Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Fracture Mobility Nursing
Cargado por
Lea TanDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Fracture Mobility Nursing
Cargado por
Lea TanCopyright:
Formatos disponibles
Impaired Physical Mobility Fracture
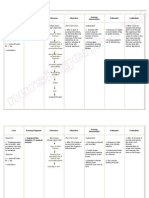
Nursing Diagnosis: Impaired Physical Mobility May be related to Neuromuscular skeletal impairment; pain/discomfort; restrictive therapies (limb immobilization) Psychological immobility Possibly evidenced by Inability to move purposefully within the physical environment, imposed restrictions Reluctance to attempt movement; limited ROM Decreased muscle strength/control Desired Outcomes Regain/maintain mobility at the highest possible level. Maintain position of function. Increase strength/function of affected and compensatory body parts. Demonstrate techniques that enable resumption of activities. Nursing Interventions Rationale Assess degree of immobility Patient may be restricted by selfproduced by injury/treatment and view/self-perception out of note patients perception of proportion with actual physical immobility. limitations, requiring information/interventions to
Encourage participation in diversional/recreational activities. Maintain stimulating environment, e.g., radio, TV, newspapers, personal possessions/pictures, clock, calendar, visits from family/friends. Instruct patient in/assist with active/passive ROM exercises of affected and unaffected extremities. Encourage use of isometric exercises starting with the unaffected limb.
promote progress toward wellness. Provides opportunity for release of energy, refocuses attention, enhances patients sense of selfcontrol/self-worth, and aids in reducing social isolation.
Provide footboard, wrist splints, trochanter/hand rolls as appropriate.
Increases blood flow to muscles and bone to improve muscle tone, maintain joint mobility; prevent contractures/atrophy and calcium resorption from disuse Isometrics contract muscles without bending joints or moving limbs and help maintain muscle strength and mass. Note: These exercises are contraindicated while acute bleeding/edema is present. Useful in maintaining functional position of extremities, hands/feet, and preventing complications (e.g., contractures/footdrop).
Place in supine position periodically if possible, when traction is used to stabilize lower limb fractures. Instruct in/encourage use of trapeze and post position for lower limb fractures.
Reduces risk of flexion contracture of hip.
Assist with/encourage self-care activities (e.g., bathing, shaving).
Provide/assist with mobility by means of wheelchair, walker, crutches, canes as soon as possible. Instruct in safe use of mobility aids.
Facilitates movement during hygiene/skin care and linen changes; reduces discomfort of remaining flat in bed. Post position involves placing the uninjured foot flat on the bed with the knee bent while grasping the trapeze and lifting the body off the bed. Improves muscle strength and circulation, enhances patient control in situation, and promotes self-directed wellness. Early mobility reduces complications of bed rest (e.g., phlebitis) and promotes healing and normalization of organ function. Learning the correct way to use aids is important to maintain
Monitor blood pressure (BP) with resumption of activity. Note reports of dizziness.
Reposition periodically and encourage coughing/deepbreathing exercises. Auscultate bowel sounds. Monitor elimination habits and provide for regular bowel routine. Place on bedside commode, if feasible, or use fracture pan. Provide privacy.
Encourage increased fluid intake to 20003000 mL/day (within cardiac tolerance), including acid/ash juices.
optimal mobility and patient safety. Postural hypotension is a common problem following prolonged bed rest and may require specific interventions (e.g., tilt table with gradual elevation to upright position). Prevents/reduces incidence of skin and respiratory complications (e.g., decubitus, atelectasis, pneumonia). Bed rest, use of analgesics, and changes in dietary habits can slow peristalsis and produce constipation. Nursing measures that facilitate elimination may prevent/limit complications. Fracture pan limits flexion of hips and lessens pressure on lumbar region/lower extremity cast. Keeps the body well hydrated, decreasing risk of urinary infection, stone formation, and constipation
Provide diet high in proteins, carbohydrates, vitamins, and minerals, limiting protein content until after first bowel movement.
Increase the amount of roughage/fiber in the diet. Limit gas-forming foods.
Consult with physical/occupational therapist and/or rehabilitation specialist.
In the presence of musculoskeletal injuries, nutrients required for healing are rapidly depleted, often resulting in a weight loss of as much as 20/30 lb during skeletal traction. This can have a profound effect on muscle mass, tone, and strength. Note: Protein foods increase contents in small bowel, resulting in gas formation and constipation. Therefore, gastrointestinal (GI) function should be fully restored before protein foods are increased. Adding bulk to stool helps prevent constipation. Gas-forming foods may cause abdominal distension, especially in presence of decreased intestinal motility. Useful in creating individualized activity/exercise program. Patient may require long-term assistance with movement, strengthening,
Initiate bowel program (stool softeners, enemas, laxatives) as indicated. Refer to psychiatric clinical nurse specialist/therapist as indicated.
and weight-bearing activities, as well as use of adjuncts, e.g., walkers, crutches, canes; elevated toilet seats; pickup sticks/reachers; special eating utensils. Done to promote regular bowel evacuation. Patient/SO may require more intensive treatment to deal with reality of current condition/prognosis, prolonged immobility, perceived loss of control.
! ! !
Risk for Trauma Fracture
Nursing Diagnosis: Risk for Trauma Risk factors may include Loss of skeletal integrity (fractures)/movement of bone fragments
Desired Outcomes Maintain stabilization and alignment of fracture(s). Display callus formation/beginning union at fracture site as appropriate. Demonstrate body mechanics that promote stability at fracture site. Nursing Interventions Rationale Maintain bed rest/limb rest as Provides stability, reducing indicated. Provide support of possibility of disturbing joints above and below fracture alignment/muscle spasms, which site, especially when enhances healing moving/turning. Place a bedboard under the Soft or sagging mattress may mattress or place patient on deform a wet (green) plaster cast, orthopedic bed. crack a dry cast, or interfere with pull of traction. Support fracture site with Prevents unnecessary movement pillows/folded blankets. Maintain and disruption of alignment. Proper neutral position of affected part placement of pillows also can with sandbags, splints, trochanter prevent pressure deformities in the roll, footboard. drying cast. Use sufficient personnel for Hip/body or multiple casts can be turning. Avoid using abduction extremely heavy and cumbersome. bar for turning patient with spica Failure to properly support limbs in cast. casts may cause the cast to break.
Evaluate splinted extremity for resolution of edema.
Maintain position/integrity of traction
Ascertain that all clamps are functional. Lubricate pulleys and check ropes for fraying. Secure and wrap knots with adhesive tape.
Coaptation splint (e.g., JonesSugar tong) may be used to provide immobilization of fracture while excessive tissue swelling is present. As edema subsides, readjustment of splint or application of plaster/fiberglass cast may be required for continued alignment of fracture. Traction permits pull on the long axis of the fractured bone and overcomes muscle tension/shortening to facilitate alignment and union. Skeletal traction (pins, wires, tongs) permits use of greater weight for traction pull than can be applied to skin tissues. Ensures that traction setup is functioning properly to avoid interruption of fracture approximation.
Keep ropes unobstructed with weights hanging free; avoid lifting/releasing weights.
Assist with placement of lifts under bed wheels if indicated.
Position patient so that appropriate pull is maintained on the long axis of the bone. Review restrictions imposed by therapy, e.g., not bending at waist/sitting up with Buck traction or not turning below the waist with Russell traction. Assess integrity of external Hoffman traction provides fixation device. stabilization and rigid support for fractured bone without use of ropes, pulleys, or weights, thus allowing for greater patient mobility/comfort and facilitating
Optimal amount of traction weight is maintained. Note:Ensuring free movement of weights during repositioning of patient avoids sudden excess pull on fracture with associated pain and muscle spasm. Helps maintain proper patient position and function of traction by providing counterbalance. Promotes bone alignment and reduces risk of complications (e.g., delayed healing/nonunion). Maintains integrity of pull of traction.
Review follow-up/serial x-rays.
Administer alendronate (Fosamax) as indicated.
Initiate/maintain electrical stimulation if used.
!
wound care. Loose or excessively tightened clamps/nuts can alter the compression of the frame, causing misalignment. Provides visual evidence of proper alignment or beginning callus formation/healing process to determine level of activity and need for changes in/additional therapy. Acts as a specific inhibitor of osteoclast-mediated bone resorption, allowing bone formation to progress at a higher ratio, promoting healing of fractures/decreasing rate of bone turnover in presence of osteoporosis. May be indicated to promote bone growth in presence of delayed healing/nonunion.
También podría gustarte
- Mobility Nursing Diagnosis GuideDocumento3 páginasMobility Nursing Diagnosis GuideYan ReyesAún no hay calificaciones
- NCP - Impaired Mobility RT Fracture & TractionDocumento2 páginasNCP - Impaired Mobility RT Fracture & TractionTracy Small100% (4)
- Nursing diagnosis impaired mobilityDocumento2 páginasNursing diagnosis impaired mobilityAi Rou100% (1)
- Impaired Bed MobilityDocumento2 páginasImpaired Bed MobilityMary Louisse LastimadoAún no hay calificaciones
- (NCPS) Impaired Physical Mobility 2Documento2 páginas(NCPS) Impaired Physical Mobility 2roren100% (1)
- NCPDocumento3 páginasNCPeun kyung shinAún no hay calificaciones
- Impaired Physical Mobility RT Neuromuscular Skeletal Impairment.Documento3 páginasImpaired Physical Mobility RT Neuromuscular Skeletal Impairment.Abegail Abaygar100% (2)
- Impaired Physical MobilityDocumento3 páginasImpaired Physical Mobilityvidagurl0% (1)
- NCP For Impaired Physical MobilityDocumento1 páginaNCP For Impaired Physical Mobilityitzme_andreaAún no hay calificaciones
- NCP OrthoDocumento5 páginasNCP OrthoMyluck Elaine Wailan100% (4)
- Activity IntoleranceDocumento2 páginasActivity IntoleranceSenyorita KHaye100% (4)
- NCP Close Complete Fracture Knowledge DeficitDocumento2 páginasNCP Close Complete Fracture Knowledge DeficitArt Christian Ramos0% (1)
- NCP Impaired Physical MobilityDocumento2 páginasNCP Impaired Physical MobilityJohn Michael FernandezAún no hay calificaciones
- NCP-Impaired Physical MobilityDocumento3 páginasNCP-Impaired Physical MobilityradarsoulAún no hay calificaciones
- NCP FractureDocumento2 páginasNCP Fracturemawel50% (2)
- NCP Epidural HemDocumento32 páginasNCP Epidural HemKatrina PonceAún no hay calificaciones
- Orif NCPDocumento1 páginaOrif NCPLighto Ryusaki100% (1)
- NXCP Disturbed Sensory Perception3Documento2 páginasNXCP Disturbed Sensory Perception3marielle_dellaAún no hay calificaciones
- NCP FractureDocumento1 páginaNCP FractureJonathan Bermundo Barba0% (1)
- NCP Fracture Risk For InfectionDocumento3 páginasNCP Fracture Risk For InfectionMiggsAún no hay calificaciones
- ImmobilityDocumento1 páginaImmobilitymicopoliAún no hay calificaciones
- NCP - BedriddenDocumento4 páginasNCP - Bedriddenadelaigner_racho589475% (4)
- Disturbed Sensory PerceptionDocumento3 páginasDisturbed Sensory PerceptionJashtine JingcoAún no hay calificaciones
- Nursing Care Plan Impaired AdjustmentDocumento1 páginaNursing Care Plan Impaired Adjustmentderic100% (2)
- Fracture NCPDocumento4 páginasFracture NCPCharlene Grace ReginoAún no hay calificaciones
- NCP: FracturesDocumento21 páginasNCP: FracturesJavie100% (1)
- Nursing Care Plan for Skin AbscessDocumento1 páginaNursing Care Plan for Skin AbscessKriz_sakuradreamAún no hay calificaciones
- Nursing Care Plan: West Visayas State University College of NursingDocumento4 páginasNursing Care Plan: West Visayas State University College of NursingLizaEllaga100% (1)
- Nursing Care Plan For Hip Fracture Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationDocumento1 páginaNursing Care Plan For Hip Fracture Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationJaylord VerazonAún no hay calificaciones
- NCP PowerlessnessDocumento6 páginasNCP PowerlessnessopxAún no hay calificaciones
- NCP Bed MobilityDocumento1 páginaNCP Bed MobilityDiana Laura Lei100% (2)
- NCPDocumento4 páginasNCPMichelleAún no hay calificaciones
- NCP 2Documento2 páginasNCP 2Neil Abraham Mendoza Lalap100% (2)
- Impaired Physical Mobility...Documento3 páginasImpaired Physical Mobility...Christy BerryAún no hay calificaciones
- NCP For Impaired Physical MobilityDocumento2 páginasNCP For Impaired Physical MobilityFielMendoza0% (1)
- NCP FractureDocumento3 páginasNCP Fracturesarzlasco09Aún no hay calificaciones
- NCP - Risk For InfectionDocumento2 páginasNCP - Risk For InfectionJet Bautista100% (1)
- NCP PottsDocumento3 páginasNCP PottsFenie Jane Quinlat LapastoraAún no hay calificaciones
- Nursing Care Plan for Stroke ClientDocumento2 páginasNursing Care Plan for Stroke ClientGayzel Dela Cruz50% (2)
- Assessment Diagnosis Planning Implimentation Rationale ResponseDocumento4 páginasAssessment Diagnosis Planning Implimentation Rationale Responsekhate fonteAún no hay calificaciones
- Nursing Care Plan Impaire Physical MobilityDocumento2 páginasNursing Care Plan Impaire Physical Mobilityderic90% (10)
- Nursing Care Plan (ImpairedphyssicalDocumento5 páginasNursing Care Plan (ImpairedphyssicalkuroroexileAún no hay calificaciones
- NCP Spiritual DistressDocumento3 páginasNCP Spiritual DistressAngelo ArabejoAún no hay calificaciones
- Activity in Eyes ConceptDocumento2 páginasActivity in Eyes ConceptWiljohn de la CruzAún no hay calificaciones
- NCP SelfMutilationDocumento4 páginasNCP SelfMutilationjhienelAún no hay calificaciones
- NCP Impaired Physical MobilityDocumento2 páginasNCP Impaired Physical MobilityKristine Young0% (1)
- NCP GrievingDocumento3 páginasNCP GrievingAecee Jose-Macayan100% (4)
- NCP Gouty ArthritisDocumento21 páginasNCP Gouty ArthritisArianne Kamille Andes67% (3)
- NCP For FractureDocumento4 páginasNCP For FracturePeejay Padigdig Feliciano100% (2)
- Nursing Care Plan Orthopedic Philipine CenterDocumento4 páginasNursing Care Plan Orthopedic Philipine CenterAnonymous NZTQVgjaAún no hay calificaciones
- NCP - Risk For Peripheral Neurovascular DysfunctionDocumento2 páginasNCP - Risk For Peripheral Neurovascular DysfunctionRene John Francisco50% (4)
- Nursing Care for Impaired Physical MobilityDocumento3 páginasNursing Care for Impaired Physical MobilityMeljonesDaan100% (1)
- Impaired Physical MobilityDocumento3 páginasImpaired Physical MobilityCalimlim Kim100% (1)
- Nursing Care Plan for Patient with Impaired Physical MobilityDocumento4 páginasNursing Care Plan for Patient with Impaired Physical Mobilityssairej06100% (3)
- Impaired Physical MobilityDocumento2 páginasImpaired Physical MobilityAl-Qadry NurAún no hay calificaciones
- Transfer and AmbulationDocumento108 páginasTransfer and AmbulationGladys YaresAún no hay calificaciones
- Discharge Planning InstructionsDocumento3 páginasDischarge Planning Instructionsad3_aaaAún no hay calificaciones
- HEalth Education Plan CVADocumento4 páginasHEalth Education Plan CVAJoenaCoy ChristineAún no hay calificaciones
- FUNDA REVIEW 2 Body MechanicsDocumento27 páginasFUNDA REVIEW 2 Body Mechanicslovie dooAún no hay calificaciones
- Body Mechanics: Fundamental of Nursing IDocumento55 páginasBody Mechanics: Fundamental of Nursing Irlinao100% (3)
- Richard Gutierrez Happy For Girlfriend, GMA Boss: Finally, Forgiveness "Finally, They Were Able To Forgive EachDocumento2 páginasRichard Gutierrez Happy For Girlfriend, GMA Boss: Finally, Forgiveness "Finally, They Were Able To Forgive EachLea TanAún no hay calificaciones
- ArticleDocumento3 páginasArticleLea TanAún no hay calificaciones
- Give ThanksDocumento1 páginaGive ThanksLea TanAún no hay calificaciones
- ArthritisDocumento6 páginasArthritisLea TanAún no hay calificaciones
- Message: Mayor Neil B. CredoDocumento1 páginaMessage: Mayor Neil B. CredoLea TanAún no hay calificaciones
- Intimidated by RobinDocumento2 páginasIntimidated by RobinLea TanAún no hay calificaciones
- An AbandonedDocumento1 páginaAn AbandonedLea TanAún no hay calificaciones
- Twilight (Frontpage)Documento2 páginasTwilight (Frontpage)Lea TanAún no hay calificaciones
- Richard Gutierrez Happy For Girlfriend, GMA Boss: Finally, Forgiveness "Finally, They Were Able To Forgive EachDocumento2 páginasRichard Gutierrez Happy For Girlfriend, GMA Boss: Finally, Forgiveness "Finally, They Were Able To Forgive EachLea TanAún no hay calificaciones
- Celiac DiseaseDocumento60 páginasCeliac DiseaseLea TanAún no hay calificaciones
- Rationale For Tobacco Use As A Risk Factor For Chronic DiseaseDocumento2 páginasRationale For Tobacco Use As A Risk Factor For Chronic DiseaseLea TanAún no hay calificaciones
- Rationale For Tobacco Use As A Risk Factor For Chronic DiseaseDocumento2 páginasRationale For Tobacco Use As A Risk Factor For Chronic DiseaseLea TanAún no hay calificaciones
- RiverDocumento1 páginaRiverLea TanAún no hay calificaciones
- Aaron AbstractDocumento1 páginaAaron AbstractLea TanAún no hay calificaciones
- Resume StudentUniverse 1Documento5 páginasResume StudentUniverse 1Lea TanAún no hay calificaciones
- Grade 5 BarriosDocumento1 páginaGrade 5 BarriosLea TanAún no hay calificaciones
- Valeriano V. Lopez JR., MD, MPH, MhaDocumento1 páginaValeriano V. Lopez JR., MD, MPH, MhaJess L PayagAún no hay calificaciones
- ItDocumento1 páginaItLea TanAún no hay calificaciones
- Bullying 1Documento6 páginasBullying 1Lea TanAún no hay calificaciones
- 25 Things That Happen Inside Your Body When You SmokeDocumento6 páginas25 Things That Happen Inside Your Body When You SmokeLea TanAún no hay calificaciones
- Municipality of DAUINDocumento5 páginasMunicipality of DAUINLea TanAún no hay calificaciones
- Posted An Instagram Photo of Himself Kissing The Actress On The Cheek. The Other Photo Luis PostedDocumento1 páginaPosted An Instagram Photo of Himself Kissing The Actress On The Cheek. The Other Photo Luis PostedLea TanAún no hay calificaciones
- Recommendations:: 1) Promoting Healthy LifestyleDocumento4 páginasRecommendations:: 1) Promoting Healthy LifestyleLea TanAún no hay calificaciones
- Bullying 5 PDFDocumento8 páginasBullying 5 PDFLea TanAún no hay calificaciones
- Lea Luz Marie D. Tan Pastor My StandpointDocumento1 páginaLea Luz Marie D. Tan Pastor My StandpointLea TanAún no hay calificaciones
- Nutritional Status Record: Department of EducationDocumento1 páginaNutritional Status Record: Department of EducationLea TanAún no hay calificaciones
- Ru CopdDocumento18 páginasRu CopdLea TanAún no hay calificaciones
- Nutritional Status Record: Department of EducationDocumento1 páginaNutritional Status Record: Department of EducationLea TanAún no hay calificaciones
- Nutritional Status Record: Department of EducationDocumento1 páginaNutritional Status Record: Department of EducationLea TanAún no hay calificaciones
- Synchronized Natural Incubation by Free-Range Native ChickensDocumento2 páginasSynchronized Natural Incubation by Free-Range Native ChickensFilbert John MillanAún no hay calificaciones
- Unit explores Christian morality and conscienceDocumento1 páginaUnit explores Christian morality and conscienceRose Angela Mislang Uligan100% (1)
- Journal of Alloys and Compounds: Wei Li, Zhijun Xu, Ruiqing Chu, Peng Fu, Guozhong ZangDocumento4 páginasJournal of Alloys and Compounds: Wei Li, Zhijun Xu, Ruiqing Chu, Peng Fu, Guozhong ZangSamah SamahAún no hay calificaciones
- Material Safety Data Sheet - MSDS: Section 1. Chemical Product and Company IdentificationDocumento5 páginasMaterial Safety Data Sheet - MSDS: Section 1. Chemical Product and Company IdentificationPubcrawlAún no hay calificaciones
- Classification of Placenta PDFDocumento5 páginasClassification of Placenta PDFAdarsh jainAún no hay calificaciones
- SHS-Physical Science (Biological Macromolecules) : I-Introductory ContentDocumento13 páginasSHS-Physical Science (Biological Macromolecules) : I-Introductory ContentJane182004Aún no hay calificaciones
- Solution Guide For PpeDocumento45 páginasSolution Guide For PpeTrek Apostol57% (7)
- English Qualification TestDocumento5 páginasEnglish Qualification TestMoh FaisolAún no hay calificaciones
- Polycab HT XlpeDocumento33 páginasPolycab HT Xlpezafrikhan875Aún no hay calificaciones
- Earthbag House For HaitiDocumento22 páginasEarthbag House For HaitiRaymond KatabaziAún no hay calificaciones
- Cardiopulmonary System: Relevant Anatomy & Physiology: HeartDocumento12 páginasCardiopulmonary System: Relevant Anatomy & Physiology: HeartJulia SalvioAún no hay calificaciones
- Mathematics 5 Q1 W10Documento31 páginasMathematics 5 Q1 W10Aices Jasmin Melgar BongaoAún no hay calificaciones
- Applied Acoustics: André M.N. Spillere, Augusto A. Medeiros, Julio A. CordioliDocumento13 páginasApplied Acoustics: André M.N. Spillere, Augusto A. Medeiros, Julio A. CordioliAbdelali MoumenAún no hay calificaciones
- Site Master FileDocumento51 páginasSite Master FileMilonhg100% (2)
- HistorydylaneditDocumento6 páginasHistorydylaneditapi-19858424Aún no hay calificaciones
- M. Valerio Assignment 6.1Documento1 páginaM. Valerio Assignment 6.1Mark Kristian ValerioAún no hay calificaciones
- ASME B31.4-2016 Pipeline Transportation Systems For Liquids and SlurriesDocumento1 páginaASME B31.4-2016 Pipeline Transportation Systems For Liquids and SlurriesJose Rodrigo Salguero DuranAún no hay calificaciones
- Service Manual: EQ1030T47D-820 Light Commercial TruckDocumento175 páginasService Manual: EQ1030T47D-820 Light Commercial TruckYonny ColqueAún no hay calificaciones
- Modicon TM172PDG42R DatasheetDocumento14 páginasModicon TM172PDG42R DatasheetRonnie SolomonAún no hay calificaciones
- Makalah Bahasa Inggris - Narrative TextDocumento21 páginasMakalah Bahasa Inggris - Narrative TextFenny KartikaAún no hay calificaciones
- MICROPAR PPT Group ADocumento43 páginasMICROPAR PPT Group AEben Alameda-PalapuzAún no hay calificaciones
- INChO 2008 Question PaperDocumento23 páginasINChO 2008 Question PaperChaitanya GaurAún no hay calificaciones
- Consumer preference towards branded milk: A comparative analysis of Verka milk and Amul milkDocumento12 páginasConsumer preference towards branded milk: A comparative analysis of Verka milk and Amul milkBhawna RehanAún no hay calificaciones
- 2021 ESC Guidelines For The Diagnosis and Treatment of Acute and Chronic Heart FailureDocumento137 páginas2021 ESC Guidelines For The Diagnosis and Treatment of Acute and Chronic Heart FailuredianAún no hay calificaciones
- DG350 ManualDocumento17 páginasDG350 ManualCareergamingAún no hay calificaciones
- B.pharm Course Handbook 2017 18Documento74 páginasB.pharm Course Handbook 2017 18Md RaquibAún no hay calificaciones
- F588 PDFDocumento8 páginasF588 PDFOscar Gutiérrez-JuncoAún no hay calificaciones
- Technical PaperDocumento6 páginasTechnical PaperSIJO MONACHANAún no hay calificaciones
- Tramadol Drug StudyDocumento1 páginaTramadol Drug Studymilkv82% (11)
- Orrick PostedbyrequestDocumento4 páginasOrrick PostedbyrequestmungagungadinAún no hay calificaciones