Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Ebp Uti
Cargado por
api-234511817Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Ebp Uti
Cargado por
api-234511817Copyright:
Formatos disponibles
Running head: EBN & CAUTIS
Evidence-Based Nursing & Reducing Catheter-Associated Urinary Tract Infections Dana L Knoll Ferris State University
EBN & CAUTIS
Evidence-Based Nursing & Reducing Catheter-Associated Urinary Tract Infections Nursing practice is a constantly evolving profession that all the while keeps one goal in mind: the patient. Nursing in its earliest form was based on the need of physical and emotional comfort for the ill. Nursing as we now know it began in the mid 18th mid 19th century and has continued to establish itself as a professional discipline (Taylor, 2011, p. 7). Within the last 20 years nursing has undergone another change in its practice. Evidence-based practice (EBP), also referred to as evidence-based nursing (EBN) within the profession, has come to the forefront of nursing care. Nursing literature now focuses on research proven best-practices that continue to support the one target of all nursing care, the patient. Evidence-Based Practice In Nursing Although Florence Nightingale referred to nursing research, it was not until a century later that nurses began receiving advanced nursing degrees and developing studies of nursing practices (ANA, 2010, p. 16). This beginning of nursing research in the early 20th century was the beginning of evidence-based practice in nursing. As defined by the American Nurses Association, EBP is A scholarly and systematic problem-solving paradigm that results in the delivery of high-quality health care (2010, p. 65). EBN blends current evidence, practicegenerated data, expertise from a multidisciplinary team and patient values and preferences in an effort to achieve the best possible outcomes for patients (ANA, 2010, p. 16). The current body of research indicates that evidence-based practice, mixed with a good dose of caring, results in improved quality of care for patients thus, less varied and better patient outcomes. History of Urinary Tract Infections Urinary tract infections (UTI) have been recorded throughout history, as far back as ancient Egypt and they continue to be one of the most common infectious diseases to this day
EBN & CAUTIS
(Nickels, 2005). It was not until the mid-19th century that UTI was understood to be the result of microorganisms. Even after knowledge of this microbial etiology, UTIs were not appropriately treated until the early 20th century with the advent of antimicrobial agents. As Nickels perfectly summarizes, management of UTI has evolved from essentially palliative care to an efficient, evidence based strategy (2005). As previously stated, UTI continues to be one of the most prevalent infectious diseases, yet the concern has now shifted to the prevalence of hospital acquired infections (HAI), specifically CAUTI. Catheter-Associated Urinary Tract Infections As defined by the California Department of Public Health (CDPH), a CAUTI is a UTI where an indwelling urinary catheter was in place for >2 days when all elements of the UTI infection criterion were first present together (2013). Approximately 1.7 million patients acquire an HAI and 36% of these infections are catheter-associated urinary tract infections (Finan, 2012). A number of risk factors have been identified, such as age, gender, length of catheterization, diabetes, malnutrition, and fecal incontinence as well as lack of policy/procedure implemented by the facility (CDPH, 2013). Although these risk factors exist, the biggest risk factor seems to be length of catheterization. Statistically, risk for UTI rises to 9.4% if an indwelling catheter remains in place for 2 days and increases by 5% for each day past that (Liljenstolpe, 2013). According to the CDPH CAUTI is the leading cause of secondary bloodstream infection, increases a hospital length of stay 2-4 days and can result in the overuse and resistance of antimicrobial agents. In addition, an estimated 69% of CAUTI can be prevented, approximately 380,000 annually (2013). Naturally, such a high prevalence and risk of complications is concerning, yet the major reason behind action to resolve CAUTIs is a result of payments The Centers for Medicare and Medicaid Services (CMS). As of October 1st, 2008,
EBN & CAUTIS facilities do not receive additional compensation to treat a CAUTI (Finan 2012). This
termination in payment has resulted in an avalanche of research in an effort to find evidencebased practice in decreasing incidence of such HAIs. Evidence-Based Practice To Resolve CAUTI This influx of research has resulted in a mixed bag of techniques and protocols, many of which have been met with some success in reducing CAUTI. The Bladder Bundle is once such protocol, initiated by the Michigan Health and Hospital Association (MHA) that touches on the seemingly overarching themes of most CAUTI prevention recommendations. The five key practices of this protocol are: 1. Nurse-initiated urinary catheter discontinuation protocol. 2. Urinary catheter reminders and removal prompts. 3. Alternatives to indwelling urinary catheterization. 4. Portable bladder ultrasound monitoring. 5. Insertion care and maintenance. (Saint et al, 2009) The first key practice, a nurse controlled catheter discontinuation, eliminates one step of the catheter removal process. According to the CDPH, physicians are frequently unaware of length of catheterization (75%) or even which of their patients are catheterized (>50%) (2013). This is by no means a critique of physician practices, but evidence that nurses are able to alleviate some responsibility from physicians, which will result in better patient care. As previously stated, each day that an indwelling urinary catheter is left in place, risk of bacteriuria increases by 5%, adding up to 100% risk of infection by day 30 (CDPH, 2013). Implementation of catheter reminder and removal prompts will serve as another cue to physicians and/or nurses to reevaluate the current placement of a urinary catheter. This cue may
EBN & CAUTIS
change the length of catheterization from 7 days to 4, 5, or 6 days, thus decreasing the chance of infection. A major factor in CAUTI is inappropriate catheter use. The CDPH estimates that 10 30% of medical surgical, 60 90% of intensive care (ICU) and 5 10% of nursing home patients have a urinary catheter placed. Of the non-ICU patients, 40 50% have no medical/valid indication for urinary catheter use (2013). Facilities need to determine clear protocols and criteria to necessitate insertion of an indwelling catheter. The Center for Disease Control has developed a list of appropriate indications for indwelling urinary catheters. This list should be present in all facilities and protocol developed based upon these appropriate indications. Bladder scanners are used to determine the amount of urine within the bladder. They can measure the amount of urinary retention and determine if decreased urine output is due to urinary retention or simply reduced urine in the bladder (CDPH, 2013). Determining whether urinary retention is an actual issue and how much urinary retention is present can help to decrease the use of indwelling urinary catheters or determine whether a catheter should be used long term or intermittently. Lastly, the catheter insertion and maintenance is of the utmost importance. There are only two sources for bacteria causing a CAUTI: the own patients perineal flora and bacteria on the hands of personnel. Microbes can enter the bladder via the external surface or internal surface of the catheter (CDPH, 2013). Extraluminal contamination implies a breach in the aseptic technique of catheter insertion or improper cleansing of the catheter line post-insertion. Intraluminal contamination indicates a break in the closed drainage line or contamination of the urine collection bag. What all of this indicates is that only trained personnel should be inserting
EBN & CAUTIS
and/or cleaning the catheter and its associated apparatus. Without proper aseptic and cleansing techniques, the catheter can easily be contaminated and bacteria can enter the bladder on the internal or external side of the catheter tubing. In addition to the clear list of Dos, the CDPH also compiled a list of procedures/techniques that have no evidence to support their use in preventing a UTI. These include, Complex urinary drainage systems, routinely changing catheters or drainage bags, routine antimicrobial prophylaxis, cleaning the periurethral area with antiseptics, antimicrobial irrigation of the bladder [and] antiseptic/antimicrobial solution instillation into drainage bags (2013). Conclusion This specific problem of CAUTI lends itself to being a great vessel for nursing driven research. Nurses are the medical personnel most closely taking care of the patients and are in the best position for conducting and monitoring such endeavors. Research continues to grow on a daily basis and thus incidences of such hospital acquired infections decrease. A chain reaction follows so that complications related to CAUTIs decrease, patient hospital length of stay decreases and finally, positive patient outcomes increase. All of the research that may seem to be conducted because of insurance compensation and money is ultimately done for the patient, the number one priority of every nurse.
EBN & CAUTIS References
American Nurses Association. (2010). Nursing scope and standards of practice (2nd ed.). Silver Spring, MD: Nursesbooks.org California Department of Public Health. (2013). Catheter-associated urinary tract infection (CAUTI) prevention: basics of infection prevention 2 day mini-course [Powerpoint slides]. Retrieved from http://www.cdph.ca.gov/programs/hai/Documents/Slide-Set-2-CAUTI-Prevention.pdf Finan, D. (2012). Improving patient outcomes: reducing the risk of CAUTIs. The Kansas Nurse, 87(2), 19 23. Retrieved June 18, 2013, from the Academic OneFile database. Liljenstolpe, S. (2013). Don't skip the SCIP. Arizona Nurse, 66(2), 6. Retrieved June 13, 2013, from the Academic OneFile database. Nickel, J. (2005). Management of urinary tract infections: historical perspective and current strategies: part 1before antibiotics. The Journal of Urology, 173, 21 26. Doi: 10.1097/01.ju.0000141496.59533.b2 Saint, S., et al. (2009). Translating health care-associated urinary tract infection prevention research into practice via the bladder bundle. Joint Commission Journal on Quality and Patient Safety, 35(9), 449-455. Taylor, C. (2011). Introduction to Nursing. Fundamentals of nursing: the art and science of nursing care (7th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.
También podría gustarte
- Apa Qs Theory PaperDocumento5 páginasApa Qs Theory Paperapi-234511817Aún no hay calificaciones
- Essay NursingDocumento5 páginasEssay Nursingapi-520141947Aún no hay calificaciones
- Zurmehly 2018Documento6 páginasZurmehly 2018DavennBacudAún no hay calificaciones
- Nurs 363 Ebp Group Project Final Paper 1Documento11 páginasNurs 363 Ebp Group Project Final Paper 1api-269170045Aún no hay calificaciones
- Nurse-Directed Interventions To Reduce Catheter-Associated Urinary Tract InfectionsDocumento10 páginasNurse-Directed Interventions To Reduce Catheter-Associated Urinary Tract InfectionsAngernani Trias WulandariAún no hay calificaciones
- Galiczewski 2016Documento11 páginasGaliczewski 2016rosarioaliaga2609Aún no hay calificaciones
- science: Auditing Urinary Catheter CareDocumento7 páginasscience: Auditing Urinary Catheter CareNissa ErLinaAún no hay calificaciones
- Reducing UTIs Through Nursing EducationDocumento22 páginasReducing UTIs Through Nursing Educationايمان عمرانAún no hay calificaciones
- Implementing An Evidence-Based Practice Protocol For Prevention of Catheterized Associated Urinary Tract Infections in A Progressive Care UnitDocumento9 páginasImplementing An Evidence-Based Practice Protocol For Prevention of Catheterized Associated Urinary Tract Infections in A Progressive Care UnitLina Mahayaty SembiringAún no hay calificaciones
- Cauti101 508Documento40 páginasCauti101 508Yahia HassaanAún no hay calificaciones
- Clin Infect Dis.-2004-Wilson-1150-8 PDFDocumento9 páginasClin Infect Dis.-2004-Wilson-1150-8 PDFjessicacookAún no hay calificaciones
- Ebp FormativeDocumento12 páginasEbp Formativeapi-288858560Aún no hay calificaciones
- Analisis Jurnal: Disusun Dalam Rangka Memenuhi Tugas Stase Keperawatan DasarDocumento6 páginasAnalisis Jurnal: Disusun Dalam Rangka Memenuhi Tugas Stase Keperawatan DasarNur FitriAún no hay calificaciones
- Nurs490 Cauti Safety Paper NeuburgDocumento17 páginasNurs490 Cauti Safety Paper Neuburgapi-452041818100% (1)
- Runa Debbarma Urinary Tract InfectionDocumento18 páginasRuna Debbarma Urinary Tract InfectionMs Runa DebbarmaAún no hay calificaciones
- Patel 1108 eDocumento12 páginasPatel 1108 eIgnacia VergaraAún no hay calificaciones
- Final Cauti Leadership Analysis Paper Nurs440Documento9 páginasFinal Cauti Leadership Analysis Paper Nurs440api-251662522Aún no hay calificaciones
- Defi of TermsDocumento5 páginasDefi of TermsRazaCreciaLastrillaMenesesAún no hay calificaciones
- Successful Strategy To Decrease Indwelling Catheter Utilization Rates inDocumento7 páginasSuccessful Strategy To Decrease Indwelling Catheter Utilization Rates inWardah Fauziah El SofwanAún no hay calificaciones
- Lab UtiDocumento9 páginasLab UtiAni RahayuAún no hay calificaciones
- Laboratory Diagnosis of Urinary Tract Infections in Adult PatientsDocumento9 páginasLaboratory Diagnosis of Urinary Tract Infections in Adult PatientsTony ZhangAún no hay calificaciones
- Evidence of Self-Directed Learning: 1. Reflection On Ectopic Pregnancy RetrievedDocumento3 páginasEvidence of Self-Directed Learning: 1. Reflection On Ectopic Pregnancy RetrievedJasha MaeAún no hay calificaciones
- Laboratory Diagnosis of Urinary Tract InfectionsDocumento9 páginasLaboratory Diagnosis of Urinary Tract InfectionsArturo OrtúñezAún no hay calificaciones
- Urinary GuidelinesDocumento9 páginasUrinary GuidelinesCabinet VeterinarAún no hay calificaciones
- ASGE Infection Control During GI EndosDocumento10 páginasASGE Infection Control During GI Endosmonir61Aún no hay calificaciones
- Benchmark Capstone Project Change Proposal Week 8Documento15 páginasBenchmark Capstone Project Change Proposal Week 8Kerry-Ann Brissett-SmellieAún no hay calificaciones
- البحث السادس PDFDocumento32 páginasالبحث السادس PDFايمان عمرانAún no hay calificaciones
- WFSA UpdateDocumento60 páginasWFSA UpdateSyaiful FatahAún no hay calificaciones
- A New Point-Of-Care Test For The Rapid Detection of Urinary Tract InfectionsDocumento8 páginasA New Point-Of-Care Test For The Rapid Detection of Urinary Tract InfectionsAntika CahyatiAún no hay calificaciones
- Catheter Associated Urinary Tract Infection Literature ReviewDocumento8 páginasCatheter Associated Urinary Tract Infection Literature Reviewea1yd6vnAún no hay calificaciones
- Catheter Associated Urinary Tract Infections: Running Head: CAUTI Prevention 1Documento4 páginasCatheter Associated Urinary Tract Infections: Running Head: CAUTI Prevention 1api-484953296Aún no hay calificaciones
- Ebp Cauti Research PaperDocumento11 páginasEbp Cauti Research Paperapi-598708595Aún no hay calificaciones
- Sanya Bidla Com MedDocumento20 páginasSanya Bidla Com MedHanzala KhanAún no hay calificaciones
- Laboratory Diagnosis of Urinary Tract Infections in Adult PatientsDocumento9 páginasLaboratory Diagnosis of Urinary Tract Infections in Adult PatientsAngga Krisna ArthaAún no hay calificaciones
- Application of Catheter-Associated Urinary Tract Infection Bundles EssayDocumento26 páginasApplication of Catheter-Associated Urinary Tract Infection Bundles EssayHosam GomaaAún no hay calificaciones
- Early removal of urinary catheter for postnatal patientsDocumento5 páginasEarly removal of urinary catheter for postnatal patientsbernardyauxd_9131424Aún no hay calificaciones
- Ebp Picc Line - RevisedDocumento6 páginasEbp Picc Line - Revisedapi-234544335Aún no hay calificaciones
- Review Higginson PDFDocumento4 páginasReview Higginson PDFSonalManeAún no hay calificaciones
- Intervention To Reduce Catheter-Related Bloodstream Infections in An Intensive Care Unit at A Regional Hospital in Southern TaiwanDocumento2 páginasIntervention To Reduce Catheter-Related Bloodstream Infections in An Intensive Care Unit at A Regional Hospital in Southern TaiwanTessa Elviana SeptiAún no hay calificaciones
- Catheter-Associated Urinary Tract InfectionsDocumento3 páginasCatheter-Associated Urinary Tract InfectionsFernand Son Dela CruzAún no hay calificaciones
- Childhood Intussusceptions at A Tertiary Care Hospital in Northwestern Tanzania: A Diagnostic and Therapeutic Challenge in Resource-Limited SettingDocumento8 páginasChildhood Intussusceptions at A Tertiary Care Hospital in Northwestern Tanzania: A Diagnostic and Therapeutic Challenge in Resource-Limited Settingegi lewisAún no hay calificaciones
- Final Quality Improvement PaperDocumento8 páginasFinal Quality Improvement Paperapi-251822043Aún no hay calificaciones
- Glaser 2017Documento7 páginasGlaser 2017Dicky StefanusAún no hay calificaciones
- Ventilator-Associated Pneumonia Prevention: We Still Have A Long Way To Go!Documento2 páginasVentilator-Associated Pneumonia Prevention: We Still Have A Long Way To Go!AzmachamberAzmacareAún no hay calificaciones
- Cauti PreventionDocumento25 páginasCauti Preventionapi-340511634Aún no hay calificaciones
- Problem StatementoiDocumento4 páginasProblem StatementoiBrian Dreamyeyes KendleyAún no hay calificaciones
- Qi Project FinalDocumento6 páginasQi Project Finalapi-642984838Aún no hay calificaciones
- Articulo en InglesDocumento8 páginasArticulo en Inglesdante yonathan villegas lozanoAún no hay calificaciones
- 10 Mertz ClusterRCThandhygieneDocumento8 páginas10 Mertz ClusterRCThandhygieneEddyOmburahAún no hay calificaciones
- A Nurse-Driven Process For TimelyDocumento7 páginasA Nurse-Driven Process For TimelyWardah Fauziah El SofwanAún no hay calificaciones
- Chapter 1Documento32 páginasChapter 1Robee Camille Desabelle-SumatraAún no hay calificaciones
- 240 Epb PaperDocumento8 páginas240 Epb Paperapi-204875536Aún no hay calificaciones
- Contributing Factors in Increasing Health Care Associated Infection (Hai's) in Phlebitis CasesDocumento8 páginasContributing Factors in Increasing Health Care Associated Infection (Hai's) in Phlebitis CasesJenny MaulidyaAún no hay calificaciones
- Inter Plebitis 1Documento25 páginasInter Plebitis 1Bella FebriantiAún no hay calificaciones
- Nurse Driven Protocols ArticleDocumento7 páginasNurse Driven Protocols ArticlePaolo VegaAún no hay calificaciones
- Jaime 12-12-16Documento15 páginasJaime 12-12-16api-354204098Aún no hay calificaciones
- Abubakar Et Al Sistematic ReviewDocumento35 páginasAbubakar Et Al Sistematic ReviewIrfan MadamangAún no hay calificaciones
- Fundamental Aspects of Infection Prevention and ControlDe EverandFundamental Aspects of Infection Prevention and ControlAún no hay calificaciones
- Post-cholecystectomy Bile Duct InjuryDe EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorAún no hay calificaciones
- Practical Trends in Anesthesia and Intensive Care 2018De EverandPractical Trends in Anesthesia and Intensive Care 2018Aún no hay calificaciones
- NP Autonomy PaperDocumento19 páginasNP Autonomy Paperapi-234511817Aún no hay calificaciones
- Aprn PresentationDocumento12 páginasAprn Presentationapi-234511817Aún no hay calificaciones
- Pico PosterDocumento1 páginaPico Posterapi-234511817Aún no hay calificaciones
- DLK ResumeDocumento1 páginaDLK Resumeapi-234511817Aún no hay calificaciones
- Osp PaperDocumento12 páginasOsp Paperapi-234544335Aún no hay calificaciones
- Ed CLDocumento1 páginaEd CLapi-234511817Aún no hay calificaciones
- 440 SelfassessDocumento20 páginas440 Selfassessapi-234511817Aún no hay calificaciones
- StiflyerDocumento2 páginasStiflyerapi-234511817Aún no hay calificaciones
- Plan FirstDocumento2 páginasPlan Firstapi-234511817Aún no hay calificaciones
- Newborn AssessmentDocumento4 páginasNewborn Assessmentapi-234511817Aún no hay calificaciones
- Ebp Scratch TestDocumento3 páginasEbp Scratch Testapi-234511817Aún no hay calificaciones
- Teen Pregnancy 1Documento10 páginasTeen Pregnancy 1api-238698438Aún no hay calificaciones
- 250 Risk AssessmentDocumento11 páginas250 Risk Assessmentapi-234511817Aún no hay calificaciones
- What Is Hiv/Aids?: Human Immunodeficiency Virus (Hiv)Documento2 páginasWhat Is Hiv/Aids?: Human Immunodeficiency Virus (Hiv)Rockie Geronda EsmaneAún no hay calificaciones
- CytologyDocumento12 páginasCytologyEsther HutagalungAún no hay calificaciones
- Carte EsmoDocumento112 páginasCarte EsmoSabina Alexandra Olan100% (1)
- Valagro Red Kendal RootDocumento2 páginasValagro Red Kendal RooteldhoAún no hay calificaciones
- Witch Hunting in Assam Practices Causes Legal Issues and Challenges by Jehirul Islam and AfruzAra AhmedDocumento11 páginasWitch Hunting in Assam Practices Causes Legal Issues and Challenges by Jehirul Islam and AfruzAra AhmedDaisy GoswamiAún no hay calificaciones
- Lesson PlanDocumento5 páginasLesson Planapi-456870847Aún no hay calificaciones
- AarticuloDocumento6 páginasAarticuloJENNIFER ANDREA OLAYA VARGASAún no hay calificaciones
- Effect of Intravenous Pamidronate Treatment in Children With Osteogenesis ImperfectaDocumento5 páginasEffect of Intravenous Pamidronate Treatment in Children With Osteogenesis Imperfectavikash singhAún no hay calificaciones
- Ageing - Physical and Psychological Changes. Pathological Ageing-11!19!2011Documento4 páginasAgeing - Physical and Psychological Changes. Pathological Ageing-11!19!2011TaylorAún no hay calificaciones
- Pad AbhyangaDocumento7 páginasPad AbhyangaTrusha PatelAún no hay calificaciones
- Chapter 2 RRL Group 4Documento8 páginasChapter 2 RRL Group 4Yuan JimenezAún no hay calificaciones
- Introduction Clinical TrialsDocumento22 páginasIntroduction Clinical TrialsSharadAún no hay calificaciones
- Bailey and Love) Shock Is A LifeDocumento14 páginasBailey and Love) Shock Is A LifeRaghav AgrawalAún no hay calificaciones
- Growing Plants / GerminationDocumento62 páginasGrowing Plants / GerminationJulia Katrina RoxasAún no hay calificaciones
- Reparation, Characterization, and Optimization of Microemulsion For Topical Delivery of ItraconazoleDocumento10 páginasReparation, Characterization, and Optimization of Microemulsion For Topical Delivery of ItraconazoleVeni UNAún no hay calificaciones
- Unveiling Tetanus A Comprehensive Exploration of The Causes Symptoms Prevention and TreatmentDocumento12 páginasUnveiling Tetanus A Comprehensive Exploration of The Causes Symptoms Prevention and TreatmentMikhil mchaeladdictionsAún no hay calificaciones
- Paediatric Examination Handbook 2015Documento66 páginasPaediatric Examination Handbook 2015Ulfa Rahmadanti SetiawanAún no hay calificaciones
- Unit 2 Blood - Body BitsDocumento3 páginasUnit 2 Blood - Body BitsJohnny Miller60% (5)
- Unit VII Mental Health and Mental HealthDocumento13 páginasUnit VII Mental Health and Mental HealthOmprakash Swami89% (9)
- By Dr. James C. Ekwensi, Dr. Thomas Gray, Dr. Abdulhalim Khan, and Khadijat B. MomohDocumento71 páginasBy Dr. James C. Ekwensi, Dr. Thomas Gray, Dr. Abdulhalim Khan, and Khadijat B. MomohChukwu NedumAún no hay calificaciones
- Cardiac MedicationsDocumento8 páginasCardiac Medicationsangeline totaram100% (2)
- Preface - 2017 - Pathologic Basis of Veterinary DiseaseDocumento3 páginasPreface - 2017 - Pathologic Basis of Veterinary DiseaseKamilahAún no hay calificaciones
- Masturbation It Might Feel Good But ItsDocumento7 páginasMasturbation It Might Feel Good But ItsKshivam KhandelwalAún no hay calificaciones
- Caesarean SectionDocumento20 páginasCaesarean Sectionapi-3705046100% (3)
- Sepsis AlgorithmDocumento1 páginaSepsis AlgorithmAshly Nygil100% (1)
- Trauma Recovery and Empowerment ModelDocumento12 páginasTrauma Recovery and Empowerment Modeljimmiefking_64670597Aún no hay calificaciones
- Auto Urine Therapy PDFDocumento130 páginasAuto Urine Therapy PDFBashu Poudel100% (8)
- Pharmacographia IndicaDocumento615 páginasPharmacographia IndicaSatish Vaidya100% (1)
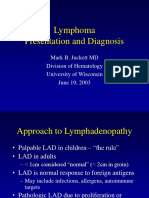
- Lymphoma CancerDocumento34 páginasLymphoma CancerwasihaiderkAún no hay calificaciones
- Deficiency Diseases InformationDocumento4 páginasDeficiency Diseases InformationJasvinder SinghAún no hay calificaciones