Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Clinical Observation On The Management of Insomnia With Single-Finger Pushing Manipulation Plus Medication PDF
Cargado por
tatodo1Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Clinical Observation On The Management of Insomnia With Single-Finger Pushing Manipulation Plus Medication PDF
Cargado por
tatodo1Copyright:
Formatos disponibles
J. Acupunct. Tuina. Sci. 2010, 8 (1): 38-41 DOI: 10.
1007/s11726-010-0038-3
Special Topic Study
Clinical Observation on the Management of Insomnia with Single-finger Pushing Manipulation plus Medication
ZHOU Jing () Tuina Department of Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 201203, P. R. China
60 30 ( P<0. 05) P<0.01 AbstractObjective: To observe the clinical efficacy of treating insomnia with single-finger pushing manipulation. Methods: Sixty patients diagnosed with insomnia were randomized into a treatment group and a control group, 30 subjects in each. The treatment group was treated by single-finger pushing tuina manipulation of inducing yang to yin plus conventional medication, and the control group was prescribed with conventional medication only. The Pittsburgh Sleep Quality Index (PSQI) was adopted to detect the sleep condition before and after treatments. Results: The scores in the treatment group were significantly better than that in the control group (P<0.05), especially the improvement of the score of sleeping medications (P<0.01). Conclusion: The single-finger pushing tuina manipulation of inducing yang to yin can efficiently improve the sleep quality of insomnia patients, and obviously reduce the dose of sleeping medications, making it an ideal non-medication therapy. Key WordsTuina; Massage; Insomnia CLC NumberR246.6 Document CodeA Insomnia refers to a sort of sleep disorder syndrome with disturbance in the onset and maintenance of sleep, which makes the sleep quality insufficient for the body and negatively influences the daily activities of the patients. The increase in medical costs and the decrease in efficiency as a result of poor sleep quality have become a public health problem worldwide. Although there are dozens of sleeping medications commonly used in the clinic, longtime use may cause various side-effects or dependence. This study aimed to observe the improvement of sleep quality in insomnia patients after receiving tuina therapy as well as the conventional medication treatment.
Author ZHOU Jing (1972- ), female, associate chief physician, master of medicine
1 Clinical Data
1.1 Diagnostic criteria The diagnosis of insomnia was referred to the International Classification of Sleep Disorders (ICSD) and International Classification of Diseases, Tenth Revision (ICD-10)[1]. Complaint of difficulty initiating or maintaining sleep with a sleep latency longer than 30 min; this sleep disorder occurred at least 3 times a week, and its duration is longer than 2 weeks; the sleep disturbance has caused obvious pain or had influenced daily activities; there is nothing within everyday activities left unresolved nor any psychological conflict that could be related to insomnia (the fears towards sleep is not included).
38 Shanghai Research Institute of Acupuncture and Meridian and Springer-Verlag Berlin Heidelberg 2010
J. Acupunct. Tuina. Sci. 2010, 8 (1): 38-41
1.2 Inclusion criteria Included subjects should be in accordance with the diagnostic criteria of insomnia; the participants were aged from 18 to 70 years old. However, the gender was not taken into consideration. 1.3 Exclusion criteria The subjects were excluded if one of the following conditions was confirmed. Psychotic patient; the insomnia was induced by drugs or physical illnesses. 1.4 Statistical analysis The statistical analysis was conducted by the SPSS 10.0 software. In the aspect of sleep quality, 7 factors and the final score of PQSI were compared before and after the treatments respectively. The Chi-Square test was used for enumeration data and the t-test for the measurement data. 1.5 General data The 60 participants with insomnia were included from the outpatient, and randomized into 2 groups by the random number table. There were no statistical differences in comparison of gender, duration, and age between the two groups, which made them comparable (table 1).
Table 1. Comparison of the general data between the two groups Groups Treatment Control Gender (male/female) 11/19 9/21 Duration (month) 1315.38 1419.26 Average age (year) 39.63 8.53 38.13 9.99
inducing yang to yin was employed. First, the patient was asked to take a prone position. The physician conducted gun-rolling manipulation on the Governor Vessel and bilateral Bladder Meridian on the back of the patient for 10 min, then, performed ca-wiping manipulation from Dazhui (GV 14) to Changqiang (GV 1) of the Governor Vessel with the index and middle finger 3 times. It was followed by nie-pinching manipulation applied to the Governor Vessel from Changqiang (GV 1) to Dazhui (GV 14) and also the first and second line of the Bladder Meridian 5 times. Afterwards, the patient was asked to change to a supine position with eyes closed and forehead covered by a towel. The physician was on the cephalic side of the patient, performing singlefinger pushing manipulation at Baihui (GV 20) and mo-rubbing manipulation at Yintang (Ex-HN 3) by the index and middle finger, together for about 10 min; the double-finger tui-pushing manipulation was applied to Baihui (GV 20) and Taiyang (ExHN 5) till the patient felt slightly sleepy, and this would take about another 10 min. Finally, the single-finger pushing manipulation was performed at Jingming (BL 1) and along the orbit, together with wiping manipulation on cheeks, forehead and the top of the head for 5 min. Tuina therapy was given once every other day and 10 treatments made up a treatment course. The participants were treated for 2 courses. 2.2 Control group The control group was asked to take Alprazolam 0.4 mg orally every night before sleep.
3 Results 2 Treatment Methods
2.1 Treatment group The treatment group was treated by single-finger pushing tuina manipulation of inducing yang to yin plus medication treatment. 2.1.1 Conventional medication Alprazolam 0.4 mg was taken orally every night before sleep. 2.1.2 Tuina The single-finger pushing tuina manipulation of 3.1 Scoring methods The PSQI was used to detect the sleep quality respectively before treatment and a week after treatment. It took about 5 min each time and was conducted by the same person. 3.2 Treatment results After the treatment, the scores of the sleep quality, sleep latency, sleep duration, sleep efficiency and sleeping medications and the global score in the treatment group had significantly improved
Shanghai Research Institute of Acupuncture and Meridian and Springer-Verlag Berlin Heidelberg 2010 39
J. Acupunct. Tuina. Sci. 2010, 8 (1): 38-41
compared with pre-treatment (P<0.01); the sleep disorder had also improved (P<0.05); and the improvement of daily activities was not statistically significant In the control group, compared with pre-treatment, the global score and all the factors except for daily activities and sleeping medications of post-treatment were better (P<0.05). It indicated that both of the two therapies can improve sleep.
The post-treatment comparison showed that the scores were significantly better in the treatment group than in the control group (P<0.05), especially concerning sleeping medications (P<0.01), which implied that the therapy of tuina plus Alprazolam had a more significant effect in the management of insomnia, and could reduce the dosage of sleeping medications.
Table 2. The comparison of the PSQI scores before and after the treatment between the two groups ( x s) Groups n Time Sleep quality Sleep latency 2.270.83 Sleep duration 1.441.05 Sleep efficiency 1.401.12 Sleep disorder 1.520.59 Sleeping medications 3.000.01 Daily function 2.190.60 Global score 13.935.21
Treatment 30
Before 2.240.55 treatment
Control
After 1.280.801)4) 1.210.761)4) 0.550.631)4) 0.260.511)4) 1.210.492)4) 0.130.481)3) 1.920.604) 9.154.311)4) treatment Before 2.200.85 2.250.89 1.421.15 1.391.17 1.550.73 3.000.00 2.240.44 14.555.17 treatment 30 After 1.740.732) 1.690.862) 0.970.752) 0.780.722) 1.360.582) 3.000.00 2.330.72 11.553.882) treatment
Note: Compared to the pre-treatment in the same group, 1) P<0.01, 2) P<0.05; compared to the control group of post-treatment, 3) P<0.01, 4) P<0.05
4 Discussion
Primary insomnia is a common sleep disturbance, which should include psychophysiological insomnia, subjective insomnia and childhood-onset insomnia approved by a majority of professions[2]. At present, insomnia patients are mainly treated by medication and psychological therapy. However, long-term medication treatment tends to cause addiction, or various levels of adverse effects. A large number of patients fail to adhere to psychotherapy because of its low efficiency, though it has no noted side-effects. In the management of insomnia with singlefinger pushing tuina manipulation of inducing yang to yin plus medication conducted by this study, the results showed that, after 20 treatments, the sleep quality index was significantly lower in the treatment group than in the control group (P<0.05). It implies that tuina plus medication has an advantage in improving sleep quality compared to the mono-conventional-medication therapy, and tuina therapy can notably reduce the using of sleeping medications in insomnia patients. So, besides medication and psychotherapy, as another effective method for treating insomnia, tuina
therapy can not only reduce the using of sleeping medications, but also obtain efficacy in a shorter time-frame, from which the insomnia patients can greatly benefit from if combined with good sleeping patterns. According to traditional Chinese medicine, the disharmony between yang and yin is considered to be the general pathogenesis of insomnia[3]. In the Huang Di Nei Jing (Yellow Emperors Inner Canon), it paid much attention to the interaction between insomnia with the defensive qi when talking about the mechanism of insomnia. It believed that insomnia could be managed when the qi activity was unblocked and it was harmonious and balanced between yin and yang. Performing nie-pinching and gun-rolling manipulation on the Governor Vessel can activate the Wei-Defensive qi resident in the yang meridians[4]. The acupoint Baihui (GV 20) can promote yang qi in the whole body, and performing single-finger pushing manipulation at the point plus the Governor Vessel can bring yang qi into full play. Yintang (Ex-HN 3) is an extra point, but it is located on the passage of the Governor Vessel. Baihui (GV 20) is the meeting point of yang, linking to every part of the whole body. So, an-pressing the two points does not only have a function of sedation
40 Shanghai Research Institute of Acupuncture and Meridian and Springer-Verlag Berlin Heidelberg 2010
J. Acupunct. Tuina. Sci. 2010, 8 (1): 38-41
and soothing the mind, but also can regulate yin and yang, bringing yang qi back into balance to induce yang to yin and to modulate yin and yang. The key point for the manipulation on the head is sedating and soothing the mind. Using single-finger pushing manipulation gently and repeatedly at Yintang (Ex-HN 3), Jingming (BL 1), Taiyang (Ex-HN 5) and Baihui (GV 20) can strengthen the flow of meridian qi. Only when the meridians are unblocked, qi and blood can flow without any obstruction, and the qi, blood and spirit can achieve a good interaction with each other, the mind can be cultivated and the spirit can become calm[5]. Generally speaking, tuina therapy is a safe and efficient method, and can achieve a significant therapeutic effect for treating insomnia when combined with medication treatment, which is worth promoting in primary medical care.
References
[1] WU Ren-gang, ZHANG Chun-gai, DENG Jun. Sleep Behavior and Coping Style in Chronic InsomniasChinese Mental Health Journal, 2003, 17(10): 716. [2] PAN Ji-yang, ZHAO Geng-yuan. Study of the Subjective Sleep Quality and Mental Health Status in the Primary Insomnia PatientsChinese Journal of Nervous and Mental Diseases, 2000, 26(4): 241. [3] YU Xue-qing, CHEN Yu-long. Discussion on the Treatment of Insomnia in Canon of Yellow Emperor. Forum on Traditional Chinese Medicine, 2000, 15(1): 22. [4] HUANG Ying. Clinical Observation on the Management of 37 Insomnia Cases with Tuina plus Moxibustion. Chinese Manipulation & Qi Gong Therapy, 2001, 17(1): 13. [5] WANG Shan, ZHANG Min-shang, WANG Qiu-jing. Acupuncture plus Cephalic Tuina in the Management of 58 Insomnia Cases. Shanghai Journal of Acupuncture and Moxibustion, 2008, 27(11): 23. Translator: HONG Jue () Received Date: December 10, 2009
Shanghai Research Institute of Acupuncture and Meridian
One of the largest research organizations of acupuncture and meridian in China, founded in 1958; Possesses a group of specialists capable of clinical and experimental research, and teaching; Studying in depth acupuncture treatment for diseases of immune, nerve, endocrine, digestive, urinary and genital systems; Undertakes responsibility of WHO research projects and is bed-side teaching unit for domestic and foreign students, visiting scholars, as well as the students for mastership and doctoral; Completed with clinic and research department; Accepts acupuncturists and students aboard majoring in acupuncture for bed-side study and training; send senior doctors abroad have cooperated with public and private medical organizations in Hong Kong, Macao, Taiwan, and so on. Address: No.650, South Wanping Road, Shanghai 200030, P. R. China Phn: 0086-021-64382190 Email: zjtnyx@126.com
Shanghai Research Institute of Acupuncture and Meridian and Springer-Verlag Berlin Heidelberg 2010 41
También podría gustarte
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Saudi Council ExaminationDocumento15 páginasSaudi Council Examinationdedxdreamth95% (40)
- Professor Li Ding Way of Examining Points and Regulating Qi and Acupuncture PDFDocumento4 páginasProfessor Li Ding Way of Examining Points and Regulating Qi and Acupuncture PDFtatodo1Aún no hay calificaciones
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- * 通讯作者:cxb13633227588@ 126. com, 18931258090Documento4 páginas* 通讯作者:cxb13633227588@ 126. com, 18931258090tatodo1Aún no hay calificaciones
- Effect of Different Wavelengths On Superoxide Dismutase: Research ArticleDocumento3 páginasEffect of Different Wavelengths On Superoxide Dismutase: Research Articletatodo1Aún no hay calificaciones
- Allergic Treatment in Taiwan PDFDocumento3 páginasAllergic Treatment in Taiwan PDFtatodo1Aún no hay calificaciones
- Case Report of Three Patients With Wei-Flaccidity Syndrome Cured by Acupuncture-Moxibustion Therapy PDFDocumento3 páginasCase Report of Three Patients With Wei-Flaccidity Syndrome Cured by Acupuncture-Moxibustion Therapy PDFtatodo1Aún no hay calificaciones
- Clinical Observation On Suspended Moxibustion at Baihui (GV 20) For Insomnia PDFDocumento2 páginasClinical Observation On Suspended Moxibustion at Baihui (GV 20) For Insomnia PDFtatodo1Aún no hay calificaciones
- Terumo PenpolDocumento6 páginasTerumo PenpolJhony SebanAún no hay calificaciones
- Approved Moh Guidelines On Submission of Documentation For Registration of Human Pharmaceutical Products RwandaDocumento436 páginasApproved Moh Guidelines On Submission of Documentation For Registration of Human Pharmaceutical Products RwandaAry Bima WinardoAún no hay calificaciones
- You Will (Probably) Survive Chapter SamplerDocumento28 páginasYou Will (Probably) Survive Chapter SamplerAllen & Unwin100% (1)
- Radiopharmaceuticals & Nuclear PharmacyDocumento39 páginasRadiopharmaceuticals & Nuclear PharmacyKhalid HussainAún no hay calificaciones
- Post Dam and Relief Chamber FullDocumento35 páginasPost Dam and Relief Chamber FullnaomiAún no hay calificaciones
- Spinal Healthcare Rehab - Propsal 2.5 Professional AdvisorDocumento23 páginasSpinal Healthcare Rehab - Propsal 2.5 Professional AdvisorInternational Homeopathic Medical SocietyAún no hay calificaciones
- Abstracts and Proceedings WDSC 2009Documento110 páginasAbstracts and Proceedings WDSC 2009Rajasree KarunamoorthyAún no hay calificaciones
- PIL 18047 LatestDocumento2 páginasPIL 18047 LatestWendy EscalanteAún no hay calificaciones
- Silver Is The New BlackDocumento30 páginasSilver Is The New BlackSeptriyani KaswindiartiAún no hay calificaciones
- A Compendium of Tranfusion Prectice Guidelines ARC Edition 4.0 Jan 2021Documento75 páginasA Compendium of Tranfusion Prectice Guidelines ARC Edition 4.0 Jan 2021H Stuard B CocAún no hay calificaciones
- B.pharmacy AyurvedaDocumento55 páginasB.pharmacy Ayurvedapokeman693Aún no hay calificaciones
- DMDS MSDSDocumento11 páginasDMDS MSDSamirhosseine00Aún no hay calificaciones
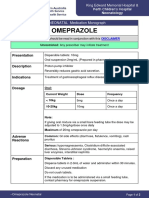
- OmeprazoleDocumento2 páginasOmeprazolephawphawphawAún no hay calificaciones
- PackagingDocumento29 páginasPackagingSagar TummaAún no hay calificaciones
- John O. Agwunobi MD Mba MPHDocumento1 páginaJohn O. Agwunobi MD Mba MPHStalyn DíazAún no hay calificaciones
- Rose Pharmacy JaipurDocumento6 páginasRose Pharmacy JaipurAmit KochharAún no hay calificaciones
- AntiepilepticiDocumento29 páginasAntiepilepticiIskraAún no hay calificaciones
- Social and Psychological Manipulation PDFDocumento287 páginasSocial and Psychological Manipulation PDFNicolae BeianAún no hay calificaciones
- Nursing Practice IDocumento45 páginasNursing Practice IWilmaBongotanPadawilAún no hay calificaciones
- History Taking and MSE AIIMS PatnaDocumento34 páginasHistory Taking and MSE AIIMS PatnaShivendra Kumar100% (1)
- Alprazolam Effect On ThyroidDocumento7 páginasAlprazolam Effect On ThyroidswatiAún no hay calificaciones
- Hostel Prospectus BookletDocumento12 páginasHostel Prospectus BookletsansharmajsAún no hay calificaciones
- WC500059147 PDFDocumento140 páginasWC500059147 PDFAnaStankovićAún no hay calificaciones
- Research ProposalDocumento25 páginasResearch ProposaladerindAún no hay calificaciones
- 2022 Society of Critical Care Medicine Clinical.15Documento37 páginas2022 Society of Critical Care Medicine Clinical.15diegorojasAún no hay calificaciones
- Sebaceous CystDocumento4 páginasSebaceous CystristaniatauhidAún no hay calificaciones
- Pressure TestDocumento9 páginasPressure Testwferry27100% (1)
- 24 Stem Cell Therapy in Neurological Disorders 4th EditionDocumento362 páginas24 Stem Cell Therapy in Neurological Disorders 4th EditionIbraaheem RafeeuAún no hay calificaciones
- Article 007Documento6 páginasArticle 007Dyah Putri Ayu DinastyarAún no hay calificaciones