Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Checklist Facility Preparedness
Cargado por
Henry Schein0 calificaciones0% encontró este documento útil (0 votos)
117 vistas2 páginasChecklist Facility Preparedness
Derechos de autor
© © All Rights Reserved
Formatos disponibles
PDF, TXT o lea en línea desde Scribd
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoChecklist Facility Preparedness
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PDF, TXT o lea en línea desde Scribd
0 calificaciones0% encontró este documento útil (0 votos)
117 vistas2 páginasChecklist Facility Preparedness
Cargado por
Henry ScheinChecklist Facility Preparedness
Copyright:
© All Rights Reserved
Formatos disponibles
Descargue como PDF, TXT o lea en línea desde Scribd
Está en la página 1de 2
July 11, 2013 Centers for Disease Control and Prevention (CDC) Page 1 of 2
Healthcare Facility Preparedness Checklist for MERS-CoV
All U.S. healthcare facilities need to be prepared for new and emerging infectious disease threats such as
Middle East Respiratory Syndrome Coronavirus (MERS-CoV). All hospitals should be equipped and ready
to care for a limited number of infected patients as part of routine operations and also to potentially care
for a larger number of patients in the context of escalating transmission. Facilities should outline plans
for administrative, environmental, and communication measures and define the individual work
practices that will be required to detect the introduction of MERS-CoV or other emerging infectious
diseases, prevent spread, and manage the impact on patients, the facility, and staff.
The following checklist highlights some key areas for healthcare facilities to review in preparation for
MERS-CoV. The checklist format is not intended to set forth mandatory requirements or establish
national standards.
Ensure facility infection control policies are consistent with the Centers for Disease Control
and Preventions MERS-CoV guidance (http://www.cdc.gov/coronavirus/mers/infection-
prevention-control.html)
Review procedures for rapidly implementing appropriate isolation and infection practices
for potential MERS-CoV patients
Review policies and procedures for screening and work restrictions for exposed or ill HCP
including ensuring that HCP have ready access, including via telephone, to medical
consultation
Review procedures for laboratory submission of specimens for MERS-CoV testing
Review plans for implementation of surge capacity procedures and crisis standards of care
Develop plans for visitor restriction if MERS-CoV is circulating in the community
Ensure that specific persons have been designated within the facility who are responsible
for communication with public health officials and dissemination of information to other
HCP at the facility
Confirm the local or state health department contact for reporting MERS-CoV cases and
confirm reporting requirements
Assure ability to implement triage activities based on public health guidance including at the
facility and using remote (i.e., phone, internet-based) methods where appropriate to
minimize demand on the health care system
Ensure that negative-pressure airborne infection isolation rooms are functioning correctly
and are appropriately monitored for airflow and exhaust handling
Ensure that HCP who will provide patient-care have been medically cleared, fit-tested, and
trained for respirator use
Provide education and refresher training in the next six weeks to HCP regarding MERS-CoV
diagnosis, how to obtain specimen testing, appropriate PPE use, triage procedures including
July 11, 2013 Centers for Disease Control and Prevention (CDC) Page 2 of 2
patient placement, HCP sick leave policies, and how and to whom MERS-CoV cases should
be reported, procedures to take following unprotected exposures (i.e., not wearing
recommended PPE) to suspected MERS-CoV patients at the facility
Assess availability of personal protective equipment (PPE) and other infection control
supplies (e.g., hand hygiene supplies) that would be used for both healthcare personnel
(HCP) protection and source control for infected patients (e.g., facemask on the patient)
Have contingency plans if the demand for PPE or other supplies exceeds supply
Assess effectiveness of environmental cleaning procedures; provide education/refresher
training for cleaning staff (http://www.cdc.gov/HAI/toolkits/Evaluating-Environmental-
Cleaning.html)
Monitor the situation at CDCs MERS website:
http://www.cdc.gov/coronavirus/mers/index.html
For more information, visit http://www.cdc.gov/coronavirus/mers/preparedness/checklist-facility-
preparedness.html.
También podría gustarte
- National Infection Control Guidelines - 2016 Draft For ConsultationDocumento341 páginasNational Infection Control Guidelines - 2016 Draft For Consultationlimiya vargheseAún no hay calificaciones
- Documentation of Clinical Trial Monitoring: A practical guide compliant with Good Clinical PracticeDe EverandDocumentation of Clinical Trial Monitoring: A practical guide compliant with Good Clinical PracticeCalificación: 5 de 5 estrellas5/5 (1)
- Local Resumption of Elective Surgery GuidanceDocumento10 páginasLocal Resumption of Elective Surgery Guidancevjgg810199Aún no hay calificaciones
- Hospital Checklist Ebola PreparednessDocumento6 páginasHospital Checklist Ebola PreparednessVasu KodagantiAún no hay calificaciones
- Ats PR Assembly Re Opening PR Document FinalDocumento8 páginasAts PR Assembly Re Opening PR Document FinalElliot AndersonAún no hay calificaciones
- Guide To Infection Prevention in Outpatient Settings: Minimum Expectations For Safe CareDocumento16 páginasGuide To Infection Prevention in Outpatient Settings: Minimum Expectations For Safe CareJun AnteolaAún no hay calificaciones
- Standatds of Ambulatory Care 7 2011Documento17 páginasStandatds of Ambulatory Care 7 2011nikky costeAún no hay calificaciones
- WHO 2019 nCoV Lab Testing 2021.1 EngDocumento16 páginasWHO 2019 nCoV Lab Testing 2021.1 EngEddy KurniawanAún no hay calificaciones
- Hospital Checklist Ebola PreparednessDocumento6 páginasHospital Checklist Ebola PreparednessMark ReinhardtAún no hay calificaciones
- Guide To Infection Prevention For Outpatient Settings:: Minimum Expectations For Safe CareDocumento42 páginasGuide To Infection Prevention For Outpatient Settings:: Minimum Expectations For Safe Caresalcais9042Aún no hay calificaciones
- Curry International TB CentreDocumento11 páginasCurry International TB CentreLennyOctaviaAún no hay calificaciones
- COVID-19 Office Prep ChecklistDocumento4 páginasCOVID-19 Office Prep ChecklistMohammad SahyouniAún no hay calificaciones
- Guide infection prevention outpatient careDocumento42 páginasGuide infection prevention outpatient careAli GhanemAún no hay calificaciones
- Cpms College of Nursing: Assignment ON Infection SurveillanceDocumento9 páginasCpms College of Nursing: Assignment ON Infection SurveillanceAmy Lalringhluani ChhakchhuakAún no hay calificaciones
- ASE Reintro Statement FINALDocumento14 páginasASE Reintro Statement FINALIrina Cabac-PogoreviciAún no hay calificaciones
- Infection Control Policy5967286291Documento41 páginasInfection Control Policy5967286291Shyam PrasadAún no hay calificaciones
- Infection Prevention - General Principles - UpToDateDocumento25 páginasInfection Prevention - General Principles - UpToDatemayteveronica1000Aún no hay calificaciones
- Final HICC Manual AIIMSDocumento35 páginasFinal HICC Manual AIIMSNaMakAún no hay calificaciones
- Job Descriptionof ICNDocumento5 páginasJob Descriptionof ICNsari sasiAún no hay calificaciones
- Utah State Hospital Policies and Procedures Infection ControlDocumento75 páginasUtah State Hospital Policies and Procedures Infection ControlMichael SilvaAún no hay calificaciones
- ICU Prep Strategies for COVID-19Documento24 páginasICU Prep Strategies for COVID-19Even EdomekoAún no hay calificaciones
- Reopening Healthcare Facilities for Non-COVID CareDocumento3 páginasReopening Healthcare Facilities for Non-COVID CareDaniel RusseAún no hay calificaciones
- Guidance for preventing and controlling COVID-19 in nursing homesDocumento6 páginasGuidance for preventing and controlling COVID-19 in nursing homesAdrian RuxandaAún no hay calificaciones
- Basic Concepts in Infection Prevention and Control 2023Documento44 páginasBasic Concepts in Infection Prevention and Control 2023Tannov SiregarAún no hay calificaciones
- IPC Program of WorksDocumento5 páginasIPC Program of WorksElmira MalaboAún no hay calificaciones
- Local Guidelines for Infection PreventionDocumento10 páginasLocal Guidelines for Infection PreventionCris GalendezAún no hay calificaciones
- Minnesota Guidelines For Resuming Time Sensitive Surgery and Procedures: COVID-19 BackgroundDocumento5 páginasMinnesota Guidelines For Resuming Time Sensitive Surgery and Procedures: COVID-19 BackgroundJill BurcumAún no hay calificaciones
- Blood Borne Pathogens PolicyDocumento8 páginasBlood Borne Pathogens PolicyChris KristoffersonAún no hay calificaciones
- 26 FTPDocumento2 páginas26 FTPwatsonmexAún no hay calificaciones
- Infection Control Program 2020 - 2021Documento9 páginasInfection Control Program 2020 - 2021HIBA OMERAún no hay calificaciones
- Joint Statement Resuming Elective Surgery After COVID19Documento4 páginasJoint Statement Resuming Elective Surgery After COVID19vjgg810199Aún no hay calificaciones
- Standard Operating Procedure For ControlDocumento31 páginasStandard Operating Procedure For ControlRizky PrakasaAún no hay calificaciones
- Aislamientos Pacientes Con Fibrosis Quistica ICHE03Documento48 páginasAislamientos Pacientes Con Fibrosis Quistica ICHE03haedugaAún no hay calificaciones
- RCDSO Guidelines Infection Prevention and ControlDocumento56 páginasRCDSO Guidelines Infection Prevention and ControlMoaz AlbabaAún no hay calificaciones
- HOSPITAL INFECTION PREVENTION AND CONTROL GUIDELINESDocumento65 páginasHOSPITAL INFECTION PREVENTION AND CONTROL GUIDELINESRazaCreciaLastrillaMenesesAún no hay calificaciones
- 2019 Novel Coronavirus (COVID-19) : Availability of Personal Protective EquipmentDocumento4 páginas2019 Novel Coronavirus (COVID-19) : Availability of Personal Protective EquipmentPetroAún no hay calificaciones
- PneumoniaDocumento12 páginasPneumoniaadolfrc9200Aún no hay calificaciones
- WHO 2019 NCoV Ag RDTs Self Testing 2022.1 EngDocumento16 páginasWHO 2019 NCoV Ag RDTs Self Testing 2022.1 EngLeong Sen FongAún no hay calificaciones
- Barrera E, 2015. F-A-S-T A Refocused, Intensified, Administrative TuberculosisDocumento4 páginasBarrera E, 2015. F-A-S-T A Refocused, Intensified, Administrative Tuberculosisje8aAún no hay calificaciones
- Materi CSSD - Arlina - Cek List Rawat Jalan PpiDocumento8 páginasMateri CSSD - Arlina - Cek List Rawat Jalan PpiGulam ArsyadAún no hay calificaciones
- Functioning of Infection Control CommitteeDocumento3 páginasFunctioning of Infection Control Committeetummalapalli venkateswara raoAún no hay calificaciones
- RCDSO Infection ControlDocumento56 páginasRCDSO Infection ControlsnaniraqAún no hay calificaciones
- Planning For A Psychiatric COVID-19-Positive UnitDocumento5 páginasPlanning For A Psychiatric COVID-19-Positive UnitOmaira TovarAún no hay calificaciones
- Checklist For Preparing Your IR Service For COVID-19Documento8 páginasChecklist For Preparing Your IR Service For COVID-19uroshkgAún no hay calificaciones
- Sop Number Title of SOP Author Consultation With StakeholdersDocumento23 páginasSop Number Title of SOP Author Consultation With StakeholdersMr. BamsAún no hay calificaciones
- p.1-2 - Standards in Infection Control For Healthcare FacilitiesDocumento19 páginasp.1-2 - Standards in Infection Control For Healthcare FacilitiestiredandsleepyAún no hay calificaciones
- CDC Guidelines on Standard and Transmission-Based PrecautionsDocumento6 páginasCDC Guidelines on Standard and Transmission-Based PrecautionsKomite PPI RSUDPCAún no hay calificaciones
- IPC Guidelines For COVID 19Documento15 páginasIPC Guidelines For COVID 19Henry OseiAún no hay calificaciones
- ASA APSF Statement On Perioperative Testing For COVID-Updated June 15 2022Documento7 páginasASA APSF Statement On Perioperative Testing For COVID-Updated June 15 2022HIRANGERAún no hay calificaciones
- Fishbone CDiff - Revised 0310Documento1 páginaFishbone CDiff - Revised 0310Anonymous A5wp71HzAún no hay calificaciones
- 16 TB ControlDocumento4 páginas16 TB ControlnwosuchibuikesunAún no hay calificaciones
- Manejo Ambulatorio AdultosDocumento18 páginasManejo Ambulatorio AdultosCarlos Huaman ZevallosAún no hay calificaciones
- Protocol for Infection Control in Outpatient Clinics During COVID-19Documento3 páginasProtocol for Infection Control in Outpatient Clinics During COVID-19ahmad abadaAún no hay calificaciones
- Policy Recommendation On Covid-19Documento4 páginasPolicy Recommendation On Covid-19RapplerAún no hay calificaciones
- 229110A NorovirusControlRecomm508A 1 PDFDocumento3 páginas229110A NorovirusControlRecomm508A 1 PDFBlessingAún no hay calificaciones
- MSQH 5th Edition Draft Standard 5 - Prevention and Control of InfectionDocumento22 páginasMSQH 5th Edition Draft Standard 5 - Prevention and Control of InfectionEsmar A. Hamid Kenoh0% (1)
- Ppi Wevinar 2019Documento48 páginasPpi Wevinar 2019flyspellAún no hay calificaciones
- Infection Control: WWW - Health.gov - AuDocumento3 páginasInfection Control: WWW - Health.gov - Auwewe.trillanesAún no hay calificaciones
- Telemedicine in the ICUDe EverandTelemedicine in the ICUMatthew A. KoenigAún no hay calificaciones
- Dental Trey Supports Emergency Outpatient Clinic in MargheraDocumento2 páginasDental Trey Supports Emergency Outpatient Clinic in MargheraHenry ScheinAún no hay calificaciones
- Henry Schein Offers Theoretical-Practical Courses CAD / CAM and GESDEN G5 in The Association of Hygienists of Catalonia (AHIADEC)Documento2 páginasHenry Schein Offers Theoretical-Practical Courses CAD / CAM and GESDEN G5 in The Association of Hygienists of Catalonia (AHIADEC)Henry ScheinAún no hay calificaciones
- 2017 02 16 HenryScheinEspaña Nota de Prensa Prepare To Care Mundo A Sorrir ESDocumento2 páginas2017 02 16 HenryScheinEspaña Nota de Prensa Prepare To Care Mundo A Sorrir ESHenry ScheinAún no hay calificaciones
- Henry Schein Dental Team Supports The Practice Pink Program For The Benefit of The Austrian Children's Cancer AidDocumento1 páginaHenry Schein Dental Team Supports The Practice Pink Program For The Benefit of The Austrian Children's Cancer AidHenry ScheinAún no hay calificaciones
- Henry Schein Dental Netherlands Supports The Teddy Bear HospitalDocumento2 páginasHenry Schein Dental Netherlands Supports The Teddy Bear HospitalHenry ScheinAún no hay calificaciones
- Henry Schein Organizes Region Events 2016Documento2 páginasHenry Schein Organizes Region Events 2016Henry ScheinAún no hay calificaciones
- Austria - Team Schein Showing HeartDocumento3 páginasAustria - Team Schein Showing HeartHenry ScheinAún no hay calificaciones
- Henry Schein Is Primary Donor To The Solidarity Clinic of Zerca y Lejos in MadridDocumento2 páginasHenry Schein Is Primary Donor To The Solidarity Clinic of Zerca y Lejos in MadridHenry ScheinAún no hay calificaciones
- Henry Schein Dental UK and International College of Dentists Support HealthServe Dental Clinic in SingaporeDocumento3 páginasHenry Schein Dental UK and International College of Dentists Support HealthServe Dental Clinic in SingaporeHenry ScheinAún no hay calificaciones
- 2017 02 16 HenryScheinEspaña Nota de Prensa Prepare To Care Mundo A Sorrir ESDocumento2 páginas2017 02 16 HenryScheinEspaña Nota de Prensa Prepare To Care Mundo A Sorrir ESHenry ScheinAún no hay calificaciones
- Henry Schein Portugal Presents Its Novelties For 2017 at Expo-DentáriaDocumento2 páginasHenry Schein Portugal Presents Its Novelties For 2017 at Expo-DentáriaHenry ScheinAún no hay calificaciones
- Henry Schein Spain Team Members Bring Access To Medical Care To The Most DisadvantagedDocumento2 páginasHenry Schein Spain Team Members Bring Access To Medical Care To The Most DisadvantagedHenry ScheinAún no hay calificaciones
- Henry Schein Organizes Region Events 2016Documento2 páginasHenry Schein Organizes Region Events 2016Henry ScheinAún no hay calificaciones
- Henry Schein Krugg Presented at The Colloquium Dental of CasertaDocumento2 páginasHenry Schein Krugg Presented at The Colloquium Dental of CasertaHenry ScheinAún no hay calificaciones
- Henry Schein Medical "Action Days"Documento1 páginaHenry Schein Medical "Action Days"Henry ScheinAún no hay calificaciones
- WaveOne Gold WorkshopDocumento2 páginasWaveOne Gold WorkshopHenry ScheinAún no hay calificaciones
- 2016 10 25 Henry Schein Press Release HSC Practice Pink SpainDocumento2 páginas2016 10 25 Henry Schein Press Release HSC Practice Pink SpainHenry ScheinAún no hay calificaciones
- Biodentine Bioroot Education EveningDocumento1 páginaBiodentine Bioroot Education EveningHenry ScheinAún no hay calificaciones
- Decontamination The Code of PracticeDocumento2 páginasDecontamination The Code of PracticeHenry ScheinAún no hay calificaciones
- Press Release: Good Health Begins With A Healthy Mouth: Toothbrushes and Toothpaste For RefugeesDocumento1 páginaPress Release: Good Health Begins With A Healthy Mouth: Toothbrushes and Toothpaste For RefugeesHenry ScheinAún no hay calificaciones
- Henry's Angels Continue To Support Local CharitiesDocumento2 páginasHenry's Angels Continue To Support Local CharitiesHenry ScheinAún no hay calificaciones
- Netherlands Dental Event 7-4-16Documento1 páginaNetherlands Dental Event 7-4-16Henry ScheinAún no hay calificaciones
- Press Release: Henry Schein Dental and Software of Excellence Organize The First Dental Management EventDocumento1 páginaPress Release: Henry Schein Dental and Software of Excellence Organize The First Dental Management EventHenry ScheinAún no hay calificaciones
- Good Health Begins With A Healthy Mouth: Toothbrushes and Toothpaste For RefugeesDocumento2 páginasGood Health Begins With A Healthy Mouth: Toothbrushes and Toothpaste For RefugeesHenry ScheinAún no hay calificaciones
- Henry Schein Opens New Logistics CenterDocumento2 páginasHenry Schein Opens New Logistics CenterHenry Schein100% (1)
- Press Release: Good Health Begins With A Healthy Mouth: Toothbrushes and Toothpaste For RefugeesDocumento1 páginaPress Release: Good Health Begins With A Healthy Mouth: Toothbrushes and Toothpaste For RefugeesHenry ScheinAún no hay calificaciones
- Henry Schein Dental UK Supports Alaska Mission of MercyDocumento3 páginasHenry Schein Dental UK Supports Alaska Mission of MercyHenry ScheinAún no hay calificaciones
- Czech Republic Conference, Henry Schein, Henry Schein DentalDocumento1 páginaCzech Republic Conference, Henry Schein, Henry Schein DentalHenry ScheinAún no hay calificaciones
- Arseus Lab Opens Novux® Technology Center, Powered by DatronDocumento2 páginasArseus Lab Opens Novux® Technology Center, Powered by DatronHenry ScheinAún no hay calificaciones
- TORCH in PregnancyDocumento63 páginasTORCH in PregnancyKinjal VasavaAún no hay calificaciones
- Intrauterine InfectionDocumento64 páginasIntrauterine Infectionthapan87100% (1)
- DHIS PHC Facility Monthly Report FormDocumento4 páginasDHIS PHC Facility Monthly Report FormUmair SaleemAún no hay calificaciones
- Communicable Diseases GR.8 HealthDocumento40 páginasCommunicable Diseases GR.8 HealthAiza May RosasAún no hay calificaciones
- COVID-19 Test Report for Vajaram ChoudharyDocumento2 páginasCOVID-19 Test Report for Vajaram ChoudharyJitendra MalviyaAún no hay calificaciones
- Lab Test Spot Urine Microalbumin Creatinine RatioDocumento1 páginaLab Test Spot Urine Microalbumin Creatinine Ratiorajanarora72Aún no hay calificaciones
- Grile NeonatologieDocumento3 páginasGrile NeonatologieCarmelina-Ofelia ConstandinAún no hay calificaciones
- What Is A Urinary Tract InfectionDocumento3 páginasWhat Is A Urinary Tract InfectionVanessa MendezAún no hay calificaciones
- Prepatellar Bursitis - Housemaid's KneeDocumento2 páginasPrepatellar Bursitis - Housemaid's KneeenadAún no hay calificaciones
- Tribute ofDocumento10 páginasTribute ofAlvaro Andres Flores JimenezAún no hay calificaciones
- Assessment Diagnosis Planning Implementation Rationale Evaluation Subjective Data: Short Term: Independent: Short Term: Goal Partially MetDocumento3 páginasAssessment Diagnosis Planning Implementation Rationale Evaluation Subjective Data: Short Term: Independent: Short Term: Goal Partially MetPrincess Mildred AbdonAún no hay calificaciones
- Lifestyle, Genetics and Environment Predispose to DiseaseDocumento4 páginasLifestyle, Genetics and Environment Predispose to DiseaseJohnnette BedoniaAún no hay calificaciones
- IntussusceptionDocumento3 páginasIntussusceptionHasan MohammedAún no hay calificaciones
- Cohort Study Hansana PDFDocumento28 páginasCohort Study Hansana PDFTukai KulkarniAún no hay calificaciones
- Child India March 2021Documento35 páginasChild India March 2021suheena.CAún no hay calificaciones
- Anti-Inflammatory Effect of Panyawan Stem For ToothacheDocumento10 páginasAnti-Inflammatory Effect of Panyawan Stem For ToothacheNolemae NavalesAún no hay calificaciones
- Carolyn R. Zalameda-Castro, MDDocumento9 páginasCarolyn R. Zalameda-Castro, MDeza floresAún no hay calificaciones
- Vaccines in Zimbabwe InformationDocumento8 páginasVaccines in Zimbabwe InformationIsaac GumboAún no hay calificaciones
- 10 Healty Gateways Info For Ships To Prepare For COVID-19 PDFDocumento16 páginas10 Healty Gateways Info For Ships To Prepare For COVID-19 PDFDennis VolodchenkoAún no hay calificaciones
- Skin Pathology: DR Shehu Abdullahi 19/01/2023Documento23 páginasSkin Pathology: DR Shehu Abdullahi 19/01/2023Mohammed HussainAún no hay calificaciones
- Ethical Issues in Mandatory Smallpox VaccinationDocumento2 páginasEthical Issues in Mandatory Smallpox VaccinationFaizaNadeemAún no hay calificaciones
- Severeulcerative Colitis Associated With Coombs Positive Autoimmune Hemolytic Anemia Treated With InfliximabDocumento4 páginasSevereulcerative Colitis Associated With Coombs Positive Autoimmune Hemolytic Anemia Treated With InfliximabIJAR JOURNALAún no hay calificaciones
- Initial Patient Assessment in OpdDocumento4 páginasInitial Patient Assessment in OpdLokender Goyal100% (1)
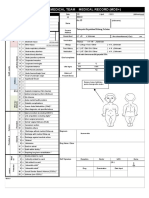
- Emergency Medical Team Medical Record (MDS+) : MDS - Check All That ApplyDocumento2 páginasEmergency Medical Team Medical Record (MDS+) : MDS - Check All That ApplySyafiraIdhatunNasyiahAún no hay calificaciones
- Drugs For Hypertension MIMSDocumento13 páginasDrugs For Hypertension MIMSriczen mae vilaAún no hay calificaciones
- Hiv CounsellingDocumento73 páginasHiv Counsellingomotayofaith360Aún no hay calificaciones
- Viral ChartsDocumento2 páginasViral ChartsPlay ListAún no hay calificaciones
- Importance of Shat Kriyakala in Disease Diagnosis and ManagementDocumento6 páginasImportance of Shat Kriyakala in Disease Diagnosis and ManagementSHUBHAM RAOAún no hay calificaciones
- Pharmaceutical Chemistry Chapter 11 Important QuestionsDocumento7 páginasPharmaceutical Chemistry Chapter 11 Important QuestionsMahesh Kokne100% (1)
- Intestinal Flukes Liver Flukes Lung Flukes Blood Flukes: SinensisDocumento3 páginasIntestinal Flukes Liver Flukes Lung Flukes Blood Flukes: SinensisCHO-ON KIMAún no hay calificaciones