both groups, mean umbilical arterial base defcit values
were within the range considered normal for vaginal deliv-
ery (<10), although the spinal group had a higher mean
umbilical arterial base defcit (7.1 vs 4.7 mEq/L, P = 0.02)
and a lower median umbilical arterial pH (7.20 vs 7.23, P =
0.046). There were no signifcant intergroup differences in
other markers of neonatal compromise, including require-
ment for neonatal resuscitation, Apgar score <7, umbilical
arterial pH <7.2, and need for neonatal intermittent positive
pressure ventilation. Maternal heart rate and arterial blood
pressure values were also acceptable in both groups.
Notably, in the Dyer et al.
32
study, the mean ephedrine
dose (14 vs 3 mg, P = 0.002) was signifcantly higher in the
spinal anesthesia group. The authors point out that there
was no correlation between ephedrine use and neona-
tal base defcit in either group. Of note, post hoc analysis
showed that unless diastolic blood pressure exceeded 110
mm Hg, there was no intergroup difference in neonatal base
defcit. However, the clinical signifcance of this observa-
tion remains unknown, especially since the study was not
powered to assess this subset of patients. The trend toward
lower umbilical arterial pH in the spinal group, in which
ephedrine doses were higher, has prompted some authors
33
to recommend phenylephrine as the frst-line vasopressor
in severe preeclampsia. This recommendation is consistent
with the fnding that, in some studies, ephedrine is associ-
ated with greater fetal acidemia than phenylephrine among
healthy parturients presenting for cesarean delivery.
33
690 www.anesthesia-analgesia.org ANESTHESIA & ANALGESIA
E FOCUSED REVIEW
STRATEGIES TO REDUCE NEURAXIAL
ANESTHESIAINDUCED HYPOTENSION
In preeclamptic women, a prophylactic crystalloid bolus
before spinal anesthesia increases central venous pressure
for <2 minutes.
10
Preeclamptic parturients are at increased
risk of pulmonary edema due to increased capillary per-
meability, decreased colloid oncotic pressure, increased
hydrostatic pressure, and, in some cases, left ventricular
dysfunction. Given the transient impact of IV fuid boluses
on central venous pressure and the increased susceptibil-
ity of preeclamptic parturients to pulmonary edema, trials
involving severely preeclamptic parturients have used judi-
cious crystalloid doses (Table2). This practice is consistent
with the shift toward less perioperative crystalloid adminis-
tration to healthy parturients,
34
which refects evidence that
fuid boluses, by themselves, do not prevent hypotension.
No studies have specifcally addressed fuid management
for spinal anesthesia in preeclampsia. Prophylactic phenyl-
ephrine infusions have not been studied in the setting of
uteroplacental insuffciency, and there is insuffcient evi-
dence to suggest their evidence-based use in the preeclamp-
tic population.
One strategy to minimize hemodynamic disruption
(in cases of signifcant fetal compromise, with reversal of
umbilical artery end-diastolic fow) is CSE anesthesia using
a small intrathecal local anesthetic dose.
35
The incidence of
spinal anesthesiainduced hypotension is local anesthetic
dose dependent, thus CSE compared with single-shot spi-
nal anesthesia has been shown to be associated with a lower
risk of hypotension.
36
However, no studies have compared
CSE with spinal anesthesia in severe preeclampsia.
HEMODYNAMIC MONITORING DURING SPINAL
ANESTHESIA IN SEVERE PREECLAMPSIA
The spectrum of hemodynamic profles observed in severe
preeclampsia refects disease severity,
37
whether hyper-
tension has been treated
38,39
and varied approaches to
antihypertensive therapy and comorbidities. Among non-
laboring, term preeclamptic parturients, the incidence of
global diastolic dysfunction, typically mild, is 40%.
40
The
ASA practice guidelines for obstetric anesthesia state that
the literature is silent or insuffcient to determine whether
invasive hemodynamic monitoring improves outcomes in
women with pregnancy-related hypertensive disorders.
No specifc monitor has been proven to impact maternal or
fetal outcomes in the setting of preeclampsia.
20
An arterial
catheter can facilitate detection and treatment of blood pres-
sure changes, especially in patients with severe or volatile
hypertension. Echocardiography can provide information
about volume status and cardiac function. In preeclamp-
sia, central venous pressure often does not correlate with
pulmonary capillary wedge pressure,
41
which in turn may
not refect left ventricular stroke work.
39
Also, pulmonary
artery and central venous catheters confer a reported 4%
risk of complications among hypertensive parturients.
42
Proponents of less invasive monitors that estimate stroke
volume, such as arterial waveform analysis
43
and imped-
ance cardiography, highlight the favorable riskbeneft
ratio and the correlation of these data (in the early postpar-
tum period among severely preeclamptic patients)
44
with
thermodilution-derived measurements. Further evaluation T
a
b
l
e
4
.
P
r
o
s
p
e
c
t
i
v
e
T
r
i
a
l
C
o
m
p
a
r
i
n
g
S
p
i
n
a
l
A
n
e
s
t
h
e
s
i
a
w
i
t
h
G
e
n
e
r
a
l
A
n
e
s
t
h
e
s
i
a
A
m
o
n
g
P
a
r
t
u
r
i
e
n
t
s
w
i
t
h
P
r
e
e
c
l
a
m
p
s
i
a
U
n
d
e
r
g
o
i
n
g
E
m
e
r
g
e
n
t
C
e
s
a
r
e
a
n
D
e
l
i
v
e
r
y
d
u
e
t
o
N
o
n
r
e
a
s
s
u
r
i
n
g
F
e
t
a
l
H
e
a
r
t
R
a
t
e
A
u
t
h
o
r
,
s
t
u
d
y
t
y
p
e
S
a
m
p
l
e
s
i
z
e
S
p
i
n
a
l
d
o
s
e
G
e
n
e
r
a
l
a
n
e
s
t
h
e
s
i
a
d
o
s
e
P
r
e
h
y
d
r
a
t
i
o
n
E
p
h
e
d
r
i
n
e
d
o
s
i
n
g
C
o
n
c
l
u
s
i
o
n
s
I
m
p
o
r
t
a
n
t
c
h
a
r
a
c
t
e
r
i
s
t
i
c
s
D
y
e
r
e
t
a
l
.
,
3
2
p
r
o
s
p
e
c
t
i
v
e
r
a
n
d
o
m
i
z
e
d
S
p
i
n
a
l
(
n
=
3
5
)
v
e
r
s
u
s
g
e
n
e
r
a
l
(
n
=
3
5
)
H
y
p
e
r
b
a
r
i
c
b
u
p
i
v
a
c
a
i
n
e
9
m
g
+
f
e
n
t
a
n
y
l
1
0
g
T
h
i
o
p
e
n
t
o
n
e
5
m
g
/
k
g
,
s
u
x
a
m
e
t
h
o
n
i
u
m
1
.
5
m
g
/
k
g
,
m
a
g
n
e
s
i
u
m
s
u
l
f
a
t
e
3
0
4
5
m
g
/
k
g
;
e
n
d
-
t
i
d
a
l
i
s
o
f
u
r
a
n
e
(
0
.
7
5
1
.
5
)
,
n
i
t
r
o
u
s
o
x
i
d
e
(
5
0
%
)
;
a
f
t
e
r
d
e
l
i
v
e
r
y
:
m
o
r
p
h
i
n
e
0
.
0
5
0
.
1
0
m
g
/
k
g
<
7
5
0
m
L
c
r
y
s
t
a
l
l
o
i
d
F
o
r
S
B
P
<
1
0
0
m
m
H
g
,
o
r
S
B
P
<
7
5
%
b
a
s
e
l
i
n
e
:
e
p
h
e
d
r
i
n
e
5
m
g
e
v
e
r
y
m
i
n
u
t
e
,
u
n
t
i
l
S
B
P
2
5
%
o
f
b
a
s
e
l
i
n
e
S
p
i
n
a
l
a
n
e
s
t
h
e
s
i
a
g
r
o
u
p
:
l
o
w
e
r
m
e
d
i
a
n
u
m
b
i
l
i
c
a
l
a
r
t
e
r
y
p
H
(
7
.
2
0
[
r
a
n
g
e
:
6
.
9
3
7
.
3
4
]
v
s
7
.
2
3
[
r
a
n
g
e
:
7
.
0
5
7
.
4
]
,
P
=
0
.
0
4
6
)
a
n
d
l
a
r
g
e
r
m
e
a
n
u
m
b
i
l
i
c
a
l
a
r
t
e
r
y
b
a
s
e
d
e
f
c
i
t
(
7
.
1
4
.
0
v
s
4
.
7
3
.
3
m
E
q
/
L
,
P
=
0
.
0
2
)
S
p
i
n
a
l
a
n
e
s
t
h
e
s
i
a
g
r
o
u
p
r
e
c
e
i
v
e
d
m
o
r
e
e
p
h
e
d
r
i
n
e
(
1
4
1
8
v
s
3
9
m
g
,
P
=
0
.
0
0
2
)
D
a
t
a
a
r
e
p
r
e
s
e
n
t
e
d
a
s
m
e
a
n
S
D
,
m
e
d
i
a
n
[
r
a
n
g
e
]
,
o
r
a
s
a
p
e
r
c
e
n
t
a
g
e
.
S
B
P
=
s
y
s
t
o
l
i
c
b
l
o
o
d
p
r
e
s
s
u
r
e
.
Spinal Anesthesia in Severe Preeclampsia
September 2013
Volume 117
Number 3 www.anesthesia-analgesia.org 691
of these monitors in the peripartum management of severe
preeclampsia is ongoing.
45,46
COAGULOPATHY
In preeclampsia, endothelial dysfunction can stimulate exces-
sive platelet activation and consumption, which may con-
tribute to the increased incidence of thrombocytopenia. The
incidence of spinalepidural hematoma among preeclamp-
tic patients undergoing neuraxial procedures is unknown.
Large survey studies have found that the incidence of spi-
nalepidural hematoma after neuraxial anesthesia is lower
among parturients than the general population.
4749
These
studies have also shown that whether
47
or not
47,49
analysis is
limited to parturients, spinalepidural hematoma is less com-
mon after spinal anesthesia than CSE or epidural anesthe-
sia. However, retrospective studies may underestimate the
incidence of spinalepidural hematoma and/or the number
of neuraxial techniques performed. Evidence suggests that
the incidence of spinalepidural hematoma has increased
since the 1990s.
50
In large retrospective reviews
47,48
and case
reports,
50
laboratory evidence of deranged hemostasis was
found in a large proportion of pregnant and nonpregnant
patients who developed spinalepidural hematomas after
neuraxial procedures. In 1 large retrospective study,
47
the
only 2 cases of obstetric spinalepidural hematoma occurred
in patients with the syndrome of hemolysis, elevated liver
enzymes, and low platelets. Spinal anesthesia may confer a
lower risk of spinal/epidural hematoma than CSE or epi-
dural anesthesia, since smaller caliber needles are associated
with a lower incidence of spinal hematoma
51
and single-shot
spinal anesthesia avoids the risks of an indwelling catheter.
While there is no defnitive data for a safe platelet
count, based on a consensus statement from the American
Society of Regional Anesthesia
50
and case series data,
52
expert
opinions from the hematology literature
53
and from the
American Society of Hematologists pertaining to immune
thrombocytopenia,
54
many anesthesiologists require a plate-
let count of at least 75,000 or 80,000/L (and, if the platelet
count is <150,000/L, normal partial thromboplastin [PTT]
and prothrombin [PT] times) before initiating spinal anes-
thesia in patients with severe preeclampsia.
55
The ASA prac-
tice guidelines advise that the use of a platelet count may
reduce the risk of anesthesia-related complications in pre-
eclampsia.
20
In a prospective study by Leduc et al.
56
involving
100 women with severe preeclampsia or chronic hyperten-
sion with preeclampsia (26 of whom developed hemolysis,
elevated liver enzymes, and low platelets syndrome), no
parturient had an elevated PT or PTT or a low fbrinogen
level in the absence of a platelet count <150,000/L. Of the
patients whose initial platelet count was <150,000/L, 75%
went on to develop a platelet count <100,000/L. On the
basis of these fndings, the authors recommended following
serial platelet counts for intrapartum preeclamptic parturi-
ents and checking PT, PTT, and fbrinogen levels only if the
platelet count decreases below 100,000/L. While the Leduc
et al.
56
study monitored hemostasis labs every 6 hours, for
patients with clinical signs of worsening coagulopathy, a
more recent assessment of platelet count and coagulation
indices should be considered. Clinical judgment is critical in
selecting the anesthetic approach for a preeclamptic patient
with a marginal platelet count or coagulation profle.
AREAS FOR FURTHER RESEARCH
Further research is needed to elucidate strategies to opti-
mize hemodynamics and uteroplacental perfusion among
severely preeclamptic parturients during spinal anesthesia
for cesarean delivery. Specifc areas of interest include the
effect of prophylactic phenylephrine infusions on neona-
tal outcomes, optimal strategies for fuid management for
severely preeclamptic parturients during spinal anesthesia,
and the role of minimally invasive cardiac output monitors
in tailoring hemodynamic therapy.
E
DISCLOSURES
Name: Vanessa G. Henke, MD.
Contribution: This author helped design and conduct the
study, analyze the data, and write the manuscript.
Attestation: Vanessa G. Henke approved the fnal manuscript.
Name: Brian T. Bateman, MD.
Contribution: This author helped design the study and write
the manuscript.
Attestation: Brian T. Bateman approved the fnal manuscript.
Name: Lisa R. Leffert, MD.
Contribution: This author helped design and conduct the
study and write the manuscript.
Attestation: Lisa R. Leffert approved the fnal manuscript.
This manuscript was handled by: Cynthia A. Wong, MD.
REFERENCES
1. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-
eclampsia. Lancet 2010;376:63144
2. Heron MP, Hoyert DL, Murphy SL, Xu J. Deaths: fnal data for
2006. National Vital Statistics Reports; vol 57, No 14. Available
at: http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.
pdf. Accessed December 11, 2010
3. Gogarten W. Preeclampsia and anaesthesia. Curr Opin
Anaesthesiol 2009;22:34751
4. Diagnosis and management of preeclampsia and eclamp-
sia. ACOG Practice Bulletin No. 33. American College of
Obstetricians and Gynecologists. Obstet Gynecol 2002;99:15967
5. Lindheimer MD, Taler SJ, Cunningham FG. Hypertension in
pregnancy. J Am Soc Hypertens 2008;2:48494
6. Pritchard JA, Cunningham FG, Pritchard SA. The Parkland
Memorial Hospital protocol for treatment of eclampsia: evalua-
tion of 245 cases. Am J Obstet Gynecol 1984;148:95163
7. Assali NS, Prystowsky H. Studies on autonomic blockade.
I. Comparison between the effects of tetraethylammonium
chloride (TEAC) and high selective spinal anesthesia on blood
pressure of normal and toxemic pregnancy. J Clin Invest
1950;29:135466
8. Jones GR, Ware HH, Garber EC, McElrath PJ. Continuous
spinal anesthesia in the treatment of severe preeclampsia and
eclampsia. Southern Med J 1952;45:3441
9. Wallace DH, Leveno KJ, Cunningham FG, Giesecke AH,
Shearer VE, Sidawi JE. Randomized comparison of general and
regional anesthesia for cesarean delivery in pregnancies com-
plicated by severe preeclampsia. Obstet Gynecol 1995;86:1939
10. Karinen J, Rasanen J, Alahuhta S, Jouppila R, Jouppila P.
Maternal and uteroplacental haemodynamic state in pre-
eclamptic patients during spinal anesthesia for cesarean sec-
tion. Br J Anasth 1996;76:61620
11. Hood DD, Curry R. Spinal versus epidural anesthesia for cesar-
ean section in severely preeclamptic patients: a retrospective
survey. Anesthesiology 1999;90:127682
12. Brizgys RV, Dailey PA, Shnider SM, Kotelko DM, Levinson G.
The incidence and neonatal effects of maternal hypotension
during epidural anesthesia for cesarean section. Anesthesiology
1987;67:7826
13. Aya AG, Vialles N, Tanoubi I, Mangin R, Ferrer JM, Robert
C, Ripart J, de La Coussaye JE. Spinal anesthesia-induced
hypotension: a risk comparison between patients with severe
692 www.anesthesia-analgesia.org ANESTHESIA & ANALGESIA
E FOCUSED REVIEW
preeclampsia and healthy women undergoing preterm cesar-
ean delivery. Anesth Analg 2005;101:86975
14. Aya AG, Mangin R, Vialles N, Ferrer JM, Robert C, Ripart J, de
La Coussaye JE. Patients with severe preeclampsia experience
less hypotension during spinal anesthesia for elective cesarean
delivery than healthy parturients: a prospective cohort com-
parison. Anesth Analg 2003;97:86772
15. Clark VA, Sharwood-Smith GH, Stewart AV. Ephedrine require-
ments are reduced during spinal anaesthesia for caesarean sec-
tion in preeclampsia. Int J Obstet Anesth 2005;14:913
16. Visalyaputra S, Rodanant O, Somboonviboon W, Tantivitayatan
K, Thienthong S, Saengchote W. Spinal versus epidural anesthe-
sia for cesarean delivery in severe preeclampsia: a prospective
randomized, multicenter study. Anesth Analg 2005;101:8628
17. Sharwood-Smith G, Clark V, Watson E. Regional anesthesia for
cesarean section in severe preeclampsia: spinal anesthesia is the
preferred choice. Int J Obstet Anesth 1999;8:859
18. Chiu CL, Mansor M, Ng KP, Chan YK. Retrospective review
of spinal versus epidural anaesthesia for caesarean section in
preeclamptic patients. Int J Obstet Anesth 2003;12:237
19. Santos AC, Birnbach DJ. Spinal anesthesia for cesarean delivery
in severely preeclamptic women: dont throw out the baby with
the bathwater! Anesth Analg 2005;101:85961
20. American Society of Anesthesiologists Task Force on Obstetric
Anesthesia. Practice guidelines for obstetric anesthesia: an
updated report by the American Society of Anesthesiologists
Task Force on Obstetric Anesthesia. Anesthesiology 2007;
106:84363
21. Hgerdal M, Morgan CW, Sumner AE, Gutsche BB. Minute
ventilation and oxygen consumption during labor with epi-
dural analgesia. Anesthesiology 1983;59:4257
22. Jouppila P, Jouppila R, Hollmn A, Koivula A. Lumbar epidural
analgesia to improve intervillous blood fow during labor in
severe preeclampsia. Obstet Gynecol 1982;59:15861
23. Abboud T, Artal R, Sarkis F, Henriksen EH, Kammula RK.
Sympathoadrenal activity, maternal, fetal, and neonatal
responses after epidural anesthesia in the preeclamptic patient.
Am J Obstet Gynecol 1982;144:9158
24. Izci B, Riha RL, Martin SE, Vennelle M, Liston WA, Dundas KC,
Calder AA, Douglas NJ. The upper airway in pregnancy and
pre-eclampsia. Am J Respir Crit Care Med 2003;167:13740
25. Munnur U, de Boisblanc B, Suresh MS. Airway problems in
pregnancy. Crit Care Med 2005;33:S25968
26. McClure J, Cooper G; on behalf of the Centre for Maternal
and Child Enquiries. Chapter 8: Anaesthesia. In: Lewis G,
ed. Saving Mothers Lives: Reviewing Maternal Deaths to
Make Motherhood Safer: 20062008. The Eighth Report of the
Confdential Enquiries into Maternal Deaths in the United
Kingdom. Br J Obstet Gynecol 2011;118 (Suppl 1):1203
27. Bateman BT, Schumacher HC, Bushnell CD, Pile-Spellman J,
Simpson LL, Sacco RL, Berman MF. Intracerebral hemorrhage
in pregnancy: frequency, risk factors, and outcome. Neurology
2006;67:4249
28. Ramanathan J, Angel JJ, Bush AJ, Lawson P, Sibai B. Changes in
maternal middle cerebral artery blood fow velocity associated
with general anesthesia in severe preeclampsia. Anesth Analg
1999;88:35761
29. Neilson J; on behalf of the Centre for Maternal and Child
Enquiries. Chapter 3: Pre-eclampsia and eclampsia. In: Lewis
G, ed. Saving Mothers Lives: Reviewing maternal deaths to
make motherhood safer: 20062008. The Eighth Report of the
Confdential Enquiries into Maternal Deaths in the United
Kingdom. Br J Obstet Gynecol 2011;118 (Suppl 1):1203
30. Park BY, Jeong CW, Jang EA, Kim SJ, Jeong ST, Shin MH, Lee J,
Yoo KY. Dose-related attenuation of cardiovascular responses
to tracheal intubation by intravenous remifentanil bolus in
severe pre-eclamptic patients undergoing Caesarean delivery.
Br J Anaesth 2011;106:827
31. Yoo KY, Jeong CW, Park BY, Kim SJ, Jeong ST, Shin MH, Lee J.
Effects of remifentanil on cardiovascular and bispectral index
responses to endotracheal intubation in severe pre-eclamptic
patients undergoing caesarean delivery under general anesthe-
sia. Br J Anesth 2009;102:8129
32. Dyer RA, Els I, Farbas J, Torr GJ, Schoeman LK, James MF.
Prospective, randomized trial comparing general with spinal
anesthesia for cesarean delivery in preeclamptic patients with a
nonreassuring fetal heart trace. Anesthesiology 2003;99:5619
33. Smiley RM. Burden of proof. Anesthesiology 2009;111:4702
34. Habib AS. A review of the impact of phenylephrine adminis-
tration on maternal hemodynamics and maternal and neonatal
outcomes in women undergoing cesarean delivery under spi-
nal anesthesia. Anesth Analg 2012;114:37790
35. Ramanathan J, Vaddadi AK, Arheart KL. Combined spinal and
epidural anesthesia with low doses of intrathecal bupivacaine
in women with severe preeclampsia: a preliminary report. Reg
Anesth Pain Med 2001;26:4651
36. Rawal N, Schollin J, Wesstrm G. Epidural versus combined
spinal epidural block for cesarean section. Acta Anaesthesiol
Scand 1988;32:616
37. Bosio PM, McKenna PJ, Conroy R, OHerlihy C. Maternal cen-
tral hemodynamics in hypertensive disorders of pregnancy.
Obstet Gynecol 1999;94:97884
38. Groenendijk R, Trimbos JB, Wallenburg HC. Hemodynamic
measurements in preeclampsia: preliminary observations. Am
J Obstet Gynecol 1984;150:2326
39. Visser W, Wallenburg HC. Central hemodynamic obser-
vations in untreated preeclamptic patients. Hypertension
1991;17:10727
40. Melchiorre K, Sutherland GR, Baltabaeva A, Liberati M,
Thilaganathan B. Maternal cardiac dysfunction and remod-
eling in women with preeclampsia at term. Hypertension
2011;57:8593
41. Bolte AC, Dekker GA, van Eyck J, van Schijndel RS, van Geijn
HP. Lack of agreement between central venous pressure
and pulmonary capillary wedge pressure in preeclampsia.
Hypertens Pregnancy 2000;19:26171
42. Young P, Johanson R. Haemodynamic, invasive and echocar-
diographic monitoring in the hypertensive parturient. Best
Pract Res Clin Obstet Gynaecol 2001;15:60522
43. Montenij LJ, de Waal EE, Buhre WF. Arterial waveform anal-
ysis in anesthesia and critical care. Curr Opin Anaesthesiol
2011;24:6516
44. Dyer RA, Piercy JL, Reed AR, Strathie GW, Lombard CJ,
Anthony JA, James MF. Comparison between pulse waveform
analysis and thermodilution cardiac output determination in
patients with severe pre-eclampsia. Br J Anaesth 2011;106:7781
45. Pauca AL. Pressure wave analysis is useful to understand
the pathophysiology of preeclampsia, but perhaps not the
rapid changes during cesarean delivery. Anesthesiology
2008;108:7734
46. Dyer RA, Piercy JL, Reed AR. The role of the anaesthetist in
the management of the pre-eclamptic patient. Curr Opin
Anaesthesiol 2007;20:16874
47. Moen V, Dahlgren N, Irestedt L. Severe neurological compli-
cations after central neuraxial blockades in Sweden 1990-1999.
Anesthesiology 2004;101:9509
48. Bateman BT, Mhyre JM, Ehrenfeld J, Kheterpal S, Abbey KR,
Argalious M, Berman MF, Jacques PS, Levy W, Loeb RG,
Paganelli W, Smith KW, Wethington KL, Wax D, Pace NL,
Tremper K, Sandberg WS. Brief report: the risk and outcomes
of epidural hematomas after perioperative and obstetric epi-
dural catheterization: a report from the multicenter periop-
erative outcomes group research consortium. Anesth Analg
2013;116:13805
49. Cook TM, Counsell D, Wildsmith JA; Royal College of
Anaesthetists Third National Audit Project. Major complica-
tions of central neuraxial block: report on the Third National
Audit Project of the Royal College of Anaesthetists. Br J Anaesth
2009;102:17990
50. Horlocker TT, Wedel DJ, Rowlingson JC, Enneking FK, Kopp
SL, Benzon HT, Brown DL, Heit JA, Mulroy MF, Rosenquist
RW, Tryba M, Yuan CS. Regional anesthesia in the patient
receiving antithrombotic or thrombolytic therapy: American
Society of Regional Anesthesia and Pain Medicine Evidence-
Based Guidelines (Third Edition). Reg Anesth Pain Med
2010;35:64101
Spinal Anesthesia in Severe Preeclampsia
September 2013
Volume 117
Number 3 www.anesthesia-analgesia.org 693
51. Horlocker TT, Wedel DJ, Schroeder DR, Rose SH, Elliott BA,
McGregor DG, Wong GY. Preoperative antiplatelet therapy
does not increase the risk of spinal hematoma associated with
regional anesthesia. Anesth Analg 1995;80:3039
52. Douglas MJ. Platelets, the parturient and regional anesthesia.
Int J Obstet Anesth 2001;10:11320
53. van Veen JJ, Nokes TJ, Makris M. The risk of spinal haematoma
following neuraxial anaesthesia or lumbar puncture in throm-
bocytopenic individuals. Br J Haematol 2010;148:1525
54. Neunert C, Lim W, Crowther M, Cohen A, Solberg L Jr,
Crowther MA; American Society of Hematology. The American
Society of Hematology 2011 evidence-based practice guideline
for immune thrombocytopenia. Blood 2011;117:4190207
55. Douglas MJ. Platelets, the parturient and regional anesthesia.
Int J Obstet Anesth 2001;10:113120
56. Leduc L, Wheeler JM, Kirshon B, Mitchell P, Cotton DB.
Coagulation profle in severe preeclampsia. Obstet Gynecol
1992;79:148
También podría gustarte
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Automation in Pharmacy PDFDocumento39 páginasAutomation in Pharmacy PDFanthonyAún no hay calificaciones
- SMART Asthma TherapyDocumento4 páginasSMART Asthma TherapyKen Won100% (1)
- Issues in CPPD Nomenclature and ClassificationDocumento8 páginasIssues in CPPD Nomenclature and ClassificationMonika Diaz KristyanindaAún no hay calificaciones
- 4th Year MBBS Batches & GroupsDocumento2 páginas4th Year MBBS Batches & GroupsSohail Abbas KhanAún no hay calificaciones
- Lab 7 HIV Detection Using ELISADocumento24 páginasLab 7 HIV Detection Using ELISAAhmed AbedoAún no hay calificaciones
- Guatemala HandoutDocumento2 páginasGuatemala Handoutapi-308909264Aún no hay calificaciones
- 2231 - AMedP-5.1 EDA V1 EDocumento52 páginas2231 - AMedP-5.1 EDA V1 EDaniel CharlesAún no hay calificaciones
- Surgery KGMU Proff Chapterwise by Arif Naseem 2009-2021Documento4 páginasSurgery KGMU Proff Chapterwise by Arif Naseem 2009-2021DR. PARDEEP SHARMAAún no hay calificaciones
- Discharge PlanDocumento2 páginasDischarge Plan2G Balatayo Joshua LeoAún no hay calificaciones
- 2Documento6 páginas2muiAún no hay calificaciones
- Acute Pancriatis Special HDocumento9 páginasAcute Pancriatis Special HInga CeagleiAún no hay calificaciones
- Hearing Loss in Adults Assessment and Management PDF 1837761878725 PDFDocumento20 páginasHearing Loss in Adults Assessment and Management PDF 1837761878725 PDFxtineAún no hay calificaciones
- October 2023 PRC PLE Schedule and Reminders 2Documento4 páginasOctober 2023 PRC PLE Schedule and Reminders 2TrisAún no hay calificaciones
- Reva Rubin Dan Ramona MercerDocumento8 páginasReva Rubin Dan Ramona MercerFifi FruitasariAún no hay calificaciones
- Luka Bakar: Nama: Melvin Andrean NIM: 112018161 Pembimbing: Kpt. Dr. Anwar Lewa, SP - BP-RE, M.BiomedDocumento47 páginasLuka Bakar: Nama: Melvin Andrean NIM: 112018161 Pembimbing: Kpt. Dr. Anwar Lewa, SP - BP-RE, M.BiomedIpd CengkarengAún no hay calificaciones
- Interview Paper SW 3010Documento7 páginasInterview Paper SW 3010api-319252753Aún no hay calificaciones
- What Is Subinvolution?Documento5 páginasWhat Is Subinvolution?Xierl BarreraAún no hay calificaciones
- Q2 Lesson 7Documento25 páginasQ2 Lesson 7mint hvryAún no hay calificaciones
- Full Psych DB InterviewDocumento30 páginasFull Psych DB InterviewAdam GAún no hay calificaciones
- Features of CHN: Learning ObjectivesDocumento6 páginasFeatures of CHN: Learning ObjectivesAkeroAún no hay calificaciones
- MLP Registration FormDocumento6 páginasMLP Registration FormDoll JonesAún no hay calificaciones
- Iep Forms EngDocumento23 páginasIep Forms EngElsa PimentelAún no hay calificaciones
- Kriyakala AvastaDocumento13 páginasKriyakala Avastakundagol100% (1)
- Power of Plants 1Documento14 páginasPower of Plants 1api-399048965Aún no hay calificaciones
- Difhtheria in ChildrenDocumento9 páginasDifhtheria in ChildrenFahmi IdrisAún no hay calificaciones
- BABY BLUES PresentationDocumento8 páginasBABY BLUES PresentationcipisedAún no hay calificaciones
- Letter of Support Template - 0 PDFDocumento2 páginasLetter of Support Template - 0 PDFselamitspAún no hay calificaciones
- Sarcopenia, European Definition and DiagnosisDocumento12 páginasSarcopenia, European Definition and DiagnosisRémi DelauzunAún no hay calificaciones
- Determinan Gejala Mental Emosional Pelajar SMP-SMA Di Indonesia Tahun 2015Documento11 páginasDeterminan Gejala Mental Emosional Pelajar SMP-SMA Di Indonesia Tahun 2015NurLestariAún no hay calificaciones
- Jan 5, 2021 TDIR Worksheet (COG 2)Documento122 páginasJan 5, 2021 TDIR Worksheet (COG 2)Clarabelle Mae Dela RosaAún no hay calificaciones