Documentos de Académico
Documentos de Profesional
Documentos de Cultura
SABER-Nursing Care Plan #1 - JG
Cargado por
Jessica MontoyaDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
SABER-Nursing Care Plan #1 - JG
Cargado por
Jessica MontoyaCopyright:
Formatos disponibles
Page 1 of 7
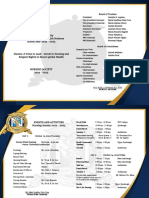
Nursing Care Plan
ASSOCIATE NURSING PROGRAM Student Name: ___Blanca Suarez________ Date: 10/23/2012 Instructor: ___Adria Diaz________ Clinical Site: ____Palmetto Hospital_______
Initial: J. Gonzalez Sex: M / F Date of Admission: 10/23 /2012
Patient Information DOB: 10/01/1947 Age: 65 Ethnic Group: White / AA / Hispanic / Asian Allergy: PCN HGT: 57 Weight: 220 lbs. Diet: NAS, low fat, regular
Admitting Diagnoses: 1) Congestive Heart Failure- CHF 2) Coronary Artery Disease- CAD 3) Acute decompensated heart failure- ADHF 4) Hypertension- HTN Past Medical History: Immunizations: influenza virus 10/01/2012, Tuberculosis 10/01/2012.
NKA. Hospitalizations: His medical history includes coronary artery disease x 10 years. He had a balloon angioplasty in 2000 and an M.I. in 1988. . CAD x 10 years. CHF x 5 years. MI 1990. This is his third admission for CHF since his diagnosis five years ago. Experienced an allergy to Penicillin; experienced rash and hives in 1985.
Past Surgical History:
Balloon Angioplasty (1 vessel) 10/2000 Status Post Cholycystectomy 1990 Status Post Appendectomy 1985 Status Post open repair and internal fixation of left femur fracture, 1983
NURSING CARE PLAN
Page 2 of 7
Social History: Retired accountant, college educational level, lives with eldest daughter E. Gonzalez, Hispanic, Catholic.
He is hearing impaired and wears bilateral hearing aids. He wears glasses and reads with some difficulty. 2 PPD x 40 years. Quit 1995. Denies ETOH, drug use.
Family history:
Mother 79, deceased of CAD. Father 54, deceased, heart attack. No brothers or sisters. There is a positive family history of hypertension, but no diabetes, or cancer.
History of Present Illness: J.G. was admitted with a diagnosis of chronic congestive heart failure (CHF) with acute exacerbation and Acute decompensated
heart failure (ADHF). Client became fatigued and presented to E.R. with increased SOB and dyspnea on exertion (DOE) c/o increasing fatigue and severe shortness of breath (SOB), orthopnea Sleeps with 3 pillows. Lower extremity edema.
Objective Finding Admission Vital Sign: BP: 176/96 HR: 103 Rhythm- Iregular S1-s2 mild heart murmur HR: 89 Coagulation
PT 11 secs PTT 65 secs
RR: 22
Temp: 98.6 Taken Oral route Temp: 98.5 Other: (U/A, ABGs, Protombin, etc)
Digoxin level 2.6 ng/mL Dilantin level 18 ug/mL Arterial PH 7.20 pCO2 30 mm Hg PO2 80% PaO2: 70 mm Hg HCO3: 21% mEq/l SaO2: 90%
Current Vital Sign: BP: 160/80 Laboratory Studies: CBC Metabolic Panel
WBC 5,000-10,000/mm3 RBCs 4.2-6.1 x 106/g Hgb 11.5-17.5 g/dl Hct 40-52%
RR: 21 Lipid Profile
Na+ 160 mEq/L K+ 3.3 mEq/L CL-- 102 mEq/L Ca+ 9.1 mg/ dl Serum albumin 2.8 g/dl Glucose 99 mg/dl Serum digoxin level 2.6 ng/dl Bun 30 mg/dl Cr 0.6 mg/dl Sodium 138 mEq/L Cloride 102 mEq/L Potassium 3.3 mEq/L Calcium 9.1 mg/dL Cholesterol <260 mg/dL
LDL 160-189 mg/dL HDL 60 mg/dL Cholesterol total 260 mg/dl Triglycerides 180 mg/dl
NURSING CARE PLAN
Page 3 of 7
Imaging Result: (X-Ray, CT scan, MRI, MRCP, ultrasound.)
10/01/2012- Chest x--ray--mild left ventricular hypertrophy; pulmonary congestion resolving. 07/01/2012- ECG- observable CAD, acute myocardial ischemia, left ventricular hypertrophy, conduction defects and dysrthymias. 06/01/2012- Left ventriculography- decreased LV function
Endoscopic Result: (colonoscopy, EGD..)
Endoscopic ultrasound (EUS) 07/01/2005 yielding positive results for swollen/inflamed appendix. Laparoscopy related to appendectomy, 07/01/2005: There is no blood in the abdomen, no hernias, no intestinal obstruction, and no cancer in any visible organs. The liver is normal.
Physical Assessment findings HEENT:
Oxygenation/breathing: labored breathing, moderate respiratory distress uses 3 pillows at night, c/o increased fatigue & SOB, crackles L base, wheezes, decreased breath sounds. General appearance- admitted in moderate respiratory distress. Circulation: S1, S2, Mild heart murmur, decreased elevated BP, dysrythmia. Capillary refill: Prolonged >3 secs. Pink nail bed color. Edema: Bilat. Ankle +2 pitting. Pacemaker: N/A. Homans Sign: Negative. Level of consciousness: Awake, alert Oriented x 4 (time, place, person, event). Behavior: Cooperative, anxious. PEERLA: Pupils Equal and Round; Reactive to Light and Accommodation, night vision visual difficulty, Hx of cataracts, visual loss, dry burning sensation in eyes, trouble reading. Conjunctiva & sclera moist, glossy, visible small blood vessels, yellow fat deposits under lids. Lacrimal gland, Lacrimal sac, Nasolacrimal duct No edema or tenderness over the lacrimal gland and no tearing. Eyelids and lashes: intact, no redness, no discharge, swelling or lesions, lashes evenly distributed and curve outward. Ears: external canal, tympanic membrane: shiny, translucent, pearly gray. The ear lobes are bean shaped, parallel, and symmetrical, the upper connection of the ear lobe is parallel with the outer cantus of the eye. No lesions noted on inspection, skin is same in color as in the complexion. The auricles firm cartilage on palpation. There is no pain or tenderness on the palpation of the auricles and mastoid process. The ear canal has normally some cerumen of inspection, no discharges or lesions. Nose: Symmetric and straight, no flaring, uniform in color, air moves freely as the clients breathes through the nares. Nasal Cavity: Mucosa is pink, no lesions and nasal septum intact and in middle with no tenderness. Neck: Easily moveable without resistance, no abnormal adenopathy in the cervical or supraclavicular areas. Trachea is midline and thyroid gland is normal without masses. Oral mucosa/tongue: pale, dry. Dentures Mouth: Symmetrical, pale lips, light pink gums and able to purse lips. Gag reflex: Present which is elicited through the use of a tongue depressor. Gastrointestinal: No complaints of dysphagia, nausea, vomiting, or change in stool pattern, consistency, or color. He complains of epigastric pain, burning in quality, approximately twice a month, which he notices primarily at night. Genitourinary: No complaints of dysuria, nocturia, polyuria, or hematuria. Abdomen: The abdomen is symmetrical with mild distention; bowel sounds are normal in quality and intensity in some areas; a bruit is heard in the right paraumbilical area. No masses or splenomegaly are noted; liver span is 8 cm by percussion. Extremities: mild cyanosis, no clubbing, mild edema are noted in lower extremities. Peripheral pulses in the femoral, popliteal, anterior tibial, dorsalis pedis, brachial, and radial areas are irregular. Nodes: No palpable nodes in the cervical, supraclavicular, axillary or inguinal areas.
NURSING CARE PLAN
Page 4 of 7
Medication List
Medication/Order Dose
Digoxin
Indication
Increase cardiac output
Usual Dose
QD 0.25 mg
Side effects
Headache, dysrhythmias, hypotension, AV block, blurred vision, yellow--green halos, Circulatory collapse, loss of hearing, hypokalemia, Hypochloremic alkalosis hyperglycemia, nausea, polyuria, renal failure, thrombocytopenia, anemia, rash pruritis, Postural hypotension, collapse, HA, flushing, dizziness N/V, anorexia, diarrhea, cramps
Nursing Intervention
Apical pulse 1 minute. Hold P < 60. Assess lytes, BUN/Cr, ALT, AST, H&H. I & O, daily wts, dig level. Assess client for s/s dehydration. adm in a.m. K+ replacement if < 3.0. adm. With food if nauseated.
Lasix
Decrease edema and blood pressure
PO BID 40 mg
Nitro--Bid (Nitroglycerin) Vasodilator (Nitrate) Metamucil (Psyllium)
Prevent chest pain; increase cardiac output Dilates Coronary arteries; decreases preload and afterload Prevent Constipation. Bulkforming laxative
2.5 mgs. P.O. QID
15 ml P. O. qHs
KCl Potassium supplement
Replace Potassium Needed for 20 mEq Transmission of nerve P. O. BID impulses and cardiac contraction
Cardiac depression, dysrhythmias, arrest, peak T waves, low R & RST, prolonged PR interval, wide QRS
Assess BP, pulse, pain. May develop tolerance. Adm. with 8 oz. H20 on empty stomach, 1 hr. before or 2 hrs. after Assess then adm. alone for better absorption. Give with 8 ozs of H20 followed by 8 oz. fluid Assess EKG, K+ level, I & after meal. Do not give IM or SQ powder, dissolve in 8 oz. cold water/juice
NURSING CARE PLAN
Page 5 of 7
Nursing Care Plan
Once evaluated patients past and present history, select at least three nursing diagnoses from highest to lowest priority. Give nursing interventions (dependent/independent/collaborative) for each nursing diagnoses with rational for each intervention. Determine a short and long term goal for each nursing diagnoses.
Nursing Diagnoses
(.related to...secondary to .evidenced by..)
Desired Outcome
Nursing Interventions / Rationales
ND1) Breathing Pattern, Ineffective Gas Exchange, Impaired
Short term goal: Within 30 min. of treatment/intervention, patient has adequate gas exchange, as evidenced by normal breath sounds and skin color, HR 100 bpm or less, Pao2 80 mm Hg or higher, and Paco2, 45 mm Hg or less
Interventions: 1) Dependant interventions: Administer medications and assess the medication effects. Independent intervention: Assess patients: intake and output; weight; lung sounds; vital signs; skin turgor and mucous membranes. Assess patient for JVD, edema and signs/symptoms of fluid overload. Monitor oximetry and ABG values and report significant findings. Rationale: oximetry of 92% or less and the presence of hypoxemia (decreased Pao2) and hypercapnia (increased Paco2) signify decreased oxygenation. The presence of crackles may signify alveolar fluid congestion and systolic dysfunction (left sided) heart failure. Decreased breath sounds signify fluid overload or decreased ventilation. Independent interventions: 2) Assess lungs sounds q 4 hrs Count apical pulse rate q 4 hrs Assist patient into high fowlers position with the HOB up 90 degrees. Rationale: Reduce workload of heart; increase the force and efficiency of myocardial contraction. These anatomical positions facilitate ease of breathing & promote rest. This position decreases work of breathing, reduces cardiac workload, and prompts gas exchange. These are signs of increasing respiratory distress that require prompt intervention. 3) Independent intervention: Assess general appearance for weakness, fatigue, edema q shift and prn. Keep head of bed elevated Monitor fluid intake, restrict sodium intake as ordered. Monitor Lab work; K+, NA, BUN, Creatinine Teach patient about medications and activity restrictions. Teach the importance of fluid and sodium restrictions.
ND2) Fluid volume excess as evidenced by edema. Dyspnea on exertion (DOE): c/o shortness of breath with mild exertion.
Explain measures that can be taken to treat or prevent excess fluid volume by discharge. Demonstrate adequate tissue perfusion until discharge. Short term goal: Lungs clear to auscultation by time of Discharge
ND3) Decreased cardiac output. Ineffective tissue Perfusion, as evidenced by edema in extremities.
Short term goal: Describe symptoms that indicate the need to consult with health care provider by the end of the AM assessment. By the end of the AM assessment, patient will identify
Keep the client warm and have the client wear socks and shoes when
NURSING CARE PLAN
Page 6 of 7 changes in lifestyle needed to increase tissue perfusion. Long term goal: Client will have Adequate cardiac output Client will be able to perform/resume ADL without increased exertion.
mobile. DO NOT apply heat Maintains vasodilation and blood supply. Heat can damage ischemic tissues
Rationale: These s/s develop as the heart attempts to compensate for a decreased C.O. w/ resultant decrease in O2 supply to bodys tissues. Reduce workload of heart; increase the force & efficiency of myocardial contraction & eliminate the excessive accumulation of body water by avoiding excess fluid intake; Controlling the diet & monitoring diuretic and angiotensin. Fluid restriction will reduce myocardial workload and sodium restriction will promote excretion of excess fluid. Educate client on the importance of healthy diet in order to keep healthy weight, eat healthy foods like fruits & vegetables, client will be able to reduce BMI, & increase C/O & be more resistant to perform ADL.
NURSING CARE PLAN
Page 7 of 7
Evaluation
(To be completed by faculty only)
Collection of Patient Information: __________________ (25%) Collection of Patients Objective Finding:____________________ (25%) Care Plan Development: ___________________ (50%) Comments:
FINAL GRADE: __________________________ (100%)
NURSING CARE PLAN
También podría gustarte
- CC Concept MapDocumento11 páginasCC Concept Mapapi-546355187Aún no hay calificaciones
- M13 - Solution of TrianglesDocumento5 páginasM13 - Solution of Triangles9703693564Aún no hay calificaciones
- Problem/PICOT/Evidence Search (PPE) Worksheet: Chamberlain College of NursingDocumento3 páginasProblem/PICOT/Evidence Search (PPE) Worksheet: Chamberlain College of NursingWeke-sir CollinsAún no hay calificaciones
- Nursing Research A1Documento12 páginasNursing Research A1Joanna Jaira SalcedoAún no hay calificaciones
- STUDENT-Sepsis - Fundamental - Reasoning Fillable-1Documento5 páginasSTUDENT-Sepsis - Fundamental - Reasoning Fillable-1Laura PoultneyAún no hay calificaciones
- Coronary Artery Disease and HypertensionDocumento8 páginasCoronary Artery Disease and HypertensionsnehaAún no hay calificaciones
- Lydia Hall ReportDocumento21 páginasLydia Hall ReportMia Zendaya100% (1)
- This Study Resource Was: Chamberlain College of NursingDocumento5 páginasThis Study Resource Was: Chamberlain College of NursingHugsAún no hay calificaciones
- Clinical Log Term II PDFDocumento9 páginasClinical Log Term II PDFPriscilla S100% (1)
- Nursing Care PlanDocumento10 páginasNursing Care PlanmariasomorayAún no hay calificaciones
- FrankensteinDocumento24 páginasFrankensteinLisa WardAún no hay calificaciones
- ACTIVITY 1: Nursing Care PlanDocumento4 páginasACTIVITY 1: Nursing Care PlanChelsea JardelezaAún no hay calificaciones
- Case Study No. 11 - Hydroelectric Power Plant in The PhilippinesDocumento26 páginasCase Study No. 11 - Hydroelectric Power Plant in The PhilippinespicefeatiAún no hay calificaciones
- Benefits of Teamwork in NursingDocumento12 páginasBenefits of Teamwork in NursingdatmojoAún no hay calificaciones
- HDL Coder™ ReferenceDocumento487 páginasHDL Coder™ ReferenceVictor Colpo NavarreteAún no hay calificaciones
- ETOH Case StudyDocumento5 páginasETOH Case StudyCharme Jean RaygonAún no hay calificaciones
- VALDEZ - Nursing Process of Diabetes Mellitus PDFDocumento4 páginasVALDEZ - Nursing Process of Diabetes Mellitus PDFDexel Lorren ValdezAún no hay calificaciones
- Release emotions with simple questionsDocumento10 páginasRelease emotions with simple questionsDubravko ThorAún no hay calificaciones
- PATIENT 1 Nursing Assessment FormDocumento5 páginasPATIENT 1 Nursing Assessment FormndemboloveAún no hay calificaciones
- C C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMDocumento4 páginasC C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMjohkieAún no hay calificaciones
- Anemia-Careplan For AdultDocumento29 páginasAnemia-Careplan For AdultdjbhetaAún no hay calificaciones
- Keith RN Asthma Case StudyDocumento16 páginasKeith RN Asthma Case StudyCHARLES MAINAAún no hay calificaciones
- Nursing Care Plan for Stroke PatientDocumento12 páginasNursing Care Plan for Stroke PatientMj WilliamsAún no hay calificaciones
- Transitional Care Case Study-Pulling It All TogetherDocumento13 páginasTransitional Care Case Study-Pulling It All TogethermatthewAún no hay calificaciones
- Reflection QuestionsDocumento21 páginasReflection QuestionsJulia BrownAún no hay calificaciones
- Decision Making, Problem Solving, and Critical Thinking: Requisites For Successful Leadership and ManagementDocumento28 páginasDecision Making, Problem Solving, and Critical Thinking: Requisites For Successful Leadership and Managementkit_dalkis5Aún no hay calificaciones
- Analog To Digital Conversion (ADC)Documento62 páginasAnalog To Digital Conversion (ADC)Asin PillaiAún no hay calificaciones
- Head To Toe Assessment (Elder)Documento2 páginasHead To Toe Assessment (Elder)ZnarfAún no hay calificaciones
- Openstack Deployment Ops Guide PDFDocumento197 páginasOpenstack Deployment Ops Guide PDFBinank PatelAún no hay calificaciones
- Physical Assessment Summary for Weak Hospitalized PatientDocumento3 páginasPhysical Assessment Summary for Weak Hospitalized PatientRijelAún no hay calificaciones
- Alcoholic Liver Cirrhosis Case StudyDocumento26 páginasAlcoholic Liver Cirrhosis Case StudyVin Mamuric Meneses100% (1)
- Life and DeathDocumento23 páginasLife and DeathJea Joel MendozaAún no hay calificaciones
- Electrolyte ImbalanceDocumento4 páginasElectrolyte ImbalanceDoneva Lyn MedinaAún no hay calificaciones
- Nursing Pharmacology: NAME: - BRANCHDocumento4 páginasNursing Pharmacology: NAME: - BRANCHMa-Anne Joyce RodiAún no hay calificaciones
- Leadership & Management in Nursing NCLEX Practice Quiz (80 Questions)Documento38 páginasLeadership & Management in Nursing NCLEX Practice Quiz (80 Questions)Mack MakaAún no hay calificaciones
- Nursing Process Overview: Health Assessment NotesDocumento40 páginasNursing Process Overview: Health Assessment NotesEliakim III InsongAún no hay calificaciones
- Hypovolemic ShockDocumento12 páginasHypovolemic ShockHassanal DimaporoAún no hay calificaciones
- NCPDocumento2 páginasNCPMelissa David100% (1)
- Understand Congestive Heart FailureDocumento5 páginasUnderstand Congestive Heart FailureOanh HoangAún no hay calificaciones
- NCP Acute Pain NCSDocumento3 páginasNCP Acute Pain NCSPaolo Vittorio Perdigueros GonzalesAún no hay calificaciones
- MELD Related Files Liver MELD-PlusDocumento45 páginasMELD Related Files Liver MELD-PlusUKAún no hay calificaciones
- CH 20 Nursing Care of Patients With HIVDocumento2 páginasCH 20 Nursing Care of Patients With HIVZachary T Hall100% (1)
- Decreased Cardiac Output RM 7Documento9 páginasDecreased Cardiac Output RM 7api-283470660Aún no hay calificaciones
- C 13Documento11 páginasC 13Jo100% (1)
- Health PromotionDocumento5 páginasHealth Promotionapi-433917537Aún no hay calificaciones
- Practice Summary Paper For PortfolioDocumento9 páginasPractice Summary Paper For Portfolioapi-290938460Aún no hay calificaciones
- Nursing Diagnosis GuideDocumento9 páginasNursing Diagnosis Guidekhikmatul mu'jizahAún no hay calificaciones
- Chapter 64 - Administration of Injectable MedicationsDocumento11 páginasChapter 64 - Administration of Injectable Medicationskristie donaldAún no hay calificaciones
- PNR Final ExamDocumento18 páginasPNR Final ExaminaderbiAún no hay calificaciones
- Case Study 63 ReportDocumento15 páginasCase Study 63 ReportJadder InnacioAún no hay calificaciones
- Learning Log of Reflective Practice FormDocumento8 páginasLearning Log of Reflective Practice FormTomii HajiAún no hay calificaciones
- P1 MS 3 Nur 200Documento16 páginasP1 MS 3 Nur 200Xandra Joie Ondoy TabotaboAún no hay calificaciones
- FHP (Gordon's Approach) FormatDocumento25 páginasFHP (Gordon's Approach) FormatbereketAún no hay calificaciones
- Anti Neoplastic AgentsDocumento116 páginasAnti Neoplastic AgentsAbii KetiAún no hay calificaciones
- Final Teaching PlanDocumento2 páginasFinal Teaching Planapi-352581650Aún no hay calificaciones
- Concept MapDocumento1 páginaConcept Mapapi-246466200Aún no hay calificaciones
- Nursing Care Plan For Subarachnoid HemorrhagicDocumento2 páginasNursing Care Plan For Subarachnoid HemorrhagicAshram Smart100% (1)
- n360 Concept Map Care Plan Week 3 Sheryl SatoDocumento15 páginasn360 Concept Map Care Plan Week 3 Sheryl Satoapi-283363983Aún no hay calificaciones
- Adult Care Plan Impair Gas ExchangeDocumento2 páginasAdult Care Plan Impair Gas ExchangeVic DangAún no hay calificaciones
- Self Assessment 151Documento8 páginasSelf Assessment 151api-314649823Aún no hay calificaciones
- Bates’ Guide to Physical Examination and History Taking Chapter 16: The Musculoskeletal System MCQDocumento12 páginasBates’ Guide to Physical Examination and History Taking Chapter 16: The Musculoskeletal System MCQmanesAún no hay calificaciones
- Transcultural Nursing - Sas 2Documento3 páginasTranscultural Nursing - Sas 2Allyza Jane SartigaAún no hay calificaciones
- Heart Healthy Lifestyle Lesson Plan For 2817Documento5 páginasHeart Healthy Lifestyle Lesson Plan For 2817api-354388331Aún no hay calificaciones
- A Descriptive Research On The Diocese of Kalookan Salubong Rehabilitation ProgramDocumento78 páginasA Descriptive Research On The Diocese of Kalookan Salubong Rehabilitation ProgramRogerGalangueAún no hay calificaciones
- MS CaseDocumento28 páginasMS CaseJuwaka OsakaAún no hay calificaciones
- Lewis COPD Case StudyDocumento2 páginasLewis COPD Case Studyatarisgurl08Aún no hay calificaciones
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDe EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideAún no hay calificaciones
- Material Safety Data Sheet: Development Associates, IncDocumento3 páginasMaterial Safety Data Sheet: Development Associates, IncDedi MulyadiAún no hay calificaciones
- Analysis I - SyllabusDocumento3 páginasAnalysis I - SyllabusJUan GAbrielAún no hay calificaciones
- Conditional Sentences in NT Greek Ruben VideiraDocumento62 páginasConditional Sentences in NT Greek Ruben Videiraruviso100% (1)
- ICO Basic SyllabusDocumento11 páginasICO Basic SyllabusRaúl Plasencia Salini100% (1)
- IT Technician CVDocumento3 páginasIT Technician CVRavi KumarAún no hay calificaciones
- Atomic Structure - One Shot by Sakshi Mam #BounceBackDocumento231 páginasAtomic Structure - One Shot by Sakshi Mam #BounceBackchansiray7870Aún no hay calificaciones
- Health Benefits of Kidney BeansDocumento17 páginasHealth Benefits of Kidney BeansShyneAneeshAún no hay calificaciones
- Delhi Police ResultDocumento26 páginasDelhi Police ResultExam Aspirant100% (1)
- Sankalp Sanjeevani NEET: PhysicsDocumento11 páginasSankalp Sanjeevani NEET: PhysicsKey RavenAún no hay calificaciones
- Srimanta Shankardev: Early LifeDocumento3 páginasSrimanta Shankardev: Early LifeAnusuya BaruahAún no hay calificaciones
- Iso 696 1975Documento8 páginasIso 696 1975Ganciarov MihaelaAún no hay calificaciones
- BCMEDocumento9 páginasBCMEVenkateshwaran VenkyAún no hay calificaciones
- Limit Switch 1LX7001-J AZBILDocumento8 páginasLimit Switch 1LX7001-J AZBILHoàng Sơn PhạmAún no hay calificaciones
- Manage a micro business with BSB30315Documento3 páginasManage a micro business with BSB30315Theo A W JacksonAún no hay calificaciones
- Thick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHDocumento13 páginasThick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHPrabhu PrasadAún no hay calificaciones
- Stress-Busting Plan for Life's ChallengesDocumento3 páginasStress-Busting Plan for Life's Challengesliera sicadAún no hay calificaciones
- Academic Language Use in Academic WritingDocumento15 páginasAcademic Language Use in Academic WritingDir Kim FelicianoAún no hay calificaciones
- Sri Lanka, CBSLDocumento24 páginasSri Lanka, CBSLVyasIRMAAún no hay calificaciones
- School newspaper report teaches Present PerfectDocumento2 páginasSchool newspaper report teaches Present PerfectMiro MiroAún no hay calificaciones
- Nurses Week Program InvitationDocumento2 páginasNurses Week Program InvitationBenilda TuanoAún no hay calificaciones
- MUM202001007 - 300 TR Price BOQ ChillerDocumento4 páginasMUM202001007 - 300 TR Price BOQ ChillerB DASAún no hay calificaciones
- The Four Principles of SustainabilityDocumento4 páginasThe Four Principles of SustainabilityNeals QuennevilleAún no hay calificaciones
- Goldenberg and Reddy (2017)Documento10 páginasGoldenberg and Reddy (2017)Mariana ToniniAún no hay calificaciones