Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Central Control of Body Weight and Appetite: J Clin Endocrinol Metab, November 2008, 93 (11) :S37-S50
Cargado por
Niar MarhaliTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Central Control of Body Weight and Appetite: J Clin Endocrinol Metab, November 2008, 93 (11) :S37-S50
Cargado por
Niar MarhaliCopyright:
Formatos disponibles
S U P P L E M E N T R e v i e w
Central Control of Body Weight and Appetite
Stephen C. Woods and David A. DAlessio
Departments of Psychiatry (S.C.W.) and Medicine (D.A.D.), University of Cincinnati, Cincinnati, Ohio 45237
Context: Energy balance is critical for survival and health, and control of food intake is an integral part of this process. This report reviews hormonal signals that influence food intake and their clinical applications. Evidence Acquisition: A relatively novel insight is that satiation signals that control meal size and adiposity signals that signify the amount of body fat are distinct and interact in the hypothalamus and elsewhere to control energy homeostasis. This review focuses upon recent literature addressing the integration of satiation and adiposity signals and therapeutic implications for treatment of obesity. Evidence Synthesis: During meals, signals such as cholecystokinin arise primarily from the GI tract to cause satiation and meal termination; signals secreted in proportion to body fat such as insulin and leptin interact with satiation signals and provide effective regulation by dictating meal size to amounts that are appropriate for body fatness, or stored energy. Although satiation and adiposity signals are myriad and redundant and reduce food intake, there are few known orexigenic signals; thus, initiation of meals is not subject to the degree of homeostatic regulation that cessation of eating is. There are now drugs available that act through receptors for satiation factors and which cause weight loss, demonstrating that this system is amenable to manipulation for therapeutic goals. Conclusions: Although progress on effective medical therapies for obesity has been relatively slow in coming, advances in understanding the central regulation of food intake may ultimately be turned into useful treatment options. (J Clin Endocrinol Metab 93: S37S50, 2008)
he past decade has seen an increasing recognition that a complex interplay exists between the central nervous system (CNS) and the activity of numerous organs involved in energy homeostasis. This requires the transmission of key information to the brain, and control of food intake is one component of energy balance where endocrine signaling from the periphery to the CNS has a particularly important role. Considered broadly, energy homeostasis consists of the interrelated processes integrated by the brain to maintain energy stores at appropriate levels for given environmental conditions. Energy homeostasis thus includes the regulation of nutrient levels in key storage organs (e.g. fat in adipose tissue and glycogen in the liver and elsewhere) as well as in the blood (e.g. blood glucose). To accomplish this, the brain receives continuous information about energy stores and fluxes in critical organs, about food that is
0021-972X/08/$15.00/0 Printed in U.S.A. Copyright 2008 by The Endocrine Society doi: 10.1210/jc.2008-1630 Received July 28, 2008. Accepted September 8, 2008.
being eaten and absorbed, and about basal and situational energy needs by tissues. The brain in turn controls tissues that have important roles in energy homeostasis, like the liver and musculoskeletal system, as well as the secretion of key metabolically active hormones, primarily through the autonomic nervous system. The brain is thus able to respond to ongoing as well as unanticipated demands via well-coordinated responses to prevent shortfalls in energy stores while maintaining biochemical homeostasis. This review focuses on hormonal and related signals that inform the brain of energy levels, thereby influencing energy intake and ultimately body weight. As a general rule, signals arising in the periphery that influence food intake and energy expenditure can be partitioned into two broad categories (Fig. 1) (13). One comprises the signals generated during meals that cause satiation (i.e. feelings of fullAbbreviations: AgRP, Agouti-related peptide; apo A-IV, Apolipoprotein A-IV; ARC, arcuate nucleus; CCK, cholecystokinin; DPP-IV, dipeptidyl peptidase IV; GI, gastrointestinal; GLP-1, glucagon-like peptide-1; GLP-1r, GLP-1 receptor; GRP, gastrin-releasing peptide; LHA, lateral hypothalamic area; MC3R, melanocortin 3 receptor; MC4R, melanocortin 4 receptor; MSH, -melanocyte-stimulating hormone; NMB, neuromedin B; NPY, neuropeptide-Y; POMC, proopiomelanocortin; PVN, paraventricular nuclei; PYY, peptide tyrosine-tyrosine.
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
jcem.endojournals.org
S37
S38
Woods and DAlessio
Central Control of Body Weight and Appetite
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
FIG. 1. Model summarizing different levels of control over energy homeostasis. During meals, signals such as CCK, GLP-1, and distension of the stomach that arise from the gut (stomach and intestine) trigger nerve impulses in sensory nerves traveling to the hindbrain. These satiation signals synapse with neurons in the nucleus of the solitary tract (NTS) where they influence meal size. Ghrelin from the stomach both acts on the vagus nerve and stimulates neurons in the ARC directly. Signals related to body fat content such as leptin and insulin, collectively called adiposity signals, circulate in the blood to the brain. They pass through the blood-brain barrier in the region of the ARC and interact with neurons that synthesize POMC or NPY and AgRP. ARC neurons in turn project to other hypothalamic areas including the PVN and the LHA. The net output of the PVN is catabolic and enhances the potency of satiation signals in the hindbrain. The net output of the LHA, on the other hand, is anabolic, suppressing the activity of the satiation signals. In this way body fat content tends to remain relatively constant over long intervals by means of changes of meal size.
ness that contribute to the decision to stop eating) and/or satiety (i.e. prolongation of the interval until hunger or a drive to eat reappears). The prototypical satiation signal is the duodenal peptide cholecystokinin (CCK), which is secreted in response to dietary lipid or protein and which activates receptors on local sensory nerves in the duodenum, sending a message to the brain via the vagus nerve that contributes to satiation. The second category includes hormones such as insulin and leptin that are secreted in proportion to the amount of fat in the body. These adiposity hormones enter the brain by transport through the blood-brain barrier and interact with specific neuronal receptors primarily in the hypothalamus to affect energy balance. Satiation and adiposity signals interact with other factors in the hypothalamus and elsewhere in the brain to control appetite and body weight, and they are the topic of this review. Body weight (adiposity) is a homeostatically regulated variable, and its long-term maintenance can only occur via a close linkage of energy intake to energy expenditure. This means that over long intervals, the amount of food consumed must provide energy equivalent to the amount of energy expended. Humans and most mammals acquire energy in discrete episodes or meals. For many modern-day humans, the impetus to begin a meal is rarely if ever based on a biological deficit or need such as insufficient glucose. Rather, appetite and hunger occur, and meals are initiated based on habit, time of day, specific social situations, convenience, or stress, factors that are not linked to energy needs and so are nonhomeostatic (4 6). Arguably, this
has been the case throughout human evolution as well, with the initiation of feeding governed by nonhomeostatic factors such as food availability or having a safe haven to eat. Thus, the homeostatic influence over food intake is often left to the control over how many calories are consumed once a meal begins; i.e. on meal size. Consistent with this, many of the secretions of the gastrointestinal (GI) tract during a meal, such as CCK, are proportional to the number of calories consumed, and some of these secretions function as satiation signals to the CNS to help limit meal size (see reviews in Refs. 79). In contrast to satiation signals that are phasically secreted during meals, adiposity signals are more tonically active, providing an ongoing message to the brain proportional to total body fat. Insulin is tonically secreted in basal amounts, with phasic increments occurring during meals, and both components of total insulin secretion (i.e. basal and meal-stimulated) are directly proportional to body fat (10). Leptin is secreted in direct proportion to body adiposity, following a diurnal pattern with less direct connection to meals than insulin (11). As an individual changes body weight through caloric restriction or overeating, the amounts of insulin and leptin secreted into the blood change in parallel, and this in turn is reflected as an altered signal of body fatness, tantamount to body energy stores, reaching the brain (13). These adiposity signals interact with anabolic and catabolic neural circuits, causing a change in sensitivity of the brain to satiation signals. For example, during food deprivation or dieting, reduced brain insulin/leptin signaling renders neural cir-
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
jcem.endojournals.org
S39
cuits controlling meal size less sensitive to satiation signals such as CCK. As a consequence, the homeostatic setting is geared for the intake of larger meals because more food must be consumed before a sufficient satiation signal is generated to stop eating. This situation of extra-large meals persists until body weight (and hence the insulin/leptin signal) returns to normal. Conversely, after excessive weight gain, the increased insulin/leptin brain signal results in increased sensitivity to satiation signals, and smaller meals are consumed until the excess weight is lost. A major dilemma facing clinicians and others involved in public health is the slippage in the latter limb of this homeostatic system that permits excessive energy storage, obesity, and the associated diseases of nutritional excess; e.g. diabetes, cardiovascular disease, and some cancers.
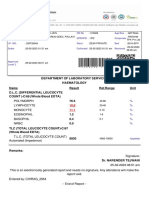
TABLE 1. GI hormones that affect satiation
Peptide CCK GLP-1 PYY Apo A-IV Enterostatin Bombesin/GRP/NMB Oxyntomodulin Amylin Ghrelin Effect on food intake Decrease Decrease Decrease Decrease Decrease Decrease Decrease Decrease Increase
Satiation Signals
By definition, satiation factors, when administered to humans or animals at the start of a meal, result in a smaller-than-normal meal being consumed. Exogenously administered satiation factors, or endogenous secretion of these compounds, activates specific receptors that cause premature cessation of eating. There are several excellent reviews of satiation signals such that only the salient points need to be reviewed here (79, 1214). It is generally accepted that for an endogenous compound to be considered a satiation signal, it is secreted in response to food ingestion, acts within the time frame of a single meal, reduces meal size without creating malaise or incapacitation, and is effective at physiological doses, and removing or antagonizing its endogenous activity increases meal size (7, 15). The best-established satiation signals are secreted from specialized enteroendocrine cells in the wall of the GI tract in response to the digestion and absorption of meals. In the classic model of satiation, local sensory nerves express receptors for these gut peptides as they are secreted such that the brain is immediately informed about the nutritional content of the meal by monitoring the level of hormones secreted to cope with it. As a complex meal is consumed, the mix of macronutrients (carbohydrates, fats, and proteins) stimulates a proportional blend of satiation peptides, and an overall message indicating meal content is integrated in the hindbrain where it activates appropriate responses, including ultimately cessation of the meal. In humans, this is associated with a sensation of fullness. Although not all intestinal hormones double as satiation signals, they all presumably contribute to the assimilation of nutrients; i.e. by stimulating the secretion of appropriate enzymes, water, and other compounds into the lumen of the gut and regulating GI motility. Table 1 provides a list of GI and other meal-related hormones/ peptides that are generally considered to be satiation signals. Cholecystokinin CCK was the compound first identified to fit the criteria for a satiation factor, so that much is known about its actions. Consequently, CCK has become the model for the larger class of satiation factors. When food containing fat or protein is consumed and enters the duodenum, CCK is secreted from I cells.
CCK enters the blood and has hormonal influences on gut motility, contraction of the gallbladder, pancreatic enzyme secretion, gastric emptying, and gastric acid secretion (16 19). However, CCK also diffuses locally to provide a paracrine stimulus to CCK-1 receptors on nearby branches of vagal sensory nerves (20 23). Through this mechanism a message, generally that ingested fat/protein is being processed and will soon be absorbed, is conveyed to the hindbrain and relayed to the hypothalamus where it is integrated into the composite information on energy homeostasis (20, 24 28) (Fig. 2). The decrease of meal size elicited by exogenous CCK is dosedependent, with higher doses causing greater reductions of meal size. However, CCK does not prevent meals from occurring; rather, it decreases the size of the meal once it has begun, reducing hunger and increasing fullness without concomitant sensations of illness or malaise. When a CCK-1 receptor antagonist is administered before the presentation of food to animals or humans, larger-than-normal meals are consumed (29 31), providing compelling evidence that endogenous CCK normally acts to sup-
FIG. 2. Satiation signals arising in the GI system converge on the dorsal hindbrain (D) where they are integrated with taste and other inputs. The dorsal hindbrain makes direct connections with the ventral hindbrain (V) where neural circuits direct the autonomic nervous system to influence blood glucose and where the motor control over eating behavior is located. The dorsal hindbrain also conveys information on satiation and other factors anteriorly to the hypothalamus and other brain areas. These areas in turn integrate satiation and adiposity signals as well as available nutrients with experience, the social situation and stressors, and with time of day and other factors. The integrated information is then conveyed posteriorly back to the ventral hindbrain as well as to the pituitary to influence all aspects of energy homeostasis. Animals lacking neural connections between the hindbrain and the hypothalamus reduce the intake of individual bouts of eating when the stomach is distended or they are administered CCK. However, those animals cannot regulate their body weight and are not sensitive to past experience, time of day, or social factors (243).
S40
Woods and DAlessio
Central Control of Body Weight and Appetite
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
press intake during meals. However, the effect of exogenous CCK is short-lived; the meal-reducing signal does not carry over to a second meal. Moreover, the effect of repeated or chronic administration of CCK (32, 33) has no effect on body weight because the short-term regulation of meal size is overridden by overall energy balance. That is, in the context of lower adiposity, leptin and insulin signals to the brain are reduced and satiation factors like CCK have a reduced effect to restrict meal size. There is strong experimental evidence supporting a role for CCK as a satiation factor in humans. CCK levels increase after meals, and infusion of an exogenous CCK-1 receptor agonist, CCK-33, to postprandial levels suppresses food intake (34, 35). Furthermore, infusion of a CCK-1 receptor antagonist to healthy humans causes an increase in caloric intake, strongly implicating endogenous CCK as a brake on meal size (29, 36). The effects of CCK-1 agonism and antagonism are similar in lean and obese humans and are associated with appropriate changes in hunger and fullness. Interestingly, blockade of CCK-1 receptors affects the postprandial responses of other GI hormones, attenuating the usual rise in peptide YY (PYY) and abolishing the suppression of ghrelin (37). This latter finding suggests that beyond directly inhibiting food intake, CCK acts as a proximal mediator of the broader satiation process. Two minor single nucleotide polymorphisms in the CCK-1 receptor gene promoter have been associated with increased body fatness, but the mechanism of this association has not been explained (38). Glucagon-like peptide-1 Glucagon-like peptide-1 (GLP-1) is derived from proglucagon in intestinal L cells that are most prevalent in the ileum and colon (39). GLP-1 secretion is elicited by nutrients, but the mechanism whereby the distal L cells are stimulated early within meals may require neurohumoral signals initiated in the proximal regions of the small intestine (40). GLP-1 has a broad range of actions on glucose metabolism (41), most prominently stimulation of insulin secretion, but also inhibition of glucagon release. Because GLP-1 inhibits GI motility and secretions, it has been implicated as a major component of the ileal brake, an inhibitory feedback mechanism that regulates transit of nutrients through the course of the GI tract (42, 43). It has generally been assumed that GLP-1 mediates these various actions through an endocrine mechanism, by binding directly to key target tissues like pancreatic islet cells. However, this mechanism has recently been called into question, in large part because GLP-1 is rapidly metabolized in the circulation by the protease dipeptidyl peptidase IV (DPP-IV) (44). Indeed, the half-life of GLP-1 in human plasma is only 12 min, and the product of DPP-IV action, a truncated GLP-1, is inactive with regard to glucose metabolism (45). Because the GLP-1 receptor (GLP-1r) is expressed by peripheral and CNS neurons as well as by cells in the pancreatic islets and the GI tract, recent attention has focused on neural mechanisms of GLP-1 action (46 48). GLP-1 administration reduces food intake in animals and humans (49 54), and these anorectic actions are thought to be mediated through both peripheral and central mechanisms. A population of neurons that synthesize GLP-1 is located in the brain stem and projects to hypothalamic and brain stem areas
important in the control of energy homeostasis (55, 56). Centrally administered GLP-1 reduces food intake through at least two mechanisms. GLP-1r in the hypothalamus appear to reduce intake by acting on caloric homeostatic circuits (57 60), whereas GLP-1r in the amygdala reduce food intake by eliciting symptoms of stress or malaise (61, 62). Systemically administered GLP-1 elicits satiation in healthy (53), obese (63), and diabetic (64, 65) humans. Because the halflife of active GLP-1 is less than 2 min, any direct effects are likely transient, and the reduction of food intake may result from inhibitory effects of GLP-1 on GI transit and reduced gastric emptying (66). However, peripherally administered GLP-1 does cross the blood-brain barrier (67), perhaps enabling circulating GLP-1 to interact with the brain GLP-1r. Because it both reduces food intake and stimulates insulin secretion, the GLP-1 system has been adapted to the treatment of type 2 diabetes (68, 69). DPP-IV-resistant, long-acting GLP-1r agonists are effective at reducing blood glucose in persons with type 2 diabetes and also cause weight loss (70). In addition, inhibitors of DPP-IV, which elevate endogenous GLP-1 levels, are also effective at improving glycemic control in diabetic patients (71, 72). The effect of chronic GLP-1r agonists to cause weight loss is not consistent with the general principle that satiation peptides are subservient to long-term regulators of energy balance, such as leptin (3). One potential explanation is that because GLP-1 can activate nonhomeostatic pathways that suppress food intake and otherwise reduce body weight, the effects of chronic administration of GLP-1r agonists work around the homeostatic systems controlling body weight. Indeed, nausea, a hallmark feature of nonhomeostatic anorexia, is very common with GLP-1r agonist treatment (73), although this response wanes with continued treatment and is not present in all persons who lose weight. Another possible explanation for why patients treated with indictable GLP-1r agonists lose weight is that repeated pharmacological doses of a satiation signal can overcome homeostatic restraints. Consistent with this hypothesis is the failure of DPP-IV inhibitor treatment, which has a smaller effect to raise circulating concentrations of GLP-1r agonist activity than do injectable GLP-1 mimetics to cause weight loss. Although it is not yet clear how GLP-1r agonists cause weight loss, the fact that they do challenges the current model of the interaction of satiation factors with overall energy homeostasis. Glicentin, GLP-2, oxyntomodulin, and glucagon Other peptides derived from the processing of proglucagon include glicentin, GLP-2, and oxyntomodulin, as well as glucagon itself (39). Glicentin inhibits gastric acid secretion (74), but at least in rats, does not affect food intake (75). In contrast, oxyntomodulin, a C-terminally extended congener of glucagon, does reduce food intake in animals when given centrally or peripherally (75, 76). Although a unique receptor for oxyntomodulin has yet to be identified, oxyntomodulin may exert its anorectic effect through the GLP-1r because subthreshold doses of the GLP-1r antagonist, exendin (9 39), block both GLP-1 and oxyntomodulin-induced reductions in food intake (75). Oxyntomodulin is thought to cross the blood-brain barrier and stimulate neurons in the arcuate nucleus (ARC) that express GLP-1r
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
jcem.endojournals.org
S41
and control energy homeostasis (77, 78). Long-term treatment with oxyntomodulin causes a persistent decrease in food intake and attenuated weight gain in rats (79). Interestingly, weight loss in animals given oxyntomodulin chronically is greater than what would be anticipated from reduced caloric intake (78), suggesting additional effects on energy expenditure. Short-term treatment with iv oxyntomodulin decreases hunger, reduces consumption of an ad libitum meal, and has an anorectic action that persists for 12 h after cessation of treatment in lean humans (80). Moreover, in obese subjects randomized to injections of oxyntomodulin or placebo before each meal for 4 wk, there was a significant loss of weight associated with active treatment. Oxyntomodulin caused an approximately 0.5 kg/wk reduction in body weight and was generally well tolerated. These findings suggest that at least two proglucagon products may have a role in the regulation of food intake. Distinguishing between the effects of GLP-1 and oxyntomodulin, in particular the relative in vivo actions on the GLP-1r, is an important next step in applying these compounds to clinical medicine. GLP-2 acts through a specific GLP-2 receptor to stimulate intestinal mucosal growth and has become the focus of research on short-bowel syndrome (81, 82). GLP-2 and GLP-1 have nearly 50% sequence homology and are secreted in parallel from perfused ileal preparations (83). Intracranial administration of GLP-2 reduces food intake in rats, and the effect can be blocked with a specific GLP-1r antagonist (84). More recent studies in humans found no effect of iv GLP-2 on food intake (85). Glucagon is the most widely studied hormone cleaved from preproglucagon (39). It is secreted from both pancreatic A cells and probably also in small amounts from the distal intestine. The best known action of glucagon is to increase hepatic glucose production by stimulating glycogenolysis and gluconeogenesis. Glucagon also reduces meal size when administered systemically (86, 87), but not centrally (88), the signal being detected in the liver and relayed to the brain (89). A role for glucagon in the normal control of meal size was demonstrated by the observation that blocking endogenous glucagon action in rats increases food intake (90, 91). There is little convincing evidence that glucagon plays a role in food intake in healthy humans. Peptide tyrosine-tyrosine (PYY) PYY is a member of a family of homologous peptides that also includes pancreatic polypeptide and neuropeptide-Y (NPY). Like proglucagon-derived peptides, PYY is synthesized and secreted by L cells in the distal ileum and colon (92). PYY is secreted as PYY (136) and is metabolized to PYY (336) by DPP-IV (93, 94). Receptors that mediate the effects of PYY, including reduction of food intake, belong to the NPY receptor family and include Y1, Y2, Y4, and Y5 (95). However, PYY (336) is a highly selective agonist activity for the Y2 receptor, and it also reduces food intake in humans and animals (96, 97). Like GLP-1, PYY has been implicated in GI motility and is considered a major component of the ileal brake (98, 99). Secretion of PYY is stimulated by food intake (100) and also by the presence of nutrients within the ileum itself (101); lipid seems to be a particularly effective stimulus. Similar to the case with GLP-1, it is not clear whether PYY release requires direct nutrient contact with L cells,
or if neurohumoral signals originating from the more proximal GI tract mediate the response. There is evidence that PYY influences food intake through its interaction with Y2 receptors in the ARC because it freely crosses the blood-brain barrier (102) and because systemic PYY (336) is ineffective in reducing food intake in the Y2-deficient mouse (103). Studies in humans have demonstrated that PYY signaling reduces food intake and that abnormalities in this system are present in obese subjects. PYY secretion is proportional to the caloric content of meals, with larger meals eliciting a significantly larger response (104, 105). Fasting and postprandial levels of PYY are lower in obese adults compared with lean controls (105, 106). The attenuated rise in PYY after eating has also been observed in obese adolescents (107). Infusion of PYY (336) into lean and obese humans reduced food consumption measured during test meals (104 106), although there remains some question as to whether this effect of PYY (336) is pharmacological or occurs at circulating levels seen after eating. Obese subjects did not differ in their sensitivity to PYY, and there was no difference in the relative PYY (136) and PYY (336) levels after exogenous administration. Taken together, these findings suggest that abnormal PYY production, rather than anorectic action of metabolism, could contribute to obesity. Interestingly, there is evidence that genetic variations in the PYY and Y2 sequences are associated with body weight. A common gene polymorphism in the Y2 receptor has been associated with a reduced likelihood of obesity in a cohort study of men with a broad range of BMI (108). Additionally, in a survey of lean and very obese men, a polymorphism in the PYY allele was found to segregate with increased body weight; this genetic variant of PYY was also found to have reduced binding to its receptor and an attenuated anorectic effect in mice (109). In total, the data collected in human studies support a role for PYY in the regulation of food intake and build the strongest case for any of the satiation factors in the pathogenesis of obesity. Apolipoprotein A-IV Apolipoprotein A-IV (apo A-IV) is synthesized by intestinal mucosal cells during the packaging of digested lipids into chylomicrons that subsequently enter the blood via the lymphatic system (110). Apo A-IV is also synthesized in the ARC (111). Systemic or central administration of apo A-IV reduces food intake and body weight of rats (112), and administration of apo A-IV antibodies increases food intake (113). Apo A-IV appears to work by interacting with the CCK signal (114). Because both intestinal and hypothalamic apo A-IV are regulated by absorption of lipid but not carbohydrate (115), this peptide may be an important link between short- and long-term regulators of body fat (see review by Tso and Liu in Ref. 116). Enterostatin A second digestion-related peptide, enterostatin, is also closely tied to intestinal processing of lipid. The exocrine pancreas secretes lipase and colipase to aid in the digestion of fat, and enterostatin, a pentapeptide, is cleaved from colipase in the intestinal lumen and enters the circulation. Administration of exogenous enterostatin either systemically (117, 118) or directly
S42
Woods and DAlessio
Central Control of Body Weight and Appetite
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
into the brain (119) reduces food intake, and, when rats are given a choice of foods, the reduction is specific for fats; that is, enterostatin does not decrease the intake of carbohydrate or protein (120). Therefore, two peptides that are secreted from the gut during the digestion and absorption of lipids, apo A-IV and enterostatin, act as signals that decrease food intake, and at least one of them selectively reduces the intake of fat. Macronutrient specificity has not been assessed with apo A-IV. There are no data from human studies to confirm the findings with apo A-IV and enterostatin on food intake. Bombesin-family peptides Members of the bombesin family of peptides including bombesin itself (an amphibian peptide) and its mammalian analogs, gastrin-releasing peptide (GRP) and neuromedin B (NMB), reduce food intake when administered systemically in humans and animals or into the CNS of animals (121123). Consistent with the possibility that these peptides act endogenously to reduce food intake, mice deficient for the GRP receptor eat significantly larger meals and develop late-onset obesity (124). Whereas most satiation factors act by reducing the size of an ongoing meal (4), bombesin peptides are an interesting exception in that when they are administered between meals, they increase the amount of time until the subsequent meal begins; i.e. they increase satiety as well as satiation (125, 126). Both bombesin and GRP reduce food intake when infused into human subjects (127, 128). Antagonism of endogenous bombesin receptors has demonstrable effects on gastric, intestinal, and gallbladder function but has not been studied with regard to food intake (129, 130). Therefore the case for GRP as a physiological mediator of satiation in humans is not as strong as for CCK. Amylin Amylin (also called islet amyloid polypeptide) is a peptide hormone secreted by pancreatic B cells in tandem with insulin secretion, which inhibits gastric emptying and gastric acid secretion, lowers glucagon concentrations, and reduces food intake (131). Amylin causes a dose-dependent reduction of meal size when administered systemically or directly into the brain (132136), and antagonism of amylin action in the CNS causes increased food intake and body weight (137). Consistent with this, targeted deletion of the amylin gene causes increased body weight in mice. Amylin signals through the calcitonin receptor when it has been modified by receptor activity modifying proteins (138, 139), and in contrast to many satiation peptides that reduce food intake by stimulating the visceral afferent nerves, amylin seems to act as a hormone, directly stimulating neurons in the area postrema in the hindbrain (133, 140). In fact, the anorectic action of amylin shares features with both satiation signals (phasic, meal-induced secretion) and adiposity signals (chronic interruption of action in rodents causes increased body fatness). Amylin seems to interact with both types of regulation in that the ability of amylin to reduce meal size is augmented when brain insulin action is elevated (141) and the effects of CCK and bombesin are muted in the absence of amylin signaling (142).
Amylin has been developed as a therapeutic, with the synthetic analog pramlintide now available for the treatment of type 1 and type 2 diabetes and clinical trials under way to determine the efficacy in treating obesity. In diabetic patients treated with pramlintide for 1 yr, weight loss averaged approximately 2 kg relative to placebo-treated controls (143, 144). Similar to treatment with the GLP-1r agonist exendin-4, pramlintide presents supraphysiological levels of amylin-like activity to patients, and the primary side effect is nausea. Nonetheless, the clinical experience with pramlintide supports the idea that chronic activity of a satiating compound can cause weight loss. Ghrelin Ghrelin, a product of specific endocrine cells in the stomach and duodenum, actually stimulates food intake and is the most potent known circulating orexigen (145). Ghrelin is secreted from the fundic region of the stomach and has been identified as the endogenous ligand for the GH secretagogue receptor. Fasting increases plasma ghrelin (146), and exogenous ghrelin increases food intake when administered peripherally or centrally (147 149). Ghrelin has also been linked to the anticipatory aspects of meal ingestion because levels peak shortly before scheduled meals in humans and rats (150) and fall shortly after meals end. Moreover, elevated ghrelin has been linked to the hyperphagia and obesity of individuals with the Prader-Willi syndrome (151). Ghrelin is also unique among the GI signals in that its message appears to be conveyed directly to receptors in the hypothalamus (152155), although, as is the case for CCK, GLP-1, and other GI signals, there are ghrelin receptors on vagal sensory nerves (156) but they do not appear to signal satiation (157). Satiation signals: summary of general principles Satiation appears to be a complex phenomenon, mediated by a number of GI peptides. Although it is clear that the different satiation factors respond to specific nutrient stimuli (e.g. CCK to protein and fat, GLP-1 to carbohydrate and fat, PYY primarily to fat, and so on), it has not been proven that mixed meals of differing macronutrient content elicit the release of distinct cocktails of GI hormones. However, given the wide range of specific factors that seem to mediate satiation, it is logical to presume that this process is subject to highly refined regulation. Especially important is the modulation of the action of satiation by factors such as leptin and insulin that are responsive to body adiposity. This interaction is the critical site of endocrine regulation of eating and energy homeostasis. A key feature of the system regulating food intake is that most if not all of the peptides that are made in the GI tract and influence satiation are also synthesized in the brain. This includes CCK, GLP-1, GLP-2, oxyntomodulin, apo A-IV, GRP, NMB, PYY, and ghrelin. Exceptions are the pancreatic hormones that influence energy homeostasis (i.e. insulin, glucagon, and amylin) and the adipose tissue/stomach hormone leptin; and each of these latter hormones has long-term effects on body fat as well. The fact that so many peripheral signals that influence food intake are also synthesized locally in the brain raises the question of whether and how the same signals secreted from different places in the body interact. A simple generalization is that, if a peptide
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
jcem.endojournals.org
S43
reduces (or increases) food intake when administered systemically, it probably has the same action when administered centrally. With regard to changes of food intake, this is true of CCK, GLP-1, apo A-IV, GRP, NMB, PYY, and ghrelin. Interestingly, it is also generally true that peptide signals that are not synthesized in the brain nonetheless have the same effect on food intake when administered directly into the brain. This is true of leptin, insulin, and amylin, but not glucagon. It is worth contemplating why there is such a large imbalance among GI hormones that suppress and stimulate food intake; i.e. whereas numerous peptides secreted from the stomach and intestines decrease food intake, only one known factor, ghrelin, increases it. One possibility relates to the phenomenon of satiation itself and the benefits of meal termination. Meals end long before any physical limit of the stomach is reached. This is easily demonstrated when food is diluted with noncaloric bulk and animals increase the volume of food consumed to attain their normal caloric load (158, 159). It has therefore been argued that a primary function of satiation signals is to prevent the consumption of too many calories at one time, lest the influx of nutrients and substrates overwhelm the capacity of the animal to maintain homeostasis (5, 160). That is, an important role of the GI tract is to analyze and respond to the incoming macronutrients while a meal is being eaten, helping to preempt excessive challenges to biochemical homeostasis. A corollary to this role for satiation signals is that adequate food intake does not require much specific stimulation, only the absence of inhibitory signals for food intake combined with the presence of food. Until recently there was some question as to whether manipulation of meal size by factors activating the satiation system could have therapeutic efficacy for weight reduction. One possibility was that because the effects of satiation peptides are dependent on body adiposity, their action would become muted as food intake decreased due to homeostatic regulation of body energy stores. Evidence for this was demonstrated for the satiating action of CCK in genetically obese Zucker rats (161, 162), but not for rats rendered obese by lesions of the ventromedial hypothalamus (163). Furthermore, rats genetically prone to becoming obese when fed a high-fat diet (diet-induced obesity rats) are actually more sensitive to the satiating action of CCK both before and after becoming obese (164). Some strains of genetically obese mice are comparably as sensitive as lean controls (165), and CCK works well in obese humans when administered iv (166). Hence, there is no general principle with regard to sensitivity in obesity, at least with regard to CCK. There is evidence that the satiating action of GLP-1 is leptin-dependent (167). All of these observations were made with animals having relatively free access to their diets so that they could vary their meal patterns in the service of maintaining body fat; i.e. when individuals are constrained to eating only small meals, they compensate by eating more often, thereby maintaining daily caloric intake and body weight. This has been observed when CCK is administered before every meal in experimental animals; animals receiving this treatment eat smaller and more frequent meals while keeping body weight constant (33, 168). In contrast, if animals are constrained to eating only three meals a day and receive a satiating peptide at each mealtime, they cannot compensate and conse-
quently lose weight (169). The advent of long-acting formulations of GLP-1 and amylin, peptides that seem to have a role in satiation (170, 171), has resulted in weight loss (172, 173). However, at present it is not clear that the chronic effects of GLP-1 and amylin receptor agonists are entirely due to continued hypophagia as opposed to other, nonbehavioral actions of the compounds. Understanding how a chronic pharmacological stimulus to the satiation system lowers body weight is important for refining the models for normal energy homeostasis.
Adiposity Signals
Insulin from the pancreatic B cells and leptin from white adipocytes (as well as the stomach and other tissues) are each secreted in direct proportion to body fat. Both hormones are transported through the blood-brain barrier (174, 175) and gain access to neurons in the hypothalamus and elsewhere in the brain to influence energy homeostasis. Hence, neurons sensitive to insulin and/or leptin receive a signal directly proportional to the amount of fat in the body. Consistent with this, if exogenous insulin or leptin is added locally into the brain, the individual responds as if excess fat exists in the body; i.e. food intake is reduced and body weight is lost. Analogously, if either the leptin or the insulin signal is reduced locally in the brain, the individual responds as if insufficient fat is present in the body, more food is eaten, and the individual gains weight. There are many reviews of these phenomena (1, 2, 87, 176 178). An important distinction is that whereas satiation signals primarily influence how many calories are eaten during individual meals, adiposity signals are more directly related to how much fat the body carries and maintains. Developing novel compounds that interact directly with the normal detection of and response to adiposity signals would therefore seem a more promising therapeutic approach for obesity. A key question therefore is whether agonists for the leptin and/or insulin receptor would be viable targets for the pharmaceutical industry. One obstacle is that to be effective, any compound would have to gain access to key receptors in the brain, yet any such compound would most likely have to be administered systemically. Administering insulin systemically elicits hypoglycemia and other side effects, and hypoglycemia per se increases food intake (179 181), thus working against the therapeutic intent. Systemically administered insulin does result in reduced food intake when plasma glucose is prevented from decreasing in animal models (182, 183), but this would be difficult to achieve therapeutically. Alternatively, there are reports that some formulations of nasally administered insulin elicit reduced food intake and body weight in humans without altering plasma glucose (184, 185). Leptin does not have the same counterproductive systemic effects as insulin, and in fact improves insulin sensitivity and circulating lipoprotein concentrations in subjects with metabolic abnormalities associated with anti-HIV treatment (186). Moreover, chronic leptin treatment of patients with generalized lipodystrophy causes significant improvements of insulin resistance, hypertriglyceridemia, hepatic steatosis, and glucose metabolism (187), responses found across the spectrum of lipodystrophies.
S44
Woods and DAlessio
Central Control of Body Weight and Appetite
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
However, the results of clinical trials using leptin in healthy obese subjects have been variable, with significant weight loss, but not of a remarkable magnitude, and some bothersome side effects related to peptide administration. Insulin and leptin resistance characterize the obese state, meaning that more of each hormone is required to achieve a particular physiological effect than occurs in lean individuals. Individuals with diabetes cannot achieve a maximum insulin response because of defects in insulin secretion and insulin action. The insulin and leptin resistance that characterizes peripheral tissues in obesity is also manifested in the brain. For one thing, the transport of both hormones from the blood to the brain is compromised in obesity such that less signal reaches critical neurons (188 190), and the ability of those neurons to respond is also compromised. When insulin is administered locally into the brain near the hypothalamus, both genetically obese (191) and dietary obese individuals (192) have a reduced or absent reduction of food intake, and this is the case for leptin as well (193). Hence, an inability on the part of the brain to respond to signals indicating that there is excess fat in the body may be a contributing and/or confounding factor in obesity. An insulin mimetic that interacts with the insulin receptor and is efficacious when given orally or directly into the brain has been reported to reduce food intake and body weight in obese rodents (194, 195), but it evidently has problematic side effects.
Central Integrating Circuits
Although receptors for insulin and leptin are found in several discrete areas throughout the brain, many that are especially important for controlling energy homeostasis are localized in the ARC of the hypothalamus (Fig. 1). The ARC is ideally suited as a receptor site for body adiposity as well as for integration of diverse hormonal and neural signals because there is evidence that blood-borne molecules have relatively greater access to receptors there than to other brain areas, and this is thought to be due in part to a relatively leaky blood-brain barrier in the ARC (196, 197). Two categories of ARC neurons are particularly important. One synthesizes the prepropeptide, proopiomelanocortin (POMC), and in the ARC POMC is cleaved to -melanocytestimulating hormone (MSH) as a neurotransmitter. MSH acts at melanocortin 3 and melanocortin 4 receptors (MC3R and MC4R) on neurons in other hypothalamic areas and elsewhere in the brain to reduce food intake, and synthetic agonists for MC3R/MC4R are available that cause hypophagia and weight loss in experimental animals (see reviews in Refs. 1, 2, 196, and 198 202). The catabolic action of both leptin and insulin relies upon MSH signaling because administration of antagonists to MC3R/MC4R blocks each of their actions in the brain (203, 204). The second group of ARC neurons synthesizes and secretes two neuropeptides important in energy homeostasis, and their axons project to many of the same brain areas as POMC neurons. Agouti-related peptide (AgRP) is an antagonist at MC3R and MC4R (199) such that one action of these neurons is to counter the activity of POMC neurons. NPY acts at Y receptors to stim-
ulate food intake (205207). When either AgRP or NPY is administered chronically into the brain, body weight increases (202, 208 211). In fact, when a single dose of AgRP is administered into the brain near the ARC, food intake is increased for 1 wk or more (212, 213). Insulin and leptin each have a net effect to suppress the activity of NPY/AgRP neurons in the ARC. The POMC and NPY/AgRP neurons in the ARC share many important features. Each is the origin of tracts projecting to other hypothalamic and brain areas, the two tracts often occurring in parallel. The POMC-originating tract has an overall catabolic effect such that when it is more active food intake is reduced, energy expenditure is increased, and if prolonged, body fat is lost. Conversely, the NPY/AgRP-originating tract is anabolic, with heightened activity causing more food to be ingested and body fat to increase. Under normal conditions, both circuits are active such that a change of input that is either stimulatory or inhibitory to either type of neuron elicits rapid changes of many energetic parameters. In the acute situation, both food intake and plasma glucose are altered because the ARC influences circuits projecting to behavioral sites as well as autonomic circuits influencing hepatic glucose secretion and pancreatic insulin secretion (214 216). Another important aspect of the area including the ARC and nearby hypothalamic nuclei is that receptors for many of the satiation signals discussed above are expressed there; i.e. circulating ghrelin is thought to interact directly with ARC neurons (152), which are also directly or indirectly sensitive to changes of CCK, GLP-1, NMB, and apo A-IV. Because most of these peptides are made within the brain, the origin of molecules altering ARC activity may not be directly from the plasma as occurs with insulin, leptin, and ghrelin. Numerous circuits from the hindbrain satiation area and elsewhere in the brain project to the region of the ARC (25, 27, 217). Finally, ARC neurons are also sensitive to local levels of energy-rich nutrients, including glucose (218), some long-chain fatty acids e.g. oleic acid (219, 220), and some amino acids e.g. leucine (221). Thus, the ARC is situated to be sensitive to a wide array of signals important in energy regulation (216, 222224). It is directly sensitive to hormones whose secretion is proportional to body fat (insulin and leptin); it receives information on ongoing meals either directly or indirectly; and it is sensitive to local levels of nutrients. Importantly, numerous neuronal circuits interconnect the ARC and nearby hypothalamic areas with the nucleus of the solitary tract, enabling the hypothalamic homeostatic network to be constantly aware of ongoing GI activity while at the same time influencing brain stem autonomic areas projecting to the GI tract, liver, pancreas, and other tissues (25, 27, 225227). The ARC can therefore be considered as a key afferent as well as efferent area for the regulation of energy homeostasis. Although ARC neurons project throughout the brain, two nearby target areas are thought to be especially important. The paraventricular nuclei (PVN) express both MC3R/MC4R and various Y receptors, and PVN neurons in turn synthesize and secrete neuropeptides that have a net catabolic action, including CRH and oxytocin. Administration of exogenous CRH (228) or oxytocin (229) into the brain reduces food intake. Hence, a catabolic circuit exists in which an increase of body fat is associated
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
jcem.endojournals.org
S45
with increased insulin and leptin, increased MSH, and decreased NPY and AgRP activity, and consequently increased activity of CRH, oxytocin, and other catabolic signals; all of these lead in turn to reduced food intake and increased energy expenditure. The lateral hypothalamic area (LHA) has a contrasting profile from the PVN (230). It also receives direct inputs from the ARC, and it contains neurons that synthesize and secrete anabolic peptides, including melanin-concentrating hormone and the orexins. Administration of melanin-concentrating hormone (231, 232) or orexin agonists (233) increases food intake and body weight gain. The architecture and functioning of these opposing hypothalamic circuits therefore enables rapid and fine-tuned control over energy homeostasis because the brain can simultaneously turn up one system (e.g. catabolic or anabolic) while turning down the other.
influencing not only when meals occur but how much food is consumed as well. Only when extraneous factors are tightly controlled in laboratory animal experiments, or else when ingestion is precisely monitored and quantified over periods of days or weeks in free-feeding humans, do the effects of these homeostatic signals become apparent.
Acknowledgments
Address all correspondence and requests for reprints to: Stephen C. Woods, Department of Psychiatry, University of Cincinnati, 2170 East Galbraith Road, Cincinnati, Ohio 45237. E-mail: steve.woods@ psychiatry.uc.edu. This work was supported by National Institutes of Health Awards DK 17844 and DK 57900. Disclosure Summary: S.C.W. received lecture fees from Sanofi-Aventis and from Merck. D.A.D. received lecture fees from Merck, Takeda, and MannKind.
Integration of Satiation and Adiposity Signals
Total food intake each day is the sum of the intake in individual meals (including snacks). As discussed above, the time that meals are initiated is often under the control of nonhomeostatic influences (4, 5, 160, 234). Hence, whatever regulatory control exists for body weight must be exerted on how much is eaten in individual meals, and meal termination is consequently under the influence of satiation signals. The efficacy of satiation signals to terminate a meal varies with the amount of fat in the body as signaled to the brain by leptin and insulin. When an individual has been food restricted (or been on a diet) and loses weight, leptin and insulin secretion both decline, and a reduced adiposity signal reaches the ARC. This in turn lowers sensitivity to satiation signals such as CCK, and the consequence is that more food is eaten during meals before satiation or feeling full occurs. Conversely, individuals who have overeaten and gained weight have elevated levels of adiposity signals and enhanced sensitivity to satiation signals, reducing the trajectory of weight gain or even promoting weight loss. When low doses of leptin or insulin are infused directly into the brain near the ARC, they greatly enhance the ability of satiation signals to reduce food intake e.g. much less CCK or other satiation signals is required to terminate a meal (235241), and when the adiposity signal in the brain is reduced, satiation signals are less efficacious (242).
References
1. Schwartz MW, Woods SC, Porte Jr D, Seeley RJ, Baskin DG 2000 Central nervous system control of food intake. Nature 404:661 671 2. Woods SC, Seeley RJ, Porte Jr D, Schwartz MW 1998 Signals that regulate food intake and energy homeostasis. Science 280:1378 1383 3. Woods SC 2005 Signals that influence food intake and body weight. Physiol Behav 86:709 716 4. Strubbe JH, Woods SC 2004 The timing of meals. Psychol Rev 111:128 141 5. Woods SC 1991 The eating paradox: how we tolerate food. Psychol Rev 98:488 505 6. Woods SC, Ramsay DS 2007 Homeostasis: beyond Curt Richter. Appetite 49:388 398 7. Moran TH, Kinzig KP 2004 Gastrointestinal satiety signals II. Cholecystokinin. Am J Physiol 286:G183G188 8. Moran TH 2004 Gut peptides in the control of food intake: 30 years of ideas. Physiol Behav 82:175180 9. Strader AD, Woods SC 2005 Gastrointestinal hormones and food intake. Gastroenterology 128:175191 10. Polonsky KS, Given E, Carter V 1988 Twenty-four-hour profiles and pulsatile patterns of insulin secretion in normal and obese subjects. J Clin Invest 81: 442 448 11. Teff KL, Townsend RR 2004 Prolonged mild hyperglycemia induces vagally mediated compensatory increase in C-peptide secretion in humans. J Clin Endocrinol Metab 89:5606 5613 12. Kaplan JM, Moran TH 2004 Gastrointestinal signaling in the control of food intake. In: Stricker EM, Woods SC, eds. Handbook of behavioral neurobiology. Neurobiology of food and fluid intake. Vol. 4, no. 2. New York: Kluwer Academic/Plenum Publishing; 273303 13. Wren AM, Bloom SR 2007 Gut hormones and appetite control. Gastroenterology 132:2116 2130 14. Wren AM 2008 Gut and hormones and obesity. Front Horm Res 36:165181 15. Smith GP, Gibbs J 1992 The development and proof of the cholecystokinin hypothesis of satiety. In: Dourish CT, Cooper SJ, Iversen SD, Iversen LL, eds. Multiple cholecystokinin receptors in the CNS. Oxford, UK: Oxford University Press; 166 182 16. Chandra R, Liddle RA 2007 Cholecystokinin. Curr Opin Endocrinol Diabetes Obes 14:63 67 17. Grider JR 1994 Role of cholecystokinin in the regulation of gastrointestinal motility. J Nutr 124:1334S1339S 18. Raybould HE 2007 Mechanisms of CCK signaling from gut to brain. Curr Opin Pharmacol 7:570 574 19. Schwartz GJ, Moran TH, White WO, Ladenheim EE 1997 Relationships between gastric motility and gastric vagal afferent responses to CCK and GRP in rats differ. Am J Physiol 272:R1726 R1733 20. Edwards GL, Ladenheim EE, Ritter RC 1986 Dorsomedial hindbrain participation in cholecystokinin-induced satiety. Am J Physiol 251:R971R977 21. Lorenz DN, Goldman SA 1982 Vagal mediation of the cholecystokinin satiety effect in rats. Physiol Behav 29:599 604
Conclusion
The brain receives and integrates diverse information pertinent to the maintenance of energy homeostasis. Adiposity signals such as insulin and leptin act in the arcuate nuclei to provide a background tone, and this tone in turn determines the sensitivity of the brain to satiation signals influencing how much food is eaten at any one time. It is important to recognize that this homeostatic mechanism provides at most a background influence, and that it only subtly influences intake during any given meal. This is because social factors, palatability, habits, the presence of predators, stress, and many other factors are also always at work,
S46
Woods and DAlessio
Central Control of Body Weight and Appetite
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
22. Moran TH, Shnayder L, Hostetler AM, McHugh PR 1988 Pylorectomy reduces the satiety action of cholecystokinin. Am J Physiol 255:R1059 R1063 23. Moran TH, Baldessarini AR, Salorio CF, Lowery T, Schwartz GJ 1997 Vagal afferent and efferent contributions to the inhibition of food intake by cholecystokinin. Am J Physiol 272:R1245R1251 24. Berthoud HR, Earle T, Zheng H, Patterson LM, Phifer C 2001 Food-related gastrointestinal signals activate caudal brainstem neurons expressing both NMDA and AMPA receptors. Brain Res 915:143154 25. Berthoud HR 2007 Interactions between the cognitive and metabolic brain in the control of food intake. Physiol Behav 91:486 498 26. Rinaman L 2004 Hindbrain contributions to anorexia. Am J Physiol Regul Integr Comp Physiol 287:R1035R1036 27. Rinaman L 2007 Visceral sensory inputs to the endocrine hypothalamus. Front Neuroendocrinol 28:50 60 28. Rinaman L, Hoffman GE, Dohanics J, Le WW, Stricker EM, Verbalis JG 1995 Cholecystokinin activates catecholaminergic neurons in the caudal medulla that innervate the paraventricular nucleus of the hypothalamus in rats. J Comp Neurol 360:246 256 29. Beglinger C, Degen L, Matzinger D, DAmato M, Drewe J 2001 Loxiglumide, a CCK-A receptor antagonist, stimulates calorie intake and hunger feelings in humans. Am J Physiol 280:R1149 R1154 30. Hewson G, Leighton GE, Hill RG, Hughes J 1988 The cholecystokinin receptor antagonist L364,718 increases food intake in the rat by attenuation of endogenous cholecystokinin. Br J Pharmacol 93:79 84 31. Reidelberger RD, ORourke MF 1989 Potent cholecystokinin antagonist L-364,718 stimulates food intake in rats. Am J Physiol 257:R1512R1518 32. Crawley JN, Beinfeld MC 1983 Rapid development of tolerance to the behavioural actions of cholecystokinin. Nature 302:703706 33. West DB, Fey D, Woods SC 1984 Cholecystokinin persistently suppresses meal size but not food intake in free-feeding rats. Am J Physiol 246: R776 R787 34. Lieverse RJ, Jansen JB, Masclee AA, Lamers CB 1995 Satiety effects of a physiological dose of cholecystokinin in humans. Gut 36:176 179 35. Gutzwiller JP, Degen L, Matzinger D, Prestin S, Beglinger C 2004 Interaction between GLP-1 and CCK-33 in inhibiting food intake and appetite in men. Am J Physiol Regul Integr Comp Physiol 287:R562R567 36. Lieverse RJ, Jansen JB, Masclee AA, Rovati LC, Lamers CB 1994 Effect of a low dose of intraduodenal fat on satiety in humans: studies using the type A cholecystokinin receptor antagonist loxiglumide. Gut 35:501505 37. Degen L, Drewe J, Piccoli F, Grani K, Oesch S, Bunea R, DAmato M, Beglinger C 2007 Effect of CCK-1 receptor blockade on ghrelin and PYY secretion in men. Am J Physiol Regul Integr Comp Physiol 292:R1391R1399 38. Funakoshi A, Miyasaka K, Matsumoto H, Yamamori S, Takiguchi S, Kataoka K, Takata Y, Matsusue K, Kono A, Shimokata H 2000 Gene structure of human cholecystokinin (CCK) type-A receptor: body fat content is related to CCK type-A receptor gene promoter polymorphism. FEBS Lett 466:264 266 39. Holst JJ 1997 Enteroglucagon. Annu Rev Physiol 59:257271 40. Dube PE, Brubaker PL 2004 Nutrient, neural and endocrine control of glucagon-like peptide secretion. Horm Metab Res 36:755760 41. Drucker DJ, Nauck MA 2006 The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 368:1696 1705 42. Giralt M, Vergara P 1999 Glucagonlike peptide-1 (GLP-1) participation in ileal brake induced by intraluminal peptones in rat. Dig Dis Sci 44:322329 43. Nauck MA, Niedereichholz U, Ettler R, Holst JJ, Orskov C, Ritzel R, Schmiegel WH 1997 Glucagon-like peptide-1 inhibition of gastric emptying outweighs its insulinotropic effects in healthy humans. Am J Physiol 273:E981E988 44. Mentlein R 1999 Dipeptidyl-peptidase IV (CD26)role in the inactivation of regulatory peptides. Regul Pept 85:9 24 45. Vahl TP, Paty BW, Fuller BD, Prigeon RL, DAlessio DA 2003 Effects of GLP-1-(736)NH2, GLP-1-(737), and GLP-1- (9 36)NH2 on intravenous glucose tolerance and glucose-induced insulin secretion in healthy humans. J Clin Endocrinol Metab 88:17721779 46. Knauf C, Cani PD, Perrin C, Iglesias MA, Maury JF, Bernard E, Benhamed F, Gremeaux T, Drucker DJ, Kahn CR, Girard J, Tanti JF, Delzenne NM, Postic C, Burcelin R 2005 Brain glucagon-like peptide-1 increases insulin secretion and muscle insulin resistance to favor hepatic glycogen storage. J Clin Invest 115:3554 3563 47. Knauf C, Cani PD, Kim DH, Iglesias MA, Chabo C, Waget A, Colom A, Rastrelli S, Delzenne NM, Drucker DJ, Seeley RJ, Burcelin R 2008 Role of central nervous system glucagon-like peptide-1 receptors in enteric glucosesensing. Diabetes, 57:26032612 48. Vahl TP, Tauchi M, Durler TS, Elfers EE, Fernandes TM, Bitner RD, Ellis KS, Woods SC, Seeley RJ, Herman JP, DAlessio DA 2007 Glucagon-like pep-
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67. 68. 69.
70.
tide-1 (GLP-1) receptors expressed on nerve terminals in the portal vein mediate the effects of endogenous GLP-1 on glucose tolerance in rats. Endocrinology 148:4965 4973 Tang-Christensen M, Larsen PJ, Goke R, Fink-Jensen A, Jessop DS, Moller M, Sheikh SP 1996 Central administration of GLP-1-(736) amide inhibits food and water intake in rats. Am J Physiol 271:R848 R856 Turton MD, OShea D, Gunn I, Beak SA, Edwards CM, Meeran K, Choi SJ, Taylor GM, Heath MM, Lambert PD, Wilding JP, Smith DM, Ghatei MA, Herbert J, Bloom SR 1996 A role for glucagon-like peptide-1 in the central regulation of feeding see comments. Nature 379:69 72 Donahey JC, van Dijk G, Woods SC, Seeley RJ 1998 Intraventricular GLP-1 reduces short- but not long-term food intake or body weight in lean and obese rats. Brain Res 779:75 83 Naslund E, Gutniak M, Skogar S, Rossner S, Hellstrom PM 1998 Glucagonlike peptide 1 increases the period of postprandial satiety and slows gastric emptying in obese men. Am J Clin Nutr 68:525530 Gutzwiller JP, Goke B, Drewe J, Hildebrand P, Ketterer S, Handschin D, Winterhalder R, Conen D, Beglinger C 1999 Glucagon-like peptide-1: a potent regulator of food intake in humans. Gut 44:81 86 van Dijk G, Thiele TE, Donahey JCK, Campfield LA, Smith FJ, Burn P, Bernstein IL, Woods SC, Seeley RJ 1996 Central infusion of leptin and GLP-1 (736) amide differentially stimulate c-Fos-like immunoreactivity in the rat brain. Am J Physiol 271:R1096 R1100 Shughrue PJ, Lane MV, Merchenthaler I 1996 Glucagon-like peptide-1 receptor (GLP1-R) mRNA in the rat hypothalamus. Endocrinology 137: 5159 5162 Navarro M, Rodriquez de Fonseca F, Alvarez E, Chowen JA, Zueco JA, Gomez R, Eng J, Blazquez E 1996 Colocalization of glucagon-like peptide-1 (GLP-1) receptors, glucose transporter GLUT-2, and glucokinase mRNAs in rat hypothalamic cells: evidence for a role of GLP-1 receptor agonists as an inhibitory signal for food and water intake. J Neurochem 67:19821991 Kinzig KP, DAlessio DA, Seeley RJ 2002 The diverse roles of specific GLP-1 receptors in the control of food intake and the response to visceral illness. J Neurosci 22:10470 10476 Larsen PJ, Tang-Christensen M, Jessop DS 1997 Central administration of glucagon-like peptide-1 activates hypothalamic neuroendocrine neurons in the rat. Endocrinology 138:4445 4455 McMahon LR, Wellman PJ 1997 Decreased intake of a liquid diet in nonfood-deprived rats following intra-PVN injections of GLP-1 (736) amide. Pharmacol Biochem Behav 58:673 677 McMahon LR, Wellman PJ 1997 PVN infusion of GLP-1(736) amide suppresses feeding and drinking but does not induce conditioned taste aversions or alter locomotion in rats. Am J Physiol 274:R23R29 Seeley RJ, Blake K, Rushing PA, Benoit SC, Eng J, Woods SC, DAlessio D 2000 The role of CNS GLP-1-(736) amide receptors in mediating the visceral illness effects of lithium chloride. J Neurosci 20:1616 1621 Kinzig KP, DAlessio DA, Herman JP, Sakai RR, Vahl TP, Figueredo HF, Murphy EK, Seeley RJ 2003 CNS glucagon-like peptide-1 receptors mediate endocrine and anxiety responses to interoceptive and psychogenic stressors. J Neurosci 23:6163 6170 Naslund E, Barkeling B, King N, Gutniak M, Blundell JE, Holst JJ, Rossner S, Hellstrom PM 1999 Energy intake and appetite are suppressed by glucagon-like peptide-1 (GLP-1) in obese men. Int J Obes Relat Metab Disord 23:304 311 Toft-Nielsen MB, Madsbad S, Holst JJ 1999 Continuous subcutaneous infusion of glucagon-like peptide 1 lowers plasma glucose and reduces appetite in type 2 diabetic patients. Diabetes Care 22:11371143 Gutzwiller JP, Drewe J, Goke B, Schmidt H, Rohrer B, Lareida J, Beglinger C 1999 Glucagon-like peptide-1 promotes satiety and reduces food intake in patients with diabetes mellitus type 2. Am J Physiol 276:R1541R1544 Delgado-Aros S, Kim DY, Burton DD, Thomforde GM, Stephens D, Brinkmann BH, Vella A, Camilleri M 2002 Effect of GLP-1 on gastric volume, emptying, maximum volume ingested, and postprandial symptoms in humans. Am J Physiol 282:G424 G431 Kastin AJ, Akerstrom V, Pan W 2002 Interactions of glucagon-like peptide-1 (GLP-1) with the blood-brain barrier. J Mol Neurosci 18:714 Ahren B 2007 GLP-1-based therapy of type 2 diabetes: GLP-1 mimetics and DPP-IV inhibitors. Curr Diab Rep 7:340 347 Madsbad S, Krarup T, Deacon CF, Holst JJ 2008 Glucagon-like peptide receptor agonists and dipeptidyl peptidase-4 inhibitors in the treatment of diabetes: a review of clinical trials. Curr Opin Clin Nutr Metab Care 11: 491 499 Mafong DD, Henry RR 2008 Exenatide as a treatment for diabetes and obesity: implications for cardiovascular risk reduction. Curr Atheroscler Rep 10:55 60
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
jcem.endojournals.org
S47
71. Flatt PR, Bailey CJ, Green BD 2008 Dipeptidyl peptidase IV (DPP IV) and related molecules in type 2 diabetes. Front Biosci 13:3648 3660 72. Pei Z 2008 From the bench to the bedside: dipeptidyl peptidase IV inhibitors, a new class of oral antihyperglycemic agents. Curr Opin Drug Discov Devel 11:512532 73. Kim D, MacConell L, Zhuang D, Kothare PA, Trautmann M, Fineman M, Taylor K 2007 Effects of once-weekly dosing of a long-acting release formulation of exenatide on glucose control and body weight in subjects with type 2 diabetes. Diabetes Care 30:14871493 74. Kirkegaard P, Moody AJ, Holst JJ, Loud FB, Olsen PS, Christiansen J 1982 Glicentin inhibits gastric acid secretion in the rat. Nature 297:156 157 75. Dakin CL, Gunn I, Small CJ, Edwards CM, Hay DL, Smith DM, Ghatei MA, Bloom SR 2001 Oxyntomodulin inhibits food intake in the rat. Endocrinology 142:4244 4250 76. Dakin CL, Small CJ, Batterham RL, Neary NM, Cohen MA, Patterson M, Ghatei MA, Bloom SR 2004 Peripheral oxyntomodulin reduces food intake and body weight gain in rats. Endocrinology 145:26872695 77. Wynne K, Park AJ, Small CJ, Meeran K, Ghatei MA, Frost GS, Bloom SR 2006 Oxyntomodulin increases energy expenditure in addition to decreasing energy intake in overweight and obese humans: a randomised controlled trial. Int J Obes (Lond) 30:1729 1736 78. Wynne K, Bloom SR 2006 The role of oxyntomodulin and peptide tyrosine-tyrosine (PYY) in appetite control. Nat Clin Pract Endocrinol Metab 2:612 620 79. Dakin CL, Small CJ, Park AJ, Seth A, Ghatei MA, Bloom SR 2002 Repeated ICV administration of oxyntomodulin causes a greater reduction in body weight gain than in pair-fed rats. Am J Physiol Endocrinol Metab 283: E1173E1177 80. Cohen MA, Ellis SM, Le Roux CW, Batterham RL, Park A, Patterson M, Frost GS, Ghatei MA, Bloom SR 2003 Oxyntomodulin suppresses appetite and reduces food intake in humans. J Clin Endocrinol Metab 88:4696 4701 81. Drucker DJ 1999 Glucagon-like peptide 2. Trends Endocrinol Metab 10: 153156 82. Jeppesen PB 2003 Clinical significance of GLP-2 in short-bowel syndrome. J Nutr 133:37213724 83. Orskov C, Holst JJ, Knuhtsen S, Baldissera FG, Poulsen SS, Nielsen OV 1986 Glucagon-like peptides GLP-1 and GLP-2, predicted products of the glucagon gene, are secreted separately from pig small intestine but not pancreas. Endocrinology 119:14671475 84. Tang-Christensen M, Larsen PJ, Thulesen J, Romer J, Vrang N 2000 The proglucagon-derived peptide, glucagon-like peptide-2, is a neurotransmitter involved in the regulation of food intake. Nat Med 6:802 807 85. Schmidt PT, Naslund E, Gryback P, Jacobsson H, Hartmann B, Holst JJ, Hellstrom PM 2003 Peripheral administration of GLP-2 to humans has no effect on gastric emptying or satiety. Regul Pept 116:2125 86. Geary N 1998 Glucagon and the control of meal size. In: Smith GP, ed. Satiation. From gut to brain. New York: Oxford University Press; 164 197 87. Woods SC, Lutz TA, Geary N, Langhans W 2006 Pancreatic signals controlling food intake; insulin, glucagon, and amylin. Philos Trans R Soc Lond B Biol Sci 361:1219 1235 88. Woods SC, Lotter EC, McKay LD, Porte Jr D 1979 Chronic intracerebroventricular infusion of insulin reduces food intake and body weight of baboons. Nature 282:503505 89. Geary N, Le Sauter J, Noh U 1993 Glucagon acts in the liver to control spontaneous meal size in rats. Am J Physiol 264:R116 R122 90. Langhans W, Zieger U, Scharrer E, Geary N 1982 Stimulation of feeding in rats by intraperitoneal injection of antibodies to glucagon. Science 218:894 896 91. Le Sauter J, Noh U, Geary N 1991 Hepatic portal infusion of glucagon antibodies increases spontaneous meal size in rats. Am J Physiol 261:R162R165 92. Adrian TE, Bacarese-Hamilton AJ, Smith HA, Chohan P, Manolas KJ, Bloom SR 1987 Distribution and postprandial release of porcine peptide YY. J Endocrinol 113:1114 93. Grandt D, Schimiczek M, Beglinger C, Layer P, Goebell H, Eysselein VE, Reeve Jr JR 1994 Two molecular forms of peptide YY (PYY) are abundant in human blood: characterization of a radioimmunoassay recognizing PYY 136 and PYY 336. Regul Pept 51:151159 94. Mentlein R, Dahms P, Grandt D, Kruger R 1993 Proteolytic processing of neuropeptide Y and peptide YY by dipeptidyl peptidase IV. Regul Pept 49: 133144 95. Larhammar D 1996 Structural diversity of receptors for neuropeptide Y, peptide YY and pancreatic polypeptide. Regul Pept 65:165174 96. Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, Dakin CL, Wren AM, Brynes AE, Low MJ, Ghatei MA, Cone RD, Bloom SR 2002
97. 98. 99.
100.
101.
102.
103. 104.
105.
106.
107.
108.
109.
110. 111.
112.
113.
114.
115.
116. 117.
118.
119.
120.
Gut hormone PYY(336) physiologically inhibits food intake. Nature 418:650 654 Vincent RP, le Roux CW 2008 The satiety hormone peptide YY as a regulator of appetite. J Clin Pathol 61:548 552 Lin HC, Zhao XT, Wang L, Wong H 1996 Fat-induced ileal brake in the dog depends on peptide YY. Gastroenterology 110:14911495 Pironi L, Stanghellini V, Miglioli M, Corinaldesi R, De Giorgio R, Ruggeri E, Tosetti C, Poggioli G, Morselli Labate AM, Monetti N, Gozzetti G, Barbara L, Go VLW 1993 Fat-induced ileal brake in humans: a dose-dependent phenomenon correlated to the plasma levels of peptide YY. Gastroenterology 105:733739 Pfluger PT, Kampe J, Castaneda TR, Vahl T, DAlessio DA, Kruthaupt T, Benoit SC, Cuntz U, Rochlitz HJ, Moehlig M, Pfeiffer AF, Koebnick C, Weickert MO, Otto B, Spranger J, Tschop MH 2007 Effect of human body weight changes on circulating levels of peptide YY and peptide YY336. J Clin Endocrinol Metab 92:583588 Spiller RC, Trotman IF, Higgins BE, Ghatei MA, Grimble GK, Lee YC, Bloom SR, Misiewicz JJ, Silk DB 1984 The ileal brakeinhibition of jejunal motility after ileal fat perfusion in man. Gut 25:365374 Nonaka N, Shioda S, Niehoff ML, Banks WA 2003 Characterization of blood-brain barrier permeability to PYY336 in mouse. J Pharmacol Exp Ther 306:948 953 Batterham RL, Bloom SR 2003 The gut hormone peptide YY regulates appetite. Ann NY Acad Sci 994:162168 Degen L, Oesch S, Casanova M, Graf S, Ketterer S, Drewe J, Beglinger C 2005 Effect of peptide YY336 on food intake in humans. Gastroenterology 129: 1430 1436 le Roux CW, Batterham RL, Aylwin SJ, Patterson M, Borg CM, Wynne KJ, Kent A, Vincent RP, Gardiner J, Ghatei MA, Bloom SR 2006 Attenuated peptide YY release in obese subjects is associated with reduced satiety. Endocrinology 147:3 8 Batterham RL, Cohen MA, Ellis SM, Le Roux CW, Withers DJ, Frost GS, Ghatei MA, Bloom SR 2003 Inhibition of food intake in obese subjects by peptide YY336. N Engl J Med 349:941948 Stock S, Leichner P, Wong AC, Ghatei MA, Kieffer TJ, Bloom SR, Chanoine JP 2005 Ghrelin, peptide YY, glucose-dependent insulinotropic polypeptide, and hunger responses to a mixed meal in anorexic, obese, and control female adolescents. J Clin Endocrinol Metab 90:21612168 Lavebratt C, Alpman A, Persson B, Arner P, Hoffstedt J 2006 Common neuropeptide Y2 receptor gene variant is protective against obesity among Swedish men. Int J Obes (Lond) 30:453 459 Ahituv N, Kavaslar N, Schackwitz W, Ustaszewska A, Collier JM, Hebert S, Doelle H, Dent R, Pennacchio LA, McPherson R 2006 A PYY Q62P variant linked to human obesity. Hum Mol Genet 15:387391 Tso P, Liu M, Kalogeris TJ, Thomson AB 2001 The role of apolipoprotein A-IV in the regulation of food intake. Annu Rev Nutr 21:231254 Liu M, Doi T, Shen L, Woods SC, Seeley RJ, Zheng S, Jackman A, Tso P 2001 Intestinal satiety protein apolipoprotein AIV is synthesized and regulated in rat hypothalamus. Am J Physiol 280:R1382R1387 Fujimoto K, Fukagawa K, Sakata T, Tso P 1993 Suppression of food intake by apolipoprotein A-IV is mediated through the central nervous system in rats. J Clin Invest 91:1830 1833 Fujimoto K, Machidori H, Iwakiri R, Yamamoto K, Fujisaki J, Sakata T, Tso P 1993 Effect of intravenous administration of apolipoprotein A-IV on patterns of feeding, drinking and ambulatory activity in rats. Brain Res 608: 233237 Lo CM, Zhang DM, Pearson K, Ma L, Sun W, Sakai RR, Davidson WS, Liu M, Raybould HE, Woods SC, Tso P 2007 Interaction of apolipoprotein AIV with cholecystokinin on the control of food intake. Am J Physiol Regul Integr Comp Physiol 293:R1490 R1494 Liu M, Shen L, Doi T, Woods SC, Seeley RJ, Tso P 2003 Neuropeptide Y and lipid increase apolipoprotein AIV gene expression in rat hypothalamus. Brain Res 971:232238 Tso P, Liu M 2004 Apolipoprotein A-IV, food intake, and obesity. Physiol Behav 83:631 643 Okada S, York DA, Bray GA, Erlanson-Albertsson C 1991 Enterostatin (Val-Pro-Asp-Pro-Arg), the activation peptide of procolipase, selectively reduces fat intake. Physiol Behav 49:11851189 Shargill NS, Tsuji S, Bray GA, Erlanson-Albertsson C 1991 Enterostatin suppresses food intake following injection into the third ventricle of rats. Brain Res 544:137140 Mei J, Erlanson-Albertsson C 1992 Effect of enterostatin given intravenously and intracerebroventricularly on high-fat feeding in rats. Regul Pept 41:209 218 Okada S, York DA, Bray GA, Mei J, Erlanson-Albertsson C 1992 Differential
S48
Woods and DAlessio
Central Control of Body Weight and Appetite
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
121. 122.
123. 124.
125. 126.
127.
128.
129.
130.
131. 132.
133. 134. 135. 136. 137.
138.
139.
140.
141. 142.
143.
144.
145. 146.
inhibition of fat intake in two strains of rat by the peptide enterostatin. Am J Physiol 262:R1111R1116 Muurahainen NE, Kissileff HR, Pi-Sunyer FX 1993 Intravenous infusion of bombesin reduces food intake in humans. Am J Physiol 264:R350 R354 Ladenheim EE, Wirth KE, Moran TH 1996 Receptor subtype mediation of feeding suppression by bombesin-like peptides. Pharmacol Biochem Behav 54:705711 Stein LJ, Woods SC 1982 Gastrin releasing peptide reduces meal size in rats. Peptides 3:833 835 Ladenheim EE, Hampton LL, Whitney AC, White WO, Battey JF, Moran TH 2002 Disruptions in feeding and body weight control in gastrin-releasing peptide receptor deficient mice. J Endocrinol 174:273281 Stuckey JA, Gibbs J, Smith GP 1985 Neural disconnection of gut from brain blocks bombesin-induced satiety. Peptides 6:1249 1252 Rushing PA, Henderson RP, Gibbs J 1998 Prolongation of the postprandial intermeal interval by gastrin-releasing peptide 127 in spontaneously feeding rats. Peptides 19:175177 Lieverse RJ, Jansen JB, van de Zwan A, Samson L, Masclee AA, Rovati LC, Lamers CB 1993 Bombesin reduces food intake in lean man by a cholecystokinin-independent mechanism. J Clin Endocrinol Metab 76:14951498 Gutzwiller JP, Drewe J, Hildebrand P, Rossi L, Lauper JZ, Beglinger C 1994 Effect of intravenous human gastrin-releasing peptide on food intake in humans. Gastroenterology 106:1168 1173 Hildebrand P, Lehmann FS, Ketterer S, Christ AD, Stingelin T, Beltinger J, Gibbons AH, Coy DH, Calam J, Larsen F, Beglinger C 2001 Regulation of gastric function by endogenous gastrin releasing peptide in humans: studies with a specific gastrin releasing peptide receptor antagonist. Gut 49:2328 Degen LP, Peng F, Collet A, Rossi L, Ketterer S, Serrano Y, Larsen F, Beglinger C, Hildebrand P 2001 Blockade of GRP receptors inhibits gastric emptying and gallbladder contraction but accelerates small intestinal transit. Gastroenterology 120:361368 Ludvik B, Kautzky-Willer A, Prager R, Thomaseth K, Pacini G 1997 Amylin: history and overview. Diabet Med 14(Suppl 2):S9 S13 Chance WT, Balasubramaniam A, Zhang FS, Wimalawansa SJ, Fischer JE 1991 Anorexia following the intrahypothalamic administration of amylin. Brain Res 539:352354 Lutz TA 2006 Amylinergic control of food intake. Physiol Behav 89:465 471 Lutz TA, Del Prete E, Scharrer E 1994 Reduction of food intake in rats by intraperitoneal injection of low doses of amylin. Physiol Behav 55:891 895 Lutz TA, Geary N, Szabady MM, Del Prete E, Scharrer E 1995 Amylin decreases meal size in rats. Physiol Behav 58:11971202 Rushing PA, Hagan MM, Seeley RJ, Lutz TA, Woods SC 2000 Amylin: a novel action in the brain to reduce body weight. Endocrinology 141:850 853 Rushing PA, Hagan MM, Seeley RJ, Lutz TA, DAlessio DA, Air EL, Woods SC 2001 Inhibition of central amylin signaling increases food intake and body adiposity in rats. Endocrinology 142:5035 Martinez A, Kapas S, Miller MJ, Ward Y, Cuttitta F 2000 Coexpression of receptors for adrenomedullin, calcitonin gene-related peptide, and amylin in pancreatic -cells. Endocrinology 141:406 411 Christopoulos A, Christopoulos G, Morfis M, Udawela M, Laburthe M, Couvineau A, Kuwasako K, Tilakaratne N, Sexton PM 2003 Novel receptor partners and function of receptor activity-modifying proteins. J Biol Chem 278:32933297 Lutz TA, Senn M, Althaus J, Del Prete E, Ehrensperger F, Scharrer E 1998 Lesion of the area postrema/nucleus of the solitary tract (AP/NTS) attenuates the anorectic effects of amylin and calcitonin gene-related peptide (CGRP) in rats. Peptides 19:309 317 Rushing PA, Lutz TA, Seeley RJ, Woods SC 2000 Amylin and insulin interact to reduce food intake in rats. Horm Metab Res 32:62 65 Mollet A, Meier S, Grabler V, Gilg S, Scharrer E, Lutz TA 2003 Endogenous amylin contributes to the anorectic effects of cholecystokinin and bombesin. Peptides 24:9198 Whitehouse F, Kruger DF, Fineman M, Shen L, Ruggles JA, Maggs DG, Weyer C, Kolterman OG 2002 A randomized study and open-label extension evaluating the long-term efficacy of pramlintide as an adjunct to insulin therapy in type 1 diabetes. Diabetes Care 25:724 730 Hollander PA, Levy P, Fineman MS, Maggs DG, Shen LZ, Strobel SA, Weyer C, Kolterman OG 2003 Pramlintide as an adjunct to insulin therapy improves long-term glycemic and weight control in patients with type 2 diabetes: a 1-year randomized controlled trial. Diabetes Care 26:784 790 Wiedmer P, Nogueiras R, Broglio F, DAlessio D, Tschop MH 2007 Ghrelin, obesity and diabetes. Nat Clin Pract Endocrinol Metab 3:705712 Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, Weigle DS 2001 A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes 50:1714 1719
147. Asakawa A, Inui A, Kaga T, Yuzuriha H, Nagata T, Ueno N, Makino S, Fujimiya M, Niijima A, Fujino MA, Kasuga M 2001 Ghrelin is an appetitestimulatory signal from stomach with structural resemblance to motilin. Gastroenterology 120:337345 148. Wren AM, Small CJ, Abbott CR, Dhillo WS, Seal LJ, Cohen MA, Batterham RL, Taheri S, Stanley SA, Ghatei MA, Bloom SR 2001 Ghrelin causes hyperphagia and obesity in rats. Diabetes 50:2540 2547 149. Tscho p M, Smiley DL, Heiman ML 2000 Ghrelin induces adiposity in rodents. Nature 407:908 913 150. Drazen DL, Vahl TP, DAlessio DA, Seeley RJ, Woods SC 2006 Effects of a fixed meal pattern on ghrelin secretion: evidence for a learned response independent of nutrient status. Endocrinology 147:2330 151. Cummings DE, Clement K, Purnell JQ, Vaisse C, Foster KE, Frayo RS, Schwartz MW, Basdevant A, Weigle DS 2002 Elevated plasma ghrelin levels in Prader Willi syndrome. Nat Med 8:643 644 152. Cowley MA, Smith RG, Diano S, Tschop M, Pronchuk N, Grove KL, Strasburger CJ, Bidlingmaier M, Esterman M, Heiman ML, Garcia-Segura LM, Nillni EA, Mendez P, Low MJ, Sotonyi P, Friedman JM, Liu H, Pinto S, Colmers WF, Cone RD, Horvath TL 2003 The distribution and mechanism of action of ghrelin in the CNS demonstrates a novel hypothalamic circuit regulating energy homeostasis. Neuron 37:649 661 153. Lawrence CB, Snape AC, Baudoin FM, Luckman SM 2002 Acute central ghrelin and GH secretagogues induce feeding and activate brain appetite centers. Endocrinology 143:155162 154. Cummings DE 2006 Ghrelin and the short- and long-term regulation of appetite and body weight. Physiol Behav 89:71 84 155. Traebert M, Riediger T, Whitebread S, Scharrer E, Schmid HA 2002 Ghrelin acts on leptin-responsive neurones in the rat arcuate nucleus. J Neuroendocrinol 14:580 586 156. Date Y, Murakami N, Toshinai K, Matsukura S, Niijima A, Matsuo H, Kangawa K, Nakazato M 2002 The role of the gastric afferent vagal nerve in ghrelin-induced feeding and growth hormone secretion in rats. Gastroenterology 123:1120 1128 157. Arnold M, Mura A, Langhans W, Geary N 2006 Gut vagal afferents are not necessary for the eating-stimulatory effect of intraperitoneally injected ghrelin in the rat. J Neurosci 26:1105211060 158. Adolph EF 1947 Urges to eat and drink in rats. Am J Physiol 151:110 125 159. Janowitz HD, Grossman MI 1949 Effect of variations in nutritive density of food in dogs and rats. Am J Physiol 158:184 193 160. Woods SC, Strubbe JH 1994 The psychobiology of meals. Psychon Bull Rev 1:141155 161. McLaughlin CL, Baile CA 1979 Cholecystokinin, amphetamine and diazepam and feeding in lean and obese Zucker rats. Pharmacol Biochem Behav 10:8793 162. Niederau C, Meereis-Schwanke K, Klonowski-Stumpe H, Herberg L 1997 CCK resistance in Zucker obese versus lean rats. Regul Pept 70:97104 163. Kulkosky PJ, Breckenridge C, Krinsky R, Woods SC 1976 Satiety elicited by the C-terminal octapeptide of cholecystokinin-pancreozymin in normal and VMH-lesioned rats. Behav Biol 18:227234 164. Chandler PC, Wauford PK, Oswald KD, Maldonado CR, Hagan MM 2004 Change in CCK-8 response after diet-induced obesity and MC3/4-receptor blockade. Peptides 25:299 306 165. Strohmayer AJ, Smith GP 1981 Cholecystokinin inhibits food intake in genetically obese (C57BL/6j-ob) mice. Peptides 2:39 43 166. Pi-Sunyer X, Kissileff HR, Thornton J, Smith GP 1982 C-terminal octapeptide of cholecystokinin decreases food intake in obese men. Physiol Behav 29:627 630 167. Williams DL, Baskin DG, Schwartz MW 2006 Leptin regulation of the anorexic response to glucagon-like peptide-1 receptor stimulation. Diabetes 55:33873393 168. West DB, Greenwood MRC, Marshall KA, Woods SC 1987 Lithium chloride, cholecystokinin and meal patterns: evidence the cholecystokinin suppresses meal size in rats without causing malaise. Appetite 8:221227 169. West DB, Williams RH, Braget DJ, Woods SC 1982 Bombesin reduces food intake of normal and hypothalamically obese rats and lowers body weight when given chronically. Peptides 3:61 67 170. DAlessio DA, Vahl TP 2004 Glucagon-like peptide 1: evolution of an incretin into a treatment for diabetes. Am J Physiol Endocrinol Metab 286: E882E890 171. DAlessio DA, Vahl TP 2005 Utilizing the GLP-1 signaling system to treat diabetes: sorting through the pharmacologic approaches. Curr Diab Rep 5:346 352 172. Buse JB, Klonoff DC, Nielsen LL, Guan X, Bowlus CL, Holcombe JH, Maggs DG, Wintle ME 2007 Metabolic effects of two years of exenatide treatment on diabetes, obesity, and hepatic biomarkers in patients with type 2 diabetes:
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
jcem.endojournals.org
S49
173.
174. 175. 176. 177. 178. 179. 180. 181. 182. 183. 184.
185.
186.
187.
188.
189.
190.
191.
192.
193. 194.
195.
196.
197.
198. 199. 200.
an interim analysis of data from the open-label, uncontrolled extension of three double-blind, placebo-controlled trials. Clin Ther 29:139 153 Poon T, Nelson P, Shen L, Mihm M, Taylor K, Fineman M, Kim D 2005 Exenatide improves glycemic control and reduces body weight in subjects with type 2 diabetes: a dose-ranging study. Diabetes Technol Ther 7:467 477 Banks WA 2006 The blood-brain barrier as a regulatory interface in the gut-brain axes. Physiol Behav 89:472 476 Woods SC, Seeley RJ, Baskin DG, Schwartz MW 2003 Insulin and the bloodbrain barrier. Curr Pharm Des 9:795 800 Benoit SC, Clegg DJ, Seeley RJ, Woods SC 2004 Insulin and leptin as adiposity signals. Recent Prog Horm Res 59:267285 Friedman JM 2002 The function of leptin in nutrition, weight, and physiology. Nutr Rev 60:S1S14; discussion S68- 84:85 87 Seeley RJ, Woods SC 2003 Monitoring of stored and available fuel by the CNS: implications for obesity. Nat Rev Neurosci 4:901909 Grossman SP 1986 The role of glucose, insulin and glucagon in the regulation of food intake and body weight. Neurosci Biobehav Rev 10:295315 Langhans W 1996 Metabolic and glucostatic control of feeding. Proc Nutr Soc 55:497515 Lotter EC, Woods SC 1977 Injections of insulin and changes of body weight. Physiol Behav 18:293297 Nicolaidis S, Rowland N 1976 Metering of intravenous versus oral nutrients and regulation of energy balance. Am J Physiol 231:661 668 Vanderweele DA, Haraczkiewicz E, Van Itallie TB 1982 Elevated insulin and satiety in obese and normal weight rats. Appetite 3:99 109 Hallschmid M, Benedict C, Schultes B, Fehm HL, Born J, Kern W 2004 Intranasal insulin reduces body fat in men but not in women. Diabetes 53: 3024 3029 Hallschmid M, Benedict C, Born J, Fehm HL, Kern W 2004 Manipulating central nervous mechanisms of food intake and body weight regulation by intranasal administration of neuropeptides in man. Physiol Behav 83:55 64 Lee JH, Chan JL, Sourlas E, Raptopoulos V, Mantzoros CS 2006 Recombinant methionyl human leptin therapy in replacement doses improves insulin resistance and metabolic profile in patients with lipoatrophy and metabolic syndrome induced by the highly active antiretroviral therapy. J Clin Endocrinol Metab 91:26052611 Javor ED, Cochran EK, Musso C, Young JR, Depaoli AM, Gorden P 2005 Long-term efficacy of leptin replacement in patients with generalized lipodystrophy. Diabetes 54:1994 2002 Israel PA, Park CR, Schwartz MW, Green PK, Sipols AJ, Woods SC, Porte Jr D, Figewicz DP 1993 Effect of diet-induced obesity and experimental hyperinsulinemia on insulin uptake into CSF of the rat. Brain Res Bull 30:571575 Owen OE, Reichard GAJ, Boden G, Shuman C 1974 Comparative measurements of glucose, -hydroxybutyrate, acetoacetate, and insulin in blood and cerebrospinal fluid during starvation. Metabolism 23:714 Stein LJ, Dorsa DM, Baskin DG, Figlewicz DP, Ikeda H, Frankmann SP, Greenwood MR, Porte Jr D, Woods SC 1983 Immunoreactive insulin levels are elevated in the cerebrospinal fluid of genetically obese Zucker rats. Endocrinology 113:2299 2301 Ikeda H, West DB, Pustek JJ, Figlewicz DP, Greenwood MRC, Porte Jr D, Woods SC 1986 Intraventricular insulin reduces food intake and body weight of lean but not obese Zucker rats. Appetite 7:381386 Woods SC, DAlessio DA, Tso P, Rushing PA, Clegg DJ, Benoit SC, Gotoh K, Liu M, Seeley RJ 2004 Consumption of a high-fat diet alters the homeostatic regulation of energy balance. Physiol Behav 83:573578 Cota D, Matter EK, Woods SC, Seeley RJ 2008 The role of hypothalamic mTORC1 signaling in diet-induced obesity. J Neurosci 28:72027208 Air EL, Strowski MZ, Benoit SC, Conarello SL, Salituro GM, Guan XM, Liu K, Woods SC, Zhang BB 2002 Small molecule insulin mimetics reduce food intake and body weight and prevent development of obesity. Nat Med 8:179 183 Zhang B, Salituro G, Szalkowski D, Li Z, Zhang Y, Royo I, Vilella D, Diez MT, Pelaez F, Ruby C, Kendall RL, Mao X, Griffin P, Calaycay J, Zierath JR, Heck JV, Smith RG, Moller DE 1999 Discovery of a small molecule insulin mimetic with antidiabetic activity in mice. Science 284:974 977 Cone RD, Cowley MA, Butler AA, Fan W, Marks DL, Low MJ 2001 The arcuate nucleus as a conduit for diverse signals relevant to energy homeostasis. Int J Obes Relat Metab Disord 25(Suppl 5):S63S67 Peruzzo B, Pastor FE, Blazquez JL, Schobitz K, Pelaez B, Amat P, Rodriguez EM 2000 A second look at the barriers of the medial basal hypothalamus. Exp Brain Res 132:10 26 Ahima RS, Saper CB, Flier JS, Elmquist JK 2000 Leptin regulation of neuroendocrine systems. Front Neuroendocrinol 21:263307 Cone RD 2005 Anatomy and regulation of the central melanocortin system. Nat Neurosci 8:571578 Elmquist JK, Coppari R, Balthasar N, Ichinose M, Lowell BB 2005 Identi-
201. 202.
203.
204. 205.
206.
207.
208.
209. 210.
211.
212.
213.
214.
215. 216. 217. 218. 219.
220.
221. 222. 223.
224. 225.
226. 227. 228.
fying hypothalamic pathways controlling food intake, body weight, and glucose homeostasis. J Comp Neurol 493:6371 Schwartz MW, Porte Jr D 2005 Diabetes, obesity, and the brain. Science 307:375379 Morton GJ, Cummings DE, Baskin DG, Barsh GS, Schwartz MW 2006 Central nervous system control of food intake and body weight. Nature 443:289 295 Benoit SC, Air EL, Coolen LM, Strauss R, Jackman A, Clegg DJ, Seeley RJ, Woods SC 2002 The catabolic action of insulin in the brain is mediated by melanocortins. J Neurosci 22:9048 9052 Seeley R, Yagaloff K, Fisher S, Burn P, Thiele T, van DG, Baskin D, Schwartz M 1997 Melanocortin receptors in leptin effects. Nature 390:349 Stanley BG, Leibowitz SF 1984 Neuropeptide Y: stimulation of feeding and drinking by injection into the paraventricular nucleus. Life Sciences 35:26352642 Clark JT, Kalra PS, Crowley WR, Kalra SP 1984 Neuropeptide Y and human pancreatic polypeptide stimulate feeding behavior in rats. Endocrinology 115:427 429 Corp ES, Melville LD, Greenberg D, Gibbs J, Smith GP 1990 Effect of fourth ventricular neuropeptide Y and peptide YY on ingestive and other behaviors. Am J Physiol 259:R317R323 Zarjevski N, Cusin I, Vetter R, Rohner-Jeanrenaud F, Jeanrenaud B 1993 Chronic intracerebroventricular neuropeptide-Y administration to normal rats mimics hormonal and metabolic changes of obesity. Endocrinology 133: 17531758 Wilson BD, Ollmann MM, Barsh GS 1999 The role of agouti-related protein in regulating body weight. Mol Med Today 5:250 256 Vettor R, Zarjevski N, Cusin I, Johner-Jeanrenaud F, Jeanrenaud B 1994 Induction and reversibility of an obesity syndrome by intracerebroventricular neuropeptide Y administration to normal rats. Diabetologia 37:12021208 Ollmann M, Wilson B, Yang Y, Kerns J, Chen Y, Gantz I, Barsh G 1997 Antagonism of central melanocortin receptors in vitro and in vivo by agoutirelated protein. Science 278:135138 Hagan MM, Rushing PA, Pritchard LM, Schwartz MW, Strack AM, Van der Ploeg HT, Woods SC, Seeley RJ 2000 Long-term orexigenic effects of AgRP(83132) involve mechanisms other than melanocortin receptor blockade. Am J Physiol 279:R47R52 Hagan MM, Benoit SC, Rushing PA, Pritchard LM, Woods SC, Seeley RJ 2001 Immediate and prolonged patterns of agouti-related peptide-(83132)induced c-Fos activation in hypothalamic and extrahypothalamic sites. Endocrinology 142:1050 1056 Porte Jr D, Baskin DG, Schwartz MW 2005 Insulin signaling in the central nervous system: a critical role in metabolic homeostasis and disease from C. elegans to humans. Diabetes 54:1264 1276 Schwartz MW 2006 Central nervous system regulation of food intake. Obesity (Silver Spring) 14(Suppl 1):1S 8S Woods SC, Seeley RJ, Cota D 2008 Regulation of food intake through hypothalamic signaling networks involving mTOR. Annu Rev Nutr 28:295311 Berthoud HR 2002 Multiple neural systems controlling food intake and body weight. Neurosci Biobehav Rev 26:393 428 Levin BE 2006 Metabolic sensing neurons and the control of energy homeostasis. Physiol Behav 89:486 489 Lam TK, Pocai A, Gutierrez-Juarez R, Obici S, Bryan J, Aguilar-Bryan L, Schwartz GJ, Rossetti L 2005 Hypothalamic sensing of circulating fatty acids is required for glucose homeostasis. Nat Med 11:320 327 Obici S, Feng Z, Morgan K, Stein D, Karkanias G, Rossetti L 2002 Central administration of oleic acid inhibits glucose production and food intake. Diabetes 51:271275 Cota D, Proulx K, Woods SC, Seeley RJ 2006 Role of leucine in regulating food intake. Science 313:1236 1238 Cota D, Proulx K, Seeley RJ 2007 The role of CNS fuel sensing in energy and glucose regulation. Gastroenterology 132:2158 2168 Seeley RJ, York DA 2005 Fuel sensing and the central nervous system (CNS): implications for the regulation of energy balance and the treatment for obesity. Obes Rev 6:259 265 Fehm HL, Kern W, Peters A 2006 The selfish brain: competition for energy resources. Prog Brain Res 153:129 140 Berthoud HR 2006 Homeostatic and non-homeostatic pathways involved in the control of food intake and energy balance. Obesity (Silver Spring) 14(Suppl 5):197S200S Grill HJ, Kaplan JM 2002 The neuroanatomical axis for control of energy balance. Front Neuroendocrinol 23:2 40 Schwartz GJ 2006 Integrative capacity of the caudal brainstem in the control of food intake. Philos Trans R Soc Lond B Biol Sci 361:12751280 Richard D, Huang Q, Timofeeva E 2000 The corticotropin-releasing hor-
S50
Woods and DAlessio
Central Control of Body Weight and Appetite
J Clin Endocrinol Metab, November 2008, 93(11):S37S50
229.
230.
231.
232.
233. 234.
235.
mone system in the regulation of energy balance in obesity. Int J Obes Relat Metab Disord 24:S36 S39 Verbalis JG, Blackburn RE, Olson BR, Stricker EM 1993 Central oxytocin inhibition of food and salt ingestion: a mechanism for intake regulation of solute homeostasis. Regul Pept 45:149 154 Broberger C, De Lecea L, Sutcliffe JG, Hokfelt T 1998 Hypocretin/orexinand melanin-concentrating hormone-expressing cells form distinct populations in the rodent lateral hypothalamus: relationship to the neuropeptide Y and agouti gene-related protein systems. J Comp Neurol 402:460 474 Qu D, Ludwig DS, Gammeltoft S, Piper M, Pelleymounter MA, Cullen MJ, Mathes WF, Przypek R, Kanarek R, Maratos-Flier E 1996 A role for melaninconcentrating hormone in the central regulation of feeding behaviour. Nature 380:243247 Nahon JL 2006 The melanocortins and melanin-concentrating hormone in the central regulation of feeding behavior and energy homeostasis. C R Biol 329:623 638; discussion 653 655 Sweet DC, Levine AS, Billington CJ, Kotz CM 1999 Feeding response to central orexins. Brain Res 821:535538 Strubbe JH, van Dijk G 2002 The temporal organization of ingestive behaviour and its interaction with regulation of energy balance. Neurosci Biobehav Rev 26:485 498 Matson CA, Wiater MF, Kuijper JL, Weigle DS 1997 Synergy between
236. 237. 238.
239.
240.
241.
242.
243.
leptin and cholecystokinin (CCK) to control daily caloric intake. Peptides 18:12751278 Matson CA, Ritter RC 1999 Long-term CCK-leptin synergy suggests a role for CCK in the regulation of body weight. Am J Physiol 276:R1038 R1045 Riedy CA, Chavez M, Figlewicz DP, Woods SC 1995 Central insulin enhances sensitivity to cholecystokinin. Physiol Behav 58:755760 Emond M, Schwartz GJ, Ladenheim EE, Moran TH 1999 Central leptin modulates behavioral and neural responsivity to CCK. Am J Physiol 276: R1545R1549 Figlewicz DP, Stein LJ, West D, Porte Jr D, Woods SC 1986 Intracisternal insulin alters sensitivity to CCK-induced meal suppression in baboons. Am J Physiol 250:R856 R860 Ladenheim EE, Emond M, Moran TH 2005 Leptin enhances feeding suppression and neural activation produced by systemically administered bombesin. Am J Physiol Regul Integr Comp Physiol 289:R473R477 Morton GJ, Blevins JE, Williams DL, Niswender KD, Gelling RW, Rhodes CJ, Baskin DG, Schwartz MW 2005 Leptin action in the forebrain regulates the hindbrain response to satiety signals. J Clin Invest 115:703710 McMinn JE, Sindelar DK, Havel PJ, Schwartz MW 2000 Leptin deficiency induced by fasting impairs the satiety response to cholecystokinin. Endocrinology 141:4442 4448 Grill HJ, Smith GP 1988 Cholecystokinin decreases sucrose intake in chronic decerebrate rats. Am J Physiol 254:R853R856
También podría gustarte
- Rundown 26september - XLS'Documento4 páginasRundown 26september - XLS'Niar MarhaliAún no hay calificaciones
- Ishikawa IskemiaDocumento2 páginasIshikawa IskemiaNiar MarhaliAún no hay calificaciones
- Ishikawa Iskemia-DikonversiDocumento2 páginasIshikawa Iskemia-DikonversiNiar MarhaliAún no hay calificaciones
- WJG 16 2978 PDFDocumento13 páginasWJG 16 2978 PDFNiar MarhaliAún no hay calificaciones
- Intestinal PathophysiologyDocumento12 páginasIntestinal PathophysiologyNiar MarhaliAún no hay calificaciones
- Figure 1 Prevalence of Malnutrition Using The Pre-Set Definition and Five Screening ToolsDocumento1 páginaFigure 1 Prevalence of Malnutrition Using The Pre-Set Definition and Five Screening ToolsNiar MarhaliAún no hay calificaciones
- Modeling AutismDocumento15 páginasModeling AutismNiar MarhaliAún no hay calificaciones
- Skeletal Muscle Wasting Rev PDFDocumento13 páginasSkeletal Muscle Wasting Rev PDFNiar MarhaliAún no hay calificaciones
- RecomendationDocumento13 páginasRecomendationNiar MarhaliAún no hay calificaciones
- Hypokalemia MDRDocumento7 páginasHypokalemia MDRNiar MarhaliAún no hay calificaciones
- GIE Colonscopy Prep and Diet GuideDocumento4 páginasGIE Colonscopy Prep and Diet GuideNiar MarhaliAún no hay calificaciones
- Hypoalbumonemia in CKDDocumento9 páginasHypoalbumonemia in CKDNiar MarhaliAún no hay calificaciones
- The DASH Diet PlanDocumento50 páginasThe DASH Diet PlanNiar Marhali67% (3)
- Malnutrition in Acute Strok - ReviewDocumento8 páginasMalnutrition in Acute Strok - ReviewNiar MarhaliAún no hay calificaciones
- Weight Variation 2011 PDFDocumento5 páginasWeight Variation 2011 PDFNiar MarhaliAún no hay calificaciones
- Efek Konseling 2012 PDFDocumento5 páginasEfek Konseling 2012 PDFNiar MarhaliAún no hay calificaciones
- Nutrition For Respiratory Disease PDFDocumento46 páginasNutrition For Respiratory Disease PDFNiar MarhaliAún no hay calificaciones
- MikronutrienDocumento13 páginasMikronutrienNiar MarhaliAún no hay calificaciones
- Malnutrition in Acute Strok - ReviewDocumento8 páginasMalnutrition in Acute Strok - ReviewNiar MarhaliAún no hay calificaciones
- Body Weight in TBDocumento8 páginasBody Weight in TBNiar MarhaliAún no hay calificaciones
- Nutr Suppl 2011 PDFDocumento8 páginasNutr Suppl 2011 PDFNiar MarhaliAún no hay calificaciones
- D 800 Iu Indo 2009 PDFDocumento5 páginasD 800 Iu Indo 2009 PDFNiar MarhaliAún no hay calificaciones
- Dietary Antioxidant SupplementsDocumento6 páginasDietary Antioxidant SupplementsNiar MarhaliAún no hay calificaciones
- Natrium TuberculosisDocumento2 páginasNatrium TuberculosisNiar MarhaliAún no hay calificaciones
- Asimp Na 1950Documento13 páginasAsimp Na 1950Niar MarhaliAún no hay calificaciones
- Enteral Nutri On Copd PatientDocumento7 páginasEnteral Nutri On Copd PatientRod Rafael De LeonAún no hay calificaciones
- Update On Tuberculous Pleural EffusionDocumento8 páginasUpdate On Tuberculous Pleural EffusionChristian TabarezAún no hay calificaciones
- Antropoetri Pada LansiaDocumento9 páginasAntropoetri Pada LansiaNiar MarhaliAún no hay calificaciones
- Leptin and Energy MetabDocumento7 páginasLeptin and Energy MetabNiar MarhaliAún no hay calificaciones
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Lesson Plan For Grade 9Documento206 páginasLesson Plan For Grade 9Anonymous 7BpT9OWP100% (1)
- Assessment of The Heart and Neck VesselsDocumento7 páginasAssessment of The Heart and Neck Vesselsclyde i amAún no hay calificaciones
- GGL Pelvis DelimitareDocumento12 páginasGGL Pelvis DelimitareStefan AnaAún no hay calificaciones
- February 1998Documento16 páginasFebruary 1998Kennie Ramirez100% (1)
- Sex and Sexual FunctionDocumento9 páginasSex and Sexual FunctionimanolkioAún no hay calificaciones
- ArchDocumento73 páginasArchRebin AliAún no hay calificaciones
- AUBF Notes 1Documento9 páginasAUBF Notes 1ChiAún no hay calificaciones
- Electromiografia RevneurolDocumento14 páginasElectromiografia RevneurolCelia GodoyAún no hay calificaciones
- Morphology of CicadidaeDocumento108 páginasMorphology of CicadidaeKrisztina Margit HorváthAún no hay calificaciones
- Rgci Care Reports1677339022895Documento1 páginaRgci Care Reports1677339022895Akshay ChaudhryAún no hay calificaciones
- ZOOLOGyDocumento144 páginasZOOLOGytemp93630Aún no hay calificaciones
- Changes in The Body: What Is Puberty?Documento4 páginasChanges in The Body: What Is Puberty?Mitch MarananAún no hay calificaciones
- WWW - Tu-Chemnitz - de Informatik KI Scripts Ws0910 Neuron HHDocumento16 páginasWWW - Tu-Chemnitz - de Informatik KI Scripts Ws0910 Neuron HHkarlTronxoAún no hay calificaciones
- Tingkat Organisasi Tubuh Sistem OrganDocumento19 páginasTingkat Organisasi Tubuh Sistem OrgansanoizuAún no hay calificaciones
- Live Blood AnalysisDocumento8 páginasLive Blood Analysiswirasasmita.ygmail.com100% (4)
- B CellDocumento13 páginasB CellSrini VasanAún no hay calificaciones
- Recent Advances in ScoliosisDocumento356 páginasRecent Advances in ScoliosisJosé Ramírez100% (5)
- Ballantyne - The Massachusetts General Hospital Handbook ofDocumento229 páginasBallantyne - The Massachusetts General Hospital Handbook ofadyna_popa_79462000850% (2)
- Unit 6 Human Biology Biology Lecture NotesDocumento6 páginasUnit 6 Human Biology Biology Lecture NotesGrace Melissa ChoiAún no hay calificaciones
- Thyroid Function Tests: A Review: G. Shivaraj, B. Desai Prakash, V. Sonal, K. Shruthi, H. Vinayak, M. AvinashDocumento9 páginasThyroid Function Tests: A Review: G. Shivaraj, B. Desai Prakash, V. Sonal, K. Shruthi, H. Vinayak, M. Avinashbelakang rumahAún no hay calificaciones
- The Mindboggling WorkbookDocumento20 páginasThe Mindboggling WorkbookNikola Kljusev100% (2)
- Homeopathic Remedies For Hydronephrosis - Homeo ExpertDocumento7 páginasHomeopathic Remedies For Hydronephrosis - Homeo ExpertDr. Kazy Habibur RahmanAún no hay calificaciones
- Thyroid SwellingDocumento8 páginasThyroid SwellingDn Ezrinah Dn Esham50% (2)
- 2019 Pathophysiology Textbook Part2 ZsmuDocumento58 páginas2019 Pathophysiology Textbook Part2 ZsmuSagar KhairwalAún no hay calificaciones
- Holiday National Heroes Day: Ii. ContentDocumento4 páginasHoliday National Heroes Day: Ii. ContentLendel Mariz O. CepilloAún no hay calificaciones
- Biology Class 9 Revised Syllabus Break Up 2020-21-23Documento7 páginasBiology Class 9 Revised Syllabus Break Up 2020-21-23MohammadAún no hay calificaciones
- 8.1 Transport System in MammalsDocumento41 páginas8.1 Transport System in MammalsTheresa IzaAún no hay calificaciones
- Haemostasis: Case StudyDocumento19 páginasHaemostasis: Case StudyTusabe FredAún no hay calificaciones
- 6 Cardiac A&P WorkbookDocumento29 páginas6 Cardiac A&P WorkbookClayson BuftonAún no hay calificaciones
- Cardiolab: A Virtual Laboratory For The Analysis of Human Circulatory SystemDocumento18 páginasCardiolab: A Virtual Laboratory For The Analysis of Human Circulatory SystemCarito PulgarinAún no hay calificaciones