Documentos de Académico
Documentos de Profesional
Documentos de Cultura
A High
Cargado por
ARIF AHAMMEDTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
A High
Cargado por
ARIF AHAMMEDCopyright:
Formatos disponibles
a high-frequency antigen may be a challenge. Autologous donations should be encouraged.
Other sources of antigennegative blood may include family members and the rare donor registry. Fortunately, because these antigens do occur so frequently, it is rare to find a patient with an antibody to one of them. Antibodies to the so-called HTLA antigens also fall under this category. Although these antibodies are usually not clinically significant themselves, up to 25 percent of patients with an HTLA antibody also make clinically significant antibodies. 44 It is not necessary to determine the specificity of the HTLA antibody, but removal of these antibodies is usually necessary to identify any underlying alloantibodies. Some HTLA antibodies, notably anti-Ch and anti-Rg, may be neutralized by normal serum, which contains complement. Routine blood bank enzymes will destroy anti-Ch, -Rg, and -JMH, whereas anti-Kna and -McCa are destroyed by dithiothreitol (DTT).
Case Three: Antibody to a Low-Frequency Antigen
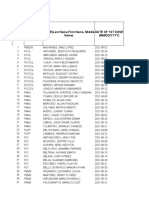
Low-frequency antigens are present in less than 10 percent of the population. Antibodies to these antigens are uncommon because exposure to the antigen is rare. The antibody screen will most likely be negative, therefore no panel will have been performed. Antibodies to these antigens should be suspected when an antiglobulin crossmatch is incompatible and other sources of explanation, such as ABO incompatibility or positive donor DAT, have been eliminated. These antibodies may also be suspected when an infant has a positive DAT and there is no known blood group discrepancy between mother and infant. Testing with additional antigen-positive cells will be required to confirm the specificity. Panel cells that are positive for these rare antigens are normally indicated on the panel profile sheet or listed on the extended typing form. In Figure 1217, positive reactions were seen only with cell 4 that matched the pattern of anti-Jsa. All other antibodies could be ruled out except for the other low-frequency, antiLua. Testing two other cells positive for the Jsa antigen to satisfy the 3 and 3 rule and phenotyping the patient for the Jsa antigen should be done to complete the antibody identification workup. If additional cells are not readily available, consult a reference laboratory. Because these antigens are infrequent, finding antigen-negative units for crossmatch is usually not difficult
Case Four: Cold-Reacting Autoantibodies
Most adult sera contain low titers of cold-reacting autoantibodies, most notably autoanti-I, -H, and -IH. These antibodies are usually IgM and of no clinical significance. They are troublesome in that they may interfere with the detection of significant antibodies, resulting in prolonged workups and delayed transfusions. Cold-reacting autoantibodies may be suspected when the screening cells, panel cells, and the autocontrol are all positive at the immediate spin phase and get weaker or disappear with incubation at 37_C (Fig. 1218). In this case, reactions were reduced at 37_C and were no longer apparent at the AHG phase. The use of cord blood cells, which lack the I antigen,
confirms the presence of anti-I in this sample. Certain autoantibodies may fix complement and are only detected at the AHG phase when using complement containing AHG reagent. These autoantibodies may be mistaken for weakly reacting IgG antibodies. Many laboratories avoid detection of cold autoantibodies by omitting the immediate spin phase of the antibody screen and by using monospecific anti-IgG Coombs serum. One of the least complex methods used to prevent
También podría gustarte
- Recipient Lymphocytotoxic HLA Antibodies To DonorDocumento2 páginasRecipient Lymphocytotoxic HLA Antibodies To DonorARIF AHAMMEDAún no hay calificaciones
- GlobulinDocumento2 páginasGlobulinARIF AHAMMEDAún no hay calificaciones
- When No HLADocumento2 páginasWhen No HLAARIF AHAMMEDAún no hay calificaciones
- Tested by RFLP Has To Do With The Fact That The Allele DesignationDocumento1 páginaTested by RFLP Has To Do With The Fact That The Allele DesignationARIF AHAMMEDAún no hay calificaciones
- RBCs LeukoreducedDocumento2 páginasRBCs LeukoreducedARIF AHAMMEDAún no hay calificaciones
- Four Possible HaplotypesDocumento1 páginaFour Possible HaplotypesARIF AHAMMEDAún no hay calificaciones
- Be Given When Selecting Positive Control Cells To Ensure ThatDocumento2 páginasBe Given When Selecting Positive Control Cells To Ensure ThatARIF AHAMMEDAún no hay calificaciones
- SerumDocumento2 páginasSerumARIF AHAMMEDAún no hay calificaciones
- On A Given ChromosomeDocumento1 páginaOn A Given ChromosomeARIF AHAMMEDAún no hay calificaciones
- Of The A and B Specificities Were Established Before The DiscoveryDocumento1 páginaOf The A and B Specificities Were Established Before The DiscoveryARIF AHAMMEDAún no hay calificaciones
- 37Documento2 páginas37ARIF AHAMMEDAún no hay calificaciones
- Platelet ConcentratesDocumento2 páginasPlatelet ConcentratesARIF AHAMMEDAún no hay calificaciones
- Tests Have Been Developed That Use A Biologic Response of LymphocytesDocumento2 páginasTests Have Been Developed That Use A Biologic Response of LymphocytesARIF AHAMMEDAún no hay calificaciones
- Approved in The United States For Treatment of Patients WithDocumento1 páginaApproved in The United States For Treatment of Patients WithARIF AHAMMEDAún no hay calificaciones
- B Lood Groups Were Discovered Over A Hundred YearsDocumento1 páginaB Lood Groups Were Discovered Over A Hundred YearsARIF AHAMMEDAún no hay calificaciones
- IntroductionDocumento2 páginasIntroductionARIF AHAMMEDAún no hay calificaciones
- Despite ThisDocumento2 páginasDespite ThisARIF AHAMMEDAún no hay calificaciones
- Intrauterine Exchange TransfusionDocumento2 páginasIntrauterine Exchange TransfusionARIF AHAMMEDAún no hay calificaciones
- SeventhDocumento2 páginasSeventhARIF AHAMMED PAún no hay calificaciones
- He Patient Was PregnantDocumento2 páginasHe Patient Was PregnantARIF AHAMMEDAún no hay calificaciones
- ChargesDocumento2 páginasChargesARIF AHAMMEDAún no hay calificaciones
- RBC AliquotsDocumento1 páginaRBC AliquotsARIF AHAMMEDAún no hay calificaciones
- Immune Serum GlobulinDocumento2 páginasImmune Serum GlobulinARIF AHAMMEDAún no hay calificaciones
- Cryoprecipitate Is The ColdDocumento2 páginasCryoprecipitate Is The ColdARIF AHAMMEDAún no hay calificaciones
- Laboratory Methods For The Diagnosis of Vibrio Cholerae Chapter 4Documento11 páginasLaboratory Methods For The Diagnosis of Vibrio Cholerae Chapter 4ARIF AHAMMEDAún no hay calificaciones
- Vhse MLT Standard ListDocumento8 páginasVhse MLT Standard ListARIF AHAMMEDAún no hay calificaciones
- BO/RhDocumento2 páginasBO/RhARIF AHAMMEDAún no hay calificaciones
- Nothing RelevantDocumento1 páginaNothing RelevantARIF AHAMMEDAún no hay calificaciones
- 10 Days BacteriologyDocumento1 página10 Days BacteriologyARIF AHAMMEDAún no hay calificaciones
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5782)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Artificial Intelligence AssignmentDocumento3 páginasArtificial Intelligence AssignmentAli musa baffaAún no hay calificaciones
- RMNCH Strategy English Version Final - 09mar16 PDFDocumento96 páginasRMNCH Strategy English Version Final - 09mar16 PDFKaran CourtneyAún no hay calificaciones
- Checklist for Linen Laundry AssessmentDocumento8 páginasChecklist for Linen Laundry AssessmentMarriz Bustaliño Tan75% (4)
- Diseases PIDSRDocumento25 páginasDiseases PIDSRaringkinking100% (1)
- Routine Infant Immunization Schedule in the PhilippinesDocumento2 páginasRoutine Infant Immunization Schedule in the PhilippinesknotstmAún no hay calificaciones
- EPEC PathogenDocumento6 páginasEPEC Pathogenuypaul97Aún no hay calificaciones
- QuesDocumento26 páginasQuesJoyce LauAún no hay calificaciones
- Epidemiology concepts and definitionsDocumento13 páginasEpidemiology concepts and definitionsPeter MainyaAún no hay calificaciones
- Genital Herpes: Causes, Symptoms, TreatmentDocumento2 páginasGenital Herpes: Causes, Symptoms, TreatmentEpi PanjaitanAún no hay calificaciones
- Essential Oils Phytochemicals Used For Treatment MRSA Diabetic Foot TBDocumento23 páginasEssential Oils Phytochemicals Used For Treatment MRSA Diabetic Foot TBSurgicalgownAún no hay calificaciones
- COVID-19 Proof of Vaccination - Preuve de Vaccination Contre La COVID-19Documento2 páginasCOVID-19 Proof of Vaccination - Preuve de Vaccination Contre La COVID-19NOS BEATSAún no hay calificaciones
- DHQ Manual Accounting FormatDocumento36 páginasDHQ Manual Accounting FormatMark PayumoAún no hay calificaciones
- Polio Field and Laboratory Surveillance Requirements in The Context of nOPV2 Use 20201218Documento30 páginasPolio Field and Laboratory Surveillance Requirements in The Context of nOPV2 Use 20201218francissimwinga08Aún no hay calificaciones
- Introduction To Oncology NursingDocumento35 páginasIntroduction To Oncology NursingDesh Deepak100% (1)
- KMITL English Exit ExamDocumento6 páginasKMITL English Exit ExamNARAWITH PUTTHAAún no hay calificaciones
- Situation Report: Rohingya Refugee Crisis: HighlightsDocumento19 páginasSituation Report: Rohingya Refugee Crisis: HighlightsShohag MahmudAún no hay calificaciones
- A Presentation OnDocumento21 páginasA Presentation OnSafeer ShibiAún no hay calificaciones
- BGHMC-NR Sample ChartingDocumento2 páginasBGHMC-NR Sample ChartingRI NA100% (2)
- Pathology Collaboration Drives InnovationDocumento1 páginaPathology Collaboration Drives Innovationmellier2468309Aún no hay calificaciones
- MICROBIOLOGY HOMEWORK SET B-AnswersDocumento7 páginasMICROBIOLOGY HOMEWORK SET B-AnswerschristinejoanAún no hay calificaciones
- The Relationship and Pathways Between Maternal Education and Child Nutritional StatusDocumento106 páginasThe Relationship and Pathways Between Maternal Education and Child Nutritional StatusWiljohn de la CruzAún no hay calificaciones
- CHN 002Documento17 páginasCHN 002betiful100% (6)
- History of Drug Discovery 1Documento7 páginasHistory of Drug Discovery 1Brent FontanillaAún no hay calificaciones
- Health Talk On VectorDocumento18 páginasHealth Talk On VectorZarifah Adilah Abdul RahmanAún no hay calificaciones
- Crimean-Congo Haemorrhagic Fever: CHAPTER 2.1.3BDocumento8 páginasCrimean-Congo Haemorrhagic Fever: CHAPTER 2.1.3BWormInchAún no hay calificaciones
- TablasneofaxDocumento67 páginasTablasneofaxFrancisco Tomas Lopez CabreraAún no hay calificaciones
- Fwd. Epi 8Documento40 páginasFwd. Epi 8Sumayya ChughtaiAún no hay calificaciones
- Dec. 13 Letter of Instruction From Peterborough Public Health To Food PremisesDocumento4 páginasDec. 13 Letter of Instruction From Peterborough Public Health To Food PremisesPeterborough ExaminerAún no hay calificaciones
- Sentence Correction MCQ Set 1Documento10 páginasSentence Correction MCQ Set 1Omer SaleemAún no hay calificaciones
- Communicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistDocumento846 páginasCommunicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistGrn Mynjrkxz100% (1)