Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Howto Companion April2012
Cargado por
lybrakissDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Howto Companion April2012
Cargado por
lybrakissCopyright:
Formatos disponibles
14
|
companion
How to perform
reliable veterinary
haematology in practice
Sampling
Venepuncture should be clean and quick,
using as large a needle as possible with
minimal suction. Typically use the jugular
vein with a 2123 gauge needle and
2.55 ml syringe. A peripheral vein (e.g.
cephalic), can be used in large dogs if it
is easier to locate and sample, for
example in overweight animals. A clean
and quick sampling is better than repeated
attempts at any single vein. If the first
attempt fails, it is advisable to use a new
needle and change the site slightly or use
a different vein.
These guidelines minimise trauma to
the cells which risks artefact and cell lysis.
Lysis reduces red cell numbers, PCV and
can artificially elevate the haemoglobin
concentrations. A clean technique
minimises tissue damage and activation of
platelets during sampling. Therefore
platelet clumping and clot formation is
prevented which will artificially reduce
platelet numbers and potentially white cells
as well, especially neutrophils.
The blood is typically placed into EDTA
(ethylenediamine tetra-acetic acid)
anticoagulant for many veterinary species.
Anti-coagulant tubes should always be
filled, without the needle attached, to
the correct level because:
Underfilling results in a relative
anticoagulant excess. This excess
EDTA shrinks the cells and alters their
morphology. It can therefore also
stored at room temperature, not the fridge,
as condensation can damage the cells.
If chemical restraint or sampling
occurs under general anaesthesia, this
must be noted. Changes in blood
pressure will have significant effects on
circulating cell numbers. This is seen
naturally/physiologically in animals that are
agitated during sampling. Agitation results
in an increased blood pressure and
splenic contraction, increasing numbers of
circulating white cells, especially
neutrophils and red cells. Conversely,
sedation or anaesthesia lowers blood
pressure and causes splenic
sequestration, reducing the number of
circulating cells, both red cells (falsely low
PCV) and white cells (false leukopenia).
Performing a complete/full
blood count (CBC/FBC)
Ideally, the blood sample should be
processed at least 510 minutes after filling
the EDTA tube to prevent artefacts, such as
cell shrinkage, being introduced before the
blood and EDTA have time to equilibrate.
Analysis varies from a simple spun
microhaematocrit measurement to a full
analysisfive part white cell differential.
Roger Powell, of PTDS veterinary laboratory, a
chapter author for the new edition of the BSAVA
Manual of Canine and Feline Haematology and
Transfusion Medicine, describes how to get the
most out of your practice laboratory
artificially affect the MCV and PCV. If
the tube is less than half full, the
PCV can be reduced by 5%. This
effect is compounded if the animal is
actually anaemic.
Overfilling can allow clotting, which can
prevent automated analysis and alter
cell numbers.
If the needle is still in place the cells
are traumatised (see Figure 1) and
more likely to lyse.
The blood should be gently mixed by
inversion and rolling in your hand, not
shaking. At least one fresh blood smear
should now be made from the EDTA
anticoagulated blood , especially if the
sample is posted to an external lab. Blood
cells begin to degenerate as soon as they
leave the body, with significant changes
being seen after 12 hours. Morphological
features are then often lost, artificial
features created or clinical interpretation
severely hampered. As such, smears
made after postage may not be
representative. Smearing straight from the
syringe typically creates platelet clumps
and uneven smearing as the blood clots
(see Figure 1). The reader is referred to
Elizabeth Villiers excellent previous How
to companion article (December 2008)
for more detailed information on blood
smearing and examination.
Once smeared, the sample is
processed or stored in the fridge if being
posted externally. The slides should be
Figure 1: Fresh blood smear showing significant
in vitro artefact, with red cell lysis and
haemoglobin crystals alongside a damaged
neutrophil (top) and lymphocyte (bottom)
14-18 HOW TO.indd 14 19/03/2012 10:17
companion
|
15
Packed cell volume (PCV)
This is the volume of red cells produced
after high speed (1115,000 rpm)
centrifugation of resuspended whole blood
in a microhaematocrit tube for 5 minutes.
Whilst not identical to the haemocrit (HCT)
it is, or should be, equivalent to the
calculated HCT (see later) produced by the
analyser. It is worth noting that the PCV is
affected by excess EDTA, whereas the
HCT can be less affected.
When performing a manual PCV, the
microhaematocrit tube must be 2/3 to
3/4 full; too little exaggerates red cell
packing on centrifugation, whereas too
much reduces the force and prevents
packing. Whilst this is often not clinically
significant, it can be significant when
compounded by changes in cell numbers,
such as in anaemia.
Automated analyser cell
counting
These form the cornerstone of veterinary
haematology, with three main types being
available. Before any blood is run through
an analyser, it should be:
Stirred thoroughly and checked for
clots using either a microhaematocrit
tube or cocktail stick. If this is not
performed and clots are present, cell
counts can be unknowingly affected or
the analyser blocked/damaged.
Gently and evenly resuspended, by
inverting and rolling for at least 1
minute, especially if the tube has been
left standing for a period of time. If not
performed, cell counts can be
artificially affected depending on the
degree of cell settling.
There are a large number of
haematology analysers available, capable
of producing erythrocyte parameters (RBC,
Hb, HCT/PCV, MCV, MCH and MCHC) with
a three or five part white cell differential
(neutrophils, lymphocytes, monocytes,
eosinophils and basophils) and platelet
count. These machines vary in accuracy
from correct measurements through to
misleading or even inaccurate results. A
laser flow cytometer calculates the
leukogram and erythrogram; the basic
principles are described below.
Generating a leukogram
In general, newer impedance and laser
cytometer analysers can be accurate in
many healthy and some diseased
situations. Even haematology analysers in
commercial referral labs, costing many
thousands of pounds more, can and do
make differential errors. As such,
confirming white cell differentials and
assessing cell morphology in a blood
smear is a vital part of the complete
blood count. Staining in practice typically
will be achieved using a rapid based kit
and the reader is referred to Kath
Tennants How to article in companion
(June 2008) for further information.
However, a good analyser counts
thousands of cells resulting in a
numerical precision superior to any
manual count (typically this involves
counting 100500 cells). Therefore the
analyser leukocyte differential count is only
altered if the manual smear differential is
significantly different. Other analysers that
cannot reliably differentiate cells should
only be used to provide total cell counts;
the differential count should be provided
by smear examination.
Understanding the methods that these
machines use for cell counting help
understand circumstances in which
manual correction of the differential count
might be required.
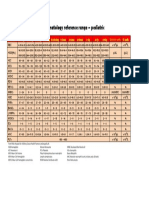
Presence of nucleated erythrocytes
The white cells are often counted after the
red cells have been lysed, however
corrected (true) white cell count =
100
(nRBC + 100)
x nucleated cell count
HCT (l/l) =
MCV (f) x RBC (x 10
12
/l)
10
MCHC (g/dl) =
Hb (g/dl) x 100
HCT (l/l)
MCH (pg) =
Hb (g/dl) x 10
RBC (x 10
12
/l)
immature nucleated red cells are resistant
to lysis. The analyser assumes that all
cells counted following lysis are leukocytes
which may not be true. Therefore most
white cell counts are in fact a nucleated
cell count. Therefore if nucleated red cells
are present (in significant numbers) when
examining the smear, the white cell count
needs correcting as follows:
Generating an erythrogram
Once the cells are counted (RBC), size
(MCV) and haemoglobin (Hb) measured,
the analyser calculates several red cell
parameters: HCT, Mean Cell Haemoglobin
Concentration (MCHC) and Mean Cell
Haemoglobin (MCH):
MCHC is a useful parameter for
monitoring the analysers red cell
performance. It is calculated from the Hb
and HCT in most machines using two
independent techniques. Values less than
28 are likely artefactual, as diseases such
as iron deficiency rarely produce values
this low. Conversely if the value is elevated,
artefact, such as agglutination, haemolysis
or lipaemia, is likely. If the MCHC falls
outside the reference values, assessing for
potential artefact is recommended initially,
before ascribing the value to a disease.
14-18 HOW TO.indd 15 19/03/2012 10:17
16
|
companion
How to perform reliable veterinary
haematology in practice
A good general check to perform on all
erythrograms to ascertain the analyser
is working correctly is to check that the
Hb value is about one third the HCT/
PCV ( 3).
Types of analyser commonly
used in veterinary practice
1) Quantitative buffy coat (QBC)
analysers
These machines use two separate
methods to determine the erythrogram
and leucogram.
The PCV and MCHC are measured,
and the other red cell parameters are
then all calculated.
The white cell counts are determined
from the width and fluorescence of
various cell layers/bands in a
centrifuged buffy coat artificially
expanded by a float. The layer width
and degree of fluorescence reflect cell
numbers, assuming that the cells are
all normal size. The differentiation of
white cell types is based on the
variable fluorescence of leukocytes
when stained to create a differential of
mononuclear cells (lymphocytes and
monocytes) from granulocytes
(neutrophils and eosinophils). This
fluorescence is very reliant on an
absence of background interference
and healthy normal cells. Often in
disease the size, nature and RNA
content of the cells changes, and thus
the discrimination is lost. Similarly if the
distinction between the bands is lost,
counting can be inaccurate or simply
wrong. Therefore whilst these
analysers typically give an accurate
total white cell count in healthy
animals, the differential count is
often unreliable and misleading in
clinical patients. Figure 2 provides an
illustrative example.
2) Impedance counters
These analysers sort cells using
impedance. The cells are diluted in an
electrolyte solution and then drawn through
an aperture within an electrode. As each
cell passes through, it creates a pulse of
resistance the more pulses, the more
cells there are (Coulter principle). The size
of each resistance (impedance) pulse is
proportional to the size of cell. The size of
cells types (platelet versus red versus
white) differ between species so these
machines must be set and calibrated to the
appropriate species. If there is overlap in
size between two cells types, impedance
counters fail to distinguish the cells and will
ascribe them to the wrong type. Most
commonly platelets will be miscounted as
red cells if their size overlaps (see Figure
3), or platelet and red blood cell clumps as
white blood cells.
Figure 2: (A) Buffy coat profile from a 1-year-old
MN Labrador with pyrexia of unknown origin.
The automated analysis reported a signficant
eosinophilia (with no flags) for which the dog
was investigated. Blood film examination by a
haematologist revealed a significant
lymphocytosis. The majority of these cells were
granular lymphocytes (B) which the analyser
was mis-classifying as eosinophils due to their
granularity. The dog had an idiosyncratic and
eventually self-resolving reaction to a booster
vaccination
A
B
A
Figure 3: (A) Dog with iron-deficiency anaemia
due to gastrointestinal blood loss. The
combination of microcytosis and a
thrombocytosis with macroplatelets prevents
accurate automated differentiation, as the
platelet histogram merges into the red cells on
the right side, the set discrimination threshold
(dotted line) not being applicable in this
instance. (B) The macroplatelet (left) is the
same size as adjacent red blood cells
B
14-18 HOW TO.indd 16 19/03/2012 10:17
companion
|
17
3) Laser flow cytometers
These are more recently available as
affordable bench top analysers but still
remain much more expensive than
impedance or QBC analysers. A stream of
single file cells is passed through a laser
beam, resulting in scattering of the light.
This scatter is both forward (related to the
size of the cell) and to the side (related to
the complexity/granularity of the cell). This
scattering effect can be enhanced by use
of certain lysing solutions to leave only a
few cell types for analysis, and the use of
dyes which cause cellular granules of
fluoresce under laser light. A number of
graphical plots are produced to aid
analysis and interpretation. These produce
reliable red and white cell analysis in some
situations, but are still subject to artefacts
or problems during many diseases see
Figure 4.
How are the results reported?
Graphical displays
When counting and assessing the cells, all
the above methods produce one or more
graphical displays, histograms or scatter
plots, both of cell size and also various
cellular constituents. Without doubt, using
and visually assessing these displays
enhances the information that is gained
from the analysis. Whilst this does not
replace the need to look at a fresh blood
smear, it can identify potential artefacts
and significant changes in cell populations
that would otherwise be misdiagnosed or
not identified if only numerical values are
assessed. For example, red cell indices
are typically reported as mean values. A
significant change in the red cell
population has to occur before the mean
value changes. The red cell and platelet
distribution width values (if provided) are a
numerical indicator of the histograms or
scatter plots width so can show such
Figure 4: (A) Laser flow analyser print out and scatter plots from an entire male dog with generalised
malaise and hyperglobulinaemia. The red cell numbers are discordantly low and the MCV high due
to rouleaux red cell clumping and scattered platelet clumps (B2), with eccentrocytosis (B1). White
cell differential checking showed no basophilia or monocytosis but there was a left-shifted
moderately toxic neutrophilia (B3) with reactive lymphocytes (B2). The dog had an infected
prostatic abscess
A
B1
B2
B3
Figure 5: Impedance RBC histogram from
a dog with iron-deficient regenerative
anaemia (black line); and a healthy dog
(dotted red line). The peaks are similar and
therefore the MCV was within reference
limits, but the histogram clearly shows
increased numbers of small cells
(microcytosis), as well as macrocytosis due
to regeneration
changes more readily (Figure 5).
All analyser problems are more
significant and dramatic the more
diseased an animal is. Automated flags
and comments are often misleading,
especially if the disease is haematological
(e.g. leukaemia). Abnormally large cellular
material can however be identified on
these graphical displays. This prompts
analysis of the smear as it is expected that
the automated differentiation will likely
have ascribed them to the wrong cell line
(see Figure 6).
There is as yet no good way for these
analysers to detect or report morphological
changes such as toxicity in neutrophils that
14-18 HOW TO.indd 17 19/03/2012 10:17
18
|
companion
How to perform reliable veterinary
haematology in practice
would be evident in a blood film to the
trained eye (such as in Figure 4).
In summary
1. Check the sampling information for
significant pre-analytical factors.
2. Check the RBC, Hb and HCT/PCV
values are relatively similar within
their reference intervals. Also check
the Hb value is approximately 1/3 of
the PCV/HCT.
3. Check the MCHC value is not elevated
nor inappropriately low.
4. If these criteria are not met, look for
significant artefactual factors and
correct by repeat analysis where
possible.
5. Check the white cell graphical print out
for abnormal or irregular areas and
blurring/coalescing of cell groups or
histograms. If present, the film must be
Figure 6: (A) Numerical values from an impedance
analyser suggesting a mild lymphocytosis. (B) The
graphical display clearly shows an abnormal WBC
pattern with very large cellular material peaking at
about 300 whereas white cells in health are much
smaller (<300). (C) This was an acute lymphoblastic
leukaemia, the cells shown here being enlarged
and accounting for the graphical pattern
A
C
B
examined and potentially the sample
re-analysed.
6. If the platelet count is low, check the
smear for large platelets and/or
clumps. Resampling may be required
for accurate counting.
7. Examine or send away a blood smear
to identify artefacts and significant cell
morphology.
8. Repeat the haematology as required to
assess shifts in pattern and disease,
potentially from day to day.
Accurate and precise veterinary
haematology or a complete blood count
always requires both automated analysis
and blood smear examination. With a few
minutes spent examining a blood smear
and the numerical and graphical output of
in house haematology machines, reliable
results are readily achievable.
NOW AVAILABLE
FROM BSAVA
BSAVA Manual of
Canine and Feline
Haematology and
Transfusion Medicine,
2nd editon
Edited by Michael Day
and Barbara Kohn
With the advent of automated haematology
and serum biochemistry analysers, most
clinics now do their own laboratory work
in-house. Clinical pathology, and specically
haematology, are achieving prominence
in general practce. Most practtoners
now want to get extra miles out of their
analysers, in additon to evaluatng the
patent, blood and bone marrow smears, and
additonal diagnostcs.
The second editon provides a ready source
of practcal informaton for veterinary
surgeons in general practce and is also
useful for undergraduate veterinary students,
veterinary nurses and veterinary graduates
embarking on further qualicatons in small
animal medicine.
Contents: Haematology; Erythrocyte
disorders; Leucocyte disorders;
Haemostasis; Disorders of haemostasis;
Transfusion medicine.
Member price 59*
(BSAVA members* if you are atending
the WSAVA/FECAVA/BSAVA Congress in
April, remember to bring your membership
card to get an extra 5 o the normal
member price)
Non-member price 95
14-18 HOW TO.indd 18 19/03/2012 10:17
También podría gustarte
- Practical Transfusion Medicine for the Small Animal PractitionerDe EverandPractical Transfusion Medicine for the Small Animal PractitionerAún no hay calificaciones
- Media Analysis For SoundDocumento32 páginasMedia Analysis For SoundJerralynDavisAún no hay calificaciones
- Guidelines For Taking Diagnostic Samples From Pigs: BloodDocumento6 páginasGuidelines For Taking Diagnostic Samples From Pigs: BloodchiralicAún no hay calificaciones
- Urinary Catheter Placement For Feline ObstructionDocumento6 páginasUrinary Catheter Placement For Feline ObstructionWilliam ChandlerAún no hay calificaciones
- Clinical Veterinary Advisor Dogs and Cats by Etienne Cote DVMDACVIMCardiology and Small Animal Internal Medicine 5 Star ReviewDocumento2 páginasClinical Veterinary Advisor Dogs and Cats by Etienne Cote DVMDACVIMCardiology and Small Animal Internal Medicine 5 Star ReviewAndres GarciaAún no hay calificaciones
- FieldManual A Field Manual For Collection of Specimens To Enhance Diagnosis of Animal Diseases PDFDocumento150 páginasFieldManual A Field Manual For Collection of Specimens To Enhance Diagnosis of Animal Diseases PDFrazadrpkAún no hay calificaciones
- Current Diagnostic Techniques in Veterinary Surgery PDFDocumento2 páginasCurrent Diagnostic Techniques in Veterinary Surgery PDFKirti JamwalAún no hay calificaciones
- Anesthesia Guidelines For Dogs and CatsDocumento9 páginasAnesthesia Guidelines For Dogs and CatsNatalie KingAún no hay calificaciones
- Veterinary Critical CareDocumento15 páginasVeterinary Critical Caresudanfx100% (1)
- J.L. Vegad-A Colour Atlas of Poultry Diseases - An Aid For Farmers and Poultry Professionals-International Book Distributing Co (2008)Documento131 páginasJ.L. Vegad-A Colour Atlas of Poultry Diseases - An Aid For Farmers and Poultry Professionals-International Book Distributing Co (2008)Jajang MasbroAún no hay calificaciones
- BR Lyoquest en 0111 - 0 PDFDocumento4 páginasBR Lyoquest en 0111 - 0 PDFmarcelloairesAún no hay calificaciones
- Amputation of Tail in AnimalsDocumento8 páginasAmputation of Tail in AnimalsSabreen khattakAún no hay calificaciones
- Fluidtherapy GuidelinesDocumento11 páginasFluidtherapy Guidelineshamida fillahAún no hay calificaciones
- Veterinary Cytology by Leslie C. Sharkey, M. Judith Radin, Davis SeeligDocumento994 páginasVeterinary Cytology by Leslie C. Sharkey, M. Judith Radin, Davis SeeligBê LagoAún no hay calificaciones
- Immunolocalization of Aquaporin-5 Expression in Sweat Gland Cells From Normal and Anhidrotic Horses (Pages 17-23)Documento7 páginasImmunolocalization of Aquaporin-5 Expression in Sweat Gland Cells From Normal and Anhidrotic Horses (Pages 17-23)jenAún no hay calificaciones
- Section 8 - Equine Bacterial DiseasesDocumento3 páginasSection 8 - Equine Bacterial DiseasesRakesh KumarAún no hay calificaciones
- Sutures عبد الرحمن الزميليDocumento54 páginasSutures عبد الرحمن الزميليعبد الرحمن خالد الزميليAún no hay calificaciones
- Veterinary Surgical InstrumentsDocumento93 páginasVeterinary Surgical InstrumentsEster ToledanoAún no hay calificaciones
- RUV40404 Certificate IV in Veterinary NursingDocumento36 páginasRUV40404 Certificate IV in Veterinary NursingEdward FergusonAún no hay calificaciones
- Outcomes of Dogs Undergoing Limb Amputation, Owner Satisfaction With Limb Amputation Procedures, and Owner Perceptions Regarding Postsurgical Adaptation: 64 Cases (2005-2012)Documento7 páginasOutcomes of Dogs Undergoing Limb Amputation, Owner Satisfaction With Limb Amputation Procedures, and Owner Perceptions Regarding Postsurgical Adaptation: 64 Cases (2005-2012)William ChandlerAún no hay calificaciones
- Fluidtherapy Guidelines PDFDocumento11 páginasFluidtherapy Guidelines PDFJoão Pedro PereiraAún no hay calificaciones
- Feline Blood TransfusionDocumento4 páginasFeline Blood TransfusionPhilipsAún no hay calificaciones
- Birds and Exotics - MCannon PDFDocumento42 páginasBirds and Exotics - MCannon PDFAl OyAún no hay calificaciones
- FELINE-Clinical Forms of Acquired Myasthenia Gravis in CatsDocumento7 páginasFELINE-Clinical Forms of Acquired Myasthenia Gravis in Catstaner_soysurenAún no hay calificaciones
- How Became A Millionaire Veterinary Practitioners by Jibachha Veterinary HospitalDocumento10 páginasHow Became A Millionaire Veterinary Practitioners by Jibachha Veterinary HospitalAnonymous JzaNyfT3Aún no hay calificaciones
- Canine and Feline Skin Cytology-1Documento10 páginasCanine and Feline Skin Cytology-1Hernany BezerraAún no hay calificaciones
- LPM-UNIT-III-16 Breeding Ram BuckDocumento16 páginasLPM-UNIT-III-16 Breeding Ram BuckSachin PatilAún no hay calificaciones
- SOP: Blood Collection in SwineDocumento6 páginasSOP: Blood Collection in SwineHenri YudamuktiAún no hay calificaciones
- Accd e BookDocumento154 páginasAccd e BookAchmad Nur MmadAún no hay calificaciones
- Canine Ehrlichiosis With Uveitis in A Pug Breed Dog: Case StudDocumento2 páginasCanine Ehrlichiosis With Uveitis in A Pug Breed Dog: Case StudDR HAMESH RATREAún no hay calificaciones
- Diseases of Poultry1b2Documento30 páginasDiseases of Poultry1b2Mohamed AktharAún no hay calificaciones
- Complications of Fluid TherapyDocumento13 páginasComplications of Fluid TherapyElizabeth ArriagadaAún no hay calificaciones
- 2015 Proceeding - Management of The Patient With Canine Parvovirus EnteritisDocumento7 páginas2015 Proceeding - Management of The Patient With Canine Parvovirus EnteritisJHack2Aún no hay calificaciones
- Sample Collection VMCDocumento11 páginasSample Collection VMCAnuj TewariAún no hay calificaciones
- Veterinary Post Mortem TechnicDocumento263 páginasVeterinary Post Mortem TechnicEdgar EndressAún no hay calificaciones
- Surgery of The Bovine Large IntestineDocumento18 páginasSurgery of The Bovine Large IntestineJhon Bustamante CanoAún no hay calificaciones
- Companion March2013Documento36 páginasCompanion March2013lybrakissAún no hay calificaciones
- 9 A31 Ad 01Documento302 páginas9 A31 Ad 01bhoopendrabisht100% (3)
- Special Veterinary Pathology: The Canadian Veterinary Journal. La Revue Veterinaire Canadienne February 1990Documento2 páginasSpecial Veterinary Pathology: The Canadian Veterinary Journal. La Revue Veterinaire Canadienne February 1990Alonso Guardado100% (1)
- Suspensory Ligament Rupture Tech During Small Animal OH PDFDocumento8 páginasSuspensory Ligament Rupture Tech During Small Animal OH PDFRiesky NudialestariAún no hay calificaciones
- Lab Manual VPE311Documento40 páginasLab Manual VPE311Friends ZoneAún no hay calificaciones
- Canine InsulinomaDocumento5 páginasCanine Insulinomasoff4ikaAún no hay calificaciones
- Urine Sediment Guide PDFDocumento4 páginasUrine Sediment Guide PDFMuhammad FaridAún no hay calificaciones
- Elective Caesarean Section on a GoatDocumento17 páginasElective Caesarean Section on a GoatAbdirazak AlkhaalidAún no hay calificaciones
- PDFDocumento657 páginasPDFJesús Enrique Turín Vilca100% (1)
- Agappe Chitra Magna IFU 14 May PDFDocumento2 páginasAgappe Chitra Magna IFU 14 May PDFDharmesh PatelAún no hay calificaciones
- Brucellosis in Cattle Interim Manual For The Veterinarian & AHT - Sept2016 - SignedDocumento54 páginasBrucellosis in Cattle Interim Manual For The Veterinarian & AHT - Sept2016 - SignedSuraj_Subedi100% (3)
- Vet Guide PMDDocumento8 páginasVet Guide PMDdanxAún no hay calificaciones
- Radiographic Signs of Pulmonar DiseaseDocumento10 páginasRadiographic Signs of Pulmonar DiseaseMarleeng CáceresAún no hay calificaciones
- Feline Urethrostomy Procedure ExplainedDocumento2 páginasFeline Urethrostomy Procedure Explainedclara FAún no hay calificaciones
- The Value of Haematology in Avian Clinical Practice Master Class TheoryDocumento24 páginasThe Value of Haematology in Avian Clinical Practice Master Class TheoryKhoirun Nisa0% (1)
- Female Rat Reproductive Cycle PDFDocumento10 páginasFemale Rat Reproductive Cycle PDFogheeluvAún no hay calificaciones
- Carbohydrate and Lipid MetabolismDocumento47 páginasCarbohydrate and Lipid MetabolismShirley Faye SalesAún no hay calificaciones
- EnucleationDocumento6 páginasEnucleationRameez SarwarAún no hay calificaciones
- Vet Drug ResiduesDocumento512 páginasVet Drug ResiduesWel_elhawarry100% (1)
- NAVLE Competencies FINALDocumento19 páginasNAVLE Competencies FINALShubham HarishAún no hay calificaciones
- ACKD in DogsDocumento9 páginasACKD in DogsGreomary Cristina MalaverAún no hay calificaciones
- M.C. Muhlbauer, S.K. Kneller - Radiography of The Dog and Cat - Guide To Making and Interpreting Radiographs-Wiley-Blackwell (2024)Documento579 páginasM.C. Muhlbauer, S.K. Kneller - Radiography of The Dog and Cat - Guide To Making and Interpreting Radiographs-Wiley-Blackwell (2024)dpcamposhAún no hay calificaciones
- Radiography & Surgery - SA & LADocumento80 páginasRadiography & Surgery - SA & LAMelrose Del Pilar CondinoAún no hay calificaciones
- Clinical Atlas of Canine and Feline Ophthalmic DiseaseDe EverandClinical Atlas of Canine and Feline Ophthalmic DiseaseAún no hay calificaciones
- XPress Studio HD 5.1 InstallIDocumento31 páginasXPress Studio HD 5.1 InstallIlybrakissAún no hay calificaciones
- Xpress Pro 4.5 UGSuppDocumento248 páginasXpress Pro 4.5 UGSupplybrakissAún no hay calificaciones
- Infinity Connect Mobile Userguide V1.10.aDocumento17 páginasInfinity Connect Mobile Userguide V1.10.alybrakissAún no hay calificaciones
- Pexip Infinity Scheduling Meetings Quickguide V32.aDocumento4 páginasPexip Infinity Scheduling Meetings Quickguide V32.alybrakissAún no hay calificaciones
- Collected Works of PoeDocumento208 páginasCollected Works of PoeTrần Tú BíchAún no hay calificaciones
- MesopotamDocumento35 páginasMesopotamlybrakissAún no hay calificaciones
- MotivationalDocumento43 páginasMotivationallybrakissAún no hay calificaciones
- Infinity Connect Desktop Userguide V1.12.aDocumento25 páginasInfinity Connect Desktop Userguide V1.12.alybrakissAún no hay calificaciones
- Infinity Connect Webapp Userguide V32.aDocumento35 páginasInfinity Connect Webapp Userguide V32.alybrakissAún no hay calificaciones
- LE 069 LE 078 InstructionsDocumento4 páginasLE 069 LE 078 InstructionslybrakissAún no hay calificaciones
- Document ActDocumento15 páginasDocument ActlybrakissAún no hay calificaciones
- A Little PrincessDocumento196 páginasA Little PrincessShona ButtAún no hay calificaciones
- Pexip Infinity Management API V32.aDocumento53 páginasPexip Infinity Management API V32.aozz12345Aún no hay calificaciones
- About AbrahamDocumento25 páginasAbout AbrahamlybrakissAún no hay calificaciones
- AramanicDocumento50 páginasAramaniclybrakissAún no hay calificaciones
- The Call of CthulhuDocumento14 páginasThe Call of CthulhuLOKADAún no hay calificaciones
- 1017 Intelligence Quotient IQ Test Interview Questions Answers GuideDocumento7 páginas1017 Intelligence Quotient IQ Test Interview Questions Answers GuideRaniel MamaspasAún no hay calificaciones
- C Enu Faci PT DragosteDocumento95 páginasC Enu Faci PT DragostelybrakissAún no hay calificaciones
- 1017 Intelligence Quotient IQ Test Interview Questions Answers GuideDocumento7 páginas1017 Intelligence Quotient IQ Test Interview Questions Answers GuideRaniel MamaspasAún no hay calificaciones
- How-To-may-2014 CompanionHow To Utilize Radiotherapy For Dogs With Oral TumoursIntroductionDocumento6 páginasHow-To-may-2014 CompanionHow To Utilize Radiotherapy For Dogs With Oral TumoursIntroductionlybrakissAún no hay calificaciones
- How-To-september-2014 2014how To Manage Feline Ureteric ObstructionDocumento5 páginasHow-To-september-2014 2014how To Manage Feline Ureteric ObstructionlybrakissAún no hay calificaciones
- 1017 Intelligence Quotient IQ Test Interview Questions Answers GuideDocumento7 páginas1017 Intelligence Quotient IQ Test Interview Questions Answers GuideRaniel MamaspasAún no hay calificaciones
- How-To-june-2014 CompanionHow To Approach The Canine AthleteInDocumento6 páginasHow-To-june-2014 CompanionHow To Approach The Canine AthleteInlybrakissAún no hay calificaciones
- Stiri WWWDocumento5 páginasStiri WWWlybrakissAún no hay calificaciones
- Companion September 2014 Low ResDocumento32 páginasCompanion September 2014 Low ReslybrakissAún no hay calificaciones
- How-To-April-2014 Companion How To Manage Urethral in Dogs Urethral ObstructionDocumento6 páginasHow-To-April-2014 Companion How To Manage Urethral in Dogs Urethral ObstructionlybrakissAún no hay calificaciones
- How To February 2014 Anesteziezi o PasareDocumento6 páginasHow To February 2014 Anesteziezi o PasarelybrakissAún no hay calificaciones
- How-To-August-2014 2014how To Deal With A Patient With Thermal BurnsImmediateDocumento5 páginasHow-To-August-2014 2014how To Deal With A Patient With Thermal BurnsImmediatelybrakissAún no hay calificaciones
- Companion July 2014 Low ResDocumento36 páginasCompanion July 2014 Low ReslybrakissAún no hay calificaciones
- Companion August 2014 Low ResDocumento36 páginasCompanion August 2014 Low ReslybrakissAún no hay calificaciones
- Micros 60 CS-CT User's ManualDocumento124 páginasMicros 60 CS-CT User's ManualHenry VelásquezAún no hay calificaciones
- Hematologic Tests Explained: Hemoglobin, Hematocrit & Interfering FactorsDocumento12 páginasHematologic Tests Explained: Hemoglobin, Hematocrit & Interfering FactorsMark Jireck AndresAún no hay calificaciones
- SuriDocumento5 páginasSurikevins chiloAún no hay calificaciones
- Horiba ABX Micros 60 - User Manual PDFDocumento136 páginasHoriba ABX Micros 60 - User Manual PDFkang opik100% (1)
- Haematology Diagnosis-Army USADocumento205 páginasHaematology Diagnosis-Army USAManuela BotisAún no hay calificaciones
- Normal Laboratory ValuesDocumento8 páginasNormal Laboratory ValuesStephanieAún no hay calificaciones
- Complete Blood Picture: Test Name Value Units Reference Range 3.44 7.4 76 22 28.5Documento107 páginasComplete Blood Picture: Test Name Value Units Reference Range 3.44 7.4 76 22 28.5anil tanankiAún no hay calificaciones
- Micros ES60Documento200 páginasMicros ES60VictorAún no hay calificaciones
- ICSH Recommendations For The Standardization of Peripheral Blood Cell Morphological Features PDFDocumento17 páginasICSH Recommendations For The Standardization of Peripheral Blood Cell Morphological Features PDFAbas Suherli100% (1)
- Flagging XT Series: Product Specialist PT. Saba IndomedikaDocumento58 páginasFlagging XT Series: Product Specialist PT. Saba IndomedikaDiah Puspita RiniAún no hay calificaciones
- Hematology Reference RangeDocumento1 páginaHematology Reference RangeNheeya WarzAún no hay calificaciones
- Basic HematologyDocumento89 páginasBasic Hematologydrafq2000Aún no hay calificaciones
- Byagagaire - Xylazine Hydrochloride and Ketamine Hydrochloride Combinations For General Anaesthesia in SheepDocumento182 páginasByagagaire - Xylazine Hydrochloride and Ketamine Hydrochloride Combinations For General Anaesthesia in SheepThamil ArasanAún no hay calificaciones
- Age-Related Hematology and Biochemistry in Purnathadi BuffaloDocumento6 páginasAge-Related Hematology and Biochemistry in Purnathadi Buffaloprajakta kuralkarAún no hay calificaciones
- Afriani2018-Fe Dan ZincDocumento6 páginasAfriani2018-Fe Dan ZincTitin FirawiwiraraAún no hay calificaciones
- Research Proposal/Synopsis For M.S Thesis Department of BiologyDocumento22 páginasResearch Proposal/Synopsis For M.S Thesis Department of BiologyBasit KhanAún no hay calificaciones
- Approach To The Child With AnemiaDocumento9 páginasApproach To The Child With Anemiasack26_11_93Aún no hay calificaciones
- H-7021 Automated Hematology Analyzer Operation ManualDocumento54 páginasH-7021 Automated Hematology Analyzer Operation ManualMan Dai Nhan100% (1)
- XFA6100Documento5 páginasXFA6100AlexeyAún no hay calificaciones
- Hematology 1Documento5 páginasHematology 1jaish8904100% (1)
- Smoking Effects on Erythrocyte Indices in College StudentsDocumento6 páginasSmoking Effects on Erythrocyte Indices in College StudentsKimo ChiAún no hay calificaciones
- Polysitemia VeraDocumento3 páginasPolysitemia VeraedwinsyahAún no hay calificaciones
- RBC count and anemia tests explainedDocumento6 páginasRBC count and anemia tests explainedSharmaine Grace FlorigAún no hay calificaciones
- Spots For Hematology PracticalDocumento17 páginasSpots For Hematology PracticalPhysiology by Dr RaghuveerAún no hay calificaciones
- Hema I Chapter 11 - RBC IndicesDocumento15 páginasHema I Chapter 11 - RBC IndicesKumneger DereseAún no hay calificaciones
- RBC IndicesDocumento13 páginasRBC IndicespremAún no hay calificaciones
- Jurnal: PROFIL HEMATOLOGI TIKUS (Rattus Norvegicus) Galur Sprague-Dawley Jantan Umur 7 Dan 10 MingguDocumento10 páginasJurnal: PROFIL HEMATOLOGI TIKUS (Rattus Norvegicus) Galur Sprague-Dawley Jantan Umur 7 Dan 10 MingguZAQ 79Aún no hay calificaciones
- Full Blood Count Apr04, DR Eva RaikDocumento7 páginasFull Blood Count Apr04, DR Eva RaikDanielcc LeeAún no hay calificaciones
- Blood SmearDocumento7 páginasBlood SmearMarice Ferrufino SchmidtAún no hay calificaciones
- The Study On The Anti - Anemic Effect of Banana Peel Extract Against Gentamicin - Induced Anemic Male Albino RATS (Rattus Norvegicus)Documento32 páginasThe Study On The Anti - Anemic Effect of Banana Peel Extract Against Gentamicin - Induced Anemic Male Albino RATS (Rattus Norvegicus)Maraiah BautistaAún no hay calificaciones