Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Principles of Bacterial Infections and Anti-Infectives: Cause, Pathogenicity, and Virulence
Cargado por
jheannie02Descripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Principles of Bacterial Infections and Anti-Infectives: Cause, Pathogenicity, and Virulence
Cargado por
jheannie02Copyright:
Formatos disponibles
Principles of Bacterial Infections and Anti-Infectives: Cause, Pathogenicity, and Virulence
Bacterial infections are caused by micro-organisms, generally referred to as pathogens. In order for pathogens to infect an individual, they must first find a method of entering the body, such as: 1. 2. 3. 4. A break in skin integrity Inhalation into the lungs Ingestion of a contaminated substance Contact with mucous membranes
Two important factors affect a micro-organisms ability to cause infection: 1. 2. Pathogenicity Virulence
Pathogenicity of a micro-organism refers to how quickly the organism can reproduce or multiply, and its ability to avoid the bodys natural defense mechanisms (immune system responses). The virulence of a micro-organism refers to the measurement of the organisms pathogenicity. Some organisms can cause a life-threatening disease even in small numbers. This potential depends on two factors: the organisms invasiveness (ability to grow rapidly) and its toxicity (release of exotoxins andendotoxins).
Principles of Bacterial Infections and Anti-Infectives: Classifications of Pathogens
It is necessary to identify the invading micro-organism to determine which antibiotic drug will be most effective against that pathogen. An antibiotic is usually effective against pathogens with similar classifications. Bacteria are classified according to the structure of their cell wall, shape, or use of oxygen. Cell wall classification: 1. 2. Gram-positive bacteria Gram-negative bacteria
Cellular shape classification: 1. 2. 3. Rod shapes (bacilli) Spherical shapes (cocci) Spiral shapes (spirilla)
Oxygen use classification:
1. 2.
Aerobic (need oxygen) Anaerobic (do not need oxygen)
Principles of Bacterial Infections and Anti-Infectives: Drug Classifications and Mechanisms of Action
Anti-infective drugs treat a multitude of infections, such as viral, parasitic, fungal, or bacterial. Antibiotics are drugs used to treat bacterial infections. Antibiotics are either produced in a laboratory or derived from natural elements taken from micro-organisms used to destroy other infectious pathogens. Drugs are classified either by their chemical class (structure of the antibacterial drug) or pharmacologic classification (how they attack the pathogen). Antibiotic drugs are effective against bacterial infections due to their bacteriostatic or bacteriocidal effect. Bacteriostatic drugs work by slowing down the ability of micro-organisms to grow and multiply. This provides additional time for the bodys immune system to destroy the invading pathogen. Bacteriocidal drugs actually destroy the pathogen. Mechanisms of action of antibiotic drugs include: 1. 2. 3. 4. 5. 6. Inhibiting cell wall synthesis Inhibiting protein synthesis Disrupting cell membrane Inhibiting nucleic acid synthesis Inhibiting metabolic pathways Miscellaneous mechanisms
Principles of Bacterial Infections and Anti-Infectives: Acquired Resistance
Acquired resistance is a term used to describe the current ineffectiveness of an antibiotic against a pathogen that in the past it was able to destroy. As pathogens multiply, they produce mutations (changes in the genetic makeup) of the original bacterial cell. This results in a pathogen that is no longer susceptible to the antibiotic. As these mutations continue to multiply, a person can develop an infection that is considered drug-resistant. The infection that is now resistant to the anti-infective drug can be transmitted from host to host. Infections acquired in the hospital setting are referred to as nosocomial infections or health care associated infections (HAIs). Most often they are from resistant strains of bacterial infections, such as: 1. Methicillin-resistant Staphylococcus aureus (MRSA)
2.
Vancomycin-resistant Enterococcus (VRE)
Principles of Bacterial Infections and Anti-Infectives: C&S Testing and Prophylactic Treatment
To treat a bacterial infection effectively and efficiently, the health care provider must know the causative organism and the anti-infective agent to which that organism is susceptible. If the client is treated with the wrong antibiotic, recovery may be delayed, and the client may also be placed at risk for developing resistant strains of the infection. Culture and sensitivity (C&S) testing is carried out in the laboratory as follows: 1. 2. 3. 4. The bacterium is grown in the laboratory and identified (cultured). Specimens may come from blood, sputum, spinal fluid, urine, stool, or purulent drainage. Once the organism is identified, the lab performs several tests to determine which antibiotic is most effective in killing it (sensitivity). Because sensitivity identification can take several days, the health care provider often prescribes a broad-spectrum antibiotic to avoid delaying treatment. After the organism is determined, the health care provider prescribes a drug, or changes a previously prescribed drug to a narrow-spectrum antibiotic.
Anti-infective agents are often given to prevent infections in high-risk individuals, including clients: 1. 2. 3. 4. 5. 6. 7. 8. With decreased immune response (HIV or AIDS) With deep puncture wounds With a prosthetic heart valve who will be undergoing a surgical or dental procedure (to prevent endocarditis) Undergoing cardiovascular surgery, orthopedic surgery, and any surgery that is related to the alimentary canal (to prevent post-op infections) Who may be traveling to an area where malaria is endemic Who have been in close contact with someone who has tuberculosis or is suspected to have tuberculosis Who are HIV-positive mothers (use of antiretrovirals to prevent infection of the child at birth) With confirmed exposure to HIV-contaminated fluids because of health care work (use of antiretrovirals)
Principles of Bacterial Infections and Anti-Infectives: Host Factors
Host factors must be considered when selecting the right course of antibiotic treatment modalities. Failure to take host factors into account can negatively affect the effectiveness of treatment or delay treatment, both of which can lead to development of resistant strains of infection. Drug dosages may have to be increased, or a change in the choice of an anti-infective drug or route of administration may be needed.
Host factors include: 1. 2. Host defensesClients who have weak immune systems may be prescribed a more aggressive drug regimen or need additional treatment time. Local conditionsCertain infections are difficult to treat based on their location, such as the following: 1. For infections of the central nervous system (CNS), the medication must be able to cross the blood-brain barrier. 2. Inflammation due to injury can make it difficult for anti-infectives to reach targeted sites. 3. Large collections of pus or large hematomas can make it difficult for anti-infectives to reach targeted sites. 4. The location of the pathogen in the cell. Infections located intracellularly are more difficult to treat. Drug allergies AgeDosages may have to be decreased for infants and older adults. PregnancyCertain anti-infectives cross the placenta and may be damaging to the fetus. BreastfeedingCertain antibiotics can be secreted in breast milk.
3. 4. 5. 6.
Urinary Tract and Mycobacterial Infections: Cause and Treatment of Urinary Tract Infections
Click on the picture to enlarge.
Cause of Urinary Tract Infections Urinary tract infections (UTIs) are caused by bacteria that invade the kidneys, ureters, urinary bladder,
and/or urethra. Females are more at risk for acquiring UTIs because the urethra in a female is considerably shorter than the male urethra and is located very close to the anus. Because this area is high in bacteria normally found in the gastrointestinal (GI) tract, the close proximity increases females susceptibility to acquire UTIs. Infections can occur in any part of the urinary tract. Clients frequently complain of dysuria and an increased urge to void, even though only small amounts of urine are produced. They also feel a burning sensation after voiding. Clients with kidney infections may present with nausea, vomiting, chills, acute costovertebral angle, and flank pain. As with any infection, the client may experience a fever. You should complete a urinalysis to confirm a urinary tract infection and the causative organism. Treatment Considerations The drug of choice to treat a urinary tract infection is based on the severity of the infection, underlying comorbid conditions, population to treat, and frequency of occurrence. Choice of pharmacotherapy is based on the following circumstances: 1. 2. 3. 4. 5. 6. Acute uncomplicated cystitis Complicated urinary tract infections Urinary infections in infants and children Urinary infections in pregnant women Urinary infections in older adults Recurring urinary tract infections
Urinary Tract and Mycobacterial Infections: Drugs for Urinary Tract Infections
Sulfonamides Sulfonamides are antibacterial drugs in the pharmacologic class of folic acid inhibitors. They are effective as broad-spectrum antibiotics to treat urinary tract infections. Sulfonamides are active against both gram-positive and gram-negative pathogens. They stop the growth of bacteria by suppressing folic acid synthesis, so they are considered bacteriostatic. Common adverse effects of these drugs include nausea, vomiting, anorexia, rash, and crystalluria. Examples of sulfonamides include:
Generic Names sulfadiazine sulfadoxine-pyrimethamine sulfamethoxazole-trimethoprim (SMZ-TMP) sulfisoxazole
Brand Names Microsulfon Fansidar Bactrim, Septra Gantrisin
Routes PO PO PO, IV TMP PO
Urinary Antiseptics Urinary antiseptics are orally administered antibacterial drugs in the pharmacologic class of urinary tract antiseptics. They concentrate in the kidneys without reaching toxic side effects in the blood. Urinary antiseptics are not normally the first drug of choice, but they are highly effective on pathogens that are resistant to SMZ-TMP or the fluoroquinolones. Common adverse effects include headache, rash, nausea, vomiting, and hypersensitivity reactions. Examples of urinary antiseptics and other drugs for UTI include:
Generic Names fosfomycin methenamine hippurate methenamine mandelate nitrofurantoin Monurol
Brand Names
Routes PO PO PO PO
Hiprex, Urex Mandelamine Furadantin, Macrobid, Macrodantin
Urinary Tract and Mycobacterial Infections: Cause and Diagnosis of Tuberculosis
Click on the image to view the video
Mycobacterium tuberculosis is a pathogen responsible for causing tuberculosis (TB). TB is an airborne infection transmitted from host to host through sneezing, coughing, or talking.
TB was nearly eradicated from the United States during the 20th century. However, it resurged from 1985 to 1992 due to an increase in individuals with compromised immune systems, such as those with HIV/AIDS.2 An increase has also been attributed to the large number of individuals immigrating to the United States from countries where TB is endemic. Methods used to diagnose TB include: 1. Tuberculin skin test (purified protein-derivative [PPD]): This test requires an intradermal injection of the purified protein derivative. Injection sites are read within 4872 hours to see if a reaction (induration) has occurred. A positive reaction indicates that the client has been exposed to the infectious pathogen, but does not diagnose the disease.3 Sputum cultures Chest radiography Amplified DNA/RNA tests
2. 3. 4.
Urinary Tract and Mycobacterial Infections: Drugs for Tuberculosis
Click on the picture to enlarge.
Infection with Mycobacterium tuberculosis, the pathogen that causes TB, typically requires antibiotic therapy for a minimum of 612 months. This pathogen has a very thick mycolic acid layer that makes penetration by antibiotics difficult. In some cases, clients may need treatment for up to 2 years, especially those individuals with resistant strains of the infection. Clients are also treated with at least two antibiotics and may be prescribed as many as seven.4 Antibiotics are also prescribed as prophylaxis to prevent infection in individuals who have been in close contact with someone diagnosed with active TB. Clients should have culture and sensitivity (C&S) testing completed before initiating a drug regimen for TB. Because it may take several weeks to get definite results from the C&S testing, treatment begins immediately to prevent further spread of the infectious agent. First-line antituberculosis drugs are considered safer, with less toxicity, than second-line drugs. First-line antituberculosis drugs are administered as follows: 1. Standard regimenThe client is prescribed the following antibiotics for the first 2 months:5
1. 2. 3. 4.
Isoniazid (INH) Rifampin (Rifadin, Rimactane) Pyrazinamide (PZA) Ethambutol (Myambutol)This drug will be stopped if the C&S shows that the first three medications are effective against the strain of infection.
2. Continuation phaseThe client continues with the following medications for another 4 months. Both are taken 23 times per week:6 1. 2. IsoniazidClick to review more about the prototype drug isoniazid. Rifampin
Second-line drugs are prescribed when drug resistance to the first-line drugs has developed. Following is a list of second-line antituberculosis drugs:
Second-Line Drugs aminoglycosides: amikacin (Amikin), kanamycin (Kantrex), streptomycin aminosalicylic acid (Paser)
Routes parenteral
Adverse Effects ototoxicity, kidney impairment
PO
nausea, vomiting, diarrhea, abdominal pain, joint pain, rapid onset of high fever ototoxicity, renal toxicity neurotoxicity nausea, vomiting, diarrhea, abdominal pain, excessive salivation, metallic taste, anorexia, weight loss, seizures Usually used to prevent the possibility of infection with resistant strains of other pathogens
capreomycin (Capastat) cycloserine (Seromycin) ethionamide (Trecator)
IM PO PO
fluoroquinolones: ciprofloxacin (Cipro), ofloxacin (Floxin)
PO
Urinary Tract and Mycobacterial Infections: Tuberculosis Treatment for At-Risk Populations
Some individuals are carefully screened or observed during treatment for potential side effects or noncompliance with the medication regimen. The following are considered at-risk populations for TB treatment: HIV-positive, pregnant, and chemoprophylaxis clients. As a nurse, you should adhere to the following standard protocols for treatment.
HIV-Positive Clients: 1. 2. Clients with HIV should participate in direct observation therapy (DOT) to ensure compliance with the medication regimen. Clients being treated for HIV must be monitored closely for drug-to-drug interactions, because these clients take a significant amount of antiretroviral agents.
Pregnant Clients: 1. 2. 3. For some medications, the safety of the standard TB treatment has not been fully established, or has been found to cause adverse effects to the fetus. Pyrazinamide (PZA) is not always prescribed because the safety of the medication for pregnant women has not been established. Ethambutol (Myambutol) in high doses has been shown to produce birth defects in animals. It is currently prescribed for pregnant women because it has not been demonstrated to cause fetal abnormalities. Streptomycin is not a drug of choice for pregnant women because it has been shown to cause hearing impairment in the child. Mothers can continue with breastfeeding while taking these drugs because no adverse effects have been noted.
4. 5.
Chemoprophylaxis Clients: Individuals in high-risk categories are often prescribed treatment for TB. However, because treatment for TB is very costly and can have some significant adverse effects, not everyone suspected to have latent TB is treated. Treatment for TB is typically given to the following high-risk individuals: 1. 2. 3. 4. 5. 6. Clients with HIV Clients undergoing immunosuppressive therapy People who work or live in nursing homes People in residential facilities (prisoners or AIDS clients) People who have immigrated from countries where TB is endemic People who have been in close contact with someone who has active TB
The drug regimen for prophylaxis treatment includes one of the following:7 1. 2. 3. Isoniazid (9 months) Rifampin and pyrazinamide (2 months) Rifampin (4 months)
Urinary Tract and Mycobacterial Infections: Drugs for Leprosy and MAC Infections
Drugs to Treat Leprosy Mycobacterium leprae is the organism that causes leprosy. Signs and symptoms include macular skin lesions, peripheral nerve paresthesia, and loss of digits. It is believed that leprosy spreads from host to host through the respiratory route, but that theory has not been confirmed. There are two types of leprosy: 1. 2. Lepromatous leprosyThe client with this type of leprosy has an impaired immune system. The disease is progressive and can cause death. TuberculoidleprosyThis type is not as progressive as lepromatous leprosy; there are periods of remission. It is also not usually fatal because the clients immune system is functioning correctly.
Drugs used to prevent resistant strains of leprosy include:8
Type of
Drugs
Regimen
Leprosy lepromatous dapsone (Aczone), clofazimine (Lamprene), rifampin (Rifadin) dapsone, rifampin 25 years
tuberculoid
612 months, and then only dapsone for additional 23 years
Drugs to Treat Mycobacterium Avium Complex Mycobacterium avium complex (MAC) infections are seen in clients with weakened immune systems, especially clients with AIDS and chronic obstructive pulmonary disease (COPD). MAC causes disease conditions of the lungs, and can cause death in those who have AIDS. However, MAC is not considered to be contagious. The MAC pathogen is found in soil and water. After a person is infected, the organism can travel throughout the body to infect any organ. The drug regimen consists of two or three drugs: 1. 2. 3. Macrolide antibiotics: clarithromycin (Biaxin) and azithromycin (Zithromax) Ethambutol (Myambutol) Rifabutin (Mycobutin)
Anti-Infective Drugs: Antibiotics Affecting the Bacterial Cell Wall
Bacteria have cell walls. Bacteria need these walls to contain the high osmotic pressure within the cell. Without the cell wall, the cell would rupture. Because humans do not have cell wall structures, antibiotics can be targeted to kill bacterial cell walls (bacteriocidal). The cell wall also protects the bacterial cell from substances such as antibiotics. Microbial cell wall classifications: 1. 2. Gram-positive cell walls are very thick. Gram-negative cell walls are thinner.
Antibiotics that affect the bacterial cell wall: 1. 2. 3. 4. Penicillins (effective against gram-positive bacteria and some gram-negative bacteria) Cephalosporins (effective against gram-negative bacteria) Carbapenems (broad-spectrum antibiotics) Miscellaneous cell wall inhibitors
Anti-Infective Drugs: Penicillins
Penicillins are antibacterial drugs in the pharmacologic class of cell wall inhibitors. Penicillin was the first antibiotic to be mass produced and was first administered in the 1940s. Penicillins are effective against gram-positive and some gram-negative bacteria. These drugs contain a beta-lactam ring that disrupts the bacteria cell walls peptidoglycan chain. This destroys the bacterial cell wall, leading to the death of the cell (thus, these drugs are bacteriocidal). Adverse effects from penicillins are uncommon. The most common side effects are fever, urticaria, and delayed skin reactions. A serious adverse effect is severe hypersensitivity reaction, such as anaphylactic response. Clients who are allergic to penicillins may also experience crosshypersensitivity with cephalosporins. To learn more: 1. 2. Click to review generic name and brand-name drugs in the various groups of penicillins. Click to review the prototype drug penicillin G potassium (Pfizerpen).
Anti-Infective Drugs: Cephalosporins
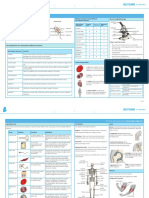
Cephalosporins, the largest group of antibiotics, are included in the pharmacologic class of cell wall inhibitors. They contain a beta-lactam ring that binds to the bacterial cell walls peptidoglycan chain. The diagram on this screen shows the structure of the beta-lactam ring. This ring destroys the bacterial cell wall, leading to the death of the cell (thus, these drugs are bacteriocidal). Cephalosporins are effective against gram-negative infections and for clients with penicillin-resistant infections. They are sometimes given to clients who are allergic to penicillin, although crosssensitivity must be considered. If cephalosporin treatment is sustained for an extended period of time, clients may develop superinfections. The most common complaints are related to diarrhea and skin rashes. Severe hypersensitivity reactions, such as anaphylaxis, are rare. Following are examples of first-, second-, third-, and fourth-generation cephalosporin agents:
Generic Names Brand Names First-Generation Agents cefadroxil cefazolin cephalexin cephradine Duricef Ancef, Kefzol Keflex Velosef
Routes PO IM, IV PO PO
Second-Generation Agents
cefaclor cefotetan cefoxitin cefprozil cefuroxime
Ceclor Cefotan Mefoxin Cefzil Ceftin, Zinacef Omnicef Spectracef Suprax Cefobid Claforan Vantin Fortaz, Tazicef Cedax Cefizox Rocephin Maxipime
PO IM, IV IM, IV PO PO, IM, IV PO PO PO IM, IV IM, IV PO IM, IV PO IM, IV IM, IV IM, IV
Third-Generation Agents
cefdinir cefditoren cefixime cefoperazone cefotaxime cefpodoxime ceftazidime ceftibuten ceftizoxime ceftriaxone
Fourth-Generation Agents
cefepime
Anti-Infective Drugs: Carbapenems and Miscellaneous Cell-Wall Inhibitors
Carbapenems Carbapenems are antibacterial drugs in the pharmacologic class of cell wall inhibitors. They are broad-spectrum antibiotics used to treat most gram-positive and gram-negative pathogens. Carbapenems are effective against both aerobic and anaerobic organisms. Carbapenems contain a beta-lactam ring that makes them bacteriocidal by inhibiting the development of the bacteria cell wall. This eventually leads to the death of the cell. Carbapenems must be administered parenterally. Few adverse effects are associated with carbapenems. The most common are skin rashes, diarrhea, nausea, and thrombophlebitis at the site of injection. Examples of carapenems are:
Generic Names doripenem ertapenem imipenem-cilastatin meropenem
Brand Names Routes Doribax Invanz Primaxin Merrem IV IM, IV IV IV
Miscellaneous Cell Wall Inhibitors Several other cell wall inhibitors have been approved for treatment against resistant microbes. These antibiotics are listed below, along with their adverse effects: 1. 2. 3. Vancomycin hydrochloride (Vancocin): red man syndrome, nausea, rash, fever, and chills. Serious effects include ototoxicity, nephrotoxicity, confusion, seizures, and chills. Aztreonam (Azactam): nausea, vomiting, diarrhea, superinfections, and pain at injection sites. Fosfomycin (Monurol): asthenia, nausea, vomiting, diarrhea, headache, and vaginitis.
Click to review more about the drug vancomycin hydrochloride.
Anti-Infective Drugs: Antibiotics Affecting Bacterial Protein Synthesis
Protein Synthesis Inhibitors Protein constitutes half of the bacterial cell weight. Protein is important to the bacterial cell because it assists substances to move in and out of the cell. Protein is also important for biochemical reactions. Some proteins produce toxins that are toxic to other pathogens and also to host cells. The following antibiotics have a bacteriostatic effect by inhibiting bacterial protein synthesis:
1.
2. 3.
Tetracyclines are effective against aerobic and anaerobic gram-negative and gram-positive pathogens. They are also effective against pathogens resistant to penicillin and other cell wall inhibitors. Macrolides can be prescribed for clients who are allergic to penicillin. They are also effective against gram-positive bacteria. Aminoglycosides are effective against aerobic gram-negative organisms.
Common adverse effects of protein synthesis inhibitors are as follows: 1. 2. 3. Tetracyclines may cause superinfections, nausea, vomiting, diarrhea, epigastric burning, discoloration of teeth, and photosensitivity. Macrolides have GI side effects such as nausea, vomiting, abdominal cramping, and diarrhea. Aminoglycosides may cause ototoxicity, nephrotoxicity, pain and inflammation at the injection site, rash, fever, nausea, diarrhea, dizziness, and tinnitus.
Click to review the generic names and brand names of drugs in the three groups of protein synthesis inhibitors discussed here. Miscellaneous Protein Synthesis Inhibitors Several antibiotics inhibit bacterial protein synthesis, but are limited in use due to the severity of possible adverse reactions. Click to review thesemiscellaneous protein synthesis inhibitors with their corresponding adverse effects.
Anti-Infective Drugs: Fluoroquinolones and Miscellaneous Antibiotics
Fluoroquinolones and Quinolones Quinolones were developed in the early 1960s to treat urinary tract infections. In the late 1980s, quinolones were developed with a fluorine side chain, thus becoming more broad spectrum.1 Fluoroquinolones are in the pharmacologic class of bacterial DNA replication inhibitors. All fluoroquinolones are effective against gram-negative pathogens. Newer drugs are effective against gram-positive pathogens. Fluoroquinolones kill the invading organism and affect DNA synthesis. Their adverse effects may include: 1. 2. 3. 4. 5. 6. 7. Cartilage toxicity GI toxicity, with effects such as nausea, vomiting, and diarrhea; hypersensitivity reactions Cardiotoxicity, with effects such as dysrhythmias Central nervous system toxicity, with symptoms such as headache, dizziness, seizures, hallucinations, confusion, toxic psychoses, and high intracranial pressure Phototoxicity Hepatotoxicity Resistance
Following are first-, second-, third-, and fourth-generation fluoroquinolones and quinolones:
Generic Names First Generation cinoxacin nalidixic acid Second Generation ciprofloxacin norfloxacin ofloxacin Third Generation gatifloxacin levofloxacin Fourth Generation gemifloxacin moxifloxacin
Brand Names Cinobac NegGram Cipro, Proquin XR Noroxin Floxin Zymer Levaquin, Quixin Factive Avelox, Vigamox
Routes PO PO PO PO PO, IV Drops PO, IV PO PO, IV
Click to review the prototype drug ciprofloxacin hydrochloride. Miscellaneous Antibiotics Click to review miscellaneous antibiotics that are not grouped into classes but are extremely effective against specific infections.
Nursing Role: Antibiotic TherapyAssessment and Planning
Assessment It is essential that you complete a health history prior to initiating antibiotic therapy, as follows: 1. Assess for drug allergies and any hypersensitivity reactions that the client may have experienced in the past. Note the prescribed medications that the client is taking, as well as any over-the-counter drugs and use of herbs. To treat the bacterial infection correctly, determine the causative pathogen and the agent(s) to which it is sensitive. Complete a culture and sensitivity test prior to administering the antibiotic. Obtain a baseline set of vitals, as well as blood work that includes WBC. Assess the clients current health status by performing a health assessment focused on the infectious process.
2.
3. 4.
Planning (Client Goals and Expected Outcomes) Work together with the individual to establish client-centered goals and outcomes. For example, the client should: 1. 2. 3. 4. Report any decrease in signs or symptoms related to the infectious process. Be able to discuss side effects and adverse effects of the drugs prescribed. Finish all medications that are prescribed. Notify the health care provider if he or she experiences any signs or symptoms related to a superinfection (sore mouth, vaginal discharge, foul-smelling feces, cough, hairy tongue), as well as any swelling of the face, tongue, or hands; fever or difficulty breathing.
Nursing Role: Antibiotic TherapyImplementation
You should frequently monitor your clients for signs and symptoms related to improvement in the infectious process, adverse effects from drugs, or deterioration of health. Report any change in the clients status to the health care provider. For example, you should:
1. 2. 3. 4. 5. 6. 7.
8. 9. 10. 11. 12. 13. 14. 15. 16. 17.
Watch for signs and symptoms that the clients condition is improving (WBC, vital signs). Observe for hypersensitivity reactions (wheezing, shortness of breath, swelling, fever). Scrutinize the skin for any signs of redness. Notify the health care provider if a rash develops. Observe for signs and symptoms of thrombocytopenia, such as bruising or nose bleeds. Assess for GI distress, such as diarrhea, particularly if it presents with fever. Administer the antibiotic as ordered, to maintain serum therapeutic drug levels. Observe for signs of superinfection (hairy tongue, vaginal discharge, foul-smelling feces, sore mouth). Keep in mind at-risk populations such as children, older adults, and individuals who have weakened immune systems. Check the clients use of over-the-counter medications and herbs, because they may interfere with the effectiveness of the antibiotic. Check that clients who are taking fluoroquinolones are taking their dose with a full glass of water, and that they are drinking several glasses of water throughout the day. Check for redness, swelling, pain, and temperature of the IV site for signs of infection and extravasation. Monitor kidney and liver function tests (monitor I & O). Check for cardiac dysrhythmias and liver impairment for clients who are prescribed fluoroquinolones. Monitor the clients compliance with the medication regimen. Observe for photosensitivity in clients who are prescribed sulfonamides or tetracyclines. Assess bleeding times for clients who are prescribed sulfonamides and are also taking an anticoagulant; they may be at risk for bleeding. Assess blood glucose levels for clients who are prescribed sulfonamides; they can become hypoglycemic. Check for food interactions, such as the following:
Drugs penicillin G
Food Interactions Do not take acidic fruit juices or beverages within one hour of taking the antibiotic, because they can interfere with the drugs effectiveness.9 Avoid alcohol because it can cause severe adverse reactions.
cephalosporins: cefamandole, cefoperazone, and cefotetan tetracyclines
Avoid milk or dairy products within 12 hours of taking the drug, because they interfere with the drugs effectiveness.10
Nursing Role: Antibiotic TherapyClient Education
As a nurse, one of your most important roles in drug therapy is providing education to the client and family. This will help maintain compliance with the drug regimen, improve client safety, and ultimately lead to an improvement in the clients health status. Teach clients to: 1. 2. Contact their health care provider immediately if they notice a negative change in their condition. Notify their health care provider if they develop a rash, diarrhea, fever, or signs of a superinfection (hairy tongue, sore mouth, vaginal discharge, foul-smelling feces). If they are experiencing any diarrhea, instruct them to avoid taking any over-the-counter antidiarrheal medications until they are advised to do so by the health care provider. Report any bleeding immediately, especially if they are taking penicillin, which may cause thrombocytopenia. Complete the full course of antibiotic treatment. Take the medication exactly as instructed to avoid developing a resistant form of the pathogen. Avoid taking over-the-counter medications or herb products until approved by their health care provider; these products can interfere with antibiotic absorption.
3. 4. 5.
6. 7. 8. 9. 10.
11. 12. 13.
Remember that antibiotics interfere with the effectiveness of oral contraceptives; it is necessary to use an additional form of birth control. Avoid alcohol if prescribed a cephalosporin. Avoid acidic fruit juices for at least one hour before and after taking a penicillin antibiotic. Keep well hydrated if prescribed penicillin, cephalosporins, or fluoroquinolones, taking at least 2,0003,000 mL per day of fluid.11 Avoid the sun if taking tetracyclines or sulfonamides; these drugs put clients at risk for sunburn. Cover the skin when in the sun and wear a sunscreen with a SPF of 15 or greater. Clients who take tetracycline need to avoid the sun for at least several days after completing a course of treatment. Do not consume any milk or dairy products within 12 hours of taking tetracycline.12 Report symptoms related to liver dysfunction (such as pale-colored stools, dark urine, or jaundice) when taking macrolides. Notify their health care provider if they experience a hearing problem, motion sickness, or an unsteady gait when taking aminoglycosides.
Nursing Role: Antituberculosis TherapyAssessment and Planning
Clients who are undergoing antituberculosis drug therapy need to be monitored very closely. Drug regimen compliance is of the upmost importance to avoid the development of resistant strains of the pathogen. During assessment, you should:
1.
2. 3. 4. 5.
Conduct a complete health history. Document any drugs that the client is currently prescribed, and any over-the-counter medicines that he/she takes. Find out if the client has a history of kidney or liver disease. Assess baseline vital signs. Complete a physical examination. Assess diagnostic criteria for TB: positive PPD and positive sputum culture. Assess for lifestyle factors such as alcohol use and alcohol abuse. Also, report if the client has had close contact with anyone who has active TB, or the client has a weakened immune system.
When planning goals and objectives with the client, ask him/her to: 1. 2. Report any visual or hearing disturbances, urination difficulties, and kidney or liver dysfunctions. Remain compliant with the drug regimen throughout the course of treatment.
Nursing Role: Antituberculosis TherapyImplementation and Client Education
Your role as a nurse includes closely monitoring each clients compliance with and understanding of the antituberculosis drug regimen. This includes monitoring adverse drug effects and checking on the clients adherence to dietary restrictions. It also involves helping to meet the clients needs, educating the client, and ultimately helping to improve the clients health status. Implementation When administering antituberculosis drug therapy, you should: 1. 2. 3. Assess closely for liver dysfunction. Observe the client for symptoms related to peripheral tingling or numbness. Monitor what foods the client eats, to prevent palpitations, high blood pressure, or flushing due to consumption of tyramine (found in such foods as aged cheese, beer or red wine, bananas, smoked and pickled fish, and chocolate).
Client Education Instruct the client to do the following while taking antituberculosis drug therapy:
1. 2. 3. 4. 5.
6.
Report any yellowing of the skin or eyes, significant lack of energy, and/or dark urine; these symptoms may indicate hepatic adverse effects. Take vitamin B6 supplements to prevent peripheral neuropathy. Refrain from eating foods that contain tyramine, such as aged cheese, beer and red wine, bananas, chocolate, and smoked and pickled fish. Remember that rifampin may cause harmless red-orange discoloration of body fluids such as urine, feces, saliva, sputum, sweat, and tears. Report the following adverse effects immediately to the health care provider: 1. Changes in vision 2. Urination difficulties 3. Jaundice of the skin or dark urine 4. Fever and/or weakness 5. Side effects associated with the GI tract, auditory changes, and peripheral tingling or numbness Take medications as instructed and keep all follow-up appointments with the health care provider.
También podría gustarte
- Royal Rife - The Cancer Cure That Worked (Barry Lynes, 1987) - 1Documento177 páginasRoyal Rife - The Cancer Cure That Worked (Barry Lynes, 1987) - 1Athina Margatina100% (2)
- The E. Coli Insulin FactoryDocumento7 páginasThe E. Coli Insulin FactoryKEZIAH HERRERA0% (1)
- The Handbook of Colloidal SilverDocumento20 páginasThe Handbook of Colloidal Silveracuario33100% (7)
- Immunocompromised DefinitionDocumento5 páginasImmunocompromised Definitionapi-511284651Aún no hay calificaciones
- Lab 5 Microbiology sbl1023Documento9 páginasLab 5 Microbiology sbl1023api-385038701Aún no hay calificaciones
- Cell TheoryDocumento26 páginasCell Theoryحفيظو عبداللهAún no hay calificaciones
- Central AcademyDocumento17 páginasCentral AcademyKartikey VermaAún no hay calificaciones
- Gunabe ASS1-MID PHARMADocumento19 páginasGunabe ASS1-MID PHARMAnaomie manaliliAún no hay calificaciones
- Bacterial ResistanceDocumento9 páginasBacterial ResistanceShifa RazaAún no hay calificaciones
- The Role of Clinical Pharmacist in Combating Antibiotic ResistanceDocumento4 páginasThe Role of Clinical Pharmacist in Combating Antibiotic ResistanceAnto BijuAún no hay calificaciones
- Antimicrobial DrugsDocumento20 páginasAntimicrobial Drugsnadar shahAún no hay calificaciones
- 1-Intro. Antibiotic Oct 14th 2018-ModifiedDocumento23 páginas1-Intro. Antibiotic Oct 14th 2018-ModifiedLeena AlateeqAún no hay calificaciones
- ANTIMICROBIALS (Israjaved)Documento23 páginasANTIMICROBIALS (Israjaved)Isra JavedAún no hay calificaciones
- L11 Antimicrobial DrugsDocumento22 páginasL11 Antimicrobial DrugsSaadAún no hay calificaciones
- Biology Project XiiDocumento14 páginasBiology Project XiiSagayaraniAún no hay calificaciones
- Anti-Microbial Resistance and PreventionDocumento29 páginasAnti-Microbial Resistance and Preventionmahamoud0% (1)
- Ntibiotic: AntibioticsDocumento14 páginasNtibiotic: AntibioticsVinayKumarAún no hay calificaciones
- Combating Antibiotic Drug Resistance in PakistanDocumento32 páginasCombating Antibiotic Drug Resistance in PakistanSalman KhanAún no hay calificaciones
- SuperbugsDocumento3 páginasSuperbugsMatei BuneaAún no hay calificaciones
- Barron - Midterm Async 1Documento15 páginasBarron - Midterm Async 1naomie manaliliAún no hay calificaciones
- Antimicrobial AgentsDocumento14 páginasAntimicrobial AgentsMay Chelle ErazoAún no hay calificaciones
- Antimicrobial Susceptibility Testing (AST)Documento41 páginasAntimicrobial Susceptibility Testing (AST)summiya100% (1)
- ANTIBIOTICS V (Basics)Documento32 páginasANTIBIOTICS V (Basics)Anamta AshfaqAún no hay calificaciones
- Stages of Infection 2Documento7 páginasStages of Infection 2Karren Taquiqui PleteAún no hay calificaciones
- Bio ProjectDocumento6 páginasBio ProjectAKM KINGAún no hay calificaciones
- Unit 1 Lec InfectiousDocumento11 páginasUnit 1 Lec Infectious2226205Aún no hay calificaciones
- Antibiotic StewardshipDocumento6 páginasAntibiotic Stewardshipkyliever100% (1)
- Clinical Pharmacy of AntibioticsDocumento53 páginasClinical Pharmacy of AntibioticsEkanita DesianiAún no hay calificaciones
- Bio Project Drug Resistance in BacteriaDocumento18 páginasBio Project Drug Resistance in BacteriaAKASH ALAMAún no hay calificaciones
- Advanced Clinical PhamacyDocumento5 páginasAdvanced Clinical Phamacypublic mailAún no hay calificaciones
- PCM Module 5Documento52 páginasPCM Module 5Andrei YabutAún no hay calificaciones
- Bab IDocumento15 páginasBab Ivalentina oliviaAún no hay calificaciones
- Dokumen - Tips Biology Investigatory Project 561e79b91f5a0Documento17 páginasDokumen - Tips Biology Investigatory Project 561e79b91f5a0Upendra LalAún no hay calificaciones
- Created By: Michael Anthony C. Macaballug, R.NDocumento115 páginasCreated By: Michael Anthony C. Macaballug, R.NRubyFranzCabangbang-QuilbanAún no hay calificaciones
- Chapter 043Documento6 páginasChapter 043borisdevic223Aún no hay calificaciones
- SuperbacteriaDocumento2 páginasSuperbacteriacolorful2154Aún no hay calificaciones
- Antibiotic Resistance - 220330 - 161213Documento2 páginasAntibiotic Resistance - 220330 - 161213Kim TaeVAún no hay calificaciones
- Hello Bio InvestDocumento16 páginasHello Bio InvestAadrica WaliaAún no hay calificaciones
- Microbial PathogenicityDocumento22 páginasMicrobial PathogenicityPhiliplukaAún no hay calificaciones
- Pharmacology Unit 2 Antimicrobial DrugsDocumento62 páginasPharmacology Unit 2 Antimicrobial DrugsAsif Ali LashariAún no hay calificaciones
- Project Micro BiologyDocumento37 páginasProject Micro Biologyfawasadekunle111Aún no hay calificaciones
- Key Points Revision: 1 Structure and Classification of BacteriaDocumento17 páginasKey Points Revision: 1 Structure and Classification of Bacteriatarun956519Aún no hay calificaciones
- Guideline Antibiotic RationalDocumento35 páginasGuideline Antibiotic RationalIstianah EsAún no hay calificaciones
- The Study of Drug Resistance in Bacteria Using Antibiotics: June 2019Documento6 páginasThe Study of Drug Resistance in Bacteria Using Antibiotics: June 20197'A'06Aditya BeheraAún no hay calificaciones
- BIOLOGY Practical File For Class 12Documento12 páginasBIOLOGY Practical File For Class 12onlyaimiitAún no hay calificaciones
- Prudent Used of AntibioticsDocumento9 páginasPrudent Used of AntibioticsBintari AnindhitaAún no hay calificaciones
- Laboratory Activity 9 Miley VirusDocumento5 páginasLaboratory Activity 9 Miley VirusJade BalanAún no hay calificaciones
- Antibiotic in BacteriaDocumento28 páginasAntibiotic in BacteriaSanjetha ElangovanAún no hay calificaciones
- 3 Infection and Response ChecklistDocumento4 páginas3 Infection and Response Checklistu19majli0Aún no hay calificaciones
- Introduction To Medical MicrobiologyDocumento9 páginasIntroduction To Medical MicrobiologyIsba Shadai Estrada GarciaAún no hay calificaciones
- BacteriologyDocumento23 páginasBacteriologyCHRISTIAN SIDAYAAún no hay calificaciones
- Biology Project Drug Resistance To BacteriaDocumento6 páginasBiology Project Drug Resistance To BacteriaAyush YadavAún no hay calificaciones
- MICROBIOLOGYDocumento9 páginasMICROBIOLOGYAmr Ramazan IbrahimAún no hay calificaciones
- Mayoclinproc 86 2 013 PDFDocumento12 páginasMayoclinproc 86 2 013 PDFMagdy Ali ELsherbenyAún no hay calificaciones
- Presentation On Antibiotic: By:-Shiv Kumar Roll No. 21 Mba BTDocumento18 páginasPresentation On Antibiotic: By:-Shiv Kumar Roll No. 21 Mba BTAnshuman ParasharAún no hay calificaciones
- Antibiotic Resistance Thesis StatementDocumento6 páginasAntibiotic Resistance Thesis Statementkatelogebellevue100% (2)
- Communicable Disease ReviewerDocumento18 páginasCommunicable Disease ReviewerMicah Jonah Elicaño100% (1)
- Infectious DiseasesDocumento43 páginasInfectious DiseasesClaire SalcedoAún no hay calificaciones
- Pharma (Intro, Penicillins, and Cephalosporins)Documento13 páginasPharma (Intro, Penicillins, and Cephalosporins)Pornillosa, Jenaehl Mikhail S.Aún no hay calificaciones
- BIOLOGYDocumento18 páginasBIOLOGYRavi KumarAún no hay calificaciones
- Microbial ResistanceDocumento16 páginasMicrobial ResistanceDixa MeAún no hay calificaciones
- Antimicrobial Drugs Used in Horses FullDocumento7 páginasAntimicrobial Drugs Used in Horses FullDr. Mahdi DerowAún no hay calificaciones
- Nature's Answer to Viral Threats: Understanding the Potency of Plant-Based AntiviralsDe EverandNature's Answer to Viral Threats: Understanding the Potency of Plant-Based AntiviralsAún no hay calificaciones
- Concise Encyclopedia of Plant PathologyDocumento638 páginasConcise Encyclopedia of Plant Pathologycoloromane67% (3)
- Biofloc Technology Aquaculture Doug ErnstDocumento26 páginasBiofloc Technology Aquaculture Doug ErnstMauricio Núñez100% (3)
- J Cube Aica Laminate 2022 2023 AICAIDDocumento93 páginasJ Cube Aica Laminate 2022 2023 AICAIDAdy SaputroAún no hay calificaciones
- 1 s2.0 S096483051730375X Main PDFDocumento8 páginas1 s2.0 S096483051730375X Main PDFJulián AndrésAún no hay calificaciones
- Endodontic Microbiology Final PPT PresentationDocumento80 páginasEndodontic Microbiology Final PPT PresentationAnji Satsangi100% (2)
- TRU - Volume 3 - Issue 2 - Pages 59-66Documento8 páginasTRU - Volume 3 - Issue 2 - Pages 59-66AmadorRevillaAún no hay calificaciones
- Basic VirologyDocumento25 páginasBasic VirologyIngrid Amadea100% (2)
- Lecture Notes On Human MetabolismDocumento358 páginasLecture Notes On Human MetabolismHai Hoang100% (2)
- Hizami Abdullah 2018 IOP Conf. Ser. Mater. Sci. Eng. 431 062003Documento10 páginasHizami Abdullah 2018 IOP Conf. Ser. Mater. Sci. Eng. 431 062003MOHAMMED HASHIRAún no hay calificaciones
- CBSE Class 11 Biology MCQs - Set 5 PDFDocumento6 páginasCBSE Class 11 Biology MCQs - Set 5 PDFsarimfayyazAún no hay calificaciones
- Dang 2009Documento13 páginasDang 2009EEDIEB Prof. Millton Marques CurvoAún no hay calificaciones
- Introduction of MicrobiologyDocumento9 páginasIntroduction of MicrobiologyRahul PalsAún no hay calificaciones
- Cells and Organisation Knowledge OrganiserDocumento2 páginasCells and Organisation Knowledge OrganiserVeena PurohitAún no hay calificaciones
- Brochure - Distance-TreatmentDocumento1 páginaBrochure - Distance-TreatmentИванАтанасовAún no hay calificaciones
- Cell and Molecular Biology Concepts and Experiments 7th Edition Test Bank Gerald KarpDocumento27 páginasCell and Molecular Biology Concepts and Experiments 7th Edition Test Bank Gerald KarpBernard Dalessio100% (36)
- Ip-Chem 13513Documento70 páginasIp-Chem 13513Brent SebastianAún no hay calificaciones
- Kyusei in USA PDFDocumento183 páginasKyusei in USA PDFBoris JabucaninAún no hay calificaciones
- DMLT Syllabus Final 2022Documento22 páginasDMLT Syllabus Final 2022Manjulata SahooAún no hay calificaciones
- 2315 1 4634 1 10 20160108Documento8 páginas2315 1 4634 1 10 20160108ayuAún no hay calificaciones
- Microbiology Mnemonics: Study Online atDocumento3 páginasMicrobiology Mnemonics: Study Online atKriselda May Torio100% (1)
- MPN TestDocumento30 páginasMPN TestQusay Al MaghayerhAún no hay calificaciones
- Domains & Kingdoms of LifeDocumento14 páginasDomains & Kingdoms of LifeRam Iyer100% (1)
- Chapter 1.0: Biodiversity: of Different Things. A Given AreaDocumento61 páginasChapter 1.0: Biodiversity: of Different Things. A Given AreaNURUL HIDAYAH BINTI SAIFUL ANUAR MoeAún no hay calificaciones
- Nur Zulaikha Yusof Ms083038Documento130 páginasNur Zulaikha Yusof Ms083038Shahrin OmarAún no hay calificaciones
- Research Plan Regional STF 2013Documento5 páginasResearch Plan Regional STF 2013Ivan CabanalanAún no hay calificaciones